Abstract
Vectorization of microRNAs has shown to be a smart approach for their potential delivery to treat many diseases (i.e., cancer, osteopathy, vascular, and infectious diseases). However, there are barriers to genetic in vivo delivery regarding stability, targeting, specificity, and internalization. Polymeric nanoparticles can be very promising candidates to overcome these challenges. One of the most suitable polymers for this purpose is chitosan. Chitosan (CS), a biodegradable biocompatible natural polysaccharide, has always been of interest for drug and gene delivery. Being cationic, chitosan can easily form particles with anionic polymers to encapsulate microRNA or even complex readily forming polyplexes. However, fine tuning of chitosan characteristics is necessary for a successful formulation. In this review, we cover all chitosan miRNA formulations investigated in the last 10 years, to the best of our knowledge, so that we can distinguish their differences in terms of materials, formulation processes, and intended applications. The factors that make some optimized systems superior to their predecessors are also discussed to reach the highest potential of chitosan microRNA nanocarriers.
1. Introduction
Genetic material delivery has always been a dreadful challenge. In the last decade, non-viral vectors have shown great promise as safer alternatives to viral vectors for gene delivery. Non-viral vectors include lipidic and polymeric systems [1]. Cationic polymers were of special interest for their ability to complex genetic material readily. One of the most important cationic polymers known is chitosan since it is a natural, biocompatible, biodegradable, and generally recognized as safe (GRAS) by the FDA [2]. Chitosan is a unique polysaccharide copolymer of N-acetyl-D-glucosamine and D-glucosamine linked by a β-(1→4) glycosidic linkage (Figure 1). It is readily derived from N-deacetylation of chitin which is abundant in the exoskeletons of crustaceans (shrimps, crabs, etc.) and the endoskeletons of cephalopods (squids) and is also found in many other species such as mollusks, insects, and fungi [3]. Depending on the duration and intensity of the deacetylation process, the amount of remaining N-acetyl-D-glucosamine moieties (called the degree of acetylation, DA) varies. This parameter, along with the degree of polymerization (DP) or in other words its molar mass (Mw), should be well controlled, as many physicochemical and even biological properties are impacted by the DA and Mw of chitosan [4]. Chitosan NPs have shown potential as highly effective and safe vectors for in vivo delivery of non-coding RNAs when formulae have been optimized [5]. A chitosan based commercial gene transfection reagent (Novafect) has also been developed by Novamatrix, Norway as a non-viral carrier for gene therapy [6].
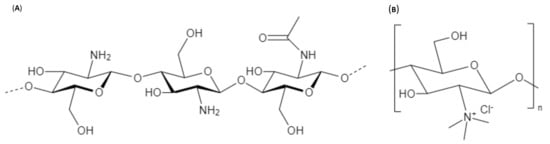
Figure 1.
Chemical structure of (A) Chitosan (CS) and (B) Tri Methyl Chitosan (TMC).
Regulatory non-coding RNAs (ncRNAs) is a term commonly used for RNA not encoding a protein yet affecting gene regulation. Classified by their average size, regulatory ncRNAs are either small non-coding RNAs (sncRNAs) typically less than 200 nt long, or lncRNAs longer than 200 nt. SncRNAs are classified into microRNA (miRNA), small interfering RNAs (siRNAs), and piwi-interacting RNAs (piRNAs) which are a class of animal specific sncRNAs that were named after PIWI proteins [7]. Both miRNAs and siRNAs have critical roles in controlling gene regulation. A lot of research has been carried out on their use for treatment of many diseases, such as cancer, osteopathy, infections, and cardiovascular diseases. Although siRNAs and miRNAs have many common features, being short double-stranded RNA molecules prompting gene silencing at the post-transcriptional level by targeting and subsequent cleavage of messenger RNA, their specific mechanisms of action and possible therapeutic applications remain different (Table 1). The major difference between them is that while siRNA is specific to just one target mRNA, miRNA has many. Hence, their therapeutic applications eventually differ [8].

Table 1.
General comparison between siRNA and miRNA. [8].
Both agents induce gene silencing through activation of RNA induced silencing complex (RISC). That leads to enzymatic cleavage of target mRNA in case of siRNA due to definite complementation of siRNA to its target. However, unlike siRNA, miRNA only achieves partial complementation to its target mRNA which makes it able to regulate expression of multiple targets (Figure 2) [8,9]. MiRNAs have been proven to have a role in all physiological and pathophysiological mechanisms in our bodies, which makes them groundbreaking for many therapeutic applications [10].
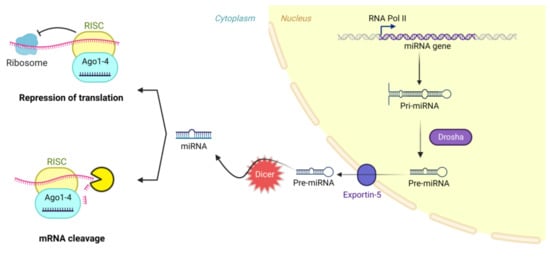
Figure 2.
RNA interference mechanism by miRNA. Created with BioRender.com.
As a result of their gene silencing mechanisms, miRNAs hold great potential for biomedical applications, but their lack of specificity remains a challenge. Moreover, using them solely as therapeutic agents faces extracellular and intracellular barriers [11]. The extracellular barrier would be the extracellular environment containing nucleases ready to cleave any RNA therapeutic and the reticuloendothelial system RES that will mark any foreign substance detected, deeming the half-life of a therapeutic ncRNA to about 10 min.
Then, if this agent was protected either by chemical modification or vectorization, it would face intracellular barriers of cellular uptake and intracellular trafficking. As RNA interference (RNAi) agents are negatively charged, they are repelled, when administered solely, by a counter negative charge of plasma membranes compromising their uptake. In addition, their diffusion through membranes will be impossible for their high molecular weight. To top it all, from a clinical perspective, administration of miRNA as such can induce an immune response and flu like symptoms [12,13].
Ideally, successful RNAi using a delivery system requires the nanocarrier material to be biocompatible, biodegradable, nonimmunogenic, and nontoxic and needs the nanocarrier to protect ncRNA molecules from enzymatic degradation, be of an optimum size (ideally < 200 nm), surface charge, and functionalization to avoid phagocytosis and get internalized by the cells, escape lysis in the endosome, and release ncRNA in cytoplasm [14].
Many vectorization materials, including lipidic, synthetic, and natural polymeric systems, have been studied to achieve this successful delivery of ncRNA. Among them, chitosan stands out as a suitably priced available natural biocompatible biodegradable safe polysaccharide with a positive charge readily available for interaction with negatively charged ncRNA forming nanoplexes. Moreover, chitosan’s protonated amine groups enhance passage across cell membranes and endocytosis [15].
A lot of research has been carried out on the formulation of different forms of CS/siRNA nanoparticles and the importance of chitosan characteristics to achieving optimal (i) particle stability for ncRNA protection in biological media, (ii) colloidal stability maintaining the size of the nanoparticles avoiding aggregation, and (iii) subsequent transfection efficiency [16] but far less focus has been given to miRNA delivery using chitosan (Figure 3). To date, in 2022, only 53 research papers, all of which are covered here, tackle NPs involving both chitosan and miRNA. Indeed, both siRNA and miRNA face similar challenges which are well reviewed in other articles concerning siRNA and include poor stability in vivo, delivery challenges, and off-target effects, and similar strategies may even be investigated to optimize their delivery [14]. However, their mechanisms of actions and biomedical applications are still distinct which demands more spotlight on miRNA.
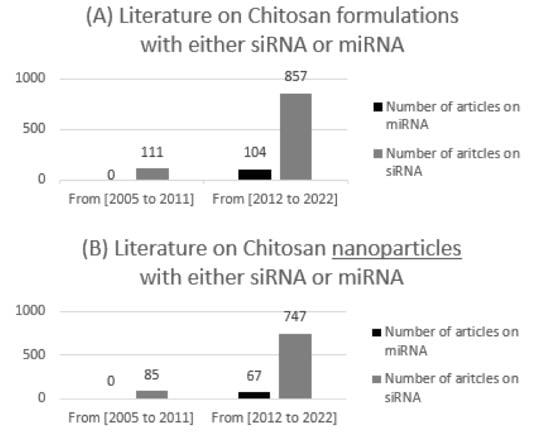
Figure 3.
The number of publications on chitosan with either siRNA or miRNA between 2005 and 2011, and 2012–2022 using Web of Science library, with (A) demonstrating all formulations and (B) demonstrating nanoparticles only.
In this article, we review all chitosan-based nano-formulations made for delivery of miRNA, which include:
- Nanoparticles formulated by direct complexation between chitosan and miRNA (referred to as nano polyplexes = nanoplexes). Polyplexes are complexes made by electrostatic interaction between a cationic polymer (such as chitosan) and negatively charged genetic materials (such as miRNAs) [17].
- Nanoparticles based on the interaction between polycationic chitosan with a counter polyanion:
- Nanoparticles made by polyelectrolyte complexation of polycationic chitosan with a counter polyanion (negatively charged polymer as hyaluronic acid (HA) or dextran sulphate (DS)), adsorbing or encapsulating miRNA (referred to as CS miRNA polyelectrolyte complexes (PECs)) [18,19,20].
- Nanoparticles made by ionic gelation of polycationic chitosan with a counter polyanionic small molecule such as tripolyphosphate (TPP), adsorbing or encapsulating miRNA (referred to as CS/TPP NPs) [21].
