Haloperidol for Pain Management: A Narrative Review
Abstract
1. Introduction
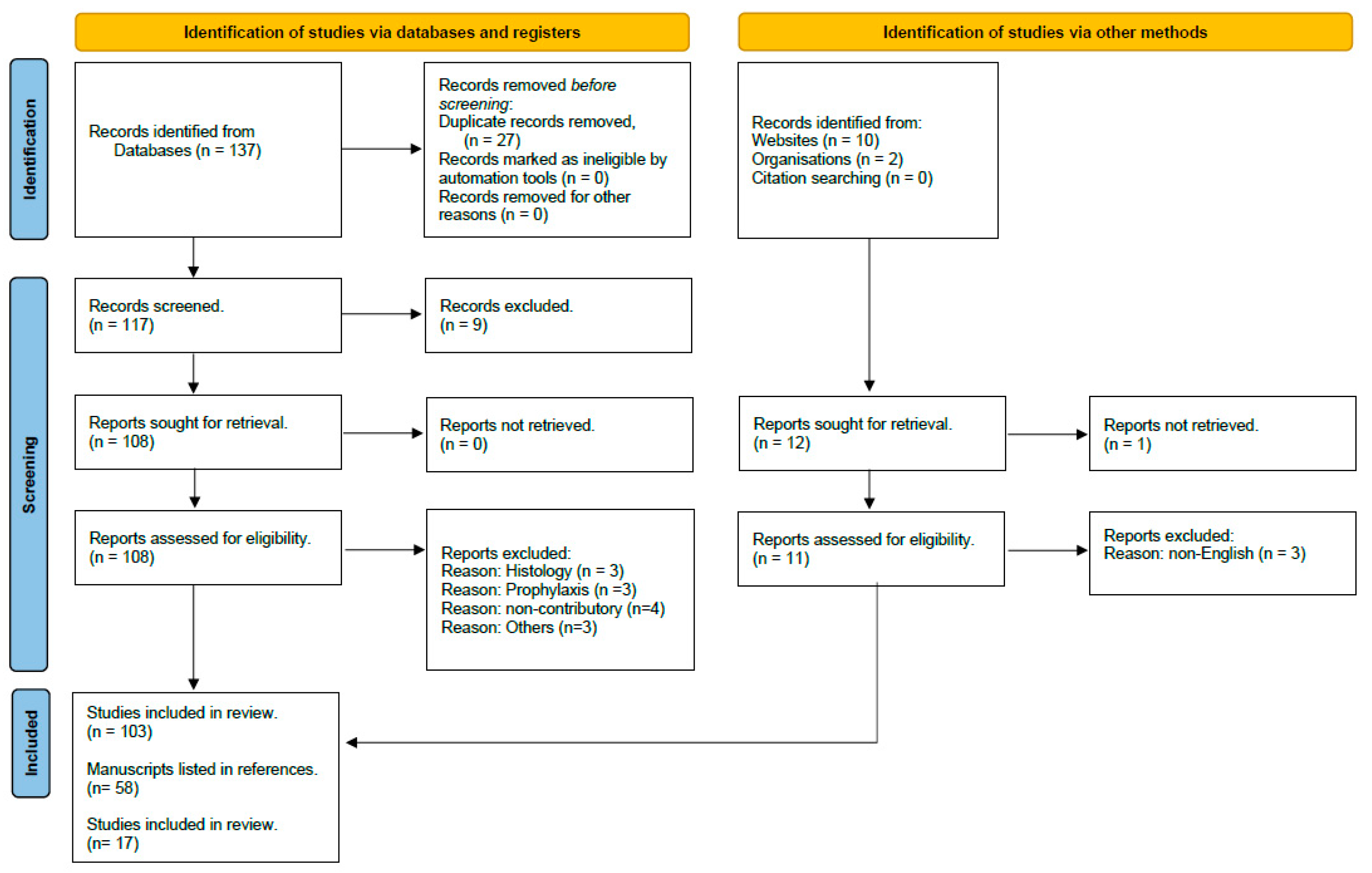
2. Material and Methods
Literature Search
3. Discussion
3.1. Pharmacokinetics and Pharmacodynamics
3.2. Analgesic Mechanisms
4. Review of Clinical Studies
4.1. Haloperidol for Acute Emergency Care Pain Conditions
4.2. Haloperidol for Acute Postoperative Pain Conditions
4.3. Haloperidol for Chronic Pain Conditions
4.4. Incidence of Adverse Effects with Haloperidol
4.5. Future Directions
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dold, M.; Samara, M.T.; Li, C.; Tardy, M.; Leucht, S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst. Rev. 2015, 1, CD009831. [Google Scholar] [CrossRef]
- Gao, K.; Kemp, D.E.; Ganocy, S.J.; Gajwani, P.; Xia, G.; Calabrese, J.R. Antipsychotic-induced extrapyramidal side effects in bipolar disorder and schizophrenia: A systematic review. J. Clin. Psychopharmacol. 2008, 28, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Granger, B.; Albu, S. The haloperidol story. Ann. Clin. Psychiatry 2005, 17, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Granger, B. The discovery of haloperidol. Encephale 1999, 25, 59–66. [Google Scholar]
- Rahman, S.; Marwaha, R. Haloperidol. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK560892/ (accessed on 28 December 2023).
