Expression of Elafin and CD200 as Immune Checkpoint Molecules Involved in Celiac Disease
Abstract
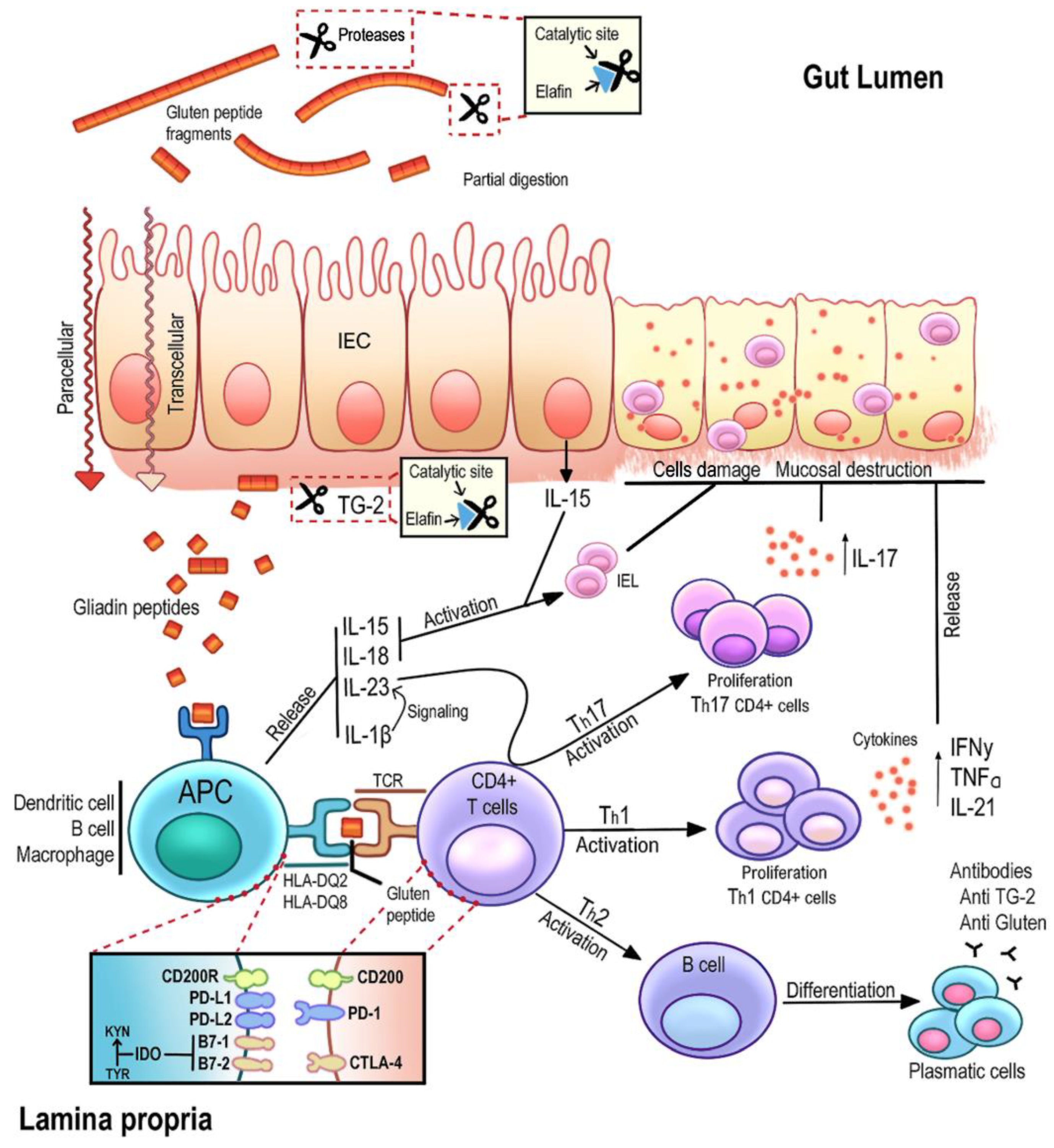
1. Introduction
2. Results
2.1. Diagnosis: Serological, Genetic, and Histological Analysis
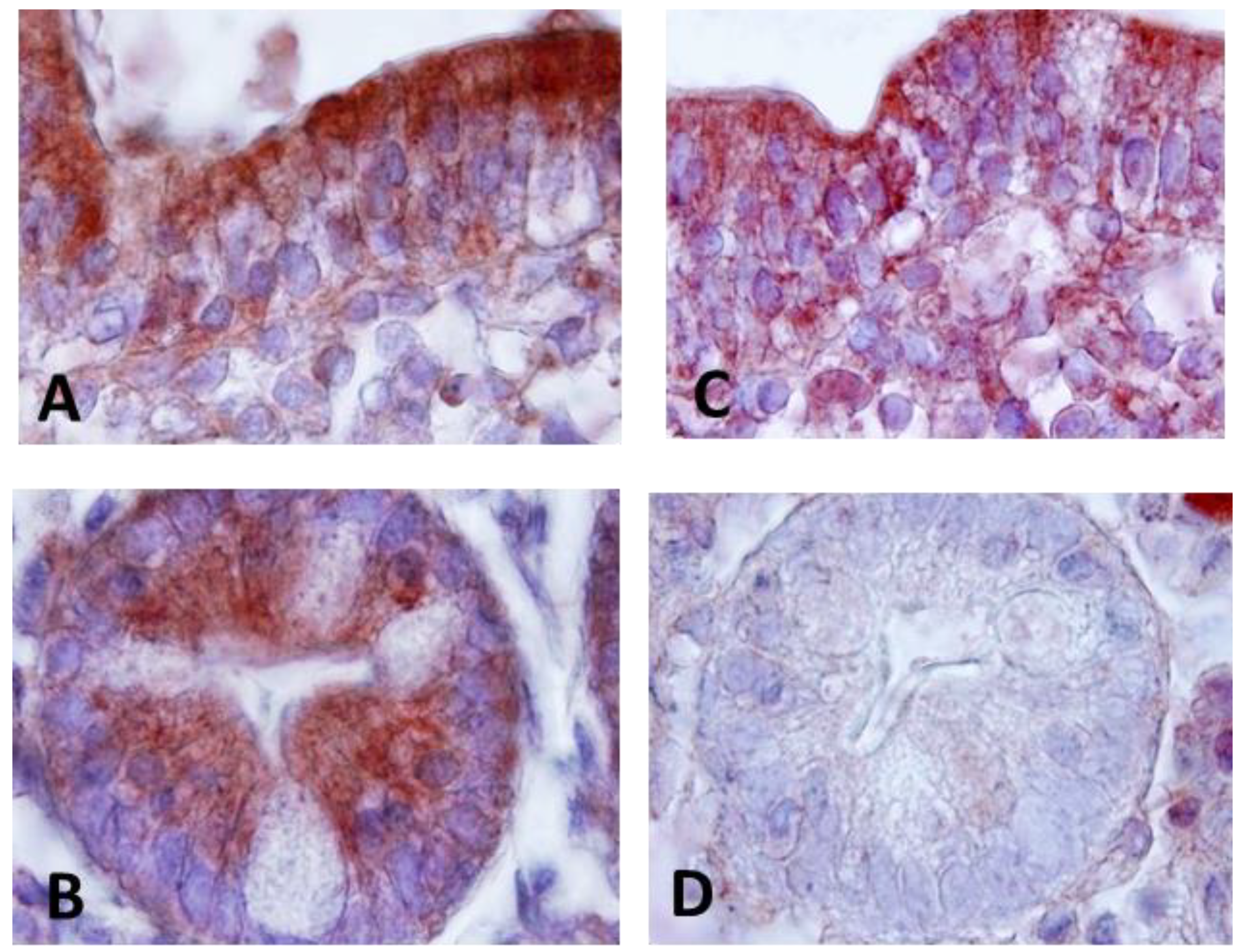
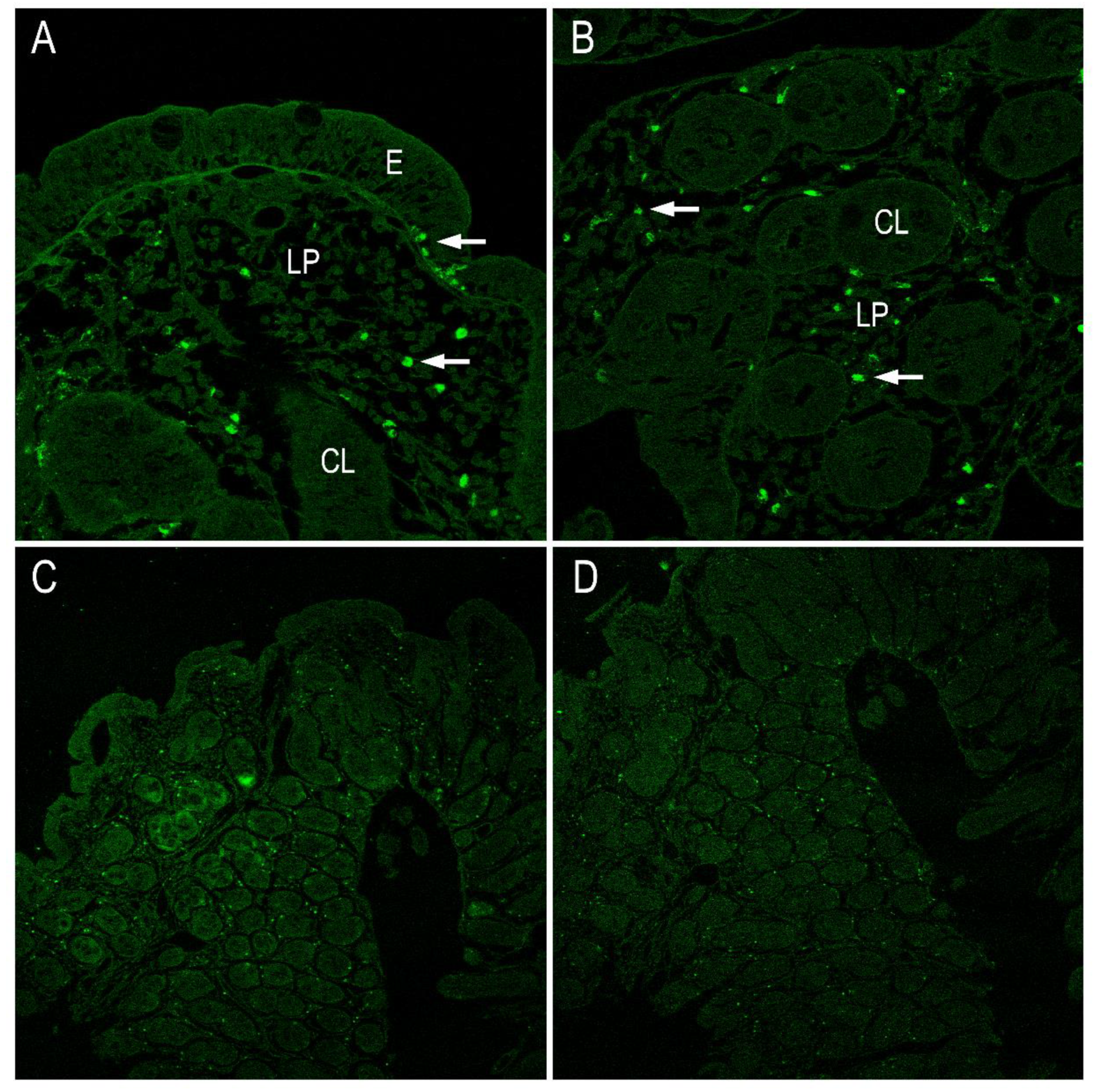
2.2. CD200, CD200R and Elafin Distribution in Intestinal Mucosa Tissue from CD Patients by Immunohistochemistry
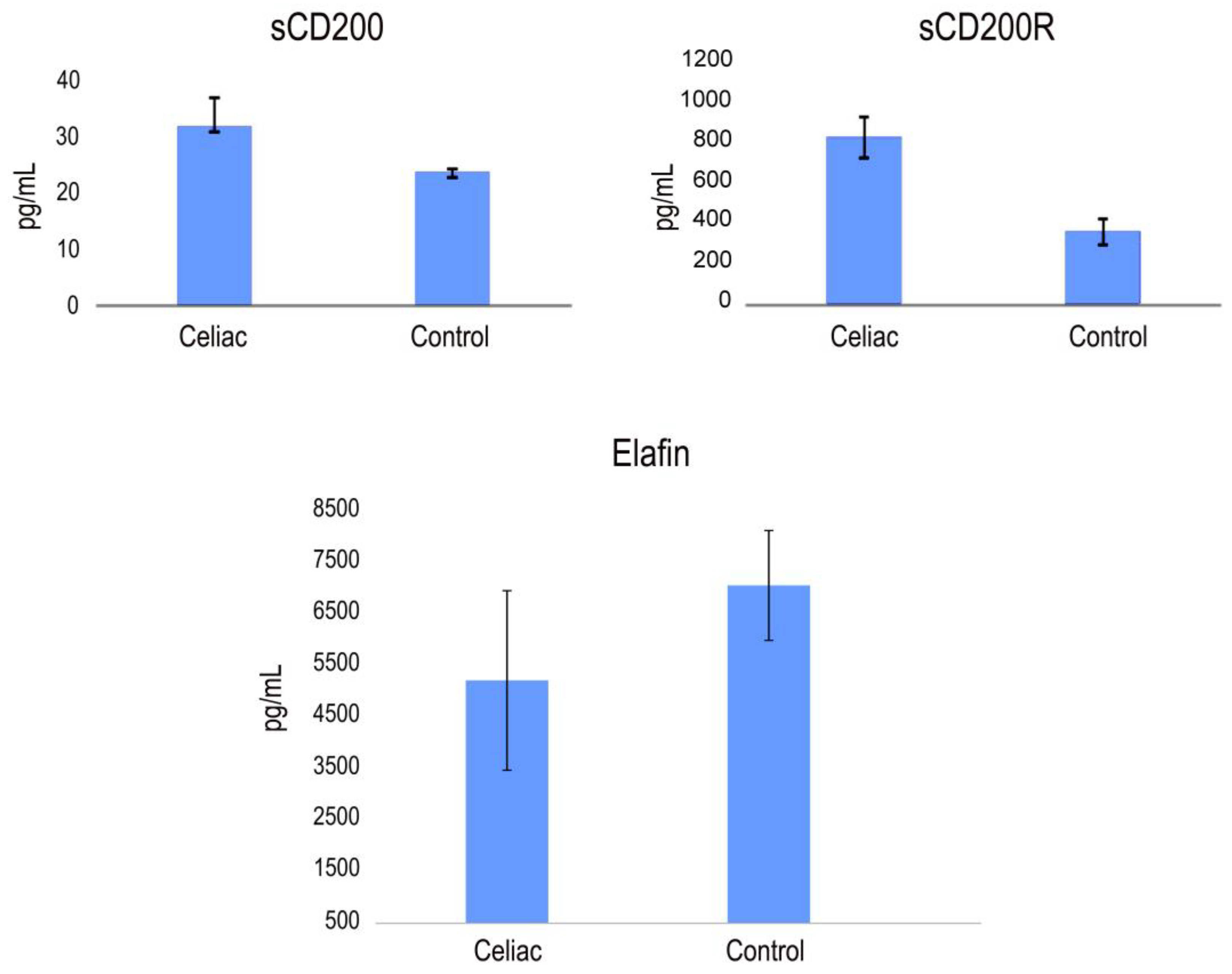
2.3. Detection of CD200, CD200R and Elafin Protein in Serum from CD Patients by ELISA Assays
2.4. CD4 and CD8 IFN-Gamma Expression in CD Patients: Gamma Interferon Responses of CD4 and CD8 T-Cell Subsets
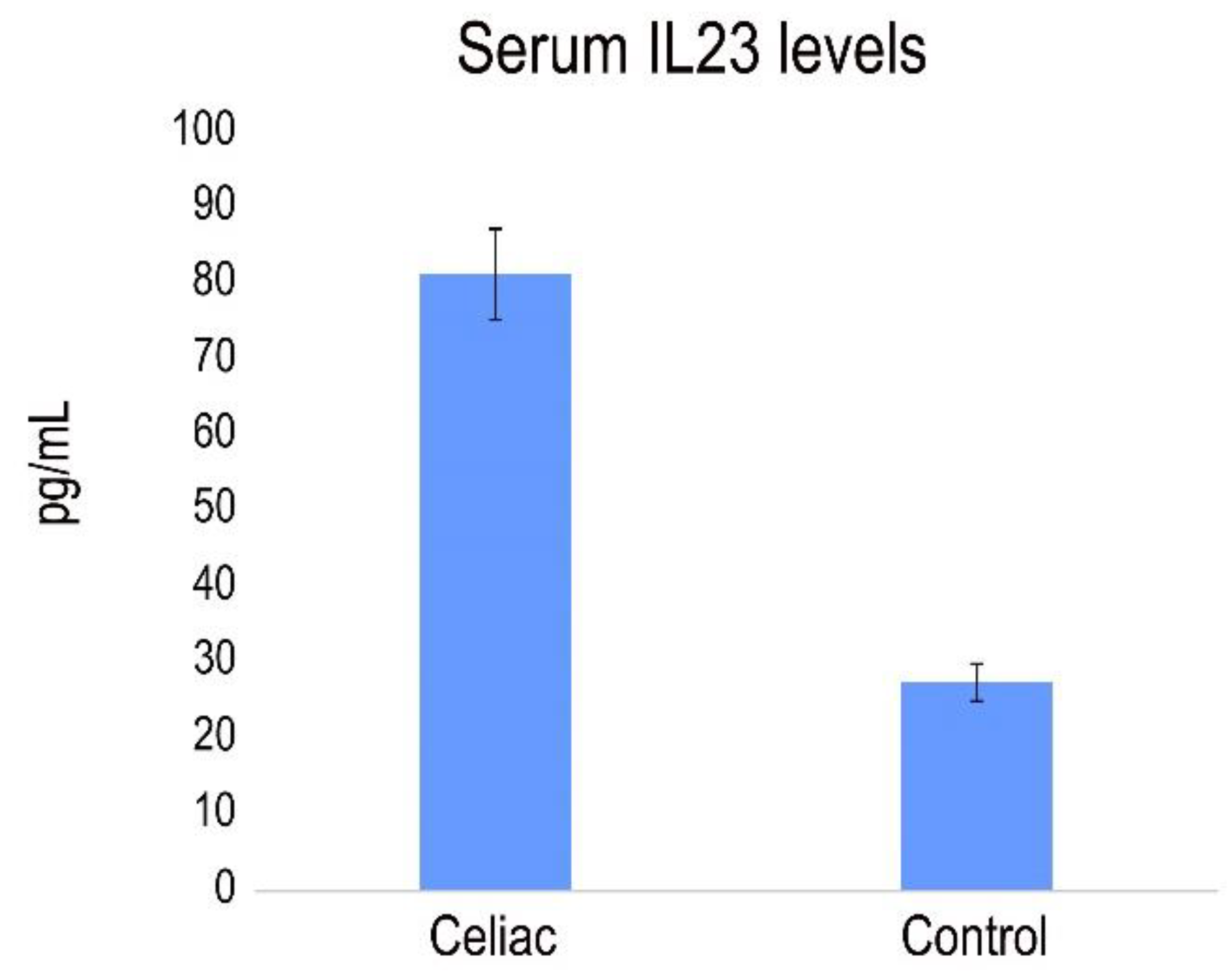
2.5. Analysis of Th1 and Th17 Cytokines
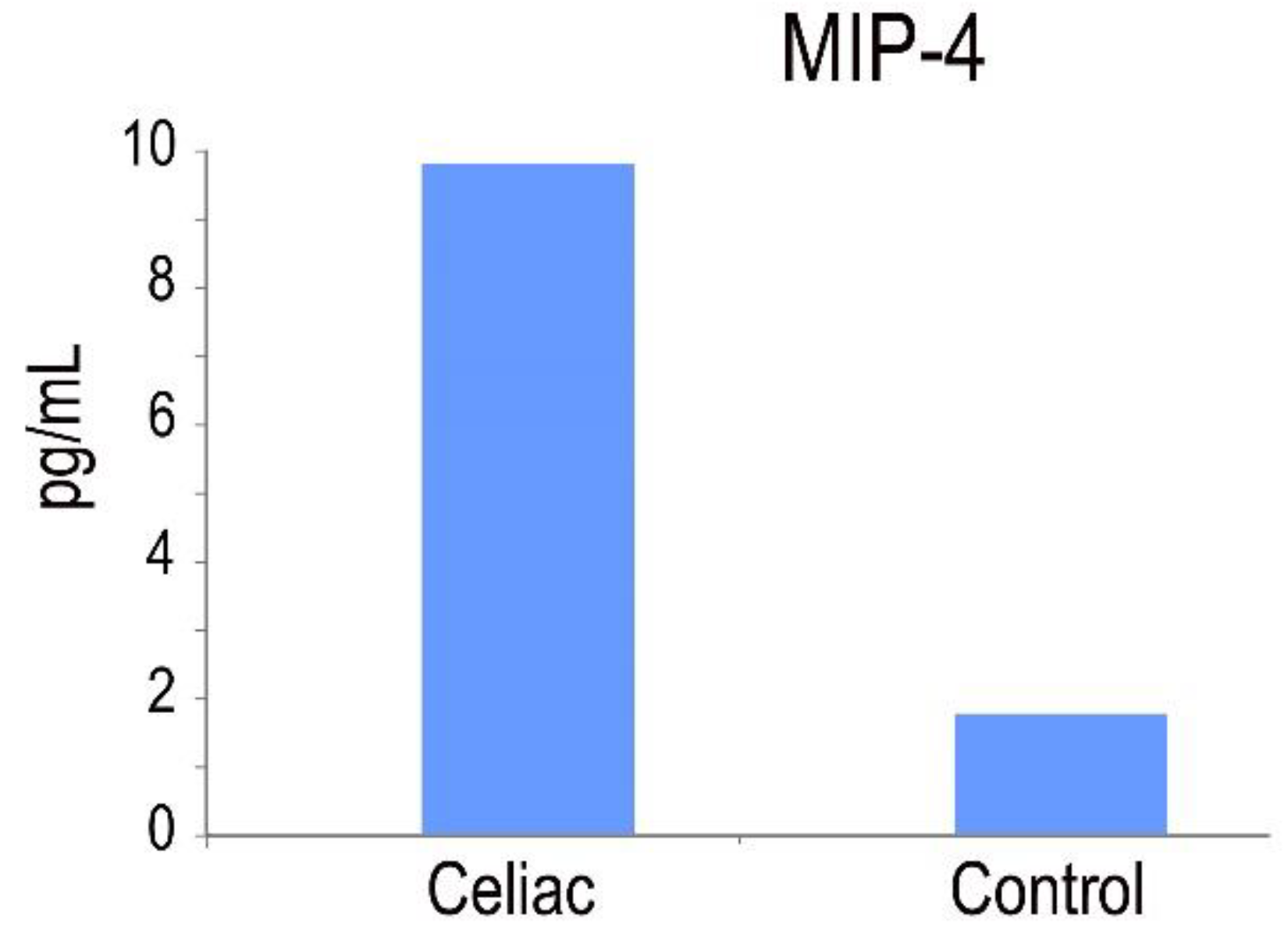
2.6. MIP-4 Protein in CD
2.7. PI3 Genotype and Frequencies
3. Discussion
4. Materials and Methods
4.1. Study Samples
4.2. Immunohistochemical Staining
4.3. ELISA Assays in Serum from Patients
4.3.1. Analysis of the Levels of Soluble CD200, CD200R and Elafin in Serum
4.3.2. Analysis and Expression of Th1 (IFNγ), Th17 (IL23) Cytokine Production
4.3.3. Quantitative Measurement of Human MIP4 Levels in the Serum
4.4. Elafin Genotype and Allele Frequencies
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-Casado, M.Á.; Lorite, P.; Ponce de León, C.; Palomeque, T.; Torres, M.I. Celiac Disease Autoimmunity. Arch. Immunol. Ther. Exp. 2018, 66, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Sollid, L.M.; Jabri, B. Triggers and drivers of autoimmunity: Lessons from coeliac disease. Nat. Rev. Immunol. 2013, 13, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Torres, M.I.; Palomeque, T.; Lorite, P. Celiac disease and other autoimmune disorders. In Autoimmunity-Pathogenesis, Clinical Aspects and Therapy of Specific Autoimmune Diseases; Chatzidionysiou, K., Ed.; Intech: Rijeka, Croatia, 2015; pp. 131–151. [Google Scholar] [CrossRef]
