Abstract
Background: Both lung transplant recipients and candidates are characterised by reduced training capacity and low average quality of life (QoL). This review investigates the impact of training on exercise ability and QoL in patients before and after lung transplant. Methods: Searches were conducted from the beginning to 7 March 2022 using the terms “exercise,” “rehabilitation,” “lung transplant,” “exercise ability,” “survival,” “quality of life” and “telerehabilitation” in six databases, including Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, CINAHL, Nursing and Allied Health, and Scopus. The inclusion criteria were studies evaluating the effects of an exercise training programme concurrent with lung transplantation as well as patients and candidates (>18 years old) through any lung diseases. The term “lung transplant rehabilitation” was used to refer to all carefully thought-out physical activities with the ultimate or intermediate objective of improving or maintaining physical health. Results: Out of 1422 articles, 10 clinical- and 3 telerehabilitation studies, candidates (n = 420) and recipients (n = 116) were related to the criteria and included in this review. The main outcome significantly improved in all studies. The 6-min walk distance, maximum exercise capacity, peak oxygen uptake, or endurance for constant load rate cycling improved measuring physical activity [aerobic exercises, breathing training, and aerobic and inspiratory muscle training sessions (IMT)]. Overall scores for dyspnoea improved after exercise training. Furthermore, health-related quality of life (HRQOL) also improved after aerobic exercise training, which was performed unsupervised or accompanied by breathing sessions. Aerobic training alone rather than combined with inspiratory muscle- (IMT) or breathing training enhanced exercise capacity. Conclusion: In conclusion, rehabilitation programmes seem to be beneficial to patients both preceding and following lung transplantation. More studies are required to determine the best training settings in terms of time scale, frequency, and work intensity in terms of improving exercise ability, dyspnoea, and HRQOL.
1. Introduction
Lung transplantation (LTx) has become a clinical reality for patients since the mid-1980s who suffer from end-stage lung disease. On the basis of statistics from the International Society for Heart and Lung Transplantation (ISHLT) database, the median patient survival among all indications was 6.7 years from 2010 to June 2017. The average survival for patients after the first year LTx is 8.9 years. Idiopathic interstitial pneumonia (IIP, 32.4%), chronic obstructive pulmonary disease (COPD, 26.1%), and cystic fibrosis (CF, 13.1%) are the predominant indications for LTx. Over the past decade, almost 4000 LTx have been reported worldwide each year [1]. To date, we are facing huge challenges, in particular, the imbalance of supply and demand among donors. This can result in an average waiting list of 326 days in the UK [2]. During this time, LTx candidates continue to suffer from medical chronicity, ventilatory restriction, training intolerance, and inactivity in everyday activities [2]. Quality of life (QoL) and peripheral and diaphragmatic muscle impairment are manifested [1,2,3]. Therefore, it is primordial to maintain a minimum daily functional capacity and prevent more complications [1,4,5]. Lung transplant rehabilitation is a highly recommended therapy for patients with long-term lung diseases who are simultaneously recovering after a transplant operation or candidates for LTx, [1,2]. There is a significant improvement in pulmonary functions after transplantation. However, the QoL is still limited by several factors, including early-onset metabolic acidosis, reduced daily exercise capacity (40–60%) of anticipated normal values, and skeletal muscle weakness [1,2,3]. In the early post-transplant period, prolonged hospital and intensive care unit (ICU) stays, which can last three to six weeks or longer if issues arise, result in prolonged inactivity and sedentary behaviour [1,2]. Furthermore, immunosuppressant medications continuously used after surgery have negative effects on the molecular structure of the skeletal muscle [1,2] and have a significant detrimental impact on HRQoL due to psychological stress [1,2,3]. When LTx patients and healthy people are compared one year after surgery, standing and walking time is dramatically reduced. However, daily sedentary time is still high [1,2,3], which might be partially explained by the malfunctioning peripheral muscles [3,4,5]. Quadriceps strength and muscle mass losses are also observed [1,2,3,4,5].
In these circumstances, exercise-based rehabilitation programmes should visibly improve the physical functioning, exercise tolerance, and levels of physical capacity of patients. In this review, the available data for rehabilitation interventions and the duration of hospitalisation will be investigated in the pre-transplant, early (≤12 months after surgery), and late (>1 year after emission regarding lung transplant procedure) post-transplant periods. Both evidence-based and empirical data will be proposed, and guidelines will be in focus for additional research.
2. Materials and Methods
From the beginning through 7 March 2022, searches were made in six databases, including the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, Scopus, Nursing and Allied Health, and CINAHL. These six databases were selected because they can be used in related systematic reviews and applied to clinical research. Medical topic headings (MeSH) relating to “rehabilitation,” “lung transplant,” “training exercise,” “exercise training capacity,” “quality of life,” “telerehabilitation.” and “survival” were the focus of the database-specific research methodologies.
