Abstract
As a second messenger in cellular signal transduction, calcium signaling extensively participates in various physiological activities, including spermatogenesis and the regulation of sperm function. Abnormal calcium signaling is highly correlated with male infertility. Calcium signaling is mainly regulated by both extracellular calcium influx and the release of calcium stores. Inositol 1,4,5-trisphosphate receptor (IP3R) is a widely expressed channel for calcium stores. After being activated by inositol 1,4,5-trisphosphate (IP3) and calcium signaling at a lower concentration, IP3R can regulate the release of Ca2+ from stores into cytoplasm, and eventually trigger downstream events. The closure of the IP3R channel caused by a rise in intracellular calcium signals and the activation of the calcium pump jointly restores the calcium store to a normal level. In this review, we aim to discuss structural features of IP3R channels and the underlying mechanism of IP3R channel-mediated calcium signaling and further focus on the research progress of IP3R expression and function in the male reproductive system. Finally, we propose key directions and strategies for research of IP3R in spermatogenesis and the regulation of sperm function to provide more understanding of the function and mechanism of IP3R channel actions in male reproduction.
1. Introduction
Ca2+ serves as a second messenger in cellular signal transduction to widely regulate many intracellular events, such as gene expression, synaptic transmission, and cellular death, differentiation and proliferation. Studies have shown that calcium signaling is also involved in spermatogenesis, sperm function, and fertilization, essential processes for male reproduction [1]. Calcium ions are stored in spermatogenic cells at various developmental stages, and also in Leydig and Sertoli cells [2]. The concentration of calcium in spermatogenic cells gradually increases from the early to late stages of spermatogenesis (spermatogonia < spermatocytes < spermatids < spermatozoa), and the concentration of calcium ions in seminiferous tubules also varies in different sections [2,3]. Calcium signaling in Leydig cells regulates the production of steroids through nuclear receptors and emergency response proteins mediated by a transcription cascade [4]. Abnormal calcium signaling can decrease testosterone levels, which results in abnormal spermatogenesis and even male infertility [5]. Some calcium-modulated or -binding proteins, such as calmodulin, are abundantly expressed in the testis [6]. The distinct distribution or oscillation of calcium levels and the expression of its regulatory proteins during spermatogenesis suggest that calcium signaling may play an essential role in spermatogenesis, in particular in the regulation of the growth and apoptosis of spermatogonia and spermatocytes [7,8]. Calcium signals also participate in the process of epididymal sperm maturation [9]. Studies have shown that some calcium channels maintain calcium homeostasis and regulate calcium signals, in turn affecting spermatogenesis. The treatment of mice with calcium channel inhibitors nifedipine and ethosuximide significantly blocked spermatogenesis at the elongating spermatid stage [10]. In addition, the expression of spermatogenesis-related genes Cerm, Transition protein 2, and Protamine 2 were significantly upregulated by these inhibitors, which further implies that calcium signaling plays a crucial role in spermatogenesis [10]. The content of Ca2+ in semen from infertile patients with asthenozoospermia and varicocele was significantly lower than that in normal males [11,12], and some patients with idiopathic infertility had significantly lower calcium levels in seminal plasma than fertile males [13,14]. These studies suggested that reduced calcium levels in seminal plasma may be a key cause of male infertility, and calcium in seminal plasma may have an important regulatory effect on sperm function. Future studies are required to verify this role. There have been many studies showing that calcium signaling regulates mature sperm function, such as the sperm acrosome reaction, capacitation, chemotaxis, and motility, as well as fertilization [1,15]. The absence of the sperm-specific calcium channel CatSper inhibited the influx of extracellular calcium, which impaired the hyperactivated mobility of sperm and led to male infertility [16]. However, there remains a lack of evidence regarding the function of calcium signaling in the different subcellular units of sperm, and the function of other calcium regulatory proteins in sperm calcium signaling and male infertility remains unknown. Intracellular calcium signaling is mainly regulated by calcium efflux, influx, and store release. Calcium efflux is regulated by the plasma membrane Ca2+-ATPase [17,18] and Na+/Ca2+ exchanger [19,20]. Although research on calcium influx during spermatogenesis has been scarce, studies in recent years have analyzed the function and mechanism of the CatSper channel in mature sperm and showed that disrupted calcium influx in sperm was closely related to male infertility. Deletion or mutation of the main subunit of CatSper often causes male sterility [16,21,22]. Research into the role and mechanism of calcium storage regulation during spermatogenesis and sperm function remains incomplete. Calcium stores combined with other key factors play critical roles in calcium homeostasis and calcium signaling. Generally, the increase in cytosolic Ca2+ is regulated by inositol 1,4,5-trisphosphate receptors (IP3Rs), ryanodine receptor channels, transient-receptor-potential channels, cyclic-nucleotide-gated channels, transient-receptor-potential-vanilloid channels, the store-operated Ca2+-channel and CatSper channel [1]. A decrease in cytosolic Ca2+ is regulated by the Ca2+-ATPase, Na+/Ca2+-exchanger, and Ca2+-transporter [23]. Many organelles, such as the autophagosomes, endoplasmic reticulum, endosomes, Golgi apparatus, lysosomes, mitochondria, nucleus, and secretory vesicles, serve as calcium stores involved in calcium signaling/homeostasis by storing or releasing Ca2+ [24]. The release and refilling of calcium stores are modulated by many Ca2+ channels, pumps, transporters, and Ca2+ binding proteins located in or coupled with calcium stores. The IP3R is one of the important receptor channels involved in the regulation of intracellular calcium stores. The IP3R is ubiquitously expressed in most cell types and evokes cellular processes such as embryonic development, gluconeogenesis and neuronal plasticity by controlling Ca2+ signals [25]. Expression profiles and pharmacological evidence suggest that IP3R may have important roles in spermatogenesis [7]. However, there is no comprehensive or in-depth literature available on IP3R in male reproduction, especially in the regulation of spermatogenesis and mature sperm function. Therefore, this review will systematically summarize the structural characteristics of the IP3R channel and its expression and function in the male reproductive system, and further discuss future research and strategies for understanding the role of IP3R in the regulation of spermatogenesis and sperm function.
