Triple-Negative Breast Cancer Unveiled: Bridging Science, Treatment Strategy, and Economic Aspects
Abstract
1. Introduction
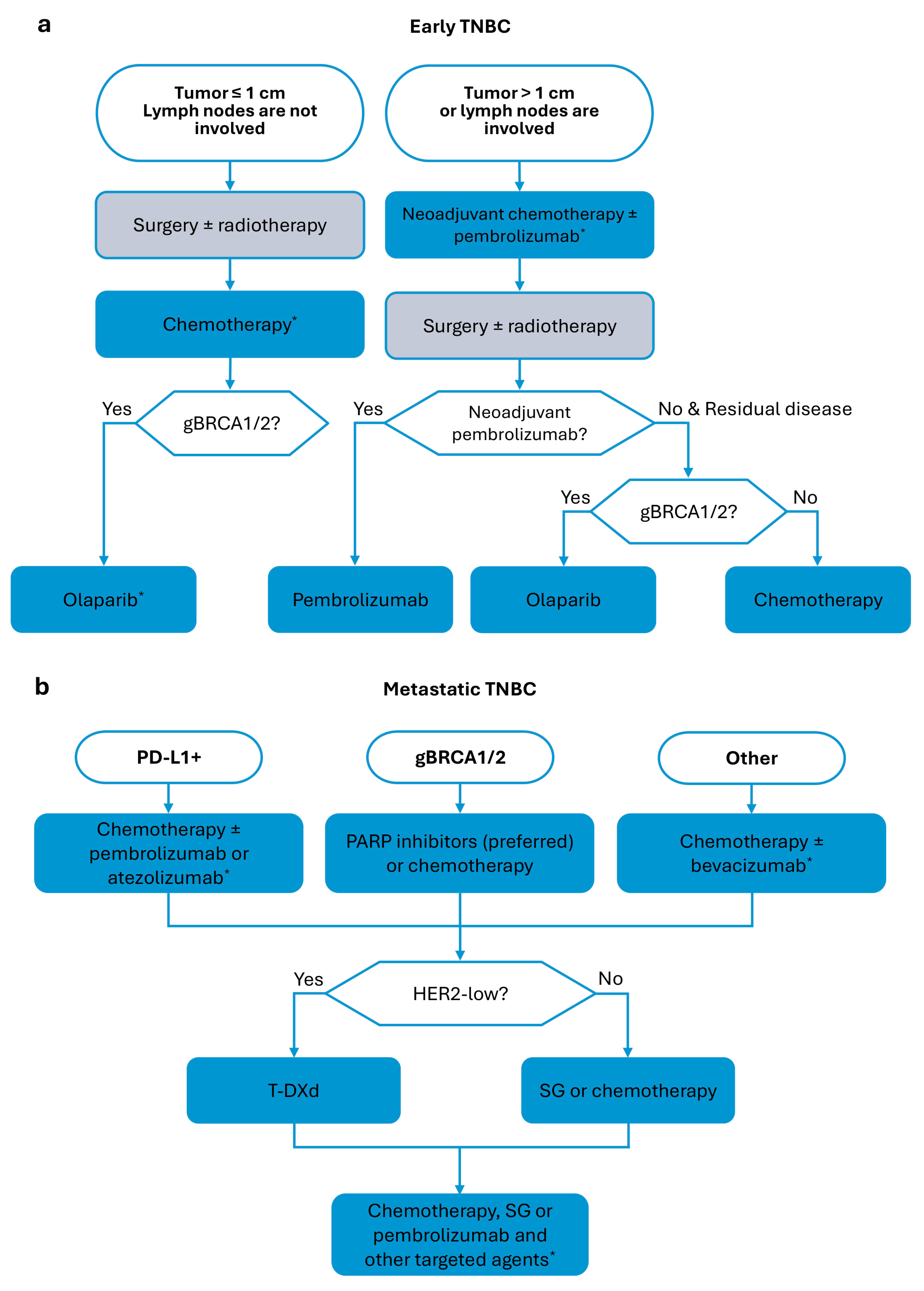
2. Approved Therapies
2.1. PARP Inhibitors
2.2. Immune Checkpoint Inhibitors
2.3. Antibody–Drug Conjugates
2.4. Others
3. Clinical Trial Landscape
3.1. Small Molecules
3.2. Antibodies
3.3. ADCs
3.4. Others
4. Cost-Effectiveness of Approved TNBC Treatment Strategies
5. TNBC Pharmaceutical Market Challenges and Perspectives
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADC | Antibody-drug conjugates |
| CDK | Cyclin-dependent kinase |
| CPS | Combined positive score |
| CRR | Complete response rate |
| CT | Chemotherapy |
| Dato-DXd | Datopotamab deruxtecan |
| DFS | Disease-free survival |
| dMMR | DNA mismatch repair deficiency |
| EFS | Event-free survival |
| EMA | European Medicines Agency |
| ESMO | European Society for Medical Oncology |
| FDA | U.S. Food and Drug Administration |
| gBRCA1/2 | Germline mutations in the breast cancer associated gene 1 or 2 |
| HER2 | Human epidermal growth factor receptor 2 |
| HR | Hormone receptors |
| ICER | Incremental cost-effectiveness ratio |
| ICI | Immune checkpoint inhibitors |
| IHC | Immunohistochemistry |
| ISH | In situ hybridization |
| LAR | Luminal androgen receptor |
| LMIC | Low- or middle-income countries |
| mAb | Monoclonal antibodies |
| MSI | Microsatellite instability |
| mTNBC | Metastatic triple-negative breast cancer |
| mTOR | Mammalian target of rapamycin |
| nab-p | Nab-paclitaxel |
| NTRK | Neurotrophic tyrosine receptor kinase |
| ORR | Overall response rate |
| OS | Overall survival |
| PARPi | Poly (ADP-ribose) polymerase (PARP) inhibitors |
| pCR | Pathological complete response |
| PD-1 | Programmed cell death protein 1 |
| PD-L1 | Programmed cell death protein 1 ligand |
| PFS | Progression-free survival |
| PI3K | Phosphoinositide 3-kinase |
| QALY | Quality-adjusted life year |
| RET | Rearranged during transfection |
| SG | Sacituzumab govitecan |
| ST | Sacituzumab tirumotecan |
| T-DXd | Fam-trastuzumab deruxtecan-nxki |
| TMB | Tumor mutational burden |
| TME | Tumor microenvironment |
| TNBC | Triple-negative breast cancer |
| TPC | Treatment of physician’s choice |
| TROP2 | Trophoblastic cell-surface antigen-2 |
| TTR | Time to reimbursement |
| VEGF | Vascular endothelial growth factor |
| WTP | Willingness-to-pay |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Kim, J.; Harper, A.; McCormack, V.; Sung, H.; Houssami, N.; Morgan, E.; Mutebi, M.; Garvey, G.; Soerjomataram, I.; Fidler-Benaoudia, M.M. Global Patterns and Trends in Breast Cancer Incidence and Mortality across 185 Countries. Nat. Med. 2025, 31, 1154–1162. [Google Scholar] [CrossRef]
- Allison, K.H.; Hammond, M.E.H.; Dowsett, M.; McKernin, S.E.; Carey, L.A.; Fitzgibbons, P.L.; Hayes, D.F.; Lakhani, S.R.; Chavez-MacGregor, M.; Perlmutter, J.; et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 2020, 38, 1346–1366. [Google Scholar] [CrossRef] [PubMed]
- Wolff, A.C.; Somerfield, M.R.; Dowsett, M.; Hammond, M.E.H.; Hayes, D.F.; McShane, L.M.; Saphner, T.J.; Spears, P.A.; Allison, K.H. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: ASCO–College of American Pathologists Guideline Update. J. Clin. Oncol. 2023, 41, 3867–3872. [Google Scholar] [CrossRef] [PubMed]
- Blows, F.M.; Driver, K.E.; Schmidt, M.K.; Broeks, A.; van Leeuwen, F.E.; Wesseling, J.; Cheang, M.C.; Gelmon, K.; Nielsen, T.O.; Blomqvist, C.; et al. Subtyping of Breast Cancer by Immunohistochemistry to Investigate a Relationship between Subtype and Short and Long Term Survival: A Collaborative Analysis of Data for 10,159 Cases from 12 Studies. PLoS Med. 2010, 7, e1000279. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.-Y.; Chang, C.-J.; Cheng, J.-S. Survival, Treatment Regimens and Medical Costs of Women Newly Diagnosed with Metastatic Triple-Negative Breast Cancer. Sci. Rep. 2022, 12, 729. [Google Scholar] [CrossRef]
- Bauer, K.R.; Brown, M.; Cress, R.D.; Parise, C.A.; Caggiano, V. Descriptive Analysis of Estrogen Receptor (ER)-Negative, Progesterone Receptor (PR)-Negative, and HER2-Negative Invasive Breast Cancer, the so-Called Triple-Negative Phenotype. Cancer 2007, 109, 1721–1728. [Google Scholar] [CrossRef]
- Dent, R.; Trudeau, M.; Pritchard, K.I.; Hanna, W.M.; Kahn, H.K.; Sawka, C.A.; Lickley, L.A.; Rawlinson, E.; Sun, P.; Narod, S.A. Triple-Negative Breast Cancer: Clinical Features and Patterns of Recurrence. Clin. Cancer Res. 2007, 13, 4429–4434. [Google Scholar] [CrossRef]
- Liedtke, C.; Mazouni, C.; Hess, K.R.; André, F.; Tordai, A.; Mejia, J.A.; Symmans, W.F.; Gonzalez-Angulo, A.M.; Hennessy, B.; Green, M.; et al. Response to Neoadjuvant Therapy and Long-Term Survival in Patients with Triple-Negative Breast Cancer. J. Clin. Oncol. 2008, 26, 1275–1281. [Google Scholar] [CrossRef]
- Steward, L.; Conant, L.; Gao, F.; Margenthaler, J.A. Predictive Factors and Patterns of Recurrence in Patients with Triple Negative Breast Cancer. Ann. Surg. Oncol. 2014, 21, 2165–2171. [Google Scholar] [CrossRef]
- Urru, S.A.M.; Gallus, S.; Bosetti, C.; Moi, T.; Medda, R.; Sollai, E.; Murgia, A.; Sanges, F.; Pira, G.; Manca, A.; et al. Clinical and Pathological Factors Influencing Survival in a Large Cohort of Triple-Negative Breast Cancer Patients. BMC Cancer 2018, 18, 56. [Google Scholar] [CrossRef] [PubMed]
- Gennari, A.; André, F.; Barrios, C.H.; Cortés, J.; De Azambuja, E.; DeMichele, A.; Dent, R.; Fenlon, D.; Gligorov, J.; Hurvitz, S.A.; et al. ESMO Clinical Practice Guideline for the Diagnosis, Staging and Treatment of Patients with Metastatic Breast Cancer. Ann. Oncol. 2021, 32, 1475–1495. [Google Scholar] [CrossRef] [PubMed]