As no translator was available, the search was limited to peer-reviewed articles in English. The authors separately evaluated the titles and abstracts to see whether the papers adhered to the predetermined PICOS (population, intervention, comparators, outcomes, and study design) standard. Lung transplant recipients and candidates (>18 years old) with any lung diseases met the inclusion criteria, and studies evaluating the effects of an exercise training regimen met the intervention criteria. Every planned and organised physical activity with the immediate or long-term goal of preserving or enhancing physical health was included in this definition.
A passive control group, an active training control group, or a specific dose, environment, or type of exercise were contrasted in randomised clinical trials (RCTs). They also looked into clinical outcomes (hospitalisations, length of stay in hospital or intensive care unit (ICU), and survival) as well as exercise training outcomes (6 min walk test (6MWT), endurance shuttle walk test (ESWT), incremental shuttle walk test (ISWT), or cardiopulmonary exercise test (CPET). General or respiratory questionnaires assessed the QoL, including HRQoL and psychological health.
3. Results
The six databases were searched, and 1,422 articles were found, mostly from PubMed/Medline (814), Cochrane Library (201), Nursing and Allied Health (172), Scopus (318), and CINAHL (89). After filtering full-text publications, 10 + 3 articles were found eligible and were included in the review. Figure 1 shows the PRISMA flow diagram of the article screening procedure.
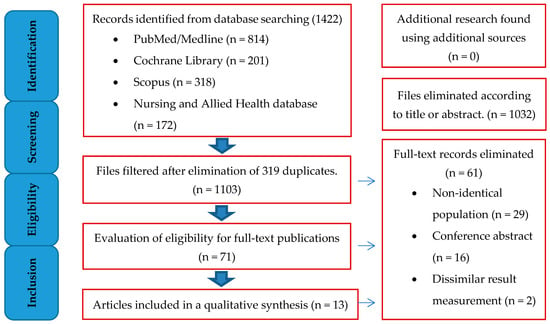
Figure 1.
PRISMA flow diagram for articles involved in selection process.
- Pretransplant rehabilitation studies
Pre-transplant candidates were included in eight studies out of ten (n = 420) with a median age of 51 years (ranging from 35 to 58 years) and an anticipated mean forced expiratory volume in 1 s (FEV1%pred) of 22 to 49%. Male applicants made up 43 to 95% of the study participants (median: 58%).
Pre-transplant studies included three randomized controlled trials (RCT) [2,3,4], two quasi-experimental studies [5,6], one cohort study, and two telerehabilitation research. Seven of eight trials [2,3,4,5,6,7] combined resistance and aerobic training, but only one [6] used Nordic Walking. Inpatient protocols were used in four research studies [2,4,6,8], whereas integrated inpatient and home-based exercise were used in two investigations [3,5]. The training sessions varied in frequency, with two to six sessions per week, and the duration of the programme was between four and twelve weeks (Table 1).

Table 1.
Pretransplant rehabilitation studies.
- Post-transplant rehabilitation studies
Four out of the thirteen studies included post-transplant patients (n = 116), whose mean forced expiratory volume in 1 s (FEV1%pred) expected values varied from 73 to 81% and whose average age was 52 years (range from 47 to 58). Male participants made up 46 and 95% of the total population (mean: 61%). There were two RCTs [2,8], one quasi-experimental [11], one pilot research study [12], a and a telerehabilitation study (home-based pulmonary rehabilitation) [13] among the post-transplant investigations. One study looked at the impact of the HIIT programme [8], and four investigations were conducted as inpatient protocols [2,11,12]. Three to five training sessions were held each week, with training programmes lasting between three and twenty weeks (Table 2).

Table 2.
Post-transplant rehabilitation studies.
3.1. Results of Pre-Transplant Pulmonary Rehabilitation
The 6MWDT was used in all six personal pre-transplant research studies to assess exercise ability after the rehabilitation programme. The outcome significantly improved in five of the studies. However, Kerti et al. [2] found no appreciable change in handgrip strength (HGS) or 6MWD after the programme. Gloeckl R et al. [4] also looked into the distinction between interval and continuous training. They claimed that no differences existed between the two research groups, and both groups successfully increased the 6MWD by a homogenous substantial amount: 29–35 m for the interval training group and 36–43 m for the continuous training group. According to Ochman M et al. [6], Nordic walking increased the distance by 6MWT in a statistically significant way after a 12-week programme. The rehabilitation programme was combined with aerobic and resistance training in all six studies (Table 1).