2. Structure and Function of the IP3R Channel
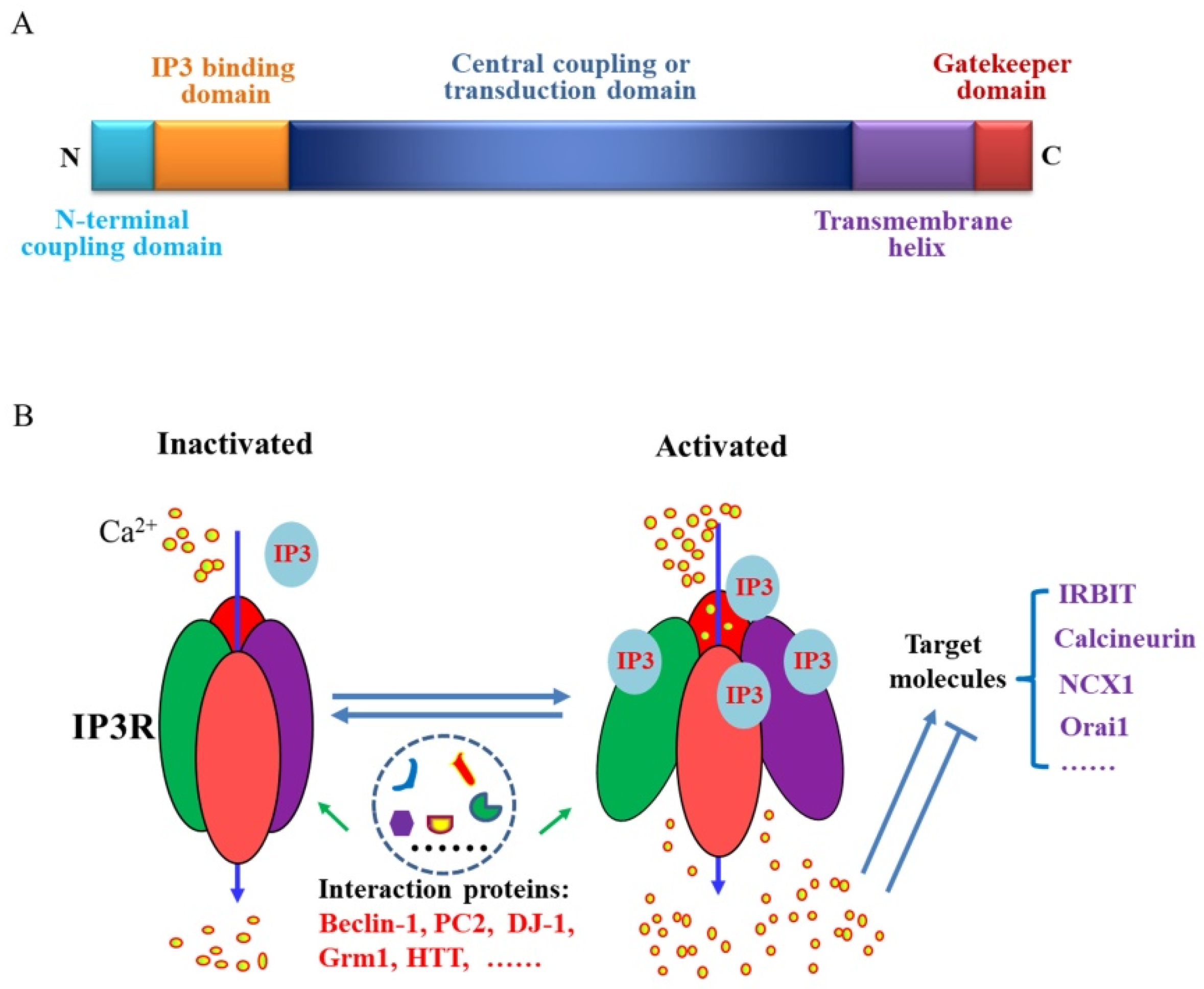
The IP3R is a calcium ion channel located in the endoplasmic reticulum and sarcoplasmic reticulum. It is a tetrameric protein receptor channel comprising four glycoproteins and has a relative molecular weight of about 260 kDa. To date, three types of IP3R channels, IP3R1, IP3R2, and IP3R3, have been identified, and all are encoded by three different genes [26]. A schematic diagram of IP3R proteins is shown in Figure 1A. Five domains found in the three types of IP3R channels include a coupling or inhibiting domain in the N-terminal region, an IP3-binding domain, a central coupling or transduction domain, a six-transmembrane helix, and a carboxy-terminal gatekeeper domain [26]. The binding domains and calcium channel domains of the three types of IP3R channels are highly homologous. The sequence identities between Type I and Type II, and between Type III and Type I, are 69% and 64%, respectively [27]. Because of this high homology, functional heterotetramer channels can be formed between all the different subtypes [28]. Thus, diverse IP3R channels can take part in the regulation of wide ranging physiological activities [29]. At present, the structures of IP3R1 and IP3R3 have been established by cryo-electron microscopy. Resting IP3R1 and IP3R3 have similar structures but different mechanisms of activation and regulation [30,31]. The structure of activated IP3R1, after combining with inositol 1,4,5-trisphosphate (IP3), remains unclear. The IP3R subtypes have diverse mechanisms for sensing stimuli from different signals and for regulating different interacting molecules. Although the affinities of the IP3-binding core of three IP3R isoforms for IP3 are similar, there are some differences in sensitivity towards IP3 (IP3R2 > IP3R1 > IP3R3) and towards the various regulatory factors and proteins [29,32]. The sensitivity to cytosolic Ca2+ also varies between the IP3R isoforms. IP3R3 is the most sensitive to modulation by Ca2+, followed by IP3R2, then IP3R1 [33]. ATP enhances Ca2+ release from IP3R channels. However, the three IP3R isoforms are reported to respond to ATP with differing sensitivities. Knockout (KO) studies in cells showed that Ca2+ release through IP3R1 was positively regulated at lower ATP concentrations than IP3R3, and IP3R2 was the isoform most sensitive to stimulatory ATP concentrations [34]. In addition, the sulfhydryl-reagent thimerosal increased the sensitivity of IP3-evoked Ca2+ release via IP3R1 and IP3R2 but inhibited IP3R3 activity [35].
Figure 1.
Diagram of the structure and regulation of the inositol 1,4,5-trisphosphate receptor (IP3R) channel. (A) Five domains of IP3R. (B) Regulation of IP3R by IP3, Ca2+ and interaction proteins.
IP3R channel activity is mainly regulated by IP3, Ca2+ and interaction proteins (Figure 1B). The classical IP3R-mediated calcium signaling pathway is as follows: phospholipase C (PLC) catalyzes the hydrolysis of phosphatidylinositol 4,5-bisphosphate to form IP3 and diacylglycerol. IP3 diffuses into the cytoplasm and binds to the IP3R receptor on the sarcoplasmic or endoplasmic reticulum to regulate the opening of the channel [36]. A low concentration of Ca2+ stimulates the opening of the IP3R channel, but a high Ca2+ concentration causes closure of the channel, which is known as Ca2+-induced Ca2+ release. In this process, calcium ions released from the endoplasmic reticulum are further amplified by other Ca2+ receptor channels, such as ryanodine receptors. To restore the level of Ca2+ in the endoplasmic reticulum or sarcoplasmic reticulum, Ca2+ ATPases (SERCA, Sarco- or Endoplasmic Reticulum Ca2+ ATPases) pump calcium ions in the cytoplasm back to the endoplasmic reticulum, and thus periodically regulate the cellular transmission of Ca2+ to participate in the regulation of various physiological activities [26]. In addition, many interaction proteins and other factors also modulate IP3R’s activity to cooperate with calcium signaling in different ways. This will be discussed in Section 4.
3. Expression of IP3Rs in Male Reproduction
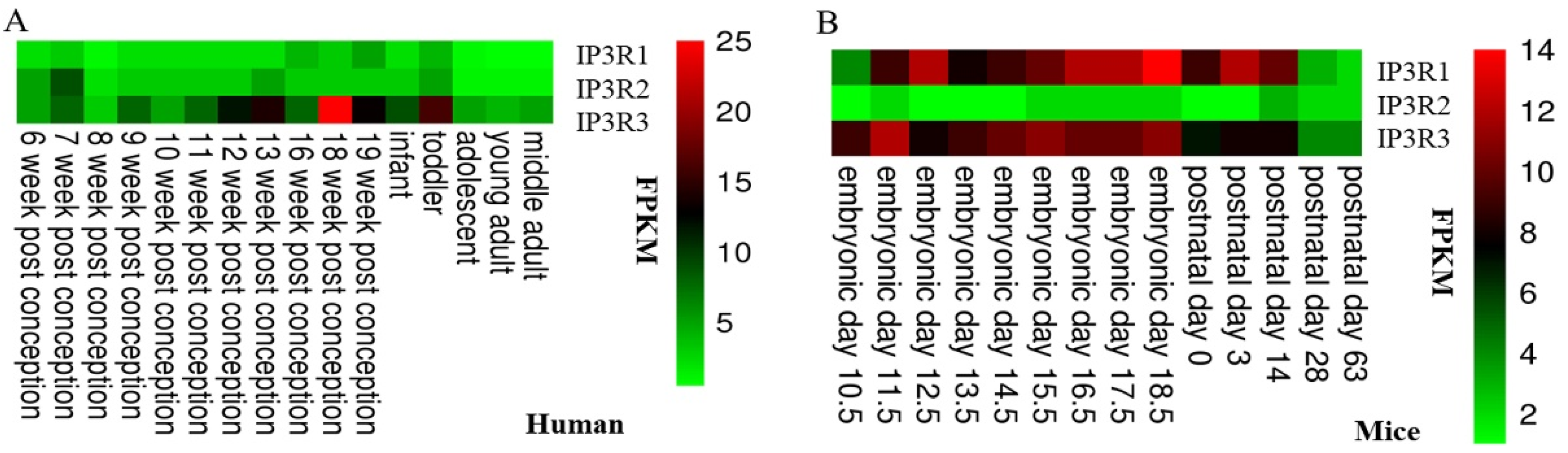
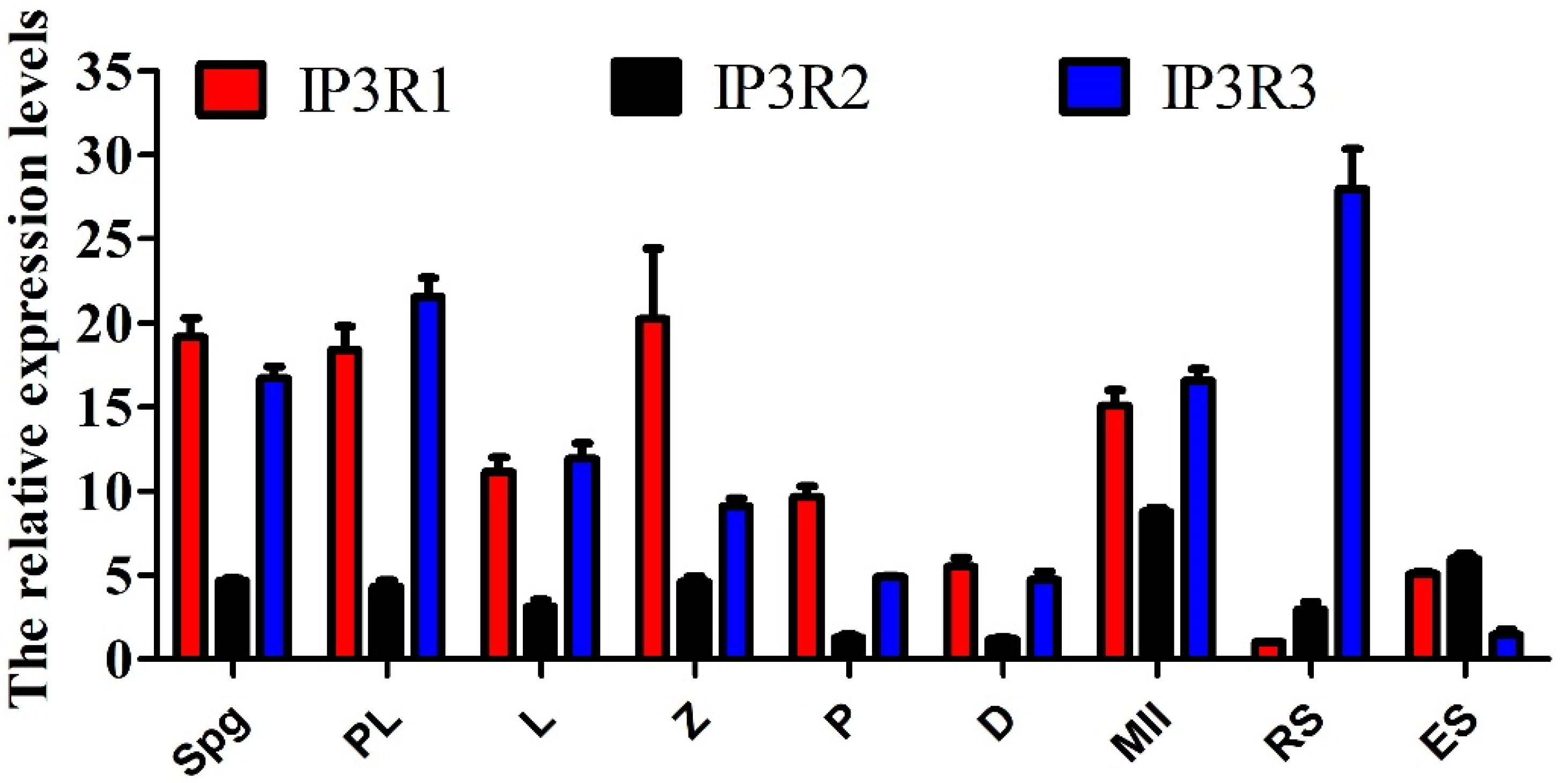
