Abstract
This paper reviews current treatments for renal cell carcinoma/cancer (RCC) with the multikinase inhibitors (MKIs) sorafenib, sunitinib, lenvatinib and axitinib. Furthermore, it compares these drugs regarding progression-free survival, overall survival and adverse effects (AE), with a focus on hypertension. Sorafenib and sunitinib, which are included in international clinical guidelines as first- and second-line therapy in metastatic RCC, are now being challenged by new-generation drugs like lenvatinib and axitinib. These drugs have shown significant clinical benefits for patients with RCC, but all four induce a variety of AEs. Hypertension is one of the most common AEs related to MKI treatment. Comparing sorafenib, sunitinib and lenvatinib revealed that sorafenib and sunitinib had the same efficacy, but sorafenib was safer to use. Lenvatinib showed better efficacy than sorafenib but worse safety. No trials have yet been completed that compare lenvatinib with sunitinib. Although axitinib promotes slightly higher hypertension rates compared to sunitinib, the overall discontinuation rate and cardiovascular complications are favourable. Although the mean rate of patients who develop hypertension is similar for each drug, some trials have shown large differences, which could indicate that lifestyle and/or genetic factors play an additional role.
1. Introduction
Hypertension is a highly prevalent and serious disease. “The 2018 ESC/ESH Guidelines for the management of arterial hypertension” [1] defined hypertension as a systolic blood pressure (SBP) ≥ 140 mmHg and a diastolic blood pressure (DBP) ≥ 90 mmHg. This condition can lead to cardiovascular diseases with fatal results [2,3].
In patients with renal cell carcinoma/cancer (RCC), new developments in targeting therapy, such as multikinase inhibitors (MKIs), have shown an improvement in progression-free survival (PFS) and overall survival (OS), and thereby an increase in the quality of life. Unfortunately, MKIs also induce numerous adverse effects (AEs), of which hypertension is a frequent occurrence [4,5,6]. Sorafenib, sunitinib, lenvatinib and axitinib are of great interest, and recent and ongoing trials are investigating these MKIs for treating RCC, with a focus on high-efficacy measures as well as optimal safety.
2. Methods
The literature for this review was mainly found online at PubMed [7] and ClinicalTrials [8]. The keywords searched in the literature included “Sorafenib”, “Sunitinib”, Lenvatinib”, Axitinib”, “RCC”, “renal cell carcinoma”, “renal cell cancer” and “hypertension”. The keywords were entered individually or linked together with the Boolean operator “AND”.
The following keywords were searched in PubMed: “Sorafenib AND RCC/renal cell carcinoma/renal cell cancer” returned 606/1600/1662 results; “Sorafenib AND hypertension” gave 478 results, “Sunitinib AND RCC/renal cell carcinoma/renal cell cancer” returned 912/2655/2714 results; “Sunitinib AND hypertension” provided 461 results; “Lenvatinib AND RCC/renal cell carcinoma/renal cell cancer” generated 26/72/74 results; “Lenvatinib AND hypertension” returned 78 results; “Axitinib AND RCC/renal cell carcinoma/renal cell cancer” returned 154/498/509 results; “Axitinib AND hypertension” provided 133 results (last accessed on 19 August 2019).
3. Renal Cell Carcinoma
3.1. Definition
In 2018, kidney cancer was the fourteenth most common cancer type worldwide [9,10], with an incidence rate of 406,262 new cases and 175,098 deaths per year. RCC is responsible for up to 85% of all renal neoplasms [11,12]. RCC development is linked to multiple risk factors; age and gender are strongly related to its development. The disease is more frequent in men, and the incidence rate peaks at 60–70 years of age [13]. In the early stages of RCC with a tumour size less than 30 mm, the disease is often asymptomatic and typically located by coincidence during a radiological examination. When the tumour grows larger than 30 mm, the patients may have symptoms such as fever, fatigue, weight loss, haematuria, flank mass, back pain, anaemia and high calcium levels [11].
RCC comprises a heterogenous group of tumours originating from the tubular epithelium in the kidney [9]. There are more than 10 histological RCC subtypes (Table 1). With >80% of all renal tumours, the clear cell RCC (ccRCC) represents the most common histological RCC subtype [12]. ccRCC is a highly vascular tumour characterized by malignant epithelial cells with clear cytoplasm and a compact growth pattern [14,15]. Due to its resistance to standard chemo- and radiotherapies, it has been considered as the most aggressive histological type of RCC [16]. Especially patients with metastatic ccRCC have a worse prognosis [17]. Papillary RCC (pRCC) is the second most common RCC subtype, and accounts for 10–15% of renal cortical neoplasms. pRCC tumours either show a hypovascular (tubulo)papillary architecture composed of a single layered small cell and scanty cytoplasm (type 1), or are characterized by pseudostratified large cells and an eosinophilic cytoplasm (type 2). pRCC is generally associated with a favourable outcome. Type 1 pRCC seems to have a better prognosis than type 2, but there is still no consensus regarding the standard treatment for metastatic pRCC although multiple gene mutations in pRCC could serve as a basis for targeted therapies [18]. First-line therapy for metastatic pRCC and metastatic ccRCC is generally similar. Treatment with antiangiogenic drugs such as bevacizumab, sunitinib or sorafenib could increase the progression-free survival in patients with both subtypes [19,20], although patients suffering from ccRCC showed a better response to antiangiogenic drugs [21].

Table 1.
Classification of histological renal cell carcinoma (RCC) subtypes (modified from Randall [12]).
Tumourigenesis for ccRCC is highly associated with hereditary von Hippel-Lindau (VHL) disease, where the VHL tumour suppressor gene is inactivated. This change leads to lower amounts of pVHL protein and pVHL-containing protein complexes, which normally inhibit hypoxia-inducible factor (HIF). Physiologically, HIF acts as a transcription factor that upregulates the expression of vascular endothelial growth factor (VEGF), platelet-derived growth factor beta (PDGF-β) and transforming growth factor alpha [12,22,23]. These factors bind to tyrosine kinase receptors (RTKs) on the cell surface—an action that results in an intracellular activation of the Ras/Raf/mitogen activated protein kinase (MEK)/extracellular-regulated kinase (ERK) and phosphoinositide 3-kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR) pathways. This activation favours the angiogenesis, survival, proliferation, differentiation and mobility of the cells. Thereby, all the essential factors for developing a tumour are fulfilled [24] (Figure 1).
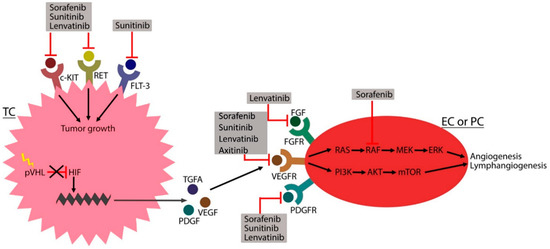
Figure 1.
The tumorigenesis of renal cell carcinoma. VHL mutation (yellow lightning flash) reduces the amount of von Hippel Lindau protein (pVHL), and thus hypoxia-inducible factor (HIF) production is not inhibited (black cross). HIF binds the DNA (green zigzag line) and upregulates the transcription of transforming growth factor α (TGFA), vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF), which stimulate receptor tyrosine kinases (RTKs) on the endothelial cell (EC) or pericyte (PC) to promote angiogenesis and lymphangiogenesis. RTK activation on the tumour cell (TC) results in tumour growth. Multikinase inhibitors (MKIs), including sorafenib, sunitinib, lenvatinib and axitinib, target these RTKs to inhibit tumorigenesis. Abbreviations: FGF (fibroblast growth factor), FGFR (fibroblast growth factor receptor), VEGFR (vascular endothelial growth factor receptor), PDGFR (platelet-derived growth factor receptor), RAS (rat sarcoma), RAF (rapidly accelerated fibrosarcoma kinase), MEK (mitogen activated protein kinase), ERK (extracellular signal-regulated kinase), PI3K (phosphoinositide 3-kinase), AKT (protein kinase B), mTOR (mammalian targeted of rapamycin), c-KIT (stem cell factor receptor), RET (rearranged during transfection), FLT-3 (FMS-like tyrosine kinase 3). Arrows indicate direct relationships.