- Loibl, S.; André, F.; Bachelot, T.; Barrios, C.H.; Bergh, J.; Burstein, H.J.; Cardoso, M.J.; Carey, L.A.; Dawood, S.; Mastro, L.D.; et al. Early Breast Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2024, 35, 159–182. [Google Scholar] [CrossRef]
- Huang, M.; Haiderali, A.; Fox, G.E.; Frederickson, A.; Cortes, J.; Fasching, P.A.; O’Shaughnessy, J. Economic and Humanistic Burden of Triple-Negative Breast Cancer: A Systematic Literature Review. PharmacoEconomics 2022, 40, 519–558. [Google Scholar] [CrossRef]
- Marra, A.; Curigliano, G. Adjuvant and Neoadjuvant Treatment of Triple-Negative Breast Cancer with Chemotherapy. Cancer J. 2021, 27, 41–49. [Google Scholar] [CrossRef]
- Obidiro, O.; Battogtokh, G.; Akala, E.O. Triple Negative Breast Cancer Treatment Options and Limitations: Future Outlook. Pharmaceutics 2023, 15, 1796. [Google Scholar] [CrossRef]
- Li, X.; Zou, L. BRCAness, DNA Gaps, and Gain and Loss of PARP Inhibitor–Induced Synthetic Lethality. J. Clin. Investig. 2024, 134, e181062. [Google Scholar] [CrossRef]
- Bryant, H.E.; Schultz, N.; Thomas, H.D.; Parker, K.M.; Flower, D.; Lopez, E.; Kyle, S.; Meuth, M.; Curtin, N.J.; Helleday, T. Specific Killing of BRCA2-Deficient Tumours with Inhibitors of Poly(ADP-Ribose) Polymerase. Nature 2005, 434, 913–917. [Google Scholar] [CrossRef]
- Farmer, H.; McCabe, N.; Lord, C.J.; Tutt, A.N.J.; Johnson, D.A.; Richardson, T.B.; Santarosa, M.; Dillon, K.J.; Hickson, I.; Knights, C.; et al. Targeting the DNA Repair Defect in BRCA Mutant Cells as a Therapeutic Strategy. Nature 2005, 434, 917–921. [Google Scholar] [CrossRef]
- Robson, M.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Delaloge, S.; Li, W.; Tung, N.; Armstrong, A.; et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N. Engl. J. Med. 2017, 377, 523–533, Erratum in N. Engl. J. Med. 2017, 377, 1700. [Google Scholar] [CrossRef] [PubMed]
- Litton, J.K.; Rugo, H.S.; Ettl, J.; Hurvitz, S.A.; Gonçalves, A.; Lee, K.-H.; Fehrenbacher, L.; Yerushalmi, R.; Mina, L.A.; Martin, M.; et al. Talazoparib in Patients with Advanced Breast Cancer and a Germline BRCA Mutation. N. Engl. J. Med. 2018, 379, 753–763. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. FDA Approves Olaparib for Germline BRCA-Mutated Metastatic Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-olaparib-germline-brca-mutated-metastatic-breast-cancer (accessed on 2 November 2024).
- U.S. Food and Drug Administration. FDA Approves Talazoparib for GBRCAm HER2-Negative Locally Advanced or Metastatic Breast Cancer. Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-talazoparib-gbrcam-her2-negative-locally-advanced-or-metastatic-breast-cancer (accessed on 2 November 2024).
- European Medicines Agency CHMP. Post-Authorisation Summary of Positive Opinion for Lynparza (II-20). EMA/CHMP/146940/2019. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-lynparza-ii-20_en.pdf (accessed on 30 January 2025).
- European Medicines Agency CHMP. Summary of Positive Opinion for Talzenna. EMA/CHMP/232257/2019. Available online: https://www.ema.europa.eu/en/documents/smop-initial/chmp-summary-positive-opinion-talzenna_en.pdf (accessed on 30 January 2025).
- Litton, J.K.; Hurvitz, S.A.; Mina, L.A.; Rugo, H.S.; Lee, K.-H.; Gonçalves, A.; Diab, S.; Woodward, N.; Goodwin, A.; Yerushalmi, R.; et al. Talazoparib versus Chemotherapy in Patients with Germline BRCA1/2-Mutated HER2-Negative Advanced Breast Cancer: Final Overall Survival Results from the EMBRACA Trial. Ann. Oncol. 2020, 31, 1526–1535. [Google Scholar] [CrossRef]
- Robson, M.E.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Delaloge, S.; Tung, N.; Armstrong, A.; Dymond, M.; et al. OlympiAD Extended Follow-up for Overall Survival and Safety: Olaparib versus Chemotherapy Treatment of Physician’s Choice in Patients with a Germline BRCA Mutation and HER2-Negative Metastatic Breast Cancer. Eur. J. Cancer 2023, 184, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Murai, J.; Huang, S.-Y.N.; Renaud, A.; Zhang, Y.; Ji, J.; Takeda, S.; Morris, J.; Teicher, B.; Doroshow, J.H.; Pommier, Y. Stereospecific PARP Trapping by BMN 673 and Comparison with Olaparib and Rucaparib. Mol. Cancer Ther. 2014, 13, 433–443. [Google Scholar] [CrossRef]
- Antolin, A.A.; Ameratunga, M.; Banerji, U.; Clarke, P.A.; Workman, P.; Al-Lazikani, B. The Kinase Polypharmacology Landscape of Clinical PARP Inhibitors. Sci. Rep. 2020, 10, 2585. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Y.; Yuan, L.; Ren, L.; Zhang, Y.; Qi, X. Comparative Efficacy, Safety, and Acceptability of Single-Agent Poly (ADP-Ribose) Polymerase (PARP) Inhibitors in BRCA-Mutated HER2-Negative Metastatic or Advanced Breast Cancer: A Network Meta-Analysis. Aging 2020, 13, 450–459. [Google Scholar] [CrossRef] [PubMed]
- McCrea, C.; Hettle, R.; Gulati, P.; Taneja, A.; Rajora, P. Indirect Treatment Comparison of Olaparib and Talazoparib in Germline BRCA-Mutated HER2-Negative Metastatic Breast Cancer. J. Comp. Eff. Res. 2021, 10, 1021–1030. [Google Scholar] [CrossRef]
- Tutt, A.N.J.; Garber, J.E.; Kaufman, B.; Viale, G.; Fumagalli, D.; Rastogi, P.; Gelber, R.D.; de Azambuja, E.; Fielding, A.; Balmaña, J.; et al. Adjuvant Olaparib for Patients with BRCA1- or BRCA2-Mutated Breast Cancer. N. Engl. J. Med. 2021, 384, 2394–2405. [Google Scholar] [CrossRef]
- Geyer, C.E.; Garber, J.E.; Gelber, R.D.; Yothers, G.; Taboada, M.; Ross, L.; Rastogi, P.; Cui, K.; Arahmani, A.; Aktan, G.; et al. Overall Survival in the OlympiA Phase III Trial of Adjuvant Olaparib in Patients with Germline Pathogenic Variants in BRCA1/2 and High-Risk, Early Breast Cancer. Ann. Oncol. 2022, 33, 1250–1268. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency CHMP. Summary of Positive Opinion for Lynparza. EMA/CHMP/602696/2022. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-lynparza-ii-51-g_en.pdf (accessed on 30 January 2025).