QoL was evaluated in four pre-transplant studies, two of them [6,7] employed the SF-36 questionnaire, which produced two total scores and eight scales; the mental elements summary (MES) and the physical elements summary (PES), whereas one study [2] used the CAT questionnaire. Florian J et al. [5] examined the number of days spent on invasive mechanical ventilation (IMV) as well as the length of stay (LOS) in the hospital and the intensive care unit (ICU) after LTx in terms of survival following LTx. The SF-36 questionnaire was used in this study, but the findings ran counter to the LOS. After the PR programme, Fontoura F et al. [7] discovered that four key dimensions (vitality, emotional role, mental health, and physical functioning) of HRQL improved considerably. Ochman M et al. [6] found no statistically significant differences in QoL. According to Florian J et al. [5], the survival rate in the pulmonary rehabilitation programme (PRP) group (89.9%) was higher than in the control group (62.9%) during the follow-up period. The experimental group had a shorter hospital stay overall (20d PRP vs. 25d CG, p = 0.046) and a shorter ICU stay (five days vs. seven days, p = 0.004) than the control group. The PRP group had higher survival rates during the five-year follow-up period of lung transplantation (89.9% vs. 60.9%, with p < 0.001) and reported lower mortality rates during ICU stays (p = 0.006).
3.2. Results of Post-Transplant Pulmonary Rehabilitation
Five different tests were applied to evaluate the exercise capacity in the post-transplant group of patients: 6MWT [2,12], muscle strength hand and quadriceps power (1 RM) [8,11], peak oxygen uptake (VO2peak) [8], and endurance and incremental shuttle walk (ISWT, ESWT) tests [11]. Ulvestad M et al. [8] found that the mixed-mode HIIT, aerobic combined with resistance training 3 times/week for 20 weeks, improved muscular strength, although VO2peak did not improve rather to normal care after the operation. Candemir I et al. [11] reported significant improvement in endurance and incremental shuttle walk (ISWT, ESWT) tests, the distance of ISWT before PR (23%) of predicted to 36% following PR (p < 0.001), and the average score of quadriceps in one maximal repetition increased from 12 (6–17) kg to 13 (8–20) kg following PR with a significant difference (p < 0.001). Handgrip force in both hands (p < 0.05) improved after PR. For the 6MWD, both studies reported an increase in the distance of 6MWT. However, Andrianopoulos V et al. [12] reported a statistically significant difference (6-min walk test +86 m; p < 0.001), and Kerti M et al. [2] reported an improvement; however, it was not significant (Table 2).
QoL was evaluated in three out of four post-transplant studies. The following questionnaires were used: CAT [2], the SF-36 questionnaire [8], St George’s Respiratory function questionnaire, the Chronic Pulmonary Sickness questionnaire, Chronic Respiratory Sickness Questionnaire (CRQ), and the Hospital Anxiety Depression Scale (HADS) for psychological, mental health [11]. Neuropsychological testing for cognitive assessment was based on the Intelligence Quotient test (IQ) and the Stroop colour-word test [12]. Both Candemir I et al. [11] and Andrianopoulos V et al. [12] investigated the effect of the early post-transplant period two months after LTx operation and one month later. They reported statistically significant improvements in body composition, QoL, and psychological health status after the programme [11] and a statistically significant difference (ES latitude 0.23–1.00; p ≤ 0.34) in 50% of the cognitive exams measuring memory and learning capacity (ES scores 0.62 and 0.31, respectively), was detected [12]. Ulvestad M et al. [8] reported significant improvement in HRQoL in the late post-transplant from six to 60 months after LTx (Table 2).
4. Discussion
This study showed how training regimens affected physical function and improved QoL for patients with LTx. Although it has been hypothesised in the literature that a rehabilitation exercise training regimen can preserve or improve fitness capacity both before and after the transplant, the information currently available is restricted to non-randomised and observational research, and results have poor quality outcomes. The 6MWT is a crucial tool to assess the successful outcomes of the rehabilitation programme if the distance tends to exceed the minimal clinically relevant difference (MCID) set for chronic respiratory diseases [14,15]. The bulk of our studies shows that the training regimens have positive effects on physical function as well as enhancements in QoL for patients with LTx.
