Abstract
Adolescent idiopathic scoliosis (AIS) is a progressive deformity of the spine. Scoliotic curves progress until skeletal maturity leading, in rare cases, to a severe deformity. While the Cobb angle is a straightforward tool in initial curve magnitude measurement, assessing the risk of curve progression at the time of diagnosis may be more challenging. Epigenetic and genetic markers are potential prognostic tools to predict curve progression. The aim of this study is to review the available literature regarding the epigenetic and genetic factors associated with the risk of AIS curve progression. This review was carried out in accordance with Preferential Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. The search was carried out in January 2022. Only peer-reviewed articles were considered for inclusion. Forty studies were included; fifteen genes were reported as having SNPs with significant association with progressive AIS, but none showed sufficient power to sustain clinical applications. In contrast, nine studies reporting epigenetic modifications showed promising results in terms of reliable markers. Prognostic testing for AIS has the potential to significantly modify disease management. Most recent evidence suggests epigenetics as a more promising field for the identification of factors associated with AIS progression, offering a rationale for further investigation in this field.
1. Introduction
Adolescent Idiopathic Scoliosis (AIS) is a complex three-dimensional deformity of the spine, with a different grade of involvement of the frontal, sagittal, and axial planes [1]. It affects 2–3% of the adolescent population [2]; females are more often involved than males [3].
The diagnosis of scoliosis is based on patient clinical examination and radiographical evaluation [4]. After AIS is diagnosed, patients need different management (ranging from observation alone to orthotic treatment and surgical correction) according to curve magnitude at the time of diagnosis and curve progression potential.
Scoliotic curves progress until skeletal maturity, causing important aesthetic problems, such as humps, with psychological problems and loss of self-esteem, coronal, and/or sagittal imbalance and muscle fatigue [5]. In rare cases, the curve progression can lead to a severe deformity with the occurrence of a lung restrictive disease, a consequent increase in right atrial and ventricular pressure, alongside neurological impairment [6].
While the Cobb angle is a straightforward tool in initial curve magnitude measurement, assessing the risk of curve progression for each patient at the time of diagnosis may be more challenging.
At the same time, identifying predictors of curve progression is still fundamental to avoid erroneous clinical management depriving patients of adequate treatment or exposing others to unnecessary one. For this purpose, many clinical parameters are widely accepted as predictors of scoliosis progression: curve location, age at diagnosis (<12 years), pre-menarche status, low Tanner stage, and peak height velocity [4,7]. Moreover, some radiographic parameters are currently considered by clinicians, such as curve magnitude at the time of diagnosis (>25°), Risser stage (0–1), open triradiate cartilage, and demonstration of significant curve progression between serial radiographs [6,7]. Figure 1 represents the parameters related to scoliosis progression.
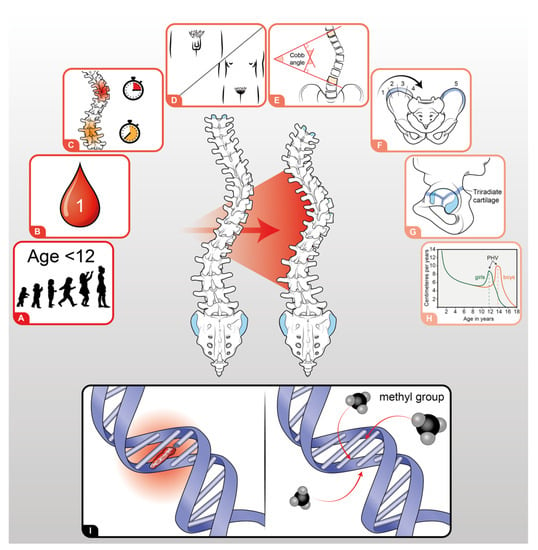
Figure 1.
Parameters related to AIS ordered following their impact on scoliosis progression: (A) Age < 12 years; (B) premenarche status; (C) localization of the main curve; (D) Tanner stage; (E) main curve Cobb angle at diagnosis; (F) Risser Stage; (G) status of triradiate cartilage; (H) high peak velocity; (I) genetic (left) and epigenetic (right) factors.
Epidemiological and genetic studies indicated AIS as a polygenic disease, and several studies investigated genetic and epigenetic factors associated with an increased risk of the onset of the scoliotic curve [8,9,10,11]. Several loci associated with AIS susceptibility were identified and evaluated in different ethnic groups, even if the value of AIS susceptibility in clinical practice is limited. Less information is available regarding candidate genetic and epigenetic factors related to scoliotic curve progression and its prediction, which would be a key tool for disease management.
Considering the significant socio-economic burden and psychological effects of a long-term follow-up and risk–benefit ratio of medical intervention, and that clinical features appear inadequate to predict disease evolution, the identification of reliable genetic factors associated with progression could be of crucial relevance in the clinical practice. Genetic and epigenetic markers are potential prognostic tools to predict progression and therefore helpful for personalized treatments and disease management.
The aim of this study is to review the available literature regarding the epigenetic and genetic factors that are associated with the risk of curve progression in patients with adolescent idiopathic scoliosis, to help clinicians in identifying those who can benefit from treatment and a long-term follow-up in this subset of patients.
2. Materials and Methods
2.1. Review Design
A review of the literature was carried out following the Preferential Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12].
The Oxford level of evidence scale [13] was used to assess the level of evidence of the included studies. The full version was used to assess randomized and non-randomized clinical trials, whereas the modified version was used to assess all other studies.
Inclusion criteria considered papers describing genetic and epigenetic factors associated with AIS curve progression published in English peer-reviewed journals. Isolated case reports/series with less than 5 patients, literature reviews, and meta-analyses were excluded. The included articles met the PICO criteria for systematic reviews (Population, Intervention, Comparison, and Outcomes). Different types of studies were considered for inclusion: case series, case-control, cohort studies, comparative studies, genome-wide association studies, and case-only studies. These studies were conducted either retrospectively or prospectively.
2.2. Search Strategy
Pubmed-MEDLINE, The Cochrane Central Registry of Controlled Trials, Google Scholar, and the Embase Biomedical Database were searched over the years 1990–2022 to identify eligible studies in the English literature describing the genetic factors associated with AIS curve progression. The online literature search was conducted in January 2022 by three reviewers (MM, FB, and GV). The authors stated the following research question: “Are there genetic and epigenetic factors correlated with scoliotic curve progression in adolescent idiopathic scoliosis patients?”. This research question matched all four PICO concepts. Subsequently, the following key concepts were formulated “Adolescent Idiopathic Scoliosis”, “curve progression”, “curve severity” and “genetic variants”, “epigenetic variants”, and “polymorphism”, and various alternative terms were considered for each key concept to include the maximum number of articles available in the literature pertaining to the research question. Details on the search strategy are summarized in Supplementary Table S1.
The following search items were combined to perform the search: ‘adolescent idiopathic scoliosis’, ‘gene’, ‘curve progression’, ‘disease progression’, ‘polymorphism’, ‘epigenetic’, and ‘evolution’.