- More complex engineered systems.
2. Parameters Affecting CS/MiRNA NPs
2.1. Chitosan Molar Mass
Chitosan molar mass is an essential parameter in the formulation of miRNA nanoparticles with optimum size and stability. CS NPs need to be stable enough to protect miRNA until it is internalized, but able to release it in cytoplasm. As studied before with CS for nucleic acid delivery, the CS chain length’s impact on NP morphological and physicochemical characteristics eventually affects their in vitro and in vivo activity [14,22].
In literature, some authors do not mention the molar mass of CS used in their studies or find it sufficient to just describe it as low or high. In this review, for uniformity, we use the same classification proposed by Ragelle et al. for CS/siRNA NPs; very high Mw would be (>300 kDa), high Mw (80-300 kDa), low Mw (10 to 80 kDa), and very low Mw CS (< 10 kDa) [14].
As concluded from work on CS siRNA NPs, CS with a very short chain length cannot condense genetic material to form intact NPs. A minimum of 15 kDa molar mass was necessary for complete binding to siRNA and therefore protection against cleavage [14]. On the other hand, a very high Mw > 300 kDa may protect the payload too much, so that it faces a challenge in gene release and subsequently less gene silencing. Only CS with molar mass 5–10 times higher than siRNA’s Mw can form compactly structured NPs of suitable size through electrostatic forces and interchain connections [23].
Most research conformed with these specifications set by experience gained with siRNA NPs. However, some exceptions can still be demonstrated. Rarely in literature has a CS of Mw more than 300 kDa been used for delivery of miRNA, however, Ning et al. reported formulation of galactosylated-CS-5-fluorouracil (GC-FU) NPs of 178.5 nm starting from 500 kDa chitosan [24]. These NPs were also loaded with liver-specific miRNA-122 to provide synergistic therapy for hepatocellular carcinoma.
2.1.1. Effect of Chitosan Molar Mass on (CS/Polyanion/MiRNA Nanoparticles)
Most researchers used a Mw around 100 kDa, which demonstrated NPs of less than 200nm that were safely tolerated by cells in vitro and had a biological effect in vivo (when in vivo studies were performed). Yet, a systematic comparison of different CS molar masses has rarely been performed in the same study. Only Tekie et al. compared three different molar masses of CS (9, 18, and 45 kDa) in formulation of polyelectrolyte complexes (PECs) made with carboxymethyl dextran. PECs of 18 and 45 kDa chitosan had higher transfection efficiency, GFP expression, and reduction of cell proliferation by miR-145 when compared with PECs made of 9 kDA Mw CS [25,26].
CS/TPP NPs had a major share of interest of many scientists [9,27,28,29,30], and all of them produced intact biologically active NPs, except for McKiernan et al. as particles were not effective compared to polyethyleneimine (PEI) NPs [27], although they were well tolerated at their size of 115 nm. Deng et al., Wu et al., and Jiang et al. all added Hyaluronic acid (HA), a polyanionic biocompatible polymer, to their systems of CS-TPP NPs [28,30,31]. For Deng et al., HA addition led to a synergistic effect with DOX enhancing its antitumor effect by repressing the expression of anti-apoptosis proto-oncogene [28]. On the other hand, Wu’s NPs had a high transfection efficiency with significant enhancement of marrow mesenchymal stem cells osteogenesis [30]. Wang et al. had a similar effect of improving osteogenesis with their CS/HA system that did not include TPP at all using the same CS Mw of 100 kDa as in Wu’s work [32].
Other polyanionic polymers, like dextran and chondroitin sulfates, were also studied. Tekie et al. used a double strategy to protect their miRNA-145 by conjugating it to dextran by a disulfide bond then further electrolyte complexation with CS of 18 kDa that led to particles of 47, 132, and 272nm depending on the dextran to chitosan molar ratios used (0.2, 1 and 5 respectively) [33]. Then an aptamer was introduced as a targeting agent to increase cellular uptake. Çelik et al. introduced both HA and chondroitin, which together with CS made a triple polysaccharide system capable of protection and delivery of the miRNA to decrease mRNA levels of its target [34].
Only Cosco et al. used CS with an extremely low molar mass (<10 kDa), but they introduced the nanoprecipitation method to form PLGA/CS miRNA NPs that were intact, and of optimal size [35]. This exception may be attributed to using a totally different formulation method (nanoprecipitation) than the ionic gelation method mentioned above. PLGA was dissolved in acetone then added to acidified water containing CS, poloxamer and miR-34a all homogenized together. As PLGA has hydrophobic properties and is negatively charged, its complexation with cationic chitosan could boost the encapsulation and delivery of negatively charged hydrophilic miRNA. These CS/PLGA nanospheres, shown in Figure 4, had a mean hydrodynamic diameter of 160nm, a positive zeta potential and a high level of entrapment efficiency up to 95%. The nanospheres structure protected miRNA from degradation and allowed high transfection efficiency and a significant antitumor effect in vitro against multiple myeloma cells [35].
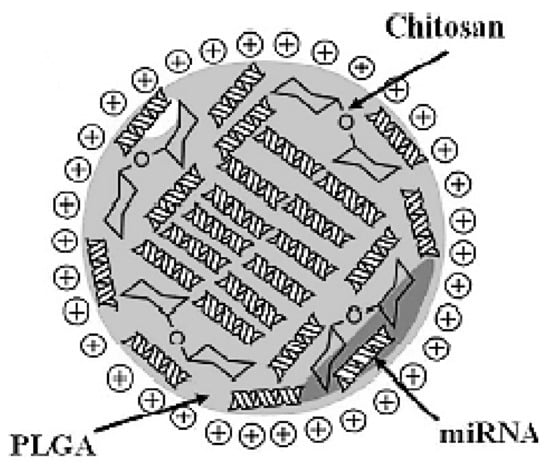
Figure 4.
Schematic representation of miRNA-34a-loaded chitosan/PLGA nanoplexes. (Reproduced from [35]). This work is licensed under a Creative Commons Attribution 4.0 International License.
2.1.2. Effect of Chitosan Molar Mass on Nanoplexes (Chitosan MiRNA Direct Polyplexes)
Following the same trend, all studies were conducted on molar masses of CS ranging from 20–200 kDa to form intact biologically active nanoplexes [24,25,36,37,38,39,40,41,42,43]. Exceptionally, few teams compared different molar masses in the same study, which gives more standardized results. Tekie et al. studied their nanoplexes using 9, 18, and 45 kDa CS at different N/P ratios (2, 5, 10, 20, 30, and 100) [25]. N/P (amine/phosphate) ratio is the molar ratio of polymer’s positively charged amine groups (N) to the negatively charged phosphate (P) groups of nucleic acids, and it is one of the most crucial physicochemical parameters for gene delivery, reviewed best in the work of Gary et al. and Alameh et al. [44,45]. As shown in Figure 5(B), a 9 kDa CS could not give NPs at N/P ratios of 5 and 10. Except for those two cases, all three molar masses used of CS gave nanoparticles at all used N/P ratios. However, only 9 kDa CS at N/P ratio 2 and 45 kDa CS at N/P ratio 10 gave a preferable polydispersity index PDI below 0.20. However, they indicated that their most efficient formulations were made of CS 18 and 45 kDA with N/P ratio of 40 and 100 although they showed delayed onset due to slow release [25].
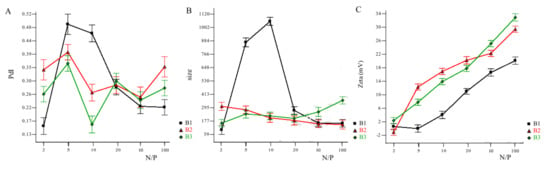
Figure 5.
Effects of chitosan Mw and N/P ratio on (A) PDI, (B) hydrodynamic size, and (C) zeta potential of nanoplexes. B1 ■, B2 ▲, and B3 ♦ are chitosan Mw of 9, 18, and 45 kDa, respectively. Reprinted with permission from ref. [25]. Copyright 2015 Int. J. Biol. Macromol.
Santos-Carballal et al. studied their CS nanoplexes using two ranges of low (1–2 kDa) and relatively higher molar masses (18–26 kDa) with varying degrees of acetylation (as shown in Table 2), all produced from the same parent CS (DA = 1.5%, Mw = 543 kDa) via nitrous depolymerization and subsequent reacetylation [36]. However, a variation in molar mass can be observed. Also, an identical degree of acetylation couldn’t be achieved between comparative higher and lower molar mass couples, especially in the highest DA% couple (49% and 67%) [46,47]. These differences may have impacted the robustness of the comparison to study the effect of molar mass. All formulations led to polyplexes of average hydrodynamic diameters less than 190 nm rendering them available for cellular uptake (Figure 6). They concluded that optimal formulations were observed using CS with a molar mass of ~40 kDa, DA of 12%, and a (+/−) charge ratio of 1.5, resulting in a high transfection efficiency similar to the commercial reagents (DharmaFECT and Novafect) under a standard protocol recommended by DharmaFECT [36].

Table 2.
Molar masses and DA% used in Santos-Carballal et al. studies [36].