3.2. Current Treatment Options
RCC management is based on TNM staging and pathological changes in the disease. The T describes the tumour size and the N the spread to regional lymph nodes. The M describes whether the tumour has metastasised [9,11]. Pathological gradation is ascertained by examining the cytological and histological changes found in a renal specimen. Surgical excision, either partial or radical nephrectomy, is the treatment of choice for patients with a surgically resectable RCC (Table 2). Targeted therapy and/or immunotherapy is the treatment of choice for patients with inoperable or metastatic RCC (mRCC; Table 3). RCC is resistant to chemotherapy, and thus targeted therapies are crucial [9].

Table 2.
Surgical treatment for renal cell carcinoma [9].

Table 3.
Medical management of renal cell carcinoma [4,24,25,26,27,28].
3.3. MKIs in the Treatment of RCC
The signalling and coordination of cellular processes is initiated by protein kinases that regulate protein phosphorylation and thereby affect the location, interaction and activity of bioactive molecules. Dysregulation of the protein kinases may introduce dramatic changes in cellular processes that, in the worst case, may lead to the development of cancer or other diseases. Cancer treatment is therefore often targeted against these protein kinases, which are involved in proliferation, differentiation, cell cycle, apoptosis and angiogenesis [29]. MKIs are drugs that target multiple types of protein kinases, including vascular epithelial growth factor receptor (VEGFR), platelet-derived growth factor receptor (PDGFR), stem cell factor receptor (c-KIT) and others [4,30,31]. Signalling inhibition is initiated by drug binding to the RTK—an action that either blocks the binding site for ATP and peptide substrates or the recruitment sites of the downstream signalling substrate proteins [32]. Unfortunately, some MKIs induce AEs that negatively affect the quality of the patient’s life. One of these effects is hypertension [9].
3.3.1. The Adverse Effect Hypertension
When treating RCC patients with MKIs, one of the most common AEs is hypertension (Table 4).

Table 4.
Adverse effects of the multikinase inhibitors sunitinib, sorafenib, lenvatinib and axitinib [33,34,35,36].
When using MKIs to treat a broad range of cancers, high rates of treatment-induced hypertension have been reported [37,38,39]. The definition of hypertension is an SBP ≥ 140 mmHg and a DBP ≥ 90 mmHg [1,40]. Primary/essential hypertension accounts for 95% of all cases. The overall mechanism of developing this type is unknown, but it can be influenced by obesity, amount of physical activity, arterial natriuretic peptide and the baroreflex. Secondary hypertension accounts for 5% of all hypertension cases and is caused by renal or endocrine factors (known mechanism). Hypertension is divided into categories depending on its severity [3].
Untreated hypertension is a risk factor for developing cardiovascular diseases, including stable and unstable angina, subarachnoid/intracerebral haemorrhage, myocardial infarction, heart failure, sudden cardiac death, ischaemic stroke and peripheral arterial disease, all of which show a high mortality rate [2].
Hypertension management can be achieved by either non-pharmacological or pharmacological therapy. Non-pharmacological therapy involves lifestyle changes, which focus on lower salt intake, reduced alcohol consumption, normalisation of the body mass index, no cigarette smoking and increased physical activity. If no effect is seen after six months, pharmacological therapy is warranted. For half of all patients with hypertension, non-pharmacological therapy may be able to normalise blood pressure.
Pharmacological therapy has an important role in hypertension management and treatment. Currently, five classes of antihypertensive therapy are recommended: angiotensin-converting enzyme inhibitors, angiotensin II receptor subtype 1 receptor inhibitors, β-adrenoreceptor antagonists, diuretics and calcium antagonists. If treatment produces no effect, the dose can be increased or another drug or a combination of multiple drugs can be used. Both mono- and combined therapies must be frequently controlled. After the required effect, the treatment can be reduced until discontinuation, but in most cases a lifelong therapy is needed [3].
3.3.2. Induction of Hypertension
The mechanism of how MKIs induce hypertension is not fully known and was recently reviewed elsewhere [39]. One explanation of how hypertension is induced is based on the production of nitric oxide (NO). Under normal conditions, binding of VEGF to VEGFR-2 on endothelial cells (ECs) results in NO production. NO diffuses to vascular smooth muscle cells (VSMCs), where it induces vasorelaxation by stimulating guanylate cyclase. VEGFR-1+2 stimulation also results in prostacyclin (PGI2) synthesis, which also causes vasorelaxation in VSMCs via adenylate cyclase activation [41,42]. Blocking VEGFR decreases NO and PGI2 synthesis and causes vasoconstriction [41]. Inhibiting VEGFRs will also increase the circulating endothelin-1 (ET-1) concentration—a change that promotes vasoconstriction. Another condition that can lead to hypertension is capillary rarefaction, a reduction in vessel density that increases vascular resistance and BP [40,41]. All these mechanisms promote vasoconstriction and will increase peripheral vascular resistance, ultimately leading to hypertension [43] (Figure 2).
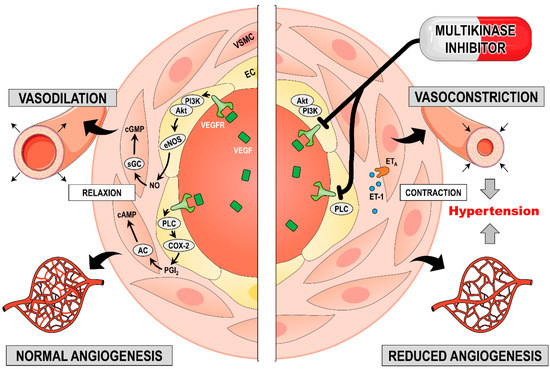
Figure 2.
The effect of multikinase inhibitors (MKIs) on blood vessels to promote hypertension. The left panel mirrors the physiological condition and the right panel shows conditions during MKI therapy. Vascular endothelial growth factor (VEGF) binding to its receptor (VEGFR) activates phosphoinositide 3-kinase (PI3K); this binding stimulates endothelial nitric oxide synthase (eNOS) and thereby NO production. NO diffusion to vascular smooth muscle cells (VSMCs) activates guanylate cyclase (GC) to produce cyclic guanosine monophosphate (cGMP), and this action causes vessel relaxation. VEGFR also activates phospholipase C (PLC), which stimulates cyclooxygenase-2 (COX-2) to generate prostacyclin (PGI2). This synthesis activates adenylate cyclase (AC) in the VSMCs and leads to cyclic adenosine monophosphate (cAMP) production, which causes vessel relaxation. Blocking VEGFR inhibits NO and PGI2 synthesis and increases endothelin-1 (ET-1) production. This combination contracts VSMCs and promotes vessel rarefaction—a phenomenon that ultimately leads to hypertension. Additional abbreviations: EC (endothelial cell), ATP (adenosine triphosphate), GTP (guanosine triphosphate), ETA (endothelin receptor A).
3.3.3. Sorafenib
Sorafenib (Figure 3A) was approved by the Food and Drug Administration (FDA) in 2005 [44] and by the European Medicines Agency (EMA) in 2006 for the treatment of RCC [45].
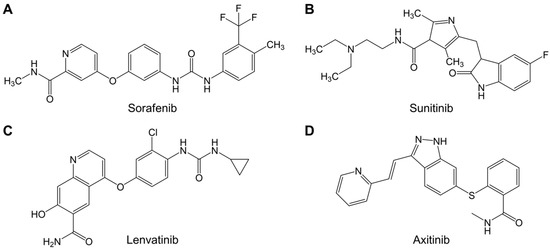
Figure 3.