- Baranoglu Kilinc, Y.; Torun, I.E.; Kilinc, E. D2 dopamine receptor-mediated mechanisms of dopaminergic system modulation in in vivo and in vitro experimental models of migraine. Eur. J. Neurosci. 2023, 59, 1177–1193. [Google Scholar] [CrossRef] [PubMed]
- Bauch, E.M.; Andreou, C.; Rausch, V.H.; Bunzeck, N. Neural Habituation to Painful Stimuli Is Modulated by Dopamine: Evidence from a Pharmacological fMRI Study. Front. Hum. Neurosci. 2017, 11, 630. [Google Scholar] [CrossRef]
- Lee, I.S.; Lee, B.; Park, H.J.; Olausson, H.; Enck, P.; Chae, Y. A new animal model of placebo analgesia: Involvement of the dopaminergic system in reward learning. Sci. Rep. 2015, 5, 17140. [Google Scholar] [CrossRef]
- Déciga-Campos, M.; Villafán-Gutiérrez, R.; Espinosa-Juárez, J.V.; Jaramillo-Morales, O.A.; López-Muñoz, F.J. Synergistic interaction between haloperidol and gabapentin in a model of neuropathic nociception in rat. Eur. J. Pharmacol. 2021, 891, 173702. [Google Scholar] [CrossRef]
- Espinosa-Juárez, J.V.; Jaramillo-Morales, O.A.; López-Muñoz, F.J. Haloperidol Decreases Hyperalgesia and Allodynia Induced by Chronic Constriction Injury. Basic. Clin. Pharmacol. Toxicol. 2017, 121, 471–479. [Google Scholar] [CrossRef]
- Kikuchi, N.; Irifune, M.; Shimizu, Y.; Yoshida, K.; Morita, K.; Kanematsu, T.; Morioka, N.; Nakata, Y.; Sakai, N. Selective blockade of N-methyl-D-aspartate channels in combination with dopamine receptor antagonism induces loss of the righting reflex in mice, but not immobility. Psychopharmacology 2015, 232, 39–46. [Google Scholar] [CrossRef]
- Leppert, W.; Okulicz-Kozaryn, I.; Kaminska, E.; Szulc, M.; Mikolajczak, P. Analgesic effects of morphine in combination with adjuvant drugs in rats. Pharmacology 2014, 94, 207–213. [Google Scholar] [CrossRef]
- Mena-Valdés, L.C.; Blanco-Hernández, Y.; Espinosa-Juárez, J.V.; López-Muñoz, F.J. Haloperidol potentiates antinociceptive effects of morphine and disrupt opioid tolerance. Eur. J. Pharmacol. 2021, 893, 173825. [Google Scholar] [CrossRef]
- Petronilho, A.; Reis, G.M.; Dias, Q.M.; Fais, R.S.; Prado, W.A. Antinociceptive effect of stimulating the zona incerta with glutamate in rats. Pharmacol. Biochem. Behav. 2012, 101, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Cooper, I.; Landersdorfer, C.B.; St John, A.G.; Graudins, A. The pharmacokinetics of intranasal droperidol in volunteers characterised via population modelling. SAGE Open Med. 2018, 6, 2050312118813283. [Google Scholar] [CrossRef]
- Mauri, M.C.; Paletta, S.; Maffini, M.; Colasanti, A.; Dragogna, F.; Di Pace, C.; Altamura, A.C. Clinical pharmacology of atypical antipsychotics: An update. EXCLI J. 2014, 13, 1163–1191. [Google Scholar]
- Baldessarini, R. Drugs and the treatment of psychiatric disorders. In The Pharmacological Basis of Therapeutics, 8th ed.; Pergamon Press: Oxford, UK, 1990; pp. 383–435. [Google Scholar]
- Fang, J.; McKay, G.; Song, J.; Remillrd, A.; Li, X.; Midha, K. In vitro characterization of the metabolism of haloperidol using recombinant cytochrome p450 enzymes and human liver microsomes. Drug Metab. Dispos. 2001, 29, 1638–1643. [Google Scholar]
- Murray, M. Role of CYP pharmacogenetics and drug-drug interactions in the efficacy and safety of atypical and other antipsychotic agents. J. Pharm. Pharmacol. 2006, 58, 871–885. [Google Scholar] [CrossRef] [PubMed]