Kerti M et al. [2] reported a reduction in HGS following the transplantation and improvement after the rehabilitation training in FVC%pred, FEV1%pred, chest mobility, BHT, and QoL two months after the lung transplant. However, 6MWD remained at the same level in the post-transplant group. These results are similar to the results of Maury et al. [16]. In the study by Maury, the exercise training programme improved the functional components before the surgery, too. This study demonstrated significant improvement in the training capacity, chest wall expansion, and QoL. In a study by Kılıç L et al. [3], the average distance of 6MWT was 300 (70–524) meters (m) before the training and increased to an average of 360 m (60 m increase, p = 0.018) after the training protocol. The dyspnoea scale scores also improved significantly after the training. Dyspnoea is a major symptom of end-stage lung disease in people who are potential candidates for lung transplants [17]. PR has already been shown to reduce dyspnoea [18], and focusing on the diaphragm muscle during training improves the MRC dyspnoea scale significantly [19]. Thus, the average pre- and post-training MRC outcomes were statistically different (p = 0.008). The British Thoracic Society recommends a rehabilitation programme twice a week for six weeks under direct supervision [20]. However, some researchers found that a PR programme was ineffective twice a week for eight weeks [21]. In this programme, patients reported a reduction in muscle weakness and less pain at the end of the test alongside improvement in the distance in the 6-min walk test after rehabilitation. Current data suggested that pre-transplant rehabilitation could guarantee greater gains in the early stage [22]. Florian J et al. [5] are some of the few scientists who have looked into how a pre-transplant rehabilitation programme affects the survival and mortality of lung transplant patients. They found that 9.0% of PRP patients needed IMV longer than 24 h (compared to 41.6% in the control group), highlighting the crucial part that PRP plays in the recovery process after lung transplantation [23,24]. However, the prediction of mortality following LTx was not correlated with risk factors previously associated with early mortality, such as sex (male sex > 65), age (55), and one-lung transplant [25,26]. This conclusion can be explained by the fact that most of the individuals in this group were under the age of 65. Interval training versus continuous exercise for lung transplant patients was examined by Gloeckl R et al. [4]. Both interval and continuous training may result in equivalent increases in an exercise training capacity. These results are consistent with those of the earlier research findings by Puhan et al. [27]. In their study, there was no dissimilation within groups in terms of physical training or HRQoL, but both groups showed physiological benefits. The same research team showed in a second study that aerobic enzyme activity and the cross-sectional areas of type I and IIa fibers improved equally with IT and CT [28]. Leg fatigue and dyspnoea levels in the IT group were significantly lower than in the CT group. The CT group required significantly more breaks during the endurance workout. The number of breaks also rose over time, even though the IT group was able to keep the same frequency of pauses during training.
Following bilateral lung transplantation, Candemir I et al. [29] examined the effectiveness of outpatient pulmonary rehabilitation two months after the procedure. Body mass index (BMI) and fat-free mass index (FFMI) increased, according to his study. Baseline BMI was also connected with improvements in functional ability, and quadriceps muscular power was seen as a key indicator of an increase in muscle mass. Skeletal, muscular power, training potential, and QoL dramatically improved after rehabilitation. After PR, the ISWT distance improved from an expected 23% to a predicted 36%. Similar outcomes were shown in another trial when muscle strength and exercise duration increased in the early post-transplant period following a home-based training programme [30]. There is still some uncertainty over the best time for PR after lung transplantation. A randomised research study found that, compared to recipients who had no PR at all [31], lung transplant recipients who undertook an early PR programme (the first three months after surgery) had higher fitness, physical activity, and a decrease in 24 h blood pressure one year after LTx. In this study, the average postoperative time before PR was 75 +/− 15 days, which can be considered an early stage of rehabilitation.
Another review from 2010 reveals that skeletal muscle power, the functional and maximal ability for exercise, and QoL significantly improve in recipients following a training programme that began as early as the first month and lasted at least six months following LTx [29]. According to Andrianopoulos V et al. [12], lung transplant recipients with COPD as an underlying disease showed a number of benefits after participating in PR in functional as well as cognitive skills. Taking part in a three-week rehabilitation programme leads to multifactorial benefits in the early post-transplant period; it correlated with a faster and more convenient recovery one month after surgery. In this study, lung transplant recipients showed a significant amelioration of physical capacity evaluated by the 6MWT following a three-week rehabilitation programme. In terms of exercise tolerance, 6MWD (350 m) for COPD patients who underwent LTx due to a prior medical condition, poor health status, a lengthy hospital stay, as well as extended periods of inactivity additionally improved by 86 m following PR discharge. The findings of Munro et al. [32] indicated a gain of 95 m following a seven-week outpatient post-transplant PR, which is comparable to this large increase.
A study by Ulvestad M. et al. [8] examining the impact of peak oxygen uptake and muscle strength after intense exercise for six to sixty months following surgery discovered that HIIT significantly increased muscle power, which was accounted by an improvement of 11% in the 1RM leg press. The benefits of the HIIT programme seem to be the greatest for people who have had lung transplants, suggesting that HIIT helps hasten recovery. Langer et al. [31] evaluated the outcomes of a low- to moderate-intensity 12-week endurance and resistance training programme. No difference was observed in VO2peak in contrast to a control group receiving activity therapy in the intervention group. In earlier non-randomised controlled trials, exercise training significantly affected VO2peak [33,34]. These uncontrolled data, however, were unable to distinguish between the impacts of exercise training and the course of the normal recuperation of the body after LTx.
The SF-36 questionnaire, a universal tool for HRQoL evaluations, was the most frequently applied tool for QoL measurements [35]. It can be difficult to focus on changes in SF-36 scores when developing a basic diagnosis, although MCID for LTx candidates has not yet been established. A study shows a value of MCID of >2–4 points for PCS and MCS scores [35], and general recommendations call for an MCID of four points [34]. Lower training symptoms (dyspnoea and lower limb tiredness) for this type of training (HIIT) led to an increase in SF-36 MCS scores with time [4,8,36,37]. QoL scores did not alter considerably, according to the findings of Candemir I et al. [32]. The number of physical function domains increased (SF-36, SGRQ activity domain, and PCS). When HRQoL scores in LTx were compared with normal, the greatest disadvantage was observed in the variation of physical health rather than any other mental health domain [29].