Three types of IP3R channel proteins are widely and differently expressed in various tissues, possibly because distinct tissues need different types of functional IP3R receptors. All three types of IP3R are expressed in the testis, spermatogenic cells, and mature sperm [37,38]. The expression of IP3R mRNA in human and mouse testes at different stages of development are depicted in Figure 2. A study in CD1 mice found that the three IP3R mRNAs were expressed in all stages of spermatocyte development [7]. IP3R protein expression exhibited a specific temporal distribution pattern, in spermatogenic cells, with expression dispersed in the cytoplasm in the early stage; then, during sperm differentiation, IP3R protein is gradually expressed on the Golgi complex [7]. Our data also displayed that IP3R1, IP3R2, and IP3R3 mRNAs were expressed in spermatogenic cells of C57/BL6 mice. In early spermatogenic cells, IP3R1 and IP3R3 had higher expression levels than IP3R2 (Figure 3). The expression of IP3R was also detected in the mature sperm of boars and humans [39], and cattle [40]. IP3R was reported to be localized in the acrosome and the principal piece of the flagellum in mature sperm of mice, but the precise location of IP3Rs in sperm remains controversial because of inconsistent results in different studies [7], and the precise subcellular location of IP3R in sperm remains to be determined. The expression of IP3R in human sperm varies slightly in different studies, possibly because of differences in the detecting antibodies. Human sperm may only contain IP3R1 and IP3R3. In sea urchin sperm, IP3R1 protein was also detected in the plasma membrane [41]. In general, most studies suggest that IP3R exists in the acrosome, principal piece of the flagellum, and cytoplasmic droplets in sperm [42,43]. Other research confirmed the presence of IP3R in the acrosome of human sperm [44]. Many organelles, such as the endoplasmic reticulum, Golgi apparatus, and lysosomes, provide the main Ca2+ stores in somatic cells. However, mature sperm lack these organelles and the mitochondria and some of the membranous structures of sperm contain many calcium regulatory factors (IP3R and SERCA), which may act to regulate Ca2+ stores. It is well known that the acrosome and mitochondria provide the prominent intracellular Ca2+ stores in mature sperm [1]. The expression level of IP3R1 decreases after the acrosome reaction, while there is no significant change in the level of IP3R3 [45]. The residual IP3R3 in the acrosome suggests that it may also play an essential role in fertilization and early embryonic development. In addition, an [3H] isotope labeling experiment showed that there was a stoichiometric interaction between IP3 and IP3R in sperm before and after the acrosome reaction [45]. IP3R acts as a “bridge” contributing to endoplasmic reticulum–mitochondrial contacts and Ca2+ transfer from the endoplasmic reticulum to mitochondria [46]. However, the expression and roles of IP3R in sperm mitochondria are still unknown. The redundant nuclear envelope (RNE), surrounding the axoneme at the base of the flagellum, provides the third Ca2+ store in sperm involved in Ca2+ mobilization [47]. Preliminary experimental evidence suggests that the RNE contains IP3R, which may regulate sperm hyperactivated motility [42].
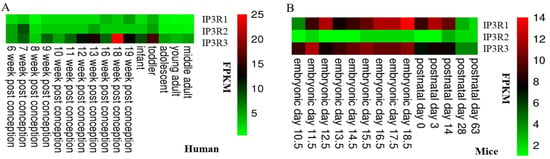
Figure 2.
mRNA expression levels of inositol 1,4,5-trisphosphate receptors (IP3Rs) in human (A) and mouse (B) testes at different stages of development. The data were obtained from the ArrayExpress database (E-MTAB-6814 and E-MTAB-6798). Fragments Per Kilobase Million (FPKM) values from RNA-seq experiments were used to indicate the mRNA expression levels of IP3Rs.
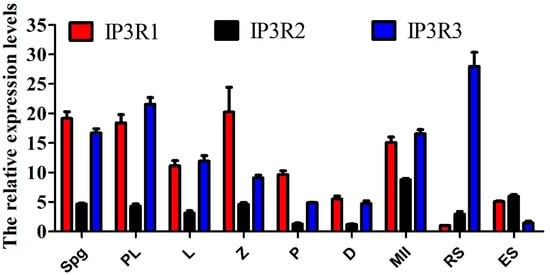
Figure 3.
mRNA expression levels of inositol 1,4,5-trisphosphate receptors (IP3Rs) in mouse spermatogenic cells. Spermatogonia (Spg), preleptotene (PL), leptotene (L), zygotene (Z), pachytene (P), diplotene (D), secondary spermatocytes (MII), round spermatids (RSs), and elongated spermatids (ES) were sorted by flow cytometry with Hochest33342/propidium staining. Total RNA was used to analyze mRNA expression levels of IP3R1, IP3R2 and IP3R3 by qPCR. β-actin served as an internal control to normalize the gene expression levels.
