Abstract
Depression, anxiety, and perceived stress are common comorbidities in patients with inflammatory bowel disease (IBD) and may negatively influence the disease course. Likewise, severe IBD may contribute to the development or worsening of psychiatric symptoms. Despite the established relevance of the gut–brain axis and frequent use of psychotropic medications in IBD patients, limited evidence exists regarding the effects of psychiatric treatments on gastrointestinal disease activity. Therefore, the aim of this systematic review is to evaluate the effectiveness of psychiatric therapies on gastrointestinal symptoms and disease activity in patients with IBD. The work was conducted in accordance with PRISMA guidelines. Searches were performed across PubMed, Web of Science, and Scopus up to July 2024. Eligible studies evaluated the effectiveness of psychiatric medications—including antidepressants, antipsychotics, anxiolytics, sedative-hypnotics, mood stabilizers, anticonvulsants, and others—on at least one gastrointestinal outcome in patients with IBD. Outcomes included changes in commonly used clinical and endoscopic scores for Crohn’s disease (CD) and ulcerative colitis (UC), number of bowel movements, stool consistency, presence of blood in stool, severity of abdominal pain, as well as in surrogate markers of disease activity following treatment. Out of 8513 initially identified articles, 22 studies involving 45,572 IBD patients met the inclusion criteria. Antidepressants, particularly bupropion, tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), venlafaxine, and duloxetine, were associated with improvements in IBD activity scores, including Crohn’s Disease Activity Index (CDAI) and Simple Endoscopic Score for Crohn’s Disease (SES-CD) for CD, Mayo score and Ulcerative Colitis Endoscopic Index of Severity (UCEIS) for UC. Case reports highlighted potential benefits of pregabalin and lithium carbonate, respectively, showed by the reduction in clinical and endoscopic score of disease activity for pregabalin and improvement of UC symptoms for lithium carbonate, while topiramate showed limited efficacy. Clonidine and naltrexone determined the reductions in clinical and endoscopic score of disease activity, including CDAI and Crohn’s disease endoscopy index severity score (CDEIS) for CD and Disease Activity Index (DAI) for UC. Despite the limited data and study heterogeneity, antidepressants, naltrexone, and clonidine were associated with improvements in IBD activity. Larger, prospective studies are needed to confirm the therapeutic potential of psychiatric medications in modulating IBD activity and to guide integrated clinical management.
1. Introduction
Symptoms of depression and anxiety, as well as perceived distress are common comorbid conditions in patients suffering from inflammatory bowel diseases (IBDs), often leading to health-related decreased quality of life and lower adherence to therapeutic programs [,,]. Recent systematic reviews and meta-analyses suggested an estimated prevalence of anxiety disorders in IBD patients of 20.7%, whereas symptoms of anxiety reached 35.1% of patients []. Depression disorders are slightly less prevalent, with rates of 15.2% of IBD patients [], whereas symptoms of depression affect up to 25.2% of patients []. Growing evidence indicate an association between stress and flares in IBD activity, with anxiety and depression being more predominant during flares []. IBD course and mental health seem to have a bidirectional relationship and to be reciprocally influenced by the following: patients with IBD and symptoms of depression or anxiety are at increased risk of poorer outcomes, therapy escalation, hospitalization, emergency department attendance, and increased disability whereas the presence of a more severe IBD at baseline appears to be associated with the development of symptoms of depression and anxiety []. Furthermore, the literature reports cases of psychiatric adverse events following treatment with the biologic drugs currently used for the treatment of IBD (e.g., infliximab), even within a few hours after the drug administration [].
Consequently, managing psychiatric symptoms associated with gastrointestinal medical conditions, including those resulting from therapy, is becoming increasingly relevant for all healthcare professionals involved in the care of IBD patients [].
Despite the relative paucity of supporting evidence regarding the pharmacological intervention for psychiatric symptoms, approximately 30% of IBD patients are treated with antidepressants, especially selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) [,]. This number was even higher in a large-scale survey conducted in Australia, where 47% of the CD patients reported current use of antidepressants and 25% believed that the treatment ameliorated their IBD []. Similarly, the use of anxiolytics, sedatives, and hypnotics is reported in 26% of IBD patients, a rate significantly higher than that observed in the general population []. Antidepressants have been shown to effectively improve anxiety, depression, and the quality of life in IBD patients. Additionally, they contribute to reducing disease activity and alleviating gastrointestinal symptoms, collectively exerting a positive impact on the disease course of IBD [].
In this systematic review, we comprehensively collected all clinical evidence in the literature on the effectiveness of psychiatric therapies in the management of gastrointestinal symptoms of IBD patients. Our focus extended beyond addressing psychiatric comorbidities to encompass the management of IBD itself. Accordingly, the primary objective of our review was to determine the influence of these treatments on specific disease activity outcomes in IBD patients. Secondarily, we discussed the efficacy of these medications on psychiatric outcomes, while also providing practical recommendations regarding the use of specific drugs that may worsen gastrointestinal symptoms.
2. Material and Methods
We conducted this systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [] (Figure 1).
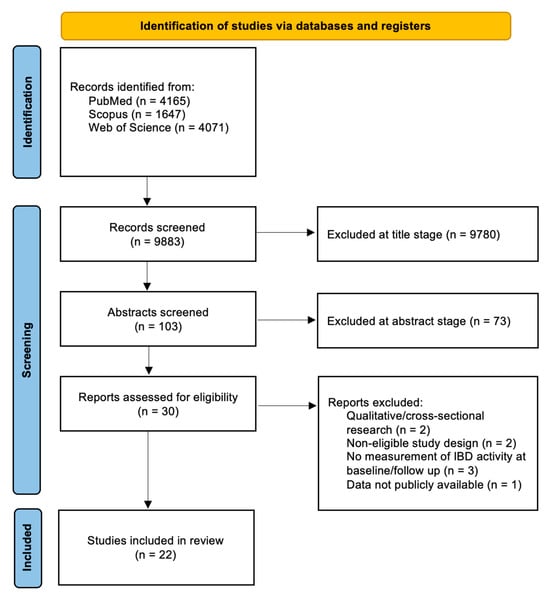
Figure 1.
PRISMA flow diagram describing the paper selection process.
2.1. Eligibility Criteria
Original peer-reviewed reports, clinical trials, retrospective and prospective cohort studies, meta-analysis, systematic reviews, and case–control studies in the English language were eligible for inclusion. The Population, Intervention, Comparison and Outcome (PICO) characteristics [] were as follows: (1) patients diagnosed with IBD, including Crohn’s disease, ulcerative colitis, and IBD-unclassified (IBD-U); (2) use of psychiatric medications, including antidepressants, antipsychotics (typical and atypical), anticonvulsants, sedative-hypnotics, anxiolytics, stimulants, anti-craving and addiction medications, mood stabilizers, and others (e.g., Clonidine, Modafinil, Suvorexant, etc.); (3) patients receiving standard IBD treatment without psychiatric medications; and (4) changes in gastroenterological (GI) outcomes, including variations in commonly used clinical and endoscopic scores for CD and UC (e.g., Partial Mayo Score (PMS) [], Harvey-Bradshaw index (HBI) [], Crohn’s Disease Activity Index (CDAI) [], Inflammatory Bowel Disease Questionnaire (IBDQ) [], Lichtiger Colitis Activity Index (LCAI) [,], Endoscopic Mayo score (EMS) [], Ulcerative Colitis Endoscopic Index of Severity (UCEIS) [], Simple Endoscopic Score for Crohn’s Disease (SES-CD) [], Disease Activity Index (DAI) [], etc.), number of bowel movements, stool consistency, presence of blood in stool, severity of abdominal pain, as well as in surrogate markers of disease activity, such as IBD-related hospitalization, IBD-related surgery, or step-up medication in terms of a redeemed prescription of corticosteroids, immunomodulators or biotechnological therapies.
Clinical studies that evaluated exclusively the post-treatment variation in the quality of life, the psychological symptoms or in any psychiatric outcome of IBD patients were not included in the study. Studies evaluating patients with irritable bowel syndrome (IBS), or other GI disorders different from IBD were excluded, as well as those including patients with an uncertain diagnosis of an IBD. In the case of mixed cohorts, only data from patients that met our eligibility criteria were taken into account. We did not include animal model studies or non-original reports. Because of the likely scarcity of studies with adequate sample size, also case series with less than 10 patients and case reports were considered, without restrictions on publication year. We did not include data presented only as abstracts at conferences.
2.2. Information Sources and Search Strategy
A literature search was performed using the following electronic databases: Web of Science (ISI), PubMed, and SCOPUS. The last search was run on 31 July 2024. The terms “inflammatory bowel disease”, “ulcerative colitis”, “Crohn’s disease”, “IBD”, “UC”, “CD” were matched with the following drugs: Acamprosate OR Agomelatine OR Alprazolam OR Amisulpride OR Amitriptyline OR Amoxapine OR Amphetamine OR Aripiprazole OR Armodafinil OR Asenapine OR Atomoxetine OR Benztropine OR Blonanserin OR Bremelanotide OR Brexanolone OR Brexpiprazole OR Buprenorphine OR Bupropion OR Buspirone OR Caprylidene OR Carbamazepine OR Cariprazine OR Chlordiazepoxide OR Chlorpromazine OR Citalopram OR Clomipramine OR Clonazepam OR Clonidine OR Clorazepate OR Clozapine OR Cyamemazine OR Desipramine OR Desvenlafaxine OR Deutetrabenazine OR Dextromethorphan OR Diazepam OR Diphenhydramine OR Disulfiram OR Donepezil OR Dothiepin OR Doxepin OR Duloxetine OR Escitalopram OR Esketamine OR Estazolam OR Eszopiclone OR Flibanserin OR Flumazenil OR Flunitrazepam OR Fluoxetine OR Flupenthixol OR Fluphenazine OR Flurzepam OR Fluvoxamine OR Gabapentin OR Galantamine OR Fuanfacine OR Haloperidol OR Hydroxyzine OR Iloperidone OR Imipramine OR Isocarboxazid OR Ketamine OR Lamotrigine OR Lemborexant OR Levetiracetam OR Levomilnacipran OR Lisdexamfetamine OR Lithium OR Lofepramine OR Lofexidine OR Loflazepate OR Lorazepam OR Loxapine OR Lumateperone OR Lurasidone OR Maprotiline OR Memantine OR Methylfolate OR Methylphenidate OR Mianserin OR Midazolam OR Milnacipran OR Mirtazapine OR Moclobemide OR Modafinil OR Molindone OR Nalmefene OR Naltrexone OR Naltrexone/Buproprion OR Nefazodone OR Nortriptyline OR Olanzapine OR Oxazepam OR Oxcarbazepine OR Paliperidone OR Paroxetine OR Perospirone OR Perphenazine OR Phenelzine OR Phentermine/Topiramate OR Pimavanserine OR Pimozide OR Pipothiazine OR Pitolisant OR Prazosin OR Pregabalin OR Propranolol OR Protriptyline OR Quazepam OR Quetiapine OR Ramelteon OR Reboxetine OR Risperidone OR Rivastigmine OR Selegiline OR Sertindole OR Sertraline OR Sildenafil OR Sodium oxybate OR Solriamfetol OR Sulpiride OR Suvoxerant OR Tasimelteon OR Temazepam OR Thioridazine OR Thiothixene OR Tiagabine OR Tianeptine OR Topiramate OR Tranylcypromine OR Trazodone OR Triazolam OR Trifluoperazine OR Trihexyphenidyl OR Triiodothyronine OR Trimipramine OR Valbenazine OR Valproate OR Varenicline OR Venlafaxine OR Vilazodone OR Vortioxetine OR Zaleplon OR Ziprasidone OR Zolpidem OR Zonisamide OR Zopiclone OR Zotepine OR Zuclopenthixol. All terms were searched both as keywords and Medical Subject Headings (MeSH). The bibliographies of relevant (according to titles and abstracts) articles were hand-searched to provide additional references.