- Fasano, A.; Catassi, C. Clinical practice. Celiac disease. N. Engl. J. Med. 2012, 367, 2419–2426. [Google Scholar] [CrossRef] [PubMed]
- Sollid, L.M. Molecular basis of celiac disease. Annu. Rev. Immunol. 2000, 18, 53–81. [Google Scholar] [CrossRef] [PubMed]
- Alaedini, A.; Green, P.H. Autoantibodies in celiac disease. Autoimmunity 2008, 41, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Kagnoff, M.F. Celiac disease: Pathogenesis of a model immunogenetic disease. J. Clin. Investig. 2007, 117, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Abadie, V.; Sollid, L.M.; Barreiro, L.B.; Jabri, B. Integration of genetic and immunological insights into a model of celiac disease pathogenesis. Annu. Rev. Immunol. 2011, 29, 493–525. [Google Scholar] [CrossRef] [PubMed]
- Di Sabatino, A.; Vanoli, A.; Giuffrida, P.; Luinetti, O.; Solcia, E.; Corazza, G.R. The function of tissue transglutaminase in celiac disease. Autoimmun. Rev. 2012, 11, 746–753. [Google Scholar] [CrossRef]
- Lindfors, K.; Mäki, M.; Kaukinen, K. Transglutaminase 2-targeted autoantibodies in celiac disease: Pathogenetic players in addition to diagnostic tools? Autoimmun. Rev. 2010, 9, 744–749. [Google Scholar] [CrossRef]
- Fleckenstein, B.; Molberg, Ø.; Qiao, S.W.; Schmid, D.G.; Von der Mülbe, F.; Elgstøen, K.; Jung, G.; Sollid, L.M. Gliadin T cell epitope selection by tissue transglutaminase in celiac disease. Role of enzyme specificity and pH influence on the transamidation versus deamidation process. J. Biol. Chem. 2002, 277, 34109–34116. [Google Scholar] [CrossRef]
- Granito, A.; Tovoli, F.; Raiteri, A.; Volta, U. Anti-ganglioside antibodies and celiac disease. Allergy Asthma Clin. Immunol. 2021, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Granito, A.; Muratori, P.; Cassani, F.; Pappas, G.; Muratori, L.; Agostinelli, D.; Veronesi, L.; Bortolotti, R.; Petrolini, N.; Bianchi, F.B.; et al. Anti-actin IgA antibodies in severe coeliac disease. Clin. Exp. Immunol. 