- U.S. Food and Drug Administration. FDA Approves Olaparib for Adjuvant Treatment of High-Risk Early Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-olaparib-adjuvant-treatment-high-risk-early-breast-cancer (accessed on 2 November 2024).
- Greenup, R.; Buchanan, A.; Lorizio, W.; Rhoads, K.; Chan, S.; Leedom, T.; King, R.; McLennan, J.; Crawford, B.; Kelly Marcom, P.; et al. Prevalence of BRCA Mutations Among Women with Triple-Negative Breast Cancer (TNBC) in a Genetic Counseling Cohort. Ann. Surg. Oncol. 2013, 20, 3254–3258. [Google Scholar] [CrossRef]
- Engel, C.; Rhiem, K.; Hahnen, E.; Loibl, S.; Weber, K.E.; Seiler, S.; Zachariae, S.; Hauke, J.; Wappenschmidt, B.; Waha, A.; et al. Prevalence of Pathogenic BRCA1/2 Germline Mutations among 802 Women with Unilateral Triple-Negative Breast Cancer without Family Cancer History. BMC Cancer 2018, 18, 265. [Google Scholar] [CrossRef]
- Li, H.; Liu, Z.-Y.; Wu, N.; Chen, Y.-C.; Cheng, Q.; Wang, J. PARP Inhibitor Resistance: The Underlying Mechanisms and Clinical Implications. Mol. Cancer 2020, 19, 107. [Google Scholar] [CrossRef]
- Beitsch, P.D.; Whitworth, P.W.; Hughes, K.; Patel, R.; Rosen, B.; Compagnoni, G.; Baron, P.; Simmons, R.; Smith, L.A.; Grady, I.; et al. Underdiagnosis of Hereditary Breast Cancer: Are Genetic Testing Guidelines a Tool or an Obstacle? J. Clin. Oncol. 2019, 37, 453–460. [Google Scholar] [CrossRef]
- Arun, B.; Couch, F.J.; Abraham, J.; Tung, N.; Fasching, P.A. BRCA-Mutated Breast Cancer: The Unmet Need, Challenges and Therapeutic Benefits of Genetic Testing. Br. J. Cancer 2024, 131, 1400–1414. [Google Scholar] [CrossRef]
- Schumacher, T.N.; Schreiber, R.D. Neoantigens in Cancer Immunotherapy. Science 2015, 348, 69–74. [Google Scholar] [CrossRef]
- Burstein, M.D.; Tsimelzon, A.; Poage, G.M.; Covington, K.R.; Contreras, A.; Fuqua, S.A.W.; Savage, M.I.; Osborne, C.K.; Hilsenbeck, S.G.; Chang, J.C.; et al. Comprehensive Genomic Analysis Identifies Novel Subtypes and Targets of Triple-Negative Breast Cancer. Clin. Cancer Res. 2015, 21, 1688–1698. [Google Scholar] [CrossRef]
- Lehmann, B.D.; Jovanović, B.; Chen, X.; Estrada, M.V.; Johnson, K.N.; Shyr, Y.; Moses, H.L.; Sanders, M.E.; Pietenpol, J.A. Refinement of Triple-Negative Breast Cancer Molecular Subtypes: Implications for Neoadjuvant Chemotherapy Selection. PLoS ONE 2016, 11, e0157368. [Google Scholar] [CrossRef] [PubMed]
- Luen, S.; Virassamy, B.; Savas, P.; Salgado, R.; Loi, S. The Genomic Landscape of Breast Cancer and Its Interaction with Host Immunity. Breast 2016, 29, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Narang, P.; Chen, M.; Sharma, A.A.; Anderson, K.S.; Wilson, M.A. The Neoepitope Landscape of Breast Cancer: Implications for Immunotherapy. BMC Cancer 2019, 19, 200. [Google Scholar] [CrossRef] [PubMed]
- Cortes, J.; Cescon, D.W.; Rugo, H.S.; Nowecki, Z.; Im, S.-A.; Yusof, M.M.; Gallardo, C.; Lipatov, O.; Barrios, C.H.; Holgado, E.; et al. Pembrolizumab plus Chemotherapy versus Placebo plus Chemotherapy for Previously Untreated Locally Recurrent Inoperable or Metastatic Triple-Negative Breast Cancer (KEYNOTE-355): A Randomised, Placebo-Controlled, Double-Blind, Phase 3 Clinical Trial. Lancet 2020, 396, 1817–1828. [Google Scholar] [CrossRef]
- Cortes, J.; Rugo, H.S.; Cescon, D.W.; Im, S.-A.; Yusof, M.M.; Gallardo, C.; Lipatov, O.; Barrios, C.H.; Perez-Garcia, J.; Iwata, H.; et al. Pembrolizumab plus Chemotherapy in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2022, 387, 217–226. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration FDA. Grants Accelerated Approval to Pembrolizumab for Locally Recurrent Unresectable or Metastatic Triple Negative Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pembrolizumab-locally-recurrent-unresectable-or-metastatic-triple (accessed on 30 January 2025).
- European Medicines Agency CHMP. Post-Authorisation Summary of Positive Opinion for Keytruda (II-99). EMA/CHMP/510671/2021. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-keytruda-ii-99_en.pdf (accessed on 30 January 2025).
- Mittendorf, E.A.; Philips, A.V.; Meric-Bernstam, F.; Qiao, N.; Wu, Y.; Harrington, S.; Su, X.; Wang, Y.; Gonzalez-Angulo, A.M.; Akcakanat, A.; et al. PD-L1 Expression in Triple-Negative Breast Cancer. Cancer Immunol. Res. 2014, 2, 361–370. [Google Scholar] [CrossRef]
- European Medicines Agency CHMP. Post-Authorisation Summary of Opinion for Keytruda (II-110). EMA/CHMP/203854/2022. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-opinion-keytruda-ii-110_en.pdf (accessed on 30 January 2025).
- U.S. Food and Drug Administration FDA. Approves Pembrolizumab for High-Risk Early-Stage Triple-Negative Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pembrolizumab-high-risk-early-stage-triple-negative-breast-cancer (accessed on 30 January 2025).
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.-A.; Shaw Wright, G.; et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef] [PubMed]
- Miles, D.; Gligorov, J.; André, F.; Cameron, D.; Schneeweiss, A.; Barrios, C.; Xu, B.; Wardley, A.; Kaen, D.; Andrade, L.; et al. Primary Results from IMpassion131, a Double-Blind, Placebo-Controlled, Randomised Phase III Trial of First-Line Paclitaxel with or without Atezolizumab for Unresectable Locally Advanced/Metastatic Triple-Negative Breast Cancer. Ann. Oncol. 2021, 32, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency CHMP. Post-Authorisation Summary of Positive Opinion for Tecentriq (X-17-II-22). EMA/366637/2019. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-tecentriq-x-17-ii-22_en.pdf (accessed on 30 January 2025).
- Schmid, P.; Rugo, H.S.; Adams, S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Henschel, V.; Molinero, L.; Chui, S.Y.; et al. Atezolizumab plus Nab-Paclitaxel as First-Line Treatment for Unresectable, Locally Advanced or Metastatic Triple-Negative Breast Cancer (IMpassion130): Updated Efficacy Results from a Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2020, 21, 44–59. [Google Scholar] [CrossRef]
- Latif, F.; Bint Abdul Jabbar, H.; Malik, H.; Sadaf, H.; Sarfraz, A.; Sarfraz, Z.; Cherrez-Ojeda, I. Atezolizumab and Pembrolizumab in Triple-Negative Breast Cancer: A Meta-Analysis. Expert Rev. Anticancer Ther. 2022, 22, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Song, J.; Yang, H.; Jin, F.; Zheng, A. Efficacy and Safety of PD-1/PD-L1 Inhibitors in Triple-Negative Breast Cancer: A Systematic Review and Meta-Analysis. Acta Oncol. 2022, 61, 1105–1115. [Google Scholar] [CrossRef]
- Qi, Y.; Yan, X.; Wang, C.; Cao, H.; Liu, G. Predictive Value of PD-L1 Expression to the Efficacy of Immune Checkpoint Inhibitors in Advanced Triple-Negative Breast Cancer: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2022, 13, 1004821. [Google Scholar] [CrossRef]
- Villacampa, G.; Tolosa, P.; Salvador, F.; Sánchez-Bayona, R.; Villanueva, L.; Dienstmann, R.; Ciruelos, E.; Pascual, T. Addition of Immune Checkpoint Inhibitors to Chemotherapy versus Chemotherapy Alone in First-Line Metastatic Triple-Negative Breast Cancer: A Systematic Review and Meta-Analysis. Cancer Treat. Rev. 2022, 104, 102352. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration FDA. Grants Accelerated Approval to Pembrolizumab for First Tissue/Site Agnostic Indication. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pembrolizumab-first-tissuesite-agnostic-indication (accessed on 30 January 2025).