Chemical structures of (A) sorafenib (C21H16ClF3N4O2), (B) sunitinib (C22H23N7O2S), (C) lenvatinib (C21H19ClN4O4), and (D) axitinib (C22H18N4OS), modified from. The sketch was generated using ChemDraw Professional 15.0.
Sorafenib inhibits RTKs, namely VEGFR-1, -2, -3, PDGFR-β, c-KIT, FMS-like tyrosine kinase-3 (FLT-3), rearranged upon transfection (RET) and the intracellular enzyme rapidly accelerated fibrosarcoma kinase (RAF) [25]. Blockage of the RTKs at the cell surface leads to inhibition of the intracellular phosphorylation cascade and the Raf/MEK/ERK and PI3K/AKT/mTOR pathways, thereby inhibiting the transcription of proteins involved in different functions. VEGFR is located on the surface of ECs, and sorafenib blocks the receptor—an action that leads to the inhibition of angiogenesis (VEGFR-1, -2) and lymphangiogenesis (VEGFR-3). Sorafenib also works as an antiangiogenic drug by inhibiting PDGFR at the surface of pericytes and smooth muscle cells. By blocking VEGFR and PDGFR, differentiation, proliferation, migration and tubular formation cannot occur. Angiogenesis is inhibited and ultimately tumourigenesis in RCC is halted. c-KIT, FLT-3 and RET are located on the tumour cell surface. Targeting these receptors will inhibit tumour growth [24,26,46]. RAF is an intracellular enzyme involved in all RTK pathways. Targeting this enzyme will thus inhibit all of the abovementioned mechanisms [24] (Figure 1).
Sorafenib is an orally administered drug with a recommended dose of 400 mg twice a day [4]. It is absorbed from the gastrointestinal tract with 92% bioavailability [47,48]. The peak concentration of the drug (Cmax) varies from patient to patient; it occurs between 2 and 12.5 h after administration and has an elimination half-life (T1/2) of 20–39 h in patients with cancer. In the blood stream, >99.5% sorafenib is protein-bound, mostly to serum albumin and α-acid glycoprotein [49].
Sorafenib is transported to the liver, where it is metabolised by the enzyme CYP3A4 to an N-oxide metabolite. Sorafenib is also conjugated by UGT1A9 to sorafenib glucuronide, which can be converted back to sorafenib in the gastrointestinal tract by β-glucuronidase [47]. Excretion of the metabolites occurs via the urinary (19%) and faecal (77%) routes [50].
3.3.4. Sunitinib
Sunitinib (Figure 3B) was FDA-approved in 2006 [44] and EMA-approved in 2006 for RCC treatment [51].
Sunitinib inhibits VEGFR-1, -2, -3, PDGFR-α, -β, c-KIT, FLT-3 and RET [25]. The mechanism of action is the same as for sorafenib; both drugs inhibit the same receptors and therefore are antiangiogenetic and antilymphangiogenetic and inhibit tumour growth [24] (Figure 1).
Sunitinib is an orally administrated drug taken at either 37.5 or 50 mg per day for 4 weeks, followed by 2 weeks of rest [52]. After intake, it is absorbed by the gastrointestinal tract (with ≥50% bioavailability) [53]. Cmax is reached after 6–12 h, and the T1/2 is 40–80 h. When transported in the blood, 65.3% binds to serum albumin and 33.7% binds to α-acid glycoprotein [54].
Sunitinib is transported to the liver, where it is metabolised by CYP3A4 to N-desethyl sunitinib (SU12662), which is an active metabolite. SU12662 is further metabolised by CYP3A4 to an inactive metabolite. Elimination of the metabolite occurs via the urinary (16%) and faecal (61%) routes [52].
3.3.5. Lenvatinib
Lenvatinib (Figure 3C) was FDA-approved in 2015 [44] and EMA-approved in 2015 for the treatment of RCC [55].
Lenvatinib inhibits VEGFR-2, fibroblast growth factor receptor (FGFR) (1, 2, 3, 4), PDGFR-α, c-KIT and RET. Lenvatinib inhibits similar tyrosine kinases to sorafenib and sunitinib; it works as an antiangiogenic (VEGFR-2 and PDGFR-α) drug and inhibits tumour growth (c-KIT and RET). Unlike sorafenib and sunitinib, lenvatinib also inhibits FGFR located on the EC surface. FGFR activation normally stimulates migration, proliferation and tubular formation, all of which lead to angiogenesis. By inhibiting FGFR, angiogenesis is blocked (Figure 1) [24].
Lenvatinib is an orally administrated drug with a recommended dose of 24 mg per day. It is rapidly absorbed in the gastrointestinal tract with a bioavailability of 90% [56]. Cmax is reached after 1.6 h and T1/2 is between 17.8 and 34.5 h [57]. Lenvatinib is primarily bound to serum albumin in the blood stream (range 97.9–98.6%) [56]. It is metabolised in both liver and kidneys and is excreted into the bile. CYP3A4 accounts for >80% of the drug elimination. The major metabolite is demethylated (M2) [58]. Excretion of the metabolites occurs via the urinary (25%) and faecal (64%) routes [57].
3.3.6. Axitinib
Axitinib (Figure 3D) was FDA- and EMA-approved in 2012 as a second-line treatment for RCC [59]. Axitinib is a potent MKI that selectively inhibits VEGFR-1, -2 and -3, PDGFR-α and-β as well as c-KIT [59].
Axitinib is administered orally with a standard starting dose of 5 mg twice daily (bid). Depending on potential AEs, the dose may be increased (7 or 10 mg) later in the treatment regimen. Axitinib is absorbed rapidly, with a bioavailability of 58% and T1/2 between 2.5 and 6.1 h. It binds to plasma proteins (>99%), mainly serum albumin. The drug is primarily metabolised in the liver by CYP3A4; less than 1% is excreted in the urine [60].
4. Results
4.1. Clinical Trials with Sorafenib, Sunitinib, Lenvatinib and Axitinib
The currently running trials for sorafenib, sunitinib, lenvatinib and axitinib in the treatment of patients with RCC are listed in Table 5, Table 6, Table 7 and Table 8, respectively.

Table 5.
Most recent sorafenib clinical trials for treating renal cell carcinoma [8].

Table 6.
Currently active clinical trials on the use of sunitinib for renal cell carcinoma therapy [8].

Table 7.
Currently active clinical trials on the use of lenvatinib for treating renal cell carcinoma [8].

Table 8.
Currently active clinical trials for the use of axitinib in renal cell carcinoma therapy [49].
Escudier et al. [33] included 903 patients previously treated for RCC who were randomly assigned to receive 400 mg sorafenib twice a day or placebo. Participants received the drug until disease progression, but some had to quit the drug due to toxicity. The median PFS was 5.5 months for patients treated with sorafenib and 2.8 months in patients receiving placebo. OS improved in sorafenib-treated patients after adjustment, with 17.8 months in the treated patients compared to 14.3 months in patients who received placebo. Even though sorafenib treatment showed notable efficacy, 87% of the patients treated with the drug developed a treatment-related AE (TRAE); hypertension developed in 17% of these patients. Only 54% of patients who received placebo developed a TRAE, and only 1% developed hypertension [33].
In Ravaud et al. [34], 615 participants with high-risk RCC were randomised to receive either 50 mg sunitinib per day or placebo for 4 weeks followed by 2 weeks off in one year or until disease recurrence, high grade AE or patients withdrew their consent. The median disease-free survival (DFS) was 6.8 years in patients treated with sunitinib (compared to 5.6 years in the placebo group). However, sunitinib treatment promoted a high frequency of AEs (34.3%), which led to dose reduction. Hypertension was one of the most frequent AEs, found in 44.7% of patients treated with sunitinib (of whom 7.8% presented grade 3 hypertension). In the placebo group, only 13.1% of patients developed hypertension [34].