2004, 137, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Arentz-Hansen, H.; Körner, R.; Molberg, O.; Quarsten, H.; Vader, W.; Kooy, Y.M.; Lundin, K.E.; Koning, F.; Roepstorff, P.; Sollid, L.M.; et al. The intestinal T cell response to alpha-gliadin in adult celiac disease is focused on a single deamidated glutamine targeted by tissue transglutaminase. J. Exp. Med. 2000, 191, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Bodd, M.; Kim, C.Y.; Lundin, K.E.; Sollid, L.M. T-cell response to gluten in patients with HLA-DQ2.2 reveals requirement of peptide-MHC stability in celiac disease. Gastroenterology 2012, 142, 552–561. [Google Scholar] [CrossRef]
- Lundin, K.E.; Scott, H.; Hansen, T.; Paulsen, G.; Halstensen, T.S.; Fausa, O.; Thorsby, E.; Sollid, L.M. Gliadin-specific, HLA-DQ (alpha 1*0501, beta 1*0201) restricted T cells isolated from the small intestinal mucosa of celiac disease patients. J. Exp. Med. 1993, 178, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Lindfors, K.; Ciacci, C.; Kurppa, K.; Lundin, K.E.A.; Makharia, G.K.; Mearin, M.L.; Murray, J.A.; Verdu, E.F.; Kaukinen, K. Coeliac disease. Nat. Rev. Dis. Primers 2019, 5, 3. [Google Scholar] [CrossRef]
- Megiorni, F.; Pizzuti, A. HLA-DQA1 and HLA-DQB1 in Celiac disease predisposition: Practical implications of the HLA molecular typing. J. Biomed. Sci. 2012, 19, 88–94. [Google Scholar] [CrossRef]
- Fallang, L.E.; Bergseng, E.; Hotta, K.; Berg-Larsen, A.; Kim, C.Y.; Sollid, L.M. Differences in the risk of celiac disease associated with HLA-DQ2.5 or HLA-DQ2.2 are related to sustained gluten antigen presentation. Nat. Immunol. 2009, 10, 1096–1101. [Google Scholar] [CrossRef]
- Kumar, V.; Wijmenga, C.; Withoff, S. From genome-wide association studies to disease mechanisms: Celiac disease as a model for autoimmune diseases. Semin. Immunopathol. 2012, 34, 567–580. [Google Scholar] [CrossRef]