- ASCO Post. FDA Grants Full Approval to Pembrolizumab for Certain Adult and Pediatric Patients with Advanced MSI-H or DMMR Solid Tumors. Available online: https://ascopost.com/news/march-2023/fda-grants-full-approval-to-pembrolizumab-for-certain-adult-and-pediatric-patients-with-advanced-msi-h-or-dmmr-solid-tumors/ (accessed on 30 January 2025).
- U.S. Food and Drug Administration FDA. Approves Pembrolizumab for Adults and Children with TMB-H Solid Tumors. Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-pembrolizumab-adults-and-children-tmb-h-solid-tumors (accessed on 30 January 2025).
- U.S. Food and Drug Administration FDA. Grants Accelerated Approval to Dostarlimab-Gxly for DMMR Advanced Solid Tumors. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-dostarlimab-gxly-dmmr-advanced-solid-tumors (accessed on 30 January 2025).
- Fu, Z.; Li, S.; Han, S.; Shi, C.; Zhang, Y. Antibody Drug Conjugate: The “Biological Missile” for Targeted Cancer Therapy. Sig. Transduct. Target Ther. 2022, 7, 1–25. [Google Scholar] [CrossRef]
- Trerotola, M.; Cantanelli, P.; Guerra, E.; Tripaldi, R.; Aloisi, A.L.; Bonasera, V.; Lattanzio, R.; de Lange, R.; Weidle, U.H.; Piantelli, M.; et al. Upregulation of Trop-2 Quantitatively Stimulates Human Cancer Growth. Oncogene 2013, 32, 222–233. [Google Scholar] [CrossRef]
- Syed, Y.Y. Sacituzumab Govitecan: First Approval. Drugs 2020, 80, 1019–1025. [Google Scholar] [CrossRef]
- Bardia, A.; Tolaney, S.M.; Punie, K.; Loirat, D.; Oliveira, M.; Kalinsky, K.; Zelnak, A.; Aftimos, P.; Dalenc, F.; Sardesai, S.; et al. Biomarker Analyses in the Phase III ASCENT Study of Sacituzumab Govitecan versus Chemotherapy in Patients with Metastatic Triple-Negative Breast Cancer. Ann. Oncol. 2021, 32, 1148–1156. [Google Scholar] [CrossRef]
- Olivier, T.; Prasad, V. Sacituzumab Govitecan in Metastatic Triple Negative Breast Cancer (TNBC): Four Design Features in the ASCENT Trial Potentially Favored the Experimental Arm. Transl. Oncol. 2022, 15, 101248. [Google Scholar] [CrossRef]
- European Medicines Agency CHMP. Summary of Positive Opinion for Trodelvy. EMA/411659/2021. Available online: https://www.ema.europa.eu/en/documents/smop-initial/chmp-summary-positive-opinion-trodelvy_en.pdf (accessed on 30 January 2024).
- U.S. Food and Drug Administration FDA. Grants Regular Approval to Sacituzumab Govitecan for Triple-Negative Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-regular-approval-sacituzumab-govitecan-triple-negative-breast-cancer (accessed on 30 January 2025).
- Modi, S.; Jacot, W.; Yamashita, T.; Sohn, J.; Vidal, M.; Tokunaga, E.; Tsurutani, J.; Ueno, N.T.; Prat, A.; Chae, Y.S.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N. Engl. J. Med. 2022, 387, 9–20. [Google Scholar] [CrossRef]
- European Medicines Agency CHMP. Post-Authorisation Summary of Positive Opinion for Enhertu (II-22). EMA/CHMP/932509/2022. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-enhertu-ii-22_en.pdf (accessed on 30 January 2025).
- U.S. Food and Drug Administration FDA. D.I.S.C.O. Burst Edition: FDA Approvals of Enhertu (Fam-Trastuzumab Deruxtecan-Nxki) for Unresectable or Metastatic HER2-Low Breast Cancer, and Nubeqa (Darolutamide) in Combination with Docetaxel for Metastatic Hormone-Sensitive Prostate Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-disco-burst-edition-fda-approvals-enhertu-fam-trastuzumab-deruxtecan-nxki-unresectable-or (accessed on 30 January 2025).
- Tarantino, P.; Viale, G.; Press, M.F.; Hu, X.; Penault-Llorca, F.; Bardia, A.; Batistatou, A.; Burstein, H.J.; Carey, L.A.; Cortes, J.; et al. ESMO Expert Consensus Statements (ECS) on the Definition, Diagnosis, and Management of HER2-Low Breast Cancer. Ann. Oncol. 2023, 34, 645–659. [Google Scholar] [CrossRef] [PubMed]
- Ivanova, M.; Porta, F.M.; D’Ercole, M.; Pescia, C.; Sajjadi, E.; Cursano, G.; De Camilli, E.; Pala, O.; Mazzarol, G.; Venetis, K.; et al. Standardized Pathology Report for HER2 Testing in Compliance with 2023 ASCO/CAP Updates and 2023 ESMO Consensus Statements on HER2-Low Breast Cancer. Virchows Arch. 2024, 484, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Fehrenbacher, L.; Cecchini, R.S.; Geyer, C.E.; Rastogi, P.; Costantino, J.P.; Atkins, J.N.; Crown, J.P.; Polikoff, J.; Boileau, J.-F.; Provencher, L.; et al. NSABP B-47/NRG Oncology Phase III Randomized Trial Comparing Adjuvant Chemotherapy With or Without Trastuzumab in High-Risk Invasive Breast Cancer Negative for HER2 by FISH and With IHC 1+ or 2. J. Clin. Oncol. 2020, 38, 444–453. [Google Scholar] [CrossRef]
- Abelman, R.O.; Wu, B.; Spring, L.M.; Ellisen, L.W.; Bardia, A. Mechanisms of Resistance to Antibody–Drug Conjugates. Cancers 2023, 15, 1278. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Bhattacharya, S.; Bowden, C.; Miller, K.; Comis, R.L. Independent Review of E2100: A Phase III Trial of Bevacizumab plus Paclitaxel versus Paclitaxel in Women with Metastatic Breast Cancer. J. Clin. Oncol. 2009, 27, 4966–4972. [Google Scholar] [CrossRef]
- European Medicines Agency. Post-Authorisation Summary of Positive Opinion for Avastin for Avastin. EMEA/CHMP/400280/2009. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-avastin_en.pdf-1 (accessed on 30 January 2025).
- Pazdur, R. Memorandum to the File BLA 125085 Avastin (Bevacizumab). Available online: www.fda.gov/media/79525/download (accessed on 30 January 2025).
- Miles, D.W.; Chan, A.; Dirix, L.Y.; Cortés, J.; Pivot, X.; Tomczak, P.; Delozier, T.; Sohn, J.H.; Provencher, L.; Puglisi, F.; et al. Phase III Study of Bevacizumab plus Docetaxel Compared with Placebo plus Docetaxel for the First-Line Treatment of Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer. J. Clin. Oncol. 2010, 28, 3239–3247. [Google Scholar] [CrossRef]
- Robert, N.J.; Diéras, V.; Glaspy, J.; Brufsky, A.M.; Bondarenko, I.; Lipatov, O.N.; Perez, E.A.; Yardley, D.A.; Chan, S.Y.T.; Zhou, X.; et al. RIBBON-1: Randomized, Double-Blind, Placebo-Controlled, Phase III Trial of Chemotherapy with or without Bevacizumab for First-Line Treatment of Human Epidermal Growth Factor Receptor 2-Negative, Locally Recurrent or Metastatic Breast Cancer. J. Clin. Oncol. 2011, 29, 1252–1260. [Google Scholar] [CrossRef]
- Vitry, A.; Nguyen, T.; Entwistle, V.; Roughead, E. Regulatory Withdrawal of Medicines Marketed with Uncertain Benefits: The Bevacizumab Case Study. J. Pharm. Policy Pract. 2015, 8, 25. [Google Scholar] [CrossRef]
- Hey, S.P.; Gyawali, B.; D’Andrea, E.; Kanagaraj, M.; Franklin, J.M.; Kesselheim, A.S. A Systematic Review and Meta-Analysis of Bevacizumab in First-Line Metastatic Breast Cancer: Lessons for Research and Regulatory Enterprises. J. Natl. Cancer Inst. 2020, 112, 335. [Google Scholar] [CrossRef]
- Conley, S.J.; Gheordunescu, E.; Kakarala, P.; Newman, B.; Korkaya, H.; Heath, A.N.; Clouthier, S.G.; Wicha, M.S. Antiangiogenic Agents Increase Breast Cancer Stem Cells via the Generation of Tumor Hypoxia. Proc. Natl. Acad. Sci. USA 2012, 109, 2784. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Cheng, H.; Liu, Y.; Liu, S.; Lowe, S.; Li, Y.; Bentley, R.; King, B.; Tuason, J.P.W.; Zhou, Q.; et al. Metformin Anticancer: Reverses Tumor Hypoxia Induced by Bevacizumab and Reduces the Expression of Cancer Stem Cell Markers CD44/CD117 in Human Ovarian Cancer SKOV3 Cells. Front. Pharmacol. 2022, 13, 955984. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency CHMP. Post-Authorisation Summary of Positive Opinion for Avastin. EMA/CHMP/295853/2011. Available online: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-avastin_en.pdf-0 (accessed on 30 January 2025).