4. Roles of IP3R in Male Reproduction
There has been limited research on the roles of IP3R in male reproduction; however, previous studies indicated that IP3R may play a key role in spermatogenesis. Some studies found that the inhibition of IP3R1 expression using specific oligonucleotides completely blocked spermatocyte proliferation in mice [36]. In Caenorhabditis elegans, IP3R mutant males produced normal sperm but were defective in sperm transfer and spicule insertion, which resulted in infertility [48]. Research in drosophila found that IP3R was required for spermatocyte division, because the IP3R antagonist 2-APB (2-aminoethoxydiphenyl borate) significantly impaired cleavage furrow stability in cytokinesis [49]. Interestingly, 2-APB also increased CatSper-mediated calcium signaling in human sperm [50]. Thapsigargin is a selective inhibitor of Ca2+ ATPase and induces the release of calcium ions from IP3-sensitive calcium stores. Thapsigargin significantly induced the acrosome reaction in sperm from hamsters, humans, and mice [51,52,53]. IP3R is thought to be involved in sperm hyperactivation [42,54] and the regulation of thermotaxis [55]. A recent study using a novel permeabilization tool, BioPORTER, to deliver IP3R antibody or IP3 to block or activate IP3R activity, respectively, showed that the IP3R1 channel was involved in the zona pellucida- and progesterone-induced acrosome reaction and calcium influx [56]. These pharmacological or in vitro findings indicated that the IP3R channel is vital for the regulation of spermatogenesis and mature sperm function. In addition, some factors of the IP3R signaling pathway combined with PLCζ may induce egg activation [57].
Research has shown that most IP3R1-deficient mice die in utero at an early stage of embryonic development. The IP3R1-deficient animals surviving to birth suffer from severe ataxia and seizures, and do not survive after the weaning period [58,59]. Phenotypic analysis of the reproductive system showed that epididymal development was significantly impaired (decreased weight) (International Mouse Phenotyping Consortium). Conversely, IP3R2 and IP3R3 knockout mice usually survive, and the fertility of male mice was not remarkably affected [60]. However, it is unclear whether calcium signaling was abnormal in spermatogenetic cells and mature sperm in these KO mice. The knockout of IP3R2 or IP3R3 alone does not affect spermatogenesis or sperm function. Because of the importance of the IP3R channel in various biological processes, it is possible that a specific mechanism of rescuing or compensation was established from other calcium regulation channels. In addition, functional heterotetrameric channels can be formed via the high homology among the three subtypes, which leads to possible compensation from other types of IP3Rs. These possibilities should be verified by models of conditional double or triple KOs of IP3Rs. A recent study demonstrated that IP3R1 located on tubulobulbar complexes, at the junction of the endoplasmic reticulum and plasma membrane, plays an important role in spermatogenesis by regulating Ca2+ signals [37,61,62]. Furthermore, the knockdown of IP3R1 in Sertoli cells gave rise to the abnormal morphology of actin protein at the junction of the tube-filled complex membrane and the endoplasmic reticulum and later stage sperm [63,64], indicating that IP3R in Sertoli cells participates in the development of tubulobulbar complexes via regulation of actin dynamics, and also indirectly regulates spermatogenesis.
As the hub of calcium signal regulation, IP3R is regulated by upstream stimulating factors or interacting molecules [65], and it also transmits signals to regulate various downstream biological processes. IP3 and many IP3 analogs can activate the IP3R channel. For instance, adenophostins have a stronger affinity for the IP3R channel receptors than IP3 itself [66]. However, 2-O-IP3, another synthetic analog of IP3, showed a weaker effect on IP3R activation than IP3 [67]. As mentioned above, 2-APB is an inhibitor of IP3R channels [68]. Xestospongin C is a reversible and nonspecific IP3R antagonist inhibiting the IP3-induced Ca2+ increase [39]. These inhibitors or agonists can be applied as a tool to determine the roles of the IP3R channel in calcium signaling. Many intracellular molecules, including cAMP [69], NADH [70], and reactive oxygen species (ROS) [71], also modulate IR3R channel activity. In addition, IP3Rs can be regulated by post-translational modification, such as phosphorylation, ubiquitination [72], and transglutaminase-mediated subunit configurations [73]. Nevertheless, how these molecules and post-translational modifications regulate IP3Rs actions in spermatogenesis remains unknown. Furthermore, as mature sperm lack most active transcriptional and translational machinery, the gene expression that normally mediates in vivo functional modulation no longer represents a key factor. Ca2+, cAMP, ROS and post-translational modification of proteins play essential roles in the modulation of a range of physiological activities that are critical for sperm function. Hence, mature sperm provide a good model to investigate the regulatory mechanisms of IP3Rs independent of transcription and translation pathways. Recent studies show the involvement of noncoding RNAs in the IP3R regulatory network and possibly Ca2+ signaling. miR-240 negatively regulates IP3R1 expression [74]. The inhibition or KO of miR-204 increased IP3R1 levels. The lncRNA eosinophil granule ontogeny transcript (EGOT) upregulated IP3R1 levels via formation of a pre-ITPR1/EGOT dsRNA that induced accumulation and enhanced alternative splicing of IP3R1 primary RNA [75]. Furthermore, a large number of miRNAs and lncRNAs are exclusively or highly expressed in the testes and related to spermatogenesis and even male infertility [76,77,78,79,80]. However, to the best of our knowledge, whether these lncRNAs take part in IP3Rs-mediated Ca2+ signal transduction in male reproduction remains undetermined.
To date, more than 100 proteins that interact with IP3R have been found [26]. This diverse set of proteins allows the production of unique spatiotemporal patterns in Ca2+ intracellular signaling to respond to various upstream stimulation factors or different downstream target molecules or events. Such proteins can manage intracellular calcium signals through inhibiting or activating the function of the IP3R channel, transmitting downstream signals to regulate gene expression via interaction proteins, or affecting the distribution of IP3R protein for a cascade amplification effect for weakly stimulated calcium signals [25]. Interaction molecules and upstream/downstream regulatory signals should be further studied to clarify the function of the IP3R channel and associated mechanism of regulation. Some reports showed that IP3R channel interaction proteins are essential in spermatogenesis and the regulation of sperm function, which provides a potential alternative process for IP3R to indirectly affect male reproduction. For example, the loss of IP3R interaction protein TMEM203 disrupted intracellular calcium signals and severely affected spermatogenesis, which resulted in the absence of mature sperm production and sterility [81]. Fyn tyrosine kinase can bind to IP3R and cause phosphorylation at tyrosine 353, which in turn leads to increased sensitivity of the IP3R channel and promotes a long-term increase in calcium signaling [82]. Male mice remained fertile after the loss of Fyn; however, testicular development was abnormal and the quantity of sperm was markedly reduced [83]. The IP3R interaction proteins known to affect male reproduction are listed in Table 1. However, further studies are needed to investigate the interplay between IP3Rs and these proteins in reproductive cells that cause impaired reproduction. Additionally, the functions of other IP3R interaction proteins in spermatogenesis and mature sperm should be examined to fully understand the role of the IP3R channel in male reproduction.

Table 1.
Effect of inositol 1,4,5-trisphosphate receptor (IP3R) interaction proteins on male fertility. AZS, asthenozoospermia.
5. Final Remarks
Well-delineated research and substantial evidence, especially in mammals, are still required to fully understand the significant roles that IP3Rs play in spermatogenesis and the regulation of sperm function. The IP3R channel is diverse because of the heterologous formation of functional channels between various subtypes, and distinct subtypes may compensate for the loss of one type of IP3R. Therefore, there may be no apparent reproductive phenotype in gene KO mice of a single type of IP3R. Considering that mice cannot survive after systemic IP3R1 KO, further studies are needed to elucidate the function and mechanism of the IP3R channel in the reproductive system through tissue-specific KO animal models of IP3R1, and models with specific double or triple KOs of IP3Rs. In the clinical research setting, we should also focus on screening and studying sperm samples with defects in multiple IP3R subtypes. Further investigation into the roles of calcium signaling mediated by this channel in the regulation of mature sperm function will provide insight into the diagnosis and treatment of male infertility. In addition, the crosstalk between IP3R and other Ca2+ stores, pumps or interaction factors, should also be investigated to fully uncover the roles and mechanisms of IP3R in male reproduction.