- Zhernakova, A.; Stahl, E.A.; Trynka, G.; Raychaudhuri, S.; Festen, E.A.; Franke, L.; Westra, H.J.; Fehrmann, R.S.; Kurreeman, F.A.; Thomson, B.; et al. Meta-analysis of genome-wide association studies in celiac disease and rheumatoid arthritis identifies fourteen non-HLA shared loci. PLoS Genet. 2011, 7, e1002004. [Google Scholar] [CrossRef]
- Hunt, K.A.; Zhernakova, A.; Turner, G.; Heap, G.A.; Franke, L.; Bruinenberg, M.; Romanos, J.; Dinesen, L.C.; Ryan, A.W.; Panesar, D.; et al. Newly identified genetic risk variants for celiac disease related to the immune response. Nat. Genet. 2008, 40, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Ponce de León, C.; Lorite, P.; López-Casado, M.Á.; Barro, F.; Palomeque, T.; Torres, M.I. Significance of PD1 Alternative Splicing in Celiac Disease as a Novel Source for Diagnostic and Therapeutic Target. Front. Immunol. 2021, 12, 678400. [Google Scholar] [CrossRef] [PubMed]
- Ponce de León, C.; López-Casado, M.A.; Lorite, P.; Palomeque, T.; Torres, M.I. Dysregulation of the PD-1/PD-L1 pathway contributes to the pathogenesis of celiac disease. Cell. Mol. Immunol. 2019, 16, 777–779. [Google Scholar] [CrossRef]
- Torres, M.I.; López-Casado, M.A.; Lorite, P.; Ríos, A. Tryptophan metabolism and indoleamine 2,3-dioxygenase expression in coeliac disease. Clin. Exp. Immunol. 2007, 148, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Gorczynski, R.M. CD200 and its receptors as targets for immunoregulation. Curr. Opin. Investig. Drugs. 2005, 65, 483–488. [Google Scholar]
- Chen, E.Y.; Chu, S.; Gov, L.; Kim, Y.K.; Lodoen, M.B.; Tenner, A.J.; Liu, W.F. CD200 modulates macrophage cytokine secretion and phagocytosis in response to poly(lactic co-glycolic acid) microparticles and films. J. Mater. Chem. B 2017, 5, 1574–1584. [Google Scholar] [CrossRef]
- Kotwica-Mojzych, K.; Jodłowska-Jędrych, B.; Mojzych, M. CD200:CD200R Interactions and Their Importance in Immunoregulation. Int. J. Mol. Sci. 2021, 5, 1602. [Google Scholar] [CrossRef]
