Abstract
Articular cartilage (AC) defects are frequent but hard to manage. Osteoarthritis (OA) is a musculoskeletal illness that afflicts between 250 and 500 million people in the world. Even though traditional OA drugs can partly alleviate pain, these drugs cannot entirely cure OA. Since cartilaginous tissue of the joints has a poor self-repair capacity and very poor proliferative ability, the healing of injured cartilaginous tissue of the joint has not been accomplished so far. Consequently, the discovery of efficacious mediations and regenerative treatments for OA is needed. This manuscript reviews the basic concepts and the recent developments on the molecular mechanisms of cartilage repair and their potential clinical applications. For this purpose, a literature exploration was carried out in PubMed for the years 2020, 2021, and 2022. On 31 October 2022 and using “cartilage repair molecular mechanisms” as keywords, 41 articles were found in 2020, 42 in 2021, and 36 in 2022. Of the total of 119 articles, 80 were excluded as they were not directly related to the title of this manuscript. Of particular note are the advances concerning the mechanisms of action of hyaluronic acid, mesenchymal stem cells (MSCs), nanotechnology, enhancer of zeste 2 polycomb repressive complex 2 subunit (EHZ2), hesperetin, high mobility group box 2 (HMGB2), α2-macroglobulin (α2M), proteoglycan 4 (Prg4)/lubricin, and peptides related to cartilage repair and treatment of OA. Despite the progress made, current science has not yet achieved a definitive solution for healing AC lesions or repairing cartilage in the case of OA. Therefore, further research into the molecular mechanisms of AC damage is needed in the coming decades.
1. Introduction
Articular cartilage (AC) is a compact extracellular matrix (ECM)-rich tissue that degenerates due to continuing mechanical stress, leading to osteoarthritis (OA). The tissue has poor intrinsic repair capacity particularly in elderly and osteoarthritic articulations. OA is the most frequent musculoskeletal illness, impacting between 250 and 500 million people in the world [1,2].
AC is an avascular tissue. Consequently, diffusivity is an essential carrier instrument for nutrients and other molecular signals controlling its cell metabolism and preservation of the ECM. Comprehending how solutes distribute into joint cartilaginous tissue is paramount to clarifying its disorders, and to creating approaches for repair and reparation of its ECM [3].
Cells in AC are zonal organized. Cells in the external area of AC are usually little in size and proliferative. Stimulation with adequate negative pressure is advantageous to cell endurance and tissue repair [4]. AC defects are frequent in the clinic but hard to manage [5]. AC degradation has been identified as the principal abnormal finding in OA. The processes that control the change from normal cartilage to cartilage with OA endure undefined [6]. OA is the most frequent chronic and degenerative articular illness. Even though traditional OA drugs can partly alleviate pain, these drugs cannot entirely cure OA [7]. OA is the most frequent articular illness, lacking illness-modifying therapies [8].
The ECM of AC is a system with three dimensions (3D) principally composed of entangled fibrils of collagen and aggregates of interfibrillar aggrecan. Throughout the appearance of OA, the ECM is put through a compound of chemical and structural modifications that are essential in the start and the advancement of the illness. Although the molecular processes implicated in the pathological remodeling of the ECM are deemed as critical, they remain, nevertheless, not entirely clarified [9].
Due to the fast aging of the world population, the amount of people with articular illness continues to rise. Consequently, a great number of subjects need adequate management for OA. Additionally, OA can substantially affect the subject’s quality of life (QoL) due to knee joint discomfort, muscle weakness in the lower limbs, or ambulatory problems. Due to the fact that AC has a poor self-repair capacity and a very poor low proliferative ability, healing of injured AC has not been accomplished so far. Contemporary pharmacological management of OA is restricted to the negligible relief of pain (e.g., intra-articular injection of hyaluronic acid or nonsteroidal anti-inflammatory medications); therefore, the discovery of efficacious medications and regenerative treatments for OA is greatly required [10].
The risk circumstances for the appearance of OA and the contemporary pharmacological and nonpharmacological approaches for its management are shown in Figure 1 [11].
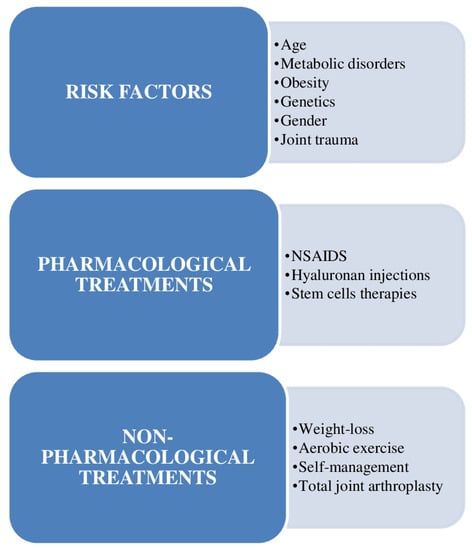
Figure 1.
Outline of the risk circumstances for the appearance of osteoarthritis (OA) and the contemporary pharmacological and nonpharmacological approaches for its management, emphasizing the scarcity of efficacious methods and the chance for invention in this field. NSAIDS = nonsteroidal anti-inflammatory drugs.
The repair of AC defects is still defying orthopedic surgery due to the avascular configuration of AC and the restricted regenerative ability of adult chondrocytes [12].
For this purpose, a literature exploration was carried out in PubMed for the years 2020, 2021, and 2022. On 31 October 2022 and using “cartilage repair molecular mechanisms” as keywords, 41 articles were found in 2020, 42 in 2021, and 36 in 2022. Of the total of 119 articles, 80 were excluded as they were not directly connected to the title of this manuscript. Therefore, 39 articles were finally analyzed, the results of which are presented below.
