Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
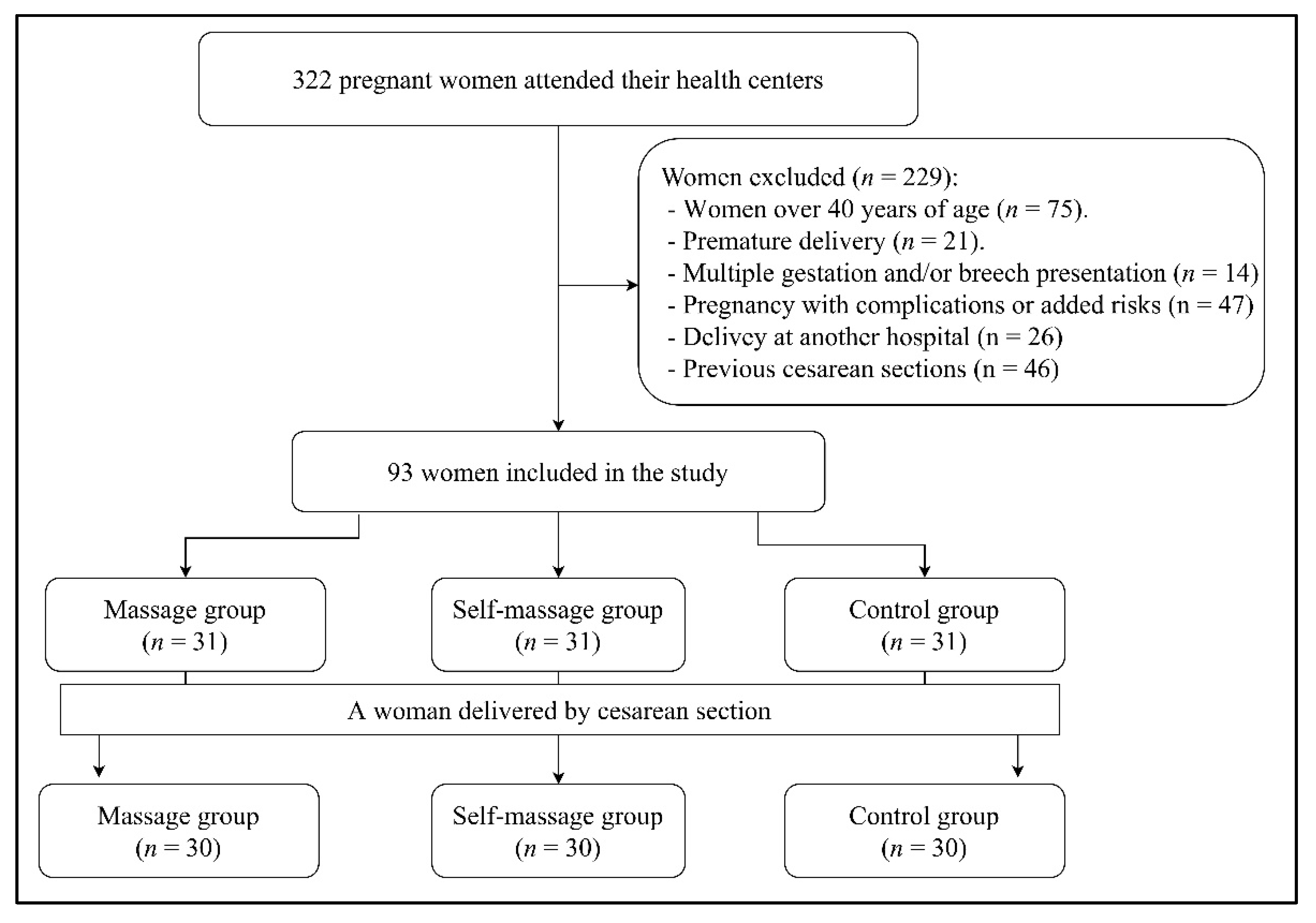
2.1. Experimental Design and Sample
2.2. Experimental Procedure
2.3. Perineal Self-Massage Intervention
2.4. Perineal Massage Intervention
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis
3.2. Bivariate Analysis
3.3. Regression Analysis: Determinants in Perineal Tear
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Handa, V.L.; Blomquist, J.L.; McDermott, K.C.; Friedman, S.; Muñoz, A. Pelvic Floor Disorders after Vaginal Birth: Effect of episiotomy, perineal laceration, and operative birth. Obstet. Gynecol. 2012, 119, 233–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frohlich, J.; Kettle, C. Perineal care. BMJ Clin. Evid. 2015, 2015, 1401. [Google Scholar] [PubMed]
- Goh, R. Perineal tears—A review. Aust. J. Gen. Pract. 2018, 47, 35–38. [Google Scholar] [CrossRef]
- Hamilton, E.F.; Smith, S.; Yang, L.; Warrick, P.; Ciampi, A. Third- and fourth-degree perineal lacerations: Defining high-risk clinical clusters. Am. J. Obstet. Gynecol. 2011, 204, 309.e1–309.e6. [Google Scholar] [CrossRef]
- Hirayama, F.; Koyanagi, A.; Mori, R.; Zhang, J.; Souza, J.; Gülmezoglu, A. Prevalence and risk factors for third- and fourth-degree perineal lacerations during vaginal delivery: A multi-country study. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Thubert, T.; Cardaillac, C.; Fritel, X.; Winer, N.; Dochez, V. Définitions, épidémiologie et facteurs de risque des lésions périnéales du 3e et 4e degrés. RPC Prévention et protection périnéale en obstétrique CNGOF. Gynecol. Obstet. Fertil. Senol. 2018, 46, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Bergman, I.; Söderberg, M.W.; Ek, M. Perineorrhaphy Compared with Pelvic Floor Muscle Therapy in Women with Late Consequences of a Poorly Healed Second-Degree Perineal Tear. Obstet. Gynecol. 2020, 135, 341–351. [Google Scholar] [CrossRef] [Green Version]
- Taithongchai, A.; Veiga, S.I.; Sultan, A.H.; Thakar, R. The consequences of undiagnosed obstetric anal sphincter injuries (OASIS) following vaginal delivery. Int. Urogynecol. J. 2020, 31, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Kudish, B.; Sokol, R.J.; Kruger, M. Trends in major modifiable risk factors for severe perineal trauma, 1996–2006. Int. J. Gynecol. Obstet. 2008, 102, 165–170. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.A.; Price, N.; Simonite, V.; Burns, E.E. Incidence of and risk factors for perineal trauma: A prospective observational study. BMC Pregnancy Childbirth 2013, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Aigmueller, T.; Umek, W.; Elenskaia, K.; Frudinger, A.; Pfeifer, J.; Helmer, H.; Huemer, H.; Tammaa, A.; van der Kleyn, M.; Tamussino, K.; et al. Guidelines for the management of third and fourth degree perineal tears after vaginal birth from the Australian Urogynecology Working Group. Int. Urogynecol. J. 2013, 24, 553–558. [Google Scholar] [CrossRef]
