Abstract
Various short-range radars, such as impulse-radio ultra-wideband (IR-UWB) and frequency-modulated continuous-wave (FMCW) radars, are currently employed to monitor vital signs, including respiratory and cardiac rates (RRs and CRs). However, these methods do not consider the motion of an individual, which can distort the phase of the reflected signal, leading to inaccurate estimation of RR and CR because of a smeared spectrum. Therefore, motion compensation (MOCOM) is crucial for accurately estimating these vital rates. This paper proposes an efficient method incorporating MOCOM to estimate RR and CR with super-resolution accuracy. The proposed method effectively models the radar signal phase and compensates for motion. Additionally, applying the super-resolution technique to RR and CR separately further increases the estimation accuracy. Experimental results from the IR-UWB and FMCW radars demonstrate that the proposed method successfully estimates RRs and CRs even in the presence of body movement.
1. Introduction
Non-contact vital sign estimation (VSE) techniques using radar systems have been extensively researched and employed for various applications [1,2,3,4,5,6,7,8,9,10,11,12,13,14]. These techniques estimate vital signs, such as respiratory and cardiac rates (RRs and CRs), by detecting very small range variations in the skin caused by these vital signs. Because lung and heart vibrations contribute to the movement of the chest and back, the phase of the reflected radar signal contains RR and CR information [15]. Numerous types of short-range radars have been used to accurately extract these phases for VSE [1,2,3,6].
To achieve accurate and cost-effective VSE, various studies have explored the use of continuous-wave (CW), frequency-modulated continuous-wave (FMCW), and impulse-radio ultra-wideband (IR-UWB) signals. One study proposed an efficient CW radar system for RR measurement under one-dimensional body motion [16]. Another method introduced motion compensation (MOCOM) to eliminate phase errors caused by random body movements [17]. This approach assumes a CW signal and uses two echo signals from both the chest and back to cancel phase errors. Schires [18] developed an IR-UWB radar system integrated into a car seat backrest, matched to the human body. Xiang [19] presented a high-precision VSE method using FMCW radar, in which noise was considerably reduced via a variation-mode decomposition (VMD) wavelet-internal-thresholding algorithm. A recently proposed method used a fuzzy rule to accurately determine RR and remove distorted CR values due to motion [20].
Additionally, substantial research has been directed at improving both hardware and software techniques for VSE. Liu et al. [21] suggested an interferometry-based frequency-sweeping technique to achieve high-ranging accuracy and a wide detection range. Gu [22], and Yavari [23] introduced methods based on digital post-distortion and compensation to enhance accuracy by mitigating undesirable interference. To further increase accuracy and suppress noise, signal decomposition methods such as wavelet transform [24] and empirical mode decomposition (EMD) [25] have been applied to VSE.
However, existing methods do not fully address the issues caused by considerable movement of an individual. Continuous motion during observation can result in substantial phase errors. The method described in [16] may fail because, generally, the movement is not one-dimensional. The approach in [17] assumes that the phases caused by forward and backward motions have opposite signs and equal magnitudes, allowing error removal by multiplying the spectra of the forward and backward radars. This method can fail if other motion components are present. Additionally, because the amplitude of the signal reflected from the front of the body is significantly larger than that from the back, spectrum multiplication cannot eliminate forward–backward motion artifacts.
The results in [18] may be significantly degraded if the back moves or if the matching condition between the body and the seat changes. The method in [19] did not incorporate MOCOM, and thus, it could fail with body movement. The approach in [20] fails if the estimated value remains inaccurate over time, as it maintains the previous result once distortion is detected. Methods in [21,22,23] are not relevant to MOCOM and may be inaccurate in the presence of movement. While decomposition methods [24,25] can successfully separate signals in low-noise environments, their accuracy is questionable owing to spectrum blurring, even at very low velocities and accelerations. Moreover, when respiratory and cardiac activities are partially blocked or the radar line-of-sight changes rapidly, the signal-to-noise ratio (SNR) can decrease significantly, leading to poor separation results. Therefore, an efficient method to eliminate the effects of motion is required.
In this study, we propose an efficient method that achieves super-resolution vital sign estimation (VSE) using a low-cost short-range radar. The proposed method involves the following steps:
- Denoising and signal separation: the radar signal is denoised using principal component analysis (PCA).
- Motion compensation (MOCOM): based on an analysis of the phase components of the echo signal, two efficient MOCOM methods, MOCOM and MOCOM , are introduced.
- Noise reduction and auto-focusing: to further reduce noise and enhance resolution, the respiratory and cardiac signals are separated again and auto-focused.
- Super-resolution spectrum estimation: the multiple signal classification (MUSIC) method [26], a super-resolution technique, is used to obtain the spectra of the separated signals with very high resolution.
The remainder of this paper is organized as follows: Section 2 introduces the radar signal model, analyzing the phase components and issues caused by movement. Section 3 details the proposed method. Section 4 presents experimental results demonstrating the method’s efficiency, and Section 5 concludes the paper.
2. Signal Model and Problem Analysis
2.1. Radar Signal Model
To apply the proposed method to various low-cost radars, the signal models of two representative short-range radars were assumed to be IR-UWB and FMCW. Using the observation geometry shown in Figure 1, the methods employed in previous studies [20,27] were modified, where is the radar line-of-sight (RLOS) vector. When there is no body movement, the range vector of the chest caused by RR is and the range variation along the RLOS is given by
where · denotes the inner product operator, denotes the variation in chest skin, represents the initial phase, and
is the real-time respiration rate, where denotes the fundamental RR frequency and represents the slight variation amplitude in the respiration rate responsible for high-order harmonics.