Author Contributions
Conceptualization, X.Z. (Xiaoning Zhang); methodology, W.Z.; software, X.Z. (Xiaoning Zhang); validation, X.Z. (Xuhui Zeng) and X.Z. (Xuhui Zeng); data curation, R.H. and Y.Z.; writing—X.Z. (Xiaoning Zhang); writing—review and editing, X.Z. (Xuhui Zeng); visualization, Y.Z.; supervision, X.Z. (Xuhui Zeng); project administration, X.Z. (Xuhui Zeng); funding acquisition, X.Z. (Xiaoning Zhang) and X.Z. (Xuhui Zeng). All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (81760283 and 31801238), the China Scholarship Council (201906825011), the National Key Research and Development Program of China (2018YFC1003500) and the Natural Science Foundation of Jiangxi Province (20165BCB18001).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Abbreviations
| IP3R | Inositol 1,4,5-trisphosphate receptor |
| PIP2 | Phosphatidylinositol 4,5-bisphosphate |
| PLC | Phospholipase C |
| 2-APB | 2-aminoethoxydiphenyl borate |
| CDK1 | Cyclin-dependent kinase 1 |
| PKA | Protein kinase A |
| PKG | Protein kinase G |
| CIB1 | Calcium and integrin binding 1 |
| HTT | Huntingtin |
| BRCA1 | Breast cancer 1, early onset |
| cAMP | Cyclic adenosine monophosphate |
| ATP | Adenosine triphosphate |
| TBCs | Tubulobulbar complexes |
| PC2 | Polycystin 2 |
| AZS | Asthenozoospermia |
References
- Finkelstein, M.; Etkovitz, N.; Breitbart, H. Ca2+ signaling in mammalian spermatozoa. Mol. Cell. Endocrinol. 2020, 516, 110953. [Google Scholar] [CrossRef] [PubMed]
- Golpour, A.; Pšenička, M.; Niksirat, H. Subcellular distribution of calcium during spermatogenesis of zebrafish, Danio rerio. J. Morphol. 2017, 278, 1149–1159. [Google Scholar] [CrossRef]
- Golpour, A.; Pšenička, M.; Niksirat, H. Ultrastructural localization of intracellular calcium during spermatogenesis of sterlet (Acipenser ruthenus). Microsc. Microanal. 2016, 22, 1155–1161. [Google Scholar] [CrossRef]
- Abdou, H.S.; Villeneuve, G.; Tremblay, J.J. The calcium signaling pathway regulates Leydig cell steroidogenesis through a transcriptional cascade involving the nuclear receptor NR4A1 and the steroidogenic acute regulatory protein. Endocrinology 2013, 154, 511–520. [Google Scholar] [CrossRef]
- Gorczyńska-Fjälling, E. The role of calcium in signal transduction processes in Sertoli cells. Reprod. Biol. 2004, 4, 219–241. [Google Scholar]
- Harchegani, A.B.; Irandoost, A.; Mirnamniha, M.; Rahmani, H.; Tahmasbpour, E.; Shahriary, A. Possible mechanisms for the effects of calcium deficiency on male infertility. Int. J. Fertil. Steril. 2019, 12, 267–272. [Google Scholar]
- Treviño, C.L.; Santi, C.M.; Beltrán, C.; Hernández-Cruz, A.; Darszon, A.; Lomeli, H. Localisation of inositol trisphosphate and ryanodine receptors during mouse spermatogenesis: Possible functional implications. Zygote 1998, 6, 159–172. [Google Scholar] [CrossRef]
- Ravindranath, N.; Papadopoulos, V.; Vornberger, W.; Zitzmann, D.; Dym, M. Ultrastructural distribution of calcium in the rat testis. Biol. Reprod. 1994, 51, 50–62. [Google Scholar] [CrossRef][Green Version]
- Ma, H.; Zhang, B.L.; Liu, B.Y.; Shi, S.; Zhang, T.C.; Shi, H.J.; Li, Z.; Shum, W.W. Vitamin K2-Dependent GGCX and MGP Are Required for Homeostatic Calcium Regulation of Sperm Maturation. iScience 2019, 14, 210–225. [Google Scholar] [CrossRef]
- Lee, J.; Kim, H.; Kim, D.; Gye, M.C. Effects of calcium channel blockers on the spermatogenesis and gene expression in peripubertal mouse testis. Arch. Androl. 2006, 52, 311–318. [Google Scholar] [CrossRef][Green Version]
- Banjoko, S.O.; Adeseolu, F.O. Seminal plasma pH, inorganic phosphate, total and ionized calcium concentrations in the assessment of human spermatozoa function. J. Clin. Diagn. Res. 2013, 7, 2483–2486. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, M.M.; Behnampour, N.; Nejabat, M.; Tabandeh, A.; Ghazi-Moghaddam, B.; Joshaghani, H.R. Impact of seminal plasma trace elements on human sperm motility parameters. Rom. J. Intern. Med. 2018, 56, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Ammar, O.; Houas, Z.; Mehdi, M. The association between iron, calcium, and oxidative stress in seminal plasma and sperm quality. Environ. Sci. Pollut. Res. 2019, 26, 14097–14105. [Google Scholar] [CrossRef]
- Skandhan, K.P.; Mazumdar, B.; Sumangala, B.; Jaya, V. Seminal plasma calcium in normal and infertile patients. Urologia. 2017, 84, 35–37. [Google Scholar] [CrossRef] [PubMed]
- Böhmer, M.; Van, Q.; Weyand, I.; Hagen, V.; Beyermann, M.; Matsumoto, M.; Hoshi, M.; Hildebrand, E.; Kaupp, U.B. Ca2+ spikes in the flagellum control chemotactic behavior of sperm. EMBO J. 2005, 24, 2741–2752. [Google Scholar] [CrossRef]
- Lishko, P.V.; Mannowetz, N. CatSper: A unique calcium channel of the sperm flagellum. Curr. Opin. Physiol. 2018, 2, 109–113. [Google Scholar] [CrossRef]
- Lestari, S.W.; Miati, D.N.; Seoharso, P.; Sugiyanto, R.; Pujianto, D.A. Sperm Na+, K+-ATPase α4 and plasma membrane Ca2+-ATPase (PMCA) 4 regulation in asthenozoospermia. Syst. Biol. Reprod. Med. 2017, 63, 294–302. [Google Scholar] [CrossRef]
- Olli, K.E.; Li, K.; Galileo, D.S.; Martin-DeLeon, P.A. Plasma membrane calcium ATPase 4 (PMCA4) co-ordinates calcium and nitric oxide signaling in regulating murine sperm functional activity. J. Cell. Physiol. 2018, 233, 11–22. [Google Scholar] [CrossRef]
- Krasznai, Z.; Krasznai, Z.T.; Morisawa, M.; Bazsáné, Z.K.; Hernádi, Z.; Fazekas, Z.; Trón, L.; Goda, K.; Márián, T. Role of the Na+/Ca2+ exchanger in calcium homeostasis and human sperm motility regulation. Cell Motil. Cytoskelet. 2006, 63, 66–76. [Google Scholar] [CrossRef]
- Reddy, P.R.; Patni, A.; Sharma, A.; Gupta, S.; Tiwary, A.K. Effect of 2′, 4′-dichlorobenzamil hydrochloride, a Na+–Ca2+ exchange inhibitor, on human spermatozoa. Eur. J. Pharmacol. 2001, 418, 153–155. [Google Scholar] [CrossRef]
- Sun, X.-H.; Zhu, Y.-Y.; Wang, L.; Liu, H.-L.; Ling, Y.; Li, Z.-L.; Sun, L.-B. The Catsper channel and its roles in male fertility: A systematic review. Reprod. Biol. Endocrinol. 2017, 15, 65. [Google Scholar] [CrossRef]
- Hwang, J.Y.; Mannowetz, N.; Zhang, Y.; Everley, R.A.; Gygi, S.P.; Bewersdorf, J.; Lishko, P.V.; Chung, J.-J. Dual sensing of physiologic pH and calcium by EFCAB9 regulates sperm motility. Cell 2019, 177, 1480–1494. [Google Scholar] [CrossRef]
- Wacquier, B.; Voorsluijs, V.; Combettes, L.; Dupont, G. Coding and decoding of oscillatory Ca2+ signals. Semin. Cell Dev. Biol. 2019, 94, 11–19. [Google Scholar] [CrossRef]
- Yang, J.; Zhao, Z.; Gu, M.; Feng, X.; Xu, H. Release and uptake mechanisms of vesicular Ca2+ stores. Protein Cell 2019, 10, 8–19. [Google Scholar] [CrossRef]