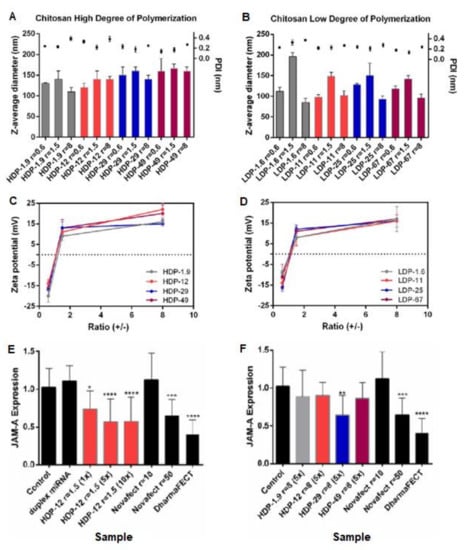
Figure 6.
CS-miRNA polyplexes after 30 min incubation at 37o degrees. Z-average diameter in nm, polydispersity index PDI, and zeta potential ZP in samples formulated using (A,C) higher molar mass CS and (B,D) lower molar mass CS, with their respective transfection efficiency expressed as downregulation of JAM-A mRNA in MCF-7 cells: (E) complexes containing high molar mass CS with DA 12% (HDP-12) at (N/P) charge ratio = 1.5; and (F) complexes containing CS HDP-1.9, HDP-12, HDP-29, and HDP-49 at (N/P) charge ratio = 8. With HDP-DA%: Higher degree of polymerization/molar mass - degree of acetylation percent. DharmaFECT (5 µL/well) and Novafect O 25 were used as positive controls and no treatment was used as a negative control. Statistical comparisons were between each treatment and the control of untreated cells using non-parametric Kruskal–Wallis test (* p < 0.1; ** p < 0.01; *** p < 0.001; **** p < 0.0001), licensed under a Creative Commons Attribution 4.0 International License [36].
Louw et al. used three different molar masses to form CS miRNA polyplexes. A size ~ 200 nm was achieved, and particles reduced activation of microglial cells in rat model showing a very exciting potential for spinal cord injury treatment by having a transfection efficiency that is even higher than viral vectors. Yet, the definite molar mass that gave these results was never mentioned. Indeed, undisclosed details can be noticed sometimes in literature for such a crucial parameter [40].
2.2. Degree of Acetylation (DA) of Chitosan/Deacetylation Degree (DD)
Chitosan can be re-acetylated in solution to a required tailored DA allowing the modulation of the density of primary amines on the polymer chains [48]. Upon protonation in weakly acidic media (i.e., at a pH lower than the pKa of chitosan around ~6.4), the amine moieties provide the positive charges for complexation with the genetic material. Hence, the less DA chitosan has, the greater the density of positive charges it acquires. According to extensive research with siRNA, a high positive charge density is required to achieve strong enough electrostatic interactions with Chitosan, to obtain stable nanoparticles and to mediate endosomal escape [16]. Therefore, a DA of < 30% is required to complex siRNA and form efficient nanoplexes, have more efficient endosomal escape, and eliminate the need for a cross linker as TPP. The results of Alameh et al. in 2018 showed a significant effect of CS DA on the charge density of siRNA nanocomplexes, with optimal in vitro knock down rates using a 10 kDa CS with a 28% DA, and demonstrated a minor effect of the DP and N/P ratio on knock down efficiency [45].
Accordingly, almost all research on chitosan miRNA nanoplexes used CS with a DA ≤ 25%. However, in 2015 Santos-Carballal et al. had more efficient downregulation of the target gene using a higher DA of ~30% and proved that larger complexes were obtained with higher DAs because of extra hydrophobic chains with no positive charge to interact with miRNA [36]. Additionally, miRNA would remain protected from degradation within these chitosan polyplexes due to their enhanced conformational flexibility. Moreover, the release of the RNA, subsequent to cell uptake, was favored due to the weak interactions between the carrier and its payload, an essential factor for the effectiveness of gene therapy, which led them to investigate the binding affinity between CS and miRNA using SPR spectroscopy.
3. Chemical Modifications to Chitosan Reported in MiRNA Formulations
CS is readily derived by partial deacetylation of chitin which is available from many natural sources (i.e., shrimp, crab, squids, insects, and fungi) [3]. Although the source should not be a factor affecting the physicochemical properties of nanoparticles, no study has been conducted to prove so. As a matter of fact, research teams usually keep using one source they are familiar with, which is acceptable as long as a validated purification process [49,50] is implemented to make sure there are no residual impurities.
The most essential reactions needed upon handling chitosan, unless used as commercialized, are reacetylation and depolymerization. Reacetylation of the primary amine group of CS is needed to tune its charge density, solubility and other physicochemical characteristics eventually affecting NPs behavior. The reaction is usually performed in a hydroalcoholic medium ensuring homogeneous N-acetylation reaction with acetic anhydride as described by Vachoud et al. [48].
Depolymerization is needed to obtain the exact lower molar mass needed to achieve desired NPs physicochemical characteristics. CS can be depolymerized chemically, enzymatically, or even by physical techniques reviewed by Younes et al. and Pandit et al. [51,52]. For the scope of our review, nitrous deamination reaction is the most well-known chemical technique to obtain CS of lower molar mass. Briefly, CS is dissolved in an acetic acid/ammonium acetate buffer of pH 4.5, then sodium nitrite is added and left stirring for a specific duration, as shown in Figure 7, needed to obtain the desired molar mass before quenching the reaction using ammonium hydroxide [36,46,47,49,53].
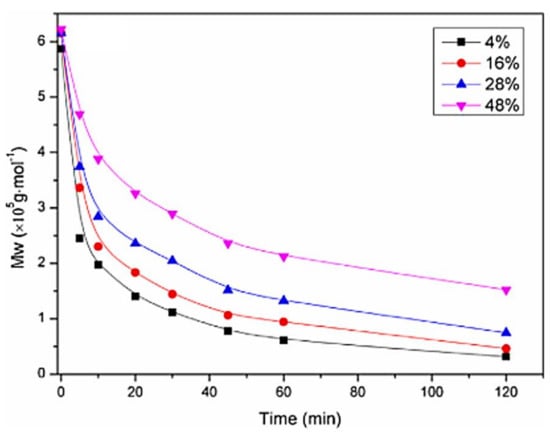
Figure 7.
Depolymerization kinetics specifying nitrous deamination reaction duration for 4 different DA% chitosan with the same parent molar mass. Reprinted with permission from ref. [53]. Copyright 2015 Carbohydr. Polym.
There are many possible modifications of CS to attain different characteristics (Figure 8), depending on the intended application, as it has three groups available for chemical alteration: a primary amine and two hydroxyl moieties (Figure 2). Hence, one can investigate grafting macro/small molecules to these hydroxyl groups and/or the quaternization of the primary amine [14]. Moreover, surface functionalization of chitosan NPs became a valid option to investigate active targeting ensuring better uptake and higher transfection efficiency. Ligands such as REDV peptide in the works of Zhou et al. [39,54,55], RGD peptide [56], aptamers [33,57], folic acid [58,59], galactose [24,60], mannose [61], and glutathione [50] have all been investigated within the scope of CS/miR NPs. Most studies were concerning active targeting against cancer cells, however, Pereira et al. investigated the use of lactoferrin and stearic acid to enhance the brain targeting ability of their CS nanoplexes to treat Alzheimer’s disease [62].
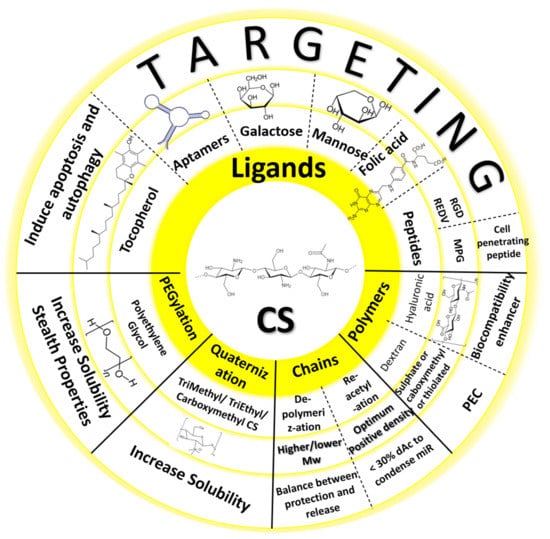
Figure 8.
Possible chemical modifications to chitosan in miRNA formulations.
Many teams worked with quaternization of CS’s primary amine, which increases the solubility of CS [39,54,63,64]. They worked on Trimethyl CS (TMC) (Figure 2), except for the Safari team that worked on Triethyl CS (TEC) and N-Diethyl N-methyl (DEMC), and all teams had promising results in vitro. Zhou’s PEGylated TMC NPs enhanced endothelization in vivo when loaded in an electrospun bilayer scaffold.
PEGylation (i.e., attachment of polyethylene glycol) is a well-documented modification of drug nano-delivery systems. Sun et al. and Zhou et al. grafted PEG to their CS too to increase solubility and stability and avoid opsonization and subsequent rapid elimination in vivo [39,54,65,66]. PEG was usually used as a linker between CS and alkyl chains or ligands that can increase uptake of NPs by specific receptor mediated endocytosis. Sun et al. gave their CS amphiphilic properties by modifying it into PEGylated dioleoyl grafted carboxymethyl CS (DO-g-CMCS-mPEG), which was amphiphilic enough to self-assemble forming chitosomes (mimicking liposomes formed by amphiphilic lipids) (Figure 9) enabling them to co-load both hydrophobic docetaxel and hydrophilic anti-miR-21 in one NP formulation with an average particle size of 90nm [65].
