Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
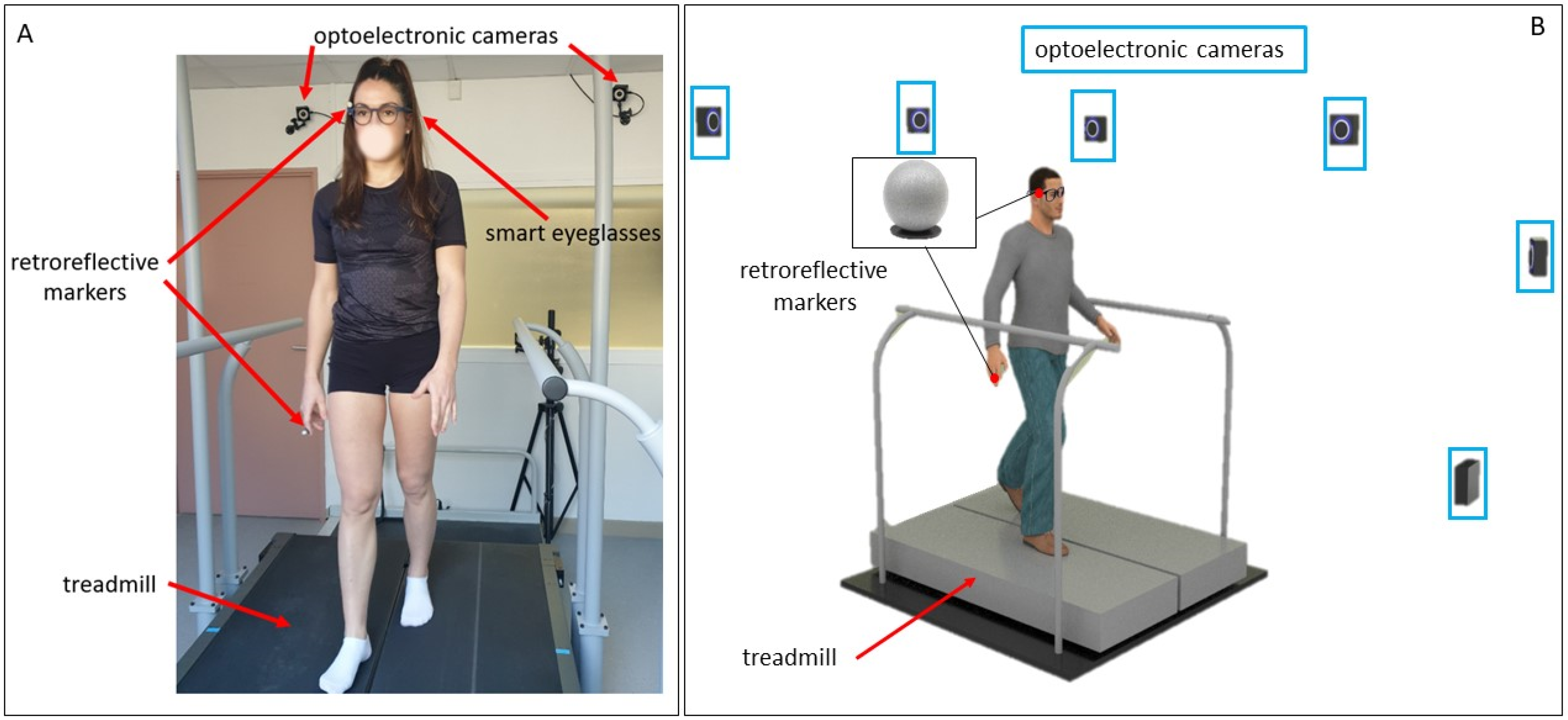
2.3. Apparatus, Data Collection
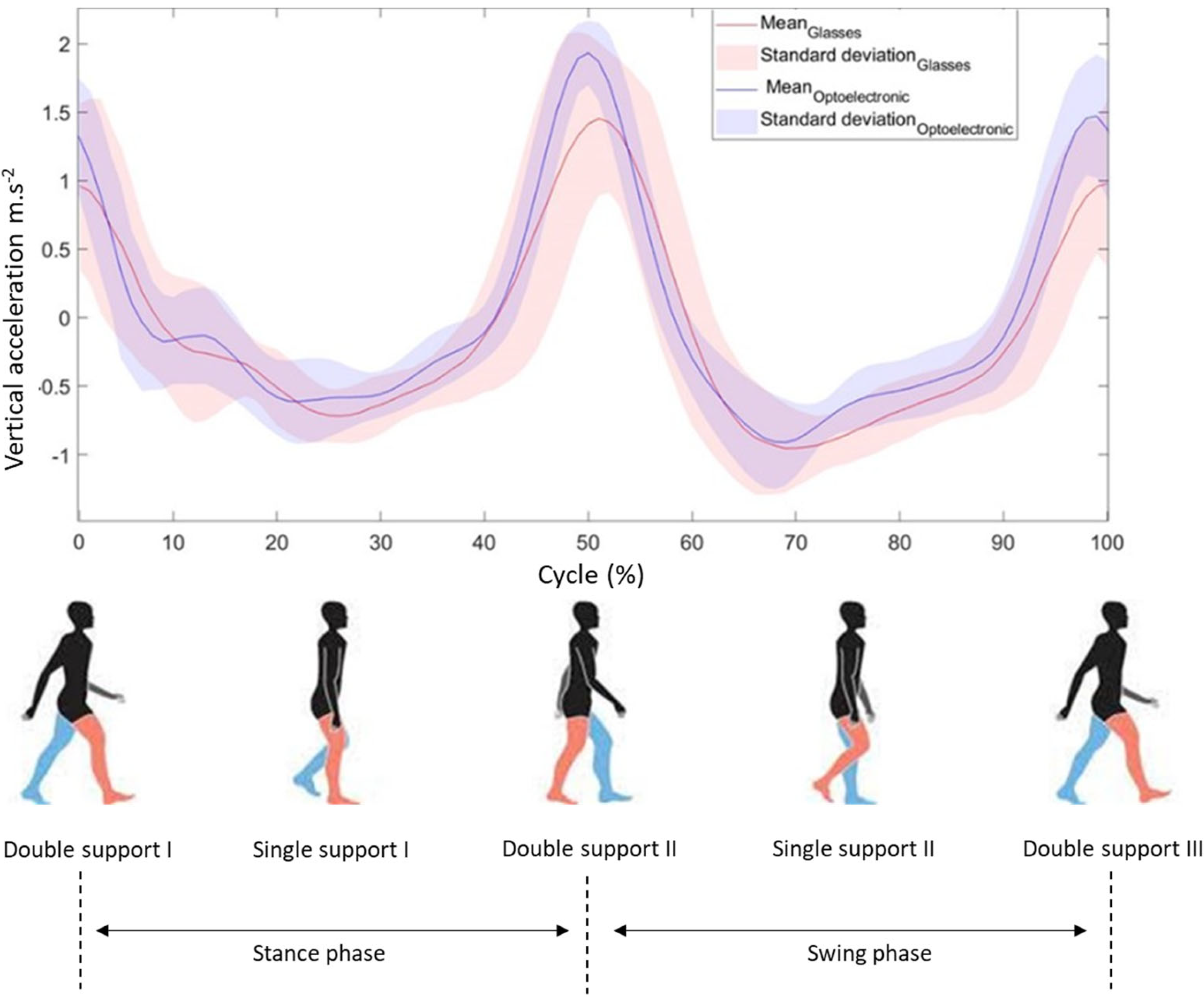
2.4. Analysis
2.5. Statistics
3. Results
3.1. Intra- and Inter-Session Reproducibility of Step Duration and Step Length Measured with the Glasses and Optoelectronic System
3.2. Intra- and Inter-Session Reliability of the Glasses and the Optoelectronic System
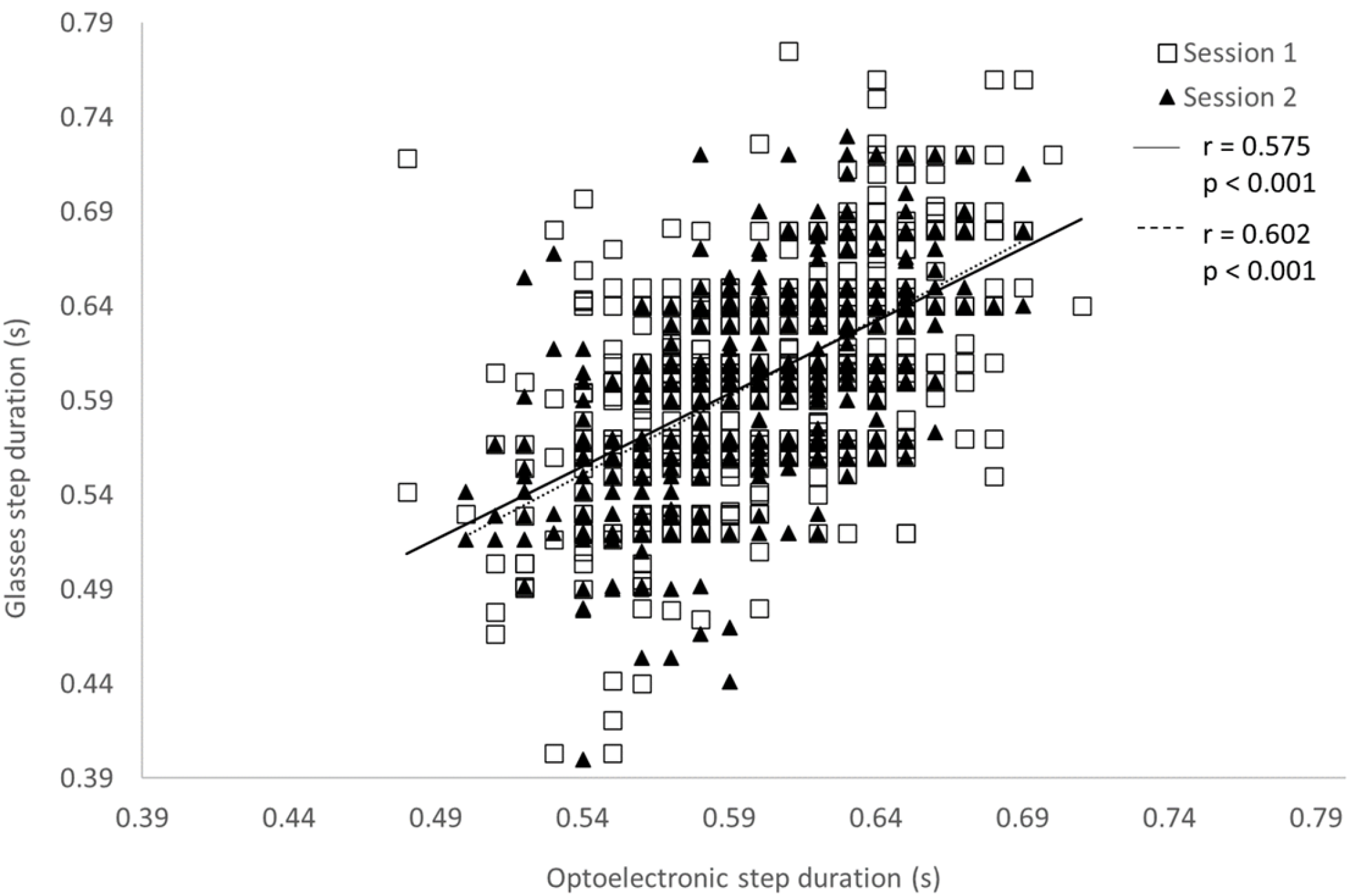
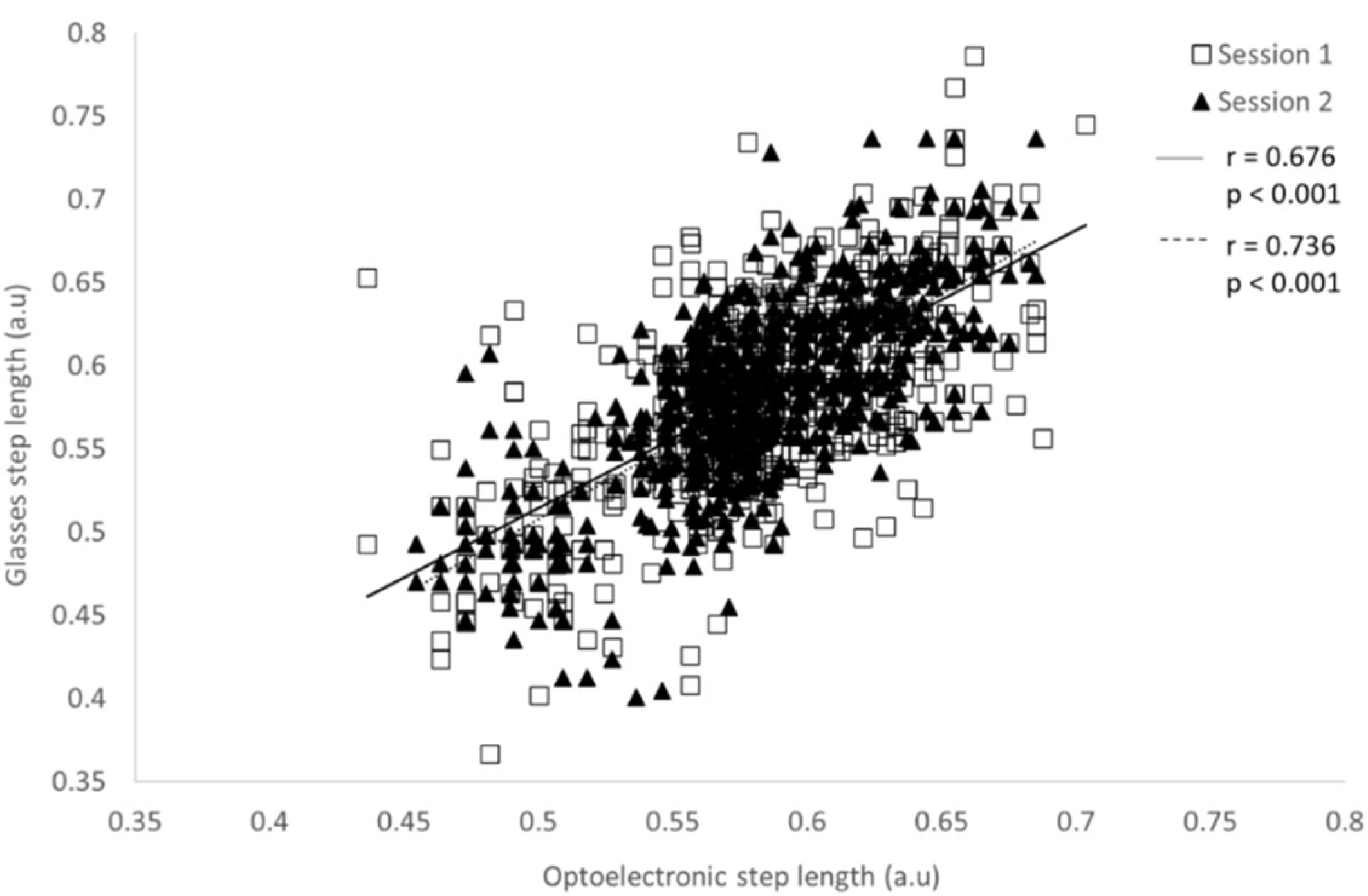
3.3. Concurrent Validity of Intra- and Inter-Session Reliability of the Glasses and the Optoelectronic System
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bohannon, R.W. Number of Pedometer-Assessed Steps Taken Per Day by Adults: A Descriptive Meta-Analysis. Phys. Ther. 2007, 87, 1642–1650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait Speed and Survival in Older Adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk Factors for Falls among Elderly Persons Living in the Community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Pavic, A.; Goodwin, V.A. Wearable Inertial Sensors to Measure Gait and Posture Characteristic Differences in Older Adult Fallers and Non-Fallers: A Scoping Review. Gait Posture 2020, 76, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Galna, B.; Verghese, J.; Coleman, S.; Burn, D.; Rochester, L. Independent Domains of Gait in Older Adults and Associated Motor and Nonmotor Attributes: Validation of a Factor Analysis Approach. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 820–827. [Google Scholar] [CrossRef] [Green Version]
- Ritt, M.; Schülein, S.; Lubrich, H.; Bollheimer, L.C.; Sieber, C.C.; Gassmann, K.-G. High-Technology Based Gait Assessment in Frail People: Associations between Spatio-Temporal and Three-Dimensional Gait Characteristics with Frailty Status across Four Different Frailty Measures. J. Nutr. Health Aging 2017, 21, 346–353. [Google Scholar] [CrossRef]
- Latt, M.D.; Menz, H.B.; Fung, V.S.; Lord, S.R. Acceleration Patterns of the Head and Pelvis During Gait in Older People With Parkinson’s Disease: A Comparison of Fallers and Nonfallers. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2009, 64, 700–706. [Google Scholar] [CrossRef] [Green Version]