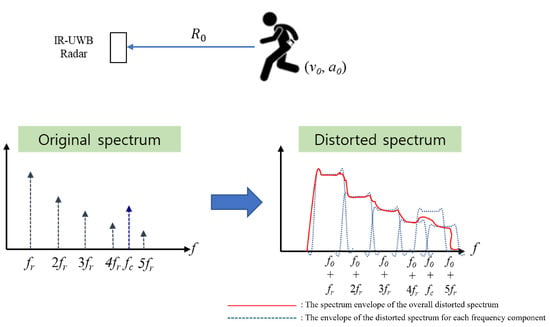
Figure 1.
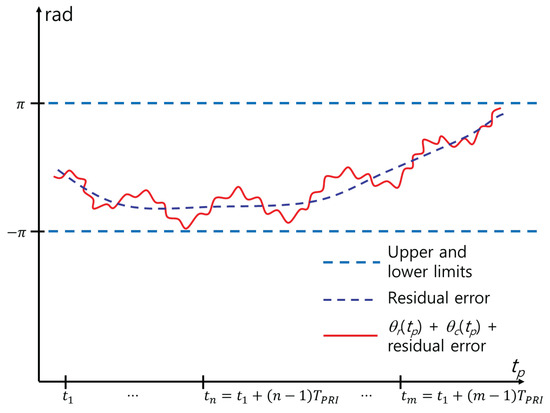
Example of the spectrum distortion caused by and .
Similarly, the range vector of the chest caused by the CR is and its projection along the RLOS is
where is the variation in the chest skin, is the initial phase, and
is the real-time CR function.
For the transmitted signal, we assumed the following functions of the IR-UWB and FMCW radars with bandwidth B:
where
where denotes the amplitude, denotes the Gaussian pulse with B, denotes the carrier frequency of the transmitted signal, , and denotes the width of the transmitted chirp. The received FMCW signal is compressed into a sinc function by de-chirping and employing a Fourier transform (FT) [28].
For the chest observed with a given pulse repetition time , the received signal of the IR-UWB and FMCW radars is expressed as
where and for the IR-UWB and FMCW radars, respectively. is the slow time sampled at , and the time delay is
c is the velocity of light, and is the range variation of the body that should be removed. is the amplitude of the received signal and can be expressed by the radar equation as follows:
where and are the gains of the transmitting and receiving antennas, respectively; is the wavelength, is the radar cross-section, and R is the distance to the chest.
is down-converted to baseband signal as follows:
Assuming , where is the initial range and and are the velocity and acceleration of the body, respectively, (11) becomes
2.2. Effect of the Motion of the Rigid Body
The clipped signal at range r with maximum energy is a function of only and contains information on and . is given by
The Fourier transform of can be expressed as
where denotes the FT operation, and ⊗ denotes the convolution operation.
As the first component is a constant envelope of one, its effect can be eliminated. The FT of the second exponential component in the above equation is a linear frequency modulation signal due to the acceleration shifted by the Doppler frequency . Using the stationary phase method [29], it can be transformed into
where is a rectangle function, is the coherent processing interval, and K is given by
The FT of the third and fourth components can be divided into in-phase and quadrature components as follows:
where and are the in-phase and quadrature components of RR, respectively, and and are those of CR. , , , and can be approximated using the Bessel function of the first type of order i as follows [17]:
where , , and for and . Notably, i and j cannot be zero simultaneously, as they represent the DC component.
Equations (2), (4), and (19)–(22) represent spectra of RR and CR, composed of harmonics of and ; as is higher for smaller i and RR has a larger (e.g., m) than (e.g., m), has the largest amplitude. However, the harmonics of may have negative effects on when they coincide with .
The convolution of the discrete spectra of (17) and (18) with the FT of (15) yielded a distorted spectrum owing to the frequency modulation caused by the acceleration and shift of the modulated spectrum (Figure 1). In the case where m/s and , a peak appears at a false location owing to , and when m/s and , the spectrum can be blurred because of the convolution with the Doppler bandwidth caused by . With nonzero and , the spectrum is severely distorted, as the peaks are both displaced and blurred. Therefore, MOCOM is an indispensable preprocessing step for accurate RRE and CRE.
Eliminating the effect of and using MOCOM is challenging. One probable method is to estimate first by identifying the largest peak in and subsequently focusing the spectrum by finding . However, the exact value of can seldom be found because the shape of the spectrum caused by may not be flat; because of Gibbs’ phenomenon, overshot values can be larger than that at , and the fluctuation of the Doppler bandwidth owing to and the interference by neighboring harmonics makes the spectrum more irregular. Therefore, should not occur in the presence of and .
The problem of finding peaks in the spectrum of can be solved simply by using the phase information, that is, the arctangent demodulation of , given as
where and are the in-phase and quadrature components of , respectively and is the wavelength of . is significantly distorted by because it is considerably larger than and (Figure 2). To avoid ambiguity in extracting , a phase unwrapping technique should be used [20].
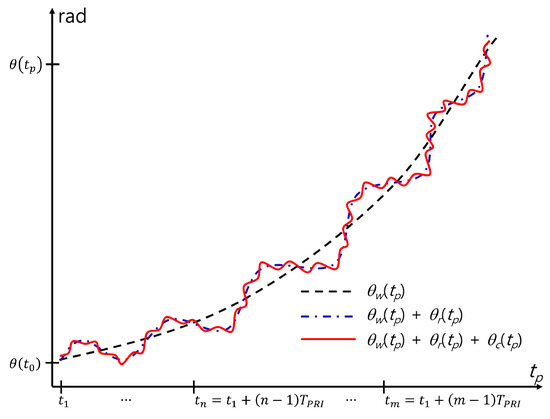
Figure 2.