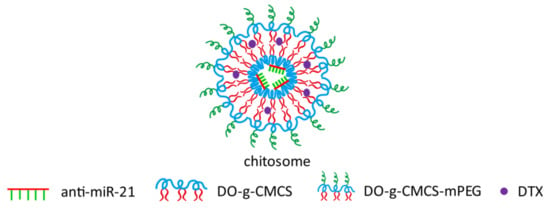
Figure 9.
Chitosome outline containing anti-miRNA-21, dioleoyl grafted carboxymethyl CS (DO-g-CMCS), PEGylated dioleoyl grafted carboxymethyl CS (DO-g-CMCS-mPEG), docetaxel (DTX). Reprinted with permission from ref. [65]. Copyright 2020 Drug Deliv. Transl. Res.
4. Formulation Processes
The two main methods used in the literature for forming CS miRNA NPs are simple complexation and ionic gelation. Simple complexation is based on mixing miRNA with CS at definite N/P and weight ratios, both of which should be optimized with CS characteristics to form intact biologically active NPs [45]. Using this method, Santos-Carballal et al. showed that an N/P ratio of 1.5 was sufficient to achieve transfection efficiencies similar to commercial reagents (Novafect or DharmaFECT) without inducing toxicity (Figure 6) [36].
Ionic gelation on the other hand, depends on ionic interaction between the anionic charges of miRNA and the cationic charges of CS, in the presence of a crosslinking agent like tripolyphosphate TPP stabilizing and strengthening the interactions between CS and miRNA [16,67]. Katas and his team reported CS-TPP NPs to be better gene delivery vectors compared to CS/siRNA polyplexes for higher binding and loading efficiencies. CS/SiRNA interaction strength was than with simple mixing that shows siRNA and CS easily dissociating from each other. This translated into 82% gene knock down using ionic gelation compared to 51% only with simple complexation, when tested with Chinese Hamster Ovary cells (CHO K1). However, lower transfection efficiency was observed when tested with HEK 293 human kidney cells, with ionic gelation still maintaining higher transfection efficiency than simple complexation [68].
Very similarly to these methods, polyelectrolyte complexation can provide a safe and green process for formulation of miRNA NPs. A green nanomedicine process would be quick, suitably priced, and would ensure the use of only nontoxic reagents [69]. Polyelectrolyte complexes (PECs) are safe vectors spontaneously formed by mixing two water solutions of oppositely charged polyelectrolytes with no need for organic solvents, surfactants or crosslinkers [18]. It is basically the same concept as the two methods above, but it uses polyanionic polymers instead of negatively charged miRNA only in simple mixing or TPP in ionic gelation. Moreover, the formulation process is so straightforward that it only requires the addition of one polyanion solution to another polycation solution or vice versa, forming NPs instantly under low shear rate at room temperature as in “one-shot addition method” investigated by Delair et al. or dripping as formulated by Carvalho et al. [19,20]. Using this method can both increase stability of NPs and convey beneficial characteristics of the polyanion used, as for the use of HA that enhances the biocompatibility of NPs [28,32,34,70].
Three articles, by Deng et al., Wang et al. and Wu et al., have shown the use of both HA and TPP as polyanions, and both Deng and Wang et al. encapsulated their intended miRNA into CS NPs by adding it to the polyanion solution before NP formulation. Deng et al. encapsulated both doxorubicin DOX and miRNA-34a into CS NPs. These DOX-miRNA-34a co-loaded HA-CS NPs achieved 80% intracellular uptake giving a promising result toward a synergistic effect against triple negative breast cancer. On the other hand, Wang et al. added the intended miRNA to the preformulated CS/TPP/HA NPs by gentle pipetting, vortexed for a few seconds then left them for 1 h at room temperature for a complete formulation. No study was published for systemic analysis of which process is better in terms of encapsulation, release, and transfection efficiency. Hence, the manner and order of adding miRNA, either before or after NPs formulation, remains unaddressed as there are various types, molar masses, and degrees of acetylation of CS and other external factors, such as pH, ionic strength, charge ratios, and even transfection medium used, that would make a consensus on that matter almost impossible. However, Katas et al. proved that, for their system of CS glutamate-TPP, lower gene silencing was observed with systems adsorbing siRNA onto NPs (added after formulation) than systems entrapping siRNA (added to TPP solution before mixing with CS) which was attributed to more exposure to cleavage by nucleases and/or weaker binding to CS when tested with gel retardation assay [68]. Eventually, genetic material can be either (i) adsorbed or surface-associated over the NPs, (ii) complexed with the polycation forming the NP, or (iii) encapsulated inside the NP [71].
Exceptionally, Çelik et al. made quite unique triple polysaccharide nanoparticles composed of CS, HA, and Chondritin Sulfate (ChoS) with TPP again as a crosslinker. Here, miRNA was added dropwise to preformulated NPs dispersion at an N/P ratio of 30. Another exceptional formulation was achieved by Tekie et al. who made glutathione responsive CS PECs composed of chitosan complexed with a miRNA145 conjugated thiolated dextran (miR-TD) for gene delivery. A disulfide bond connected miRNA and TD, enhancing the stability and efficacy of miRNA, and allowing for glutathione responsive cleavage and release in cancer cells. Above all, a targeting aptamer was decorated onto the formed PECs that greatly improved the uptake by cancer cells [33].
No consensus can be made claiming which system is best. The three options of (i) direct CS/miRNA polyplex with simple mixing, (ii) adding TPP for the formulation with ionic gelation, or (iii) adding a polyanion (such as HA or DS) with or replacing TPP completely for totally green polyelectrolyte complexation are all available and all made sound results in their respective in vitro and in vivo tests, when performed. However, CS should be tailored differently in each method. To mix directly with miRNA, we would need lower DA (up to 30% according to Santos). Adding TPP helps when higher DA CS are used and there is not enough charge density to form intact acceptable size NPs. Exchanging TPP with HA or other polyanions adds biocompatibility characteristics to the system and removes the need for a chemical cross linker, hence the choice of the system will depend mainly on the personalized intended use of CS NPs.
5. Therapeutic Applications of Chitosan MiRNA Delivery Systems
There are two main therapeutic approaches dealing with miRNA therapeutics: either restoring miRNA using a miRNA mimic in diseases in which this miR is downregulated like various cancer phenotypes [72] or inhibiting the function of miRNA through miRNA antagonists (antagomirs) in diseases showing miRNA overexpression [73]. Both strategies are included in Table 3 collectively as the distinction is already clear whether miRNA was used as a therapeutic agent or a therapeutic target.

Table 3.
Different CS miRNA NPs, their therapeutic applications, and in vitro and in vivo tests performed for their analysis.
5.1. Cancer
As demonstrated in Table 3 and Figure 10, CS miRNA NPs have been investigated mainly for cancer therapy [24,26,27,33,34,35,37,41,42,53,56,63,64,65,66,67,68]. Not only can that be attributed to the great characteristics of CS as a natural biocompatible biodegradable modifiable drug delivery system, but CS also has its own biological activities per se [4,92]. CS has been proven to possess an anticancer effect in bladder tumor cells, osteosarcoma, cervical cancer, and breast cancer cell lines [93,94,95], which may be of a synergistic anticancer effect when used in miRNA therapeutics.
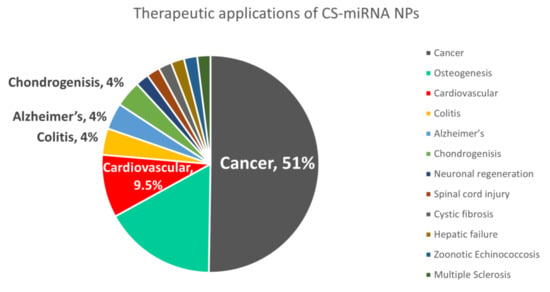
Figure 10.
The percent of research focus on different therapeutic applications using chitosan miRNA NPs (out of 53 papers on topic from 2012 to 2022, covered in Table 3).
As shown in the table, CS/miR nanoplexes made by simple complexation have all shown outstanding results tackling cancer with high transfection efficiencies in their respective studies. Ning and his team achieved suppressed tumor growth using their galactosylated CS with liver-specific miR 122 [24].
Besides nanoplexes, obtained by mere mixing of a chitosan solution and a miR solution, more sophisticated formulation processes were used, leading to chitosomes, lipopolyplexes, or nanobombs. Sun and their team achieved improved chemosensitivity of triple negative breast cancer cell line through synergy between anti-miR-21 and docetaxel in their “chitosomes” [65]. Furthermore, some research aimed at getting the best of polymer and lipids simultaneously, coming up with “lipopolyplexes” [96,97]. Recently, a near-infrared laser activated NP system, “Nano-bomb”, was developed to overcome the limitations of both materials [86]. Wang and their team developed this three-phase water-in-oil-in-water (w/o/w) structure encapsulating miR-34a indocyanine green, and ammonium bicarbonate in the inner hydrophilic phase dispersed in the polymeric hydrophobic phase of PLGA, Pluronic F127, and DPPC. The external hydrophilic phase consisted of HA and chitosan-modified-Pluronic F127. They called it a nano-bomb for the NIR laser photothermal response obtained by indocyanine green leading to the conversion of ammonium bicarbonate into gases allowing the system to escape endosome leading to efficient miR-34a delivery and gene therapy of prostate cancer stem-like cells (CSCs) [86].