2. Basic Concepts
AC has a restricted ability for repair. The first try to repair cartilaginous tissue utilizing tissue engineering was published in 1977. Since then, cell-based procedures have been used in orthopedic surgery [13]. There are a number of elements implicated in cellular treatment and tissue engineering for the repair of cartilaginous tissue. Treatments for the repair of cartilaginous tissue need any compound of cells, biomaterials, mechanical loading, and/or bioactive effectors (Figure 2) [13].
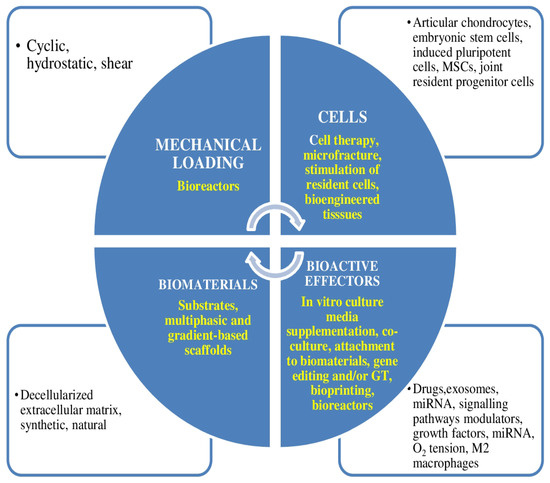
Figure 2.
Elements implicated in cellular therapy and tissue engineering for the repair of cartilaginous tissue. Therapies for cartilage repair need any compound of cells, biomaterials, mechanical loading, and/or bioactive effectors. In yellow, the four main ways in which they can be used for cartilage tissue engineering are shown. MSCs = mesenchymal stem cells.
Figure 3 shows a schematic summary of approaches for the repair of cartilaginous tissue [13]. All aforementioned treatments can be improved with bioactive effectors or mechanical loading.
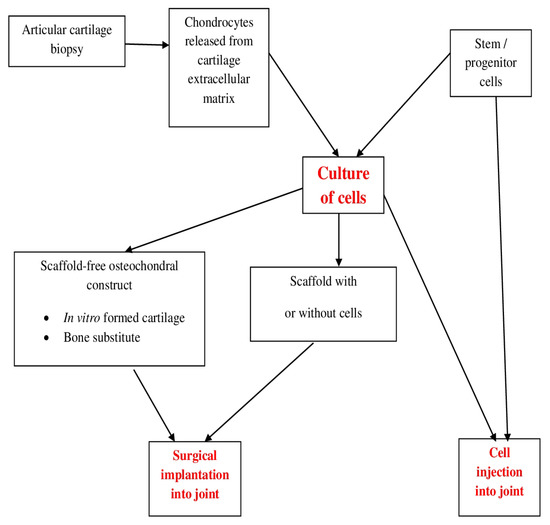
Figure 3.
Outline of approaches for the repair of cartilaginous tissue. All methods exhibited can be improved with bioactive effectors or mechanical loading.
Figure 4 shows the main emergent therapeutic goals in OA. Pathological goals mainly gather into those facilitating repair, those neutralizing pain, and those constraining tissue swelling. There is a mutual association between inflammatory and repair processes in the OA articulation, both of which impact pain [14].
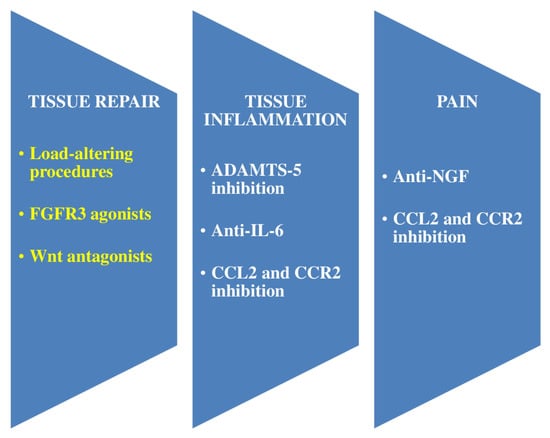
Figure 4.
Main emergent therapeutic objectives in osteoarthritis (OA) are shown. Pathological objectives mainly gather into those facilitating repair, those neutralizing pain, and those preventing tissue inflammation (resulting in turn in degeneration). There is a mutual correlation between inflammatory and repair processes in the OA articulation, both of which impact pain. Objectives that demonstrate effectiveness in murine experiments and for which therapeutic approaches are being studied in clinical trials are shown. White color indicates promotion, and yellow color represents suppression. Peripheral pain emerges from joint pathology and may prevent tissue swelling and facilitate tissue repair by suppressing mechanical overload of the articulation. FGFR = fibroblast growth factor receptor. IL = interleukin. ADAMTS = a disintegrin and metalloproteinase with thrombospondin motif. CCL = C-C motif chemokine. CCR = C-C chemokine receptor. NGF = nerve growth factor.
Figure 5 shows an outline of nanotechnology-based uses in osteoarthritis (OA) diagnostics and treatment [11].