- Monteiro, M.V.D.C.; Pereira, G.M.V.; Aguiar, R.A.P.; Azevedo, R.L.; Correia-Junior, M.D.; Reis, Z. Risk factors for severe obstetric perineal lacerations. Int. Urogynecol. J. 2016, 27, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, D.S.; Thakar, R.; Sultan, A.H. Obstetric anal sphincter injuries: Review of anatomical factors and modifiable second stage interventions. Int. Urogynecol. J. 2015, 26, 1725–1734. [Google Scholar] [CrossRef]
- Ochandorena-Acha, M.; Noell-Boix, R.; Yildirim, M.; Cazorla-Sánchez, M.; Iriondo-Sanz, M.; Troyano-Martos, M.J.; Casas-Baroy, J.C. Experiences and coping strategies of preterm infants’ parents and parental competences after early physiotherapy intervention: Qualitative study. Physiother. Theory Pract. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Beaumont, T. Consumer Evaluation of Antenatal Physiotherapy Education: How Useful Was It Really? Int. J. Childbirth 2018, 8, 87–100. [Google Scholar] [CrossRef]
- Ray-Griffith, S.L.; Wendel, M.P.; Stowe, Z.N.; Magann, E.F. Chronic pain during pregnancy: A review of the literature. Int. J. Women’s Health 2018, 10, 153–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallo, R.B.S.; Santana, L.S.; Marcolin, A.C.; Duarte, G.; Quintana, S.M. Sequential application of non-pharmacological interventions reduces the severity of labour pain, delays use of pharmacological analgesia, and improves some obstetric outcomes: A randomised trial. J. Physiother. 2018, 64, 33–40. [Google Scholar] [CrossRef]
- Farrag, R.E.; Omar, A.M. Using of Birthing Ball during the first Stage of Labor: Its Effect on the Progress of Labor and Outcome among Nulliparous Women. Int. J. Nurs. Didact. 2018, 8, 1–10. [Google Scholar] [CrossRef]
- Badaoui, A.; Kassm, S.A.; Naja, W. Fear and Anxiety Disorders Related to Childbirth: Epidemiological and Therapeutic Issues. Curr. Psychiatry Rep. 2019, 21, 27–30. [Google Scholar] [CrossRef]
- Toivanen, R.A.; Korja, R.; Saisto, T.; Rouhe, H.; Muotka, J.; Salmela–Aro, K. Changes in emotions and personal goals in primiparous pregnant women during group intervention for fear of childbirth. J. Reprod. Infant Psychol. 2018, 36, 363–380. [Google Scholar] [CrossRef] [Green Version]