- Koning, N.; van Eijk, M.; Pouwels, W.; Brouwer, M.S.; Voehringer, D.; Huitinga, I.; Hoek, R.M.; Raes, G.; Hamann, J. Expression of the inhibitory CD200 receptor is associated with alternative macrophage activation. J. Innat. Immunol. 2010, 2, 195–200. [Google Scholar] [CrossRef]
- Hatherley, D.; Barclay, A.N. The CD200 and CD200 receptor cell surface proteins interact through their N-terminal immunoglobulin-like domains. Eur. J. Immunol. 2004, 34, 1688–1694. [Google Scholar] [CrossRef]
- Deraison, C.; Bonnart, C.; Langella, P.; Roget, K.; Vergnolle, N. Elafin and its precursor trappin-2: What is their therapeutic potential for intestinal diseases? Br. J. Pharmacol. 2023, 180, 144–160. [Google Scholar] [CrossRef]
- Shaw, L.; Wiedow, O. Therapeutic potential of human elafin. Biochem. Soc. Trans. 2011, 39, 1450–1454. [Google Scholar] [CrossRef] [PubMed]
- Galipeau, H.J.; Wiepjes, M.; Motta, J.P.; Schulz, J.D.; Jury, J.; Natividad, J.M.; Pinto-Sanchez, I.; Sinclair, D.; Rousset, P.; Martin-Rosique, R.; et al. Novel role of the serine protease inhibitor elafin in gluten-related disorders. Am. J. Gastroenterol. 2014, 109, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Marsh, M.N. Gluten, major histocompatibility complex, and the small intestine: A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology 1992, 102, 330–354. [Google Scholar] [CrossRef] [PubMed]
- Torres, M.I.; López Casado, M.A.; Palomeque, T.; Lorite, P. Immune Checkpoints as a Novel Source for Diagnostic and Therapeutic Target in Celiac Disease. In Celiac Disease; IntechOpen: Rijeka, Croatia, 2021; pp. 1–17. [Google Scholar] [CrossRef]
- Chen, D.X.; He, H.; Gorczynski, R.M. Synthetic peptides from the N terminal regions of CD200 and CD200R1 modulate immunosuppressive and anti-inflammatory effects of CD200-CD200R1 interaction. Int. Immunol. 2005, 17, 289–296. [Google Scholar] [CrossRef]