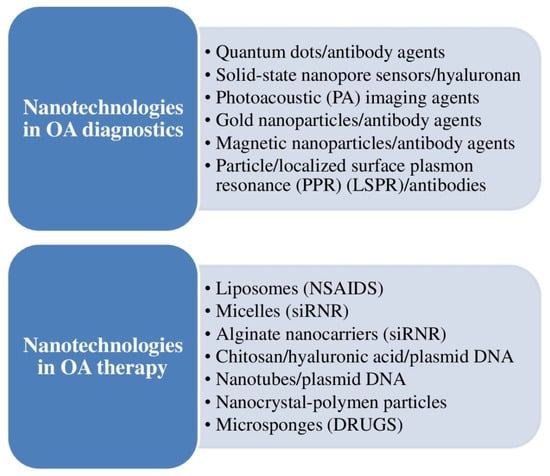
Figure 5.
Outline of nanotechnology-based uses in the diagnosis and treatment of osteoarthritis (OA).
3. Recent Developments
3.1. Hyaluronic Acid
In a murine study, Luo et al. discovered that intra-articular injections of hyaluronic acid facilitated the chondrogenic differentiation of human amniotic mesenchymal stem cells (hAMSCs). In other words, hyaluronic acid notably improved the expression of chondrocyte-specific markers including collagen type 2 alpha 1 (Col2α1), acan, and SRY-box transcription factor 9 (Sox9) in hAMSCs, with intense synergistic impact on chondrogenic differentiation, together with the frequently utilized inducer, transforming growth factor β3 (TGF-β3). Hyaluronic acid turns on the RASL11B gene to stimulate the chondrogenic differentiation of hAMSCs via the activation of Sox9 and extracellular signal-regulated protein kinase (ERK)/Smad signaling, therefore rendering an approach for the repair of cartilaginous defects by hyaluronic acid-based stem cell treatment [15]. Galla et al. published a new form of hyaluronic acid that seemed to be well-absorbed and disseminated to chondrocytes, maintaining their biological functions. Hence, the oral administration of GreenIuronic® (Vivatis Pharma GBHE, Grüner Deich 1-3, Hamburg, Germany) in humans can be deemed a sound approach to attain an advantageous therapeutic impact on OA [16].
3.2. Mesenchymal Stem Cells (MSCs)
Intra-articular injections of MSCs have been examined as a possible treatment for the management of knee OA, with some proof of accomplishment in initial human trials. Salerno et al. showed that ample in vitro aging of bone marrow-derived human MSCs causes a decline of chondrogenesis but no decrease in trophic repair. By combining transcriptomic and proteomic information utilizing Ingenuity pathway analysis, Salerno et al. discovered that diminished chondrogenesis with passage is connected to downregulation of the forkhead transcription factor M1 (FOXM1) signaling pathway while preservation of trophic repair is connected to C-X-C motif chemokine ligand 12 (CXCL12). In a try at creating functional markers of MSC power, Salerno et al. recognized the decline of messenger ribonucleic acid (mRNA) expression for metalloproteinase 13 (MMP13) was connected with the decline of chondrogenic power of MSCs and the endured release of elevated amounts of TIMP metallopeptidase inhibitor 1 (TIMP1) protein was connected with the preservation of trophic repair ability. Salerno et al. reckoned that early passage MMP13+, TIMP1-secretinghigh MSCs should be utilized for autologous OA treatments devised to perform through engraftment and chondrogenesis, while later passage MMP13−, TIMP1-secretinghigh MSCs could be used for allogeneic OA treatment devised to perform through trophic repair [17].
Zhang et al. observed that miR-199b-5p overexpression restrained the growth of C3H10T1/2 cells but facilitated transforming growth factor-β3 (TGF-β3)-induced C3H10T1/2 cells of chondrogenic differentiation. The findings of this study might render a new perception on miRNA-mediated MSC treatment for cartilage-related conditions [18].
Casari et al. stated that adipose tissue (AT) has turned into a fountain of MSCs for regenerative medicine employments, particularly skeletal diseases. They compared AT processed by centrifugation (C-AT) with microfragmentation (MF-AT). Bringing into sharp focus MF-AT, Casari et al. afterward evaluated the effect of synovial fluid (SF) alone on both MF-AT and isolated AT-MSC to better comprehend their cartilage repair processes. The findings of this study showed that MF has a positive impact on the preservation of AT histology and might activate the expression of trophic factors that ameliorate tissue repair by processed AT [19].
According to Ren et al., the stemness and differentiation traits of bone marrow mesenchymal stem cells (BMSCs) in three-dimensional (3D) culture are very important for stem cell treatment and engineering repair of cartilaginous tissue [20].
Yan X et al. showed that MSC treatment using a deoxyribonucleic acid (DNA) supramolecular hydrogel facilitated the creation of quality cartilage, diminished bone spurs, and normalized subchondral osseous tissue under the elevated friction condition of OA [2].
A study from Yan B et al. established the anti-OA effectiveness, safety, and a paracrine-based mechanism of adipose-derived stem cells (ADSCs), rendering an encouraging cell-based treatment alternative for OA management [8].
Norouzi-Barough et al. reported the therapeutic possibility of MSC-derived exosomes as a cell-free therapy method for the management of cartilage defects [21].
Feng et al. reported that 3N-cadherin can eventually facilitate chondrogenic differentiation of BMSCs by restraining the Wnt signaling pathway. They compared and examined the impact of N-cadherin on chondrogenic differentiation of BMSCs to analyze the related mechanism, so as to render a theoretical basis for the clinical treatment (repair and regeneration) of AC injuries [22].
According to Zhang et al., induced pluripotent stem cells (iPSCs) are a limitless fountain for cartilage regeneration as they can produce a broad range of cell types. They encountered that in chondrogenic induction medium, shaking culture alone substantially upregulated the chondrogenic markers SOX9, Col2a1, and aggrecan in iPSCs-Tet/BMP-4 by day 21. The culture system reported by Zhang et al. could be a valuable implement for further research of the mechanism of BMP-4 in controlling iPSC differentiation toward the chondrogenic lineage and should ease investigation in cartilage development, repair, and OA [23].