- Dieb, A.S.; Shoab, A.Y.; Nabil, H.; Gabr, A.; Abdallah, A.A.; Shaban, M.M.; Attia, A.H. Perineal massage and training reduce perineal trauma in pregnant women older than 35 years: A randomized controlled trial. Int. Urogynecol. J. 2019, 31, 613–619. [Google Scholar] [CrossRef]
- Shahoei, R.; Hashemi-Nasab, L.; Gaderkhani, G.; Zaheri, F.; Shahoei, F. The impact of perineal massage during pregnancy on perineal laceration during childbirth and postpartum: A randomized clinical trial study. Chronic Dis. J. 2018, 4, 13–20. [Google Scholar]
- Schreiner, L.; Crivelatti, I.; De Oliveira, J.M.; Nygaard, C.C.; Dos Santos, T.G. Systematic review of pelvic floor interventions during pregnancy. Int. J. Gynecol. Obstet. 2018, 143, 10–18. [Google Scholar] [CrossRef]
- Beckmann, M.M.; Stock, O.M. Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst. Rev. 2013, 4, CD005123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romina, S.; Ramezani, F.; Falah, N.; Mafi, M.; Ranjkesh, F. Effect of Perineal Massage with Ostrich Oil on the Episiotomy and Lacerations in Nulliparous Women: A Randomized Controlled Clinical Trial. Iran. J. Nurs. Midwifery Res. 2020, 25, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Garson, G.D. Testing Statistical Assumptions; Statistical Associates Publishing: Raleigh, NC, USA, 2012. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Laurence Erlbaum Associates: Hillsdale, MI, USA, 1988. [Google Scholar]
- Macarthur, A.J.; Macarthur, C. Incidence, severity, and determinants of perineal pain after vaginal delivery: A prospective cohort study. Am. J. Obstet. Gynecol. 2004, 191, 1199–1204. [Google Scholar] [CrossRef]
- Manresa, M.; Pereda, A.; Goberna-Tricas, J.; Webb, S.S.; Terre-Rull, C.; Bataller, E. Postpartum perineal pain and dyspareunia related to each superficial perineal muscle injury: A cohort study. Int. Urogynecol. J. 2020, 31, 2367–2375. [Google Scholar] [CrossRef] [PubMed]
- Abdelhakim, A.M.; Eldesouky, E.; Elmagd, I.A.; Mohammed, A.; Farag, E.A.; Mohammed, A.E.; Hamam, K.M.; Hussein, A.S.; Ali, A.S.; Keshta, N.H.A.; et al. Antenatal perineal massage benefits in reducing perineal trauma and postpartum morbidities: A systematic review and meta-analysis of randomized controlled trials. Int. Urogynecol. J. 2020, 31, 1735–1745. [Google Scholar] [CrossRef]
- Viannay, P.; de la Codre, F.; Brochard, C.; Thubert, T.; Meurette, G.; Legendre, G.; Venara, A. Management and consequences of obstetrical anal sphincter injuries: Review. J. Visc. Surg. 2021, 158, 231–241. [Google Scholar] [CrossRef]
- Demirel, G.; Golbasi, Z. Effect of perineal massage on the rate of episiotomy and perineal tearing. Int. J. Gynecol. Obstet. 2015, 131, 183–186. [Google Scholar] [CrossRef]