4.1. Telerehabilitation in Pulmonary Rehabilitation
Restrictions imposed due to the COVID-19 pandemic have had a negative impact on the healthcare system, including the rehabilitation of patients [38]. Telerehabilitation, as with any other technology, the primary problem is always accessibility, e.g., no stable internet connection, no smartphone app, no tablet/laptop, and no stable mobile internet access. Telerehabilitation is defined as the delivery of rehabilitation at a distance using a variety of information communication technologies, e.g., live video conferences, mobile apps, automated chatbots, etc. [38,39]. To date, little is known about the efficacy and effectiveness of telerehabilitation in lung transplant patients. However, there are some initial published results, e.g., an eight-week telerehabilitation programme was safe and effective, with increased patient exercise capacity, physical activity, lower limb strength, and improved balance [9,10,40]. Preoperative telerehabilitation is multimodal and has been shown to reduce postoperative complications and accelerate recovery, thus reducing morbidity and hospitalization [41]. Post-operative telerehabilitation in terms of physical activity can be varied, but in general, it always depends on the procedure and the region affected. Physiotherapy aims to fully restore range of motion and muscle imbalance, and an important adjunct is individualising nutritional therapy and psychotherapy, resulting in improved QoL for patients [9,41,42].
One of the undesirable effects of the COVID-19 pandemic is increased passive time at home, resulting in decreased cardiopulmonary capacity, muscle mass, and muscle strength, whereas regular exercise and physical activity significantly reduce fatigue and psychosocial dysfunction while increasing aerobic fitness, optimising body composition and QoL [43]. Resistance exercise increases contractile protein mass, reduces sarcopenia and body fat in rehabilitation participants, and increases muscle strength; sub-intensive aerobic exercise increases the mitochondrial number and oxidative enzyme activity in skeletal muscles and develops more efficient mitochondrial regulation in the body [44]. A number of studies suggest [10,13,41,45] that telerehabilitation is cost-effective and associated with patient satisfaction and adherence, but there are still underdeveloped components of telerehabilitation that need to be improved. Nevertheless, telerehabilitation is a very promising option for patient care, not only during the pandemic but also as a maintenance part of normal rehabilitation based on face-to-face encounters.
4.2. Limitations of the Study
Our review was a review and not a systematic review of the literature, so studies may have been omitted. We focused primarily on RCT studies in English, so publications in other languages may have been omitted from the review. Due to manuscript length limitations, conference abstracts and meta-analyses were not included in this mini-review. Focusing on the exception of pre-transplant 6MWT, there is a lot of variation in the studies’ descriptions of the rehabilitation programmes, as well as what is measured afterward and when. There is probably a selection bias (because of the different physical conditions of the patients or who are being entered into the outpatient versus inpatient programmes).
5. Conclusions
In conclusion, rehabilitation programmes seem to be advantageous to patients both before and after lung transplantation. To achieve gains in exercise capacity, dyspnoea, and HRQoL, appropriate exercise parameters in terms of intensity, frequency, and duration are unavoidable. It is important to conduct more studies on the immediate and long-term impact of physical activity and/or training on survival and mortality, transplant rejection, risk, hypertension, infection rates, the onset of diabetes and/or obesity, and other effects on QOL.
