Integrative Analysis of Circulating Metabolite Profiles and Magnetic Resonance Imaging Metrics in Patients with Traumatic Brain Injury
Abstract
1. Introduction
2. Results
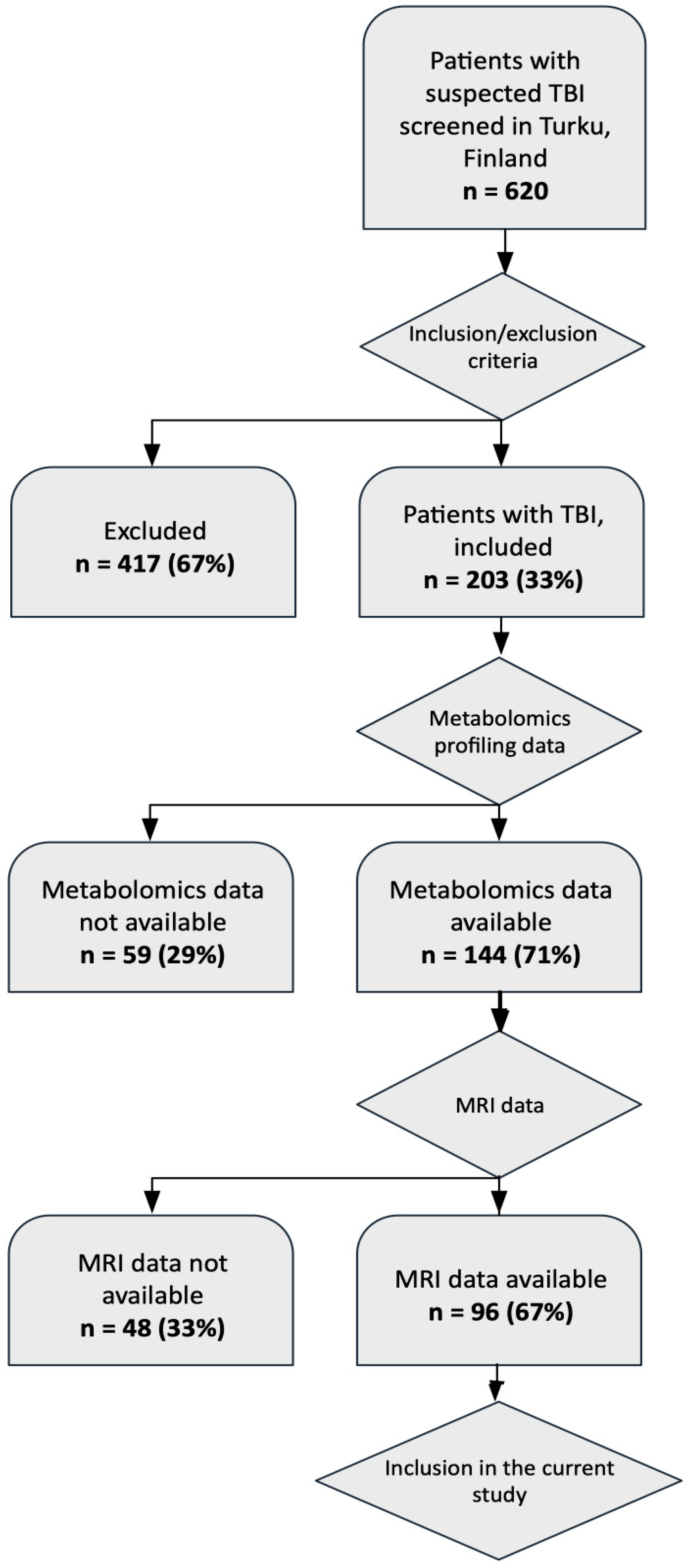
2.1. Study Setting and Data Survey
2.2. Metabolites Associate with Positive sMRI Findings
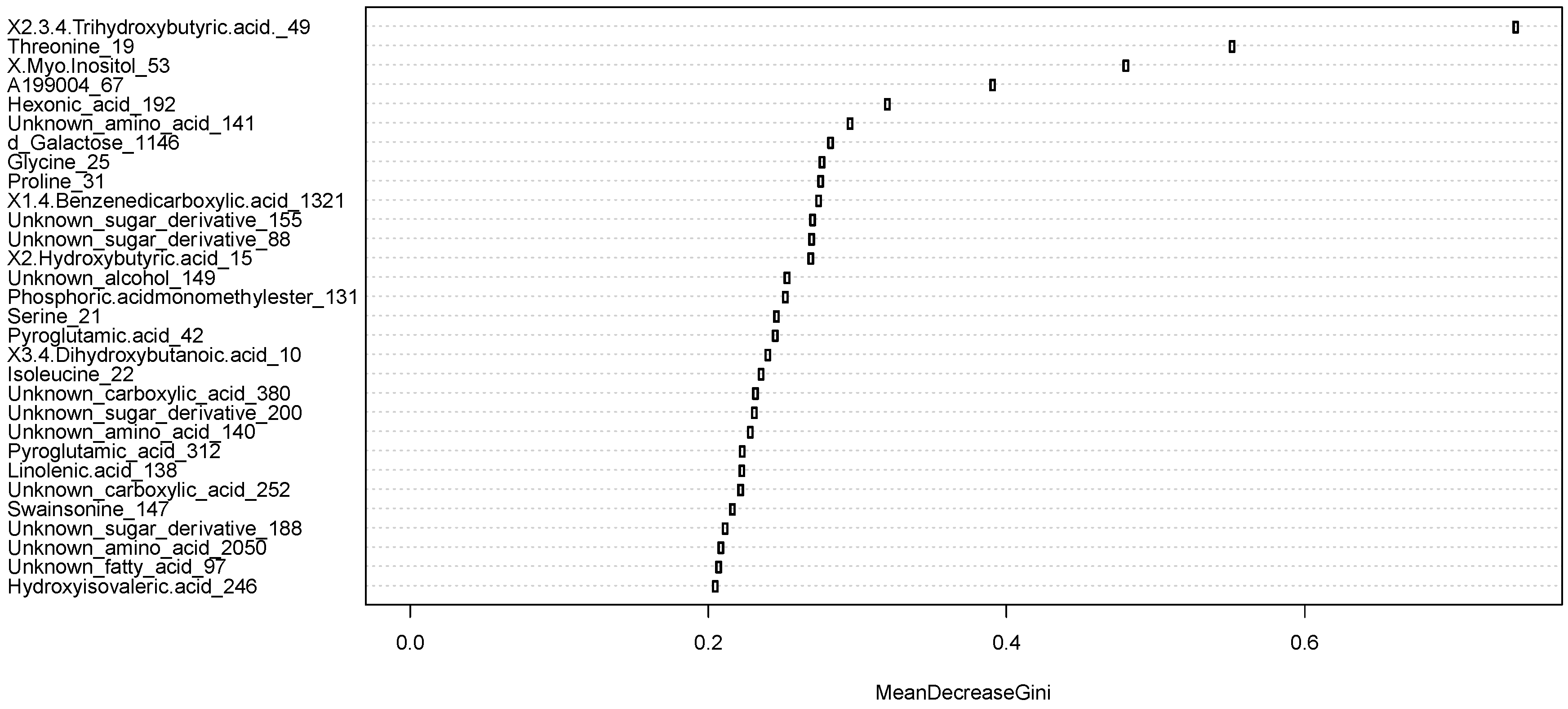
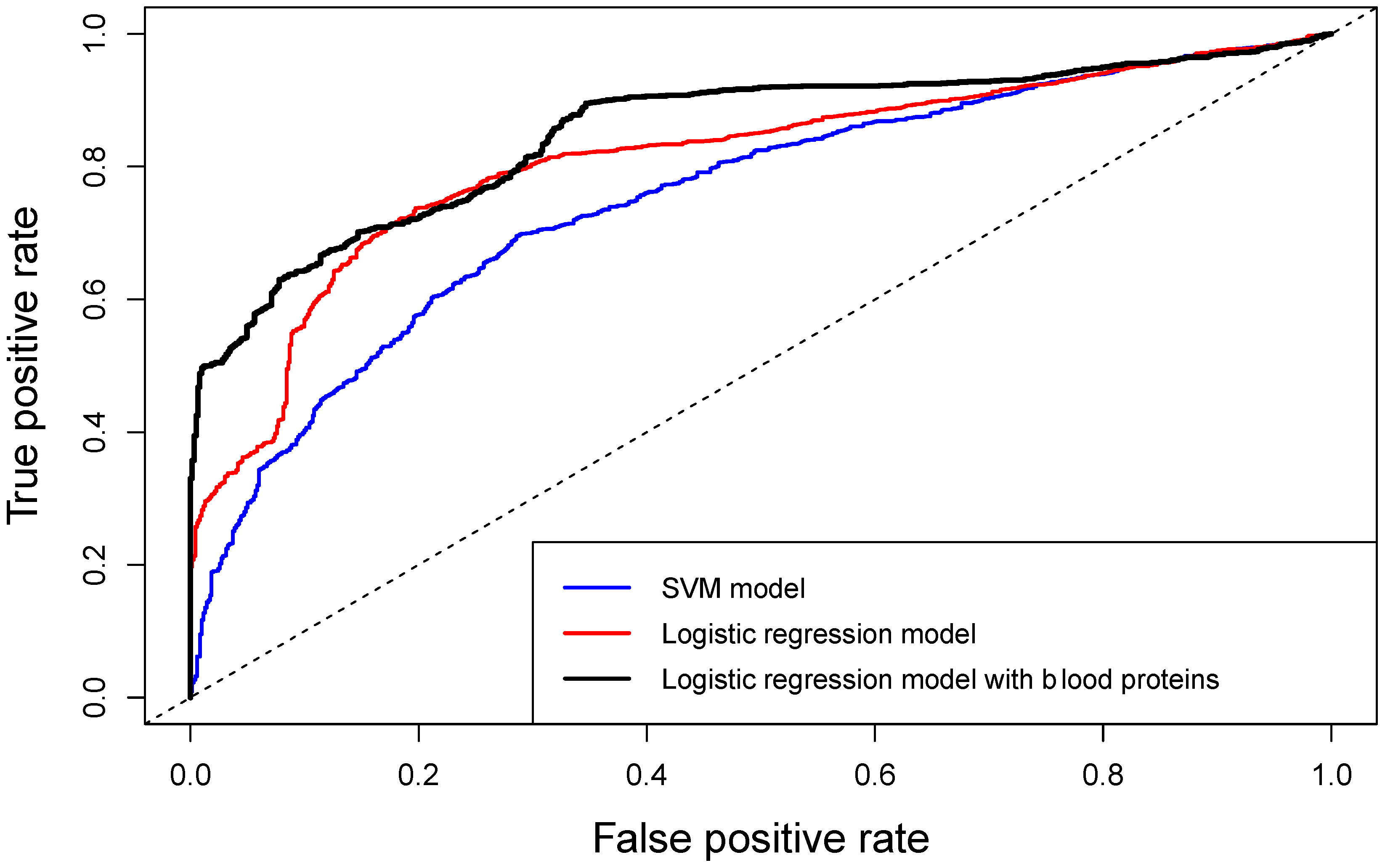
2.3. Discrimination of Positive vs. Negative sMRI Findings with Circulating Metabolites
2.4. Discrimination of Positive vs. Negative sMRI Findings with Circulating Metabolites Together with Protein Biomarkers
3. Discussion
4. Limitations
5. Materials and Methods
5.1. Ethics Statement
5.2. Data Description
5.3. Metabolomics Analysis
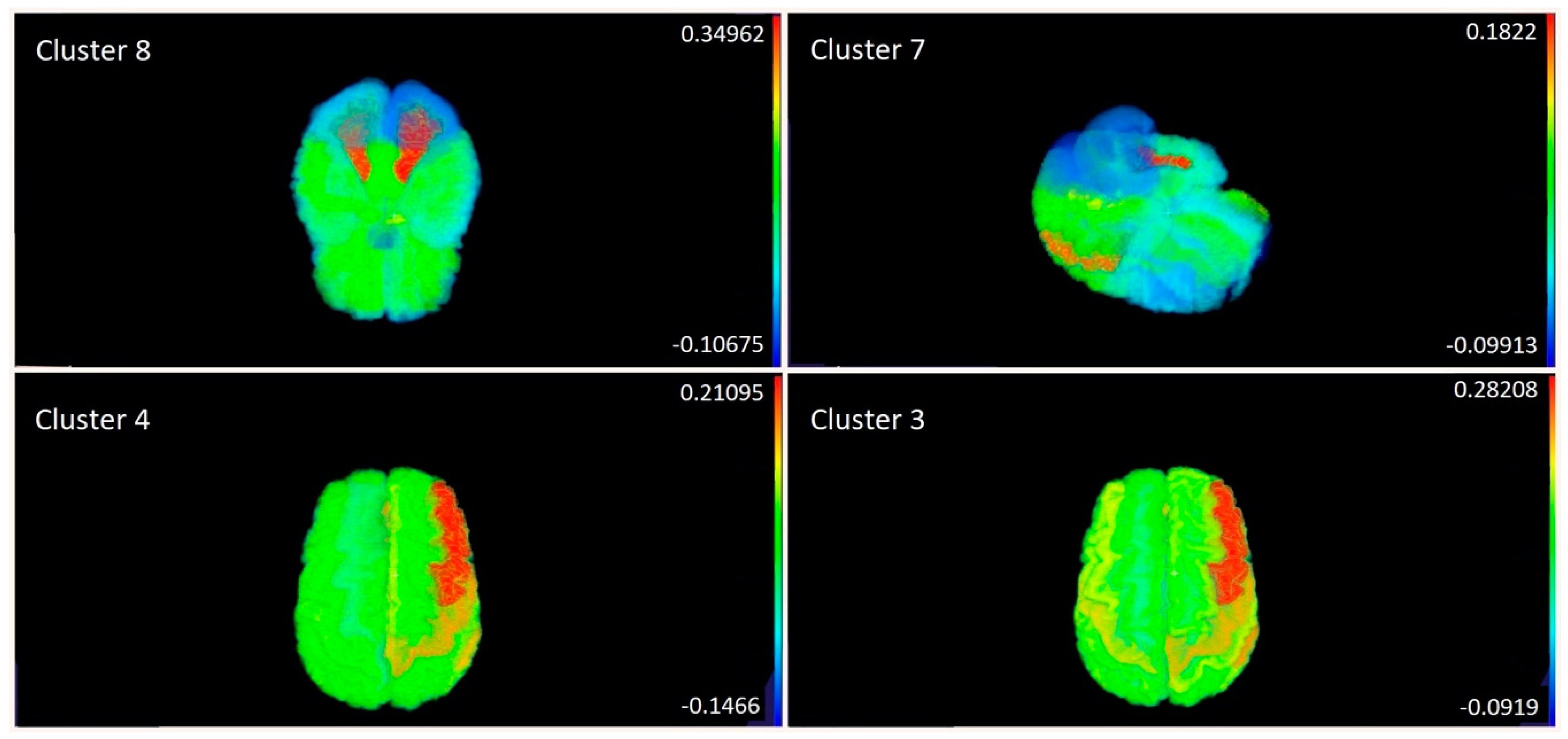
5.4. MRI Analysis
5.5. Data Analysis
5.5.1. Clustering of Metabolites
5.5.2. Feature Selection
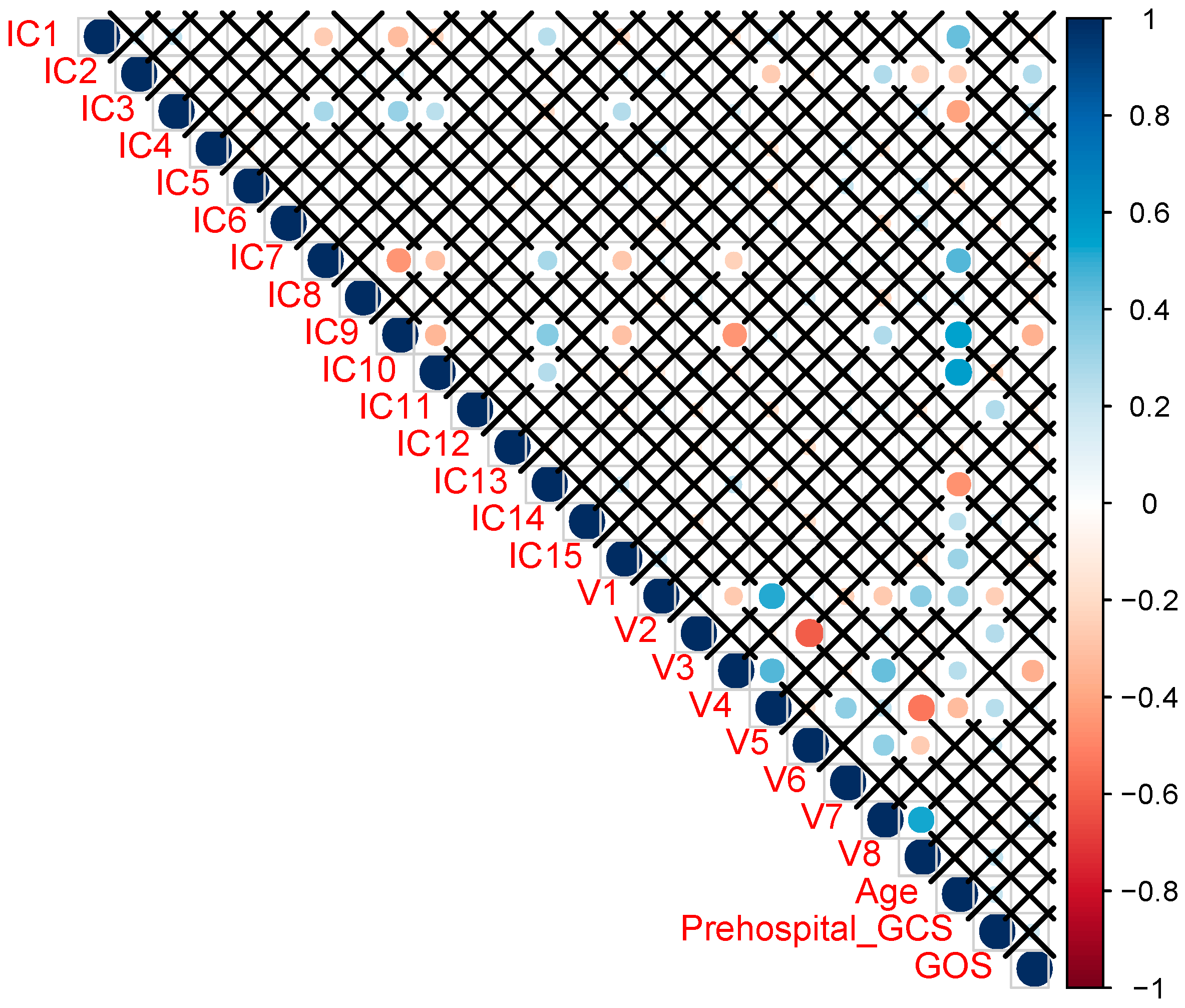
5.5.3. Correlation Analysis—Mapping
5.5.4. Predictive Analysis
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Majdan, M.; Plancikova, D.; Brazinova, A.; Rusnak, M.; Nieboer, D.; Feigin, V.; Maas, A. Epidemiology of traumatic brain injuries in Europe: A cross-sectional analysis. Lancet Public Health 2016, 1, e76–e83. [Google Scholar] [CrossRef]
- Hyder, A.A.; Wunderlich, C.A.; Puvanachandra, P.; Gururaj, G.; Kobusingye, O.C. The impact of traumatic brain injuries: A global perspective. J. Neurorehabilit. 2007, 22, 341–353. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Stocchetti, N.; Bullock, R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008, 7, 728–741. [Google Scholar] [CrossRef]
- Saatman, K.E.; Duhaime, A.C.; Bullock, R.; Maas, A.I.; Valadka, A.; Manley, G.T. Classification of traumatic brain injury for targeted therapies. J. Neurotrauma 2008, 25, 719–738. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.I.R.; Lingsma, H.F.; Roozenbeek, B. Predicting outcome after traumatic brain injury. Handb. Clin. Neurol. 2015, 128, 455–474. [Google Scholar] [CrossRef]
- Lakshmanan, R.; Loo, J.A.; Drake, T.; Leblanc, J.; Ytterberg, A.J.; McArthur, D.L.; Vespa, P.M. Metabolic crisis after traumatic brain injury is associated with a novel microdialysis proteome. Neurocrit. Care 2010, 12, 324–336. [Google Scholar] [CrossRef]