Example of the phase distortion caused by and .
Considering the effects of the surrounding clutter and noise, (23) is modified as follows:
where and are the phases of system noise and background clutter, respectively. As includes a linear mixture of the effects of the body, noise, and clutter, RRE and CRE become more challenging.
When Fourier transformed, is the linear component of each component, as follows:
Because is constant, has a large amplitude at Hz. In addition, and are the two cosine functions of and , respectively, and the peaks can appear at the corresponding frequencies. However, the effect of should be removed before the FT of , because it has a very large amplitude (see Figure 3). In addition, the effects of and should be minimized.
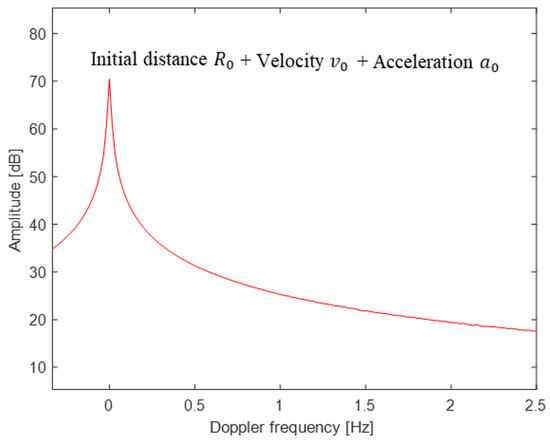
Figure 3.
Example of blurred noise due to m/s and ( dB). Note that even very small velocities and accelerations can alter the spectrum of the phase.
3. Proposed Method
3.1. Summary of the Proposed Method
This subsection introduces an efficient method for estimating the vital parameters and with super-resolution by compensating for motion and applying the MUSIC algorithm (Figure 4).
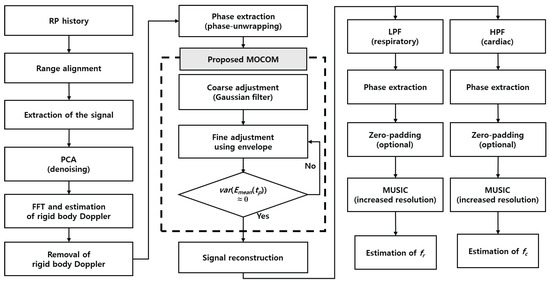
Figure 4.
Proposed signal processing procedure.
- ①
- Range alignment: the range profile history is aligned to position the scatterer at the same location during the coherent processing interval, thereby eliminating range migration caused by movement.
- ②
- Radar signal clipping: the radar signal is clipped around the range bin with the maximum energy to enhance SNR.
- ③
- PCA denoising: PCA helps isolate the vital signals from the background noise and clutter, which is critical for accurate estimation.
- ④
- Removal of the rigid-body Doppler: the Doppler frequency corresponding to the rigid body’s velocity is estimated using a fast Fourier transform (FFT) and is then compensated.
- ⑤
- Phase unwrapping: a phase unwrapping technique is applied to extract the phase history.
- ⑥
- MOCOM (Gaussian filtering): The phase history is coarsely estimated using a Gaussian filter to remove phase errors caused by body movement.
- ⑦
- MOCOM (Envelope fitting): the envelope of the phase history is fitted to minimize residual errors that were not compensated for in MOCOM .
- ⑧
- Signal reconstruction: the complex signal is reconstructed using amplitude- and motion-compensated phases.
- ⑨
- Signal separation: low-pass (LPF) and high-pass filters (HPF) are used to separate the respiratory and cardiac signals.
- ⑩
- Phase adjustment: residual phase errors are removed using a phase-adjustment technique for each of the separated signals.
- ⑪
- Vital parameters estimation: and are estimated by identifying the maximum peaks in each super-resolution spectrum, which are generated via zero-padding and the MUSIC algorithm.
3.2. Main Idea of the Proposed Method
3.2.1. Range Alignment
First, because in (7) is heavily dependent on and , the scatterer migrates into neighboring range bins. Consequently, cannot be formed by clipping at a fixed range . Therefore, the RPs should be aligned such that the scatterer is located in the same range bin for all . While exact estimation of motion parameters and is impossible without errors, we used a widely adopted non-parametric method. Among various methods, we employed entropy minimization, which is commonly used in inverse synthetic aperture radar imaging [30].
The entropy between two RPs and is defined by
where
and is the maximum range. According to this criterion, the value that minimizes the 1D entropy is the shift that aligns well with . Consequently, the second RP of and the relative shift minimizing (26) along with the average of the aligned RPs are determined. The RP is aligned with a shift by .
3.2.2. Extraction of Vital Signals and Denoising Using PCA
Because the RPs of the body can be contaminated by noise or surrounding clutter, the phase of the RP can be distorted. In addition, determining the exact location of the chest is difficult, because the reflected signal is the sum of several body parts, mainly the torso, which can be buried within the torso signal. Therefore, we applied PCA to denoise and decompose vital signals.
Assuming n RPs, let be an matrix constructed by sampling range bins around the range bin with the maximum energy as follows:
where
the covariance matrix is calculated by
where H is the conjugate transpose of the vector. Subsequently, the eigenvalue decomposition of is used, given by
According to PCA, the orthonormal eigenvectors corresponding to large eigenvalues span the signal subspace of the , while those corresponding to small eigenvalues span the noise subspace. Additionally, because the large-valued torso signal corresponds to projected onto the eigenvector with the largest eigenvalue, the small-valued respiratory and cardiac signals can be separated by projections onto eigenvectors with smaller eigenvalues. The matrix is projected onto as
Finally, the denoised sum of the respiratory and the cardiac signal is
and it is used instead of the in (13). Note that is a function of .