- Molaaghaee-Rouzbahani, S.; Asri, N.; Jahani-Sherafat, S.; Amani, D.; Masotti, A.; Baghaei, K.; Yadegar, A.; Mirjalali, H.; Rostami-Nejad, M. The modulation of macrophage subsets in celiac disease pathogenesis. Immun. Inflamm. Dis. 2022, 10, e741. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.M.; Fasano, A.; Mann, D.L. Monocytes differentiated with IL-15 support Th17 and Th1 responses to wheat gliadin: Implications for celiac disease. Clin. Immunol. 2010, 135, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Schutyser, E.; Richmond, A.; Van Damme, J. Involvement of CC chemokine ligand 18 (CCL18) in normal and pathological processes. J. Leukoc. Biol. 2005, 78, 14–26. [Google Scholar] [CrossRef]
- Serena, G.; Huynh, D.; Lima, R.S.; Vise, L.M.; Freire, R.; Ingano, L.; Leonard, M.M.; Senger, S.; Fasano, A. Intestinal Epithelium Modulates Macrophage Response to Gliadin in Celiac Disease. Front. Nutr. 2019, 5, 167–173. [Google Scholar] [CrossRef]
- Lubberts, E. The IL-23-IL-17 axis in inflammatory arthritis. Nat. Rev. Rheumatol. 2015, 11, 415–429. [Google Scholar] [CrossRef]
- Sarra, M.; Pallone, F.; Macdonald, T.T.; Monteleone, G. IL-23/IL-17 axis in IBD. Inflamm. Bowel. Dis. 2010, 16, 1808–1813. [Google Scholar] [CrossRef]
- Guyot, N.; Zani, M.L.; Maurel, M.C.; Dallet-Choisy, S.; Moreau, T. Elafin and its precursor trappin-2 still inhibit neutrophil serine proteinases when they are covalently bound to extracellular matrix proteins by tissue transglutaminase. Biochemistry 2005, 44, 15610–15618. [Google Scholar] [CrossRef] [PubMed]
- Ren, P.; Lu, L.; Cai, S.; Chen, J.; Lin, W.; Han, F. Alternative Splicing: A New Cause and Potential Therapeutic Target in Autoimmune Disease. Front. Immunol. 2021, 12, 713540. [Google Scholar] [CrossRef] [PubMed]
- Solé, X.; Guinó, E.; Valls, J.; Iniesta, R.; Moreno, V. SNPStats: A web tool for the analysis of association studies. Bioinformatics 2006, 22, 1928–1929. [Google Scholar] [CrossRef] [PubMed]



| rs1733103 | ||