- Glenn, T.C.; Kelly, D.F.; Boscardin, W.J.; McArthur, D.L.; Vespa, P.; Oertel, M.; Martin, N.A. Energy dysfunction as a predictor of outcome after moderate or severe head injury: Indices of oxygen, glucose, and lactate metabolism. J. Cereb. Blood Flow Metab. 2003, 23, 1239–1250. [Google Scholar] [CrossRef]
- Koh, S.X.; Lee, J.K. S100B as a marker for brain damage and blood-brain barrier disruption following exercise. Sports Med. 2014, 44, 369–385. [Google Scholar] [CrossRef]
- Jeter, C.B.; Hergenroeder, G.W.; Ward, N.H., 3rd; Moore, A.N.; Dash, P.K. Human mild traumatic brain injury decreases circulating branched-chain amino acids and their metabolite levels. J. Neurotrauma 2013, 30, 671–679. [Google Scholar] [CrossRef]
- Clausen, F.; Hillered, L.; Gustafsson, J. Cerebral glucose metabolism after traumatic brain injury in the rat studied by 13C-glucose and microdialysis. Acta Neurochir 2011, 153, 653–658. [Google Scholar] [CrossRef]
- Papa, L.; Brophy, G.M.; Welch, R.D.; Lewis, L.M.; Braga, C.F.; Tan, C.N.; Hack, D.C. Time Course and Diagnostic Accuracy of Glial and Neuronal Blood Biomarkers GFAP and UCH-L1 in a Large Cohort of Trauma Patients With and Without Mild Traumatic Brain Injury. JAMA Neurol. 2016, 73, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Papa, L.; Akinyi, L.; Liu, M.C.; Pineda, J.A.; Tepas, J.J., 3rd; Oli, M.W.; Wang, K.K. Ubiquitin C-terminal hydrolase is a novel biomarker in humans for severe traumatic brain injury. Crit. Care Med. 2010, 38, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Gao, G.; Feng, J.; Jin, Y.; Wang, C.; Mao, Q.; Jiang, J. Glial fibrillary acidic protein as a biomarker in severe traumatic brain injury patients: A prospective cohort study. Crit. Care 2015, 19, 362. [Google Scholar] [CrossRef] [PubMed]