- Preusser, M.; Fülöp, G.; Berghoff, A.S.; Heinzl, H.; Steger, G.G.; Greil, R.; Zielinski, C.C.; Bartsch, R. Influence of the American ODAC Statement on Austrian Bevacizumab Prescribing Practice for Metastatic Breast Cancer. Oncologist 2012, 17, e13–e17. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.; Chin, S.-F.; Rueda, O.M.; Vollan, H.-K.M.; Provenzano, E.; Bardwell, H.A.; Pugh, M.; Jones, L.; Russell, R.; Sammut, S.-J.; et al. The Somatic Mutation Profiles of 2,433 Breast Cancers Refine Their Genomic and Transcriptomic Landscapes. Nat. Commun. 2016, 7, 11479. [Google Scholar] [CrossRef]
- Schmid, P.; Abraham, J.; Chan, S.; Wheatley, D.; Brunt, A.M.; Nemsadze, G.; Baird, R.D.; Park, Y.H.; Hall, P.S.; Perren, T.; et al. Capivasertib Plus Paclitaxel Versus Placebo Plus Paclitaxel as First-Line Therapy for Metastatic Triple-Negative Breast Cancer: The PAKT Trial. J. Clin. Oncol. 2020, 38, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; McArthur, H.L.; Cortés, J.; Xu, B.; Cardoso, F.; Casalnuovo, M.L.; Demirci, U.; Freitas, R.; Ghosh, J.; Hegg, R.; et al. LBA19 Capivasertib (C) + Paclitaxel (P) as First-Line Treatment of Metastatic Triple-Negative Breast Cancer (MTNBC): The CAPItello-290 Phase III Trial. Ann. Oncol. 2024, 35, S1212–S1213. [Google Scholar] [CrossRef]
- Schmid, P.; Turner, N.C.; Barrios, C.H.; Isakoff, S.J.; Kim, S.-B.; Sablin, M.-P.; Saji, S.; Savas, P.; Vidal, G.A.; Oliveira, M.; et al. First-Line Ipatasertib, Atezolizumab, and Taxane Triplet for Metastatic Triple-Negative Breast Cancer: Clinical and Biomarker Results. Clin. Cancer Res. 2024, 30, 767–778. [Google Scholar] [CrossRef]
- Lehmann, B.D.; Bauer, J.A.; Schafer, J.M.; Pendleton, C.S.; Tang, L.; Johnson, K.C.; Chen, X.; Balko, J.M.; Gómez, H.; Arteaga, C.L.; et al. PIK3CA Mutations in Androgen Receptor-Positive Triple Negative Breast Cancer Confer Sensitivity to the Combination of PI3K and Androgen Receptor Inhibitors. Breast Cancer Res. 2014, 16, 406. [Google Scholar] [CrossRef]
- Sharifi, M.N.; O’Regan, R.M.; Wisinski, K.B. Is the Androgen Receptor a Viable Target in Triple Negative Breast Cancer in 5 Years? Clin. Breast Cancer 2023, 23, 813–824. [Google Scholar] [CrossRef]
- Eikesdal, H.P.; Yndestad, S.; Elzawahry, A.; Llop-Guevara, A.; Gilje, B.; Blix, E.S.; Espelid, H.; Lundgren, S.; Geisler, J.; Vagstad, G.; et al. Olaparib Monotherapy as Primary Treatment in Unselected Triple Negative Breast Cancer. Ann. Oncol. 2021, 32, 240–249. [Google Scholar] [CrossRef]
- Abraham, J.E.; Pinilla, K.; Dayimu, A.; Grybowicz, L.; Demiris, N.; Harvey, C.; Drewett, L.M.; Lucey, R.; Fulton, A.; Roberts, A.N.; et al. The PARTNER Trial of Neoadjuvant Olaparib with Chemotherapy in Triple-Negative Breast Cancer. Nature 2024, 629, 1142–1148. [Google Scholar] [CrossRef]
- Jain, A.; Barge, A.; Parris, C.N. Combination Strategies with PARP Inhibitors in BRCA-Mutated Triple-Negative Breast Cancer: Overcoming Resistance Mechanisms. Oncogene 2025, 44, 193–207. [Google Scholar] [CrossRef]
- Morganti, S.; Marra, A.; De Angelis, C.; Toss, A.; Licata, L.; Giugliano, F.; Taurelli Salimbeni, B.; Berton Giachetti, P.P.M.; Esposito, A.; Giordano, A.; et al. PARP Inhibitors for Breast Cancer Treatment: A Review. JAMA Oncol. 2024, 10, 658–670. [Google Scholar] [CrossRef]
- Sambade, M.J.; Van Swearingen, A.E.D.; McClure, M.B.; Deal, A.M.; Santos, C.; Sun, K.; Wang, J.; Mikule, K.; Anders, C.K. Efficacy and Pharmacodynamics of Niraparib in BRCA-Mutant and Wild-Type Intracranial Triple-Negative Breast Cancer Murine Models. Neuro-Oncol. Adv. 2019, 1, vdz005. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, F.; Gao, H.; Xu, Y. Successful Treatment of a Patient with Brain Metastases from Endometrial Cancer Using Niraparib: A Case Report. Ann. Palliat. Med. 2021, 10, 818–827. [Google Scholar] [CrossRef] [PubMed]
- Attarwala, H. TGN1412: From Discovery to Disaster. J. Young Pharm. 2010, 2, 332. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Ouyang, Q.; Sun, T.; Zhang, Q.; Teng, Y.; Cui, J.; Wang, H.; Yin, Y.; Wang, X.; Zhou, X.; et al. TORCHLIGHT: A Randomized, Double-Blind, Phase III Trial of Toripalimab versus Placebo, in Combination with Nab-Paclitaxel(Nab-P) for Patients with Metastatic or Recurrent Triple-Negative Breast Cancer (TNBC). J. Clin. Oncol. 2023, 41, LBA1013. [Google Scholar] [CrossRef]
- Conte, P.F.; Dieci, M.V.; Bisagni, G.; Schmid, P.; Fotia, V.; Piacentini, F.; De Laurentiis, M.; Favaretto, A.G.; Tamberi, S.; Bianchi, G.V.; et al. A-BRAVE Trial: A Phase III Randomized Trial with Avelumab in Early Triple-Negative Breast Cancer with Residual Disease after Neoadjuvant Chemotherapy or at High Risk after Primary Surgery and Adjuvant Chemotherapy. J. Clin. Oncol. 2024, 42, LBA500. [Google Scholar] [CrossRef]
- Tarantino, P.; Corti, C.; Schmid, P.; Cortes, J.; Mittendorf, E.A.; Rugo, H.; Tolaney, S.M.; Bianchini, G.; Andrè, F.; Curigliano, G. Immunotherapy for Early Triple Negative Breast Cancer: Research Agenda for the next Decade. npj Breast Cancer 2022, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bagegni, N.A.; Davis, A.A.; Clifton, K.K.; Ademuyiwa, F.O. Targeted Treatment for High-Risk Early-Stage Triple-Negative Breast Cancer: Spotlight on Pembrolizumab. Breast Cancer Targets Ther. 2023, 14, 113–123. [Google Scholar] [CrossRef]
- Voorwerk, L.; Slagter, M.; Horlings, H.M.; Sikorska, K.; van de Vijver, K.K.; de Maaker, M.; Nederlof, I.; Kluin, R.J.C.; Warren, S.; Ong, S.; et al. Immune Induction Strategies in Metastatic Triple-Negative Breast Cancer to Enhance the Sensitivity to PD-1 Blockade: The TONIC Trial. Nat. Med. 2019, 25, 920–928. [Google Scholar] [CrossRef]
- Giugliano, F.; Valenza, C.; Tarantino, P.; Curigliano, G. Immunotherapy for Triple Negative Breast Cancer: How Can Pathologic Responses to Experimental Drugs in Early-Stage Disease Be Enhanced? Expert Opin. Investig. Drugs 2022, 31, 855–874. [Google Scholar] [CrossRef] [PubMed]
- Rusak, A.; Jablonska, K.; Piotrowska, A.; Grzegrzolka, J.; Nowak, A.; Wojnar, A.; Dziegiel, P. The Role of CHI3L1 Expression in Angiogenesis in Invasive Ductal Breast Carcinoma. Anticancer Res. 2018, 38, 3357–3366. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, N.M.; Jaradat, S.K.; Al-Shami, K.M.; Alkhalifa, A.E. Targeting Angiogenesis in Breast Cancer: Current Evidence and Future Perspectives of Novel Anti-Angiogenic Approaches. Front. Pharmacol. 2022, 13, 838133. [Google Scholar] [CrossRef]