- Spina, E.; de Leon, J. Metabolic drug interactions with newer antipsychotics: A comparative review. Basic. Clin. Pharmacol. Toxicol. 2007, 100, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Lawson, G.M. Monitoring of serum haloperidol. Mayo Clin. Proc. 1994, 69, 189–190. [Google Scholar] [CrossRef]
- Cobos, E.J.; Baeyens, J.M. Use of Very-Low-Dose Methadone and Haloperidol for Pain Control in Palliative Care Patients: Are the Sigma-1 Receptors Involved? J. Palliat. Med. 2015, 18, 660. [Google Scholar] [CrossRef]
- Richelson, E. Receptor pharmacology of neuroleptics: Relation to clinical effects. J. Clin. Psychiatry 1999, 60 (Suppl. S10), 5–14. [Google Scholar] [PubMed]
- Bonifazi, A.; Battiti, F.O.; Sanchez, J.; Zaidi, S.A.; Bow, E.; Makarova, M.; Cao, J.; Shaik, A.B.; Sulima, A.; Rice, K.C.; et al. Novel Dual-Target μ-Opioid Receptor and Dopamine D3 Receptor Ligands as Potential Nonaddictive Pharmacotherapeutics for Pain Management. J. Med. Chem. 2021, 64, 7778–7808. [Google Scholar] [CrossRef]
- Roldan, C.J.; Chambers, K.A.; Paniagua, L.; Patel, S.; Cardenas-Turanzas, M.; Chathampally, Y. Randomized Controlled Double-blind Trial Comparing Haloperidol Combined with Conventional Therapy to Conventional Therapy Alone in Patients with Symptomatic Gastroparesis. Acad. Emerg. Med. 2017, 24, 1307–1314. [Google Scholar] [CrossRef]
- Honkaniemi, J.; Liimatainen, S.; Rainesalo, S.; Sulavuori, S. Haloperidol in the acute treatment of migraine: A randomized, double-blind, placebo-controlled study. Headache 2006, 46, 781–787. [Google Scholar] [CrossRef]
- McCoy, J.J.; Aldy, K.; Arnall, E.; Petersen, J. Treatment of Headache in the Emergency Department: Haloperidol in the Acute Setting (THE-HA Study): A Randomized Clinical Trial. J. Emerg. Med. 2020, 59, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, R.; Stalcup, P.; Croft, B.; Darracq, M.A. Haloperidol undermining gastroparesis symptoms (HUGS) in the emergency department. Am. J. Emerg. Med. 2017, 35, 1118–1120. [Google Scholar] [CrossRef]
- Masoumi, K.; Delirrooyfard, A.; Salehzadeh, M. Comparison of the analgesic effects of haloperidol with or without morphine in patients with acute renal colic: A randomized double-blind clinical trial study. Am. J. Emerg. Med. 2019, 37, 1422–1427. [Google Scholar] [CrossRef]
- Heard, K.; Bebarta, V.S.; Hoppe, J.A.; Monte, A.A. Does administration of haloperidol or ketorolac decrease opioid administration for abdominal pain patients? A retrospective study. Am. J. Emerg. Med. 2020, 38, 517–520. [Google Scholar] [CrossRef]
- Knudsen-Lachendro, K.; Stith, K.; Vicarel, L.A.; Harbert, B.; Fertel, B.S. Study of Haloperidol for Abdominal Pain in the Emergency Department (SHAPE). West. J. Emerg. Med. 2021, 22, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.M.; Moradi, M.M.; Safaie, A.; Baratloo, A.; Payandemehr, P. Sub dissociative dose of ketamine with haloperidol versus fentanyl on pain reduction in patients with acute pain in the emergency department; A randomized clinical trial. Am. J. Emerg. Med. 2022, 54, 165–171. [Google Scholar] [CrossRef]
- Afzalimoghaddam, M.; Edalatifard, M.; Nejati, A.; Momeni, M.; Isavi, N.; Karimialavijeh, E. Midazolam Plus Haloperidol as Adjuvant Analgesics to Morphine in Opium Dependent Patients: A Randomized Clinical Trial. Curr. Drug Abuse Rev. 2016, 9, 142–147. [Google Scholar] [CrossRef]