- Pelinka, L.E.; Kroepfl, A.; Leixnering, M.; Buchinger, W.; Raabe, A.; Redl, H. GFAP versus S100B in serum after traumatic brain injury: Relationship to brain damage and outcome. J. Neurotrauma 2004, 21, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Mondello, S.; Sorinola, A.; Czeiter, E.; Vamos, Z.; Amrein, K.; Synnot, A.; Buki, A. Blood-Based Protein Biomarkers for the Management of Traumatic Brain Injuries in Adults Presenting to Emergency Departments with Mild Brain Injury: A Living Systematic Review and Meta-Analysis. J. Neurotrauma 2018. [Google Scholar] [CrossRef]
- Posti, J.P.; Takala, R.S.K.; Lagerstedt, L.; Dickens, A.M.; Hossain, I.; Mohammadian, M.; Blennow, K. Correlation of Blood Biomarkers and Biomarker Panels with Traumatic Findings on Computed Tomography after Traumatic Brain Injury. J. Neurotrauma 2019, 36, 2178–2189. [Google Scholar] [CrossRef]
- Oresic, M.; Posti, J.P.; Kamstrup-Nielsen, M.H.; Takala, R.S.K.; Lingsma, H.F.; Mattila, I.; Hyotylainen, T. Human Serum Metabolites Associate With Severity and Patient Outcomes in Traumatic Brain Injury. EBioMedicine 2016, 12, 118–126. [Google Scholar] [CrossRef]
- Dickens, A.M.; Posti, J.P.; Takala, R.S.K.; Ala-Seppala, H.; Mattila, I.; Coles, J.P.; Oresic, M. Serum Metabolites Associated with Computed Tomography Findings after Traumatic Brain Injury. J. Neurotrauma 2018, 35, 2673–2683. [Google Scholar] [CrossRef]
- Yue, J.K.; Yuh, E.L.; Korley, F.K.; Winkler, E.A.; Sun, X.; Puffer, R.C.; Zafonte, R. Association between plasma GFAP concentrations and MRI abnormalities in patients with CT-negative traumatic brain injury in the TRACK-TBI cohort: A prospective multicentre study. Lancet Neurol. 2019, 18, 953–961. [Google Scholar] [CrossRef]
- McMahon, P.J.; Panczykowski, D.M.; Yue, J.K.; Puccio, A.M.; Inoue, T.; Sorani, M.D.; Okonkwo, D.O. Measurement of the glial fibrillary acidic protein and its breakdown products GFAP-BDP biomarker for the detection of traumatic brain injury compared to computed tomography and magnetic resonance imaging. J. Neurotrauma 2015, 32, 527–533. [Google Scholar] [CrossRef]
- Ledig, C.; Heckemann, R.A.; Hammers, A.; Lopez, J.C.; Newcombe, V.F.; Makropoulos, A.; Rueckert, D. Robust whole-brain segmentation: Application to traumatic brain injury. Med. Image Anal. 2015, 21, 40–58. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, S. Least squares quantization in PCM. J. IEEE Trans. Inf. 1982, 28, 129–137. [Google Scholar] [CrossRef]