- Nedeljković, M.; Vuletić, A.; Mirjačić Martinović, K. Divide and Conquer—Targeted Therapy for Triple-Negative Breast Cancer. Int. J. Mol. Sci. 2025, 26, 1396. [Google Scholar] [CrossRef]
- Xu, B.; Yin, Y.; Fan, Y.; Ouyang, Q.; Song, L.; Wang, X.; Li, W.; Li, M.; Yan, X.; Wang, S.; et al. Sacituzumab Tirumotecan (SKB264/MK-2870) in Patients (Pts) with Previously Treated Locally Recurrent or Metastatic Triple-Negative Breast Cancer (TNBC): Results from the Phase III OptiTROP-Breast01 Study. J. Clin. Oncol. 2024, 42, 104. [Google Scholar] [CrossRef]
- Tarantino, P.; Lee, D.; Foldi, J.; Soulos, P.R.; Gross, C.P.; O’Meara, T.; Grinda, T.; Waks, A.G.; Winer, E.P.; Lin, N.U.; et al. Abstract P1-08-08: Real-World Efficacy of Immediate Subsequent Lines of Therapy after Trastuzumab Deruxtecan (T-DXd) in Patients with Metastatic Breast Cancer (MBC)—Retrospective Study from the Nationwide Flatiron Database. Clin. Cancer Res. 2025, 31, P1-08. [Google Scholar] [CrossRef]
- Rugo, H.S.; Cortes, J.; Barrios, C.H.; Cabrera, P.; Xu, B.; Huang, C.-S.; Kim, S.-B.; Melisko, M.; Nanda, R.; Pieńkowski, T.; et al. GLORIA: Phase III, Open-Label Study of Adagloxad Simolenin/OBI-821 in Patients with High-Risk Triple-Negative Breast Cancer. Future Oncol. 2022, 18, 3801–3813, Erratum in JAMA Intern. Med. 2018, 178, 1433. [Google Scholar] [CrossRef] [PubMed]
- Simmons, A.; Haggery, R. Disease Analysis: Breast Cancer: Triple-Negative. Datamonitor, Powered by BIOMEDTRACKER. 2024. Available online: https://www.biomedtracker.com/reportdetail.cfm?reportid=1361 (accessed on 30 January 2025).
- Edlin, R.; Round, J.; Hulme, C.; McCabe, C. Cost-Effectiveness Analysis and Efficient Use of the Pharmaceutical Budget: The Key Role of Clinical Pharmacologists. Br. J. Clin. Pharmacol. 2010, 70, 350–355, Erratum in Biostatistics 2019, 20, 366. https://doi.org/10.1093/biostatistics/kxy072. [Google Scholar] [CrossRef]
- Cedillo, S.; González-Domínguez, A.; Ivanova-Markova, Y.; López López, R.; López-Tarruella Cobo, S.; Peña Pedrosa, J.A. Cost-Utility Analysis of Adjuvant Olaparib for Germline BRCA1/2-Mutated, High-Risk HER2-Negative Early Breast Cancer in Spain. PharmacoEconomics Open 2024, 8, 887–896. [Google Scholar] [CrossRef]
- Polyzoi, M.; Ekman, M.; Reithmeier, A.; Jacob, J.; Karlsson, E.; Bertranou, E.; Linderholm, B.; Hettle, R. Cost-Effectiveness Analysis of Adjuvant Olaparib Versus Watch and Wait in the Treatment of Germline BRCA1/2-Mutated, High-Risk, HER2-Negative Early Breast Cancer in Sweden. PharmacoEconomics Open 2024, 8, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Zettler, C.M.; De Silva, D.L.; Blinder, V.S.; Robson, M.E.; Elkin, E.B. Cost-Effectiveness of Adjuvant Olaparib for Patients With Breast Cancer and Germline BRCA1/2 Mutations. JAMA Netw. Open 2024, 7, e2350067. [Google Scholar] [CrossRef]
- Wu, H.-L.; Luo, Z.-Y.; He, Z.-L.; Gong, Y.; Mo, M.; Ming, W.-K.; Liu, G.-Y. All HER2-Negative Breast Cancer Patients Need GBRCA Testing: Cost-Effectiveness and Clinical Benefits. Br. J. Cancer 2023, 128, 638–646. [Google Scholar] [CrossRef]
- Saito, S.; Nakazawa, K.; Nagahashi, M.; Ishikawa, T.; Akazawa, K. Cost–Effectiveness of BRCA1/2 Mutation Profiling to Target Olaparib Use in Patients with Metastatic Breast Cancer. Pers. Med. 2019, 16, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Tuffaha, H.; Scuffham, P. Cost-Effectiveness Analsysis of Germline BRCA Mutation Testing and Olaparib Treatment in Metastatic Breast Cancer: An Evaluation of Codependent Technologies. Value Health 2019, 22, S454. [Google Scholar] [CrossRef]
- Pan, J.; Ren, N.; Ren, L.; Yang, Y.; Xu, Q. Cost-Effectiveness of Talazoparib for Patients with Germline BRCA1/2 Mutated HER2-Negative Advanced Breast Cancer in China and the US. Sci. Rep. 2024, 14, 13935. [Google Scholar] [CrossRef]
- Lima, A.O.d.L.; Špacírová, Z.; Fénix-Caballero, S.; Hoces, A.M.; Vegas, A.S.; Aranzana, M.C.; Sierra-Sánchez, J.F.; Díaz, M.D.; Del Rey, E.J. Cost-Utility of Talazoparib Monotherapy Treatment for Locally Advanced or Metastatic Breast Cancer in Spain. Breast 2021, 58, 27–33. [Google Scholar] [CrossRef]
- Schwarz, F.; Arefian, H.; Hartmann, M.; Runnebaum, I. Cost-Effectiveness of Talazoparib for Patients with Locally Advanced or Metastasized Breast Cancer in Germany. PLoS ONE 2022, 17, e0278460. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Han, M.; Liu, A.; Shi, B. Economic Evaluation of Sacituzumab Govitecan for the Treatment of Metastatic Triple-Negative Breast Cancer in China and the US. Front. Oncol. 2021, 11, 734594. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Li, S.; Li, Y.; Li, J. Cost-Effectiveness of Sacituzumab Govitecan versus Chemotherapy in Patients with Relapsed or Refractory Metastatic Triple-Negative Breast Cancer. BMC Health Serv. Res. 2023, 23, 706. [Google Scholar] [CrossRef]
- Wu, Y.; Hu, S.; Liu, X.; Chen, Y.; Luan, J.; Wang, S. Cost-Effectiveness of Sacituzumab Govitecan versus Single-Agent Chemotherapy for Metastatic Triple-Negative Breast Cancer: A Trial-Based Analysis. Cost Eff. Resour. Alloc. 2024, 22, 32. [Google Scholar] [CrossRef]
- Paulissen, J.H.J.; van Schoonhoven, A.V.; Olin, E.; Postma, A.J.; Mbanya, Z.; Dunton, K.J.; Postma, M.J.; van Hulst, M.; Freriks, R.D. Cost-Effectiveness of Trastuzumab Deruxtecan in Patients with Unresectable or Metastatic HER2-Low Breast Cancer Who Have Received Prior Chemotherapy. Adv. Ther. 2025, 42, 322–333. [Google Scholar] [CrossRef]
- Yang, J.; Han, J.; Zeng, N.; Yan, X. Cost-Effectiveness of Trastuzumab Deruxtecan in Previously Treated Human Epidermal Growth Factor Receptor 2-Low Metastatic Breast Cancer. Ther. Adv. Med. Oncol. 2023, 15, 17588359231169984. [Google Scholar] [CrossRef]
- Huang, M.A.; Fasching, P.; Haiderali, A.; Xue, W.; Yang, C.; Pan, W.; Zhou, Z.-Y.; Hu, P.; Chaudhuri, M.; Le Bailly De Tilleghem, C.; et al. Cost-Effectiveness of Neoadjuvant Pembrolizumab Plus Chemotherapy Followed by Adjuvant Single-Agent Pembrolizumab for High-Risk Early-Stage Triple-Negative Breast Cancer in the United States. Adv. Ther. 2023, 40, 1153–1170. [Google Scholar] [CrossRef] [PubMed]
- Favre-Bulle, A.; Huang, M.; Haiderali, A.; Bhadhuri, A. Cost-Effectiveness of Neoadjuvant Pembrolizumab plus Chemotherapy Followed by Adjuvant Pembrolizumab in Patients with High-Risk, Early-Stage, Triple-Negative Breast Cancer in Switzerland. PharmacoEconomics Open 2024, 8, 91–101. [Google Scholar] [CrossRef]