3.3. Mechanisms of Diffusion in Articular Cartilage (AC)
Travascio et al. observed that diffusivity was impacted by molecular size, with the extent of the diffusion coefficients diminishing as the Stokes radius of the probe augmented. This report rendered new data on the mechanisms of diffusion in AC. The results of this study can be exploited to further analyze OA and to plan therapies for the restoration or replacement of cartilaginous tissue [3].
3.4. Mechanisms of miRNA Control of the Transcriptome of Tissue-Engineered Cartilage in Reaction to IL-1β and TNF-α
In an in vitro murine-induced pluripotent stem cell (miPSC) experiment, Ross et al. demonstrated that delivery of miR-17-5p and miR-20a-5p imitates substantially diminished degradative enzyme activity levels while also reducing expression of swelling-related genes in cytokine-treated cells [24].
3.5. SIRT1 has an Essential Coordination Function in BMP2-Induced Chondrogenic Differentiation of Stem Cells and Cartilage Preservation under Oxidative Stress
Lu et al. affirmed that silent mating type information regulator 2 homolog-1 (SIRT1) is an essential histone deacetylase that controls proliferation, differentiation, aging, and swelling processes; moreover, it is a crucial factor for chondrogenesis. In their study, Lu et al. established the experimental basis for examining the utilization of SIRT1 in the repair of cartilage defects [5].
3.6. Nanotechnology for OA Clinical Management
Mohammadinejad et al. stated that nanotechnology can be beneficial for the diagnosis, follow-up, and treatment of OA (Figure 5). Nanotubes, magnetic nanoparticles, and other nanotechnology-based medication and gene delivery systems may be utilized for aiming molecular pathways and pathogenic processes implicated in OA appearance [11]. According to Li et al., bioactive extracellular vesicle (EV)-based nanotherapeutics have revealed new views for clinicians, making feasible strong instruments and therapies for regenerative medicine (cartilage repair and regeneration) [25].
3.7. Ezh2 Ameliorates Osteoarthritis (OA) by Triggering TNFSF13B
Du et al. examined the expression of EZH2 (enhancer of zeste 2 polycomb repressive complex 2 subunit), an H3K27me3 (histone H3 lysine 27 trimethylation) transferase, in human OA cartilages and its regulations in controlling OA pathogenesis. The results of this study revealed that an EZH2-positive subpopulation existed in OA subjects and that EZH2-TNFSF13B signaling was accountable for controlling chondrocyte healing and hypertrophy. Therefore, EZH2 may act as a new possible objective for the diagnosis and management of OA [26].
3.8. Hesperetin (HPT) Averts Cartilage Degradation
Wu et al. studied whether hesperetin (HPT) had chondroprotective impact against the tumor necrosis factor-α (TNF-α)-induced inflammatory reaction of chondrocytes and connected mechanisms and determined the effect of HPT on OA induced by anterior cruciate ligament transection (ACLT). The results of this study demonstrated that HPT has a substantial protective and anti-inflammatory impact on chondrocytes via the AMPK signaling pathway, efficaciously averting cartilage degeneration. Taking into account the diverse beneficial impacts of HPT, it can be utilized as a possible natural medication to manage OA [27].
3.9. Intrinsic Restoration Reaction in Cartilage, Mediated by Aggrecan-Dependent Sodium Flux
Keppie et al. reported an intrinsic reparation mechanism, regulated by matrix stiffness and mediated by the free sodium concentration, in which heparan sulfate-bound growth factors are liberated from cartilage following detrimental load. They recognized aggrecan as a depot for sequestered sodium, explicating why OA tissue loses its capacity to repair. Medications that re-establish matrix sodium to permit adequate liberation of growth factors following load were foreseen to facilitate intrinsic cartilage repair in OA [1].
3.10. Clock Knockdown Attenuated Reactive Oxygen Species-Mediated Senescence of Chondrocytes via Re-Establishing Autophagic Flux
Zhong et al. studied the possible function and mechanism of the circadian gene clock in OA pathology. They encountered that clock knockdown can attenuate ROS-mediated senescence of chondrocytes via re-establishing autophagic flux in noncircadian mode, rendering a possible therapeutic goal for OA [6].
3.11. HMGB2 Facilitates Chondrocyte Proliferation under Negative Pressure via the Phosphorylation of AKT
Liu et al. found that high-mobility group box 2 (HMGB2) exhibited an improvement effect on chondrocyte proliferation under negative pressure through the phosphorylation of AKT [4].
3.12. Regenerative Potential of OA Human Infrapatellar Fat Pad (IPFP)-Derived Progenitors Osteochondral Defects
In an animal experiment performed in femoral bones of mice, van Schaik et al. demonstrated viability in producing ex vivo osteochondral defects and showed the regenerative capacity of OA human IPFP-derived progenitors. Therefore, the rat model reported by van Schaik et al. could be utilized to investigate the impact of aging and OA on tissue regeneration and to examine molecular processes of cartilage repair utilizing genetically modified mice [28].
3.13. Function and Mechanism of Arginine–Glycine–Aspartic Acid (Arg–Gly–Asp, RGD) Peptide Family in Cartilage Tissue Engineering
According to Yang et al., given that the majority of the scaffold materials utilized in cartilage tissue engineering are biologically inactive, it is crucial to augment the cellular adhesion capacity throughout tissue engineering restoration. RGD polypeptide families were deemed as appropriate prospects for the management of a diversity of illnesses and for the regeneration of diverse tissues [29].