5.2. Regenerative Medicine
Almost one third of literature on CS/miR NPs is for regenerative medicine applications. Naturally, CS has a great reputation in the regenerative medicine field as it stimulates tissue regeneration, alone or in combinations, and can convey valuable characteristics as antimicrobial and mucoadhesive properties to the systems incorporating it at definite parameters [98]. Moreover, CS has a chemical structural similarity to extracellular matrix (ECM) [99] that can be seen in the extensive research in CS/miRNA NPs for osteogenesis [30,31,32,83,84,85,87], chondrogenesis [34,89], neural tissue [76], and even blood vessels regeneration [39,54,55,64]. Jiang et al. formulated their chitosan antimir-133a/b NPs using the ionic gelation method with TPP, and hyaluronic acid then incorporated these NPs in a chitosan glycerophosphate gel making a sustained release formulation that was cytocompatible and promoted osteogenesis in vivo in a calvarial bone defect mouse model [31]. Li et al. also incorporated their CS/TPP/mir-222 NPs within silk nanofibrous scaffolds aiming at a transplantation therapy for neuronal regeneration. Their system showed good cytocompatibility and improved neural stem cells (NSCs) differentiation [76]. Zhou et al. also loaded their REDV functionalized PEGylated trimethyl chitosan miR-126 NPs into an electrospun bilayer vascular scaffold that accelerated vascular endothelial cells proliferation and could enhance reendothelialization in vivo [54].
5.3. Other Fields of Therapy
MiRNAs are involved in all physiological and pathophysiological mechanisms which make the opportunities for therapeutic applications endless [10]. Recently, they have received more attention for controlling inflammation [100]. Shamaeizadeh et al. investigated the use of a formulation of glutathione targeted tragacanthic acid modified CS polyplexes with miR-219a-5p for treatment of multiple sclerosis and they could prove decreased inflammation and brain cells regeneration when injecting their NPs into cuprizone MS mice model [50]. Louw et al. have also shown that their CS miR-124 polyplexes were able to reduce reactive oxygen species and TNF-α in vitro and reduce activation of microglial cells in rats in vivo aiming to treat spinal cord injury. Many more therapeutic applications are applicable depending on the miRNA chosen [40]. Cystic fibrosis [27], hepatic failure [82], and zoonotic echinococcosis [77] were also possible to investigate with CS/miR NPs
6. Conclusions and Prospects
Just recently in 2020, a huge surge of interest in nanomedicine has been noticed with the three phases of: waiting for a vaccine for COVID-19, the discovery of a vaccine based on nanomedicine and gene delivery, and the last phase of controversy gaining public trust with such a new system. This nanomedicine renaissance should be exploited to go further in therapeutic applications that have been overshadowed by the interest in cancer therapeutics. Fields like vaccinology, cardiovascular, hepatic, and renal diseases could use the benefits of nanomedicine. Among these nanomedicine candidates, CS NPs could provide a cheap, sustainable, stable, naturally available, and safer alternative to viral gene delivery. For it to reach the same efficiency of viral vectors, all it needs is a little push using the most recent, standardized, and consistent findings on making an efficient biologically active CS miRNA NP that is stable enough to protect miRNA from the extracellular environment, reach targeted cells, be uptaken and have weak enough binding to release miRNA in the cytoplasm for efficient gene silencing.
Achieving a systematic comparison between different factors (i.e., molar mass, degree of acetylation, N/P ratio, nanoparticle concentration, polyanions addition, and targeting moiety addition) in the same study is needed to reach a valid consensus. Recent Apliterature in the last 10 years showed more consistency and more promising results having more systemic literature-based modifications. Starting with using a molar mass of 10 kDa at least, a DA ≤ 30%, N/P ratio of 1.5–20, and PEGylation/ligand grafting when necessary is a good starting point for any future experiments. Depending on intended applications, the addition of other components to the formulations (as polyanions) can convey beneficial characteristics to the CS miRNA system. That offers a new perspective of CS and an opportunity for a theoretically old/practically new system to be exploited at its best for many therapeutic applications.
Author Contributions
Conceptualization, H.H.G., T.D. and A.M.; methodology, H.H.G., T.D. and A.M.; formal analysis, H.H.G., T.D. and A.M.; investigation, H.H.G., T.D. and A.M.; resources, H.H.G., T.D. and A.M.; data curation, H.H.G., T.D. and A.M.; writing—review and editing, H.H.G., T.D. and A.M.; funding acquisition, A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie-Sklodowska Curie grant agreement No. 813716.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sung, Y.K.; Kim, S.W. Recent Advances in the Development of Gene Delivery Systems. Biomater. Res. 2019, 23, 8. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Fuentes, M.; Alonso, M.J. Chitosan-Based Drug Nanocarriers: Where Do We Stand? J. Control. Release 2012, 161, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Peniche, C.; Argüelles-Monal, W.; Goycoolea, F.M. Chitin and Chitosan: Major Sources, Properties and Applications. In Monomers, Polymers and Composites from Renewable Resources; Elsevier Ltd.: Amsterdam, The Netherlands, 2008; pp. 517–542. ISBN 9780080453163. [Google Scholar]
- El Gueddari, N.E.; Moerschbacher, B.M.; Boucher, I.; Jamieson, K. Advances in Chitin Science. Eur. Chitin Soc. Montr. 2004, VII, 56–59. [Google Scholar]
- Rupaimoole, R.; Han, H.D.; Lopez-Berestein, G.; Sood, A.K. MicroRNA Therapeutics: Principles, Expectations, and Challenges. Chin. J. Cancer 2011, 30, 368–370. [Google Scholar] [CrossRef] [PubMed]
- Klausner, E.A.; Zhang, Z.; Chapman, R.L.; Multack, R.F.; Volin, M.V. Ultrapure Chitosan Oligomers as Carriers for Corneal Gene Transfer. Biomaterials 2010, 31, 1814–1820. [Google Scholar] [CrossRef]
- Zhang, P.; Wu, W.; Chen, Q.; Chen, M. Non-Coding RNAs and Their Integrated Networks. J. Integr. Bioinform. 2019, 16, 3. [Google Scholar] [CrossRef]
- Lam, J.K.W.; Chow, M.Y.T.; Zhang, Y.; Leung, S.W.S. SiRNA versus MiRNA as Therapeutics for Gene Silencing. Mol. Ther. Nucleic Acids 2015, 4, e252. [Google Scholar] [CrossRef] [Green Version]
- Denizli, M.; Aslan, B.; Mangala, L.S.; Jiang, D.; Lopez-berestein, G.; Sood, A.K. Chitosan Nanoparticles for MiRNA Delivery. Methods Mol. Biol. 2017, 1632, 219–230. [Google Scholar] [CrossRef]
- Dasgupta, I.; Chatterjee, A. Recent Advances in MiRNA Delivery Systems. Methods Protoc. 2021, 4, 10. [Google Scholar] [CrossRef]
- Chen, Y.; Gao, D.Y.; Huang, L. In Vivo Delivery of MiRNAs for Cancer Therapy: Challenges and Strategies. Adv. Drug Deliv. Rev. 2015, 81, 128–141. [Google Scholar] [CrossRef] [Green Version]
- Yin, H.; Kanasty, R.L.; Eltoukhy, A.A.; Vegas, A.J.; Dorkin, J.R.; Anderson, D.G. Non-Viral Vectors for Gene-Based Therapy. Nat. Rev. Genet. 2014, 15, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Petros, R.A.; Desimone, J.M. Strategies in the Design of Nanoparticles for Therapeutic Applications. Nat. Rev. Drug Discov. 2010, 9, 615–627. [Google Scholar] [CrossRef] [PubMed]