- Aminian, K.; Najafi, B.; Büla, C.; Leyvraz, P.-F.; Robert, P. Spatio-Temporal Parameters of Gait Measured by an Ambulatory System Using Miniature Gyroscopes. J. Biomech. 2002, 35, 689–699. [Google Scholar] [CrossRef]
- Galna, B.; Lord, S.; Rochester, L. Is Gait Variability Reliable in Older Adults and Parkinson’s Disease? Towards an Optimal Testing Protocol. Gait Posture 2013, 37, 580–585. [Google Scholar] [CrossRef]
- Hageman, P.A.; Blanke, D.J. Comparison of Gait of Young Women and Elderly Women. Phys. Ther. 1986, 66, 1382–1387. [Google Scholar] [CrossRef]
- McDonough, A.L.; Batavia, M.; Chen, F.C.; Kwon, S.; Ziai, J. The Validity and Reliability of the GAITRite System’s Measurements: A Preliminary Evaluation. Arch. Phys. Med. Rehabil. 2001, 82, 419–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lienhard, K.; Schneider, D.; Maffiuletti, N.A. Validity of the Optogait Photoelectric System for the Assessment of Spatiotemporal Gait Parameters. Med. Eng. Phys. 2013, 35, 500–504. [Google Scholar] [CrossRef] [PubMed]
- Culhane, K.M.; O’Connor, M.; Lyons, D.; Lyons, G.M. Accelerometers in Rehabilitation Medicine for Older Adults. Age Ageing 2005, 34, 556–560. [Google Scholar] [CrossRef] [Green Version]
- Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait Analysis Using Wearable Sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef] [PubMed]
- Brodie, M.A.D.; Beijer, T.R.; Canning, C.G.; Lord, S.R. Head and Pelvis Stride-to-Stride Oscillations in Gait: Validation and Interpretation of Measurements from Wearable Accelerometers. Physiol. Meas. 2015, 36, 857–872. [Google Scholar] [CrossRef] [Green Version]
- Van Schooten, K.S.; Pijnappels, M.; Rispens, S.M.; Elders, P.J.M.; Lips, P.; van Dieën, J.H. Ambulatory Fall-Risk Assessment: Amount and Quality of Daily-Life Gait Predict Falls in Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 608–615. [Google Scholar] [CrossRef] [Green Version]
- Chigateri, N.G.; Kerse, N.; Wheeler, L.; MacDonald, B.; Klenk, J. Validation of an Accelerometer for Measurement of Activity in Frail Older People. Gait Posture 2018, 66, 114–117. [Google Scholar] [CrossRef]