- Hyvärinen, A.; Karhunen, J.; Oja, E. Independent Component Analysis, Adaptive and Learning Systems for Signal Processing, Communications, and Control; John Wiley & Sons: Hoboken, NJ, USA, 2001; Volume 1, pp. 11–14. [Google Scholar]
- Marcus, D.S.; Wang, T.H.; Parker, J.; Csernansky, J.G.; Morris, J.C.; Buckner, R.L. Open Access Series of Imaging Studies (OASIS): Cross-sectional MRI data in young, middle aged, nondemented, and demented older adults. J. Cogn. Neurosci. 2007, 19, 1498–1507. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.K. Random decision forests. Paper presented at the Proceedings of 3rd international conference on document analysis and recognition. In Proceedings of the 3rd International Conference on Document Analysis and Recognition, Montreal, QC, Canada, 14–16 August 1995. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Archer, K.J.; Kimes, R.V. Empirical characterization of random forest variable importance measures. Comput. Stat. Data Anal. 2008, 52, 2249–2260. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Zoerle, T. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: A European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef]
- Posti, J.P.; Dickens, A.M.; Orešič, M.; Hyötyläinen, T.; Tenovuo, O. Metabolomics profiling as a diagnostic tool in severe traumatic brain injury. Front. Neurol. 2017, 8, 398. [Google Scholar] [CrossRef]
- Jaeger, C.; Glaab, E.; Michelucci, A.; Binz, T.M.; Koeglsberger, S.; Garcia, P.; Buttini, M. The mouse brain metabolome: Region-specific signatures and response to excitotoxic neuronal injury. Am. J. Pathol. 2015, 185, 1699–1712. [Google Scholar] [CrossRef]
- Cole, J.H.; Jolly, A.; de Simoni, S.; Bourke, N.; Patel, M.C.; Scott, G.; Sharp, D.J. Spatial patterns of progressive brain volume loss after moderate-severe traumatic brain injury. Brain J. Neurol. 2018, 141, 822–836. [Google Scholar] [CrossRef]
- McKee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 45–66. [Google Scholar] [CrossRef]