3.14. 3D Bioprinting Gradient-Structured Constructs for Anisotropic Cartilage Regeneration
Sun et al. created an anisotropic gradient-structured cartilage scaffold by 3D bioprinting, in which bone marrow stromal cell (BMSC)-laden anisotropic hydrogel micropatterns were utilized for heterogeneous chondrogenic differentiation and physically gradient synthetic poly (ε-caprolactone) (PCL) to give mechanical strength. The results of their study rendered a new prospect for the regeneration and repair of cartilaginous tissue [30].
3.15. LncRNA-CRNDE Regulates BMSC Chondrogenic Differentiation to Promote Cartilage Repair in Osteoarthritis through SIRT1/SOX9
Shi et al. observed that the long noncoding RNA (lncRNA)-colorectal neoplasia differentially expressed gene (CRNDE) controlled BMSC chondrogenic differentiation to facilitate the repair of cartilaginous tissue in OA via SIRT1/SOX9 [7].
3.16. Manipulation of Histone Signals to Control Chondrocyte Roles or Manage Injuries of the Cartilaginous Tissue
Wan et al. affirmed that the utilization of small molecules and medications can manipulate histone signals to control chondrocyte roles or manage cartilage injuries and OA [31].
3.17. The Function of Histone Deacetylase 4 (HDAC4)-Controlled Chondrocyte Hypertrophy in the Start and Appearance of Age-Related OA
Dong et al. reported that HDAC4 expression controls the beginning and appearance of age-related OA by regulating chondrocyte hypertrophy. Therefore, the findings of this study might aid in the early diagnosis and management of age-related OA [32].
3.18. The Impact of Osmolarity and FK506 (Tacrolimus, Fujimycin) on Calcineurin Action, Cell Expansion, Extracellular Matrix Quality, and BMP- and TGF-β (Transforming Growth Factor Beta) Signaling
Jahr et al. discovered that physiological osmolarity facilitated terminal chondrogenic differentiation of progenitor cells via the sensitization of the TGF-β superfamily signaling at the type I receptor. The findings of this study could be of help to future cell-based cartilage repair approaches [33].
3.19. Mechanism by which OA Is Started and Advances in the Cartilage Extracellular Matrix (ECM)
Jaabar et al. showed the likelihood of imitating the unevenness actions of chondrocytes by employing enzymatic digestions of healthy cartilage, by means of the compound action of hyaluronidase and collagenase. This produced damage completely similar to that seen in advanced OA. Targeting the homeostatic equilibrium of chondrocyte metabolism via the regulation of enzymatic responses implicated in catabolic processes could be a potential curative treatment of OA [9].
3.20. Proteoglycan 4 (Prg4)/Lubricin Functions in a Protective Manner against OA
Takahata et al. reported that proteoglycan 4 (Prg4)/lubricin, which is in a specific manner expressed in the external area of AC and the synovial membrane, protects against OA, and controls the transcriptional regulation of Prg4 in chondrocytes of AC [10].
3.21. Chondroinductive/Chondroconductive Peptides and Their Functionalized Biomaterials for Cartilage Tissue Engineering
According to Zhu et al., peptides that are derived from and imitate the roles of chondroconductive cartilage ECM and chondroinductive growth factors, constitute a distinctive category of bioactive drugs for chondrogenic functionalization. Taking into account that they can be chemically synthesized, peptides exhibit superior reproducibility, more stable effectiveness, better modifiability, and producing efficacy compared to naturally derived biomaterials and recombinant growth factors. Therefore, peptides can be utilized for cartilage tissue engineering [12].
3.22. Reversal of Tissue Degradation Detected with Joint Distraction
According to Jansen et al., the reversal of tissue degradation found with joint distraction could be due to one or a compound of diverse processes, including partial unloading, fluctuation of the pressure of the synovial fluid, mechanical and biochemical modifications in subchondral osseous tissue, adhesion and chondrogenic dedication of articulation-derived MSCs, or a modification in the molecular ambience of the articulation [34].
3.23. α2-Macroglobulin (α2M) Is Important to Chondral Protection in Post-traumatic OA
Zhao et al. showed that α2MRS injection substantially lowered the levels of inflammatory factors, ameliorated gait, and demonstrated substantially inferior degradation of cartilaginous tissue than the groups that did not experience α2M-rich serum (α2MRS) injections. This study emphasized the chondroprotective impact of α2MRS, clarified its possible utilizations against cartilage degradation, and could render a basis for the clinical translation of α2MRS [35].
3.24. The Potential Role of Nano-Antioxidants
It has been reported by Khezri et al. that curcumin nanoformulations have several pleiotropic pharmacological effects. That is why curcumin, a natural compound, can be used in the treatment of osteoarthritis. The impact of curcumin and its nanoformulations on the differentiation of MSCs has been shown. Additionally, osteogenic differentiation of MSCs in the scaffolds has been demonstrated [36].
3.25. The Possible Role of Mitochondria Targeting in Tissue Repairing
It has been reported by Chodari et al. that adequate mitochondrial biogenesis is required for efficacious cell function and homeostasis, which depends on the control of ATP production and preservation of mitochondrial DNA (mtDNA). These phenomena are essential in the mechanisms of inflammation and aging, among others. Polyphenols have been deemed as the principal components of plants, fruits, and natural extracts with demonstrated long lasting therapeutic impact. These components control the intracellular pathways of mitochondrial biogenesis. The impact of several natural polyphenol compounds from various plant kingdoms on regulating signaling pathways of mitochondrial biogenesis make them potential options for the management of OA and defects of AC [37].