3.2.3. Estimation and Removal of the Rigid-Body Doppler
The Doppler frequency corresponding to the rigid body velocity is estimated by
where denotes the FFT function. The rigid-body phase error is removed using
3.2.4. MOCOM
Although the rigid-body Doppler is removed using (35), the spectrum can be blurred by the effect of the acceleration of the rigid body. In addition, because the FT of the acceleration component yields a Doppler bandwidth with an irregular passband (Figure 1), the estimation of v0 may not be accurate. Consequently, Equation (35) may yield an estimation error, resulting in a shift in the frequency components of .
This problem can be solved using only unwrapped . includes the linear sum of , , and , and can be addressed separately. Because the spectrum is severely blurred in the frequency domain of the phase, extracting this component by applying signal-separation methods is difficult. In addition, because the shape of the unwrapped phase includes the effects of motion, removing the motion component from the time domain is more profitable.
The error can be perfectly removed once the motion component is accurately estimated using a proper polynomial, such as to describe , and a curve-fitting algorithm to find the parameter . However, the curve-fitting algorithm is time-consuming, and numerous phase errors can occur if does not match accurately. Therefore, we coarsely compensated for the motion using a smoothing kernel function to smooth . Among the various methods, we used the following Gaussian kernel:
where is the sampling interval of , is the standard deviation of the kernel, and is the mean value of .
The smoothed phase for the MOCOM is given by
Equation (37) is time consuming; therefore, it is converted in the frequency domain as follows:
where is the inverse FT. Finally, by directly subtracting from as follows:
the effect of is eliminated. This method is direct and relatively simple (Figure 5). However, includes errors because various errors caused by phase unwrapping and noise cause a mismatch between and the actual phase trajectory. In Figure 5, red and blue lines represent and the residual error caused by this mismatch, respectively. As a result, additional MOCOM is required. Therefore, we define this MOCOM as MOCOM to distinguish it from the additional MOCOM, MOCOM .
3.2.5. MOCOM
The MOCOM proposed in this study reduces the residual error, as shown in Figure 5. Owing to the sinusoidal nature of the respiratory and cardiac signals, the sum of the motion-compensated signals in the time domain fluctuates within constant upper and lower limits (Figure 6). Therefore, the ideal MOCOM flattens the phase by estimating the unknown residual error, as shown in Figure 3. A parametric method is ineffective for estimating that curve. Instead, we successively use three phase envelopes after MOCOM : the upper, lower, and mean envelopes (Figure 7).
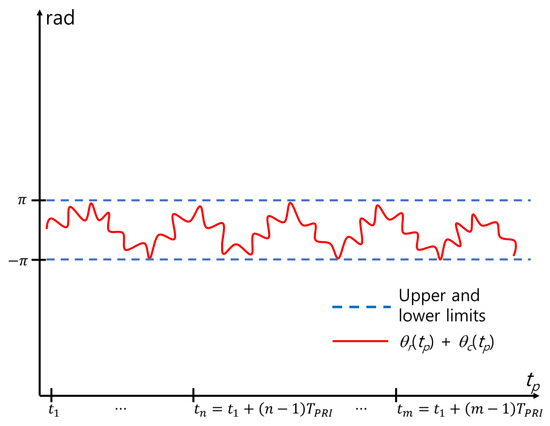
Figure 6.
Phase after ideal MOCOM.
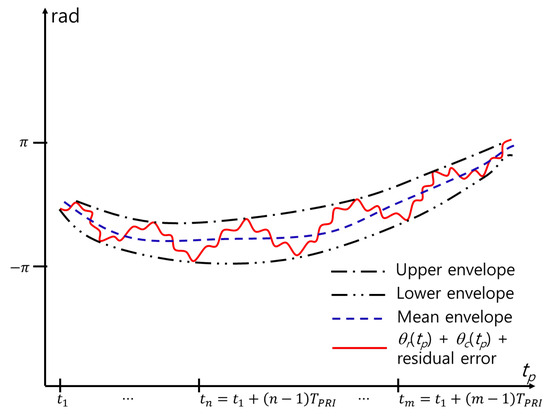
Figure 7.
Envelopes for MOCOM .
Various methods for detecting the envelope of a signal in a communication area exist, such as squaring, low-pass filtering, and the Hilbert transform [31,32]. In this study, we use a simple detection method by using the maximum (or minimum) within a window with length L. By moving a window from left to right with a given time step , the maximum value within the window is stored as , and the minimum value is stored as , where . is the length of the time frame, and is the function that determines the nearest integer (Figure 8). Zeros are added when the number of signals is smaller than L near the start and end of .
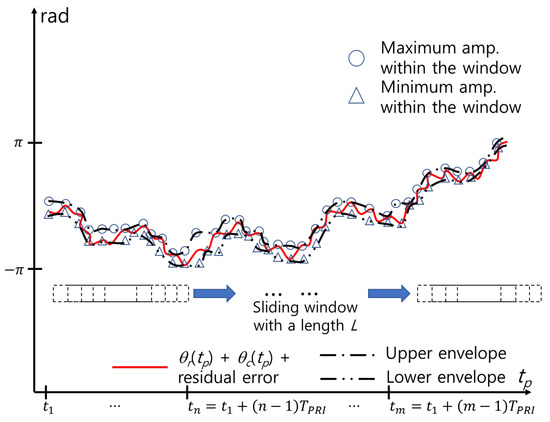
Figure 8.