Author Contributions
Conceptualization: Y.A. and J.T.V.; methodology: Z.K. and A.B.; software M.F.; validation: S.N., I.M., and J.T.V.; formal analysis: L.B. and K.T.; investigation Y.A., I.M., and J.T.V.; resources: L.B. and A.B.; data curation M.F., Z.K., and Y.A.; writing—original draft preparation: all authors; writing—review and editing: all authors; visualization: S.N., I.M., and M.F.; supervision: J.T.V.; project administration: Y.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| BHT | Breath Holding Time |
| BMI | Body Mass Index |
| CF | Cystic Fibrosis |
| CG | Control Group |
| COPD | Chronic Obstructive Pulmonary Disease |
| CPET | Cardiopulmonary Exercise Test |
| CT | Continuous Training |
| FEV1 | Forced Expiratory Volume in one Second |
| FFMI | Fat-Free Mass Index |
| FVC | Forced Vital Capacity |
| HGS | Hand Grip Strength |
| HIIT | High-Intensity Interval Training |
| HRQoL | Health-related Quality of Life |
| ICU | Intensive Care Unit |
| IIP | Idiopathic Interstitial Pneumonia |
| ISHLT | International Society for Heart and Lung Transplantation |
| IT | Interval Training |
| LTx | Lung Transplantation |
| MeSH | Medical Subject Headings |
| PRP | Pre-Rehabilitation Program |
| Qol | Quality of Life |
| RCT | Randomized Controlled Trials |
| 6MWD | Six-minute Walk Distance |
| 6MWT | Six-minute Walk Test |
References
- Hume, E.; Ward, L.; Wilkinson, M.; Manifield, J.; Clark, S.; Vogiatzis, I. Exercise training for lung transplant candidates and recipients: A systematic review. Eur. Respir. Rev. 2020, 29, 200053. [Google Scholar] [CrossRef]
- Kerti, M.; Bohacs, A.; Madurka, I.; Kovats, Z.; Gieszer, B.; Elek, J.; Renyi-Vamos, F.; Varga, J.T. The effectiveness of pulmonary rehabilitation in connection with lung transplantation in Hungary. Ann. Palliat. Med. 2021, 10, 3906–3915. [Google Scholar] [CrossRef]
- Kilic, L.; Pehlivan, E.; Balci, A.; Bakan, N.D. Effect of 8-week Pulmonary Rehabilitation Program on Dyspnea and Functional Capacity of Patients on Waiting List for Lung Transplantation. Turk. Thorac. J. 2020, 21, 110–115. [Google Scholar] [CrossRef]
- Gloeckl, R.; Halle, M.; Kenn, K. Interval versus continuous training in lung transplant candidates: A randomized trial. J. Heart Lung Transplant. 2012, 31, 934–941. [Google Scholar] [CrossRef]
- Florian, J.; Watte, G.; Teixeira, P.J.Z.; Altmayer, S.; Schio, S.M.; Sanchez, L.B.; Nascimento, D.Z.; Camargo, S.M.; Perin, F.A.; Camargo, J.D.J.; et al. Pulmonary rehabilitation improves survival in patients with idiopathic pulmonary fibrosis undergoing lung transplantation. Sci. Rep. 2019, 9, 9347. [Google Scholar] [CrossRef]
- Ochman, M.; Maruszewski, M.; Latos, M.; Jastrzębski, D.; Wojarski, J.; Karolak, W.; Przybyłowski, P.; Zeglen, S. Nordic Walking in Pulmonary Rehabilitation of Patients Referred for Lung Transplantation. Transplant. Proc. 2018, 50, 2059–2063. [Google Scholar] [CrossRef]
- Da Fontoura, F.F.; Berton, D.C.; Watte, G.; Florian, J.; Schio, S.M.; Camargo, J.D.J.P.; Teixeira, P.J.Z.; Moreira, J.D.S. Pulmonary Rehabilitation in Patients with Advanced Idiopathic Pulmonary Fibrosis Referred for Lung Transplantation. J. Cardiopulm. Rehabil. Prev. 2018, 38, 131–134. [Google Scholar] [CrossRef]
- Ulvestad, M.; Durheim, M.T.; Kongerud, J.S.; Lund, M.B.; Edvardsen, E. Effect of high-intensity training on peak oxygen uptake and muscular strength after lung transplantation: A randomized controlled trial. J. Heart Lung Transplant. 2020, 39, 859–867. [Google Scholar] [CrossRef]
- Wickerson, L.; Helm, D.; Gottesman, C.; Rozenberg, D.; Singer, L.G.; Keshavjee, S.; Sidhu, A. Telerehabilitation for Lung Transplant Candidates and Recipients During the COVID-19 Pandemic: Program Evaluation. JMIR mHealth uHealth 2021, 9, e28708. [Google Scholar] [CrossRef] [PubMed]
- Layton, A.M.; Irwin, A.M.; Mihalik, E.C.; Fleisch, E.; Keating, C.L.; DiMango, E.A.; Shah, L.; Arcasoy, S.M. Telerehabilitation Using Fitness Application in Patients with Severe Cystic Fibrosis Awaiting Lung Transplant: A Pilot Study. Int. J. Telemed. Appl. 2021, 2021, 6641853. [Google Scholar] [CrossRef]
- Candemir, I.; Ergun, P.; Kaymaz, D.; Demir, N.; Taşdemir, F.; Sengul, F.; Egesel, N.; Yekeler, E. The Efficacy of Outpatient Pulmonary Rehabilitation After Bilateral Lung Transplantation. J. Cardiopulm. Rehabilitation Prev. 2019, 39, E7–E12. [Google Scholar] [CrossRef]