A study suggested that intercellular transfer of healthy mitochondria to chondrocytes could represent a new, acellular approach to increase mitochondrial content and function in cartilage [38].
3.26. The Use of Infrapatellar Fat Pad-Derived Mesenchymal Stem Cells in Articular Cartilage Regeneration
According to Vehadi et al., the origin of MSCs is a relevant factor to be taken into account. The infrapatellar fat pad (IPFP) is a rich source of MSCs. Additionally, it has been demonstrated that these cells have many pros over other tissues in terms of ease of isolation, expansion, and chondrogenic differentiation. Therefore, it is why IPFP-derived MSCs are already being used in orthopedic surgery for the treatment of OA and other injuries of AC [39]. Table 1 summarizes the main data from the literature on molecular processes of cartilage repair and their potential clinical applications.

Table 1.
Main data from the literature on molecular processes of cartilage repair and their potential clinical applications.
4. Conclusions
Hyaluronic acid triggers the RASL11B gene to augment the chondrogenic differentiation of hAMSCs through the stimulation of Sox9 and ERK/Smad signaling, thus rendering a new approach for the repair of cartilage defects by hyaluronic acid-based stem cell therapy. ADSCs have shown to be anti-OA efficacious and safe, ADSCs-CM facilitated the rapid growth in the number of chondrocytes and substantially re-established the IL-1β-induced abnormal expressions of molecular markers IL-6, aggrecan, MMP3, MMP13, collagen II, collagen X, ADAMTS5, ADAMTS9, SOX6, and SOX9 in chondrocytes. Compared to MSCs, MSC-derived exosomes have many pros such as non-immunogenicity, easy access, easy storage, and great stability under different circumstances. Exosomes could be deemed as an alternate approach for cell-based treatment in regenerative medicine. The 3N-cadherin can facilitate chondrogenic differentiation of BMSCs by restraining the Wnt signaling pathway. Nanotechnology can be valuable for the diagnosis, follow-up, and treatment of OA. HPT has substantial protective and anti-inflammatory impact on chondrocytes via the AMPK signaling pathway, efficaciously averting cartilage degeneration. lncRNA-CRNDE controls BMSC chondrogenic differentiation to facilitate cartilage repair in OA via SIRT1/SOX9. HDAC4 expression controls the start and appearance of age-related OA by regulating chondrocyte hypertrophy. Prg4/lubricin functions in a protective mode against OA. It has been shown that α2-macroglobulin (α2M) protects against post-traumatic OA.
The suggestion of this article for future work is that we must continue to continuously and relentlessly investigate the intimate mechanisms of articular cartilage degeneration with aging in order to find therapeutic solutions to slow or prevent it. Additionally, efforts should be made to try to improve the healing capacity of chondrocytes with various therapeutic strategies, such as those discussed in this article.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author has no conflict of interest.
References
- Keppie, S.J.; Mansfield, J.C.; Tang, X.; Philp, C.J.; Graham, H.K.; Önnerfjord, P.; Wall, A.; McLean, C.; Winlove, C.P.; Sherratt, M.J.; et al. Matrix-bound growth factors are released upon cartilage compression by an aggrecan-dependent sodium flux that is lost in osteoarthritis. Function 2021, 2, zqab037. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Yang, B.; Chen, Y.; Song, Y.; Ye, J.; Pan, Y.; Zhou, B.; Wang, Y.; Mao, F.; Dong, Y.; et al. Anti-friction MSCs delivery system improves the therapy for severe osteoarthritis. Adv. Mater. 2021, 33, e2104758. [Google Scholar] [CrossRef] [PubMed]
- Travascio, F.; Valladares-Prieto, S.; Jackson, A.R. Effects of solute size and tissue composition on molecular and macromolecular diffusivity in human knee cartilage. Osteoarthr. Cartil. Open 2020, 2, 100087. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; He, F.; Zhou, P.; Xie, M.; Wang, H.; Yang, H.; Huo, W.; Zhang, M.; Yu, S.; Wang, M. HMGB2 promotes chondrocyte proliferation under negative pressure through the phosphorylation of AKT. Biochim. Biophys. Acta Mol. Cell Res. 2021, 1868, 119115. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhou, L.; Wang, L.; He, S.; Ren, H.; Zhou, N.; Hu, Z. The role of SIRT1 in BMP2-induced chondrogenic differentiation and cartilage maintenance under oxidative stress. Aging 2020, 12, 9000–9013. [Google Scholar] [CrossRef]