- Ragelle, H.; Vandermeulen, G.; Préat, V. Chitosan-Based SiRNA Delivery Systems. J. Control. Release 2013, 172, 207–218. [Google Scholar] [CrossRef]
- Guzman-Villanueva, D.; El-Sherbiny, I.M.; Herrera-Ruiz, D.; Vlassov, A.V.; Smyth, H.D.C. Formulation Approaches to Short Interfering RNA and MicroRNA: Challenges and Implications. J. Pharm. Sci. 2012, 101, 2271–2280. [Google Scholar] [CrossRef]
- Ragelle, H.; Riva, R.; Vandermeulen, G.; Naeye, B.; Pourcelle, V.; Le Duff, C.S.; D’Haese, C.; Nysten, B.; Braeckmans, K.; De Smedt, S.C.; et al. Chitosan Nanoparticles for SiRNA Delivery: Optimizing Formulation to Increase Stability and Efficiency. J. Control. Release 2014, 176, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Vetter, V.C.; Wagner, E. Targeting Nucleic Acid-Based Therapeutics to Tumors: Challenges and Strategies for Polyplexes. J. Control. Release 2022, 346, 110–135. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Zhu, L.; Li, Y.; Zhang, X.; Xu, S.; Yang, G.; Delair, T. Chitosan-Based Colloidal Polyelectrolyte Complexes for Drug Delivery: A Review. Carbohydr. Polym. 2020, 238, 116126. [Google Scholar] [CrossRef]
- Delair, T. Colloidal Polyelectrolyte Complexes of Chitosan and Dextran Sulfate towards Versatile Nanocarriers of Bioactive Molecules. Eur. J. Pharm. Biopharm. 2011, 78, 10–18. [Google Scholar] [CrossRef]
- Carvalho, S.G.; dos Santos, A.M.; Silvestre, A.L.P.; Meneguin, A.B.; Ferreira, L.M.B.; Chorilli, M.; Gremião, M.P.D. New Insights into Physicochemical Aspects Involved in the Formation of Polyelectrolyte Complexes Based on Chitosan and Dextran Sulfate. Carbohydr. Polym. 2021, 271, 118436. [Google Scholar] [CrossRef]
- Bugnicourt, L.; Ladavière, C. Interests of Chitosan Nanoparticles Ionically Cross-Linked with Tripolyphosphate for Biomedical Applications. Prog. Polym. Sci. 2016, 60, 1–17. [Google Scholar] [CrossRef]
- Buschmann, M.D.; Merzouki, A.; Lavertu, M.; Thibault, M.; Jean, M.; Darras, V. Chitosans for Delivery of Nucleic Acids. Adv. Drug Deliv. Rev. J. 2013, 65, 1234–1270. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Howard, K.A.; Dong, M.; Andersen, M.; Rahbek, U.L.; Johnsen, M.G.; Hansen, O.C.; Besenbacher, F.; Kjems, J. The Influence of Polymeric Properties on Chitosan/SiRNA Nanoparticle Formulation and Gene Silencing. Biomaterials 2007, 28, 1280–1288. [Google Scholar] [CrossRef] [PubMed]
- Ning, Q.; Liu, Y.F.; Ye, P.J.; Gao, P.; Li, Z.P.; Tang, S.Y.; He, D.X.; Tang, S.S.; Wei, H.; Yu, C.Y. Delivery of Liver-Specific MiRNA-122 Using a Targeted Macromolecular Prodrug toward Synergistic Therapy for Hepatocellular Carcinoma. ACS Appl. Mater. Interfaces 2019, 11, 10578–10588. [Google Scholar] [CrossRef] [PubMed]
- Tekie, F.S.M.; Atyabi, F.; Soleimani, M.; Arefian, E.; Atashi, A.; Kiani, M.; Khoshayand, M.R.; Amini, M.; Dinarvand, R. Chitosan Polyplex Nanoparticle Vector for MiR-145 Expression in MCF-7: Optimization by Design of Experiment. Int. J. Biol. Macromol. 2015, 81, 828–837. [Google Scholar] [CrossRef]
- Tekie, F.S.M.; Kiani, M.; Zakerian, A.; Pilevarian, F.; Assali, A.; Soleimani, M.; Dinarvand, R.; Arefian, E.; Atashi, A.; Amini, M.; et al. Nano Polyelectrolyte Complexes of Carboxymethyl Dextran and Chitosan to Improve Chitosan-Mediated Delivery of MiR-145. Carbohydr. Polym. 2017, 159, 66–75. [Google Scholar] [CrossRef]
- McKiernan, P.J.; Cunningham, O.; Greene, C.M.; Cryan, S.A. Targeting MiRNA-Based Medicines to Cystic Fibrosis Airway Epithelial Cells Using Nanotechnology. Int. J. Nanomed. 2013, 8, 3907–3915. [Google Scholar] [CrossRef] [Green Version]
- Deng, X.; Cao, M.; Zhang, J.; Hu, K.; Yin, Z.; Zhou, Z.; Xiao, X.; Yang, Y.; Sheng, W.; Wu, Y.; et al. Hyaluronic Acid-Chitosan Nanoparticles for Co-Delivery of MiR-34a and Doxorubicin in Therapy against Triple Negative Breast Cancer. Biomaterials 2014, 35, 4333–4344. [Google Scholar] [CrossRef]
- Gaur, S.; Wen, Y.; Song, J.H.; Parikh, N.U.; Mangala, L.S.; Blessing, A.M.; Ivan, C.; Wu, S.Y.; Varkaris, A.; Shi, Y.; et al. Chitosan Nanoparticle-Mediated Delivery of MiRNA-34a Decreases Prostate Tumor Growth in the Bone and Its Expression Induces Non-Canonical Autophagy. Oncotarget 2015, 6, 29161–29177. [Google Scholar] [CrossRef] [Green Version]
- Wu, G.; Feng, C.; Hui, G.; Wang, Z.; Tan, J.; Luo, L.; Xue, P.; Wang, Q.; Chen, X. Improving the Osteogenesis of Rat Mesenchymal Stem Cells by Chitosan-Based-MicroRNA Nanoparticles. Carbohydr. Polym. 2016, 138, 49–58. [Google Scholar] [CrossRef]
- Jiang, F.; Yin, F.; Lin, Y.; Xia, W.; Zhou, L.; Pan, C.; Wang, N.; Shan, H.; Zhou, Z.; Yu, X. The Promotion of Bone Regeneration through CS/GP-CTH/Antagomir-133a/b Sustained Release System. Nanomed. Nanotechnol. Biol. Med. 2020, 24, 102116. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, G.; Wei, M.; Liu, Q.; Zhou, J.; Qin, T.; Feng, X.; Liu, H.; Feng, Z.; Zhao, Y. Improving the Osteogenesis of Human Bone Marrow Mesenchymal Stem Cell Sheets by MicroRNA-21-Loaded Chitosan/Hyaluronic Acid Nanoparticles via Reverse Transfection. Int. J. Nanomed. 2016, 11, 2091–2105. [Google Scholar] [CrossRef] [Green Version]
- Tekie, F.S.M.; Soleimani, M.; Zakerian, A.; Dinarvand, M.; Amini, M.; Dinarvand, R.; Arefian, E.; Atyabi, F. Glutathione Responsive Chitosan-Thiolated Dextran Conjugated MiR-145 Nanoparticles Targeted with AS1411 Aptamer for Cancer Treatment. Carbohydr. Polym. 2018, 201, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Çelik, E.; Bayram, C.; Denkbaş, E.B. Chondrogenesis of Human Mesenchymal Stem Cells by MicroRNA Loaded Triple Polysaccharide Nanoparticle System. Mater. Sci. Eng. C 2019, 102, 756–763. [Google Scholar] [CrossRef]
- Cosco, D.; Cilurzo, F.; Maiuolo, J.; Federico, C.; Di Martino, M.T.; Cristiano, M.C.; Tassone, P.; Fresta, M.; Paolino, D. Delivery of MiR-34a by Chitosan/PLGA Nanoplexes for the Anticancer Treatment of Multiple Myeloma. Sci. Rep. 2015, 5, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos-Carballal, B.; Aaldering, L.J.; Ritzefeld, M.; Pereira, S.; Sewald, N.; Moerschbacher, B.M.; Götte, M.; Goycoolea, F.M. Physicochemical and Biological Characterization of Chitosan-MicroRNA Nanocomplexes for Gene Delivery to MCF-7 Breast Cancer Cells. Sci. Rep. 2015, 5, 1–15. [Google Scholar] [CrossRef]
- Pereira, P.A.; Tomás, J.F.; Queiroz, J.A.; Figueiras, A.R.; Sousa, F. Recombinant Pre-MiR-29b for Alzheimer’s Disease Therapeutics. Sci. Rep. 2016, 6, 1–11. [Google Scholar] [CrossRef]
- Kaban, K.; Salva, E.; Akbuga, J. The Effects of Chitosan/MiR-200c Nanoplexes on Different Stages of Cancers in Breast Cancer Cell Lines. Eur. J. Pharm. Sci. 2016, 95, 103–110. [Google Scholar] [CrossRef]
- Zhou, F.; Yuan, X. Targeted Delivery of MicroRNA-126 to Vascular Endothelial Cells: Via REDV Peptide Modified PEG-Trimethyl Chitosan. Biomater. Sci. 2016, 4, 849–856. [Google Scholar] [CrossRef]
- Louw, A.M.; Kolar, M.K.; Novikova, L.N.; Kingham, P.J.; Wiberg, M.; Kjems, J.; Novikov, L.N. Chitosan Polyplex Mediated Delivery of MiRNA-124 Reduces Activation of Microglial Cells in Vitro and in Rat Models of Spinal Cord Injury. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 643–653. [Google Scholar] [CrossRef] [Green Version]
- Tu, L.; Wang, M.; Zhao, W.Y.; Zhang, Z.Z.; Tang, D.F.; Zhang, Y.Q.; Cao, H.; Zhang, Z.G. MiRNA-218-Loaded Carboxymethyl Chitosan - Tocopherol Nanoparticle to Suppress the Proliferation of Gastrointestinal Stromal Tumor Growth. Mater. Sci. Eng. C 2017, 72, 177–184. [Google Scholar] [CrossRef]