2.3. Study Selection and Data Collection Process
Three reviewers, F.D.V., E.C, and A.M.D., blinded to the other reviewer’s decision, evaluated the titles and abstracts of the studies to ascertain their eligibility. They verified separately that all the inclusion and exclusion criteria were met. In cases that were not apparent, the entire text of the publications was retrieved and examined. In every instance where there was a disagreement, a fourth author (G.C.) arbitrated.
The same three reviewers (F.D.V., E.C., and A.M.D.) separately retrieved data from qualifying studies, which were then cross-checked. Disputes were rectified by agreement. Articles that combined newly enrolled patients with those from prior studies were only taken into account for the latter. For mixed cohorts, the study only included patient data that satisfied our inclusion and exclusion criteria. Due to methodological heterogeneity and the variability in outcomes assessed across the included studies—ranging from clinical to endoscopic and including both direct and surrogate endpoints—we chose not to perform a meta-analysis or any formal statistical synthesis. Instead, we conducted a descriptive analysis, discussing each study individually in terms of design, methodology, and outcomes. For this reason, we did not register a review protocol on PROSPERO. We chose to report our results in four sections according to the type of drug that was administered.
We collected study references and citations in the EndNote software application version 20 (Thomson Reuters, New York, NY, USA). A data collection form was designed in Microsoft Excel 2016 (Microsoft, Redmond, WA, USA).
3. Results
A total of 8513 studies (4165 on PubMed, 4071 on Web of Science and 1647 on Scopus) were identified overall using the abovementioned research strategies. A total of 103 articles were selected for the full abstract screening, and after that 22 articles were chosen for the synthesis of results, including 7 RCTs, 4 non-randomized controlled clinical trial, 6 observational studies, 5 case series/reports. All selected studies were in English. The 22 articles covered a population of 45.572 IBD patients, including CD, UC and IBD-U. All included studies utilized different assessment tools to evaluate both gastrointestinal and psychiatric outcomes, reflecting differences in research objectives and study populations. A summary of the primary outcome measures employed is provided in Supplementary Table S1.
Supplementary Table S2 summarizes the mechanisms of action, primary indications according to the Food and Drug Administration (FDA), and major gastrointestinal side effects of the main drugs included in the manuscript. Additionally, the table provides detailed insights and further information regarding the administration of these medications.
3.1. Antidepressants
Among the 22 selected studies, 12 were centered on the investigation of antidepressant therapies, including 4 RCTs, 5 observational cohort studies and 3 case series/reports. Four out of 12 studies (33%) investigated different antidepressant drugs (SSRIs, TCAs, serotonin noradrenergic reuptake inhibitors (SNRIs), bupropion, trazodone and mirtazapine), while 2 (17%) focused on bupropion, 1 (8%) on tianeptine, 1 (8%) on venlafaxine, 1 (8%) on phenelzine, 1 (8%) on fluoxetine, 1 (8%) on duloxetine, and 1 (8%) on TCAs. Overall, SSRIs and SNRIs constituted the most frequently prescribed classes of antidepressants.
In details, two prospective and two retrospective observational studies investigated the role of several classes of antidepressant, including SSRI, SNRI, TCAs, and trazodone, on the disease course in patients affected by IBDs []. Notably, in a prospective study of 331 IBD patients, Hall et al. observed a trend toward lower rates of escalation of medical therapy among patients receiving antidepressants at baseline, and of disease flares, hospitalization and intestinal resection rates in those with abnormal anxiety or depression scores at study entry []. Similarly, Kristensen et al.’s retrospective population-based cohort study, encompassing 42,890 IBD patients, underscored a significantly reduced relapse rate in individuals exposed to antidepressants compared to their non-exposed counterparts, with a more pronounced effect observed in CD patients than in UC patients. Additionally, patients with no prior antidepressant usage exhibited superior disease course outcomes upon antidepressant exposure compared to non-users []. Yanartas et al.’s prospective cohort study, involving 67 IBD patients treated with various antidepressant classes, evidenced significant improvements in hemoglobin levels and CDAI scores compared with baseline among individuals who adhered rigorously to the prescribed 6-month treatment regimen []. Furthermore, a retrospective case–control study, including 58 IBD patients, revealed that patients receiving various antidepressant medications, particularly citalopram and fluoxetine, experienced fewer relapses and corticosteroid courses in the year after antidepressant initiation than in the year before; these findings were absent in the control group []. Conversely, in two different surveys (2012, 2014), Mikoc-Walus et al. investigated the efficacy of several antidepressants in IBD patients concurrently undergoing treatment for depression or anxiety, revealing that 67% of patients reported no alteration in their IBD activity, 26% reported physical symptom improvement, 5% referred symptom exacerbation, and 2% attributed difficulty in distinguishing antidepressant effects from other potential causal factors [].
A randomized clinical trial (RCT) conducted by Daghaghzadeh et al. established the efficacy of duloxetine in alleviating symptom severity, as assessed by the LCAI score, in 35 individuals diagnosed with IBD []. Meanwhile, Mikocka-Walus et al. (2017) examined the utility of fluoxetine, an SSRI, in CD patients, revealing no significant improvement of CDAI scores or fecal calprotectin levels after the treatment []. Recently, Liang et al. conducted an RCT, exploring the therapeutic potential of venlafaxine, an SNRI, in 45 patients diagnosed with UC and CD. The study’s primary endpoints included the IBDQ score and disease activity assessments (CDAI for CD, Mayo score for UC), with secondary endpoints encompassing disease course, SES-CD, UCEIS, relapse rate, corticosteroid/biologic usage frequency, as well as pertinent laboratory parameters, including white blood cells count (WBC), albumin, C reactive protein (CRP), fecal calprotectin, erythrocyte sedimentation (ESR), tumor necrosis factor (TNF)-α, and interleukin (IL)-10. Notably, IBDQ scores exhibited a significant elevation in the venlafaxine cohort compared to the placebo group. Furthermore, UC and CD patients treated with venlafaxine demonstrated reduced Mayo score and CDAI score, respectively, following the 6-month assessment period. However, the study did not discern significant disparities in UCEIS and SES-CD scores between the venlafaxine and placebo cohorts at the 6-month juncture [].
Only one retrospective cohort investigation focused on the efficacy of tricyclic antidepressants (TCAs) in ameliorating gastrointestinal symptoms in IBD patients, elucidating a noteworthy improvement in the severity scores (established Likert scales) of both UC and CD cohorts. However, UC patients presented a better response to TCA that those with CD [].
Tianeptine, an atypical antidepressant, succeeded in reducing symptoms of anxiety and depression, as well as disease activity index, in 60 patients with IBD compared with placebo after 12 months [].
Interestingly, some case reports exhibited promising effects on gastrointestinal symptoms after bupropion intake. A case series of 4 patients by Kane et al. (2003) and a case report of 2 patients by Kast and Altschuler (2001) documented the achievement of clinical remission (CDAI < 150) in six patients affected by CD following bupropion administration for varied indications [,]. One patient experienced a flare-up of CD after discontinuing bupropion on her own.
Finally, in 1998, Kast et al. detailed the case of a 33-year-old woman receiving phenelzine, who experienced sustained improvement in bowel function and abdominal pain, persisting post-azathioprine and prednisone tapering, albeit experiencing CD relapse subsequent to nortriptyline transition six weeks later [].
Only a minority of the aforementioned studies specifically examined also the impact of antidepressants on psychiatric disorders in patients with IBD. A population-based study conducted by Jayasooriya (2022) revealed a higher incidence of antidepressant usage within the IBD cohort, with the greatest risk occurring during the initial year post-IBD diagnosis []. Furthermore, among IBD patients initiating antidepressant therapy, 67% received treatment for a duration less than the recommended minimum of 7 months.
The RCT featuring duloxetine by Daghaghzadeh et al., evaluated anxiety and depression with the Hospital Anxiety and Depression Scale (HADS), while Quality of Life (QOL) was assessed via the World Health Organization Quality of Life abbreviated version (WHOQOL-BREF) []. The findings indicated a significant reduction in anxiety and depression levels alongside an enhancement in physical, psychological, and social QOL domains, although no notable difference in environmental QOL was observed. Similarly, the randomized clinical trial conducted by Mikocka-Walus et al. (2017), involving fluoxetine, utilized the same assessment scales, yet fluoxetine exhibited negligible influence on psychological symptoms or QOL [].
HADS was further employed in an additional RCT featuring an SNRI, venlafaxine (Liang, 2022), which revealed a noteworthy reduction in HADS depression scores after the treatment []. Additionally, a prospective cohort study [] (Yanartas, 2016), predominantly comprising SSRI recipients, reported improvements in anxiety and depression levels as measured by HAD-A and HAD-D scales, respectively, alongside enhancements in SF-36 and ASSES scores.