- Zare, O.; Pasha, H.; Faramarzi, M. Effect of perineal massage on the incidence of episiotomy and perineal laceration. Health 2014, 6, 10–14. [Google Scholar] [CrossRef]
- Prosser, S.J.; Barnett, A.G.; Miller, Y.D. Factors promoting or inhibiting normal birth. BMC Pregnancy Childbirth 2018, 18, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Edqvist, M.; Blix, E.; Hegaard, H.K.; Ólafsdottir, O.Á.; Hildingsson, I.; Ingversen, K.; Mollberg, M.; Lindgren, H. Perineal injuries and birth positions among 2992 women with a low risk pregnancy who opted for a homebirth. BMC Pregnancy Childbirth 2016, 16, 196–203. [Google Scholar] [CrossRef] [PubMed]
- The Epidural and Position Trial Collaborative Group. Upright versus lying down position in second stage of labour in nulliparous women with low dose epidural: BUMPES randomised controlled trial. BMJ 2017, 359, j4471. [Google Scholar] [CrossRef] [Green Version]
- Davidson, K.; Jacoby, S.; Brown, M.S. Prenatal Perineal Massage: Preventing Lacerations during Delivery. J. Obstet. Gynecol. Neonatal Nurs. 2000, 29, 474–479. [Google Scholar] [CrossRef]
| All (n = 90) | Control (n = 30) | Self-Massage (n = 30) | Massage (n = 30) | |
|---|---|---|---|---|
| Age (years) | 32.7 ± 3.9 | 31.4 ± 4.4 a,b | 33.2 ± 3 a | 33.6 ± 3.8 b |
| Height (cm) | 163.8 ± 6 | 163.2 ± 5.8 | 164 ± 5.2 | 164.2 ± 6.9 |
| Weight (kg) | 57.9 ± 7.9 | 58 ± 8.6 | 59 ± 8.5 | 56.7 ± 6.3 |
| Body Mass Index (kg/m2) | 21.6 ± 2.7 | 21.7 ± 2.6 | 21.9 ± 2.7 | 21.2 ± 2.8 |
| Weight gain (kg) | 12 ± 4.1 | 12.3 ± 4.5 | 12.4 ± 4.1 | 11.3 ± 3.7 |
| Deliveries (n°) | 1.4 ± 0.5 | 1.4 ± 0.5 | 1.3 ± 0.5 | 1.5 ± 0.6 |
| Labour week (n°) | 39.3 ± 1.8 | 38.8 ± 2.4 | 39.6 ± 1.5 | 39.4 ± 1.3 |
| Baby weight (kg) | 3.3 ± 0.4 | 3.2 ± 0.6 | 3.3 ± 0.3 | 3.3 ± 0.3 |
| Duration of labour (hours) | 10.7 ± 7.9 | 9.6 ± 6.6 | 12.8 ± 9.1 | 10 ± 7.9 |
| Perineal pain (points) | 2 ± 2.5 | 2.8 ± 3 b | 2.3 ± 2.5 c | 1 ± 1.5 b,c |
| All (n = 90) | Control (n = 30) | Self-Massage (n = 30) | Massage (n = 30) | |
|---|---|---|---|---|
| Episiotomy | 37 (41.1) | 20 (66.7) | 14 (46.7) | 3 (10) |
| Perineal tear | ||||
| No | 55 (61.1) | 18 (60) | 21 (70) | 22 (73.4) |
| Mild | 29 (32.2) | 8 (26.7) | 7 (23.3) | 7 (23.3) |
| Moderate/severe | 6 (6.7) | 4 (13.3) | 2 (6.7) | 1 (3.3) |
| Position | ||||
| Lithotomy | 69 (76.7) | 27 (90.1) | 24 (80) | 18 (60.1) |
| Sideways | 5 (5.6) | 1 (3.3) | 3 (10) | 1 (3.3) |
| Sit/squat | 13 (14.4) | 1 (3.3) | 2 (6.7) | 10 (33.3) |
| Standing | 3 (3.3) | 1 (3.3) | 1 (3.3) | 1 (3.3) |
| Instrumental | ||||
| No | 72 (80) | 20 (66.7) | 25 (83.3) | 27 (90) |