Estimation of envelopes using cubic spline interpolation.
The upper envelope and lower envelope are then obtained by curve-fitting and . Among various methods, we use the cubic spline interpolation method [33]. Finally, the mean envelope is obtained as
and the error is reduced by
However, depending on the length of the window L and time step , the envelope may not describe the overall shape of . In particular, near and , the estimated envelope may increase or decrease significantly, owing to the zeros added to the window. In addition, the maximum and minimum values at a certain time may be the same, yielding a large difference from the near maximum or minimum value. In this case, may not be flat but curved near that point. This problem can be solved by applying MOCOM successively until the variance of is close to 0; that is,
3.2.6. Reconstruction of Signals and Separation of Vital Signals Using LPF and HPF
To further remove the residual phase errors and obtain super-resolution for and , the complex signal is first reconstructed as follows:
Subsequently, (43) is separated into respiratory and cardiac signals, that is, and , respectively. Because the amplitudes of the cardiac spectrum are very small and can be influenced by the ripples of the passband, we used a maximally flat Butterworth filter: LPF for the respiratory signal and HPF for the cardiac signal, in the following form:
where is the filter order.
3.2.7. Phase Adjustment
Despite its maximum flatness, contains only CR and RR frequencies. The residual phase errors may occur owing to estimation error, noise, and clutter. Consequently, residual errors should be removed using an appropriate method. The residual error is significantly reduced by using MOCOM and ; therefore, we used the 1D entropy of the following signal spectrum:
where is the filtered signal, representing either and . Subsequently, the phase-error is determined by minimizing the entropy, defined by
where
and . This method is a major topic of interest and is known as phase adjustment in radar imaging. In this study, we applied the widely used minimum entropy phase adjustment (MEPA) [34]. The MEPA is fast and can be conducted in real-time using the entropy gradient.
3.2.8. Zero-Padding and Application of MUSIC
To improve estimation accuracy, the phase-adjusted signal is zero-padded to upsample the spectrum. Subsequently, MUSIC is applied to the zero-padded (optional) signal to obtain a super-resolution spectrum. MUSIC uses the characteristic that the direction vector containing the signal is orthogonal to the noise subspace consisting of noise eigenvectors.
Using the vector containing N samples of the phase of the radar signal after the phase adjustment, which is given by
the covariance matrix , where is the ensemble average, is estimated by applying the modified spatial smoothing preprocessing to decorrelate signals from various frequency components as follows:
where
and
In (49), is the number of subarrays, and is the subarray dimension. Equation (47) is the average obtained by clipped by two windows of size moving forward and backward [26].
Assuming the number of frequency components L, the noise subspace matrix consisting eigenvectors of corresponding to the smallest eigenvalues is obtained, and the super-resolution spectrum is obtained as
where the direction vector at a frequency f is defined by
In (54), f can be set with infinite resolution, which is a major advantage of the MUSIC algorithm. In this study, we divided the signal into respiratory and cardiac signals and set f around and with a very high resolution, which may require very long observations if the FT is employed.
4. Experimental Results
4.1. Experimental Condition
To demonstrate the efficiency of the proposed method for VSE in the presence of body movement using measurements from general low-cost short-range radar, we used both IR-UWB and FMCW radars. For the IR-UWB radar, we employed the parameters of the X4M03 produced by Novelda (Oslo, Norway), and for the FMCW radar, we used those of the Distance2GoL by Infineon (Neubiberg, Germany) (see Table 1). The radar signals of both radars were modeled, and and were estimated using the proposed method. A time frame of 40 s was used to obtain the spectrum with a 0.025 Hz resolution, and the time frame was moved with a step of 1 s to ensure overlapping neighboring frames.

Table 1.
Experiments and measurement parameters.
Measurements were conducted using both the X4M03 and Distance2GoL radars. The subject was positioned approximately 2 m away from the radar sensor. Using the same frame time and frame step as in the experiment, the s and s of the received signal were estimated. To evaluate the accuracy of these estimations, actual s and s were measured using a wearable metabolic system, the K5 produced by COSMED, and compared with the estimated values (see Figure 9).

Figure 9.
Measurement of VSE.
To facilitate computation, we used MATLAB for the experiment and measurement processes. We employed the functions , , and for phase unwrapping, eigenvalue decomposition, and the Butterworth filter, respectively. For envelope detection, the parameters were set as and 6 s for IR-UWB and and 6 s for FMCW. The Butterworth filter parameters were defined as and for the ranges of RR and CR, respectively. For , was set to 0.7. The MUSIC algorithm was applied to the zero-padded signal, with zeros equal to the length of the signal added; was set to 801 for IR-UWB and 1601 for FMCW. For each radar, the frequency was sampled at 0.0033 Hz for RR and 0.005 Hz for CR.
In this study, we compared the estimation accuracy of the proposed method with that of four different previous methods cited in [16,20,25,35]. The methods are as follows:
- The method in [16] compensated for phase error by detecting constant Doppler shift due to random body movement.
- The conventional method in [20] used a fuzzy rule to mitigate the effects of random movement.
- The method in [25] employed empirical mode decomposition (EMD).
- The method in [35] used VMD to detect vital signs.
4.2. Estimation Accuracy and Robustness of the Proposed Scheme
The experimental results confirm the efficiency of the proposed method (Figure 10 and Figure 11). Entropy minimization successfully aligned the RPs of the IR-UWB and FMCW radars (Figure 10b and Figure 11b). However, the phase of the signal post-PCA was considerably distorted owing to motion, obscuring the sinusoidal patterns of the RR and CR (Figure 10c and Figure 11c).