- Petraglia, F.; Scarcella, L.; Pedrazzi, G.; Brancato, L.; Puers, R.; Costantino, C. Inertial Sensors versus Standard Systems in Gait Analysis: A Systematic Review and Meta-Analysis. Eur. J. Phys. Rehabil. Med. 2019, 55, 265–280. [Google Scholar] [CrossRef]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.F.; Esculier, J.-F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and Reliability of Wearable Inertial Sensors in Healthy Adult Walking: A Systematic Review and Meta-Analysis. J. Neuro Eng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef]
- Rucco, R.; Sorriso, A.; Liparoti, M.; Ferraioli, G.; Sorrentino, P.; Ambrosanio, M.; Baselice, F. Type and Location of Wearable Sensors for Monitoring Falls during Static and Dynamic Tasks in Healthy Elderly: A Review. Sensors 2018, 18, 1613. [Google Scholar] [CrossRef] [Green Version]
- Bet, P.; Castro, P.C.; Ponti, M.A. Fall Detection and Fall Risk Assessment in Older Person Using Wearable Sensors: A Systematic Review. Int. J. Med. Inform. 2019, 130, 103946. [Google Scholar] [CrossRef] [PubMed]
- Kobsar, D.; Masood, Z.; Khan, H.; Khalil, N.; Kiwan, M.Y.; Ridd, S.; Tobis, M. Wearable Inertial Sensors for Gait Analysis in Adults with Osteoarthritis—A Scoping Review. Sensors 2020, 20, 7143. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Gondim, I.T.G.; de Souza, C.D.C.B.; Rodrigues, M.A.B.; Azevedo, I.M.; de Sales, M.D.G.W.; Lins, O.G. Portable Accelerometers for the Evaluation of Spatio-Temporal Gait Parameters in People with Parkinson’s Disease: An Integrative Review. Arch. Gerontol. Geriatr. 2020, 90, 104097. [Google Scholar] [CrossRef] [PubMed]
- Brognara, L.; Palumbo, P.; Grimm, B.; Palmerini, L. Assessing Gait in Parkinson’s Disease Using Wearable Motion Sensors: A Systematic Review. Diseases 2019, 7, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vienne, A.; Barrois, R.P.; Buffat, S.; Ricard, D.; Vidal, P.-P. Inertial Sensors to Assess Gait Quality in Patients with Neurological Disorders: A Systematic Review of Technical and Analytical Challenges. Front. Psychol. 