- Prole, D.L.; Taylor, C.W. Inositol 1, 4, 5-trisphosphate receptors and their protein partners as signalling hubs. J. Physiol. 2016, 594, 2849–2866. [Google Scholar] [CrossRef]
- Prole, D.L.; Taylor, C.W. Structure and function of IP3 receptors. Cold Spring Harb. Perspect. Biol. 2019, 11, a035063. [Google Scholar] [CrossRef]
- Baker, M.R.; Fan, G.; Serysheva, I.I. Structure of IP3R channel: High-resolution insights from cryo-EM. Curr. Opin. Struct. Biol. 2017, 46, 38–47. [Google Scholar] [CrossRef]
- Joseph, S.K.; Lin, C.; Pierson, S.; Thomas, A.P.; Maranto, A.R. Heteroligomers of type-I and type-III inositol trisphosphate receptors in WB rat liver epithelial cells. J. Biol. Chem. 1995, 270, 23310–23316. [Google Scholar] [CrossRef]
- Parys, J.B.; Vervliet, T. New Insights in the IP 3 Receptor and Its Regulation. Adv. Exp. Med. Biol. 2020, 1131, 243–270. [Google Scholar]
- Fan, G.; Baker, M.L.; Wang, Z.; Baker, M.R.; Sinyagovskiy, P.A.; Chiu, W.; Ludtke, S.J.; Serysheva, I.I. Gating machinery of InsP3R channels revealed by electron cryomicroscopy. Nature 2015, 527, 336–341. [Google Scholar] [CrossRef]
- Paknejad, N.; Hite, R.K. Structural basis for the regulation of inositol trisphosphate receptors by Ca2+ and IP 3. Nat. Struct. Mol. Biol. 2018, 25, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Maes, K.; Missiaen, L.; De Smet, P.; Vanlingen, S.; Callewaert, G.; Parys, J.; De Smedt, H. Differential modulation of inositol 1, 4, 5-trisphosphate receptor type 1 and type 3 by ATP. Cell Calcium 2000, 27, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.; Wang, Z.; Bezprozvanny, I. Modulation of mammalian inositol 1, 4, 5-trisphosphate receptor isoforms by calcium: A role of calcium sensor region. Biophys. J. 2005, 88, 1056–1069. [Google Scholar] [CrossRef] [PubMed]
- Betzenhauser, M.J.; Wagner, L.E.; Iwai, M.; Michikawa, T.; Mikoshiba, K.; Yule, D.I. ATP modulation of Ca2+ release by Type-2 and Type-3 inositol (1, 4, 5)-triphosphate receptors differing ATP sensitivities and molecular determinants of action. J. Biol. Chem. 2008, 283, 21579–21587. [Google Scholar] [CrossRef]
- Khan, S.A.; Rossi, A.M.; Riley, A.M.; Potter, B.V.; Taylor, C.W. Subtype-selective regulation of IP3 receptors by thimerosal via cysteine residues within the IP3-binding core and suppressor domain. Biochem. J. 2013, 451, 177–184. [Google Scholar] [CrossRef][Green Version]
- Alzayady, K.J.; Wang, L.; Chandrasekhar, R.; Wagner, L.E.; Van Petegem, F.; Yule, D.I. Defining the stoichiometry of inositol 1, 4, 5-trisphosphate binding required to initiate Ca2+ release. Sci. Signal. 2016, 9, ra35. [Google Scholar] [CrossRef]
- Lyon, K.; Asghari, P.; Scriven, D.R.; Moore, E.D.; Vogl, A.W. IP3R is localized to ER-PM contact sites at unique endocytic structures involved in intercellular junction turnover events critical to spermatogenesis. FASEB J. 2017, 31, 741–745. [Google Scholar]
- Correia, J.; Michelangeli, F.; Publicover, S. Regulation and roles of Ca2+ stores in human sperm. Reproduction 2015, 150, R65–R76. [Google Scholar] [CrossRef]
- Gugssa, A.; Williams, A.; Tilahun, R.; Eckberg, W.; Anderson, W.; Ahluwalia, B.; Kaul, L.; Broomfield, D. Localization of guanylate cyclase receptor, inositol trisphosphate receptor, and calmodulin in boar spermatozoa. Int. J. Biol. 2010, 2, 13–18. [Google Scholar] [CrossRef]
- Minelli, A.; Allegrucci, C.; Rosati, R.; Mezzasoma, I. Molecular and binding characteristics of IP3 receptors in bovine spermatozoa. Mol. Reprod. Dev. 2000, 56, 527–533. [Google Scholar] [CrossRef]
- Zapata, O.; Ralston, J.; Beltraán, C.; Parys, J.B.; Chen, J.L.; Longo, F.J.; Darszon, A. Inositol triphosphate receptors in sea urchin sperm. Zygote 1997, 5, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.-C.; Suarez, S.S. An inositol 1, 4, 5-trisphosphate receptor-gated intracellular Ca2+ store is involved in regulating sperm hyperactivated motility. Biol. Reprod. 2001, 65, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Naaby-Hansen, S.; Wolkowicz, M.J.; Klotz, K.; Bush, L.A.; Westbrook, V.A.; Shibahara, H.; Shetty, J.; Coonrod, S.A.; Reddi, P.P.; Shannon, J. Co-localization of the inositol 1, 4, 5-trisphosphate receptor and calreticulin in the equatorial segment and in membrane bounded vesicles in the cytoplasmic droplet of human spermatozoa. Mol. Hum. Reprod. 2001, 7, 923–933. [Google Scholar] [CrossRef]
- Nguyen, T.M.D.; Duittoz, A.; Praud, C.; Combarnous, Y.; Blesbois, E. Calcium channels in chicken sperm regulate motility and the acrosome reaction. FEBS J. 2016, 283, 1902–1920. [Google Scholar] [CrossRef]
- Kuroda, Y.; Kaneko, S.; Yoshimura, Y.; Nozawa, S.; Mikoshiba, K. Are there inositol 1,4,5-triphosphate (IP3) receptors in human sperm? Life Sci. 1999, 65, 135–143. [Google Scholar] [CrossRef]
- Bartok, A.; Weaver, D.; Golenár, T.; Nichtova, Z.; Katona, M.; Bánsághi, S.; Alzayady, K.J.; Thomas, V.K.; Ando, H.; Mikoshiba, K. IP 3 receptor isoforms differently regulate ER-mitochondrial contacts and local calcium transfer. Nat. Commun. 2019, 10, 3726. [Google Scholar] [CrossRef]
- Taraschi, A.; Cimini, C.; Capacchietti, G.; Ramal-Sanchez, M.; Valbonetti, L.; Machado-Simoes, J.; Moussa, F.; Tagaram, I.; Mokh, S.; Al Iskandarani, M. Two-Player Game in a Complex Landscape: 26S Proteasome, PKA, and Intracellular Calcium Concentration Modulate Mammalian Sperm Capacitation by Creating an Integrated Dialogue—A Computational Analysis. Int. J. Mol. Sci. 2020, 21, 6256. [Google Scholar] [CrossRef] [PubMed]
- Gower, N.J.; Walker, D.S.; Baylis, H.A. Inositol 1, 4, 5-trisphosphate signaling regulates mating behavior in Caenorhabditis elegans males. Mol. Biol. Cell 2005, 16, 3978–3986. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wong, R.; Hadjiyanni, I.; Wei, H.-C.; Polevoy, G.; McBride, R.; Sem, K.-P.; Brill, J.A. PIP2 Hydrolysis and Calcium Release Are Required for Cytokinesis in Drosophila Spermatocytes. Curr. Biol. 2005, 15, 1401–1406. [Google Scholar] [CrossRef] [PubMed]
- Lefièvre, L.; Nash, K.; Mansell, S.; Costello, S.; Punt, E.; Correia, J.; Morris, J.; Kirkman-Brown, J.; Wilson, S.M.; Barratt, C.L. 2-APB-potentiated channels amplify CatSper-induced Ca2+ signals in human sperm. Biochem. J. 2012, 448, 189–200. [Google Scholar] [CrossRef]
- Walensky, L.D.; Snyder, S.H. Inositol 1, 4, 5-trisphosphate receptors selectively localized to the acrosomes of mammalian sperm. J. Cell Biol. 1995, 130, 857–869. [Google Scholar] [CrossRef] [PubMed]
- Llanos, M.N. Thapsigargin stimulates acrosomal exocytosis in hamster spermatozoa. Mol. Reprod. Dev. 1998, 51, 84–91. [Google Scholar] [CrossRef]