In Motzer et al. [35], 153 patients with advanced RCC (ARCC) or mRCC were investigated. The patients were randomised to receive either lenvatinib (24 mg/day), everolimus (10 mg/day) or a combination of the two drugs (18 mg lenvatinib/day + 5 mg everolimus/day) in 28-day cycles. The treatment was given until disease progression, high-grade AE or patients withdrew their consent. The median PFS for lenvatinib + everolimus was 14.6 months, 7.4 months for lenvatinib and 5.5 months for everolimus only. All patients had at least one TRAE. Hypertension was seen in 41% of patients treated with the combination, 48% of patients treated with lenvatinib alone and only 10% of patients treated with everolimus [35].
In 2005, results from the first phase I axitinib trial were released. Patients with advanced solid tumours were included and the results were promising [61]. This publication was soon followed by phase II trials that investigated axitinib in the treatment of advanced RCC [36,62,63]. The study that led to FDA and EMA approval in 2012 was the randomised, open label phase III AXIS trial. A total of 723 patients with ARCC and progression on first-line therapy were included and randomised to receive either sorafenib or axitinib. The median PFS was 6.7 months in the axitinib group, compared with 4.7 months in the sorafenib group (hazard ratio 0.665; 95% confidence interval (CI) (0.544–0.812), p < 0.001).
Furthermore, axitinib demonstrated a favourable toxicity profile; only 14 (4%) versus 29 (8%) of patients had to discontinue treatment due to AEs. The most common AEs in the axitinib arm were diarrhoea (55%), hypertension (40%) and fatigue (39%) [64]. Grade 3 and 4 hypertension were relatively seldom, occurring in 15.3% (55/359) and 0.35% (1/359) of axitinib- and sorafenib-treated patients, respectively, and 50% of those patients continued treatment for ≥9 months. Of the 12.8% (46/359) dose interruptions, 4.5% (16/359) and 0.3% (1/359) discontinuations, respectively, were hypertension-related. Less than 1% of axitinib-treated patients suffered from hypertension-induced sequelae, and while axitinib caused hypertension more frequently than sorafenib, it rarely led to therapy discontinuation or cardiovascular complications [65].
4.2. Countermeasures against Drug-Induced Hypertension
Before initiating treatment with MKIs, patients should have their BP under control. Other medical conditions, including lifestyle factors known to raise BP, should be reduced [41]. If patients have confirmed hypertension, antihypertensive drugs should be offered before starting with MKIs [66].
There is no indication that antihypertensive drugs affect the anti-tumour effect of MKIs. Therefore, patients who develop hypertension (BP > 140/90) due to MKI therapy should receive standard hypertension treatments [40,41]. However, antihypertensive drugs that inhibit CYP3A4 (e.g., diltiazem or verapamil) should be avoided, because this enzyme is important for metabolising MKIs in the liver. It is very rare that patients require an MKI dose reduction or treatment discontinuation, but these measures are recommended if the BP rises to critical high grades [66].
4.3. Biomarkers in mRCC
Targeted MKI therapies have a significant role in the treatment of metastatic RCC. In the wake of personalized medicine, the need for reliable molecular biomarkers for diagnoses, prognoses and disease monitoring is rapidly increasing. One of the major challenges lies in identifying biomarkers that reach a sufficient level of clinical validation. Numerous novel single markers including circulating protein markers in blood or urine [33], micro-RNA [67,68] and tumour-derived cell-free RNA [69] have been tested with high levels of significance in RCC (Table 9). However, to our knowledge, no single marker has yet reached clinical validation, or has been shown to improve the existing prognostic models [70]. The focus has shifted towards combinations of panels of individual molecular markers with clinical markers such as neutrophil count [71,72]. Predictive biomarkers for identifying the optimal treatment on an individualized level remain a significant challenge. At present, several predictive biomarkers are under investigation, but most still require clinical validation. However, the International mRCC Database Consortium risk model was recently prospectively validated as a predictive biomarker in mRCC [73]. The model comprises six variables including neutrophil and platelet counts. It was demonstrated that this risk model could distinguish patients with mRCC into two groups that benefitted most from either immune checkpoint blockade versus sunitinib [74]. Although the AE hypertension has been associated with improved clinical outcomes on axitinib [75] and is discussed as surrogate marker for clinical efficacy of sunitinib therapy in mRCC [76], there are still no validated predictive biomarkers available.

Table 9.
Extract of recent updates for biomarkers in RCC.
5. Discussion
In recent years, targeted therapies for treating patients with RCC, including anti-VEFGR and anti-mTOR drugs, have been used as the standard of care. These drugs demonstrate prolonged PFS and OS, and thereby improve the quality of life [4].
There are a large number of clinical trials that compared the efficacy and safety of sorafenib and sunitinib in the treatment of RCC. One trial by Cai et al. [81] investigated the two drugs as first-line treatment in patients with mRCC. The PFS was 10 months (95% CI (7–13)) for sorafenib versus 11.5 months (95% CI (9–12)) for sunitinib; there was no significant difference between the two drugs. The difference in OS, 24 months (95% CI (15–31)) for sorafenib versus 23 months (95% CI (18–25)) for sunitinib, was also not significant. There were differences with regards to the number of AEs, especially the development of hypertension, which were more frequent in sunitinib-treated patients. In this study, sorafenib and sunitinib demonstrated comparable efficacy measures (PFS and OS), but sorafenib showed a more favourable profile in terms of AE development [81].
Comparing lenvatinib with the other drugs is challenging. For example, lenvatinib is relatively new (with regards to when it was approved), and thus only a few clinical trials have been completed that tested its effect on RCC. One trial that compared lenvatinib with sorafenib in patients with hepatocellular carcinoma was published by Kudo et al. [82]. The trial showed that the OS did not differ between the two drugs, but PFS was 7.4 months (95% CI (6.9–8.8)) for lenvatinib and only 3.7 months (95% CI (3.6–4.6)) for sorafenib (p < 0.001). Lenvatinib treatment resulted in a higher percentage of high-grade AEs than sorafenib. Additionally, there was a large difference in developing hypertension (42% for lenvatinib and 30% for sorafenib). One might conclude that lenvatinib has better efficacy than sorafenib but worse safety with regards to hypertension [82].
There are no published clinical trials that compared lenvatinib and sunitinib, but there is a new trial (NCT02811861) that will investigate lenvatinib + everolimus or lenvatinib + pembrolizumab versus sunitinib in patients with ARCC [8]. Overall, sorafenib and lenvatinib seem to have a similar safety and efficacy profile.
Sorafenib was the first MKI approved for the treatment of RCC (2005). Subsequently, myriad other targeted therapies have been approved and are challenging the use of sorafenib [4]. Both axitinib and tivozanib have demonstrated a better PFS (with no differences in OS) compared to sorafenib [28,83]. Compared with temsirolimus, there is no difference in PFS, but sorafenib shows a better OS [84]. Although sorafenib is challenged based on PFS, it has a demonstrated favourable safety profile with fewer cases of hypertension compared to other MKIs [28,83] (Table 10).

Table 10.
Overview of trials that investigated axitinib, sorafenib, sunitinib and lenvatinib with other targeted therapies: special focus on hypertension.
Moreover, sunitinib has been compared with other MKIs. Sunitinib had better efficacy when compared to pazopanib and everolimus (anti-mTOR) [85,86]. In contrast, when sunitinib was compared to cabozantinib, sunitinib had worse efficacy, with a lower PFS and OS [87]. Regarding the safety profile, sunitinib showed a much lower percent of patients who developed hypertension compared to pazopanib and cabozantinib but not everolimus (Table 10) [85,86,87].
As mentioned earlier, lenvatinib is still a new drug on the market, so only a few clinical trials have been published testing lenvatinib with other targeted therapies. A trial of lenvatinib alone versus lenvatinib + everolimus demonstrated that the combination has promising benefits for PFS, OS and safety profile compared to lenvatinib treatment alone [35] (Table 10).