- Gaffigan, M.E.; Bruner, D.I.; Wason, C.; Pritchard, A.; Frumkin, K. A Randomized Controlled Trial of Intravenous Haloperidol vs. Intravenous Metoclopramide for Acute Migraine Therapy in the Emergency Department. J. Emerg. Med. 2015, 49, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Ali, W.I.; Hadi, E.A.Y.; Al-Johar, Z.A. Pain Management by a Combination of Tramadol, Haloperidol and Carbamazepine in Iraqi Burn Patients. Int. J. Med. Res. Health Sci. 2018, 7, 30–37. [Google Scholar]
- Heriwardito, A.; Manggala, S.K.; Widhyanti, S.I.; Aristya, L. Haloperidol vs. Dexamethasone in Lowering Postoperative Nausea and Vomiting and Pain in Adult After Laparoscopy: A Randomized, Double-Blind Study. Bali J. Anesthesiol. 2022, 6, 157. [Google Scholar] [CrossRef]
- Kazemi, A.P.; Jowkar, T.; Amini, A.; Heydari, S.T. Haloperidol Adjunct with Morphine on Postoperative Pain Management in Opioid-Addicted Patients Undergoing Orthopedic Surgery. Shiraz E-Med. J. 2015, 16, e59892. [Google Scholar] [CrossRef]
- Benevides, M.L.; de Souza Oliveira, S.; Aguilar-Nascimento, J.E. Combination of haloperidol, dexamethasone, and ondansetron reduces nausea and pain intensity and morphine consumption after laparoscopic sleeve gastrectomy. Braz. J. Anesthesiol. 2013, 63, 404–409. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Judkins, K.C.; Harmer, M. Haloperidol as an adjunct analgesic in the management of postoperative pain. Anaesthesia 1982, 37, 1118–1120. [Google Scholar] [CrossRef]
- Salpeter, S.R.; Buckley, J.S.; Buckley, N.S.; Bruera, E. The use of very-low-dose methadone and haloperidol for pain control in the hospital setting: A preliminary report. J. Palliat. Med. 2015, 18, 114–119. [Google Scholar] [CrossRef]
- Raft, D.; Toomey, T.; Gregg, J.M. Behavior modification and haloperidol in chronic facial pain. South. Med. J. 1979, 72, 155–159. [Google Scholar] [CrossRef]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Lee, J.S.; Hobden, E.; Stiell, I.G.; Wells, G.A. Clinically important change in the visual analog scale after adequate pain control. Acad. Emerg. Med. 2003, 10, 1128–1130. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M.; Atieh, J. New Developments in Prokinetic Therapy for Gastric Motility Disorders. Front. Pharmacol. 2021, 12, 711500. [Google Scholar] [CrossRef]
- Thia, I.; Saluja, M. An update on management of renal colic. Aust. J. Gen. Pract. 2021, 50, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Ramsay, M.A.E. Acute postoperative pain management. Bayl. Univ. Med. Cent. Proc. 2000, 13, 244–247. [Google Scholar]
- Sanders, D.S.; Azmy, I.A.; Hurlstone, D.P. A New Insight into Non-Specific Abdominal Pain. Ann. R. Coll. Surg. Engl. 2006, 88, 92–94. [Google Scholar] [CrossRef]
- McNamee, R. Regression modelling and other methods to control confounding. Occup. Environ. Med. 2005, 62, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Frey, T.M.; Florin, T.A.; Caruso, M.; Zhang, N.; Zhang, Y.; Mittiga, M.R. Effect of Intranasal Ketamine vs Fentanyl on Pain Reduction for Extremity Injuries in Children. JAMA Pediatr. 2019, 173, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Diener, H.C.; Tassorelli, C.; Dodick, D.W.; Silberstein, S.D.; Lipton, R.B.; Ashina, M.; Becker, W.J.; Ferrari, M.D.; Goadsby, P.J.; Pozo-Rosich, P.; et al. Guidelines of the International Headache Society for controlled trials of acute treatment of migraine attacks in adults: Fourth edition. Cephalalgia 2019, 39, 687. [Google Scholar] [CrossRef] [PubMed]