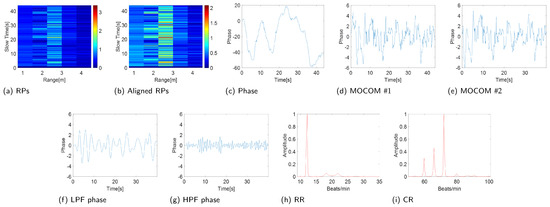
Figure 10.
Experimental results (IR-UWB: X4M03).
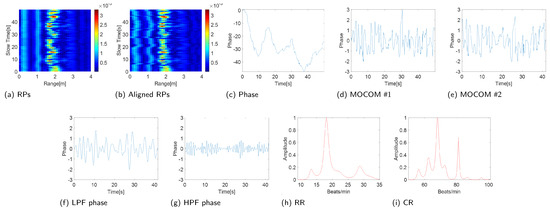
Figure 11.
Experimental results (FMCW: Distance2GoL).
The proposed MOCOM effectively removed motion artifacts. As the movement was accurately modeled by (38), the phase error was substantially reduced, revealing a clear sinusoidal pattern in the phase components’ envelope (Figure 10d and Figure 11d). Additionally, MOCOM further eliminated residual errors, resulting in an even more pronounced sinusoidal pattern (Figure 10e and Figure 11e).
After applying LPF and HPF, the phase data clearly represented RR and CR (Figure 10f,g and Figure 11f,g). Compared with the combined signal of RR and CR, the sinusoidal pattern of CR was distinctly observable. Ultimately, the MUSIC algorithm accurately estimated both RR and CR (Figure 10h,i and Figure 11h,i).
The robust VSE performance of the proposed method was validated by comparing the estimated performance of the proposed scheme with the four existing techniques, as shown in Figure 12 and Figure 13. Furthermore, to evaluate the accuracy of the proposed scheme quantitatively, we computed the root-mean-square error (RMSE) between the RR and CR measured by the wearable metabolic system and estimated by the two radar systems. The RMSE is calculated as
where and are the measured and estimated values, respectively, and denotes the number of frames.
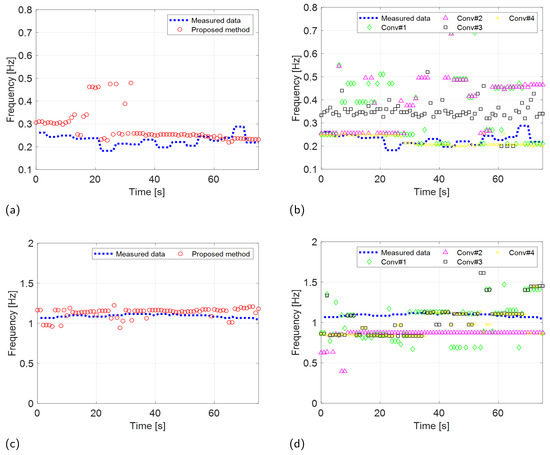
Figure 12.
Experimental results (IR-UWB: X4M03) comparing the VSE performance of the proposed and conventional methods. RR estimation of the (a) proposed and (b) conventional methods. CR estimation of the (c) proposed and (d) conventional methods.
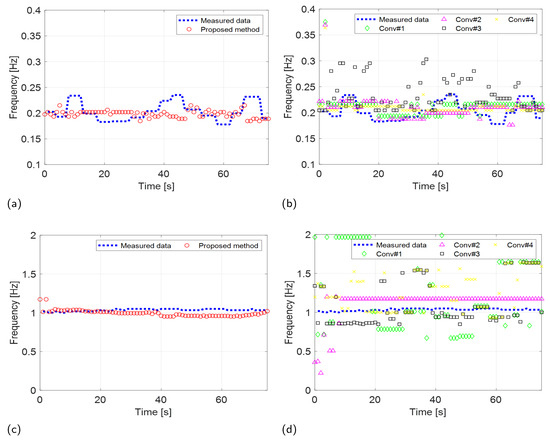
Figure 13.
Experimental results (FMCW: Distance2GoL) comparing the VSE performance of the proposed and conventional methods. RR estimation of the (a) proposed and (b) conventional methods. CR estimation of the (c) proposed and (d) conventional methods.
The results of the experiments conducted using the two radar systems are summarized in Table 2. Both the proposed and existing methods described in [35] demonstrated accurate estimation of RRs with an RMSE of less than 0.1 Hz in scenarios involving IR-UWB and FMCW radar systems. In contrast, conventional methods outlined in [16,20,25] exhibited significantly higher RMSEs when estimating RRs using the IR-UWB radar system. The performance of the proposed method in CR estimation was also significantly superior to that of the conventional methods.

Table 2.
Comparison between RMSE of estimated RR and CR of conventional methods and proposed method.
In the Fuzzy rule-based method presented in [20], the initially estimated RRs and CRs were used as threshold values for the membership function in fuzzy logic rules. This method depends solely on fuzzy rules without incorporating any compensation techniques for VSE in subjects with random body movements. Consequently, the accuracy of VSE using this approach is highly dependent on the selected fuzzy logic thresholds. Determining appropriate thresholds using initial estimates is particularly challenging in this experiment, as vital signs were estimated for a subject with random body movements, even in the initial phases of the experiment.
Conventional methods referenced in [16,25,35] identified the desired RR and CR by selecting the first maximum peak in each spectrum. These peaks were isolated using bandpass filters in [16], EMD in [25], and VMD in [35]. However, because these methods do not account for motion compensation, their VSE accuracy is compromised by phase distortions caused by random body movements. Consequently, these conventional methods are inadequate for detecting vital signs in individuals with significant body movement.