2017, 8, 817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byun, S.; Han, J.W.; Kim, T.H.; Kim, K.W. Test-Retest Reliability and Concurrent Validity of a Single Tri-Axial Accelerometer-Based Gait Analysis in Older Adults with Normal Cognition. PLoS ONE 2016, 11, e0158956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geerse, D.J.; Coolen, B.; Roerdink, M. Quantifying Spatiotemporal Gait Parameters with HoloLens in Healthy Adults and People with Parkinson’s Disease: Test-Retest Reliability, Concurrent Validity, and Face Validity. Sensors 2020, 20, 3216. [Google Scholar] [CrossRef]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of Fall Risk Assessment in Geriatric Populations Using Inertial Sensors. J. Neuro. Eng. Rehabil. 2013, 10, 91. [Google Scholar] [CrossRef] [Green Version]
- Lindemann, U.; Hock, A.; Stuber, M.; Keck, W.; Becker, C. Evaluation of a Fall Detector Based on Accelerometers: A Pilot Study. Med. Biol. Eng. Comput. 2005, 43, 548–551. [Google Scholar] [CrossRef]
- Drees. Available online: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/er881.pdf (accessed on 21 January 2022).
- Hellec, J.; Chorin, F.; Castagnetti, A.; Colson, S.S. Sit-To-Stand Movement Evaluated Using an Inertial Measurement Unit Embedded in Smart Glasses—A Validation Study. Sensors 2020, 20, 5019. [Google Scholar] [CrossRef]
- McGraw, K.O.; Wong, S.P. Forming Inferences About Some Intraclass Correlation Coefficients. Psychol. Methods 1996, 1, 30. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkinson, G.; Nevill, A.M. Statistical Methods For Assessing Measurement Error (Reliability) in Variables Relevant to Sports Medicine. Sports Med. 1998, 26, 217–238. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 8, 307–310. [Google Scholar] [CrossRef]
- Silsupadol, P.; Prupetkaew, P.; Kamnardsiri, T.; Lugade, V. Smartphone-Based Assessment of Gait During Straight Walking, Turning, and Walking Speed Modulation in Laboratory and Free-Living Environments. IEEE J. Biomed. Health Inform. 2020, 24, 1188–1195. [Google Scholar] [CrossRef]
- Hartmann, A.; Luzi, S.; Murer, K.; de Bie, R.A.; de Bruin, E.D. Concurrent Validity of a Trunk Tri-Axial Accelerometer System for Gait Analysis in Older Adults. Gait Posture 2009, 29, 444–448. [Google Scholar] [CrossRef]
- Kobsar, D.; Olson, C.; Paranjape, R.; Hadjistavropoulos, T.; Barden, J.M. Evaluation of Age-Related Differences in the Stride-to-Stride Fluctuations, Regularity and Symmetry of Gait Using a Waist-Mounted Tri-Axial Accelerometer. Gait Posture 2014, 39, 553–557. [Google Scholar] [CrossRef]