2.3. Study Selection
After screening the titles and abstracts, the full-text articles were obtained and reviewed. A manual search of the bibliography of each of the relevant articles was also performed to identify potentially missed eligible papers. Duplicates were removed. The study selection process carried out in accordance with the PRISMA flowchart is shown in Figure 2. The present systematic review was accepted for registration in the PROSPERO database for systematic reviews [14] (ID: CRD42022322089).
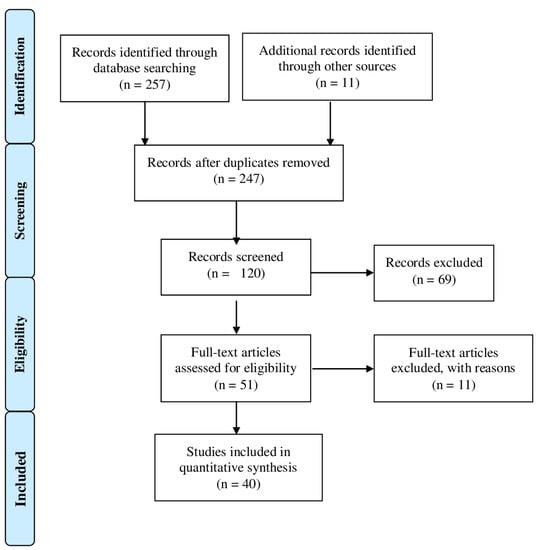
Figure 2.
Prisma 2009 flow diagram of the included studies.
2.4. Data Extraction
Two reviewers (MM and SN) extracted the data through a standardized data collection form. Three reviewers (MM, SN, and AR) checked the data for accuracy, and inconsistent results were analyzed for discussion. The extracted data concerning the study design (with the level of evidence), number of patients, demographics of patients, curve progression definition, biological sample, gene/s involved, mutation/s, and results are summarized in Table 1. The following outcomes were considered for analysis: curve severity defined as the Cobb angle; curve progression measured as the increase in the Cobb angle from the initial evaluation; epigenetic or genetic factors associated with curve progression; and clinical features of curve progression: curve location, age at diagnosis (<12 years), pre-menarche status, low Tanner stage, and peak height velocity time. Moreover, we considered some radiographic parameters currently considered by clinicians, such as the curve magnitude at the time of diagnosis (>25°), Risser stage (0–1), and open triradiate cartilage.

Table 1.
Details of the included studies. (NS = non specified).
2.5. Methodological Quality Assessment of Included Studies
The assessment of the methodological quality of the studies was performed using checklist criteria. The quality assessment tool adopted from the National Institutes of Health/National Heart, Lung, and Blood Institute was used [15]. After answering a series of multiple-choice questions, the quality of each study was reported as poor, fair, or good. All details are summarized in Supplementary Table S2.
3. Results
3.1. Included Studies
According to the research performed, a total of 40 papers [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55] met the inclusion criteria and were considered for review. Of these studies, twenty-one [18,19,21,24,31,33,35,36,37,38,39,40,41,42,44,45,47,50,54,55] were retrospective case-control studies, eight [16,17,27,28,46,48,49,53] were retrospective case series, and six [23,25,26,43,51,52] were retrospective cohort studies. In addition, there was one [30] Genome-Wide Association Study (GWAS), one [34] prospective case-control study, two [29,32] case-only studies, and one [22] retrospective comparative study.
According to the Oxford level of evidence scale, ten [16,17,27,28,29,32,46,48,49,53] of the included studies had a level of evidence IV, twenty-six [18,19,20,21,23,24,26,31,33,34,35,36,37,38,39,40,41,42,44,45,47,50,51,52,54,55] studies had a level of evidence III, while the remaining studies had a level of evidence II [22,25,30,43].
The studies analyzed both small and large-sized populations (n = 16 to 2645), describing the association between genetic and epigenetic factors involved in AIS curve progression.
The included studies are heterogeneous (or lacking data) in ethnicity, spine deformity, gender, and curve progression definition (Table 1).
3.2. Cohort Characteristics
The studies included in the search reported data on a total of 22,223 patients who underwent genome sampling and analysis, including 16,094 females (72.4%) and 1021 males (4.6%). The median age at the first visit ranged from 12.2 ± 1.2 to 18.5 ± 1.8 years and the median follow-up ranged from 12 months to 42 months. Asiatic populations (Chinese, Japanese, and Korean) [9,16,17,20,21,23,28,29,30,31,32,33,34,35,36,37,38,39,40,42,43,44,45,47,51,53,54,55,56] were the most studied by authors, but Caucasian populations (Europeans, Polish, and French-Canadian) [24,25,26,27,41,43,46,48,49,52], Russian [19], and Turkish [18] populations were also evaluated for possible associations. Two studies did not accurately describe the population demographics [30,43].
3.3. Spine Deformity Evaluation
A detail of the type of scoliotic curve was reported in eleven [16,17,19,22,24,39,40,42,47,51,53] of the selected studies (Table 1), for a total of 3949 thoracic curves (56.8%), 1019 lumbar curves (14.6%), 482 thoraco-lumbar curves (6.9%), 1304 double curves (18.7%), and 195 triple curves (2.8%).
In other studies [23,33,34,37,38,41,49,54,55], the diagnosis was generic or without accurate subtype distribution (i.e., thoracic, or thoracolumbar curve) or not reported [18,20,21,25,26,27,28,29,30,31,32,35,36,43,44,45,46,48,52,56].
As for the initial Cobb Angle, it was accurately described in twenty-three studies [16,17,18,19,21,26,27,29,31,32,34,35,37,39,40,41,44,45,46,47,48,49,50,51,55] with a median angle at first visit ranging from 20.1° ± 8.3° to 77.4° ± 16.1°; other studies reported the range of values or the minimum/maximum values [20,22,23,25,28,33,36,38,42,51,52,53,54].
Regarding the definition of curve progression, the included studies reported the following criteria: increase in the Cobb angle of more than 5° from initial evaluation [16,17,34,39,53,54] or more than 12° every year [41] or any increase on two consecutive X-ray exams taken six months apart [24], Cobb angle exceeding 30°, 40°, 45°, or 50° in an individual not growing [22,25,27,29,30,32,33,42,47,51,52], and a combination of different criteria including an increase in the Cobb angle and/or surgical correction and/or reaching skeletal maturity or not [22,25,52,53]. Twenty-four studies [18,19,20,21,23,26,28,30,31,32,35,36,37,38,40,43,44,45,48,49,50,55] did not specify criteria for spine deformity progression.
3.4. Genetic Factors Associated with Disease Progression
Genetic factors possibly influencing the progression of adolescent idiopathic scoliotic curves were analyzed on genomic DNA prevalently obtained from peripheral blood, or alternatively, from saliva [25,27,43,52].