5. Conclusions
In this study, we present a novel algorithm designed to enhance VSE accuracy in the presence of body movement by incorporating a motion compensation technique. The proposed scheme follows a four-step process: 1. Radar signal denoising using PCA: this step reduces noise and enhances signal clarity. 2. Phase distortion compensation with two MOCOM methods: These techniques correct distortions caused by body movements. 3. Separation of respiratory and cardiac signals using a bandpass filter: this step isolates the vital signs for a more accurate analysis. 4. VSE using the MUSIC method: this algorithm step ensures a precise estimation of vital signs.
Experimental results with IR-UWB and FMCW radar systems demonstrated that our method provides more accurate and robust VSE than conventional methods, especially in scenarios involving random body movements.
Future studies will focus on the biomechanical analysis of walking humans. We plan to extend our algorithm to estimate not only vital signs but also walking parameters. The presence of various micro-movements related to respiration, heartbeat, and limb movements leads to mutual interference and phase ambiguity in the received signals. To address these challenges, we aim to employ an MIMO radar system.
Author Contributions
Methodology, I.C. and M.K.; Software, S.P.; Resources, S.K. and J.J.; Writing—original draft, S.Y.; Writing—review & editing, M.K.; Project administration, B.K. and Y.B.; Funding acquisition, S.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the project titled ‘Development of Polar Region Communication Technology and Equipment for Internet of Extreme Things (IoET)’, funded by the Ministry of Science and ICT (MSIT), Republic of Korea (No. RS-2021-KS211508).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. RS-2023-00239144).
Conflicts of Interest
Author Soobum Kim was employed by the company Radsys. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction Statement
This article has been republished with a minor correction to the Funding statement. This change does not affect the scientific content of the article.
References
- Staderini, E. UWB radars in medicine. IEEE Aerosp. Electron. Syst. Mag. 2002, 17, 13–18. [Google Scholar] [CrossRef]
- Droitcour, A.; Boric-Lubecke, O.; Lubecke, V.; Lin, J.; Kovacs, G. Range correlation and I/Q performance benefits in single-chip silicon Doppler radars for noncontact cardiopulmonary monitoring. IEEE Trans. Microw. Theory Tech. 2004, 52, 838–848. [Google Scholar] [CrossRef]
- Gu, C.; Li, R.; Zhang, H.; Fung, A.Y.C.; Torres, C.; Jiang, S.B.; Li, C. Accurate Respiration Measurement Using DC-Coupled Continuous-Wave Radar Sensor for Motion-Adaptive Cancer Radiotherapy. IEEE Trans. Biomed. Eng. 2012, 59, 3117–3123. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Zhao, Z.; Wang, Y.; Zhang, H.; Lin, F. Noncontact Accurate Measurement of Cardiopulmonary Activity Using a Compact Quadrature Doppler Radar Sensor. IEEE Trans. Biomed. Eng. 2014, 61, 725–735. [Google Scholar] [CrossRef]
- An, Y.J.; Yun, G.H.; Yook, J.G. Sensitivity Enhanced Vital Sign Detection Based on Antenna Reflection Coefficient Variation. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 319–327. [Google Scholar] [CrossRef]
- Li, C.; Peng, Z.; Huang, T.Y.; Fan, T.; Wang, F.K.; Horng, T.S.; Muñoz-Ferreras, J.M.; Gómez-García, R.; Ran, L.; Lin, J. A Review on Recent Progress of Portable Short-Range Noncontact Microwave Radar Systems. IEEE Trans. Microw. Theory Tech. 2017, 65, 1692–1706. [Google Scholar] [CrossRef]
- Park, J.K.; Hong, Y.; Lee, H.; Jang, C.; Yun, G.H.; Lee, H.J.; Yook, J.G. Noncontact RF Vital Sign Sensor for Continuous Monitoring of Driver Status. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 493–502. [Google Scholar] [CrossRef]
- Zhang, Y.; Qi, F.; Lv, H.; Liang, F.; Wang, J. Bioradar Technology: Recent Research and Advancements. IEEE Microw. Mag. 2019, 20, 58–73. [Google Scholar] [CrossRef]
- Lee, H.; Kim, B.H.; Park, J.K.; Kim, S.W.; Yook, J.G. A Resolution Enhancement Technique for Remote Monitoring of the Vital Signs of Multiple Subjects Using a 24 Ghz Bandwidth-Limited FMCW Radar. IEEE Access 2020, 8, 1240–1248. [Google Scholar] [CrossRef]
- Lazaro, A.; Girbau, D.; Villariono, R. Analysis of vital signs monitoring using an IR-UWB radar. Prog. Electromagn. Res. 2010, 1, 100. [Google Scholar] [CrossRef]
- Nezirovic, A.; Yarovoy, A.G.; Ligthart, L.P. Signal Processing for Improved Detection of Trapped Victims Using UWB Radar. IEEE Trans. Geosci. Remote Sens. 2010, 48, 2005–2014. [Google Scholar] [CrossRef]