As illustrated, one of the most common AEs associated with MKI treatment is hypertension. Different AEs have been associated with improved outcome measures [5,6]. In particular, hypertension has been suggested as a possible biomarker of treatment efficacy, and has been reviewed elsewhere [88]. Especially, sunitinib-induced hypertension and neutropenia were found to be associated with longer PFS and OS in ccRCC patients. These effects are discussed as efficacy biomarkers and as a sign of response to the MKI treatment [89]. However, data are limited by the number of studies and knowledge of the mechanism of action [88]. Table 10 compares trials and the prevalence of hypertension.
VEGFR-2 inhibition abrogates NO synthesis, VEGFR-1+2 inhibition reduces PGI2 synthesis and VEGFR-(1+2+3) inhibition promotes vessel rarefaction, all of which are mechanisms involved in hypertension development [41]. Both sorafenib and sunitinib target the same receptors (VEGFR-(1+2+3)), while lenvatinib only targets VEGFR-2 [4,27,41]. Thus, while sorafenib and sunitinib have the exact same targets for potentially developing hypertension, clinical trials still show a difference between the drugs [81]. Furthermore, lenvatinib caused a higher percentage of hypertension than sorafenib [82], but sorafenib targets more receptors involved in angiogenesis. Considering this finding, one might expect that sorafenib could be a stronger inducer of hypertension than lenvatinib. Therefore, it is very important to note that other conditions like lifestyle or genetic factors may also play a role in this phenomenon.
6. Conclusions and Outlook
The evolution of targeted therapies has changed PFS and OS for patients suffering from RCC and thereby increased their quality of life. Of these targeted therapies, MKIs (especially those that target VEGFRs) inhibit angiogenesis. Sorafenib, sunitinib, lenvatinib and axitinib have all demonstrated improvements in RCC treatment. Sorafenib and sunitinib are currently being challenged by newer targeted therapies like lenvatinib, axitinib and mTOR inhibitors, among others.
A major AE when administering MKIs is hypertension. Hypertension development is linked to the VEGFR targeting, which inhibits NO and PGI2 production, induces ET-1, and promotes vasocontraction and vessel rarefaction [31]. However, the complete mechanism is not yet fully understood. There is no report about complications when patients are treated with antihypertensive drugs together with an MKI. Only in a few cases with high-grade hypertension was it necessary to decrease the dose or totally stop MKI therapy. The number of reported AEs is quite variable among clinical trials, suggesting that lifestyle and other predisposing factors may also influence AE (especially hypertension) development and should be studied in detail in the future.
Currently, numerous trials that are investigating MKI efficacy and safety for RCC treatment are recruiting participants. The combination of anti-VEGFR and anti-mTOR is a promising treatment (e.g., lenvatinib + everolimus), and perhaps in the future more combined targeted therapy regimens will be used in cancer. The main goal is to develop a drug with great efficacy and safety with the least amount of toxicity.
Author Contributions
All authors contributed to the review and searched the literature. Conceptualization, M.K. and D.G.; investigation, N.B.M., C.B., M.W., N.E.M., and M.K.; writing—original draft preparation, M.W., N.B.M., C.B., and D.G.; review and editing. M.K., D.G., N.E.M., and M.W.; visualization, N.B.M. and M.K., project administration, D.G. and M.I.; funding acquisition, D.G. and M.I.
Funding
This research was funded by the Otto von Guericke University Magdeburg, Germany, and by Aarhus University, Denmark.
Acknowledgments
We would like to thank the team of PRS and EJE (Letchworth Garden City, UK) for academic proofreading of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AC | adenylate cyclase |
| AE(s) | adverse effect(s) |
| AKT | protein kinase B |
| ARCC | advanced renal cell carcinoma |
| ATP | adenosine triphosphate |
| cAMP | cyclic adenosine monophosphate |
| ccRCC | clear cell renal cell carcinoma |
| cGMP | cyclic guanosine monophosphate |
| CI | confidence interval |
| C-KIT | stem cell factor receptor |
| Cmax | peak concentration of a drug |
| COX-2 | cyclooxygenae-2) |
| CYP3A4 | cytochrome P450 3A4 |
| DBP | diastolic blood pressure |
| DSF | disease-free survival |
| EC | endothelial cell |
| EMA | European Medicines Agency |
| eNOS | endothelial nitric oxide synthase |
| ERK | extracellular signal-regulated kinase |
| ET-1 | endothelin-1 |
| ETA | endothelin receptor A |
| FDA | Food and Drug Administration |
| FGF | fibroblast growth factor |
| FGFR | fibroblast growth factor receptor |
| FLT-3 | FMS-like tyrosine kinase 3 |
| GC | guanylyl cyclase |
| GTP | guanosine triphosphate |
| HIF | hypoxia-inducible factor |
| I.V. | intravenous |
| MEK | Mitogen-activated protein kinase |
| MET | hepatocyte growth factor receptor |
| MKI(s) | multikinase inhibitor(s) |
| mRCC | metastatic renal cell carcinoma/cancer |
| mTOR | mammalian target of rapamycin |
| NO | nitric oxide |
| OS | overall survival |
| PC | pericyte |
| PD-1 | programmed death-1 |
| PDGF | platelet-derived growth factor |
| PDGFR | platelet-derived growth factor receptor |
| PFS | progression-free survival |
| PGI2 | prostacyclin |
| PI3K | phosphoinositide 3-kinase |
| PLC | phospholipase C |
| pVHL | von Hippel-Lindau protein |
| RCC | renal cell carcinoma |
| RAF | rapidly accelerated fibrosarcoma kinase |
| RAS | rat sarcoma |
| RET | rearranged during transfection |
| RTK | tyrosine kinase receptor |
| SBP | systolic blood pressure |
| TC | tumour cell |
| TGFA | transforming growth factor alpha |
| TRAE | treatment-related adverse effect |
| TTP | time to progression |
| T1/2 | elimination half-life |
| UGT1A9 | uridine diphosphate glucuronosyltransferase 1A9 |
| VEGF | vascular endothelial growth factor |
| VEGFR | vascular endothelial growth factor receptor |
| VHL | von Hippel-Lindau |
| VSMC | vascular smooth muscle cell |
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Rapsomaniki, E.; Timmis, A.; George, J.; Pujades-Rodriguez, M.; Shah, A.D.; Denaxas, S.; White, I.R.; Caulfield, M.J.; Deanfield, J.E.; Smeeth, L.; et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014, 383, 1899–1911. [Google Scholar] [CrossRef]
- Wermelt, J.A.; Schunkert, H. Management of arterial hypertension. Herz 2017, 42, 515–526. [Google Scholar] [CrossRef] [PubMed]
- Mattei, J.; da Silva, R.D.; Sehrt, D.; Molina, W.R.; Kim, F.J. Targeted therapy in metastatic renal carcinoma. Cancer Lett. 2014, 343, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Randrup Hansen, C.; Grimm, D.; Bauer, J.; Wehland, M.; Magnusson, N.E. Effects and side effects of using sorafenib and sunitinib in the treatment of metastatic renal cell carcinoma. Int. J. Mol. Sci. 2017, 18, 461. [Google Scholar] [CrossRef] [PubMed]
- Bendtsen, M.A.F.; Grimm, D.; Bauer, J.; Wehland, M.; Wise, P.; Magnusson, N.E.; Infanger, M.; Kruger, M. Hypertension caused by lenvatinib and everolimus in the treatment of metastatic renal cell carcinoma. Int. J. Mol. Sci. 2017, 18, 1736. [Google Scholar] [CrossRef] [PubMed]
- PubMed. National Center for Biotechnology Information, U.S. National Library of Medicine. Available online: https://www.ncbi.nlm.nih.gov/pubmed/ (accessed on 26 November 2018).
- ClinicalTrials. U.S. National Library of Medicine. Available online: https://clinicaltrials.gov/ (accessed on 26 November 2018).