Numerous polymorphisms were described as associated at different levels with scoliosis curve progression (Table 1), and related genes were hypothesized for their possible involvement in disease development.
Various genes with statistically significant evidence with AIS curve progression were described: Estrogen receptor alfa and beta (ER) [16,17,24,39,51,53], Insulin-like growth factor 1 (IGF-1) [21,28], Matrillin 1 gene (MATN1) [50], Calmodulin 1 gene (CALM 1) [51], Tryptophan hydroxylase 1 (TPH-1) [53], Neurothropin 3 (NFT3) [54], Interleukin 17 receptor (IL-17RC) [55], Ladybird homebox 1 (LBX1) [20], Lysosomal-associated transmembrane protein 4 beta (LAPTM4B) [21], Basonuclin 2 (BNC2) [31], Fibrillin 1 or 2 (FBN1/2) [23,37], Tissue inhibitor of metalloproteinase 2 (TIMP 2) [41], SRY-box transcription factor 9 (SOX9) [43], chromodomain helicase DNA binding protein 7 (CDH7) [46], Transforming growth factor beta 1 (TGF-B1) [19], and microRNA 4300 (MIR4300) [47]. Five retrospective studies [25,26,27,29,52] analyzed the association of multiple indices developed by combining 53 different gene SNPs and the initial Cobb angle (“ScoliScore” test) with non-progressive or progressive AIS. Of these, three [10,27,52] showed a significant association of the Scoliscore with different grades of curve progression. Only ER-, IGF-1-, FBN1-, and MIR4300-associated polymorphisms and the “Scoliscore” SNPs were successfully replicated in different populations [16,17,21,22,23,37,51].
In more detail, Ward et al. [52] investigated the predictive value of the Scoliscore in Caucasian AIS patients, suggesting that a risk model of patients’ natural history could be possible by extracting SNPs from patients’ DNA. The prognostic score, ranging from 1 to 200, was applied to three different cohorts with known AIS outcomes (low-risk females, high-risk females, and high-risk males, where high scores corresponded to a higher risk of curve progression and vice versa). Indeed, low-risk scores (<41) had a negative predictive value close to 100% for each of the three cohorts studied.
The promising “Scoliscore” results were not entirely replicated in the Chinese population by Xu et al. [29], with only two SNPs (rs9945359 and rs17044552) found to be associated with curve progression and severity [29]. The authors stated that, despite the existing ethnic differences (Caucasian vs. Chinese), AIS patients could share two SNPs as common traits in the pathogenesis of curve progression, but the Scoliscore was not reliable in the Chinese Han population.
Similar results were obtained by three other independent studies [25,26,27] analyzing the validity of the Scoliscore in Caucasian [25,27] and French-Canadian populations [26].
Putting all these findings together, it may be hypothesized that ethnic differences between Asian and Caucasian populations could yield great divergence regarding the prognostic power of “Scoliscore”. Moreover, the result was not replicated in studies with the same Caucasian population.
Insulin-like growth factor 1 (IGF-1) has an important role in skeletal growth [57], representing a good candidate to play a role in AIS curve progression. Yeung et al. [28] first reported a weak association (p = 0.04) between the IGF-1 polymorphism and a higher Cobb angle in Chinese AIS patients, suggesting IGF-1 as a disease-modifying gene rather than an AIS-onset gene per se.
This result was not replicated in the Japanese population [58], but an association (p = 0.01) was described between the rs5742612 polymorphism in the upstream region of the IGF-1 gene and disease risk, with a significantly different distribution of IGF-1 genotypes in low- and high-risk groups in the Korean population [21].
The estrogen receptor (ER) gene has been shown to be expressed in both human osteoclasts and osteoblasts and plays a critical role in cellular proliferation in bone tissue [59]. Based on the assumption that the estrogen reaction to skeletal and sexual growth is genetically determined by ER gene polymorphism, Inoue et al. [16,17] and Zhao et al. [51] found ER1 gene polymorphism (Xbal site) to be related to curve progression. However, in Tang et al.’s [39] study, a subgroup of Chinese skeletally immature patients was followed until skeletal maturity at age 16, and the abovementioned hypothesis was not confirmed.
Other successfully replicated genetic factors are FBN1 and FBN2 variants. The FBN1/2 genes encode fibrillin, a glycoprotein of the extracellular matrix, and mutations in these genes have been reported in a variety of fibrillin-related disorders (i.e., Marfan syndrome [60]).
To determine whether FBN1 and FBN2 variants were associated with AIS curve progression, Buchan et al. [23] and Sheng et al. [37] found that rare mutations in FBN1 and 2 were particularly present in severe AIS cases when compared to non-severe cases or healthy controls.
Most of the previously reported associations between genetic markers and AIS curve progression were not replicated in other independent studies. Therefore, Ogura et al. [30] and Wang et al. [47] explored the functional role of the rs35333564 variant located in the MIR4300HG gene in different ethnic populations (Japanese and Chinese). Both studies confirmed that the MIR4300HG functional variant could significantly add risk of curve progression with similar odds ratios and p-values. Moreover, Wang’s study [47] evaluated the relative expression of MIR4300 in paraspinal muscles among surgical patients carrying different MIR4300 genotypes, discovering that the GG genotype showed remarkably lower tissue expression than the AA genotype. Interestingly, and for the first time, the tissue expression level of MIR4300 was significantly correlated with curve severity. To the authors’ best knowledge, there are no studies that contradict the abovementioned association.
Altogether, available data on genetic factors correlated with AIS evolution do not allow the prediction of disease progression based only on genetic information.
Table 2 summarizes the findings concerning genetic factors associated with AIS progression, statistical significance, and the sensitivity/specificity of each variant.

Table 2.
The reported SNPs with statistically significant evidence in AIS curve progression (NS = non-specified, OR = odds ratio).
3.5. Epigenetic Factors Associated with Disease Progression
In eukaryotes, gene expression is dynamically regulated at the chromatin level by epigenetics, defined as heritable and reversible changes in gene expression without alterations of the underlying DNA nucleotide sequence [61]. Epigenetic marks principally include DNA methylation (the addition/removal of methyl groups to/from cytosines within CpG dinucleotides) and histone post-translational modifications (such as methylation, acetylation, phosphorylation, ubiquitination, and sumoylation). These modifications give rise to local chromatin remodeling that, in turn, modifies the accessibility of regulatory elements to genes. Regulation by non-coding RNAs such as microRNAs is also part of epigenetics. Epigenetic mechanisms regulate cell differentiation and development and are involved in human disease [62].
To date, few studies concerning epigenetic factors involved in AIS progression have been published, but literature data strongly encourage further research in this field.