- Kaban, K.; Salva, E.; Akbuga, J. Modulation of the Dual-Faced Effects of MiR-141 with Chitosan/MiR-141 Nanoplexes in Breast Cancer Cells. J. Gene Med. 2019, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Xie, H.; Yu, J.; Chen, X.; Tang, S.; Sun, L.; Chen, X.; Peng, D.; Zhang, X.; Zhou, J. Atargeted Therapy for Melanoma by Graphene Oxide Composite with MicroRNA Carrier. Drug Des. Devel. Ther. 2018, 12, 3095–3106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gary, D.J.; Min, J.; Kim, Y.; Park, K.; Won, Y.Y. The Effect of N/P Ratio on the in Vitro and in Vivo Interaction Properties of Pegylated Poly[2-(Dimethylamino)Ethyl Methacrylate]-Based SiRNA Complexes. Macromol. Biosci. 2013, 13, 1059–1071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alameh, M.; Lavertu, M.; Tran-Khanh, N.; Chang, C.-Y.Y.; Lesage, F.; Bail, M.; Darras, V.; Chevrier, A.; Buschmann, M.D. SiRNA Delivery with Chitosan: Influence of Chitosan Molecular Weight, Degree of Deacetylation, and Amine to Phosphate Ratio on in Vitro Silencing Efficiency, Hemocompatibility, Biodistribution, and in Vivo Efficacy. Biomacromolecules 2018, 19, 112–131. [Google Scholar] [CrossRef] [PubMed]
- Allan, G.G.; Peyron, M. Molecular Weight Manipulation of Chitosan I: Kinetics of Depolymerization by Nitrous Acid. Carbohydr. Res. 1995, 277, 257–272. [Google Scholar] [CrossRef]
- Allan, G.G.; Peyron, M. Molecular Weight Manipulation of Chitosan II: Prediction and Control of Extent of Depolymerization by Nitrous Acid. Carbohydr. Res. 1995, 277, 273–282. [Google Scholar] [CrossRef]
- Vachoud, L.; Zydowicz, N.; Domard, A. Formation and Characterisation of a Physical Chitin Gel. Carbohydr. Res. 1997, 302, 169–177. [Google Scholar] [CrossRef]
- Roux, R.; Ladavière, C.; Montembault, A.; David, L.; Delair, T. Shear Thinning 3D-Colloidal Assemblies of Chitosan and Poly (Lactic Acid) Nanoparticles. J. Phys. Chem. 2013, 117, 7455–7464. [Google Scholar] [CrossRef]
- Shamaeizadeh, N.; Varshosaz, J.; Mirian, M.; Aliomrani, M. Glutathione Targeted Tragacanthic Acid-Chitosan as a Non-Viral Vector for Brain Delivery of MiRNA-219a-5P: An in Vitro/in Vivo Study. Int. J. Biol. Macromol. 2022, 200, 543–556. [Google Scholar] [CrossRef]
- Younes, I.; Rinaudo, M.; Harding, D.; Sashiwa, H. Chitin and Chitosan Preparation from Marine Sources. Structure, Properties and Applications. Mar. Drugs 2015, 13, 1133–1174. [Google Scholar] [CrossRef] [Green Version]
- Pandit, A.; Indurkar, A.; Deshpande, C.; Jain, R.; Dandekar, P. A Systematic Review of Physical Techniques for Chitosan Degradation. Carbohydr. Polym. Technol. Appl. 2021, 2, 100033. [Google Scholar] [CrossRef]
- Wu, D.; Delair, T. Stabilization of Chitosan/Hyaluronan Colloidal Polyelectrolyte Complexes in Physiological Conditions. Carbohydr. Polym. 2015, 119, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yuan, X. Nanofiber-Mediated MicroRNA-126 Delivery to Vascular Endothelial Cells for Blood Vessel Regeneration. Acta Biomater. 2016, 43, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Wen, M.; Zhou, P.; Zhao, Y.; Jia, X.; Fan, Y. Materials Science & Engineering C Electrospun Membranes of PELCL/PCL-REDV Loading with MiRNA-126 for Enhancement of Vascular Endothelial Cell Adhesion and Proliferation. Mater. Sci. Eng. C 2018, 85, 37–46. [Google Scholar] [CrossRef]
- Pecot, C.V.; Rupaimoole, R.; Yang, D.; Akbani, R.; Ivan, C.; Lu, C.; Wu, S.; Han, H.D.; Shah, M.Y.; Rodriguez-Aguayo, C.; et al. Tumour Angiogenesis Regulation by the MiR-200 Family. Nat. Commun. 2013, 4, 2427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khatami, F.; Matin, M.M.; Mohammad, N.; Reza, A.; Abnous, K.; Mohammad, S. Targeted Delivery System Using Silica Nanoparticles Coated with Chitosan and AS1411 for Combination Therapy of Doxorubicin and AntimiR-21. Carbohydr. Polym. 2021, 266, 118111. [Google Scholar] [CrossRef] [PubMed]
- Golafzani, F.N.; Vaziri, A.Z.; Javanmardi, M. Delivery of MiRNA-126 through Folic Acid-Targeted Biocompatible Polymeric Nanoparticles for Effective Lung Cancer Therapy. J. Bioactive Compat. Polym. 2022, 37, 168–188. [Google Scholar] [CrossRef]
- Mokri, N.; Sepehri, Z.; Faninam, F.; Khaleghi, S.; Kazemi, N.M.; Hashemi, M. Chitosan-Coated Zn-Metal-Organic Framework Nanocomposites for Effective Targeted Delivery of LNA-Antisense MiR-224 to Colon Tumor: In Vitro Studies. Gene Ther. 2021, 1–11. [Google Scholar] [CrossRef]
- Huang, Z.; Ma, J.; Chen, M.; Jiang, H.; Fu, Y.; Gan, J.; Dong, L.; Zhang, J.; Chen, J. Dual TNF- α/IL-12p40 Interference as a Strategy to Protect Against Colitis Based on MiR-16 Precursors With Macrophage Targeting Vectors. Mol. Ther. 2015, 23, 1611–1621. [Google Scholar] [CrossRef] [Green Version]
- Deng, F.; He, S.; Cui, S.; Shi, Y. A Molecular Targeted Immunotherapeutic Strategy for Ulcerative Colitis via Dual-Targeting Nanoparticles Delivering MiR-146b to Intestinal Macrophages. J. Crohn’s Colitis 2019, 13, 482–494. [Google Scholar] [CrossRef]
- Pereira, P.; Barreira, M.; Cruz, C.; Tom, J.; Lu, Â.; Pedro, A.Q.; Queiroz, A.; Sousa, F. Brain-Targeted Delivery of Pre-MiR-29b Using Polyethyleneimine Polyplexes. Pharmaceuticals 2020, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Safari, S.; Zarrintan, M.H.; Soleimani, M.; Dorkoosh, F.A.; Akbari, H.; Larijani, B.; Tehrani, M.R. Evaluation and Optimization of Chitosan Derivatives-Based Gene Delivery System via Kidney Epithelial Cells. Adv. Pharm. Bull. 2012, 2, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.; Zhou, F.; Cui, C.; Zhao, Y.; Yuan, X. Performance of TMC-g-PEG-VAPG/MiRNA-145 Complexes in Electrospun Membranes for Target-Regulating Vascular SMCs. Colloids Surf. B Biointerfaces 2019, 182, 110369. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Xu, H.; Huang, T.; Zhang, C.; Wu, J.; Luo, S. Simultaneous Delivery of Anti-MiRNA and Docetaxel with Supramolecular Self-Assembled “Chitosome” for Improving Chemosensitivity of Triple Negative Breast Cancer Cells. Drug Deliv. Transl. Res. 2020, 21, 192–204. [Google Scholar] [CrossRef]
- Feczkó, T. Polymeric Nanotherapeutics Acting at Special Regions of Body. J. Drug Deliv. Sci. Technol. 2021, 64, 102597. [Google Scholar] [CrossRef]
- Nguyen, M.A.; Wyatt, H.; Susser, L.; Geoffrion, M.; Rasheed, A.; Duchez, A.C.; Cottee, M.L.; Afolayan, E.; Farah, E.; Kahiel, Z.; et al. Delivery of MicroRNAs by Chitosan Nanoparticles to Functionally Alter Macrophage Cholesterol Efflux In Vitro and In Vivo. ACS Nano 2019, 13, 6491–6505. [Google Scholar] [CrossRef]
- Katas, H.; Alpar, H.O. Development and Characterisation of Chitosan Nanoparticles for SiRNA Delivery. J. Control. Release 2006, 115, 216–225. [Google Scholar] [CrossRef]
- Thipe, V.C.; Raphael, A.; Çakılkaya, P.; Genedy, H.H.; Kaeokhamloed, N.; Roger, E.; Katti, K.V. Green Nanotechnology—An Innovative Pathway towards Biocompatible and Medically Relevant Gold Nanoparticles. J. Drug Deliv. Sci. Technol. 2022, 70, 103256. [Google Scholar] [CrossRef]
- Wu, D.; Ensinas, A.; Verrier, B.; Primard, C.; Cuvillier, A.; Champier, G.; Paul, S.; Delair, T. Zinc-Stabilized Colloidal Polyelectrolyte Complexes of Chitosan/Hyaluronan: A Tool for the Inhibition of HIV-1 Infection. J. Mater. Chem. B 2016, 4, 5455–5463. [Google Scholar] [CrossRef]
- Ban, E.; Kwon, T.H.; Kim, A. Delivery of Therapeutic MiRNA Using Polymer-Based Formulation. Drug Deliv. Transl. Res. 2019, 9, 1043–1056. [Google Scholar] [CrossRef]