- Khandeparkar, A.; Rataboli, P.V. A study of harmful drug–drug interactions due to polypharmacy in hospitalized patients in Goa Medical College. Perspect. Clin. Res. 2017, 8, 180–186. [Google Scholar] [CrossRef]
- Emery, M.A.; Eitan, S. Drug-specific differences in the ability of opioids to manage burn pain. Burns 2020, 46, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Diemunsch, P.; Habib, A.S.; Kovac, A.; Kranke, P.; Meyer, T.A.; Watcha, M.; Chung, F.; Angus, S.; Apfel, C.C.; et al. Consensus Guidelines for the Management of Postoperative Nausea and Vomiting. Anesth. Analg. 2014, 118, 85. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Gordon, D.B.; de Leon-Casasola, O.A.; Rosenberg, J.M.; Bickler, S.; Brennan, T.; Carter, T.; Cassidy, C.L.; Chittenden, E.H.; Degenhardt, E.; et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J. Pain 2016, 17, 131–157. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Massetti, C.; Cheng, C.M.; Sharpe, B.A.; Meier, C.R.; Guglielmo, B.J. The FDA extended warning for intravenous haloperidol and torsades de pointes: How should institutions respond? J. Hosp. Med. 2010, 5, E8–E16. [Google Scholar] [CrossRef]
- Beach, S.R.; Gross, A.F.; Hartney, K.E.; Taylor, J.B.; Rundell, J.R. Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. Gen. Hosp. Psychiatry 2020, 67, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Peabody, C.A.; Brody, D.; Warner, M.D. Tardive dyskinesia after low-dose haloperidol. Biol. Psychiatry 1987, 22, 111–112. [Google Scholar] [CrossRef] [PubMed]
| Study | Mechanism Proposed | Mechanism Detail | Model of Research |
|---|---|---|---|
| Baranoglu et al., 2023 [6] | Antagonism of D2 receptor | Blockade of CGRP release and mast cell degranulation | Migraine |
| Bauch et al., 2017 [7] | Antagonism of D2 receptor | Facilitation of habituation to the absolute pain intensity | Brain models |
| Lee et al., 2015 [8] | Antagonism of D2 receptor | Haloperidol blocked the place preference effect | Conditioned place preference and hot plate test |
| Deciga-Campos et al., 2021 [9] | Blockade of sigma-1 receptors | Anti-allodynic and anti-hyperalgesic activity; efficacy like gabapentin; potency two times higher | In vitro binding assay |
| Espinosa-Juarez et al., 2017 [10] | Blockade of sigma-1 receptors | Antinociceptive effect at the spinal level | Chronic constriction injury |
| Kikuchi et al., 2015 [11] | Blockade of NMDA channels | Could induce pain suppression without anesthesia | Loss of the righting reflex |
| Leppert et al., 2014 [12] | Synergism of mu receptors | Enhanced morphine analgesia | Tail-flick test |
| Mena-Valdes 2021 [13] | Synergism of mu receptors | Antagonized morphine tolerance in neuropathic pain | Chronic constriction injury |
| Petronilho et al., 2012 [14] | Stimulation of the zona incerta | Activation of a pain-inhibitory mechanism to the spinal cord | Tail-flick test and a rat model of incision |
| Study | Indication | Design | Study Size (Female/Total %) | Excluded Populations a | Intervention Arm | Comparison Arm | Key Results, Intervention vs. Comparison | Other Results, Intervention vs. Comparison | Adverse Events Reported |
|---|---|---|---|---|---|---|---|---|---|
| Acute emergency care (11 studies) | |||||||||
| Roldan et al., 2017 [25] | Acute gastroparesis | Randomized controlled trial | 33 (73%) | Prolonged QT intervals | IV 5 mg haloperidol | IV placebo | −4.0 pain VAS (0–10) mean diff. at 1 h (p = NR) | −46% hospital admission diff. (p = 0.009); −1.6 nausea VAS (0–5) mean diff. at 1 h (p = NR) | I = 0/37 C = 0/37 |