- Kierans, A.S.; Kirov, I.I.; Gonen, O.; Haemer, G.; Nisenbaum, E.; Babb, J.S.; Lui, Y.W. Myoinositol and glutamate complex neurometabolite abnormality after mild traumatic brain injury. Neurology 2014, 82, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Ashwal, S.; Holshouser, B.; Tong, K.; Serna, T.; Osterdock, R.; Gross, M.; Kido, D. Proton spectroscopy detected myoinositol in children with traumatic brain injury. Pediatr. Res. 2004, 56, 630–638. [Google Scholar] [CrossRef]
- Chang, L.; Munsaka, S.M.; Kraft-Terry, S.; Ernst, T. Magnetic resonance spectroscopy to assess neuroinflammation and neuropathic pain. J. Neuroimmune Pharmacol. 2013, 8, 576–593. [Google Scholar] [CrossRef] [PubMed]
- Haris, M.; Cai, K.; Singh, A.; Hariharan, H.; Reddy, R. In vivo mapping of brain myo-inositol. Neuroimage 2011, 54, 2079–2085. [Google Scholar] [CrossRef] [PubMed]
- Engelke, U.F.; Zijlstra, F.S.; Mochel, F.; Valayannopoulos, V.; Rabier, D.; Kluijtmans, L.A.; Wevers, R.A. Mitochondrial involvement and erythronic acid as a novel biomarker in transaldolase deficiency. Biochim. Biophys. Acta 2010, 1802, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Jalloh, I.; Carpenter, K.L.; Grice, P.; Howe, D.J.; Mason, A.; Gallagher, C.N.; Hutchinson, P.J. Glycolysis and the pentose phosphate pathway after human traumatic brain injury: Microdialysis studies using 1,2-(13)C2 glucose. J. Cereb. Blood Flow Metab. 2015, 35, 111–120. [Google Scholar] [CrossRef]
- Harding, J.J.; Hassett, P.; Rixon, K.C.; Bron, A.J.; Harvey, D.J. Sugars including erythronic and threonic acids in human aqueous humour. J. Curr. Eye Res. 1999, 19, 131–136. [Google Scholar] [CrossRef]
- Hoffmann, G.; Seppel, C.K.; Holmes, B.; Mitchell, L.; Christen, H.; Hanefeld, F.; Nyhan, W. Quantitative organic acid analysis in cerebrospinal fluid and plasma: Reference values in a pediatric population. J. Chromatogr. B Biomed. Sci. Appl. 1993, 617, 1–10. [Google Scholar] [CrossRef]
- Ahonen, L.; Jantti, S.; Suvitaival, T.; Theilade, S.; Risz, C.; Kostiainen, R.; Hyotylainen, T. Targeted Clinical Metabolite Profiling Platform for the Stratification of Diabetic Patients. Metabolites 2019, 9, 184. [Google Scholar] [CrossRef]