In two case reports by Kast and Altschuler (2001) [] and Kast (1998) [], bupropion and phenelzine exhibited efficacy in alleviating depression symptoms in patients with CD.
Data extracted from each primary study are shown in Table 1.

Table 1.
Included studies on antidepressants for gastrointestinal outcomes in IBD patients.
3.2. Antiepileptics
Only one retrospective cohort study [] focused on topiramate use in IBD patients, based on a large cohort of IBD patients: 775 were treated with topiramate and 958 were treated with other anticonvulsant and anti-migraine medications. However, there was no difference between topiramate users concerning steroid prescription, post-exposure initiation of biologic agents, abdominal surgery or hospitalization. In this study, effects on psychological symptoms were not reported.
Interestingly, one case report described a clinical, biochemical, and subsequently endoscopic (after 6 months) improvement in a patient with CD undergoing therapy with Pregabalin for psychic and physical anxiety [].
Data extracted from each primary study are shown in Table 2.

Table 2.
Included studies on antiepileptics for gastrointestinal outcomes in IBD patients.
3.3. Hypnoinducers and Anxiolytics
According to a retrospective matched cohort study [] (Bernstein, 2022), the use of BZD and Z-drugs (to treat mood/anxiety disorders and sleep disorders) is more common in IBD patients than in controls. Nevertheless, all the available studies focus exclusively on psychological effects, not including gastrointestinal outcomes (Stokes, 1978) [], therefore none of them met our eligibility criteria.
3.4. Mood Stabilizers
Only one case report met our eligibility criteria, [] describing the administration of lithium carbonate in the manic phase of a 67-year-old patient with ulcerative colitis, in an active phase with recent endoscopic evidence of “severe, active ulcerative colitis, already undergoing therapy with salicosulfapiridine (azulfadine)”. After five days, there was considerable improvement in both gastrointestinal and psychiatric symptoms, and after two months, the endoscopic evidence revealed considerable improvement with only a few small bleeding spots. Data extracted from the primary study are shown in Table 3.

Table 3.
Included study on mood stabilizers for gastrointestinal outcomes in IBD patients.
3.5. Others
Other studies which met our eligibility criteria investigated the role of naltrexone, clonidine and lithium on the disease course of IBD patients. A total of four trials explored the effect of naltrexone in IBD, three of them focused on CD.
Lie et al. 2018 [] evaluated low-dose naltrexone (LDN) for induction of remission in IBD patients (UC and CD) not responsive to conventional therapy. LDN induced clinical improvement in 74.5% and remission in 25.5% of patients. There was no statistically significant difference between CD and UC patients in rates of response or remission. Patients achieving clinical remission had a significantly greater improvement in endoscopic score than patients not reaching clinical response. However, 14.9% reported adverse events due to LDN (vivid dreams, drowsiness, and headache).
Smith et al. in 2011 [] in an RCT, confirmed naltrexone as a promising therapy for CD: 88% of those treated with naltrexone had at least a 70-point decline in CDAI scores compared to 40% of placebo-treated patients, and 78% of active arm had an endoscopic response (a 5-point decline in the Crohn’s disease endoscopy index severity score (CDEIS) from baseline compared to 28% response in placebo-treated controls, thereby confirming their findings previously described in 2007. In addition, in 2007, Smith et al. [] also reported an improvement in QoL compared to baseline during naltrexone therapy. Smith et al. randomized pediatric patients with CD [] to placebo or LDN in another study. Naltrexone was well tolerated without any serious adverse events, and the PCDAI (Pediatric Crohn’s Disease Activity Index) significantly decreased in the active arm, with 25% of those achieving remission. According to the Impact III survey, an improvement in QoL from baseline was reported.
Regarding clonidine, two studies have investigated the efficacy of clonidine in patients with UC based on drug-mediated reduction of overall enhancement of sympathetic disease activity. Lechin et al. [] conducted a double-blind clinical trial of UC patients with severe activity, which was randomized to treatment with prednisone, sulfasalazine, or clonidine. Comparing performance among the three groups, treatment with prednisone and treatment with clonidine were significantly more effective than sulfasalazine (p < 0.001) for both. There were no significant differences between prednisone treatment and clonidine treatment. However, clonidine treatment induced more rapid therapeutic effects than prednisone, without significant adverse effects. Later, Furlan et al. [] tested the reduction in sympathetic activity by clonidine on clinical changes in UC. In addition to autonomic assessment (more information in table), they were randomly assigned to transdermal clonidine for eight weeks or placebo. Changes in the autonomic profile after clonidine were associated with reduced DAI score (concomitant amelioration of symptoms and endoscopic pattern). Normalization of the autonomic profile with clonidine was accompanied by improved disease and a general increase in sympathetic activity characterized by active UC.
Data extracted from each primary study are shown in Table 4.

Table 4.
Included studies on other psychiatric medications for gastrointestinal outcomes in IBD patients.
4. Discussion
In Western countries, between 10 and 30% of patients with IBD take antidepressant medications; nonetheless, to date only a few studies have investigated their role in the management of IBDs [,,]. Various systematic and narrative reviews have consistently acknowledged a favorable impact of antidepressants on the general well-being of patients with IBD [,,,,]. However, these reviews underscore the constrained and low-quality evidence available, leading to the conclusion that the efficacy of antidepressants in modulating IBD activity remains indeterminate. Although our research identified very few clinical trials that could establish a causal relationship between certain medications and the physical and mental health of patients with IBD, our systematic review revealed that antidepressant use might be beneficial to the disease course in patients with CD and UC, particularly for those who did not use antidepressants before the IBD onset, or with latent subclinical symptoms of anxiety and depression [] (Figure 2).
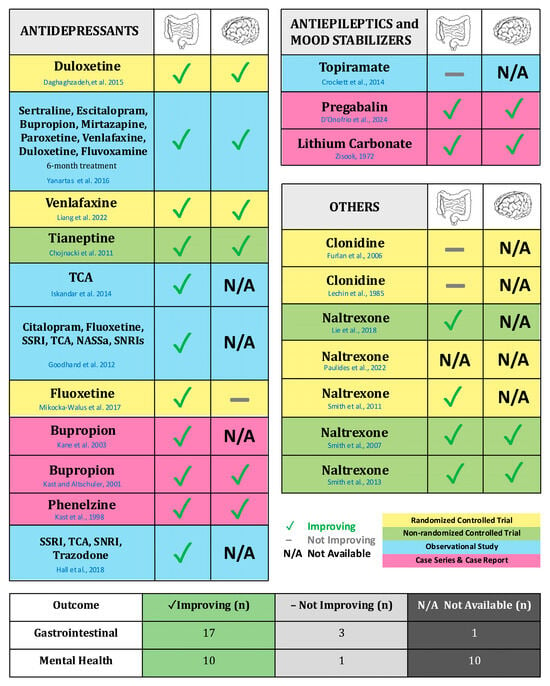
Figure 2.
Graphical summary of the studies included in the systematic review. This table summarizes the key studies included in this review, highlighting the effectiveness of certain psychotropic drugs on both gastrointestinal and psychiatric outcomes. The studies are organized by drug class—Antidepressants (Daghdhaghzadeh et al., 2015 [], Yanartaş et al., 2016 [], Liang et al., 2022 [], Chojnacki et al., 2011 [], Iskandar et al., 2014 [], Goodhand et al., 2012 [], Mikocka-Walus et al., 2017 [], Kane et al., 2003 [], Kast and Altschuler, 2001 [], Kast et al., 1998 [], Hall et al., 2018 []), Antiepileptics and Mood Stabilizers (Crockett et al., 2014 [], D’Onofrio et al., 2024 [], Zissok, 1972 []), and Others (Furlan et al., 2006 [], Lechin et al., 1985 [], Lie et al., 2018 [], Paulides et al., 2022 [], Smith et al., 2011 [], Smith et al., 2007 [], Smith et al., 2013 []). The study by Kristensen et al., 2019 [] was not included because there are no psychiatric/gastroenterological outcomes available for specific psychotropic drugs, but only for classes of drugs (antidepressants). Note: CR (Case-report); CS (Case-series); NASSa (Noradrenaline and specific serotonergic antidepressants); SNRI (Serotonin and norepinephrine reuptake inhibitors); SSRI (Selective serotonin reuptake inhibitors); TCA (Tricyclic antidepressants).
To date, only four placebo-controlled trials assessing the efficacy of antidepressants in IBD have been conducted, with one of these trials being nonrandomized [,,]. Tianeptine, an atypical antidepressant, demonstrated a reduction in symptoms of anxiety and depression, as well as a decrease in disease activity index []. Duloxetine exhibited a reduction in anxiety and depression scores, an improvement in quality of life, and a decrease in clinical disease activity indices in a cohort of IBD patients []. Likewise, venlafaxine was shown to enhance quality of life, decrease depression scores, and reduce clinical disease activity indices (CDAI and Mayo scores) []. Conversely, fluoxetine did not demonstrate any significant effect on anxiety, depression, quality of life, or clinical disease activity indices. Nonetheless, modest effects of fluoxetine on immune functions have been observed, including an increased proportion of effector memory T helper cells and a decreased proportion of effector memory T cytotoxic cells []. Notably, antidepressant use in patients with IBDs has been associated with several positive outcomes according to observational studies and case reports, including lower rates of hospitalization, surgical intervention, and medical treatment escalation []. Smaller studies corroborated these findings [,], showing reduced medical therapy escalation and fewer disease relapses among patients receiving antidepressants [], particularly in those with high baseline anxiety or depression []. Tricyclic antidepressants specifically show a better response in ulcerative colitis compared to Crohn’s disease, and bupropion has demonstrated efficacy in inducing clinical remission in patients with Crohn’s disease []. Furthermore, in a large epidemiological investigation encompassing over 400,000 individuals, the heightened risk of new-onset IBD observed among individuals with baseline depression appeared to be attenuated by the administration of antidepressants [].