- Zhong, J.; Wang, B.; Wu, B.; Shang, J.; Jiang, N.; Cui, A.; Chen, Y.; Xu, X.; Lu, H. Clock knockdown attenuated reactive oxygen species-mediated senescence of chondrocytes through restoring autophagic flux. Life Sci. 2021, 269, 119036. [Google Scholar] [CrossRef]
- Shi, C.; Zheng, W.; Wang, J. lncRNA-CRNDE regulates BMSC chondrogenic differentiation and promotes cartilage repair in osteoarthritis through SIRT1/SOX9. Mol. Cell. Biochem. 2021, 476, 1881–1890. [Google Scholar] [CrossRef]
- Yan, B.; Lv, S.; Tong, P.; Yan, L.; Chen, Z.; Zhou, L.; Yuan, Q.; Guo, L.; Shan, L. Intra-articular injection of adipose-derived stem cells ameliorates pain and cartilage anabolism/catabolism in osteoarthritis: Preclinical and clinical evidences. Front. Pharmacol. 2022, 13, 854025. [Google Scholar] [CrossRef]
- Jaabar, I.L.; Cornette, P.; Miche, A.; Wanherdrick, K.; Dupres, V.; Ehkirch, F.P.; Cambon Binder, A.; Berenbaum, F.; Houard, X.; Landoulsi, J. Deciphering pathological remodelling of the human cartilage extracellular matrix in osteoarthritis at the supramolecular level. Nanoscale 2022, 14, 8691–8708. [Google Scholar] [CrossRef]
- Takahata, Y.; Hagino, H.; Kimura, A.; Urushizaki, M.; Yamamoto, S.; Wakamori, K.; Murakami, T.; Hata, K.; Nishimura, R. Regulatory mechanisms of Prg4 and Gdf5 expression in articular cartilage and functions in osteoarthritis. Int. J. Mol. Sci. 2022, 23, 4672. [Google Scholar] [CrossRef]
- Mohammadinejad, R.; Ashrafizadeh, M.; Pardakhty, A.; Uzieliene, I.; Denkovskij, J.; Bernotiene, E.; Janssen, L.; Lorite, G.S.; Saarakkala, S.; Mobasheri, A. Nanotechnological strategies for osteoarthritis diagnosis, monitoring, clinical management, and regenerative medicine: Recent advances and tuture opportunities. Curr. Rheumatol. Rep. 2020, 22, 12. [Google Scholar] [CrossRef]
- Zhu, M.; Zhong, W.; Cao, W.; Zhang, Q.; Wu, G. Chondroinductive/chondroconductive peptides and their-functionalized biomaterials for cartilage tissue engineering. Bioact. Mater. 2021, 9, 221–238. [Google Scholar] [CrossRef]
- Zelinka, A.; Roelofs, A.J.; Kandel, R.A.; De Bari, C. Cellular therapy and tissue engineering for cartilage repair. Osteoarthr. Cartil. 2022, 30, 1547–1560. [Google Scholar] [CrossRef] [PubMed]
- Vincent, T.L. Of mice and men: Converging on a common molecular understanding of osteoarthritis. Lancet Rheumatol. 2020, 2, e633–e645. [Google Scholar] [CrossRef]
- Luo, Y.; Wang, A.T.; Zhang, Q.F.; Liu, R.M.; Xiao, J.H. RASL11B gene enhances hyaluronic acid-mediated chondrogenic differentiation in human amniotic mesenchymal stem cells via the activation of Sox9/ERK/smad signals. Exp. Biol. Med. 2020, 245, 1708–1721. [Google Scholar] [CrossRef] [PubMed]
- Galla, R.; Ruga, S.; Aprile, S.; Ferrari, S.; Brovero, A.; Grosa, G.; Molinari, C.; Uberti, F. New hyaluronic acid from plant origin to improve joint protection-An in vitro atudy. Int. J. Mol. Sci. 2022, 23, 8114. [Google Scholar] [CrossRef]
- Salerno, A.; Brady, K.; Rikkers, M.; Li, C.; Caamaño-Gutierrez, E.; Falciani, F.; Blom, A.W.; Whitehouse, M.R.; Hollander, A.P. MMP13 and TIMP1 are functional markers for two different potential modes of action by mesenchymal stem/stromal cells when treating osteoarthritis. Stem Cells 2020, 38, 1438–1453. [Google Scholar] [CrossRef]
- Zhang, M.; Yuan, S.Z.; Sun, H.; Sun, L.; Zhou, D.; Yan, J. miR-199b-5p promoted chondrogenic differentiation of C3H10T1/2 cells by regulating JAG1. J. Tissue Eng. Regen. Med. 2020, 14, 1618–1629. [Google Scholar] [CrossRef]
- Casari, G.; Resca, E.; Giorgini, A.; Candini, O.; Petrachi, T.; Piccinno, M.S.; Foppiani, E.M.; Pacchioni, L.; Starnoni, M.; Pinelli, M.; et al. Microfragmented adipose tissue is associated with improved ex vivo performance linked to HOXB7 and b-FGF expression. Stem Cell Res. Ther. 2021, 12, 481. [Google Scholar] [CrossRef]
- Ren, Y.; Zhang, H.; Wang, Y.; Du, B.; Yang, J.; Liu, L.; Zhang, Q. Hyaluronic acid hydrogel with adjustable stiffness for mesenchymal stem cell 3D culture via related molecular mechanisms to maintain stemness and induce cartilage differentiation. ACS Appl. Bio Mater. 2021, 4, 2601–2613. [Google Scholar] [CrossRef]