- Kwong, A.; Leung, R.; Chan, T.C.; Khandelwal, A.; Mishra, K.; Huang, M. Cost-Effectiveness of Pembrolizumab in Combination with Chemotherapy as Neoadjuvant Treatment and Continued as a Single Agent Adjuvant Treatment for High-Risk Early-Stage Triple-Negative Breast Cancer in Hong Kong. Oncol. Ther. 2024, 12, 525–547. [Google Scholar] [CrossRef]
- Huang, M.; Fasching, P.; Haiderali, A.; Pan, W.; Gray, E.; Zhou, Z.-Y.; Hu, P.; Chaudhuri, M.; Bailly De Tilleghem, C.L.; Cappoen, N.; et al. Cost–Effectiveness of Pembrolizumab Plus Chemotherapy as First-Line Treatment in PD-L1-Positive Metastatic Triple-Negative Breast Cancer. Immunotherapy 2022, 14, 1027–1041. [Google Scholar] [CrossRef]
- Phua, L.C.; Lee, S.C.; Ng, K.; Abdul Aziz, M.I. Cost-Effectiveness Analysis of Atezolizumab in Advanced Triple-Negative Breast Cancer. BMC Health Serv. Res. 2020, 20, 581. [Google Scholar] [CrossRef] [PubMed]
- Chisaki, Y.; Kuwada, Y.; Matsumura, C.; Yano, Y. Cost-Effectiveness Analysis of Atezolizumab Plus Nab-Paclitaxel for Advanced PD-L1 Positive Triple-Negative Breast Cancer in Japan. Clin. Drug Investig. 2021, 41, 381–389. [Google Scholar] [CrossRef]
- Prasad, V.; Mailankody, S. Research and Development Spending to Bring a Single Cancer Drug to Market and Revenues After Approval. JAMA Intern. Med. 2017, 177, 1569–1575. [Google Scholar] [CrossRef] [PubMed]
- DiMasi, J.A.; Grabowski, H.G.; Hansen, R.W. Innovation in the Pharmaceutical Industry: New Estimates of R&D Costs. J. Health Econ. 2016, 47, 20–33. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.H.; Siah, K.W.; Lo, A.W. Estimation of Clinical Trial Success Rates and Related Parameters. Biostatistics 2019, 20, 273–286. [Google Scholar] [CrossRef]
- Hercules, S.M.; Alnajar, M.; Chen, C.; Mladjenovic, S.M.; Shipeolu, B.A.; Perkovic, O.; Pond, G.R.; Mbuagbaw, L.; Blenman, K.R.; Daniel, J.M. Triple-Negative Breast Cancer Prevalence in Africa: A Systematic Review and Meta-Analysis. BMJ Open 2022, 12, e055735. [Google Scholar] [CrossRef]
- Lukong, K.E.; Ogunbolude, Y.; Kamdem, J.P. Breast Cancer in Africa: Prevalence, Treatment Options, Herbal Medicines, and Socioeconomic Determinants. Breast Cancer Res. Treat. 2017, 166, 351–365. [Google Scholar] [CrossRef]
- Sarkar, S.; Akhtar, M. Triple Negative Breast Cancer Prevalence in Indian Patients over a Decade: A Systematic Review. Int. J. Clin. Biostat. Biom. 2022, 8, 45. [Google Scholar] [CrossRef]
- Almansour, N.M. Triple-Negative Breast Cancer: A Brief Review About Epidemiology, Risk Factors, Signaling Pathways, Treatment and Role of Artificial Intelligence. Front. Mol. Biosci. 2022, 9, 836417. [Google Scholar] [CrossRef]
- Fundytus, A.; Sengar, M.; Lombe, D.; Hopman, W.; Jalink, M.; Gyawali, B.; Trapani, D.; Roitberg, F.; Vries, E.G.E.D.; Moja, L.; et al. Access to Cancer Medicines Deemed Essential by Oncologists in 82 Countries: An International, Cross-Sectional Survey. Lancet Oncol. 2021, 22, 1367–1377. [Google Scholar] [CrossRef]
- Ocran Mattila, P.; Ahmad, R.; Hasan, S.S.; Babar, Z.-U.-D. Availability, Affordability, Access, and Pricing of Anti-Cancer Medicines in Low- and Middle-Income Countries: A Systematic Review of Literature. Front. Public Health 2021, 9, 628744. [Google Scholar] [CrossRef]
- Michaeli, D.T.; Michaeli, T. Cancer Drug Prices in the United States: Efficacy, Innovation, Clinical Trial Evidence, and Epidemiology. Value Health 2023, 26, 1590–1600. [Google Scholar] [CrossRef] [PubMed]
- Godman, B.; Hill, A.; Simoens, S.; Selke, G.; Selke Krulichová, I.; Zampirolli Dias, C.; Martin, A.P.; Oortwijn, W.; Timoney, A.; Gustafsson, L.L.; et al. Potential Approaches for the Pricing of Cancer Medicines across Europe to Enhance the Sustainability of Healthcare Systems and the Implications. Expert Rev. Pharmacoecon. Outcomes Res. 2021, 21, 527–540. [Google Scholar] [CrossRef] [PubMed]
- American Society of Clinical Oncology. Position Statement on Addressing the Affordability of Cancer Drugs. J. Oncol. Pract. 2018, 14, 187–192. [Google Scholar] [CrossRef] [PubMed]
- John, A.; Yarmuth, H.R. 5376—117th Congress (2021–2022): Inflation Reduction Act of 2022. Available online: https://www.congress.gov/bill/117th-congress/house-bill/5376 (accessed on 31 January 2025).
- Horn, D.M.; Jacobson, M.; Alpert, A.E.; Duggan, M.G. Why Does the Inflation Reduction Act Exclude Expensive Cancer Treatments in Price Negotiations? JCO Oncol. Pract. 2024, 20, 254–261. [Google Scholar] [CrossRef]
- Post, H.C.; Schutte, T.; van Oijen, M.G.H.; van Laarhoven, H.W.M.; Hollak, C.E.M. Time to Reimbursement of Novel Anticancer Drugs in Europe: A Case Study of Seven European Countries. ESMO Open 2023, 8, 101208. [Google Scholar] [CrossRef]
- Barrios, C.; de Lima Lopes, G.; Yusof, M.M.; Rubagumya, F.; Rutkowski, P.; Sengar, M. Barriers in Access to Oncology Drugs—A Global Crisis. Nat. Rev. Clin. Oncol. 2023, 20, 7–15. [Google Scholar] [CrossRef]
- Pramesh, C.S.; Badwe, R.A.; Bhoo-Pathy, N.; Booth, C.M.; Chinnaswamy, G.; Dare, A.J.; de Andrade, V.P.; Hunter, D.J.; Gopal, S.; Gospodarowicz, M.; et al. Priorities for Cancer Research in Low- and Middle-Income Countries: A Global Perspective. Nat. Med. 2022, 28, 649–657. [Google Scholar] [CrossRef]

| NCT # | Phase | Treatment Arms | Therapeutic Mechanism/ Target | Inclusive TNBC Stage and Biomarkers | Primary Endpoint(s), Results | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Small molecules | ||||||||||||
| NCT02423603 | 2 | capivasertib paclitaxel | placebo paclitaxel | PI3K-Akt inhibition (pan-AKT) chemotherapy | advanced TNBC | PFS | ||||||
| NCT03997123 | 3 | capivasertib paclitaxel | placebo paclitaxel | PI3K-Akt inhibition (pan-AKT) chemotherapy | advanced TNBC | OS: 17.7 vs. 18 months, ns | ||||||
| NCT03337724 | 3 | ipatasertib paclitaxel | placebo paclitaxel | PI3K-Akt inhibition (pan-AKT) chemotherapy | advanced TNBC | PFS (altered TNBC): 7.4 vs. 6.1 months, ns; PFS (not altered TNBC): 7.1 months | ||||||
| NCT04251533 | 3 | alpelisib nab-p | placebo nab-p | PI3K-Akt inhibition (PI3K) chemotherapy | advanced TNBC; PI3K mut or PTEN loss | PFS: 7.2 vs. 5.6 months, ns; ORR (tumors with PTEN loss): 14.3% | ||||||
| NCT05954442 | 3 | everolimus investigator’s choice of chemotherapy | placebo investigator’s choice of chemotherapy | PI3K-Akt inhibition (mTOR) chemotherapy | advanced LAR TNBC; PI3K-Akt mut | PFS; ongoing | ||||||
| NCT02624973 | 2 | olaparib cyclophosphamide | PARPi chemotherapy | untreated | Predictive and prognostic value of mutations in 300 cancer-related genes; ongoing | |||||||