- Furrer, M.; Bichsel, L.; Niederer, M.; Baur, H.; Schmid, S. Validation of a Smartphone-Based Measurement Tool for the Quantification of Level Walking. Gait Posture 2015, 42, 289–294. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of Spatio-Temporal Gait Parameters from Trunk Accelerations during Human Walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Micó-Amigo, M.E.; Kingma, I.; Ainsworth, E.; Walgaard, S.; Niessen, M.; van Lummel, R.C.; van Dieën, J.H. A Novel Accelerometry-Based Algorithm for the Detection of Step Durations over Short Episodes of Gait in Healthy Elderly. J. Neuro Eng. Rehabil. 2016, 13, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zijlstra, W.; Hof, A.L. Displacement of the pelvis during human walking: Experimental data and model predictions. Gait Posture 1997, 6, 249–262. [Google Scholar] [CrossRef]
- González, R.C.; Alvarez, D.; López, A.M.; Alvarez, J.C. Ambulatory estimation of mean step length during unconstrained walking by means of COG accelerometry. Comput. Methods Biomech. Biomed. Eng. 2009, 12, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, A.; Zijlstra, W. Trunk-acceleration based assessment of gait parameters in older persons: A comparison of reliability and validity of four inverted pendulum based estimations. Gait Posture 2013, 38, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Lueken, M.; Loeser, J.; Weber, N.; Bollheimer, C.; Leonhardt, S.; Ngo, C. Model-Based Step Length Estimation Using a Pendant-Integrated Mobility Sensor. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2655–2665. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Zhang, B.; Wang, J.; Feng, W.; Jia, W.; Sun, M. Improved method of step length estimation based on inverted pendulum model. Int. J. Distrib. Sens. Netw. 2017, 13, 155014771770291. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Quantitative Gait Markers and Incident Fall Risk in Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2009, 64, 896–901. [Google Scholar] [CrossRef] [Green Version]