It is well established that the vagus nerve, which is a key component of the brain–gut axis, plays a critical role in the tonic suppression of acute inflammation in IBD. Depression has been shown to disrupt this tonic vagal inhibition of pro-inflammatory cells, thereby increasing vulnerability to intestinal inflammation. Tricyclic antidepressants have been demonstrated to alleviate intestinal inflammation by restoring vagal function []. Additional studies have reported that depression can reactivate dormant chronic colitis through a process dependent on the α7 subunit of the nicotinic acetylcholine receptor (α7nAChR), which is normalized following treatment with antidepressants []. Indeed, the most intriguing potential effect of antidepressants in IBD is for the control of intestinal and systemic inflammation. A recent meta-analysis [] showed that an antidepressant treatment lowers the levels of the pro-inflammatory cytokines IL-4 and IL-6 in peripheral blood, thus resulting in an anti-inflammatory effect. The immunomodulatory mechanism of antidepressants could also be based on a shift between T helper-1 (Th1) and T helper-2 (Th2) lymphocytes cytokines production [] (Figure 3). In animal models of IBD, desipramine demonstrated a reduction in microscopic damage and mitigated colonic myeloperoxidase activity compared to placebo []. Likewise, both desipramine and fluoxetine significantly decreased serum concentrations of IL-1β and TNF-α in an animal model (all p < 0.001) []. A recent study by Teng et al. showed that treatment with fluoxetine in C56BL/6 mice of the IBD model induced macrophages to M2-like phenotype and inhibited the production of Paneth cells, while enterocytes, goblet cells and stem cells became the dominating cells, thereby exerting a protective effect on IBD []. As is widely known, the main target of fluoxetine is the 5-HT transporter (SERT), which blocks reuptake and prolongs neurotransmitter signaling of 5-HT []. Previous data suggest that SERT inhibition may exert a systemic immunosuppressive effect, partly through stimulation of M2 macrophage polarization. Another SSRI, sertraline, has been shown to inhibit the activation of Toll-like receptor (TLR)-3, thereby interfering with innate immunity []. Moreover, SSRIs seem to block the activation and proliferation of antigen presenting cells, thus influencing adaptive immunity []. Similarly, preclinical in vivo studies suggested a potential immunosuppressive effect for SNRIs, reducing the generation of pro-inflammatory cytokines, such as TNF-α, IFN-gamma, and IL-12 []. However, in studies on humans and healthy volunteers, venlafaxine and duloxetine presented inconsistent and minor effects on cytokines, lymphocyte subpopulations or circulating levels of neurotrophic factors [,,]. These findings collectively suggest that the use of antidepressants should be considered in patients with IBD, not only for managing subclinical or mild symptoms of anxiety and depression—often underestimated and underdiagnosed—but also for potentially modulating the disease course and improving clinical outcomes in selected patients. Although studies investigating the kynurenine pathway of tryptophan degradation in IBD are lacking, the previous literature suggested that depression linked with chronic inflammatory disorders, such as cancer, might have a distinct etiology compared to other forms of depression [,]. Notably, alterations in the kynurenine pathway due to inflammation, interfering with the bioavailability of tryptophan, necessary for the synthesis of serotonin, may play a crucial role in the development and persistence of both conditions [,].
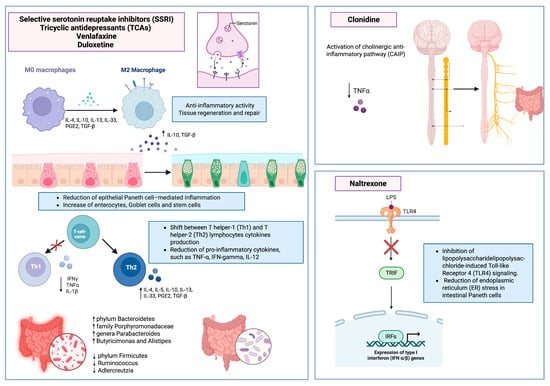
Figure 3.
Molecular and immunological mechanisms underlying the anti-inflammatory effects of selected psychiatric medications in inflammatory bowel disease. Selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), venlafaxine, and duloxetine contribute to inflammation modulation through the promotion of M2 macrophage polarization, increased production of anti-inflammatory cytokines (e.g., IL-10, TGF-β), reduction in Paneth cell-mediated epithelial inflammation, and modulation of gut microbiota composition. These drugs also induce a Th1-to-Th2 cytokine shift, reducing pro-inflammatory mediators such as TNF-α, IL-1β, and IFN-γ. Naltrexone inhibits lipopolysaccharide (LPS)-induced TLR4 signaling, reducing ER stress in Paneth cells and the expression of pro-inflammatory interferon genes. Clonidine activates the cholinergic anti-inflammatory pathway (CAIP), resulting in decreased TNF-α levels via autonomic nervous system modulation.
Hence, targeting enzymes implicated in the kynurenine pathway could present a dual therapeutic opportunity for treating both IBD (or other inflammatory conditions) and depression concurrently []. In this scenario, antidepressants may potentially facilitate this approach [].
Additionally, antidepressants may exert their anti-inflammatory effects through the modulation of intestinal microbiota composition []. Fluoxetine increases the abundance of certain taxa such as phylum Bacteroidetes, family Porphyromonadaceae, and genera Parabacteroides, Butyricimonas, and Alistipes. It decreases the abundance of phylum Firmicutes, as well as taxa like Ruminococcus and Adlercreutzia [,]. Escitalopram reduces the abundance of Ruminococcus and Adlercreutzia []. Venlafaxine and duloxetine also decrease the abundance of Ruminococcus and Adlercreutzia []. Amitriptyline, on the other hand, boosts the abundance of phylum Bacteroidetes, family Porphyromonadaceae, family Bacteroidaceae, and genera Parabacteroides, Butyricimonas, and Alistipes, while reducing the abundance of phylum Firmicutes []. Ketamine increases the abundance of bacterial genera such as Lactobacillus, Turicibacter, and Sarcina, while decreasing the abundance of opportunistic pathogens like Ruminococcus and Mucispirallum [].
Another important role of antidepressants is in the treatment of chronic pain. In a recent meta-analysis [], duloxetine was found to be the most effective antidepressant for managing chronic pain. There are also studies supporting the efficacy of milnacipran in treating chronic pain, but these studies are significantly fewer and of lower quality compared to those on duloxetine. The mechanism involves noradrenaline reuptake inhibition, which enhances analgesic effects mainly through α2-adrenergic receptors in the dorsal horn of the spinal cord []. Therefore, duloxetine might be a viable candidate for conditions involving chronic pain (such as IBD) and low mood.
A recent and intriguing meta-analysis demonstrated that antidepressants are safe and effective in treating depression comorbid with medical conditions. Additionally, the meta-analysis highlighted the ability of antidepressants to prevent depression []. Given the high prevalence of depression among individuals with IBD, it might be beneficial to consider low-dose antidepressants for those with a history of depressive episodes or even mild alterations on baseline psychometric scales for depression. Ultimately, the decision should depend on the clinical judgment of the physician, preferably with a psychiatrist’s consultation.
Despite various gastrointestinal side effects reported in the literature due to antidepressant therapy, particularly with escitalopram and sertraline, which seem to be less tolerated by the gastrointestinal tract [], researchers are increasingly interested in understanding the role of antidepressants, specifically serotonin reuptake inhibitors, in functional gastrointestinal disorders like irritable bowel syndrome (IBS). Considering that IBD can cause issues with intestinal motility leading to constipation and bloating, and to the overlap between IBD and IBS [], antidepressants may prove beneficial in managing these conditions. Notably, in a randomized controlled trial by Tack et al., it is reported that citalopram can increase colonic contractility and the occurrence of high-amplitude propagated contractions, together with an increased colonic compliance during fasting, suppressing the postprandial colonic tone [].
Additionally, antidepressants (along with other pharmacological classes) can be used in managing psychiatric side effects associated with corticosteroid therapy [], which is widely used in the management of IBD []. Symptoms seem to vary according to the corticosteroid dosage and typically emerge within the initial weeks of treatment. Unfortunately, there is a lack of knowledge regarding the risk factors associated with the onset of mood instability [].
Another promising molecule that has been investigated in patients with IBD is naltrexone. The rationale for its use as a treatment in IBD is based on the relevance of the endogenous opioid system in gut immunity [,]. Indeed, in IBD patients, the μ-opioid receptor (MOR) is overexpressed in mucosal T-lymphocytes and monocytes, and the administration of low dose Naltrexone (LDN) would appear to upregulate the endogenous encephalin and endorphin levels and to have a positive modulatory effect on the MOR [].
Additionally, it has been shown that the opioid inactive (+)-isomers of naltrexone inhibit lipopolysaccharide-induced Toll-like Receptor 4 (TLR4) signaling, a bacterial-induced inflammatory pathway contributing to IBD [,].
Furthermore, the effects of such therapy could also be expressed on the reduction in endoplasmic reticulum (ER) stress in intestinal Paneth cells, which is one of the contributing factors in IBD [,,].
In the studies analyzed, naltrexone therapy was associated with favorable clinical response rates, clinical remission, and endoscopic response (endoscopic scores improved by 48% compared to baseline, p = 0.018) []. Naltrexone also showed good tolerance in the pediatric population with CD. However, these results were obtained from cohorts with a relatively small number of participants over a limited observation period. Although most of the studies are conducted on CD, it is not entirely clear whether this therapy may also be helpful in UC patients (only one study is available) or whether there are any subclasses of patients in which it may be more effective. A multicenter study by Paulides et al. with a more significant number of patients for a longer observation time is still ongoing [].
In the literature, there are no studies evaluating how naltrexone can induce changes in the gut microbiota. However, there is evidence showing that naltrexone can improve inflammatory parameters in a murine model of enteritis [].
From a psychiatric perspective, naltrexone can also enhance positive emotional states by boosting the effects of endogenous opioids, leading to increased positive feelings and energy []. A review by Brown and Panksepp suggests that low doses of naltrexone may also play a role in promoting stress resilience, exercise, social bonding, and emotional well-being, as well as improving psychiatric conditions such as autism and depression [].
Clonidine, by activating the alpha-2 adrenergic receptors in the brainstem, inhibits the release of norepinephrine, a neurotransmitter that typically stimulates the sympathetic nervous system. The rationale for its utilization is based on the role of the cholinergic anti-inflammatory pathway (CAIP) on the potential anti-inflammatory effect on immune cells in animal models []. Experimental activation of CAIP inhibits TNF synthesis in the liver, spleen and heart, attenuating serum TNF concentrations during endotoxemia by LPS []. Furthermore, an overall increased sympathetic activity would seem to support the inflammatory process of UC, which can also be inferred from the fact that psychological stress can reactivate quiescent UC. On the other hand, increasing para-sympathetic organ drive using a nicotine patch has been shown to improve the inflammatory state in patients with UC [].