- Williams, M.; Cheng, Y.Y.; Blenkiron, C.; Reid, G. Exploring Mechanisms of MicroRNA Downregulation in Cancer. MicroRNA 2017, 6, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-piñeiro, I.; Badiola, I.; Sanchez, A. Nanocarriers for MicroRNA Delivery in Cancer Medicine. Biotechnol. Adv. 2017, 35, 350–360. [Google Scholar] [CrossRef]
- Chen, X.; Gu, S.; Chen, B.; Shen, W.; Yin, Z.; Xu, G.; Hu, J.; Zhu, T.; Li, G.; Wan, C.; et al. Biomaterials Nanoparticle Delivery of Stable MiR-199a-5p Agomir Improves the Osteogenesis of Human Mesenchymal Stem Cells via the HIF1a Pathway. Biomaterials 2015, 53, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Suardi, R.B.; Ysrafil, Y.; Sesotyosari, S.L.; Martien, R.; Wardana, T.; Astuti, I.; Haryana, S.M. The Effects of Combination of Mimic MiR-155-5p and Antagonist MiR-324-5p Encapsulated Chitosan in Ovarian Cancer SKOV3. Asian Pac. J. Cancer Prev. 2020, 21, 2603–2608. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Meng, Z.; Zhao, Z. Silk Fibroin Nanofibrous Scaffolds Incorporated with MicroRNA-222 Loaded Chitosan Nanoparticles for Enhanced Neuronal Differentiation of Neural Stem Cells. Carbohydr. Polym. 2022, 277, 118791. [Google Scholar] [CrossRef]
- Sun, Y.; Kou, Y.; He, X.; Yan, Y.; Guo, X.; Yang, X.; He, N.; Cho, W.C.; Kutyrev, I.; Harandi, M.F.; et al. Efficient Delivery of Echinococcus Multilocularis MiRNAs Using Chitosan Nanoparticles. Biomed. Pharmacother. 2022, 150, 112945. [Google Scholar] [CrossRef]
- Li, K.; Qiu, Y.; Liu, X.; Huang, F. Biomimetic Nanosystems for the Synergistic Delivery of MiR-144/451a for Oral Squamous Cell Carcinoma. Balk. Med. J. 2022, 39, 178–186. [Google Scholar] [CrossRef]
- Alswailem, R.; Alqahtani, F.Y.; Aleanizy, F.S.; Alrfaei, B.M.; Badran, M.; Alqahtani, Q.H.; Abdelhady, H.G.; Alsarra, I. MicroRNA-219 Loaded Chitosan Nanoparticles for Treatment of Glioblastoma. Artif. Cells Nanomed. Biotechnol. 2022, 50, 198–207. [Google Scholar] [CrossRef]
- Kaban, K.; Salva, E.; Akbuga, J. In Vitro Dose Studies on Chitosan Nanoplexes for MicroRNA Delivery in Breast Cancer Cells. Nucleic Acid Ther. 2017, 27, 45–55. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, Y.; Malichewe, C.; Shi, Z.; Wang, L.; Lu, Z. Chitosan Nanoparticle Mediated Upregulation of MicroRNA34a Expression to Suppress the Proliferation, Migration, Invasion of MDA-MB-231 Cells. J. Drug Deliv. Sci. Technol. 2019, 52, 1061–1069. [Google Scholar] [CrossRef]
- Chien, Y.; Chang, Y.L.; Li, H.Y.; Larsson, M.; Wu, W.W.; Chien, C.S.; Wang, C.Y.; Chu, P.Y.; Chen, K.H.; Lo, W.L.; et al. Synergistic Effects of Carboxymethyl-Hexanoyl Chitosan, Cationic Polyurethane-Short Branch PEI in MiR122 Gene Delivery: Accelerated Differentiation of IPSCs into Mature Hepatocyte-like Cells and Improved Stem Cell Therapy in a Hepatic Failure Model. Acta Biomater. 2015, 13, 228–244. [Google Scholar] [CrossRef] [PubMed]
- Sainitya, R.; Sriram, M.; Kalyanaraman, V.; Dhivya, S.; Saravanan, S.; Vairamani, M.; Sastry, T.P.; Selvamurugan, N. Scaffolds Containing Chitosan/Carboxymethyl Cellulose/Mesoporous Wollastonite for Bone Tissue Engineering. Int. J. Biol. Macromol. 2015, 80, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wu, G.; Feng, Z.; Bai, S.; Dong, Y.; Wu, G.; Zhao, Y. Microarc-Oxidized Titanium Surfaces Functionalized with MicroRNA-21-Loaded Chitosan/Hyaluronic Acid Nanoparticles Promote the Osteogenic Differentiation of Human Bone Marrow Mesenchymal Stem Cells. Int. J. Nanomed. 2015, 10, 6675–6687. [Google Scholar] [CrossRef] [Green Version]
- Meng, Y.; Liu, C.; Zhao, J.; Li, X.; Li, Z.; Wang, J.; Wang, R.; Liu, Y.; Yuan, X.; Cui, Z.; et al. An Injectable MiRNA-Activated Matrix for Effective Bone Regeneration: In Vivo. J. Mater. Chem. B 2016, 4, 6942–6954. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Agarwal, P.; Zhao, S.; Yu, J.; Lu, X.; He, X. A Near-Infrared Laser-Activated “Nanobomb” for Breaking the Barriers to MicroRNA Delivery. Adv. Mater. 2016, 28, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Balagangadharan, K.; Viji Chandran, S.; Arumugam, B.; Saravanan, S.; Devanand Venkatasubbu, G.; Selvamurugan, N. Chitosan/Nano-Hydroxyapatite/Nano-Zirconium Dioxide Scaffolds with MiR-590-5p for Bone Regeneration. Int. J. Biol. Macromol. 2018, 111, 953–958. [Google Scholar] [CrossRef]
- Wu, K.; Liu, M.; Li, N.; Zhang, L.; Meng, F.; Zhao, L.; Liu, M. Chitosan-MiRNA Functionalized Microporous Titanium Oxide Surfaces via a Layer-by-Layer Approach with a Sustained Release Profile for Enhanced Osteogenic Activity. J. Nanobiotechnol. 2020, 18, 127. [Google Scholar] [CrossRef]
- Zhao, R.; Wang, S.; Jia, L.; Li, Q.; Qiao, J.; Peng, X. Interleukin-1 Receptor Antagonist Protein (IL-1Ra) and MiR-140 Overexpression via PNNS-Conjugated Chitosan-Mediated Gene Transfer Enhances the Repair of Full-Thickness Cartilage Defects in a Rabbit Model. Bone Jt. Res. 2019, 8, 165–178. [Google Scholar] [CrossRef]
- Sukumar, U.K.; Gambhir, S.S.; Massoud, T.F.; Paulmurugan, R. Intranasal Delivery of Targeted Polyfunctional Gold-Iron Oxide Nanoparticles Loaded with Therapeutic MicroRNAs for Combined Theranostic Multimodality Imaging and Presensitization of Glioblastoma to Temozolomide. Biomaterials 2020, 218, 119342. [Google Scholar] [CrossRef]
- Motiei, M.; Aboutalebi, F.; Forouzanfar, M.; Dormiani, K. Materials Science & Engineering C Smart Co-Delivery of MiR-34a and Cytotoxic Peptides (LTX-315 and Melittin) by Chitosan Based Polyelectrolyte Nanocarriers for Specific Cancer Cell Death Induction. Mater. Sci. Eng. C 2021, 128, 112258. [Google Scholar] [CrossRef]
- Ballarín-gonzález, B.; Ebbesen, M.F.; Howard, K.A. Polycation-Based Nanoparticles for RNAi-Mediated Cancer Treatment. Cancer Lett. 2014, 352, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, M.; Yagi, K.; Iwakawa, S.; Hirai, M. Chitosan Induces Apoptosis via Caspase-3 Activation in Bladder Tumor Cells. Jpn. J. Cancer Res. 2001, 92, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, H.S.; Yadav, P.N. Anticancer Activity of Chitosan, Chitosan Derivatives, and Their Mechanism of Action. Int. J. Biomater. 2018, 2018, 2952085. [Google Scholar] [CrossRef] [Green Version]
- Abedia, Z.; Moghadamnia, A.A.; Zabihi, E.; Pourbagher, R.; Ghasemi, M.; Nouri, H.R.; Tashakorian, H.; Jenabian, N. Anticancer Properties of Chitosan against Osteosarcoma, Breast Cancer and Cervical Cancer Cell Lines. Casp. J. Intern. Med. 2019, 10, 439. [Google Scholar] [CrossRef]
- García, L.; Urbiola, K.; Düzgüneş, N.; Tros De Ilarduya, C. Lipopolyplexes as Nanomedicines for Therapeutic Gene Delivery. Methods Enzymol. 2012, 509, 327–338. [Google Scholar] [CrossRef]
- Chen, W.; Li, H.; Liu, Z.; Yuan, W. Lipopolyplex for Therapeutic Gene Delivery and Its Application for the Treatment of Parkinson’s Disease. Front. Aging Neurosci. 2016, 8, 68. [Google Scholar] [CrossRef] [Green Version]
- Sultankulov, B.; Berillo, D.; Sultankulova, K.; Tokay, T.; Saparov, A. Progress in the Development of Chitosan-Based Biomaterials for Tissue Engineering and Regenerative Medicine. Biomolecules 2019, 9, 470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campardelli, R.; Baldino, L.; Reverchon, E. Supercritical Fluids Applications in Nanomedicine. J. Supercrit. Fluids 2015, 101, 193–214. [Google Scholar] [CrossRef]
- Tahamtan, A.; Teymoori-Rad, M.; Nakstad, B.; Salimi, V. Anti-Inflammatory MicroRNAs and Their Potential for Inflammatory Diseases Treatment. Front. Immunol. 2018, 9, 1377. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).