| Genotypes | Control % (n) | Celiac % (n) |
| C/C | 74% (28) | 48% (28) |
| C/T | 18% (7) | 47% (26) |
| T/T | 8% (3) | 7% (4) |
| Alleles | Control | Celiac |
| C | 83% (63) | 71% (82) |
| T | 17% (13) | 29% (34) |
| rs41282752 | ||
| Genotypes | Control % (n) | Celiac % (n) |
| G/G | 92% (35) | 98% (57) |
| G/A | 8% (3) | 2% (1) |
| G/G | 0 | 0 |
| Alleles | Control | Celiac |
| G | 96% (73) | 99% (115) |
| A | 4% (3) | 1% (1) |
| rs41282752 | ||
| Genotypes | Control % (n) | Celiac % (n) |
| A/A | 63% (24) | 48% (28) |
| A/C | 29% (11) | 45% (26) |
| C/C | 8% (3) | 7% (4) |
| Alleles | Control | Celiac |
| A | 78% (59) | 71% (82) |
| C | 22% (17) | 29% (34) |
| rs17333103 | ||||||
| Model | Genotype | Control n (%) | Cases n (%) | OR (IC 95%) | p Value | AIC |
| Codominant | C/C | 28 (73.7%) | 28 (48.3%) | 1.00 | 0.022 | 127.3 |
| C/T | 7 (18.4%) | 26 (44.8%) | 3.71 (1.39–9.95) | |||
| T/T | 3 (7.9%) | 4 (6.9%) | 1.33 (0.27–6.51) | |||
| Dominant | C/C | 28 (73.7%) | 28 (48.3%) | 1.00 | 0.012 | 126.6 |
| C/T + T/T | 10 (26.2%) | 30 (51.7%) | 3.00 (1.24–7.28) | |||
| Recessive | C/C + C/T | 35 (92.1%) | 54 (93.1%) | 1.00 | 0.85 | 132.9 |
| T/T | 3 (7.9%) | 4 (6.9%) | 0.86 (0.18–4.10) | |||
| Overdominant | C/C + T/T | 31 (81.6%) | 32 (55.2%) | 1.00 | 0.0063 | 125.4 |
| T/T | 7 (18.4%) | 26 (44.8%) | 3.60 (1.36–9.49) | |||
| Log-Additive | 1.94 (0.95–3.97) | 0.057 | 129.3 | |||
| rs41282752 | ||||||
| Model | Genotype | Control n (%) | Cases n (%) | OR (IC 95%) | p Value | AIC |
| G/G | 35 (92.1%) | 57 (98.3%) | 1.00 | 0.14 | 130.7 | |
| G/G | 3 (7.9%) | 1 (1.7%) | 0.20 (0.02–2.05) | |||
| rs2664581 | ||||||
| Model | Genotype | Control n (%) | Cases n (%) | OR (IC 95%) | p Value | AIC |
| Codominant | A/A | 24 (63.2%) | 28 (48.3%) | 1.00 | 0.28 | 132.4 |
| C/A | 11 (28.9%) | 26 (44.8%) | 2.03 (0.83–4.94) | |||
| C/C | 3 (7.9%) | 4 (6.9%) | 1.14 (0.23–5.62) | |||
| Dominant | AA | 24 (63.2%) | 28 (48.3%) | 1.00 | 0.15 | 130.8 |