However, as previously described, studies investigating clonidine administration in patients with ulcerative colitis are limited. Lechin et al. in 1985 observed a clinical and endoscopic improvement with clonidine treatment, and it was significantly more effective when compared to sulfasalazine, while there were no significant differences between prednisone and clonidine treatment [].
Later, although they stated that their investigation must not be considered a pharmacological trial, Furlan and collaborators found that clonidine reduced systemic neural sympathetic activity and increased vagal cardiac modulation, which was associated with decreased DAI, indicated by amelioration of clinical symptoms and colon endoscopic pattern. However, several crucial variables, including smoking status, previous UC therapy, and gender, were documented but not individually examined, likely due to the limited size of the sample. The researchers did not specify whether a post hoc test was conducted during the statistical analysis. Even in this case, the number of patients treated, and the observation time are limited, so future more extensive studies are needed to aim for such an alternative or combined therapy for future clinical practice in IBD []. Notably, no significant hypotensive effects were reported during treatment in these studies.
Conversely, for drugs such as pregabalin and lithium carbonate, the precise mechanisms by which they may influence intestinal inflammation in IBD remain largely unclear. However, some preclinical data provide mechanistic insights. In a murine model of acetic acid-induced colitis, pregabalin reduced both macroscopic and microscopic intestinal damage and inflammation, decreasing colonic levels of TNF-α, IL-6, IL-1β, and myeloperoxidase (MPO) activity [DOI: 10.4103/1735-5362.329924]. Pregabalin appears to exert its effects via modulation of the glutamate/N-methyl-D-aspartate receptor (NMDA)–nuclear factor kappa B (NF-κB)–cyclooxygenase-2 (COX-2) signaling axis, leading to reduced cytokine secretion and neutrophil infiltration. Additionally, pregabalin may attenuate neurogenic inflammation through interaction with the alpha-2-delta (α2δ) subunits of voltage-gated calcium channels. In sensitized animal models, it has been shown to reduce accelerated defecation and increase the colonic nociceptive threshold, indicating a role in visceral pain modulation [].
Regarding lithium, it has been shown to inhibit glycogen synthase kinase-3 beta (GSK-3β), activate the wingless-related integration site/beta-catenin (Wnt/β-catenin) signaling pathway. This activity promotes epithelial regeneration and downregulates key inflammatory mediators such as COX-2, TNF-α, and IL-1β.
Accordingly, in dextran sulfate sodium (DSS)-induced colitis models, lithium carbonate also promoted the activation of regulatory T lymphocytes (Tregs) via the G-protein-coupled receptor 43 (GPR43), contributing to the attenuation of intestinal inflammation []. In summary, the beneficial effects observed with antidepressants, clonidine, and naltrexone likely reflect their shared ability to modulate both central and peripheral inflammatory pathways. Antidepressants exert anti-inflammatory actions via cytokine suppression, vagal tone enhancement, and microbiota modulation. Naltrexone acts through μ-opioid receptor blockade and TLR4 inhibition, while clonidine reduces sympathetic activity and activates the cholinergic anti-inflammatory pathway. In contrast, agents like topiramate lack such immunomodulatory properties, and pregabalin or lithium although promising are supported only by limited preclinical evidence.
5. Strengths and Limitations
A key strength of our systematic review lies in its global perspective, achieved through an extensive and comprehensive literature search that included studies conducted across multiple countries and over an extended time frame. Notably, this is the first systematic effort to compile all available evidence, including case series and case reports, on the efficacy of psychiatric medications in managing gastrointestinal symptoms, as well as both direct and surrogate markers of disease activity in IBD.
However, our review has certain limitations that should be acknowledged. The studies included encompass a wide range of designs—randomized and nonrandomized controlled trials, observational studies (both prospective and retrospective), case series, and case reports—which exhibit significant heterogeneity in study design, study population, intervention, definition of outcome and in the modality of outcome measurement. This heterogeneity precluded the possibility of performing a meta-analysis, limited the statistical power and impaired the overall level of evidence derived from this review.
6. Conclusions
This systematic review demonstrates the potential of several classes of psychiatric medications to improve both gastroenterological outcomes, such as inflammation and disease activity, and psychological well-being in IBD. Antidepressants, including bupropion, TCAs, SSRIs, venlafaxine, and duloxetine, have been consistently associated with improvements in both direct and surrogate markers of disease activity. While case reports suggest potential benefits from pregabalin and lithium carbonate, no improvement in disease activity has been observed with topiramate. Moreover, some RCTs have reported positive outcomes with clonidine and naltrexone in both UC and CD.
Our review also highlights the mechanisms of these psychotropic drugs that extend beyond the “simple” neurochemical modulation within the central nervous system, also contributing to an anti-inflammatory action, which may in the future allow their use as adjuvant anti-inflammatory therapies. These findings suggest that a holistic approach, integrating psychiatry with other medical disciplines in IBD care, holds promise for improving disease activity, clinical and surgical outcomes, and quality of life in IBD patients. However, further robust RCTs with larger sample sizes and standardized outcome measures, along with translational research, are necessary to evaluate whether psychiatric medications with well-established safety profiles could serve as adjuvant treatments in IBD management or function as anti-inflammatory and immunomodulatory agents.
Supplementary Materials
The supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms26136514/s1. References [,,,,,,,,,,,,,,,,] are cited in the supplementary materials.
Author Contributions
Conceptualization, F.D.V. and A.M.D.; methodology, F.D.V.; validation, A.D.G., E.C., and A.M.D.; formal analysis, G.F.F. and F.P.; investigation, A.S., M.M.; resources, G.D.K., M.P., and G.M.; data curation, E.C.; writing—original draft preparation, F.D.V.; writing—review and editing, G.M., A.D.G., and F.P.; visualization, L.R.L.; supervision, A.G., G.S., G.F., F.S., and G.C.; project administration, F.D.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
This systematic review is based on publicly available data from previously published studies. All data used in this review are accessible through the cited articles and their respective publishers. No new data were generated for this study.
Acknowledgments
Thanks to Fondazione Roma for continuous support for our scientific research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Goodhand, J.R.; Wahed, M.; Mawdsley, J.E.; Farmer, A.D.; Aziz, Q.; Rampton, D.S. Mood disorders in inflammatory bowel disease: Relation to diagnosis, disease activity, perceived stress, and other factors. Inflamm. Bowel. Dis. 2012, 18, 2301–2309. [Google Scholar] [CrossRef]
- Roderburg, C.; Yaqubi, K.; Konrad, M.; May, P.; Luedde, T.; Kostev, K.; Loosen, S.H. Association between inflammatory bowel disease and subsequent depression or anxiety disorders—A retrospective cohort study of 31,728 outpatients. J. Psychiatr. Res. 2024, 169, 231–237. [Google Scholar] [CrossRef]
- Bernstein, C.N.; Fisk, J.D.; Dolovich, C.; Hitchon, C.A.; Graff, L.A.; El-Gabalawy, R.; Lix, L.M.; Bolton, J.M.; Patten, S.B.; Marrie, R.A. Understanding Predictors of Fatigue Over Time in Persons With Inflammatory Bowel Disease: The Importance of Depressive and Anxiety Symptoms. Am. J. Gastroenterol. 2024, 119, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Neuendorf, R.; Harding, A.; Stello, N.; Hanes, D.; Wahbeh, H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. J. Psychosom. Res. 2016, 87, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Barberio, B.; Zamani, M.; Black, C.J.; Savarino, E.V.; Ford, A.C. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 359–370. [Google Scholar] [CrossRef]
- Maunder, R.G.; Levenstein, S. The role of stress in the development and clinical course of inflammatory bowel disease: Epidemiological evidence. Curr. Mol. Med. 2008, 8, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Fairbrass, K.M.; Lovatt, J.; Barberio, B.; Yuan, Y.; Gracie, D.J.; Ford, A.C. Bidirectional brain-gut axis effects influence mood and prognosis in IBD: A systematic review and meta-analysis. Gut 2022, 71, 1773–1780. [Google Scholar] [CrossRef]
- Jain, A.; Marrie, R.A.; Shafer, L.A.; Graff, L.A.; Patten, S.B.; El-Gabalawy, R.; Sareen, J.; Bolton, J.M.; Fisk, J.D.; Bernstein, C.N. Incidence of Adverse Psychiatric Events During Treatment of Inflammatory Bowel Disease With Biologic Therapies: A Systematic Review. Crohn’s Colitis 360 2020, 2, otz053. [Google Scholar] [CrossRef]