| Mean Step Duration (Standard Error) in s | Intraclass Correlation Coefficient (95% Confidence Interval) | Standard Error of the Measurement | Minimum Detectable Change | Coefficient of Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | |
| Eyeglasses | ||||||||||
| 0.72 WCC | 0.684 (0.048) | 0.676 (0.041) | 0.975 (0.948–0.986) | 0.970 (0.976–0.994) | 0.008 | 0.028 | 0.023 | 0.013 | 7.034 | 6.118 |
| 0.72 CC | 0.681 (0.049) | 0.682 (0.047) | 0.955 (0.974–0.993) | 0.987 (0.969–0.992) | 0.008 | 0.010 | 0.022 | 0.005 | 7.218 | 6.987 |
| 0.90 WCC | 0.605 (0.037) | 0.601 (0.034) | 0.979 (0.940–0.984) | 0.959 (0.945–0.985) | 0.005 | 0.007 | 0.015 | 0.019 | 6.179 | 5.719 |
| 0.90 CC | 0.587 (0.040) | 0.593 (0.038) | 0.979 (0.963–0.990) | 0.993 (0.929–0.981) | 0.006 | 0.003 | 0.016 | 0.009 | 6.754 | 6.402 |
| 1.1 WCC | 0.557 (0.044) | 0.552 (0.034) | 0.949 (0.911–0.976) | 0.950 (0.912–0.977) | 0.010 | 0.025 | 0.028 | 0.021 | 7.838 | 6.101 |
| 1.1 CC | 0.554 (0.042) | 0.544 (0.036) | 0.975 (0.956–0.988) | 0.936 (0.888–0.970) | 0.007 | 0.009 | 0.018 | 0.008 | 7.539 | 6.568 |
| OptiTrack | ||||||||||
| 0.72 WCC | 0.689 (0.030) | 0.681 (0.031) | 0.981 (0.966–0.991) | 0.991 (0.984–0.996) | 0.004 | 0.011 | 0.012 | 0.008 | 4.373 | 4.456 |
| 0.72 CC | 0.688 (0.032) | 0.684 (0.030) | 0.985 (0.956–0.988) | 0.982 (0.921–0.979) | 0.004 | 0.004 | 0.011 | 0.003 | 4.632 | 4.380 |
| 0.90 WCC | 0.605 (0.016) | 0.601 (0.016) | 0.994 (0.989–0.997) | 0.993 (0.988–0.997) | 0.001 | 0.001 | 0.004 | 0.004 | 2.726 | 2.654 |
| 0.90 CC | 0.588 (0.018) | 0.594 (0.016) | 0.995 (0.990–0.997) | 0.993 (0.988–0.997) | 0.001 | 0.001 | 0.004 | 0.004 | 3.214 | 2.731 |
| 1.1 WCC | 0.555 (0.015) | 0.553 (0.013) | 0.987 (0.978–0.994) | 0.992 (0.986–0.996) | 0.002 | 0.001 | 0.005 | 0.003 | 2.709 | 2.292 |
| 1.1 CC | 0.547 (0.013) | 0.545 (0.013) | 0.994 (0.990–0.997) | 0.992 (0.986–0.996) | 0.001 | 0.001 | 0.003 | 0.003 | 2.486 | 2.309 |
| Mean Step Length (Standard Error) (a.u) | Intraclass Correlation Coefficient (95% Confidence Interval) | Standard Error of the Measurement | Minimum Detectable Change | Coefficient of Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | |
| Eyeglasses | ||||||||||
| 0.72 WCC | 0.541 (0.038) | 0.535 (0.033) | 0.970 (0.948–0.986) | 0.987 (0.976–0.994) | 0.007 | 0.004 | 0.018 | 0.011 | 7.034 | 6.118 |