Meng et al. [34], for the first time, reported a large-scale genome-wide analysis to establish a prognostic model based on methylation status. They analyzed peripheral blood cell DNA of two monozygotic twin pairs discordant for disease progression and validated the results in additional samples. They found a positive correlation between cg01374129 site demethylation and AIS progression (AUC value of 0.805 in the ROC analysis), suggesting epigenetic regulation. Since this site is near the HAS2 gene (hyaluronan synthase 2), playing a critical role in vertebral and intervertebral disc development, they speculated cg01374129 hypomethylation deregulates HAS2 expression, impairing normal spine development and causing scoliosis progression.
Another study [48] used a genome-wide methylation approach to test the influence of DNA methylation status on curve severity, by studying DNA from peripheral blood cells of eight monozygotic twin pairs. The authors found four probes (cg02477677, cg12922161, cg16382077, and cg08826461) where increasing curve severity was associated with hypomethylation. Candidate genes affected by differential methylation include the WNT signaling pathway and neuropeptide Y.
Mao et al. [36] investigated promoter methylation of the COMP gene, encoding the cartilage oligomeric matrix protein as a target gene for AIS curve progression. COMP promoter methylation, associated with low gene expression, was found to directly correlate with AIS curve severity (high Cobb angle of the main curve).
PITX1 (pituitary homeobox 1, a member of the RIEG/PITX homeobox transcription factors) gene promoter hypermethylation in peripheral blood cells of AIS patients is significantly associated with the Cobb angle of the main curve, suggesting a relationship with disease progression [38]. Similarly, average protochaderin 10 (PCDH10) promoter methylation was higher and gene expression was lower in AIS patients compared to controls. Moreover, high PCDH10 promoter methylation was associated with the Cobb angle of major curves in AIS patients [44]. Furthermore, in this case, data were obtained by analysis of DNA from peripheral blood cells.
In paravertebral muscles, H19 and ADIPOQ genes have been shown to be expressed inconsistently [40], with lower H19 levels and higher ADIPOQ levels in concave-sided muscle tissues compared to convex-sided ones. These data positively correlated with the spinal curve and age at initiation [40], suggesting an important role of H19 and ADIPOQ not only in the onset but also in the progression of AIS.
On the contrary, the methylation status of estrogen receptor 2 (ESR2) in deep paravertebral muscles was found to be associated with the occurrence but not progression of AIS [63].
In another study, the methylation status of tissue-dependent and differentially methylated regions (T-DMRs) of the ESR1 estrogen receptor was analyzed in superficial and deep paraspinal muscles to explore the association with AIS progression. The authors found suggestive evidence that methylation status might be associated with disease severity [49].
MicroRNAs are small noncoding RNAs that also participate in the regulation of bone metabolism, osteoclast, and osteoblast function. These molecules are epigenetic factors involved in the control of specific molecular pathways in bone-related disorders.
By performing miRNA expression profile analysis on plasma samples from severe and mild AIS patients and controls, Wang et al. [45] suggested miR-151a-3p as a putative biomarker of severe AIS since it was overexpressed in severe but not mild AIS patients. MiR-151a-3p may contribute to scoliosis progression through the inhibition of GREM1 gene expression in osteoblasts interrupting bone homeostasis.
Via microarray analysis, miRNA-145-5p (miR-145) and β-catenin mRNA (CTNNB1) were found to be overexpressed in AIS bone tissue and primary osteoblasts compared to controls. Significant negative correlations between circulating miR-145 and serum sclerostin, osteopontin, and osteoprotegerin were noted in patients with AIS. The observed aberrant miRNA expression inhibited osteocyte function via Wnt/β-catenin signaling, appearing dysregulated in AIS. MiR-145 was therefore suggested as a prognostic AIS biomarker [35].
In summary, the hypomethylation of some DNA regions, the hypermethylation of some gene promoters (COMP, PITX1, PDCH10), and the overexpression of some miRNAs (miR-145, miR-151a-3p) were associated with AIS progression.
Table 3 summarizes the available data on epigenetic factors associated with AIS progression, the techniques used, the tissues analyzed, and the statistical evidence.

Table 3.
Epigenetic factors associated with AIS progression (NS = non-specified, OR = odds ratio, AUC = area under the curve).
4. Discussion
Adolescent idiopathic scoliosis (AIS) is the most common type of scoliosis, a complex phenotype resulting from the interaction of multiple genetic loci with each other and the environment [53].
AIS is a progressive musculoskeletal disease that may result in cosmetic deformity, back pain and functional deficits, psychological problems, and impaired social interactions [64,65]. Among patients initially diagnosed with AIS, curve progression before skeletal maturity occurs in approximately two-thirds of cases, and in 10% of patients, it progresses to severe scoliosis (Cobb angle >40°) in the following years [6,66]. Although X-ray exams and clinical examinations are currently considered the gold standard for AIS follow-up, they have limited sensitivity and specificity values and provide limited information on curve progression risk [5]. Serial radiographs can result in relatively high cumulative radiation doses, leading to stochastic effects with long-term increased cancer and mortality risks [67]. A recent AIS cohort study stated an overall cancer rate (mostly breast and endometrial) that was five times higher in AIS patients followed up with X-ray exams than the general population [68]. Surgical intervention is currently the ultimate solution established for patients with a severe curve or with conservative treatment failure [69]. It can achieve powerful curve correction but is characterized by high morbidity and intra and/or post-operative complications [70,71].
The control of curve progression is therefore a crucial clinical task, but its etiology is still largely unknown; therefore, new biomarkers are needed to facilitate early detection and accurate curve progression risk assessment. The identification of such biomarkers has the potential to improve patient management, minimize unnecessary orthopedic intervention, define the best applicative protocol for orthopedic treatment, and identify the subpopulation of patients in which early surgery, even with non-severe curves, can avoid operating on severe curves with worse outcomes and more risks. Since clinical features do not adequately predict disease progression, more reliable prognostic factors need to be identified to increase the accuracy of the predictive model, and genetic/epigenetic markers might represent ideal candidates for AIS management. Although the role of genetic factors in AIS development is widely accepted, their role in disease progression is still under study.
In the present work, we systematically reviewed the available literature from 1990 to the present date, concerning genetic and epigenetic factors associated with AIS progression.
Forty papers met the inclusion criteria of the present review, with fifteen genes reported as having SNPs with a significant association with progressive AIS [25,26,27,29,52]. We also considered the development of a predictive algorithm based on a panel of 53 SNPs associated with AIS curve progression, the so-called “Scoliscore”, whose ability to discriminate between patients with a low or high risk of progression failed to be replicated in some populations [25,26,27,29,52].
Available data concerning genetic factors suggest a relatively low association and, if present, an association with low predictive capacity (Table 1 and Table 2), low odd risk values, and low level of evidence (III or IV). Moreover, the low replicability in different ethnicities confirms the extreme variability of the genetic influence on curve progression, suggesting its multifactorial nature, as is the case for AIS onset. Of the 15 genes reported as having SNPs with a significant association with progressive AIS, none showed sufficient power to sustain clinical applications.