- Meizel, S.; Turner, K.O. Initiation of the human sperm acrosome reaction by thapsigargin. J. Exp. Zool. 1993, 267, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Fujinoki, M. Progesterone-enhanced sperm hyperactivation through IP3–PKC and PKA signals. Reprod. Med. Biol. 2013, 12, 27–33. [Google Scholar] [CrossRef]
- Bahat, A.; Eisenbach, M. Human sperm thermotaxis is mediated by phospholipase C and inositol trisphosphate receptor Ca2+ channel. Biol. Reprod. 2010, 82, 606–616. [Google Scholar] [CrossRef]
- Li, Y.-Y.; Jia, Y.-P.; Duan, L.-Y.; Li, K.-M. Participation of the inositol 1, 4, 5-trisphosphate-gated calcium channel in the zona pellucida-and progesterone-induced acrosome reaction and calcium influx in human spermatozoa. Asian J. Androl. 2020, 22, 192–199. [Google Scholar] [CrossRef]
- Swann, K. The soluble sperm factor that activates the egg: PLCzeta and beyond. Reproduction 2020, 160, V9–V11. [Google Scholar] [CrossRef]
- Van de Leemput, J.; Chandran, J.; Knight, M.A.; Holtzclaw, L.A.; Scholz, S.; Cookson, M.R.; Houlden, H.; Gwinn-Hardy, K.; Fung, H.-C.; Lin, X. Deletion at ITPR1 underlies ataxia in mice and spinocerebellar ataxia 15 in humans. PLoS Genet. 2007, 3, e108. [Google Scholar] [CrossRef]
- Matsumoto, M.; Nakagawa, T.; Inoue, T.; Nagata, E.; Tanaka, K.; Takano, H.; Kuno, J.; Sakakibara, S.; Yamada, M.; Yoneshima, H. Ataxia and epileptic seizures in mice lacking type 1 inositol 1, 4, 5-trisphosphate receptor. Nature 1996, 379, 168–171. [Google Scholar] [CrossRef]
- Guerra-Gomes, S.; Cunha-Garcia, D.; Marques Nascimento, D.S.; Duarte-Silva, S.; Loureiro-Campos, E.; Morais Sardinha, V.; Viana, J.F.; Sousa, N.; Maciel, P.; Pinto, L. IP3R2 null mice display a normal acquisition of somatic and neurological development milestones. Eur. J. Neurosci. 2020. [Google Scholar] [CrossRef]
- Adams, A.; Vogl, A.W. IP3R, TRPM6 and Homer1 are Localized to ER-PM Contact Sites at Tubulobulbar Complexes in Rat Testis. FASEB J. 2017, 31, 741–744. [Google Scholar]
- Lyon, K.; Adams, A.; Piva, M.; Asghari, P.; Moore, E.D.; Vogl, A.W. Ca2+ signaling machinery is present at intercellular junctions and structures associated with junction turnover in rat Sertoli cells. Biol. Reprod. 2017, 96, 1288–1302. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Adams, A.; Vogl, W. Knockdown of IP3R1 Disrupts TBC-ER Contact Sites and the Morphology of Apical Processes Encapsulating Late Spermatids. Biol. Reprod. 2020, 21, 669–680. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Vogl, W. In Vivo Knockdown of the IP3R1 Calcium Channel Disrupts ER and Actin Morphology, as well as TBC Bulb Maturation in the Apical Processes of Sertoli Cells in Rat Testes. FASEB J. 2019, 33, 610.7. [Google Scholar]
- Ivanova, H.; Vervliet, T.; Monaco, G.; Terry, L.E.; Rosa, N.; Baker, M.R.; Parys, J.B.; Serysheva, I.I.; Yule, D.I.; Bultynck, G. Bcl-2-Protein Family as Modulators of IP3 Receptors and Other Organellar Ca2+ Channels. Cold Spring Harb. Perspect. Biol. 2020, 12, a035089. [Google Scholar] [CrossRef]
- Rossi, A.M.; Riley, A.M.; Potter, B.V.; Taylor, C.W. Adenophostins: High-affinity agonists of IP3 receptors. Curr. Top. Membr. 2010, 66, 209–233. [Google Scholar]
- Rossi, A.M.; Riley, A.M.; Tovey, S.C.; Rahman, T.; Dellis, O.; Taylor, E.J.; Veresov, V.G.; Potter, B.V.; Taylor, C.W. Synthetic partial agonists reveal key steps in IP 3 receptor activation. Nat. Chem. Biol. 2009, 5, 631–639. [Google Scholar] [CrossRef]
- Rosalez, M.; Estevez-Fregoso, E.; Alatorre, A.; Abad-García, A.A.; Soriano-Ursúa, M. 2-aminoethyldiphenyl borinate: A multitarget compound with potential as a drug precursor. Curr. Mol. Pharmacol. 2020, 13, 57–75. [Google Scholar] [CrossRef]
- Taylor, C.W. Regulation of IP3 receptors by cyclic AMP. Cell Calcium 2017, 63, 48–52. [Google Scholar] [CrossRef]
- Patterson, R.L.; van Rossum, D.B.; Kaplin, A.I.; Barrow, R.K.; Snyder, S.H. Inositol 1, 4, 5-trisphosphate receptor/GAPDH complex augments Ca2+ release via locally derived NADH. Proc. Natl. Acad. Sci. USA 2005, 102, 1357–1359. [Google Scholar] [CrossRef]
- Mangla, A.; Guerra, M.T.; Nathanson, M.H. Type 3 inositol 1, 4, 5-trisphosphate receptor: A calcium channel for all seasons. Cell Calcium 2020, 85, 102132. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.; Wojcikiewicz, R. Inositol 1, 4, 5-trisphosphate receptor ubiquitination. Prog. Mol. Biol. Transl. Sci. 2016, 141, 141–159. [Google Scholar] [PubMed]
- Hamada, K.; Terauchi, A.; Nakamura, K.; Higo, T.; Nukina, N.; Matsumoto, N.; Hisatsune, C.; Nakamura, T.; Mikoshiba, K. Aberrant calcium signaling by transglutaminase-mediated posttranslational modification of inositol 1, 4, 5-trisphosphate receptors. Proc. Natl. Acad. Sci. USA 2014, 111, E3966–E3975. [Google Scholar] [CrossRef] [PubMed]
- Gabani, M.; Liu, J.; Ait-Aissa, K.; Koval, O.; Kim, Y.-R.; Castañeda, D.; Vikram, A.; Jacobs, J.S.; Grumbach, I.; Trebak, M.; et al. MiR-204 regulates type 1 IP3R to control vascular smooth muscle cell contractility and blood pressure. Cell Calcium 2019, 80, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Wang, P.; Zhang, J.; Wu, H.; Sui, S.; Zhang, J.; Wang, Q.; Qiao, K.; Yang, W.; Xu, H. Ai-lncRNA EGOT enhancing autophagy sensitizes paclitaxel cytotoxicity via upregulation of ITPR1 expression by RNA-RNA and RNA-protein interactions in human cancer. Mol. Cancer 2019, 18, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Maleki, B.; Shabani, S.; Vallian Borojeni, S. The role of miRNA in spermatogenesis and male infertility. Lab. Diagn. 2018, 10, 48–55. [Google Scholar]
- Wen, K.; Yang, L.; Xiong, T.; Di, C.; Ma, D.; Wu, M.; Xue, Z.; Zhang, X.; Long, L.; Zhang, W. Critical roles of long noncoding RNAs in Drosophila spermatogenesis. Genome Res. 2016, 26, 1233–1244. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, P.; Song, D.; Xiong, S.; Zhang, H.; Fu, J.; Gao, F.; Chen, H.; Zeng, X. Expression profiles and characteristics of human lncRNA in normal and asthenozoospermia sperm. Biol. Reprod. 2019, 100, 982–993. [Google Scholar] [CrossRef]
- Lewandowski, J.P.; Dumbović, G.; Watson, A.R.; Hwang, T.; Jacobs-Palmer, E.; Chang, N.; Much, C.; Turner, K.M.; Kirby, C.; Rubinstein, N.D. The Tug1 lncRNA locus is essential for male fertility. Genome Biol. 2020, 21, 1–35. [Google Scholar] [CrossRef]
- Chen, X.; Li, X.; Guo, J.; Zhang, P.; Zeng, W. The roles of microRNAs in regulation of mammalian spermatogenesis. J. Anim. Sci. Biotechnol. 2017, 35, 1–8. [Google Scholar] [CrossRef]
- Shambharkar, P.B.; Bittinger, M.; Latario, B.; Xiong, Z.; Bandyopadhyay, S.; Davis, V.; Lin, V.; Yang, Y.; Valdez, R.; Labow, M.A. TMEM203 Is a Novel Regulator of Intracellular Calcium Homeostasis and Is Required for Spermatogenesis. PLoS ONE 2015, 10, e0127480. [Google Scholar] [CrossRef] [PubMed]