- Hsieh, J.J.; Purdue, M.P.; Signoretti, S.; Swanton, C.; Albiges, L.; Schmidinger, M.; Heng, D.Y.; Larkin, J.; Ficarra, V. Renal cell carcinoma. Nat. Rev. Dis. Primers 2017, 3, 17009. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Garfield, K.; LaGrange, C.A. Cancer, renal cell. In Statpearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2018. [Google Scholar]
- Randall, J.M.; Millard, F.; Kurzrock, R. Molecular aberrations, targeted therapy, and renal cell carcinoma: Current state-of-the-art. Cancer Metastasis Rev. 2014, 33, 1109–1124. [Google Scholar] [CrossRef] [PubMed]
- Capitanio, U.; Bensalah, K.; Bex, A.; Boorjian, S.A.; Bray, F.; Coleman, J.; Gore, J.L.; Sun, M.; Wood, C.; Russo, P. Epidemiology of renal cell carcinoma. Eur. Urol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Grignon, D.J.; Che, M. Clear cell renal cell carcinoma. Clin. Lab. Med. 2005, 25, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Beltran, A.; Carrasco, J.C.; Cheng, L.; Scarpelli, M.; Kirkali, Z.; Montironi, R. 2009 update on the classification of renal epithelial tumors in adults. Int. J. Urol. 2009, 16, 432–443. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Wu, Y.; Zhang, J.; Fang, Z.; Liu, Z.; Xu, Z.; Fan, Y. Nomograms for predicting long-term overall survival and disease-specific survival of patients with clear cell renal cell carcinoma. OncoTargets Ther. 2018, 11, 5535–5544. [Google Scholar] [CrossRef] [PubMed]
- Cao, Q.; Ruan, H.; Wang, K.; Song, Z.; Bao, L.; Xu, T.; Xiao, H.; Wang, C.; Cheng, G.; Tong, J.; et al. Overexpression of plin2 is a prognostic marker and attenuates tumor progression in clear cell renal cell carcinoma. Int. J. Oncol. 2018, 53, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Ren, Y.; Pang, L.; Qi, Y.; Jia, W.; Tao, L.; Hu, Z.; Zhao, J.; Zhang, H.; Li, L.; et al. Papillary renal cell carcinoma: A clinicopathological and whole-genome exon sequencing study. Int. J. Clin. Exp. Pathol. 2015, 8, 8311–8335. [Google Scholar] [PubMed]
- Motzer, R.J.; Basch, E. Targeted drugs for metastatic renal cell carcinoma. Lancet 2007, 370, 2071–2073. [Google Scholar] [CrossRef]
- Escudier, B.; Eisen, T.; Stadler, W.M.; Szczylik, C.; Oudard, S.; Siebels, M.; Negrier, S.; Chevreau, C.; Solska, E.; Desai, A.A.; et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N. Engl. J. Med. 2007, 356, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Choueiri, T.K.; Plantade, A.; Elson, P.; Negrier, S.; Ravaud, A.; Oudard, S.; Zhou, M.; Rini, B.I.; Bukowski, R.M.; Escudier, B. Efficacy of sunitinib and sorafenib in metastatic papillary and chromophobe renal cell carcinoma. J. Clin. Oncol. 2008, 26, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.Y.; Kaelin, W.G. Role of VHL gene mutation in human cancer. J. Clin. Oncol 2004, 22, 4991–5004. [Google Scholar] [CrossRef] [PubMed]
- Nabi, S.; Kessler, E.R.; Bernard, B.; Flaig, T.W.; Lam, E.T. Renal cell carcinoma: A review of biology and pathophysiology. F1000Research 2018, 7, 307. [Google Scholar] [CrossRef]
- Gollob, J.A.; Wilhelm, S.; Carter, C.; Kelley, S.L. Role of Raf kinase in cancer: Therapeutic potential of targeting the Raf/MEK/ERK signal transduction pathway. Semin. Oncol. 2006, 33, 392–406. [Google Scholar] [CrossRef] [PubMed]
- Erman, M.; Benekli, M.; Basaran, M.; Bavbek, S.; Buyukberber, S.; Coskun, U.; Demir, G.; Karabulut, B.; Oksuzoglu, B.; Ozkan, M.; et al. Renal cell cancer: Overview of the current therapeutic landscape. Expert Rev. Anticancer Ther. 2016, 16, 955–968. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Gerendash, B.; Dizman, N.; Khan, A.; Pal, S.K. Advances in treatment of metastatic renal cell carcinoma. Curr. Opin. Urol. 2016, 26, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Glen, H. Lenvatinib therapy for the treatment of patients with advanced renal cell carcinoma. Future Oncol. 2016, 12, 2195–2204. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Nosov, D.; Eisen, T.; Bondarenko, I.; Lesovoy, V.; Lipatov, O.; Tomczak, P.; Lyulko, O.; Alyasova, A.; Harza, M.; et al. Tivozanib versus sorafenib as initial targeted therapy for patients with metastatic renal cell carcinoma: Results from a phase III trial. J. Clin. Oncol. 2013, 31, 3791–3799. [Google Scholar] [CrossRef] [PubMed]
- Cicenas, J.; Cicenas, E. Multi-kinase inhibitors, aurks and cancer. Med. Oncol. 2016, 33, 43. [Google Scholar] [CrossRef]
- Wehland, M.; Bauer, J.; Infanger, M.; Grimm, D. Target-based anti-angiogenic therapy in breast cancer. Curr. Pharm. Des. 2012, 18, 4244–4257. [Google Scholar] [CrossRef]
- Kristensen, T.B.; Knutsson, M.L.; Wehland, M.; Laursen, B.E.; Grimm, D.; Warnke, E.; Magnusson, N.E. Anti-vascular endothelial growth factor therapy in breast cancer. Int. J. Mol. Sci. 2014, 15, 23024–23041. [Google Scholar] [CrossRef]
- Hubbard, S.R.; Till, J.H. Protein tyrosine kinase structure and function. Annu. Rev. Biochem. 2000, 69, 373–398. [Google Scholar] [CrossRef]
- Escudier, B.; Eisen, T.; Stadler, W.M.; Szczylik, C.; Oudard, S.; Staehler, M.; Negrier, S.; Chevreau, C.; Desai, A.A.; Rolland, F.; et al. Sorafenib for treatment of renal cell carcinoma: Final efficacy and safety results of the phase iii treatment approaches in renal cancer global evaluation trial. J. Clin. Oncol. 2009, 27, 3312–3318. [Google Scholar] [CrossRef]
- Ravaud, A.; Motzer, R.J.; Pandha, H.S.; George, D.J.; Pantuck, A.J.; Patel, A.; Chang, Y.H.; Escudier, B.; Donskov, F.; Magheli, A.; et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N. Engl. J. Med. 2016, 375, 2246–2254. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Hutson, T.E.; Glen, H.; Michaelson, M.D.; Molina, A.; Eisen, T.; Jassem, J.; Zolnierek, J.; Maroto, J.P.; Mellado, B.; et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: A randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015, 16, 1473–1482. [Google Scholar] [CrossRef]
- Rini, B.I.; Wilding, G.; Hudes, G.; Stadler, W.M.; Kim, S.; Tarazi, J.; Rosbrook, B.; Trask, P.C.; Wood, L.; Dutcher, J.P. Phase II study of axitinib in sorafenib-refractory metastatic renal cell carcinoma. J. Clin. Oncol. 2009, 27, 4462–4468. [Google Scholar] [CrossRef] [PubMed]
- Milling, R.V.; Grimm, D.; Krüger, M.; Grosse, J.; Kopp, S.; Bauer, J.; Infanger, M.; Wehland, M. Pazopanib, cabozantinib, and vandetanib in the treatment of progressive medullary thyroid cancer with a special focus on the adverse effects on hypertension. Int. J. Mol. Sci. 2018, 19, 3258. [Google Scholar] [CrossRef]
- Laursen, R.; Wehland, M.; Kopp, S.; Pietsch, J.; Infanger, M.; Grosse, J.; Grimm, D. Effects and role of multikinase inhibitors in thyroid cancer. Curr. Pharm. Des. 2016, 22, 5915–5926. [Google Scholar] [CrossRef]
- Ancker, O.V.; Wehland, M.; Bauer, J.; Infanger, M.; Grimm, D. The adverse effect of hypertension in the treatment of thyroid cancer with multi-kinase inhibitors. Int. J. Mol. Sci. 2017, 18, 625. [Google Scholar] [CrossRef]
- Larochelle, P.; Kollmannsberger, C.; Feldman, R.D.; Schiffrin, E.L.; Poirier, L.; Patenaude, F.; Ruether, D.; Myers, M.; Bjarnason, G. Hypertension management in patients with renal cell cancer treated with anti-angiogenic agents. Curr. Oncol. 2012, 19, 202–208. [Google Scholar] [CrossRef]
- Robinson, E.S.; Khankin, E.V.; Karumanchi, S.A.; Humphreys, B.D. Hypertension induced by vascular endothelial growth factor signaling pathway inhibition: Mechanisms and potential use as a biomarker. Semin. Nephrol. 2010, 30, 591–601. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Ali, F.; Bailey, L.; Moreno, L.; Harrington, L.S. Role of nitric oxide and prostacyclin as vasoactive hormones released by the endothelium. Exp. Physiol. 2008, 93, 141–147. [Google Scholar] [CrossRef]
- Kappers, M.H.; van Esch, J.H.; Sluiter, W.; Sleijfer, S.; Danser, A.H.; van den Meiracker, A.H. Hypertension induced by the tyrosine kinase inhibitor sunitinib is associated with increased circulating endothelin-1 levels. Hypertension 2010, 56, 675–681. [Google Scholar] [CrossRef]
- Roskoski, R., Jr. Vascular endothelial growth factor (VEGF) and VEGF receptor inhibitors in the treatment of renal cell carcinomas. Pharmacol. Res. 2017, 120, 116–132. [Google Scholar] [CrossRef]
- European Medicines Agency. Nexavar (Sorafenib). Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/nexavar (accessed on 4 November 2018).