- Andrianopoulos, V.; Gloeckl, R.; Boensch, M.; Hoster, K.; Schneeberger, T.; Jarosch, I.; Koczulla, R.A.; Kenn, K. Improvements in functional and cognitive status following short-term pulmonary rehabilitation in COPD lung transplant recipients: A pilot study. ERJ Open Res. 2019, 5, 00060–2019. [Google Scholar] [CrossRef]
- Choi, J.; Hergenroeder, A.L.; Burke, L.; Dabbs, A.D.; Morrell, M.; Saptono, A.; Parmanto, B. Delivering an In-Home Exercise Program via Telerehabilitation: A Pilot Study of Lung Transplant Go (LTGO). Int. J. Telerehabilitation 2016, 8, 15–26. [Google Scholar] [CrossRef]
- Holland, A.E.; Nici, L. The Return of the Minimum Clinically Important Difference for 6-Minute-Walk Distance in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2013, 187, 335–336. [Google Scholar] [CrossRef]
- Mathai, S.C.; Puhan, M.A.; Lam, D.; Wise, R.A. The Minimal Important Difference in the 6-Minute Walk Test for Patients with Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2012, 186, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Maury, G.; Langer, D.; Verleden, G.; Dupont, L.; Gosselink, R.; Decramer, M.; Troosters, T. Skeletal Muscle Force and Functional Exercise Tolerance Before and After Lung Transplantation: A Cohort Study. Am. J. Transplant. 2008, 8, 1275–1281. [Google Scholar] [CrossRef] [PubMed]
- Antoniu, S.A. Descriptors of dyspnea in obstructive lung diseases. Multidiscip. Respir. Med. 2010, 5, 216–219. [Google Scholar] [CrossRef]
- Jastrzebski, D.; Gumola, A.; Gawlik, R.; Kozielski, J. Dyspnea and quality of life in patients with pulmonary fibrosis after six weeks of respiratory rehabilitation. J. Physiol. Pharmacol. 2006, 57, 139–148. [Google Scholar] [PubMed]
- Pehlivan, E.; Mutluay, F.; Balcı, A.; Kılıç, L. The effects of inspiratory muscle training on exercise capacity, dyspnea and respiratory functions in lung transplantation candidates: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1328–1339. [Google Scholar] [CrossRef]
- British Thoracic Society Standards of Care Subcommittee on Pulmonary Rehabilitation. Pulmonary rehabilitation. Thorax 2001, 56, 827–834. [Google Scholar] [CrossRef]
- Ringbaek, T.J.; Broendum, E.; Hemmingsen, L.; Lybeck, K.; Nielsen, D.; Andersen, C.; Lange, P. Rehabilitation of patients with chronic obstructive pulmonary disease. Exercise twice a week is not sufficient! Respir. Med. 2000, 94, 150–154. [Google Scholar] [CrossRef]
- Holland, A.E.; Hill, C.J.; Glaspole, I.; Goh, N.; McDonald, C.F. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir. Med. 2012, 106, 429–435. [Google Scholar] [CrossRef]
- Komatsu, T.; Oshima, A.; Chen-Yoshikawa, T.F.; Harashima, S.I.; Aoyama, A.; Inagaki, N.; Date, H. Physical activity level significantly affects the survival of patients with end-stage lung disease on a waiting list for lung transplantation. Surg. Today 2017, 47, 1526–1532. [Google Scholar] [CrossRef]
- Banga, A.; Mohanka, M.; Mullins, J.; Bollineni, S.; Kaza, V.; Ring, S.; Bajona, P.; Peltz, M.; Wait, M.; Torres, F. Hospital length of stay after lung transplantation: Independent predictors and association with early and late survival. J. Heart Lung Transpl. 2017, 36, 289–296. [Google Scholar] [CrossRef]
- Florian, J.; Rubin, A.; Mattiello, R.; Fontoura, F.F.D.; Camargo, J.D.J.P.; Teixeira, P.J.Z. Impact of pulmonary rehabilitation on quality of life and functional capacity in patients on waiting lists for lung transplantation. J. Bras. Pneumol. 2013, 39, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, S.I.; Hayes, D.; Kirkby, S.E.; Tobias, J.D.; Tumin, D. Age-Dependent Gender Disparities in Post Lung Transplant Survival Among Patients With Idiopathic Pulmonary Fibrosis. Ann. Thorac. Surg. 2016, 103, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Puhan, M.A.; Büsching, G.; Schünemann, H.J.; VanOort, E.; Zaugg, C.; Frey, M. Interval versus continuous high-intensity exercise in chronic obstructive pulmonary disease: A randomized trial. Ann. Intern. Med. 2006, 145, 816–825. [Google Scholar] [CrossRef]