- Cui, J.; Matkovich, S.J.; deSouza, N.; Li, S.; Rosemblit, N.; Marks, A.R. Regulation of the type 1 inositol 1, 4, 5-trisphosphate receptor by phosphorylation at tyrosine 353. J. Biol. Chem. 2004, 279, 16311–16316. [Google Scholar] [CrossRef] [PubMed]
- Maekawa, M.; Toyama, Y.; Yasuda, M.; Yagi, T.; Yuasa, S. Fyn tyrosine kinase in Sertoli cells is involved in mouse spermatogenesis. Biol. Reprod. 2002, 66, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Gopinathan, L.; Szmyd, R.; Low, D.; Diril, M.K.; Chang, H.-Y.; Coppola, V.; Liu, K.; Tessarollo, L.; Guccione, E.; van Pelt, A.M. Emi2 is essential for mouse spermatogenesis. Cell Rep. 2017, 20, 697–708. [Google Scholar] [CrossRef]
- Kania, E.; Roest, G.; Vervliet, T.; Parys, J.B.; Bultynck, G. IP3 receptor-mediated calcium signaling and its role in autophagy in cancer. Front. Oncol. 2017, 7, 140. [Google Scholar] [CrossRef]
- Yin, J.; Ni, B.; Yang, Y.-D.; Tang, Z.-W.; Gao, Z.-Q.; Feng, L.; Liao, W.-G.; Gao, Y.-Q. Elevation of autophagy rescues spermatogenesis by inhibiting apoptosis of mouse spermatocytes. Reproduction 2018, 156, 545–558. [Google Scholar] [CrossRef]
- Zhao, B. Regulation of cell survival by CIB1, a new modulator of 3-phosphoinositide-dependent protein kinase 1 (PDK1). Diss. Theses Gradworks 2007, 21. [Google Scholar] [CrossRef]
- Wang, X.; Peng, X.; Zhang, X.; Xu, H.; Lu, C.; Liu, L.; Song, J.; Zhang, Y. The emerging roles of CIB1 in cancer. Cell. Physiol. Biochem. 2017, 43, 1413–1424. [Google Scholar] [CrossRef]
- Yuan, W.; Leisner, T.M.; McFadden, A.W.; Clark, S.; Hiller, S.; Maeda, N.; O’Brien, D.A.; Parise, L.V. CIB1 is essential for mouse spermatogenesis. Mol. Cell. Biol. 2006, 26, 8507–8514. [Google Scholar] [CrossRef]
- Skaålhegg, B.S.; Huang, Y.; Su, T.; Idzerda, R.L.; McKnight, G.S.; Burton, K.A. Mutation of the Cα subunit of PKA leads to growth retardation and sperm dysfunction. Mol. Endocrinol. 2002, 16, 630–639. [Google Scholar] [CrossRef]
- Hedlund, P.; Aszódi, A.; Pfeifer, A.; Alm, P.; Hofmann, F.; Ahmad, M.; Fässler, R.; Andersson, K.-E. Erectile dysfunction in cyclic GMP-dependent kinase I-deficient mice. Proc. Natl. Acad. Sci. USA 2000, 97, 2349–2354. [Google Scholar] [CrossRef] [PubMed]
- Szado, T.; Vanderheyden, V.; Parys, J.B.; De Smedt, H.; Rietdorf, K.; Kotelevets, L.; Chastre, E.; Khan, F.; Landegren, U.; Söderberg, O. Phosphorylation of inositol 1, 4, 5-trisphosphate receptors by protein kinase B/Akt inhibits Ca2+ release and apoptosis. Proc. Natl. Acad. Sci. USA 2008, 105, 2427–2432. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.S.; Xu, P.-Z.; Gottlob, K.; Chen, M.-L.; Sokol, K.; Shiyanova, T.; Roninson, I.; Weng, W.; Suzuki, R.; Tobe, K. Growth retardation and increased apoptosis in mice with homozygous disruption of the Akt1 gene. Genes Dev. 2001, 15, 2203–2208. [Google Scholar] [CrossRef] [PubMed]
- Tang, T.-S.; Tu, H.; Chan, E.Y.; Maximov, A.; Wang, Z.; Wellington, C.L.; Hayden, M.R.; Bezprozvanny, I. Huntingtin and huntingtin-associated protein 1 influence neuronal calcium signaling mediated by inositol-(1, 4, 5) triphosphate receptor type 1. Neuron 2003, 39, 227–239. [Google Scholar] [CrossRef]
- Dragatsis, I.; Levine, M.S.; Zeitlin, S. Inactivation of Hdh in the brain and testis results in progressive neurodegeneration and sterility in mice. Nat. Genet. 2000, 26, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Hedgepeth, S.C.; Garcia, M.I.; Wagner, L.E.; Rodriguez, A.M.; Chintapalli, S.V.; Snyder, R.R.; Hankins, G.D.; Henderson, B.R.; Brodie, K.M.; Yule, D.I. The BRCA1 tumor suppressor binds to inositol 1, 4, 5-trisphosphate receptors to stimulate apoptotic calcium release. J. Biol. Chem. 2015, 290, 7304–7313. [Google Scholar] [CrossRef]
- Xu, X.; Aprelikova, O.; Moens, P.; Deng, C.-X.; Furth, P.A. Impaired meiotic DNA-damage repair and lack of crossing-over during spermatogenesis in BRCA1 full-length isoform deficient mice. Development 2003, 130, 2001–2012. [Google Scholar] [CrossRef]
- Conti, V.; Aghaie, A.; Cilli, M.; Martin, N.; Caridi, G.; Musante, L.; Candiano, G.; Castagna, M.; Fairen, A.; Ravazzolo, R. crv4, a mouse model for human ataxia associated with kyphoscoliosis caused by an mRNA splicing mutation of the metabotropic glutamate receptor 1 (Grm1). Int. J. Mol. Med. 2006, 18, 593–600. [Google Scholar] [CrossRef]
- Shin, D.M.; Zhao, X.-S.; Zeng, W.; Mozhayeva, M.; Muallem, S. The mammalian Sec6/8 complex interacts with Ca2+ signaling complexes and regulates their activity. J. Cell Biol. 2000, 150, 1101–1112. [Google Scholar] [CrossRef]
- Ballester, M.; Molist, J.; Lopez-Bejar, M.; Sánchez, A.; Santaló, J.; Folch, J.M.; Ibáñez, E. Disruption of the mouse phospholipase C-β1 gene in a β-lactoglobulin transgenic line affects viability, growth, and fertility in mice. Gene 2004, 341, 279–289. [Google Scholar] [CrossRef]
- Lur, G.; Sherwood, M.W.; Ebisui, E.; Haynes, L.; Feske, S.; Sutton, R.; Burgoyne, R.D.; Mikoshiba, K.; Petersen, O.H.; Tepikin, A.V. Ins P 3 receptors and Orai channels in pancreatic acinar cells: Co-localization and its consequences. Biochem. J. 2011, 436, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.M.; Goulding, E.H.; D’Agostin, D.M.; Janardhan, K.S.; Cummings, C.A.; Bird, G.S.; Eddy, E.M.; Putney, J.W. Male infertility in mice lacking the store-operated Ca2+ channel Orai1. Cell Calcium 2016, 59, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Brill, A.L.; Ehrlich, B.E. Polycystin 2: A calcium channel, channel partner, and regulator of calcium homeostasis in ADPKD. Cell. Signal 2020, 66, 109490. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.-T.; Chiou, Y.-Y.; Wang, E.; Lin, H.-K.; Lin, Y.-T.; Chi, Y.-C.; Wang, C.-K.L.; Tang, M.-J.; Li, H. Defining a link with autosomal-dominant polycystic kidney disease in mice with congenitally low expression of Pkd1. Am. J. Pathol. 2006, 168, 205–220. [Google Scholar] [CrossRef]
- Basso, V.; Marchesan, E.; Ziviani, E. A trio has turned into a quartet: DJ-1 interacts with the IP3R-Grp75-VDAC complex to control ER-mitochondria interaction. Cell Calcium 2020, 87, 102186. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, Y.; Zhao, X.; Yuan, R.; Jiang, H.; Pu, X. Downregulation of DJ-1 fails to protect mitochondrial complex I subunit NDUFS3 in the testes and contributes to the asthenozoospermia. Mediat. Inflamm. 2018, 2018, 6133075. [Google Scholar] [CrossRef]
- Jahantigh, D.; Colagar, A.H.; Salimi, S. Genetic polymorphisms and haplotypes of the DJ-1 gene promoter associated with the susceptibility to male infertility. J. Assist. Reprod. Genet. 2017, 34, 1673–1682. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).