Discordant AIS progression described in monozygotic twins [37] suggested the involvement of nongenetic factors and epigenetic processes are emerging as the best candidates [37], with a series of genes whose methylation was correlated with AIS curve severity [34,36,38]. Nine studies reporting epigenetic modifications showed promising results in terms of reliable markers suggesting epigenetics as the more promising field for the identification of factors associated with AIS progression, offering a rationale for further investigation in this field.
To the best of our knowledge, this is the first systematic scoping review where the available evidence evaluating the genetic and epigenetic factors influencing AIS curve progression was analyzed and, if necessary, integrated with additional calculations. Moreover, this work included an analysis of epigenetic factors, focusing not only on hereditable factors but also on the importance of environmental influences and tissue-related genetic expression on the AIS phenotype.
The main limitation of the present review is the presence of high heterogeneity among the included studies in terms of a lack of homogeneous study design and prospective comparative studies with high values of associations and predictive capacity, possibly representing the principal selection bias of the present work. Moreover, the absence of a clear, internationally recognized definition of progression of the curve and the low replicability of association between SNP and AIS progression in different populations generate non-reliably comparable conclusions and represent a confounding factor. The number of published papers on genetic and epigenetic factors related to AIS progression is noteworthy and surprising but without a final international consensus. Defining the factors related to AIS curve progression has the potential to completely renew the clinical management of such a frequent disease.
On the other hand, as more AIS progression-associated variants are identified, they could be incorporated into a “risk of progression scoring system” that can predict the risk of progression. Artificial intelligence may be used for this purpose, thanks to the development of algorithms based on deep learning and machine learning, employing data from spine radiographs, clinical patients’ features, and genetic/epigenetic factors to create a complete “tailored” diagnostic tool. Although this approach is fascinating, no clinical studies have attempted this approach.
Therefore, in the forthcoming years, different new biomarkers could be combined with clinical and radiographic parameters, hopefully for the development of new therapeutic strategies based on genetic factors and epigenetic modulators. In line with this mission, further prospective comparative studies with homogeneous architecture and cohorts are needed.
5. Conclusions
In conclusion, prognostic testing for AIS has the potential to significantly modify disease management. This will be achieved only after the identification of reliable markers and an understanding of the underlying biologic pathways. Genetic studies identified a series of loci associated with disease progression, whose power appears, however, insufficient to guide clinical choices. More recent evidence suggests epigenetics as a more promising field for the identification of factors associated with AIS progression, offering a rationale for further investigation in this field. More data are needed, and studies on tissues involved in the pathology, rather than peripheral blood, are necessary.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms23115914/s1.
Author Contributions
Conceptualization, A.R. and M.M.; methodology, M.M. and S.N.; formal analysis, M.M., A.R. and S.N.; data curation, M.M. and S.N.; writing—original draft preparation, M.M.; writing—review and editing, M.M., S.N., F.B., G.V., G.G., F.U. and A.R.; supervision, S.N., A.R. and C.F.; project administration, C.F.; funding acquisition, C.F. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by University of Bologna, by the Italian Health Ministry (program “5 per mille”—funds 2018) and by the IRCCS Istituto Ortopedico Rizzoli, Bologna—Italy (“Ricerca corrente” fund).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Thanks to “Grafica Biomedica” for its valuable artwork in representing the factors related to curve progression in adolescent idiopathic scoliosis.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Faldini, C.; Perna, F.; Geraci, G.; Pardo, F.; Mazzotti, A.; Pilla, F.; Ruffilli, A. Triplanar Correction of Adolescent Idiopathic Scoliosis by Asymmetrically Shaped and Simultaneously Applied Rods Associated with Direct Vertebral Rotation: Clinical and Radiological Analysis of 36 Patients. Eur. Spine J. 2018, 27, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Barile, F.; Ruffilli, A.; Manzetti, M.; Fiore, M.; Panciera, A.; Viroli, G.; Faldini, C. Resumption of Sport after Spinal Fusion for Adolescent Idiopathic Scoliosis: A Review of the Current Literature. Spine Deform. 2021, 9, 1247–1251. [Google Scholar] [CrossRef] [PubMed]
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of Adolescent Idiopathic Scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef]
- Lonstein, J.E. Adolescent Idiopathic Scoliosis. Lancet 1994, 344, 1407–1412. [Google Scholar] [CrossRef]
- Lonstein, J.E.; Carlson, J.M. The Prediction of Curve Progression in Untreated Idiopathic Scoliosis during Growth. J. Bone Jt. Surg. Ser. A 1984, 66, 1061–1071. [Google Scholar] [CrossRef]
- Pérez-Machado, G.; Berenguer-Pascual, E.; Bovea-Marco, M.; Rubio-Belmar, P.A.; García-López, E.; Garzón, M.J.; Mena-Mollá, S.; Pallardó, F.V.; Bas, T.; Viña, J.R.; et al. From Genetics to Epigenetics to Unravel the Etiology of Adolescent Idiopathic Scoliosis. Bone 2020, 140, 115563. [Google Scholar] [CrossRef]
- García-Cano, E.; Arámbula Cosío, F.; Duong, L.; Bellefleur, C.; Roy-Beaudry, M.; Joncas, J.; Parent, S.; Labelle, H. Prediction of Spinal Curve Progression in Adolescent Idiopathic Scoliosis Using Random Forest Regression. Comput. Biol. Med. 2018, 103, 34–43. [Google Scholar] [CrossRef]
- Zhu, Z.; Tang, N.L.S.; Xu, L.; Qin, X.; Mao, S.; Song, Y.; Liu, L.; Li, F.; Liu, P.; Yi, L.; et al. Genome-Wide Association Study Identifies New Susceptibility Loci for Adolescent Idiopathic Scoliosis in Chinese Girls. Nat. Commun. 2015, 6, 1–6. [Google Scholar] [CrossRef]
- Londono, D.; Kou, I.; Johnson, T.A.; Sharma, S.; Ogura, Y.; Tsunoda, T.; Takahashi, A.; Matsumoto, M.; Herring, J.A.; Lam, T.P.; et al. A Meta-Analysis Identifies Adolescent Idiopathic Scoliosis Association with LBX1 Locus in Multiple Ethnic Groups. J. Med. Genet. 2014, 51, 401–406. [Google Scholar] [CrossRef]
- Xu, L.; Huang, S.; Qin, X.; Mao, S.; Qiao, J.; Qian, B.P.; Qiu, Y.; Zhu, Z. Investigation of the 53 Markers in a DNA-Based Prognostic Test Revealing New Predisposition Genes for Adolescent Idiopathic Scoliosis. Spine 2015, 40, 1086–1091. [Google Scholar] [CrossRef]
- Xu, L.; Wu, Z.; Xia, C.; Tang, N.; Cheng, J.C.Y.; Qiu, Y.; Zhu, Z. A Genetic Predictive Model Estimating the Risk of Developing Adolescent Idiopathic Scoliosis. Curr. Genom. 2019, 20, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- OCEBM Levels of Evidence Working Group. “The Oxford 2011 Levels of Evidence”. Oxford Centre for Evidence-Based Medicine. Available online: https://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (accessed on 12 May 2022).