- Menichetti, J.; Fiorino, G.; Vegni, E. Personalizing Psychological Treatment Along the IBD Journey: From Diagnosis to Surgery. Curr. Drug Targets 2018, 19, 722–728. [Google Scholar] [CrossRef]
- Buckley, J.P.; Kappelman, M.D.; Allen, J.K.; Van Meter, S.A.; Cook, S.F. The burden of comedication among patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2013, 19, 2725–2736. [Google Scholar] [CrossRef]
- Thorkelson, G.; Bielefeldt, K.; Szigethy, E. Empirically Supported Use of Psychiatric Medications in Adolescents and Adults with IBD. Inflamm. Bowel Dis. 2016, 22, 1509–1522. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.; Andrews, J.M. Attitudes towards antidepressants among people living with inflammatory bowel disease: An online Australia-wide survey. J. Crohn’s Colitis 2014, 8, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Tarricone, I.; Regazzi, M.G.; Bonucci, G.; Rizzello, F.; Carini, G.; Muratori, R.; Poggioli, G.; Campieri, M.; EspriMici Study Group. Prevalence and effectiveness of psychiatric treatments for patients with IBD: A systematic literature review. J. Psychosom. Res. 2017, 101, 68–95. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264. [Google Scholar] [CrossRef]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The well-built clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, A12. [Google Scholar] [CrossRef]
- Kim, D.B.; Lee, K.-M.; Lee, J.M.; Chung, Y.Y.; Sung, H.J.; Paik, C.N.; Chung, W.C.; Jung, J.-H.; Choi, H.J. Correlation between Histological Activity and Endoscopic, Clinical, and Serologic Activities in Patients with Ulcerative Colitis. Gastroenterol. Res. Pract. 2016, 2016, 32051. [Google Scholar] [CrossRef]
- Vermeire, S.; Schreiber, S.; Sandborn, W.J.; Dubois, C.; Rutgeerts, P. Correlation Between the Crohn’s Disease Activity and Harvey–Bradshaw Indices in Assessing Crohn’s Disease Severity. Clin. Gastroenterol. Hepatol. 2010, 8, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Best, W.R.; Becktel, J.M.; Singleton, J.W.; Kern, F. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology 1976, 70, 439–444. [Google Scholar] [CrossRef]
- Yarlas, A.; Maher, S.; Bayliss, M.; Lovley, A.; Cappelleri, J.C.; Bushmakin, A.G.; DiBonaventura, M.D. The Inflammatory Bowel Disease Questionnaire in Randomized Controlled Trials of Treatment for Ulcerative Colitis: Systematic Review and Meta-Analysis. J. Patient Cent. Res. Rev. 2020, 7, 189–205. [Google Scholar] [CrossRef]
- Lichtiger, S.; Present, D.H.; Kornbluth, A.; Gelernt, I.; Bauer, J.; Galler, G.; Michelassi, F.; Hanauer, S. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N. Engl. J. Med. 1994, 330, 1841–1845. [Google Scholar] [CrossRef]
- Turner, D.; Seow, C.H.; Greenberg, G.R.; Griffiths, A.M.; Silverberg, M.S.; Steinhart, A.H. A systematic prospective comparison of noninvasive disease activity indices in ulcerative colitis. Clin. Gastroenterol. Hepatol. 2009, 7, 1081–1088. [Google Scholar] [CrossRef]
- Travis, S.P.L.; Schnell, D.; Krzeski, P.; Abreu, M.T.; Altman, D.G.; Colombel, J.-F.; Feagan, B.G.; Hanauer, S.B.; Lémann, M.; Lichtenstein, G.R.; et al. Developing an instrument to assess the endoscopic severity of ulcerative colitis: The Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Gut 2012, 61, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Daperno, M.; D’Haens, G.; Van Assche, G.; Baert, F.; Bulois, P.; Maunoury, V.; Sostegni, R.; Rocca, R.; Pera, A.; Gevers, A.; et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: The SES-CD. Gastrointest. Endosc. 2004, 60, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Ardizzone, S.; Bianchi Porro, G. A practical guide to the management of distal ulcerative colitis. Drugs 1998, 55, 519–542. [Google Scholar] [CrossRef]
- Hall, B.J.; Hamlin, P.J.; Gracie, D.J.; Ford, A.C. The Effect of Antidepressants on the Course of Inflammatory Bowel Disease. Can J. Gastroenterol. Hepatol. 2018, 2018, 2047242. [Google Scholar] [CrossRef]
- Kristensen, M.S.; Kjærulff, T.M.; Ersbøll, A.K.; Green, A.; Hallas, J.; Thygesen, L.C. The Influence of Antidepressants on the Disease Course Among Patients With Crohn’s Disease and Ulcerative Colitis—A Danish Nationwide Register–Based Cohort Study. Inflammatory Bowel Diseases 2019, 25, 886–893. [Google Scholar] [CrossRef]
- Yanartas, O.; Kani, H.T.; Bicakci, E.; Kilic, I.; Banzragch, M.; Acikel, C.; Atug, O.; Kuscu, K.; Imeryuz, N.; Akin, H. The effects of psychiatric treatment on depression, anxiety, quality of life, and sexual dysfunction in patients with inflammatory bowel disease. Neuropsychiatr. Dis. Treat. 2016, 12, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Goodhand, J.R.; Greig, F.I.S.; Koodun, Y.; McDermott, A.; Wahed, M.; Langmead, L.; Rampton, D.S. Do antidepressants influence the disease course in inflammatory bowel disease? A retrospective case-matched observational study. Inflamm. Bowel Dis. 2012, 18, 1232–1239. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.; Hughes, P.A.; Bampton, P.; Gordon, A.; Campaniello, M.A.; Mavrangelos, C.; Stewart, B.J.; Esterman, A.; Andrews, J.M. Fluoxetine for Maintenance of Remission and to Improve Quality of Life in Patients with Crohn’s Disease: A Pilot Randomized Placebo-Controlled Trial. J. Crohn’s Colitis 2017, 11, 509–514. [Google Scholar] [CrossRef]
- Daghaghzadeh, H.; Naji, F.; Afshar, H.; Sharbafchi, M.R.; Feizi, A.; Maroufi, M.; Tabatabaeeyan, M.; Adibi, P.; Tavakoli, H. Efficacy of duloxetine add on in treatment of inflammatory bowel disease patients: A double-blind controlled study. J. Res. Med. Sci. 2015, 20, 595–601. [Google Scholar] [CrossRef]
- Liang, C.; Chen, P.; Tang, Y.; Zhang, C.; Lei, N.; Luo, Y.; Duan, S.; Zhang, Y. Venlafaxine as an Adjuvant Therapy for Inflammatory Bowel Disease Patients With Anxious and Depressive Symptoms: A Randomized Controlled Trial. Front. Psychiatry 2022, 13, 880058. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, H.N.; Cassell, B.; Kanuri, N.; Gyawali, C.P.; Gutierrez, A.; Dassopoulos, T.; Ciorba, M.A.; Sayuk, G.S. Tricyclic antidepressants for management of residual symptoms in inflammatory bowel disease. J. Clin. Gastroenterol. 2014, 48, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Chojnacki, C.; Walecka-Kapica, E.; Klupinska, G.; Pawłowicz, M.; Florkowski, A.; Wachowska-Kelly, P.; Chojnacki, J. Evaluation of the influence of tianeptine on the psychosomatic status of patients with ulcerative colitis in remission. Pol. Merkur. Lekarski 2011, 31, 92–96. [Google Scholar]
- Kane, S.; Altschuler, E.L.; Kast, R.E. Crohn’s disease remission on bupropion. Gastroenterology 2003, 125, 1290. [Google Scholar] [CrossRef]
- Kast, R.E.; Altschuler, E.L. Remission of Crohn’s disease on bupropion. Gastroenterology 2001, 121, 1260–1261. [Google Scholar] [CrossRef]
- Kast, R.E. Crohn’s disease remission with phenelzine treatment. Gastroenterology 1998, 115, 1034–1035. [Google Scholar] [CrossRef] [PubMed]
- Jayasooriya, N.; Blackwell, J.; Saxena, S.; Bottle, A.; Petersen, I.; Creese, H.; Hotopf, M.; Pollok, R.C.G.; POP-IBD study group. Antidepressant medication use in Inflammatory Bowel Disease: A nationally representative population-based study. Aliment. Pharmacol. Ther. 2022, 55, 1330–1341. [Google Scholar] [CrossRef]
- Crockett, S.D.; Schectman, R.; Stürmer, T.; Kappelman, M.D. Topiramate use does not reduce flares of inflammatory bowel disease. Dig. Dis. Sci. 2014, 59, 1535–1543. [Google Scholar] [CrossRef]
- D’Onofrio, A.M.; Di Vincenzo, F.; Ferrajoli, G.F.; Scaldaferri, F.; Camardese, G. Low Dose Pregabalin Improves Gastrointestinal Symptoms of Crohn’s Disease. Case Rep. Gastrointest. Med. 2024, 2024, 3744500. [Google Scholar] [CrossRef]
- Bernstein, C.N.; Fisk, J.D.; Walld, R.; Bolton, J.M.; Sareen, J.; Patten, S.B.; Singer, A.; Lix, L.M.; Hitchon, C.A.; El-Gabalawy, R.; et al. Use of Benzodiazepines and Z-Drugs in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2022, 117, 2046–2054. [Google Scholar] [CrossRef]
- Stokes, D.K. Lorazepam in anxiety associated with chronic enteritis and ulcerative colitis. J. Clin. Psychiatry 1978, 39, 53–57. [Google Scholar]
- Zisook, S. Ulcerative colitis: Case responding to treatment with lithium carbonate. JAMA 1972, 219, 755. [Google Scholar] [CrossRef]
- Lie, M.R.K.L.; Van Der Giessen, J.; Fuhler, G.M.; de Lima, A.; Peppelenbosch, M.P.; Van Der Ent, C.; Van Der Woude, C.J. Low dose Naltrexone for induction of remission in inflammatory bowel disease patients. J. Transl. Med. 2018, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.P.; Bingaman, S.I.; Ruggiero, F.; Mauger, D.T.; Mukherjee, A.; McGovern, C.O.; Zagon, I.S. Therapy with the Opioid Antagonist Naltrexone Promotes Mucosal Healing in Active Crohn’s Disease: A Randomized Placebo-Controlled Trial. Dig. Dis. Sci. 2011, 56, 2088–2097. [Google Scholar] [CrossRef]
- Smith, J.P.; Stock, H.; Bingaman, S.; Mauger, D.; Rogosnitzky, M.; Zagon, I.S. Low-dose naltrexone therapy improves active Crohn’s disease. Am. J. Gastroenterol. 2007, 102, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.P.; Field, D.; Bingaman, S.I.; Evans, R.; Mauger, D.T. Safety and tolerability of low-dose naltrexone therapy in children with moderate to severe Crohn’s disease: A pilot study. J. Clin. Gastroenterol. 2013, 47, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Lechin, F.; Van Der Dijs, B.; Insausti, C.L.; Gómez, F.; Villa, S.; Lechin, A.E.; Arocha, L.; Oramas, O. Treatment of Ulcerative Colitis With Clonidine. J. Clin. Pharma 1985, 25, 219–226. [Google Scholar] [CrossRef]