| Vacuum | 11 (12.2) | 6 (20) | 2 (6.7) | 3 (10) |
| Forceps | 7 (7.8) | 4 (13.3) | 3 (10) | 0 (0) |
| Analgesia | ||||
| No | 19 (21.1) | 6 (20) | 5 (16.7) | 8 (26.7) |
| Local | 2 (2.2) | 1 (3.3) | 1 (3.3) | 0 (0) |
| Epidural | 69 (76.7) | 23 (76.7) | 24 (80) | 22 (73.3) |
| Variable | Mild Tear | Moderate/Severe Tear | ||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Massage group | ||||
| Control | 1 | 1 | ||
| Self-massage | 2.22 | 0.68–7.25 | 0.89 ** | 0.68–9.63 |
| Massage | 0.25 * | 0.02–10.32 | 0.34 ** | 0.13–7.82 |
| Weight gain | ||||
| <10 | 1 | 1 | ||
| 11–15 kg | 1.78 | 0.67–4.73 | 0.35 | 0.02–3.71 |
| 16–20 kg | 0.95 | 0.21–4.27 | 0.88 | 0.08–8.98 |
| 21–25 kg | 1.27 | 0.1–15.5 | 2.13 | 0.02–9.36 |
| Delivery position | ||||
| Lithotomy | 1 | 1 | ||
| Sideways | 1.65 | 0.25–10.67 | 3.98 | 2.36–9.36 |
| Sit/squat | 2.12 | 0.63–7.14 | 4.28 | 0.69–12.37 |
| Standing | 4.95 | 4.23–57.9 | 5.23 | 4.63–11.68 |
| Analgesia | ||||
| No | 1 | 1 | ||
| Local | 1.11 | 0.06–20.48 | 3.75 | 1.69–8.31 |
| Epidural | 0.45 | 0.16–1.28 | 1.06 | 0.11–10.12 |
| Instrumental | ||||
| No | 1 | 1 | ||
| Vacuum | 0.38 | 0.07–1.88 | 4.4 | 0.64–30.4 |
| Forceps | 0.34 | 0.08–1.88 | 1.88 | 0.45–16.35 |
| Episiotomy | ||||
| No | 1 | 1 | ||
| Yes | 0.4 | 0.06–1.96 | 1.4 | 0.02–13.54 |
| Massage group | 0.48 * | 0.01–3.14 | 0.53 ** | 0.26–8.35 |
| Weight gain | 1.11 | 0.64–1.91 | 0.67 | 0.2–2.26 |
| Delivery position | 1.54 | 0.93–2.53 | 2.2 | 0.36–6.32 |
| Analgesia | 0.67 | 0.4–1.12 | 1.05 | 0.33–3.31 |
| Instrumental | 0.56 | 0.25–1.25 | 0.88 | 0.26–3 |
| Episiotomy | 0.49 | 0.36–1.68 | 0.59 | 0.26–2.69 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez-González, M.; Leirós-Rodríguez, R.; Álvarez-Barrio, L.; López-Rodríguez, A.F. Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial. J. Clin. Med. 2021, 10, 4934. https://doi.org/10.3390/jcm10214934
Álvarez-González M, Leirós-Rodríguez R, Álvarez-Barrio L, López-Rodríguez AF. Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial. Journal of Clinical Medicine. 2021; 10(21):4934. https://doi.org/10.3390/jcm10214934
Chicago/Turabian StyleÁlvarez-González, María, Raquel Leirós-Rodríguez, Lorena Álvarez-Barrio, and Ana F. López-Rodríguez. 2021. "Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial" Journal of Clinical Medicine 10, no. 21: 4934. https://doi.org/10.3390/jcm10214934
APA StyleÁlvarez-González, M., Leirós-Rodríguez, R., Álvarez-Barrio, L., & López-Rodríguez, A. F. (2021). Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial. Journal of Clinical Medicine, 10(21), 4934. https://doi.org/10.3390/jcm10214934