- Sachs, A. Handbook of Ultra-Wideband Short-Range Sensing: Theory Sensors Applications; John Wiley and Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R.M. Techniques for Clutter Suppression in the Presence of Body Movements during the Detection of Respiratory Activity through UWB Radars. Sensors 2014, 14, 2595–2618. [Google Scholar] [CrossRef] [PubMed]
- Jürgen, S.; Herrmann, R. M-sequence-based ultra-wideband sensor network for vitality monitoring of elders at home. IET Radar Sonar Navig. 2015, 9, 125–137. [Google Scholar] [CrossRef]
- Adib, F.; Mao, H.; Kabelac, Z.; Katabi, D.; Miller, R.C. Smart Homes that Monitor Breathing and Heart Rate. In Proceedings of the CHI Conference on Human Factors in Computing Systems, New York, NY, USA, 18–23 April 2015; CHI ’15. pp. 837–846. [Google Scholar] [CrossRef]
- Tu, J.; Hwang, T.; Lin, J. Respiration Rate Measurement Under 1-D Body Motion Using Single Continuous-Wave Doppler Radar Vital Sign Detection System. IEEE Trans. Microw. Theory Tech. 2016, 64, 1937–1946. [Google Scholar] [CrossRef]
- Li, C.; Lin, J. Random Body Movement Cancellation in Doppler Radar Vital Sign Detection. IEEE Trans. Microw. Theory Tech. 2008, 56, 3143–3152. [Google Scholar] [CrossRef]
- Schires, E.; Georgiou, P.; Lande, T.S. Vital Sign Monitoring Through the Back Using an UWB Impulse Radar With Body Coupled Antennas. IEEE Trans Biomed. Circuits Syst. 2018, 12, 292–302. [Google Scholar] [CrossRef]
- Xiang, M.; Ren, W.; Li, W.; Xue, Z.; Jiang, X. High-Precision Vital Signs Monitoring Method Using a FMCW Millimeter-Wave Sensor. Sensors 2022, 22, 7543. [Google Scholar] [CrossRef]
- Choi, I.; Kim, M.; Choi, J.; Park, J.; Park, S.; Kim, K. Robust Cardiac Rate Estimation of an Individual. IEEE Sens. 2021, 21, 15053–15064. [Google Scholar] [CrossRef]
- Liu, T.H.; Hsu, M.L.; Tsai, Z.M. High Ranging Accuracy and Wide Detection Range Interferometry Based on Frequency-Sweeping Technique With Vital Sign Sensing Function. IEEE Trans. Microw. Theory Tech. 2018, 66, 4242–4251. [Google Scholar] [CrossRef]
- Gu, C.; Peng, Z.; Li, C. High-Precision Motion Detection Using Low-Complexity Doppler Radar With Digital Post-Distortion Technique. IEEE Trans. Microw. Theory Tech. 2016, 64, 961–971. [Google Scholar] [CrossRef]
- Yavari, E.; Boric-Lubecke, O. Channel Imbalance Effects and Compensation for Doppler Radar Physiological Measurements. IEEE Trans. Microw. Theory Tech. 2015, 63, 3834–3842. [Google Scholar] [CrossRef]
- He, M.; Nian, Y.; Liu, B. Noncontact heart beat signal extraction based on wavelet transform. In Proceedings of the 2015 8th International Conference on Biomedical Engineering and Informatics (BMEI), Shenyang, China, 14–16 October 2015; pp. 209–213. [Google Scholar] [CrossRef]
- Feng, J.C.; Pan, S.Y. Extraction algorithm of vital signals based on empirical mode decomposition. J. South China Univ. Technol. 2010, 38, 1–6. [Google Scholar] [CrossRef]
- Kim, K.T.; Seo, D.K.; Kim, H.T. Efficient radar target recognition using the MUSIC algorithm and invariant features. IEEE Trans. Antennas Propag. 2002, 50, 325–337. [Google Scholar] [CrossRef]
- Yoon, S.; Kim, S.; Jung, J.; Cha, S.; Baek, Y.; Koo, B.; Choi, I.; Park, S. Efficient Protocol to Use FMCW Radar and CNN to Distinguish Micro-Doppler Signatures of Multiple Drones and Birds. IEEE Access 2022, 10, 26033–26044. [Google Scholar] [CrossRef]
- Mahuza, B. Radar Systems Analysis and Design Using MATLAB, 4th ed.; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Soumekh, M. Synthetic Aperture Radar Signal Processing with MATLAB Algorithms, 1st ed.; Wiley: Hoboken, NJ, USA, 1999. [Google Scholar]
- Zheng, J.; Liu, H.; Liao, G.; Su, T.; Liu, Z.; Liu, Q.H. ISAR Imaging of Targets With Complex Motions Based on a Noise-Resistant Parameter Estimation Algorithm Without Nonuniform Axis. IEEE Sens. 2016, 16, 2509–2518. [Google Scholar] [CrossRef]
- Anupama, V.; Ranjith, M.R.; Roshini, M.; Sowmyah, N.; Vidhya, L. Comparison of curve fitting methods for synthetic generation of PPG. In Proceedings of the 2023 IEEE 20th India Council International Conference (INDICON), Hyderabad, India, 14–17 December 2023; pp. 447–451. [Google Scholar] [CrossRef]
- Pozar, D.M. Microwave Engineering; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Faires, J.D.; Burden, R.L. Numerical Methods; Brooks Cole: Pacific Grove, CA, USA, 2002. [Google Scholar]
- Wang, J.; Kasilingam, D.; Liu, X.; Zhou, Z. ISAR minimum-entropy phase adjustment. In Proceedings of the 2004 IEEE Radar Conference (IEEE Cat. No.04CH37509), Philadelphia, PA, USA, 29–29 April 2004; pp. 197–200. [Google Scholar] [CrossRef]
- Ding, C.; Yan, J.; Zhang, L.; Zhao, H.; Hong, H.; Zhu, X. Noncontact multiple targets vital sign detection based on VMD algorithm. In Proceedings of the 2017 IEEE Radar Conference (RadarConf), Seattle, WA, USA, 8–12 May 2017; pp. 0727–0730. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).