- Einarsen, C.E.; Moen, K.G.; Haberg, A.K.; Eikenes, L.; Kvistad, K.A.; Xu, J.; Skandsen, T. Patients with Mild Traumatic Brain Injury Recruited from Both Hospital and Primary Care Settings: A Controlled Longitudinal Magnetic Resonance Imaging Study. J. Neurotrauma 2019, 36, 3172–3182. [Google Scholar] [CrossRef]
- Ercole, A.; Thelin, E.P.; Holst, A.; Bellander, B.M.; Nelson, D.W. Kinetic modelling of serum S100b after traumatic brain injury. BMC Neurol. 2016, 16, 93. [Google Scholar] [CrossRef] [PubMed]
- Ala-Seppälä, H.; Heino, I.; Frantzén, J.; Takala, R.S.; Katila, A.J.; Kyllönen, A.; Tenovuo, O. Injury profiles, demography and representativeness of patients with TBI attending a regional emergency department. J. Brain Inj. 2016, 30, 1062–1067. [Google Scholar]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef] [PubMed]
- Brain Trauma Foundation. Guidelines for the management of severe traumatic brain injury 3rd edition. J. Neurotrauma 2007, 24, 1–106. [Google Scholar]
- National Institute for Health and Care Excellence. Head injury: Assessment and early management|Guidance and guidelines. NICE Guidel. 2017. [Google Scholar] [CrossRef]
- Castillo, S.; Mattila, I.; Miettinen, J.; Oresic, M.; Hyotylainen, T. Data analysis tool for comprehensive two-dimensional gas chromatography/time-of-flight mass spectrometry. Anal. Chem. 2011, 83, 3058–3067. [Google Scholar] [CrossRef] [PubMed]
- Kopka, J.; Schauer, N.; Krueger, S.; Birkemeyer, C.; Usadel, B.; Bergmüller, E.; Stitt, M. GMD@ CSB. DB: The Golm metabolome database. J. Bioinform. 2004, 21, 1635–1638. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2017. [Google Scholar]
- Storey, J.D. A direct approach to false discovery rates. J. R. Stat. Soc. Ser. B (Stat. Methodol.) 2002, 64, 479–498. [Google Scholar] [CrossRef]
- Mendez, K.M.; Reinke, S.N.; Broadhurst, D.I. A comparative evaluation of the generalised predictive ability of eight machine learning algorithms across ten clinical metabolomics data sets for binary classification. Metabolomics 2019, 15, 150. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Menon, D.K.; Steyerberg, E.W.; Citerio, G.; Lecky, F.; Manley, G.T.; Sorgner, A. Collaborative european neurotrauma effectiveness research in traumatic brain injury (center-tbi) a prospective longitudinal observational study. J. Neurosurg. 2014, 76, 67–80. [Google Scholar] [CrossRef]