| C/A + A/A | 14 (36.8%) | 30 (51.7%) | 1.84 (0.80–4.24) | |||
| Recessive | A/A + C/A | 35 (92.1%) | 54 (93.1%) | 1.00 | 0.85 | 132.9 |
| C/C | 3 (7.9%) | 4 (6.9%) | 0.86 (0.18–4.10) | |||
| Overdominant | A/A + C/C | 27 (71%) | 32 (55.2%) | 1.00 | 0.11 | 130.4 |
| C/A | 11 (28.9%) | 26 (44.8) | 1.99 (0.83–4.77) | |||
| Log-Additive | 1.44 (0.73–2.82) | 0.29 | 131.7 | |||
| Region | Primer Code | Sequence | PCR Product (bp) | SNP | Restriction Endonuclease |
|---|---|---|---|---|---|
| Exon 1 | PI3-119-F | CCCAGGTCCCTCCCAGAA | 870 | rs1733103 | BtsCI |
| PI3-969-R | CCTTCCTCCACTCCAAGTCT | rs41282752 | BsrI | ||
| Exon 2 | PI3-1080-F | CTTCCCTACTCAGGCCATGG | 463 | rs2664581 | HpyCH4III |
| PI3-1523-R | CGCTCAGCCTTCTTTTGTGT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ponce-de-León, C.; Lorite, P.; López-Casado, M.Á.; Mora, P.; Palomeque, T.; Torres, M.I. Expression of Elafin and CD200 as Immune Checkpoint Molecules Involved in Celiac Disease. Int. J. Mol. Sci. 2024, 25, 852. https://doi.org/10.3390/ijms25020852
Ponce-de-León C, Lorite P, López-Casado MÁ, Mora P, Palomeque T, Torres MI. Expression of Elafin and CD200 as Immune Checkpoint Molecules Involved in Celiac Disease. International Journal of Molecular Sciences. 2024; 25(2):852. https://doi.org/10.3390/ijms25020852
Chicago/Turabian StylePonce-de-León, Candelaria, Pedro Lorite, Miguel Ángel López-Casado, Pablo Mora, Teresa Palomeque, and María Isabel Torres. 2024. "Expression of Elafin and CD200 as Immune Checkpoint Molecules Involved in Celiac Disease" International Journal of Molecular Sciences 25, no. 2: 852. https://doi.org/10.3390/ijms25020852
APA StylePonce-de-León, C., Lorite, P., López-Casado, M. Á., Mora, P., Palomeque, T., & Torres, M. I. (2024). Expression of Elafin and CD200 as Immune Checkpoint Molecules Involved in Celiac Disease. International Journal of Molecular Sciences, 25(2), 852. https://doi.org/10.3390/ijms25020852