- Norouzi-Barough, L.; Shirian, S.; Gorji, A.; Sadeghi, M. Therapeutic potential of mesenchymal stem cell-derived exosomes as a cell-free therapy approach for the treatment of skin, bone, and cartilage defects. Connect. Tissue Res. 2022, 63, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Xuezhen, S.; Haipeng, L.; Jingbin, Z.; Bangtuo, Y.; Chunbao, L.; Wei, Q.; Yujie, L.; Mingzhu, Z. Effect of N-cadherin on chondrogenic differentiation of bone marrow-derived mesenchymal stem cells through Wnt signaling pathway. Cell Mol. Biol. 2022, 67, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Niibe, K.; Kondo, T.; Limraksasin, P.; Okawa, H.; Miao, X.; Kamano, Y.; Yamada, M.; Jiang, X.; Egusa, H. Rapid and efficient generation of cartilage pellets from mouse induced pluripotent stem cells by transcriptional activation of BMP-4 with shaking culture. J. Tissue Eng. 2022, 13, 20417314221114616. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.K.; Coutinho de Almeida, R.; Ramos, Y.F.M.; Li, J.; Meulenbelt, I.; Guilak, F. The miRNA-mRNA interactome of murine induced pluripotent stem cell-derived chondrocytes in response to inflammatory cytokines. FASEB J. 2020, 34, 11546–11561. [Google Scholar] [CrossRef]
- Li, M.; Fang, F.; Sun, M.; Zhang, Y.; Hu, M.; Zhang, J. Extracellular vesicles as bioactive nanotherapeutics: An emerging paradigm for regenerative medicine. Theranostics 2022, 12, 4879–4903. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Chen, Y.; Zhang, Q.; Lin, J.; Yu, Y.; Pan, Z.; Sun, H.; Yuan, C.; Yu, D.; Wu, H.; et al. Ezh2 ameliorates osteoarthritis by activating TNFSF13B. J. Bone Miner. Res. 2020, 35, 956–965. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Qian, Y.; Chen, C.; Feng, F.; Pan, L.; Yang, L.; Wang, C. Hesperetin exhibits anti-inflammatory effects on chondrocytes via the AMPK pathway to attenuate anterior cruciate ligament transection-induced osteoarthritis. Front. Pharmacol. 2021, 12, 735087. [Google Scholar] [CrossRef]
- van Schaik, T.J.A.; Gaul, F.; Dorthé, E.W.; Lee, E.E.; Grogan, S.P.; D’Lima, D.D. Development of an ex vivo murine osteochondral repair model. Cartilage 2021, 12, 112–120. [Google Scholar] [CrossRef]
- Yang, M.; Zhang, Z.C.; Liu, Y.; Chen, Y.R.; Deng, R.H.; Zhang, Z.N.; Yu, J.K.; Yuan, F.Z. Function and mechanism of RGD in bone and cartilage tissue engineering. Front. Bioeng. Biotechnol. 2021, 9, 773636. [Google Scholar] [CrossRef]
- Sun, Y.; Wu, Q.; Zhang, Y.; Dai, K.; Wei, Y. 3D-bioprinted gradient-structured scaffold generates anisotropic cartilage with vascularization by pore-size-dependent activation of HIF1α/FAK signaling axis. Nanomedicine 2021, 37, 102426. [Google Scholar] [CrossRef]
- Wan, C.; Zhang, F.; Yao, H.; Li, H.; Tuan, R.S. Histone modifications and chondrocyte fate: Regulation and therapeutic implications. Front. Cell Dev. Biol. 2021, 9, 626708. [Google Scholar] [CrossRef] [PubMed]
- Dong, Z.; Ma, Z.; Yang, M.; Cong, L.; Zhao, R.; Cheng, L.; Sun, J.; Wang, Y.; Yang, R.; Wei, X.; et al. The level of histone deacetylase 4 is associated with aging cartilage degeneration and chondrocyte hypertrophy. J. Inflamm. Res. 2022, 15, 3547–3560. [Google Scholar] [CrossRef] [PubMed]
- Jahr, H.; van der Windt, A.E.; Timur, U.T.; Baart, E.B.; Lian, W.S.; Rolauffs, B.; Wang, F.S.; Pufe, T. Physosmotic induction of chondrogenic maturation is TGF-β dependent and enhanced by calcineurin inhibitor FK506. Int. J. Mol. Sci. 2022, 23, 5110. [Google Scholar] [CrossRef] [PubMed]
- Jansen, M.P.; Mastbergen, S.C. Joint distraction for osteoarthritis: Clinical evidence and molecular mechanisms. Nat. Rev. Rheumatol. 2022, 18, 35–46. [Google Scholar] [CrossRef]
- Zhao, R.; Wei, X.; Zhang, C.; Wu, H.; Xiang, C.; Li, H.; Duan, W.; Duan, Z.; Li, C.; Zhao, Y.; et al. α2-macroglobulin-rich serum as a master inhibitor of inflammatory factors attenuates cartilage degeneration in a mini pig model of osteoarthritis induced by "idealized" anterior cruciate ligament reconstruction. Front. Pharmacol. 2022, 13, 849102. [Google Scholar] [CrossRef]
- Khezri, K.; Dizaj, S.M.; Saadat, Y.R.; Sharifi, S.; Shahi, S.; Ahmadian, E.; Eftekhari, A.; Abdolahinia, E.D.; Lotfipour, F. Osteogenic differentiation of mesenchymal stem cells via curcumin-containing nanoscaffolds. Stem Cells Int. 2021, 2021, 1520052. [Google Scholar] [CrossRef]
- Chodari, L.; Aytemir, M.D.; Vahedi, P.; Alipour, M.; Vahed, S.Z.; Khatibi, S.M.H.; Ahmadian, E.; Ardalan, M.; Eftekhari, A. Targeting mitochondrial biogenesis with polyphenol compounds. Oxid. Med. Cell Longev. 2021, 2021, 4946711. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.A.; Fahey, M.J.; Pugliese, B.R.; Irwin, R.M.; Antonyak, M.A.; Delco, M.L. Human mesenchymal stromal cells release functional mitochondria in extracellular vesicles. Front. Bioen. Biotechnol. 2022, 10, 870193. [Google Scholar] [CrossRef] [PubMed]
- Vahedi, P.; Moghaddamshahabi, R.; Webster, T.J.; Koyuncu, A.C.C.; Ahmadian, E.; Khan, W.S.; Mohamed, A.J.; Eftekhari, A. The use of infrapatellar fat pad-derived mesenchymal stem cells in articular cartilage regeneration: A review. Int. J. Mol. Sci. 2021, 22, 9215. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).