| Honkaniemi et al., 2006 [26] | Acute migraine | Randomized controlled trial | 40 (unknown) | Prolonged QT intervals; psychiatric conditions | IV 5 mg haloperidol in normal saline | IV normal saline alone | −4.0 pain VAS (0–10) mean diff. at 1 to 3 h (p < 0.0001) | 65% more patients reported “marked relief” (p < 0.0001) | I = 16/20 C = 1/20 |
| McCoy et al., 2020 [27] | Acute headache or migraine | Randomized controlled trial | 118 (73%) | Prolonged QT intervals | IV 2.5 mg haloperidol in normal saline | IV 5 normal saline alone | −2.9 pain VAS (0–10) mean diff. at 1 h (p unclear) | −47% less rescue analgesic needed (p = NR); +42% more reported ≥50% pain relief at 1 h (p = NR) | I = 14/58 C = 5/60 |
| Ramirez et al., 2017 [28] | Acute gastroparesis | Retrospective comparative study | 52 (62%) | -- | IM 5 mg haloperidol | Self-matched to an ED visit without haloperidol | −4.0 MME median diff. between encounters (p < 0.009) | −17% hospital admission diff. (p < 0.02); no difference in additional antiemetics given (p = NR) | I = 0/52 C = 0/52 |
| Masoumi et al., 2019 [29] | Acute renal colic | Randomized comparative trial | 140 (29%) | Substance use disorders | IV 5 mg haloperidol in normal saline + 5 mg morphine | IV normal saline + 5 mg morphine | No difference in pain VAS (0–10) at 1 h (p = 0.38) | No difference in incidence of nausea and vomiting (p = 0.40, p = 0.61) | I = 73/140 C = 72/140 |
| Heard et al., 2020 [30] | Nonspecific acute abdominal pain | Retrospective cohort study | 11,688 (67%) | -- | haloperidol used during ED encounter (dose NR) | No haloperidol used during ED encounter | RR 1.4 (95% CI 1.2–1.6) increase in IV opioid use | -- | NA |
| Knudsen-Lachendro et al., 2021 [31] | Nonspecific acute abdominal pain | Retrospective comparative study | 107 (70%) | Chronic haloperidol use | IM or IV 2–5 mg haloperidol (median 5 mg) | Self-matched to an ED visit with opioids | −5.7 MME median diff. (p < 0.001), confounded by +25% more ketorolac use in intervention arm | −24% less rescue analgesic needed (p < 0.001); −14% less rescue anti-emetic needed (p = 0.05) | I = 0/107 C = 1/107 |
| Moradi et al., 2022 [32] | Acute pain (47% trauma) | Randomized comparative trial | 200 (31%) | Psychiatric conditions; chronic pain; substance use disorder | IV 2.5 mg haloperidol + 0.3 mg/kg ketamine | IV 1 µg/kg fentanyl | −2.0 pain NRS (0–10) mean diff. at 30 min (p = NR); +56% more reported painless by 10 min (p < 0.001) | No difference in Richmond Agitation-Sedation Scale (mean for both was 0, p = NR) | I = 9/200 C = 2/200 |
| Afzalimoghaddam et al., 2016 [33] | Acute pain in opium users (% trauma unknown) | Randomized comparative trial | 87 (22%) | Prolonged QT intervals | IV 50 µg/kg morphine + IM 2.5 mg midazolam + 2.5 mg haloperidol in 5 mL distilled water | IV 50 µg/kg morphine + IM 5 mL distilled water | −1.2 pain NRS (0–10) mean diff. at 1 h (p = 0.001); −0.4 pain NRS mean diff. at 6 h (p = 0.05) | −12 additional MME given (p = 0.02) | I = 0/87 C = 0/87 |
| Gaffigan et al., 2015 [34] | Acute migraine | Randomized comparative trial | 64 (81%) | Prolonged QT intervals; heart disease; other neurologic conditions | IV 25 mg diphenhydramine + 5 mg haloperidol | IV 25 mg diphenhydramine + 10 mg metoclopramide | No difference in pain VAS (0–100) mean diff. at 80 min (p > 0.05) | No difference in nausea, restlessness, and sedation VAS (0–100) scores (p > 0.05); −21% less rescue analgesic needed (p < 0.02) | I = 17/64 C = 14/64 |