| Mean Age (SD) | 48.9 (18.9) |
| Sex | 63 males / 33 females |
| Pre-hospital GCS (SD) | 13.5 (3.1) |
| mTBI | 79 |
| moTBI | 10 |
| sTBI | 7 |
| Injury classification of MRI findings | |
| Code: 0 | 26 |
| Code: 1 | 5 |
| Code: 1,2,3,9 | 1 |
| Code: 1,3 | 7 |
| Code: 1,3,4 | 1 |
| Code: 1,3,5 | 1 |
| Code: 1,3,5,6,8 | 2 |
| Code: 1,3,5,6,9 | 1 |
| Code: 1,3,5,9 | 1 |
| Code: 1,3,6,9 | 1 |
| Code: 1,7 | 1 |
| Code: 1,9 | 4 |
| Code: 3 | 3 |
| Code: 3,5,6 | 1 |
| Code: 3,5,9 | 2 |
| Code: 3,6,8 | 1 |
| Code: 3,7,9 | 1 |
| Code: 3,8,9 | 1 |
| Code: 3,9 | 7 |
| Code: 4 | 1 |
| Code: 4,9 | 2 |
| Code: 6,8,9 | 1 |
| Code: 9 | 22 |
| Code: Unknown | 3 |
| Cluster No. | n Metabolites | Summary | Examples |
|---|---|---|---|
| 1 | 117 | Sugar intermediates, keto acids | d-Mannose, d-galactose, myo-inositol, hydroxyisovaleric acid |
| 2 | 35 | Tricarboxylic acid cycle (TCA) intermediates | Lactic acid, pyruvic acid |
| 3 | 59 | Sugar intermediates | Erythrose, gluconic acid, ribonic acid |
| 4 | 35 | Fatty acids | Arachidonic acid |
| 5 | 24 | Mostly unknowns | Glycerid acid |
| 6 | 51 | Fatty acids and intermediates | Oleic acid, stearic acid, adipic acid |
| 7 | 75 | Amino acids, microbial metabolites, sugar intermediates | Glycine, tryptophan, indole-3-propionic acid, erythronic acid |
| 8 | 55 | Amino acids | Leucine, valine, isoleucine, serine, phenylalanine, ornithine |
| Metabolites | MRI Positive | MRI Negative | p-values | |||
|---|---|---|---|---|---|---|
| ID | Name | Mean | SD | Mean | SD | |
| 19 | Threonine | 6.19 | 0.72 | 6.59 | 0.71 | 0.017 |
| 21 | Serine | 4.99 | 0.95 | 5.47 | 0.80 | 0.017 |
| 22 | Isoleucine | 5.79 | 0.74 | 6.16 | 0.71 | 0.033 |
| 25 | Glycine | 8.16 | 0.29 | 8.33 | 0.38 | 0.043 |
| 49 | Erythronic acid | 6.61 | 0.81 | 7.24 | 0.32 | 0.0000004* |
| 53 | Myo-inositol | 7.80 | 0.40 | 7.56 | 0.32 | 0.003 |
| 149 | Unknown alcohol | 3.94 | 1.28 | 4.59 | 0.79 | 0.004 |