| 0.72 CC | 0.539 (0.039) | 0.540 (0.037) | 0.975 (0.956–0.988) | 0.955 (0.921–0.979) | 0.006 | 0.008 | 0.017 | 0.022 | 7.218 | 6.987 |
| 0.90 WCC | 0.585 (0.036) | 0.581 (0.033) | 0.979 (0.964–0.990) | 0.984 (0.972–0.993) | 0.005 | 0.004 | 0.014 | 0.012 | 6.179 | 5.719 |
| 0.90 CC | 0.567 (0.038) | 0.574 (0.037) | 0.983 (0.970–0.992) | 0.977 (0.961–0.990) | 0.005 | 0.006 | 0.014 | 0.015 | 6.754 | 6.402 |
| 1.1 WCC | 0.659 (0.053) | 0.652 (0.040) | 0.972 (0.951–0.987) | 0.975 (0.956–0.988) | 0.009 | 0.006 | 0.009 | 0.006 | 7.838 | 6.101 |
| 1.1 CC | 0.656 (0.049) | 0.643 (0.042) | 0.985 (0.974–0.993) | 0.968 (0.944–0.985) | 0.006 | 0.008 | 0.006 | 0.008 | 7.539 | 6.568 |
| OptiTrack | ||||||||||
| 0.72 WCC | 0.545 (0.024) | 0.539 (0.024) | 0.981 (0.966–0.991) | 0.991 (0.984–0.996) | 0.003 | 0.002 | 0.009 | 0.007 | 4.373 | 4.456 |
| 0.72 CC | 0.545 (0.025) | 0.540 (0.037) | 0.985 (0.974–0.993) | 0.982 (0.969–0.992) | 0.003 | 0.003 | 0.008 | 0.009 | 4.632 | 4.380 |
| 0.90 WCC | 0.585 (0.016) | 0.581 (0.015) | 0.996 (0.993–0.998) | 0.996 (0.994–0.998) | 0.001 | 0.001 | 0.003 | 0.003 | 2.726 | 2.654 |
| 0.90 CC | 0.569 (0.018) | 0.575 (0.016) | 0.996 (0.993–0.998) | 0.996 (0.993–0.998) | 0.001 | 0.001 | 0.003 | 0.003 | 3.214 | 2.731 |
| 1.1 WCC | 0.655 (0.018) | 0.654 (0.015) | 0.993 (0.988–0.997) | 0.997 (0.994–0.999) | 0.001 | 0.001 | 0.004 | 0.002 | 2.709 | 2.292 |
| 1.1 CC | 0.647 (0.016) | 0.644 (0.015) | 0.997 (0.994–0.998) | 0.996 (0.993–0.998) | 0.001 | 0.001 | 0.003 | 0.003 | 2.486 | 2.309 |
| (A) | |||
| Step Duration | Intraclass Correlation Coefficient (95% Confidence Interval) | Standard Error of the Measurement | Minimum Detectable Change |
| Eyeglasses | |||
| 0.72 | 0.311 (0.174–0.522) | 0.023 | 0.063 |
| 0.90 | 0.854 (0.669–0.940) | 0.009 | 0.024 |
| 1.1 | 0.654 (0.297–0.851) | 0.014 | 0.038 |
| OptiTrack | |||
| 0.72 | 0.573 (0.186–0.806) | 0.017 | 0.047 |
| 0.90 | 0.884 (0.730–0.952) | 0.004 | 0.010 |
| 1.1 | 0.934 (0.841–0.973) | 0.005 | 0.015 |
| (B) | |||
|---|---|---|---|
| Step Length | Intraclass Correlation Coefficient (95% Confidence Interval) | Standard Error of the Measurement | Minimum Detectable Change |
| Eyeglasses | |||
| 0.72 | 0.570 (0.410–0.749) | 0.018 | 0.049 |