- Samadi, A.K.; Mukerji, R.; Shah, A.; Timmermann, B.N.; Cohen, M.S. A novel ret inhibitor with potent efficacy against medullary thyroid cancer in vivo. Surgery 2010, 148, 1228–1236. [Google Scholar] [CrossRef]
- Edginton, A.N.; Zimmerman, E.I.; Vasilyeva, A.; Baker, S.D.; Panetta, J.C. Sorafenib metabolism, transport, and enterohepatic recycling: Physiologically based modeling and simulation in mice. Cancer Chemother. Pharmacol. 2016, 77, 1039–1052. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; Huang, X.; Li, Y.; Wu, M.; Liu, J. The drug-drug interaction of sorafenib mediated by p-glycoprotein and cyp3a4. Xenobiotica 2016, 46, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Villarroel, M.C.; Pratz, K.W.; Xu, L.; Wright, J.J.; Smith, B.D.; Rudek, M.A. Plasma protein binding of sorafenib, a multi kinase inhibitor: In vitro and in cancer patients. Invest. New Drugs 2012, 30, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Lathia, C.; Lettieri, J.; Cihon, F.; Gallentine, M.; Radtke, M.; Sundaresan, P. Lack of effect of ketoconazole-mediated cyp3a inhibition on sorafenib clinical pharmacokinetics. Cancer Chemother. Pharmacol. 2006, 57, 685–692. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Sutent (Sunitinib). Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/sutent (accessed on 4 November 2018).
- Yu, H.; Steeghs, N.; Kloth, J.S.; de Wit, D.; van Hasselt, J.G.; van Erp, N.P.; Beijnen, J.H.; Schellens, J.H.; Mathijssen, R.H.; Huitema, A.D. Integrated semi-physiological pharmacokinetic model for both sunitinib and its active metabolite su12662. Br. J. Clin. Pharmacol. 2015, 79, 809–819. [Google Scholar] [CrossRef] [PubMed]
- Haznedar, J.O.; Patyna, S.; Bello, C.L.; Peng, G.W.; Speed, W.; Yu, X.; Zhang, Q.; Sukbuntherng, J.; Sweeny, D.J.; Antonian, L.; et al. Single- and multiple-dose disposition kinetics of sunitinib malate, a multitargeted receptor tyrosine kinase inhibitor: Comparative plasma kinetics in non-clinical species. Cancer Chemother. Pharmacol. 2009, 64, 691–706. [Google Scholar] [CrossRef] [PubMed]
- Toyama, Y.; Ueyama, J.; Nomura, H.; Tsukiyama, I.; Saito, H.; Hisada, T.; Matsuura, K.; Hasegawa, T. Contribution of plasma proteins, albumin and alpha 1-acid glycoprotein, to pharmacokinetics of a multi-targeted receptor tyrosine kinase inhibitor, sunitinib, in analbuminemic rats. Anticancer Res. 2014, 34, 2283–2289. [Google Scholar] [PubMed]
- European Medicines Agency. Lenvima (Lenvatinib). Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/lenvima (accessed on 4 November 2018).
- Gupta, A.; Jarzab, B.; Capdevila, J.; Shumaker, R.; Hussein, Z. Population pharmacokinetic analysis of lenvatinib in healthy subjects and patients with cancer. Br. J. Clin. Pharmacol. 2016, 81, 1124–1133. [Google Scholar] [CrossRef]
- Dubbelman, A.C.; Rosing, H.; Nijenhuis, C.; Huitema, A.D.; Mergui-Roelvink, M.; Gupta, A.; Verbel, D.; Thompson, G.; Shumaker, R.; Schellens, J.H.; et al. Pharmacokinetics and excretion of (14)c-lenvatinib in patients with advanced solid tumors or lymphomas. Invest. New Drugs 2015, 33, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Shumaker, R.C.; Aluri, J.; Fan, J.; Martinez, G.; Thompson, G.A.; Ren, M. Effect of rifampicin on the pharmacokinetics of lenvatinib in healthy adults. Clin. Drug Investig. 2014, 34, 651–659. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Albiges, L.; Gizzi, M.; Carton, E.; Escudier, B. Axitinib in metastatic renal cell carcinoma. Expert Rev. Anticancer Ther. 2015, 15, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Gross-Goupil, M.; Francois, L.; Quivy, A.; Ravaud, A. Axitinib: A review of its safety and efficacy in the treatment of adults with advanced renal cell carcinoma. Clin. Med. Insights Oncol. 2013, 7, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Rugo, H.S.; Herbst, R.S.; Liu, G.; Park, J.W.; Kies, M.S.; Steinfeldt, H.M.; Pithavala, Y.K.; Reich, S.D.; Freddo, J.L.; Wilding, G. Phase I trial of the oral antiangiogenesis agent ag-013736 in patients with advanced solid tumors: Pharmacokinetic and clinical results. J. Clin. Oncol. 2005, 23, 5474–5483. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Uemura, H.; Fujimoto, H.; Kanayama, H.O.; Shinohara, N.; Nakazawa, H.; Imai, K.; Umeyama, Y.; Ozono, S.; Naito, S.; et al. Key predictive factors of axitinib (ag-013736)-induced proteinuria and efficacy: A phase II study in japanese patients with cytokine-refractory metastatic renal cell carcinoma. Eur. J. Cancer 2011, 47, 2592–2602. [Google Scholar] [CrossRef] [PubMed]
- Rixe, O.; Bukowski, R.M.; Michaelson, M.D.; Wilding, G.; Hudes, G.R.; Bolte, O.; Motzer, R.J.; Bycott, P.; Liau, K.F.; Freddo, J.; et al. Axitinib treatment in patients with cytokine-refractory metastatic renal-cell cancer: A phase II study. Lancet Oncol. 2007, 8, 975–984. [Google Scholar] [CrossRef]
- Rini, B.I.; Escudier, B.; Tomczak, P.; Kaprin, A.; Szczylik, C.; Hutson, T.E.; Michaelson, M.D.; Gorbunova, V.A.; Gore, M.E.; Rusakov, I.G.; et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (axis): A randomised phase 3 trial. Lancet 2011, 378, 1931–1939. [Google Scholar] [CrossRef]
- Rini, B.I.; Quinn, D.I.; Baum, M.; Wood, L.S.; Tarazi, J.; Rosbrook, B.; Arruda, L.S.; Cisar, L.; Roberts, W.G.; Kim, S.; et al. Hypertension among patients with renal cell carcinoma receiving axitinib or sorafenib: Analysis from the randomized phase iii axis trial. Target. Oncol 2015, 10, 45–53. [Google Scholar] [CrossRef]
- De Jesus-Gonzalez, N.; Robinson, E.; Moslehi, J.; Humphreys, B.D. Management of antiangiogenic therapy-induced hypertension. Hypertension 2012, 60, 607–615. [Google Scholar] [CrossRef]
- Martignoni, G.; Brunelli, M.; Segala, D.; Munari, E.; Gobbo, S.; Cima, L.; Borze, I.; Wirtanen, T.; Sarhadi, V.K.; Atanesyan, L.; et al. Validation of 34betae12 immunoexpression in clear cell papillary renal cell carcinoma as a sensitive biomarker. Pathology 2017, 49, 10–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lou, N.; Ruan, A.M.; Qiu, B.; Bao, L.; Xu, Y.C.; Zhao, Y.; Sun, R.L.; Zhang, S.T.; Xu, G.H.; Ruan, H.L.; et al. Mir-144–3p as a novel plasma diagnostic biomarker for clear cell renal cell carcinoma. Urol. Oncol. 2017, 35, 36.e7–36.e14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhu, J.; George, D.J.; Nixon, A.B. Metastatic clear cell renal cell carcinoma: Circulating biomarkers to guide antiangiogenic and immune therapies. Urol. Oncol. 2016, 34, 510–518. [Google Scholar] [CrossRef] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology. Available online: https://www.nccn.org/professionals/physician_gls/f_guidelines.asp (accessed on 26 November 2018).