- Vogiatzis, I.; Terzis, G.; Nanas, S.; Stratakos, G.; Simoes, D.C.M.; Georgiadou, O.; Zakynthinos, S.; Roussos, C. Skeletal Muscle Adaptations to Interval Training in Patients With Advanced COPD. Chest 2005, 128, 3838–3845. [Google Scholar] [CrossRef]
- Wickerson, L.; Mathur, S.; Brooks, D. Exercise training after lung transplantation: A systematic review. J. Heart Lung Transplant. 2010, 29, 497–503. [Google Scholar] [CrossRef]
- Vivodtzev, I.; Pison, C.; Guerrero, K.; Mezin, P.; Maclet, E.; Borel, J.C.; Chaffanjon, P.; Hacini, R.; Chavanon, O.; Blin, D.; et al. Benefi ts of home-based endurance training in lung transplant recipients. Respir. Physiol. Neurobiol. 2011, 177, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Langer, D.; Burtin, C.; Schepers, L.; Ivanova, A.; Verleden, G.; Decramer, M.; Troosters, T.; Gosselink, R. Exercise Training After Lung Transplantation Improves Participation in Daily Activity: A Randomized Controlled Trial. Am. J. Transplant. 2012, 12, 1584–1592. [Google Scholar] [CrossRef]
- Munro, P.; Holland, A.; Bailey, M.; Button, B.; Snell, G. Pulmonary Rehabilitation Following Lung Transplantation. Transplant. Proc. 2009, 41, 292–295. [Google Scholar] [CrossRef]
- Guerrero, K.; Wuyam, B.; Mezin, P.; Vivodtzev, I.; Vendelin, M.; Borel, J.-C.; Hacini, R.; Chavanon, O.; Imbeaud, S.; Saks, V.; et al. Functional coupling of adenine nucleotide translocase and mitochondrial creatine kinase is enhanced after exercise training in lung transplant skeletal muscle. Am. J. Physiol. Integr. Comp. Physiol. 2005, 289, R1144–R1154. [Google Scholar] [CrossRef]
- Thabut, G.; Mal, H. Outcomes after lung transplantation. J. Thorac. Dis. 2017, 9, 2684–2691. [Google Scholar] [CrossRef]
- Swigris, J.J.; Brown, K.K.; Behr, J.; du Bois, R.M.; King, T.E.; Raghu, G.; Wamboldt, F.S. The SF-36 and SGRQ: Validity and first look at mimimum important differences in IPF. Respir. Med. 2010, 104, 296–304. [Google Scholar] [CrossRef]
- Farkas; Szipőcs, A.; Horváth, A.; Horváth, I.; Gálffy, G.; Varga, J.; Galambos, K.; Kugler, S.; Nagy, A.; Szalai, Z. Establishment of relationships between native and inhalation device specific spirometric parameters as a step towards patient tailored inhalation device selection. Respir. Med. 2019, 154, 133–140. [Google Scholar] [CrossRef]
- Szucs, B.; Petrekanits, M.; Varga, J. Effectiveness of a 4-week rehabilitation program on endothelial function, blood vessel elasticity in patients with chronic obstructive pulmonary disease. J. Thorac. Dis. 2018, 10, 6482–6490. [Google Scholar] [CrossRef]
- Fekete, M.; Fazekas-Pongor, V.; Balazs, P.; Tarantini, S.; Nemeth, A.N.; Varga, J.T. Role of new digital technologies and telemedicine in pulmonary rehabilitation: Smart devices in the treatment of chronic respiratory diseases. Wien. Klin. Wochenschr. 2021, 133, 1201–1207. [Google Scholar] [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabilitation Assist. Technol. 2017, 4, e7511. [Google Scholar] [CrossRef]
- Singer, J.P.; Soong, A.; Bruun, A.; Bracha, A.; Chin, G.; Hays, S.R.; Kukreja, J.; Rigler, J.; Golden, J.A.; Greenland, J.R.; et al. A Mobile Health Technology Enabled Home-Based Intervention to Treat Frailty in Adult Lung Transplant Candidates: A Pilot Study. Clin. Transplant. 2018, 32, e13274. [Google Scholar] [CrossRef]
- Langer, D. Rehabilitation in Patients before and after Lung Transplantation. Respiration 2015, 89, 353–362. [Google Scholar] [CrossRef]
- Dennett, A.; Harding, K.E.; Reimert, J.; Morris, R.; Parente, P.; Taylor, N.F. Telerehabilitation’s Safety, Feasibility, and Exercise Uptake in Cancer Survivors: Process Evaluation. JMIR Cancer 2021, 7, e33130. [Google Scholar] [CrossRef]
- Cox, N.; Corso, S.D.; McDonald, C.; Hill, C.; O’Halloran, P.; Macdonald, H.; Zanaboni, P.; Alison, J.; Hansen, H.; Holland, A. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev. 2020, 1, CD013040. [Google Scholar] [CrossRef]
- Rozenberg, D.; Wickerson, L.; Singer, L.G.; Mathur, S. Sarcopenia in lung transplantation: A systematic review. J. Heart Lung Transplant. 2014, 33, 1203–1212. [Google Scholar] [CrossRef]
- Subedi, N.; Rawstorn, J.C.; Gao, L.; Koorts, H.; Maddison, R. Implementation of Telerehabilitation Interventions for the Self-Management of Cardiovascular Disease: Systematic Review. JMIR mHealth uHealth 2020, 8, e17957. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).