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the International Prospective Register of Systematic Reviews (PROSPERO) of Systematic Review Protocols Was Associated with Increased Review Quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef] [PubMed]
- NIH National Heart, Lung and Blood Institute. Study Quality Assessment Tools. Available online: Https://Www.Nhlbi.Nih.Gov/Health-Topics/Assessing-Cardiovascular-Risk (accessed on 12 May 2022).
- Inoue, M.; Minami, S.; Nakata, Y.; Takaso, M.; Otsuka, Y.; Kitahara, H.; Isobe, K.; Kotani, T.; Maruta, T.; Moriya, H. Prediction of Curve Progression in Idiopathic Scoliosis from Gene Polymorphic Analysis. Stud. Health Technol. Inform. 2002, 91, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Minami, S.; Nakata, Y.; Kitahara, H.; Otsuka, Y.; Isobe, K.; Takaso, M.; Tokunaga, M.; Nishikawa, S.; Maruta, T.; et al. Association between Estrogen Receptor Gene Polymorphisms and Curve Severity of Idiopathic Scoliosis. Spine 2002, 27, 2357–2362. [Google Scholar] [CrossRef]
- Yilmaz, H.; Zateri, C.; Uludag, A.; Bakar, C.; Kosar, S.; Ozdemir, O. Single-Nucleotide Polymorphism in Turkish Patients with Adolescent Idiopathic Scoliosis: Curve Progression Is Not Related with MATN-1, LCT C/T-13910, and VDR BsmI. J. Orthop. Res. 2012, 30, 1459–1463. [Google Scholar] [CrossRef]
- Ryzhkov, I.I.; Borzilov, E.E.; Churnosov, M.I.; Ataman, A.V.; Dedkov, A.A.; Polonikov, A.V. Transforming Growth Factor Beta 1 Is a Novel Susceptibility Gene for Adolescent Idiopathic Scoliosis. Spine 2013, 38, E699–E704. [Google Scholar] [CrossRef]
- Jiang, H.; Qiu, X.; Dai, J.; Yan, H.; Zhu, Z.; Qian, B.; Qiu, Y. Association of Rs11190870 near LBX1 with Adolescent Idiopathic Scoliosis Susceptibility in a Han Chinese Population. Eur. Spine J. 2013, 22, 282–286. [Google Scholar] [CrossRef]
- Moon, E.S.; Kim, H.S.; Sharma, V.; Park, J.O.; Lee, H.M.; Moon, S.H.; Chong, H.S. Analysis of Single Nucleotide Polymorphism in Adolescent Idiopathic Scoliosis in Korea: For Personalized Treatment. Yonsei Med. J. 2013, 54, 500–509. [Google Scholar] [CrossRef]
- Ogura, Y.; Takahashi, Y.; Kou, I.; Nakajima, M.; Kono, K.; Kawakami, N.; Uno, K.; Ito, M.; Minami, S.; Yanagida, H.; et al. A Replication Study for Association of 5 Single Nucleotide Polymorphisms with Curve Progression of Adolescent Idiopathic Scoliosis in Japanese Patients. Spine 2013, 38, 571–575. [Google Scholar] [CrossRef]
- Buchan, J.G.; Alvarado, D.M.; Haller, G.E.; Cruchaga, C.; Harms, M.B.; Zhang, T.; Willing, M.C.; Grange, D.K.; Braverman, A.C.; Miller, N.H.; et al. Rare Variants in FBN1 and FBN2 Are Associated with Severe Adolescent Idiopathic Scoliosis. Hum. Mol. Genet. 2014, 23, 5271–5282. [Google Scholar] [CrossRef] [PubMed]
- Kotwicki, T.; Janusz, P.; Andrusiewicz, M.; Chmielewska, M.; Kotwicka, M. Estrogen Receptor 2 Gene Polymorphism in Idiopathic Scoliosis. Spine 2014, 39, E1599–E1607. [Google Scholar] [CrossRef] [PubMed]
- Roye, B.D.; Wright, M.L.; Matsumoto, H.; Yorgova, P.; McCalla, D.; Hyman, J.E.; Roye, D.P.; Shah, S.A.; Vitale, M.G. An Independent Evaluation of the Validity of a DNA-Based Prognostic Test for Adolescent Idiopathic Scoliosis. J. Bone Jt. Surg. Am. Vol. 2014, 97, 1994–1998. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.L.; Julien, C.; Eveleigh, R.; Bourque, G.; Franco, A.; Labelle, H.; Grimard, G.; Parent, S.; Ouellet, J.; Mac-Thiong, J.M.; et al. A Replication Study for Association of 53 Single Nucleotide Polymorphisms in ScoliScore Test with Adolescent Idiopathic Scoliosis in French-Canadian Population. Spine 2015, 40, 537–543. [Google Scholar] [CrossRef]
- Bohl, D.D.; Telles, C.J.; Ruiz, F.K.; Badrinath, R.; DeLuca, P.A.; Grauer, J.N. A Genetic Test Predicts Providence Brace Success for Adolescent Idiopathic Scoliosis When Failure Is Defined as Progression to > 45 Degrees. Clin. Spine Surg. 2016, 29, E146–E150. [Google Scholar] [CrossRef]
- Yeung, H.Y.; Tang, N.L.; Lee, K.M.; Ng, B.K.W.; Hung, V.W.Y.; Kwok, R.; Guo, X.; Qin, L.; Cheng, J.C.Y. Genetic Association Study of Insulin-like Growth Factor-I (IGF-I) Gene with Curve Severity and Osteopenia in Adolescent Idiopathic Scoliosis. Stud. Health Technol. Inform. 2006, 123, 18–24. [Google Scholar]
- Xu, L.; Qin, X.; Sun, W.; Qiao, J.; Qiu, Y.; Zhu, Z. Replication of Association between 53 Single-Nucleotide Polymorphisms in a DNA-Based Diagnostic Test and AIS Progression in Chinese Han Population. Spine 2016, 41, 306–310. [Google Scholar] [CrossRef][Green Version]
- Ogura, Y.; Kou, I.; Takahashi, Y.; Takeda, K.; Minami, S.; Kawakami, N.; Uno, K.; Ito, M.; Yonezawa, I.; Kaito, T.; et al. A Functional Variant in MIR4300HG, the Host Gene of MicroRNA MIR4300 Is Associated with Progression of Adolescent Idiopathic Scoliosis. Hum. Mol. Genet. 2017, 26, 4086–4092. [Google Scholar] [CrossRef]
- Xu, L.; Xia, C.; Qin, X.; Sun, W.; Tang, N.L.S.; Qiu, Y.; Cheng, J.C.Y.; Zhu, Z. Genetic Variant of BNC2 Gene Is Functionally Associated with Adolescent Idiopathic Scoliosis in Chinese Population. Mol. Genet. Genomics 2017, 292, 789–794. [Google Scholar] [CrossRef]