- Furlan, R.; Ardizzone, S.; Palazzolo, L.; Rimoldi, A.; Perego, F.; Barbic, F.; Bevilacqua, M.; Vago, L.; Porro, G.B.; Malliani, A. Sympathetic overactivity in active ulcerative colitis: Effects of clonidine. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2006, 290, R224–R232. [Google Scholar] [CrossRef]
- Paulides, E.; Lie, M.R.K.L.; Van Der Woude, C.J. Low-dose naltrexone for the induction of remission in patients with mild to moderate Crohn’s disease: Protocol for the randomised, double-blinded, placebo-controlled, multicentre LDN Crohn study. BMJ Open 2022, 12, e058358. [Google Scholar] [CrossRef]
- Fava, G.A.; Gatti, A.; Belaise, C.; Guidi, J.; Offidani, E. Withdrawal Symptoms after Selective Serotonin Reuptake Inhibitor Discontinuation: A Systematic Review. Psychother. Psychosom. 2015, 84, 72–81. [Google Scholar] [CrossRef]
- Fuller-Thomson, E.; Sulman, J. Depression and inflammatory bowel disease: Findings from two nationally representative Canadian surveys. Inflamm. Bowel Dis. 2006, 12, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Haapamäki, J.; Tanskanen, A.; Roine, R.P.; Blom, M.; Turunen, U.; Mäntylä, J.; Färkkilä, M.A.; Arkkila, P.E.T. Medication use among inflammatory bowel disease patients: Excessive consumption of antidepressants and analgesics. Scand. J. Gastroenterol. 2013, 48, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Mikocka-Walus, A.; Prady, S.L.; Pollok, J.; Esterman, A.J.; Gordon, A.L.; Knowles, S.; Andrews, J.M. Adjuvant therapy with antidepressants for the management of inflammatory bowel disease. Cochrane Database Syst. Rev. 2019, 4, CD012680. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.A.; Turnbull, D.A.; Moulding, N.T.; Wilson, I.G.; Andrews, J.M.; Holtmann, G.J. Antidepressants and inflammatory bowel disease: A systematic review. Clin. Pract. Epidemiol. Ment. Health 2006, 2, 24. [Google Scholar] [CrossRef]
- Macer, B.J.D.; Prady, S.L.; Mikocka-Walus, A. Antidepressants in Inflammatory Bowel Disease: A Systematic Review. Inflamm. Bowel Dis. 2017, 23, 534–550. [Google Scholar] [CrossRef] [PubMed]
- Frolkis, A.D.; Vallerand, I.A.; Shaheen, A.-A.; Lowerison, M.W.; Swain, M.G.; Barnabe, C.; Patten, S.B.; Kaplan, G.G. Depression increases the risk of inflammatory bowel disease, which may be mitigated by the use of antidepressants in the treatment of depression. Gut 2019, 68, 1606–1612. [Google Scholar] [CrossRef]
- Ghia, J.-E.; Blennerhassett, P.; Collins, S.M. Impaired parasympathetic function increases susceptibility to inflammatory bowel disease in a mouse model of depression. J. Clin. Investig. 2008, 118, 2209–2218. [Google Scholar] [CrossRef]
- Ghia, J.; Blennerhassett, P.; Deng, Y.; Verdu, E.F.; Khan, W.I.; Collins, S.M. Reactivation of Inflammatory Bowel Disease in a Mouse Model of Depression. Gastroenterology 2009, 136, 2280–2288.e4. [Google Scholar] [CrossRef]
- Więdłocha, M.; Marcinowicz, P.; Krupa, R.; Janoska-Jaździk, M.; Janus, M.; Dębowska, W.; Mosiołek, A.; Waszkiewicz, N.; Szulc, A. Effect of antidepressant treatment on peripheral inflammation markers—A meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 80, 217–226. [Google Scholar] [CrossRef]
- Martino, M.; Rocchi, G.; Escelsior, A.; Fornaro, M. Immunomodulation Mechanism of Antidepressants: Interactions between Serotonin/Norepinephrine Balance and Th1/Th2 Balance. Curr. Neuropharmacol. 2012, 10, 97–123. [Google Scholar] [CrossRef]
- Varghese, A.K.; Verdú, E.F.; Bercik, P.; Khan, W.I.; Blennerhassett, P.A.; Szechtman, H.; Collins, S.M. Antidepressants attenuate increased susceptibility to colitis in a murine model of depression. Gastroenterology 2006, 130, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Guemei, A.A.; El Din, N.M.N.; Baraka, A.M.; El Said Darwish, I. Do desipramine [10,11-dihydro-5-[3-(methylamino) propyl]-5H-dibenz[b,f]azepine monohydrochloride] and fluoxetine [N-methyl-3-phenyl-3-[4-(trifluoromethyl)phenoxy]-propan-1-amine] ameliorate the extent of colonic damage induced by acetic acid in rats? J. Pharmacol. Exp. Ther. 2008, 327, 846–850. [Google Scholar] [CrossRef]
- Teng, S.; Yang, Y.; Zhang, W.; Li, X.; Li, W.; Cui, Z.; Min, L.; Wu, J. Antidepressant fluoxetine alleviates colitis by reshaping intestinal microenvironment. Cell Commun. Signal. 2024, 22, 176. [Google Scholar] [CrossRef]
- Coleman, J.A.; Green, E.M.; Gouaux, E. X-ray structures and mechanism of the human serotonin transporter. Nature 2016, 532, 334–339. [Google Scholar] [CrossRef]
- Zhu, J.; Smith, K.; Hsieh, P.N.; Mburu, Y.K.; Chattopadhyay, S.; Sen, G.C.; Sarkar, S.N. High-throughput screening for TLR3-IFN regulatory factor 3 signaling pathway modulators identifies several antipsychotic drugs as TLR inhibitors. J. Immunol. 2010, 184, 5768–5776. [Google Scholar] [CrossRef] [PubMed]
- Branco-de-Almeida, L.S.; Kajiya, M.; Cardoso, C.R.; Silva, M.J.B.; Ohta, K.; Rosalen, P.L.; Franco, G.C.N.; Han, X.; Taubman, M.A.; Kawai, T. Selective serotonin reuptake inhibitors attenuate the antigen presentation from dendritic cells to effector T lymphocytes. FEMS Immunol. Med. Microbiol. 2011, 62, 283–294. [Google Scholar] [CrossRef][Green Version]
- Vollmar, P.; Nessler, S.; Kalluri, S.R.; Hartung, H.-P.; Hemmer, B. The antidepressant venlafaxine ameliorates murine experimental autoimmune encephalomyelitis by suppression of pro-inflammatory cytokines. Int. J. Neuropsychopharmacol. 2009, 12, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Martino, M.; Rocchi, G.; Escelsior, A.; Contini, P.; Colicchio, S.; de Berardis, D.; Amore, M.; Fornaro, P.; Fornaro, M. NGF serum levels variations in major depressed patients receiving duloxetine. Psychoneuroendocrinology 2013, 38, 1824–1828. [Google Scholar] [CrossRef]
- Fornaro, M.; Martino, M.; Battaglia, F.; Colicchio, S.; Perugi, G. Increase in IL-6 levels among major depressive disorder patients after a 6-week treatment with duloxetine 60 mg/day: A preliminary observation. Neuropsychiatr. Dis. Treat. 2011, 7, 51–56. [Google Scholar] [CrossRef]
- Başterzi, A.D.; Yazici, K.; Buturak, V.; Cimen, B.; Yazici, A.; Eskandari, G.; Tot Acar, S.; Taşdelen, B. Effects of venlafaxine and fluoxetine on lymphocyte subsets in patients with major depressive disorder: A flow cytometric analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2010, 34, 70–75. [Google Scholar] [CrossRef]
- Arnone, D.; Saraykar, S.; Salem, H.; Teixeira, A.L.; Dantzer, R.; Selvaraj, S. Role of Kynurenine pathway and its metabolites in mood disorders: A systematic review and meta-analysis of clinical studies. Neurosci. Biobehav. Rev. 2018, 92, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.H.; Raison, C.L. The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 2016, 16, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Sforzini, L.; Nettis, M.A.; Mondelli, V.; Pariante, C.M. Inflammation in cancer and depression: A starring role for the kynurenine pathway. Psychopharmacology 2019, 236, 2997–3011. [Google Scholar] [CrossRef] [PubMed]
- Umehara, H.; Numata, S.; Watanabe, S.-Y.; Hatakeyama, Y.; Kinoshita, M.; Tomioka, Y.; Nakahara, K.; Nikawa, T.; Ohmori, T. Altered KYN/TRP, Gln/Glu, and Met/methionine sulfoxide ratios in the blood plasma of medication-free patients with major depressive disorder. Sci. Rep. 2017, 7, 4855. [Google Scholar] [CrossRef]
- Xu, F.; Xie, Q.; Kuang, W.; Dong, Z. Interactions Between Antidepressants and Intestinal Microbiota. Neurotherapeutics 2023, 20, 359–371. [Google Scholar] [CrossRef]
- Lukić, I.; Getselter, D.; Ziv, O.; Oron, O.; Reuveni, E.; Koren, O.; Elliott, E. Antidepressants affect gut microbiota and Ruminococcus flavefaciens is able to abolish their effects on depressive-like behavior. Transl. Psychiatry 2019, 9, 133. [Google Scholar] [CrossRef]
- Zhang, W.; Qu, W.; Wang, H.; Yan, H. Antidepressants fluoxetine and amitriptyline induce alterations in intestinal microbiota and gut microbiome function in rats exposed to chronic unpredictable mild stress. Transl. Psychiatry 2021, 11, 131. [Google Scholar] [CrossRef]
- Getachew, B.; Aubee, J.I.; Schottenfeld, R.S.; Csoka, A.B.; Thompson, K.M.; Tizabi, Y. Ketamine interactions with gut-microbiota in rats: Relevance to its antidepressant and anti-inflammatory properties. BMC Microbiol. 2018, 18, 222. [Google Scholar] [CrossRef]
- Birkinshaw, H.; Friedrich, C.M.; Cole, P.; Eccleston, C.; Serfaty, M.; Stewart, G.; White, S.; Moore, R.A.; Phillippo, D.; Pincus, T. Antidepressants for pain management in adults with chronic pain: A network meta-analysis. Cochrane Database Syst. Rev. 2023, 5, CD014682. [Google Scholar] [CrossRef]
- Pan, H.-L.; Wu, Z.-Z.; Zhou, H.-Y.; Chen, S.-R.; Zhang, H.-M.; Li, D.-P. Modulation of pain transmission by G-protein-coupled receptors. Pharmacol. Ther. 2008, 117, 141–161. [Google Scholar] [CrossRef]