| Ali et al., 2018 [35] | Acute burn 15–40% body surface area | Prospective single-arm trial | 30 (unknown) | Hypertension, renal or hepatic impairment | PO 0.05–0.15 mg/kg haloperidol daily + PO 100–200 mg carbamazepine twice/day + IV 300–400 mg tramadol 12-h infusion | -- | −6.7-point mean decrease from day 1 to 7 on a Wong-Baker Faces Pain Rating Scale (0–10 range) (p < 0.001) | −6.7-point mean decrease from day 1 to 7 on study team’s self-developed pain behavior scale (0–20) (p = NR) | I = 0/30 C = 0/30 |
| Acute postoperative pain (4 studies) | |||||||||
| Heriwardito et al., 2022 [36] | Elective laparoscopic surgery | Randomized comparative trial | 80 (65%) | Psychiatric and neurologic conditions | IV 1 mg haloperidol 1 h before end of surgery | IV 5 mg dexamethasone after induction | −1.5 pain VAS (0–10) mean diff. at 6–12 and 12–24 h (p < 0.001 both) | −15% less nausea at 6–12 h; −48% less nausea at 12–24 h (p < 0.02 both); no difference in vomiting | I = 0/80 C = 0/80 |
| Kazemi et al., 2015 [37] | Elective orthopedic surgery in opium users | Randomized controlled trial | 101 (0%) | Psychiatric conditions | IV 0.1 mg/kg morphine + 20 mg haloperidol + normal saline | IV 0.1 mg/kg morphine + normal saline | −2.7 pain Likert scale (0–4) b mean diff. at 30 min; −0.1 mean diff. at 2 h (p = NR) | −8.0 MME mean diff. in extra analgesic use (p < 0.001) | I = 0/101 C = 0/101 |
| Benevides et al., 2013 [38] | Elective laparoscopic sleeve gastrectomy | Randomized comparative trial | 90 (68%) | Psychiatric conditions; prior opioid use | IV 2 mg haloperidol + 8 mg dexamethasone + 8 mg ondansetron | IV 8 mg dexamethasone + IV 8 mg ondansetron c | −1.5 pain NRS (0–10) mean diff. at 2 h for ondansetron only (p = 0.05); −1.9 pain NRS mean diff. for ondansetron + dexamethasone (p = NR) b | −0.9 nausea NRS (0–10) mean diff. at 2 h for ondansetron only (p = NR); −2.4 less MME used at 2 h for ondansetron only (p = NR) b | I = 0/90 C = 0/90 |
| Judkins and Harmer 1982 [39] | Elective major abdominal surgery | Randomized controlled trial | 34 (unknown) | -- | PO 10 mg diazepam + IV 5 mg haloperidol; PO 10 mg diazepam + IV 10 mg haloperidol d | PO 10 mg diazepam + IV placebo | No difference in pain VAS (0–100) in haloperidol arms vs. placebo at 24 h (+3.8 median diff., p = 0.82) | + 8.8 additional total MME in haloperidol arms vs. placebo (p = NR); −38 to 39 nausea VAS (0–100) median diff. in haloperidol arms vs. placebo (p = 0.005) | I = 3/34 C = 1/34 |
| Chronic pain (2 studies) | |||||||||
| Salpeter et al., 2015 [40] | Inpatient palliative care consultation for uncontrolled pain | Retrospective comparative study | 43 (67%) 42% cancer) | -- | Scheduled PO haloperidol with 2.5–15 mg methadone + PO/IV haloperidol for breakthrough pain (1.5 mg median daily haloperidol dose at 2 weeks) | Scheduled PO haloperidol with PO 2.5–15 mg methadone + PO/IV short-acting opiates for breakthrough pain (0.8 mg median daily haloperidol dose at 2 weeks) | −1.5 pain NRS (0–10) diff. in peak pain scores at 2 weeks (p = NR); −16% fewer participants reporting pain ≥7 on pain NRS at 2 weeks (p = NR) | +0.5 pain NRS diff. in peak pain scores at 2 weeks in cancer vs. noncancer participants (p = NR); baseline median MEDD 79 mg decreased to 6 mg in I arm, 15 mg in C arm (p = NR) | I = 0/43 C = 0/43 |