| NCT03150576 | 2/3 | olaparib paclitaxel and carboplatin | paclitaxel and carboplatin | PARPi chemotherapy | - | pCR: 51% vs. 52%, ns | ||||||
| NCT04915755 | 3 | niraparib | placebo | PARPi | stage I-III | Number of patients with AEs, change in ECOG performance, change in relevant laboratory parameters, and use of concomitant medications; ongoing | ||||||
| NCT04799249 | 3 | trilaciclib gemcitabine carboplatin | placebo gemcitabine carboplatin | CDK4/6 chemotherapy chemotherapy | advanced TNBC | OS; ongoing | ||||||
| Antibodies | ||||||||||||
| NCT04085276 | 3 | toripalimab nab-p | placebo nab-p | immunotherapy (PD-1 blockade) | advanced TNBC | PFS (PD-L1+): 8.4 vs. 5.6 months, significant; PFS (intention-to-treat): 8.4 vs. 6.9 months, significant | ||||||
| NCT02926196 | 3 | avelumab | observation | immunotherapy (PD-L1 blockade) | high risk, non-mTNBC | DFS: 68.3 vs. 63.4%, ns | ||||||
| NCT06313463 | 3 | carrellizumab capecitabine | placebo capecitabine | immunotherapy (PD-1 blockade) | stage I-III TNBC | DFS; ongoing | ||||||
| NCT02499367 | 2 | nivolumab observation/radiation/cyclophosphamide/cisplatin/doxorubicin | immunotherapy (PD-1 blockade) observation/radiation/chemotherapy | advanced TNBC | PFS: 1.9 months | |||||||
| NCT05078047 | 3 | reduced dose intensity of ICI | immunotherapy | advanced TNBC | PFS; ongoing | |||||||
| NCT05806060 | 3 | BP102 nab-p + capecitabine/TPC | nab-p + capecitabine/TPC | anti-angiogenic agent | advanced TNBC, basal-like immunosuppressed subtype [42] | PFS; ongoing | ||||||
| ADCs | ||||||||||||
| NCT05552001 | 3 | SG | TROP2-targeted topoisomerase 1 inhibitor delivery | advanced TNBC | ORR; ongoing | |||||||
| NCT05382299 | 3 | SG | TPC (paclitaxel/nab-p/gemcitabine/carboplatin) | TROP2-targeted topoisomerase 1 inhibitor delivery chemotherapy | untreated advanced TNBC; untreated and PD-L1- treated with ICI and PD-L1+ | PFS; ongoing | ||||||
| NCT06279364 | 3 | ST | investigator’s choice chemotherapy (paclitaxel/nab-p/capecitabine/eribulin/carboplatin) | TROP2-targeted topoisomerase 1 inhibitor delivery chemotherapy | advanced TNBC | OS, PFS; and ongoing | ||||||
| NCT05347134 | 3 | ST | eribulin capecitabine gemcitabine vinorelbine | TROP2-targeted topoisomerase 1 inhibitor delivery chemotherapy | advanced TNBC | PFS: 5.8 vs. 1.9 months, significant | ||||||
| NCT05374512 | 3 | Dato-DXd | investigator’s choice of chemotherapy: paclitaxel/nab-p/carboplatin/capecitabine/eribulin mesylate | TROP2-targeted topoisomerase 1 inhibitor delivery chemotherapy | advanced TNBC | PFS, OS; ongoing | ||||||
| Others | ||||||||||||
| NCT03562637 | 3 | adagloxad simolenin + OBI-821 SOC (observation, capecitabine, ICI ± and capecitabine) | SOC (observation, capecitabine, and ICI ± capecitabine) | vaccine observation/chemotherapy/immunotherapy | high risk early disease, Globo H+ | invasive PFS; ongoing | ||||||
| Combinatorial approaches | ||||||||||||
| NCT04177108 | 3 | (A) ipatasertib atezolizumab paclitaxel | (B) ipatasertib placebo paclitaxel | (C) placebo placebo paclitaxel | PI3K-Akt inhibition (pan-AKT) immunotherapy (PD-L1 blockade) chemotherapy | advanced TNBC; PD-L1- | PFS (A vs. C): 7.1 vs. 3.7 months, significant; PFS (B vs. C): 5.6 vs. 3.7 months, ns; OS (A vs. C): 15.7 vs. 16.6 months, ns; and OS (B vs. C): 15.3 vs. 16.6 months, ns | |||||
| ipatasertib atezolizumab paclitaxel | ipatasertib placebo paclitaxel | PI3K-Akt inhibition (pan-AKT) immumotherapy (PD-L1 blockade) chemotherapy | advanced TNBC; PD-L1+ | PFS: 5.6 vs. 5.7 months, ns; OS: NA vs. 17.2 months, ns | ||||||||
| NCT05760378 | 3 | famitinib camrelizumab nab-p/capecitabine/eribulin mesylate/carboplatin | camrelizumab nab-p/capecitabine/eribulin mesylate/carboplatin | RTK inhibition immunotherapy (PD-1 blockade) chemotherapy | advanced TNBC | PFS; ongoing | ||||||
| NCT05999149 | 3 | famitinib camrelizumab albumin-paclitaxel, carboplatin | camrelizumab albumin-paclitaxel plus carboplatin | RTK inhibition immunotherapy (PD-1 blockade) chemotherapy | stage II-III TNBC | pCR; ongoing | ||||||
| NCT05382286 | 3 | SG pembrolizumab | pembrolizumab paclitaxel, nab-p, gemcitabine | TROP2-targeted topoisomerase 1 inhibitor delivery immunotherapy (PD-1 blockade) chemotherapy | previously untreated, advanced TNBC; PD-L1+ | PFS; ongoing | ||||||
| NCT05633654 | 3 | SG pembrolizumab | pembrolizumab capecitabine | TROP2-targeted topoisomerase 1 inhibitor delivery immunotherapy (PD-1 blockade) chemotherapy | pretreated, stage I-III TNBC | invasive DFS; ongoing | ||||||
| NCT05629585 | 3 | Dato-Dxd durvalumab | Dato-Dxd | pembrolizumab capecitabine | TROP2-targeted topoisomerase 1 inhibitor delivery immunotherapy (PD1/PD-L1 blockade) chemotherapy | stage I-III TNBC | invasive DFS; ongoing | |||||
| NCT06112379 | 3 | Dato-DXd durvalumab adjuvant chemotherapy/olaparib in case of residual disease | pembrolizumab chemotherapy | TROP2-targeted topoisomerase 1 inhibitor delivery immunotherapy (PD1/PD-L1 blockade) chemotherapy | previously untreated, stage II-III TNBC | pCR, EFS; ongoing | ||||||
| NCT06072612 | 3 | SV-BR-1-GM cyclophosphamide peginterferon alfa-2a retifanlimab | TPC | SV-BR-1-GM cyclophosphamide peginterferon alfa-2a | vaccine (cell line secreting GM-CSF injected intradermally) chemotherapy immunoterhapy (interferon) immunotherapy (PD-1 blockade) | advanced TNBC | OS; ongoing | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lebedeva, V.; Ebbinghaus, M.; Hidalgo, J.V.; Hardt, O.; Pfeifer, R. Triple-Negative Breast Cancer Unveiled: Bridging Science, Treatment Strategy, and Economic Aspects. Int. J. Mol. Sci. 2025, 26, 9714. https://doi.org/10.3390/ijms26199714
Lebedeva V, Ebbinghaus M, Hidalgo JV, Hardt O, Pfeifer R. Triple-Negative Breast Cancer Unveiled: Bridging Science, Treatment Strategy, and Economic Aspects. International Journal of Molecular Sciences. 2025; 26(19):9714. https://doi.org/10.3390/ijms26199714
Chicago/Turabian StyleLebedeva, Valeriia, Mira Ebbinghaus, José Villacorta Hidalgo, Olaf Hardt, and Rita Pfeifer. 2025. "Triple-Negative Breast Cancer Unveiled: Bridging Science, Treatment Strategy, and Economic Aspects" International Journal of Molecular Sciences 26, no. 19: 9714. https://doi.org/10.3390/ijms26199714
APA StyleLebedeva, V., Ebbinghaus, M., Hidalgo, J. V., Hardt, O., & Pfeifer, R. (2025). Triple-Negative Breast Cancer Unveiled: Bridging Science, Treatment Strategy, and Economic Aspects. International Journal of Molecular Sciences, 26(19), 9714. https://doi.org/10.3390/ijms26199714