- Haddad, A.Q.; Luo, J.H.; Krabbe, L.M.; Darwish, O.; Gayed, B.; Youssef, R.; Kapur, P.; Rakheja, D.; Lotan, Y.; Sagalowsky, A.; et al. Prognostic value of tissue-based biomarker signature in clear cell renal cell carcinoma. BJU Int. 2017, 119, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Pires-Luis, A.S.; Costa-Pinheiro, P.; Ferreira, M.J.; Antunes, L.; Lobo, F.; Oliveira, J.; Henrique, R.; Jeronimo, C. Identification of clear cell renal cell carcinoma and oncocytoma using a three-gene promoter methylation panel. J. Transl. Med. 2017, 15, 149. [Google Scholar] [CrossRef] [PubMed]
- Dudani, S.; Savard, M.F.; Heng, D.Y.C. An update on predictive biomarkers in metastatic renal cell carcinoma. Eur. Urol. Focus 2019. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Aren Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthelemy, P.; Porta, C.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef] [PubMed]
- Narayan, V.; Haas, N.B. Axitinib in the treatment of renal cell carcinoma: Patient selection and perspectives. Int. J. Nephrol. Renovasc. Dis. 2016, 9, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Kollmannsberger, C. Sunitinib side effects as surrogate biomarkers of efficacy. Can. Urol. Assoc. J. 2016, 10, S245–S247. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heng, D.Y.; Xie, W.; Regan, M.M.; Harshman, L.C.; Bjarnason, G.A.; Vaishampayan, U.N.; Mackenzie, M.; Wood, L.; Donskov, F.; Tan, M.H.; et al. External validation and comparison with other models of the international metastatic renal-cell carcinoma database consortium prognostic model: A population-based study. Lancet Oncol. 2013, 14, 141–148. [Google Scholar] [CrossRef]
- Graham, J.; Dudani, S.; Heng, D.Y.C. Prognostication in kidney cancer: Recent advances and future directions. J. Clin. Oncol. 2018. [Google Scholar] [CrossRef]
- Suzuki, K.; Terakawa, T.; Furukawa, J.; Harada, K.; Hinata, N.; Nakano, Y.; Fujisawa, M. C-reactive protein and the neutrophil-to-lymphocyte ratio are prognostic biomarkers in metastatic renal cell carcinoma patients treated with nivolumab. Int. J. Clin. Oncol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kovacova, J.; Juracek, J.; Poprach, A.; Kopecky, J.; Fiala, O.; Svoboda, M.; Fabian, P.; Radova, L.; Brabec, P.; Buchler, T.; et al. Mir-376b-3p is associated with long-term response to sunitinib in metastatic renal cell carcinoma patients. Cancer Genom. Proteom. 2019, 16, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Kong, W.; Dong, B.; Zhang, J.; Chen, Y.; Xue, W.; Huang, Y.; Zhou, L.; Huang, J. Comparison of efficacy, safety, and quality of life between sorafenib and sunitinib as first-line therapy for chinese patients with metastatic renal cell carcinoma. Chin. J. Cancer 2017, 36, 64. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Motzer, R.J.; Escudier, B.; Tomczak, P.; Hutson, T.E.; Michaelson, M.D.; Negrier, S.; Oudard, S.; Gore, M.E.; Tarazi, J.; Hariharan, S.; et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: Overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013, 14, 552–562. [Google Scholar] [CrossRef]
- Hutson, T.E.; Escudier, B.; Esteban, E.; Bjarnason, G.A.; Lim, H.Y.; Pittman, K.B.; Senico, P.; Niethammer, A.; Lu, D.R.; Hariharan, S.; et al. Randomized phase III trial of temsirolimus versus sorafenib as second-line therapy after sunitinib in patients with metastatic renal cell carcinoma. J. Clin. Oncol. 2014, 32, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Hutson, T.E.; Cella, D.; Reeves, J.; Hawkins, R.; Guo, J.; Nathan, P.; Staehler, M.; de Souza, P.; Merchan, J.R.; et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N. Engl. J. Med. 2013, 369, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.J.; Halabi, S.; Eisen, T.; Broderick, S.; Stadler, W.M.; Jones, R.J.; Garcia, J.A.; Vaishampayan, U.N.; Picus, J.; Hawkins, R.E.; et al. Everolimus versus sunitinib for patients with metastatic non-clear cell renal cell carcinoma (aspen): A multicentre, open-label, randomised phase 2 trial. Lancet Oncol. 2016, 17, 378–388. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Halabi, S.; Sanford, B.L.; Hahn, O.; Michaelson, M.D.; Walsh, M.K.; Feldman, D.R.; Olencki, T.; Picus, J.; Small, E.J.; et al. Cabozantinib versus sunitinib as initial targeted therapy for patients with metastatic renal cell carcinoma of poor or intermediate risk: The alliance a031203 cabosun trial. J. Clin. Oncol. 2017, 35, 591–597. [Google Scholar] [CrossRef]
- Budolfsen, C.; Faber, J.; Grimm, D.; Krüger, M.; Bauer, J.; Wehland, M.; Infanger, M.; Magnusson, N.E. Tyrosine kinase inhibitor-induced hypertension: Role of hypertension as a biomarker in cancer treatment. Curr. Vasc. Pharmacol. 2019. [Google Scholar] [CrossRef]
- Donskov, F.; Michaelson, M.D.; Puzanov, I.; Davis, M.P.; Bjarnason, G.A.; Motzer, R.J.; Goldstein, D.; Lin, X.; Cohen, D.P.; Wiltshire, R.; et al. Sunitinib-associated hypertension and neutropenia as efficacy biomarkers in metastatic renal cell carcinoma patients. Br. J. Cancer 2015, 113, 1571–1580. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).