- Takahashi, Y.; Kou, I.; Ogura, Y.; Miyake, A.; Takeda, K.; Nakajima, M.; Minami, S.; Kawakami, N.; Uno, K.; Ito, M.; et al. A Replication Study for the Association of Rs11190870 With Curve Severity in Adolescent Idiopathic Scoliosis in Japanese. Spine 2018, 43, 688–692. [Google Scholar] [CrossRef]
- Man, G.C.W.; Tang, N.L.S.; Chan, T.F.; Lam, T.P.; Li, J.W.; Ng, B.K.W.; Zhu, Z.; Qiu, Y.; Cheng, J.C.Y. Replication Study for the Association of GWAS-Associated Loci with Adolescent Idiopathic Scoliosis Susceptibility and Curve Progression in a Chinese Population. Spine 2019, 44, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Lin, T.; Liang, S.; Gao, R.; Jiang, H.; Shao, W.; Yang, F.; Zhou, X. Value of DNA Methylation in Predicting Curve Progression in Patients with Adolescent Idiopathic Scoliosis. EBioMedicine 2018, 36, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Chen, H.; Leung, R.K.K.; Choy, K.W.; Lam, T.P.; Ng, B.K.W.; Qiu, Y.; Feng, J.Q.; Cheng, J.C.Y.; Lee, W.Y.W. Aberrant MiR-145-5p/b-Catenin Signal Impairs Osteocyte Function in Adolescent Idiopathic Scoliosis. FASEB J. 2018, 32, 6537–6549. [Google Scholar] [CrossRef] [PubMed]
- Mao, S.; Qian, B.; Shi, B.; Zhu, Z.; Qiu, Y. Quantitative Evaluation of the Relationship between COMP Promoter Methylation and the Susceptibility and Curve Progression of Adolescent Idiopathic Scoliosis. Eur. Spine J. 2018, 27, 272–277. [Google Scholar] [CrossRef]
- Sheng, F.; Xia, C.; Xu, L.; Qin, X.; Tang, N.L.S.; Qiu, Y.; Cheng, J.C.Y.; Zhu, Z. New Evidence Supporting the Role of FBN1 in the Development of Adolescent Idiopathic Scoliosis. Spine 2019, 44, E225–E232. [Google Scholar] [CrossRef]
- Shi, B.; Xu, L.L.; Mao, S.; Xu, L.L.; Liu, Z.; Sun, X.; Zhu, Z.; Qiu, Y. Abnormal PITX1 Gene Methylation in Adolescent Idiopathic Scoliosis: A Pilot Study. BMC Musculoskelet. Disord. 2018, 19, 1–6. [Google Scholar] [CrossRef]
- Tang, N.L.S.; Yeung, H.Y.; Lee, K.M.; Hung, V.W.Y.; Cheung, C.S.K.; Ng, B.K.W.; Kwok, R.; Guo, X.; Qin, L.; Cheng, J.C.Y. A Relook into the Association of the Estrogen Receptor α Gene (PvuII, XbaI) and Adolescent Idiopathic Scoliosis: A Study of 540 Chinese Cases. Spine 2006, 31, 2463–2468. [Google Scholar] [CrossRef]
- Jiang, H.; Yang, F.; Lin, T.; Shao, W.; Meng, Y.; Ma, J.; Wang, C.; Gao, R.; Zhou, X. Asymmetric Expression of H19 and ADIPOQ in Concave/Convex Paravertebral Muscles Is Associated with Severe Adolescent Idiopathic Scoliosis. Molecular 2018, 24, 1–12. [Google Scholar] [CrossRef]
- Andrusiewicz, M.; Harasymczuk, P.; Janusz, P.; Biecek, P.; Żbikowska, A.; Kotwicka, M.; Kotwicki, T. TIMP2 Polymorphisms Association with Curve Initiation and Progression of Thoracic Idiopathic Scoliosis in the Caucasian Females. J. Orthop. Res. 2019, 37, 2217–2225. [Google Scholar] [CrossRef]
- Jiang, H.; Liang, S.; He, K.; Hu, J.; Xu, E.; Lin, T.; Meng, Y.; Zhao, J.; Ma, J.; Gao, R.; et al. Exome Sequencing Analysis Identifies Frequent Oligogenic Involvement and FLNB Variants in Adolescent Idiopathic Scoliosis. J. Med. Genet. 2020, 57, 405–413. [Google Scholar] [CrossRef]
- Takeda, K.; Kou, I.; Otomo, N.; Grauers, A.; Fan, Y.H.; Ogura, Y.; Takahashi, Y.; Momozawa, Y.; Einarsdottir, E.; Kere, J.; et al. A Multiethnic Meta-Analysis Defined the Association of Rs12946942 with Severe Adolescent Idiopathic Scoliosis. J. Hum. Genet. 2019, 64, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Shi, B.; Mao, S.; Xu, L.; Li, Y.; Sun, X.; Liu, Z.; Zhu, Z.; Qiu, Y. Quantitation Analysis of PCDH10 Methylation in Adolescent Idiopathic Scoliosis Using Pyrosequencing Study. Spine 2020, 45, E373–E378. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, H.; Yang, G.; Xiao, L.; Li, J.; Guo, C. Dysregulated Bone Metabolism Is Related to High Expression of MiR-151a-3p in Severe Adolescent Idiopathic Scoliosis. BioMed Res. Int. 2020, 2020, 4243015. [Google Scholar] [CrossRef] [PubMed]
- Borysiak, K.; Janusz, P.; Andrusiewicz, M.; Chmielewska, M.; Kozinoga, M.; Kotwicki, T.; Kotwicka, M. CHD7 Gene Polymorphisms in Female Patients with Idiopathic Scoliosis. BMC Musculoskelet. Disord. 2020, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dai, Z.; Wu, Z.; Feng, Z.; Liu, Z.; Sun, X.; Xu, L.; Qiu, Y.; Zhu, Z. Genetic Variant of MIR4300HG Is Associated with Progression of Adolescent Idiopathic Scoliosis in a Chinese Population. J. Orthop. Surg. Res. 2021, 16, 1–6. [Google Scholar] [CrossRef]
- Carry, P.M.; Terhune, E.A.; Trahan, G.D.; Vanderlinden, L.A.; Wethey, C.I.; Ebrahimi, P.; McGuigan, F.; Åkesson, K.; Hadley-miller, N. Severity of Idiopathic Scoliosis Is Associated with Differential Methylation: An Epigenome-Wide Association Study of Monozygotic Twins with Idiopathic Scoliosis. Genes 2021, 12, 1191. [Google Scholar] [CrossRef]
- Janusz, P.; Chmielewska, M.; Andrusiewicz, M.; Kotwicka, M.; Kotwicki, T. Methylation of Estrogen Receptor 1 Gene in the Paraspinal Muscles of Girls with Idiopathic Scoliosis and Its Association with Disease Severity. Genes 2021, 12, 790. [Google Scholar] [CrossRef]