- Köhler-Forsberg, O.; Stiglbauer, V.; Brasanac, J.; Chae, W.R.; Wagener, F.; Zimbalski, K.; Jefsen, O.H.; Liu, S.; Seals, M.R.; Gamradt, S.; et al. Efficacy and Safety of Antidepressants in Patients With Comorbid Depression and Medical Diseases: An Umbrella Systematic Review and Meta-Analysis. JAMA Psychiatry 2023, 80, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Oliva, V.; Lippi, M.; Paci, R.; Del Fabro, L.; Delvecchio, G.; Brambilla, P.; De Ronchi, D.; Fanelli, G.; Serretti, A. Gastrointestinal side effects associated with antidepressant treatments in patients with major depressive disorder: A systematic review and meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110266. [Google Scholar] [CrossRef]
- Barros, L.L.; Farias, A.Q.; Rezaie, A. Gastrointestinal motility and absorptive disorders in patients with inflammatory bowel diseases: Prevalence, diagnosis and treatment. World. J. Gastroenterol. 2019, 25, 4414–4426. [Google Scholar] [CrossRef]
- Tack, J.; Broekaert, D.; Corsetti, M.; Fischler, B.; Janssens, J. Influence of acute serotonin reuptake inhibition on colonic sensorimotor function in man. Aliment. Pharmacol. Ther. 2006, 23, 265–274. [Google Scholar] [CrossRef]
- Kenna, H.A.; Poon, A.W.; de los Angeles, C.P.; Koran, L.M. Psychiatric complications of treatment with corticosteroids: Review with case report. Psychiatry Clin. Neurosci. 2011, 65, 549–560. [Google Scholar] [CrossRef]
- Gordon, H.; Minozzi, S.; Kopylov, U.; Verstockt, B.; Chaparro, M.; Buskens, C.; Warusavitarne, J.; Agrawal, M.; Allocca, M.; Atreya, R.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Medical Treatment. J. Crohn’s Colitis 2024, 18, 1531–1555. [Google Scholar] [CrossRef]
- Brown, E.S.; Suppes, T. Mood symptoms during corticosteroid therapy: A review. Harv. Rev. Psychiatry 1998, 5, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Vanner, S.; Kashyap, P.C.; Nasser, Y. Chronic Visceral Pain: New Peripheral Mechanistic Insights and Resulting Treatments. Gastroenterology 2024, 166, 976–994. [Google Scholar] [CrossRef] [PubMed]
- Sternini, C.; Patierno, S.; Selmer, I.-S.; Kirchgessner, A. The opioid system in the gastrointestinal tract. Neurogastroenterol. Motil. 2004, 16, 3–16. [Google Scholar] [CrossRef]
- Ramanathan, S.; Panksepp, J.; Johnson, B. Is Fibromyalgia An Endocrine/Endorphin Deficit Disorder? Is Low Dose Naltrexone a New Treatment Option? Psychosomatics 2012, 53, 591–594. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Peng, Y.; Hutchinson, M.R.; Rice, K.C.; Yin, H.; Watkins, L.R. Pharmacological characterization of the opioid inactive isomers (+)-naltrexone and (+)-naloxone as antagonists of toll-like receptor 4. Br. J. Pharmacol. 2016, 173, 856–869. [Google Scholar] [CrossRef] [PubMed]
- Watkins, L.R.; Wang, X.; Mustafa, S.; Hutchinson, M.R. In vivo veritas: (+)-Naltrexone’s actions define translational importance. Trends Pharmacol. Sci. 2014, 35, 432–433. [Google Scholar] [CrossRef] [PubMed]
- Deuring, J.J.; Fuhler, G.M.; Konstantinov, S.R.; Peppelenbosch, M.P.; Kuipers, E.J.; De Haar, C.; Van Der Woude, C.J. Genomic ATG16L1 risk allele-restricted Paneth cell ER stress in quiescent Crohn’s disease. Gut 2014, 63, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Moslehi, A.; Nabavizadeh, F.; Zekri, A.; Amiri, F. Naltrexone changes the expression of lipid metabolism—Related proteins in the endoplasmic reticulum stress induced hepatic steatosis in mice. Clin. Exp. Pharma. Physio. 2017, 44, 207–212. [Google Scholar] [CrossRef]
- Moslehi, A.; Nabavizadeh, F.; Dehpou, A.R.; Tavanga, S.M.; Hassanzadeh, G.; Zekri, A.; Nahrevanian, H.; Sohanaki, H. Naltrexone attenuates endoplasmic reticulum stress induced hepatic injury in mice. Acta Physiol. Hung. 2014, 101, 341–352. [Google Scholar] [CrossRef]
- Tawfik, D.I.; Osman, A.S.; Tolba, H.M.; Khattab, A.; Abdel-Salam, L.O.; Kamel, M.M. Evaluation of therapeutic effect of low dose naltrexone in experimentally-induced Crohn’s disease in rats. Neuropeptides 2016, 59, 39–45. [Google Scholar] [CrossRef]
- Alcaro, A.; Huber, R.; Panksepp, J. Behavioral functions of the mesolimbic dopaminergic system: An affective neuroethological perspective. Brain Res. Rev. 2007, 56, 283–321. [Google Scholar] [CrossRef]
- Brown, N.; Panksepp, J. Low-dose naltrexone for disease prevention and quality of life. Med. Hypotheses 2009, 72, 333–337. [Google Scholar] [CrossRef]
- Ghia, J.E.; Blennerhassett, P.; Kumar–Ondiveeran, H.; Verdu, E.F.; Collins, S.M. The Vagus Nerve: A Tonic Inhibitory Influence Associated With Inflammatory Bowel Disease in a Murine Model. Gastroenterology 2006, 131, 1122–1130. [Google Scholar] [CrossRef]
- Bernik, T.R.; Friedman, S.G.; Ochani, M.; DiRaimo, R.; Ulloa, L.; Yang, H.; Sudan, S.; Czura, C.J.; Ivanova, S.M.; Tracey, K.J. Pharmacological Stimulation of the Cholinergic Antiinflammatory Pathway. J. Exp. Med. 2002, 195, 781–788. [Google Scholar] [CrossRef]
- Pullan, R.D.; Rhodes, J.; Ganesh, S.; Mani, V.; Morris, J.S.; Williams, G.T.; Newcombe, R.G.; Russell, M.; Feyerabend, C.; Thomas, G.; et al. Transdermal Nicotine for Active Ulcerative Colitis. N. Engl. J. Med. 1994, 330, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Motavallian, A.; Zamani, E.; Bouzari, S.; Rezaeyan, F.; Karimian, P.; Evazalipour, M. Anti-inflammatory effect of pregabalin on acetic acid-induced colitis in the rats. Res. Pharm. Sci. 2022, 17, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Hu, S.; Liu, S.; Tang, B.; Liu, Y.; Tang, L.; Lei, Y.; Zhong, L.; Yang, S.; He, S. Lithium carbonate alleviates colon inflammation through modulating gut microbiota and Treg cells in a GPR43-dependent manner. Pharmacol. Res. 2022, 175, 105992. [Google Scholar] [CrossRef]
- Allergan USA, Inc. Highlights of Prescribing Information Celexa® (Citalopram). Ref. ID 4933291. Published Online February 2022. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020822s041lbl.pdf (accessed on 30 March 2025).
- Abbvie Inc. Highlights of Prescribing Information Lexapro® (Escitalopram). Reference ID: 5367836. Published Online April 2024. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/021323s058lbl.pdf (accessed on 30 March 2025).
- Jazz Pharmaceuticals, Inc. Highlights of Prescribing Information Luvox® (Fluvoxamine Maleate). Published Online 2008. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/022235lbl.pdf (accessed on 30 March 2025).
- Apotex Inc. Highlights of Prescribing Information Paxil (Paroxetine). Reference ID: 5274678. Published Online August 2023. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/020031s082lbl.pdf (accessed on 30 March 2025).
- Viatris Specialty LLC. Highlights of Prescribing Information ZOLOFT (Sertraline Hydrochloride). Reference ID: 5229497. Published Online August 2023. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/019839s108,20990s062lbl.pdf (accessed on 30 March 2025).
- Lilly USA, LLC. Highlights of Prescribing Information Cymbalta® (Duloxetine Delayed-Release Capsules). Reference ID: 5229383. Published Online August 2023. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/021427s055s057lbl.pdf (accessed on 30 March 2025).
- Viatris Specialty LLC. Highlights of Prescribing Information Effexor XR® (Venlafaxine Extended-Release). Reference ID: 5229419. Published Online August 2023. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/020699s118lbl.pdf (accessed on 30 March 2025).
- GlaxoSmithKline. Highlights of Prescribing Information Wellbutrin (Bupropion Hydrochloride). Reference ID: 5376823. Published Online April 2024. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/018644s061lbl.pdf (accessed on 30 March 2025).
- Merck & Co Inc. Highlights of Prescribing Information Remeron® (Mirtazapine). Reference ID: 4878026. Published Online November 2021. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/020415s038,021208s028lbl.pdf (accessed on 30 March 2025).
- Norman, T.R.; Olver, J.S. Agomelatine for depression: Expanding the horizons? Expert Opin Pharmacother. 2019, 20, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Moraczewski, J.; Awosika, A.O.; Aedma, K.K. Tricyclic Antidepressants. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK557791/ (accessed on 24 July 2024).
- Sabri, M.A.; Saber-Ayad, M.M. MAO Inhibitors. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK557395/ (accessed on 24 July 2024).
- Janssen Ortho LLC. Highlights of Prescribing Information Topamax® (Topiramate). Reference ID: 5167873. Published Online May 2023. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/020505s065,020844s056lbl.pdf (accessed on 30 March 2025).
- West-Ward Pharmaceuticals. Highlights of Prescribing Information Lithium and Lithium Carbonate. Reference ID: 5060222. Published Online October 2022. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/017812s036,018421s035,018558s030lbl.pdf (accessed on 30 March 2025).
- Duramed Pharmaceuticals, Inc. Highlights of Prescribing Information Revia® (Naltrexone Hydrochloride). Reference ID: 3383348. Published Online October 2013. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/018932s017lbl.pdf (accessed on 30 March 2025).
- Peng, L.; Morford, K.L.; Levander, X.A. Benzodiazepines and Related Sedatives. Med. Clin. N. Am. 2022, 106, 113–129. [Google Scholar] [CrossRef]
- Siriwardena, A.N.; Qureshi, Z.; Gibson, S.; Collier, S.; Latham, M. GPs’ attitudes to benzodiazepine and “Z-drug” prescribing: A barrier to implementation of evidence and guidance on hypnotics. Br. J. Gen. Pract. 2006, 56, 964–967. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).