| 0.90 | 0.923 (0.816–0.969) | 0.006 | 0.017 |
| 1.1 | 0.484 (0.065–0.758) | 0.018 | 0.049 |
| OptiTrack | |||
| 0.72 | 0.573 (0.186–0.806) | 0.013 | 0.037 |
| 0.90 | 0.937 (0.849–0.975) | 0.003 | 0.007 |
| 1.1 | 0.970 (0.926–0.739) | 0.002 | 0.007 |
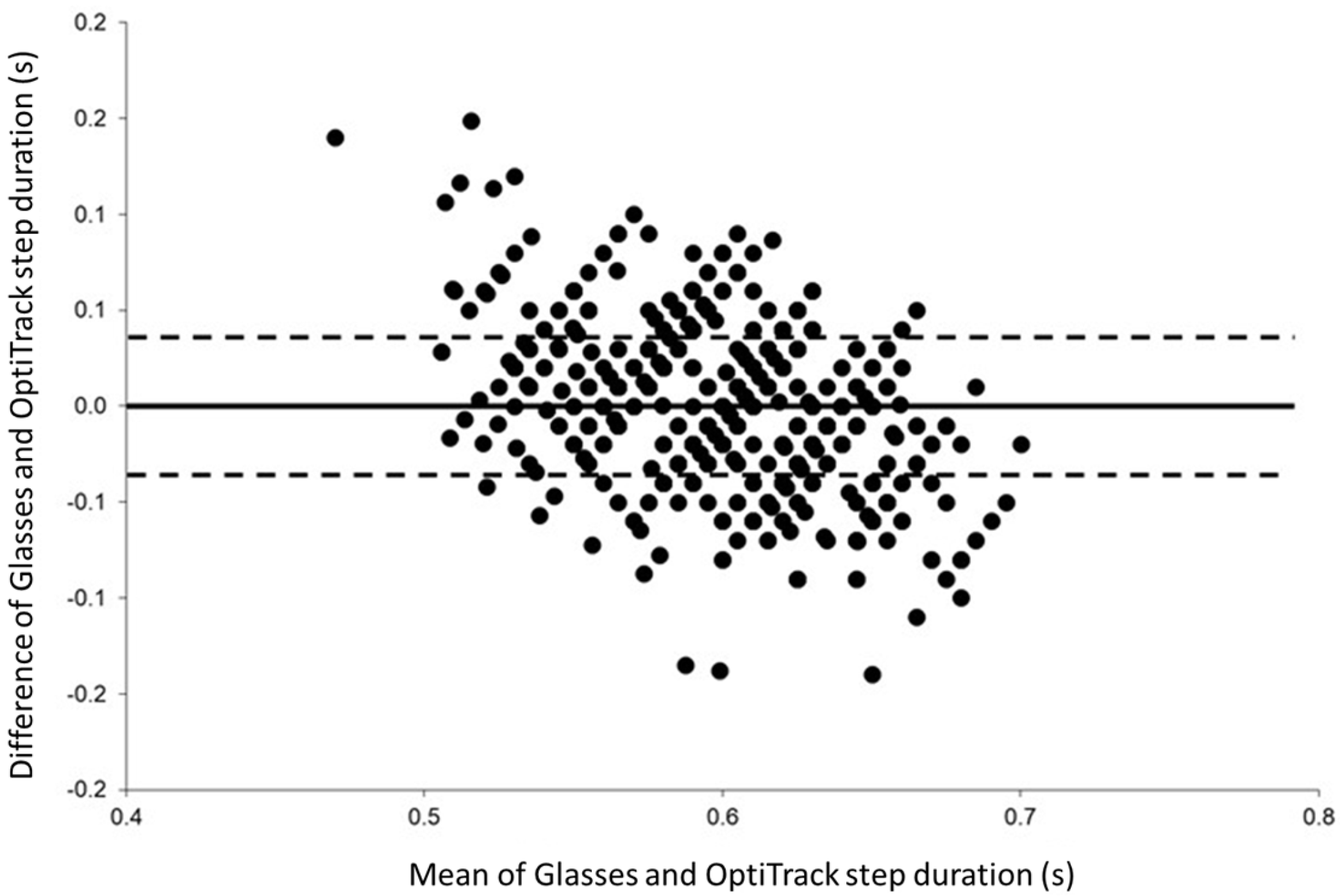
| Pearson’s Correlation (r) | Bland–Altman | |||||
|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Global | Bias (Mean Difference) | Lower Limit | Upper Limit | |
| Step Duration | ||||||
| 0.72 WCC | 0.368 *** | 0.715 *** | 0.563 *** | 0.005 | −0.115 | 0.124 |
| 0.72 CC | 0.556 *** | 0.538 *** | 0.545 *** | 0.005 | −0.111 | 0.121 |
| 0.90 WCC | 0.575 *** | 0.602 *** | 0.588 *** | 0.000 | −0.079 | 0.078 |
| 0.90 CC | 0.452 *** | 0.587 *** | 0.503 *** | 0.001 | −0.099 | 0.101 |
| 1.1 WCC | 0.326 *** | 0.503 *** | 0.393 ** | 0.000 | −0.095 | 0.095 |
| 1.1 CC | 0.483 *** | 0.496 *** | 0.488 ** | −0.004 | −0.095 | 0.088 |
| Step Length * | ||||||
| 0.72 WCC | 0.364 *** | 0.714 *** | 0.563 *** | 0.004 | −0.091 | 0.094 |
| 0.72 CC | 0.554 *** | 0.535 *** | 0.545 *** | 0.004 | −0.088 | 0.096 |
| 0.90 WCC | 0.676 *** | 0.736 *** | 0.706 *** | 0.000 | −0.076 | 0.075 |
| 0.90 CC | 0.681 *** | 0.699 *** | 0.689 *** | 0.001 | −0.084 | 0.086 |
| 1.1 WCC | 0.509 *** | 0.654 *** | 0.560 *** | −0.001 | −0.116 | 0.114 |
| 1.1 CC | 0.632 *** | 0.628 *** | 0.628 *** | −0.004 | 0.106 | −0.115 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hellec, J.; Chorin, F.; Castagnetti, A.; Guérin, O.; Colson, S.S. Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait. Sensors 2022, 22, 1196. https://doi.org/10.3390/s22031196
Hellec J, Chorin F, Castagnetti A, Guérin O, Colson SS. Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait. Sensors. 2022; 22(3):1196. https://doi.org/10.3390/s22031196
Chicago/Turabian StyleHellec, Justine, Frédéric Chorin, Andrea Castagnetti, Olivier Guérin, and Serge S. Colson. 2022. "Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait" Sensors 22, no. 3: 1196. https://doi.org/10.3390/s22031196
APA StyleHellec, J., Chorin, F., Castagnetti, A., Guérin, O., & Colson, S. S. (2022). Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait. Sensors, 22(3), 1196. https://doi.org/10.3390/s22031196