- Chen, Z.; Tang, N.L.S.; Cao, X.; Qiao, D.; Yi, L.; Cheng, J.C.Y.; Qiu, Y. Promoter Polymorphism of Matrilin-1 Gene Predisposes to Adolescent Idiopathic Scoliosis in a Chinese Population. Eur. J. Hum. Genet. 2009, 17, 525–532. [Google Scholar] [CrossRef]
- Zhao, D.; Xing Qiu, G.; Peng Wang, Y.; Guo Zhang, J.; Xiong Shen, J.; Hong Wu, Z.; Wang, H. Association of Calmodulin1 Gene Polymorphisms with Susceptibility to Adolescent Idiopathic Scoliosis. Orthop. Surg. 2009, 1, 58–65. [Google Scholar] [CrossRef]
- Ward, K.; Ogilvie, J.W.; Singleton, M.V.; Chettier, R.; Engler, G.; Nelson, L.M. Validation of DNA-Based Prognostic Testing to Predict Spinal Curve Progression in Adolescent Idiopathic Scoliosis. Spine 2010, 35, 1455–1464. [Google Scholar] [CrossRef]
- Xu, L.; Qiu, X.; Sun, X.; Mao, S.; Liu, Z.; Qiao, J.; Qiu, Y. Potential Genetic Markers Predicting the Outcome of Brace Treatment in Patients with Adolescent Idiopathic Scoliosis. Eur. Spine J. 2011, 20, 1757–1764. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Mao, S.H.; Qian, B.P.; Jiang, J.; Qiu, X.S.; Zhao, Q.; Liu, Z. A Promoter Polymorphism of Neurotrophin 3 Gene Is Associated with Curve Severity and Bracing Effectiveness in Adolescent Idiopathic Scoliosis. Spine 2012, 37, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Qiu, X.S.; Zhu, Z.Z.; Wu, W.F.; Liu, Z.; Qiu, Y. A Single-Nucleotide Polymorphism Rs708567 in the IL-17RC Gene Is Associated with a Susceptibility to and the Curve Severity of Adolescent Idiopathic Scoliosis in a Chinese Han Population: A Case-Control Study. BMC Musculoskelet. Disord. 2012, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Anderson, M.V.; Cheng, W.K.; Wongworawat, M.D. Diabetes Associated with Increased Surgical Site Infections in Spinal Arthrodesis. In Proceedings of the 2008 Meeting of the Musculoskeletal Infection Society, Lake Tahoe, CA, USA, 8–9 August 2008; Springer: New York, NY, USA, February 2009; Volume 467, pp. 1670–1673. [Google Scholar]
- Giustina, A.; Mazziotti, G.; Canalis, E. Growth Hormone, Insulin-Like Growth Factors, and the Skeleton. Endocr. Rev. 2008, 29, 535. [Google Scholar] [CrossRef]
- Takahashi, Y.; Matsumoto, M.; Karasugi, T.; Watanabe, K.; Chiba, K.; Kawakami, N.; Tsuji, T.; Uno, K.; Suzuki, T.; Ito, M.; et al. Lack of Association between Adolescent Idiopathic Scoliosis and Previously Reported Single Nucleotide Polymorphisms in MATN1, MTNR1B, TPH1, and IGF1 in a Japanese Population. J. Orthop. Res. 2011, 29, 1055–1058. [Google Scholar] [CrossRef]
- Vidal, O.; Kindblom, L.G.; Ohlsson, C. Expression and Localization of Estrogen Receptor-β in Murine and Human Bone. J. Bone Miner. Res. 1999, 14, 923–929. [Google Scholar] [CrossRef]
- Ramirez, F.; Pereira, L.; Zhang, H.; Lee, B. The Fibrillin-Marfan Syndrome Connection. Bioessays 1993, 15, 589–594. [Google Scholar] [CrossRef]
- Reik, W. Stability and Flexibility of Epigenetic Gene Regulation in Mammalian Development. Nat. 2007, 447, 425–432. [Google Scholar] [CrossRef]
- Oh, E.S.; Petronis, A. Origins of Human Disease: The Chrono-Epigenetic Perspective. Nat. Rev. Genet. 2021, 22, 533–546. [Google Scholar] [CrossRef]
- Chmielewska, M.; Janusz, P.; Andrusiewicz, M.; Kotwicki, T.; Kotwicka, M. Methylation of Estrogen Receptor 2 (ESR2) in Deep Paravertebral Muscles and Its Association with Idiopathic Scoliosis. Sci. Rep. 2020, 10, 1–14. [Google Scholar] [CrossRef]
- Ylikoski, M. Growth and Progression of Adolescent Idiopathic Scoliosis in Girls. J. Pediatr. Orthop. B 2005, 14, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Saccomani, L.; Vercellino, F.; Rizzo, P.; Becchetti, S. Adolescents with Scoliosis: Psychological and Psychopathological Aspects. Minerva Pediatr. 1998, 50, 9–14. [Google Scholar] [PubMed]
- Asher, M.A.; Min Lai, S.; Burton, D.C. Further Development and Validation of the Scoliosis Research Society (SRS) Outcomes Instrument. Spine 2000, 25, 2381–2386. [Google Scholar] [CrossRef] [PubMed]
- Luan, F.J.; Wan, Y.; Mak, K.C.; Ma, C.J.; Wang, H.Q. Cancer and Mortality Risks of Patients with Scoliosis from Radiation Exposure: A Systematic Review and Meta-Analysis. Eur. Spine J. 2020, 29, 3123–3134. [Google Scholar] [CrossRef]
- Simony, A.; Hansen, E.J.; Christensen, S.B.; Carreon, L.Y.; Andersen, M.O. Incidence of Cancer in Adolescent Idiopathic Scoliosis Patients Treated 25 Years Previously. Eur. Spine J. 2016, 25, 3366–3370. [Google Scholar] [CrossRef]
- Murphy, R.F.; Mooney, J.F. Complications Following Spine Fusion for Adolescent Idiopathic Scoliosis. Curr. Rev. Musculoskelet. Med. 2016, 9, 462–469. [Google Scholar] [CrossRef]
- Carreon, L.Y.; Puno, R.M.; Lenke, L.G.; Richards, B.S.; Sucato, D.J.; Emans, J.B.; Erickson, M.A. Non-Neurologic Complications Following Surgery for Adolescent Idiopathic Scoliosis. J. Bone Jt. Surg. Ser. A 2007, 89, 2427–2432. [Google Scholar] [CrossRef]
- Menger, R.P.; Kalakoti, P.; Pugely, A.J.; Nanda, A.; Sin, A. Adolescent Idiopathic Scoliosis: Risk Factors for Complications and the Effect of Hospital Volume on Outcomes. Neurosurg. Focus 2017, 43, E3. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).