| Raft et al., 1979 [41] | Chronic facial pain | Prospective single-arm trial | 16 (unknown) | -- | Scheduled PO 2–6 mg/day haloperidol for up to 6 weeks + relaxation therapy, physiotherapy, drug therapy, and counseling | -- | All 16 patients felt pain improved ≥65% from baseline on Tourniquet Pain Ratio; 15/16 reported ≥85% from baseline | Decreased paranoia, mania, and social introversion as measured on MMPI (p < 0.01 each); increased hypochondriasis in males (p < 0.5), depression in females (p < 0.01) | I = 2/16 C = 0/16 |
| Study | Indication | Design | Intervention | Comparison Arm | Dose Used | Participant Size | Adverse Events Reported | Intervention Arm Side Effects | Comparison Arm Side Effects |
|---|---|---|---|---|---|---|---|---|---|
| Honkaniemi et al., 2006 [26] | Acute migraine | Randomized controlled trial | IV haloperido0l + normal saline | IV normal saline alone | 5 mg | 40 | I = 16/40 C = 1/40 | 9 motor agitation and 9 sedation across 16 participants | 1 visual disturbances |
| McCoy et al., 2020 [27] | Acute headache or migraine | Randomized controlled trial | IV haloperidol | IV placebo | 2.5 mg | 118 | I = 14/118 C = 5/118 | 4 anxieties 6 restlessness (10%) 2 nausea/vomiting 4 other | 4 nausea/vomiting 1 other |
| Masoumi et al., 2019 [29] | Acute renal colic | Randomized controlled trial | IV morphine 5 mg + IV haloperidol | IV morphine 5 mg + normal saline | 5 mg | 140 | I = 73/140 C = 72/140 | 34 nausea 36 vomiting 3 extrapyramidal (4.3%) | 39 nausea 33 vomiting 0 extrapyramidal |
| Knudsen-Lachendro et al., 2021 [31] | Nonspecific acute abdominal pain | Retrospective comparative study | IV haloperidol | IV ketorolac 30 mg | 5 mg | 107 | I = 0/107 C = 1/107 | None reported | 1 mental status change |
| Moradi et al., 2022 [32] | Acute pain (47% trauma) | Randomized controlled trial | IV haloperidol + 0.3 mg/kg ketamine | IV fentanyl 1 mg/kg | 2.5 mg | 200 | I = 9/200 C = 2/200 | 5 vomiting 4 emergence reactions a | 2 apneas |
| Gaffigan et al., 2015 [34] | Acute migraine | Randomized controlled trial | IV haloperidol | IV 10 mg metoclopramide | 5 mg | 64 | I = 17/64 C = 14/64 | 5 sleepiness 10 restlessness (32%) 2 chest pain | 9 sleepiness 1 nausea 4 restlessness (12%) |
| Judkins and Harmer 1982 [39] | Elective major abdominal surgery | Randomized controlled trial | IV haloperidol | IV placebo | 5–10 mg | 34 | I = 3/34 C = 1/34 | 1 dry mouth 2 stiffness/shaking (0.1%) | 1 dry mouth |
| Raft et al., 1979 [41] | Chronic facial pain | Case series | IV haloperidol | 3 groups: * Myofascial * Neuropathic * Unidentified | 5 mg | 16 | I = 2/16 C = 0/16 | 2 sedation/confusion | -- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roldan, C.J.; Rowland, J.W.; Ye, A.L. Haloperidol for Pain Management: A Narrative Review. Pharmaceuticals 2024, 17, 1096. https://doi.org/10.3390/ph17081096
Roldan CJ, Rowland JW, Ye AL. Haloperidol for Pain Management: A Narrative Review. Pharmaceuticals. 2024; 17(8):1096. https://doi.org/10.3390/ph17081096
Chicago/Turabian StyleRoldan, Carlos J., Jonathan W. Rowland, and Alice L. Ye. 2024. "Haloperidol for Pain Management: A Narrative Review" Pharmaceuticals 17, no. 8: 1096. https://doi.org/10.3390/ph17081096
APA StyleRoldan, C. J., Rowland, J. W., & Ye, A. L. (2024). Haloperidol for Pain Management: A Narrative Review. Pharmaceuticals, 17(8), 1096. https://doi.org/10.3390/ph17081096