| 188 | Unknown sugar derivative | 2.64 | 1.07 | 3.23 | 0.90 | 0.023 |
| 192 | Hexonic acid | 3.16 | 0.70 | 2.80 | 0.78 | 0.046 |
| 312 | Pyroglutamic acid | 3.61 | 2.04 | 4.59 | 2.11 | 0.047 |
| 380 | Unknown carboxylic acid | 2.18 | 1.22 | 1.49 | 1.27 | 0.008 |
| 1321 | 1,4-Benzenedicarboxylic acid | 0.18 | 1.09 | 0.781 | 1.13 | 0.024 |
| MRI Findings Classification |
|---|
| 0 = normal |
| 1 = contusion |
| 2 = EDH |
| 3 = acute SDH |
| 4 = chronic SDH |
| 5 = tSAH |
| 6 = ICH |
| 7 = punctate hemorrhage |
| 8 = diffuse oedema |
| 9 = diffuse axonal injury/white matter damage |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomas, I.; Dickens, A.M.; Posti, J.P.; Mohammadian, M.; Ledig, C.; Takala, R.S.K.; Hyötyläinen, T.; Tenovuo, O.; Orešič, M. Integrative Analysis of Circulating Metabolite Profiles and Magnetic Resonance Imaging Metrics in Patients with Traumatic Brain Injury. Int. J. Mol. Sci. 2020, 21, 1395. https://doi.org/10.3390/ijms21041395
Thomas I, Dickens AM, Posti JP, Mohammadian M, Ledig C, Takala RSK, Hyötyläinen T, Tenovuo O, Orešič M. Integrative Analysis of Circulating Metabolite Profiles and Magnetic Resonance Imaging Metrics in Patients with Traumatic Brain Injury. International Journal of Molecular Sciences. 2020; 21(4):1395. https://doi.org/10.3390/ijms21041395
Chicago/Turabian StyleThomas, Ilias, Alex M. Dickens, Jussi P. Posti, Mehrbod Mohammadian, Christian Ledig, Riikka S. K. Takala, Tuulia Hyötyläinen, Olli Tenovuo, and Matej Orešič. 2020. "Integrative Analysis of Circulating Metabolite Profiles and Magnetic Resonance Imaging Metrics in Patients with Traumatic Brain Injury" International Journal of Molecular Sciences 21, no. 4: 1395. https://doi.org/10.3390/ijms21041395
APA StyleThomas, I., Dickens, A. M., Posti, J. P., Mohammadian, M., Ledig, C., Takala, R. S. K., Hyötyläinen, T., Tenovuo, O., & Orešič, M. (2020). Integrative Analysis of Circulating Metabolite Profiles and Magnetic Resonance Imaging Metrics in Patients with Traumatic Brain Injury. International Journal of Molecular Sciences, 21(4), 1395. https://doi.org/10.3390/ijms21041395









