Abstract
Objectives: Prevention of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease COVID-19 is a public health priority. The efficacy of non-pharmaceutical interventions such as wearing face masks to prevent SARS-CoV-2 infection has been well established in controlled settings. However, evidence for the effectiveness of face masks in preventing SARS-CoV-2 transmission within real-world settings is limited and mixed. The present systematic review evaluated the effectiveness of face mask policies and mask wearing to prevent SARS-CoV-2 transmission and COVID-19 in real-world settings. Methods: Following PRISMA guidelines, scientific databases, and gray literature, were searched through June 2023. Inclusion criteria were as follows: (1) studies/reports written in or translated to English; (2) prospectively assessed incidence of SARS-CoV-2 or COVID-19; (3) assessed the behavior and/or policy of mask-wearing; and (4) conducted in community/public settings (i.e., not laboratory). Studies were excluded if they did not parse out data specific to the effect of mask wearing (behavior and/or policy) and subsequent SARS-CoV-2 transmission or COVID-19 disease or if they relied solely on statistical models to estimate the effects of mask wearing on transmission. A total of 2616 studies were initially identified, and 470 met inclusion and exclusion criteria for full-text review. The vote counting method was used to evaluate effectiveness, and risk of bias was assessed using JBI critical appraisal tools. Results: A total of 79 unique studies met the final inclusion criteria, and their data were abstracted and evaluated. Study settings included community/neighborhood settings (n = 34, 43%), healthcare settings (n = 30, 38%), and school/universities (n = 15, 19%). A majority of studies (n = 61, 77%) provided evidence to support the effectiveness of wearing face masks and/or face mask policies to reduce the transmission of SARS-CoV-2 and/or prevention of COVID-19. Effectiveness of mask wearing did not vary substantially by study design (67–100%), type of mask (77–100%), or setting (80–91%), while 85% of masking policies specifically reported a benefit. Conclusions: This systematic literature review supports public health recommendations and policies that encourage the public to wear face masks to reduce the risk of SARS-CoV-2 infection and COVID-19 in multiple real-world settings. Effective communication strategies are needed to encourage and support the use of face masks by the general public, particularly during peak infection cycles.
1. Introduction
Since the World Health Organization (WHO) declared COVID-19 a pandemic in March of 2020 [], the U.S. and other countries have experienced several waves of respiratory syndrome coronavirus 2 (SARS-CoV-2) infections, which put great strain on hospitals and the healthcare system []. SARS-CoV-2 is responsible for the disease COVID-19, and in 2020, COVID-19 was the third leading cause of death in the U.S. and the number one cause of death for people aged 45–84 years []. As of June 2023, there have been over 6.9 million reported deaths globally due to COVID-19, and minoritized/underserved populations have been disproportionately affected [].
Public health recommendations for the prevention of SARS-CoV-2 infection include vaccination, masking, social distancing, avoiding crowds and poorly ventilated spaces, frequent washing of hands, and disinfecting high touch surfaces []. Nonpharmaceutical interventions (NPIs), which are actions that persons and communities can take to help slow the spread of respiratory virus infections, are often the most readily available interventions to help slow the transmission of infectious viruses in communities []. Wearing personal protective equipment (PPE), such as face masks, has long been used in previous pandemics (e.g., 1920 influenza), epidemics, and outbreaks as an effective strategy to protect against the spread of respiratory infectious disease []. Despite ample evidence for the efficacy and effectiveness of PPE to prevent the transmission of respiratory infections (e.g., seasonal influenza, tuberculosis, etc.), the adoption of these preventive measures by the general public has varied widely. The emergence of increasingly infectious variants such as Delta and Omicron renewed questions about the role of masks to prevent the spread of SARS-CoV-2 []. These variants contain mutations that affect transmissibility and virulence, potentially impacting the efficacy and effectiveness of vaccines, therefore increasing the need to enact NPIs to help contain viral spread, particularly during peak outbreaks [].
Enacting policies that require people to use face masks in public to curb the spread of SARS-CoV-2 has been a politicized issue []. Misinformation surrounding the efficacy and effectiveness of face masks can threaten the health of the public. At the height of the COVID-19 pandemic, a subset of the U.S. population expressed strong opposition to wearing masks and mask mandates through social media channels (e.g., Twitter) []. Some of the most common reasons cited in opposition to wearing masks were the belief that wearing masks was not necessary for certain groups (e.g., children and healthy individuals), mask mandates infringed upon personal liberty, and that masks were uncomfortable and not effective at preventing SARS-CoV-2 infection []. Thus, policymakers and public health officials need better quality evidence for the effectiveness of masking policies and the use of masks to provide evidence-based guidance to the public [].
Previous literature reviews show that masks and facial coverings are efficacious at reducing the risk of SARS-CoV-2 transmission in controlled laboratory settings [,,]; however, the effectiveness of masks in real-world settings (e.g., schools, community settings, transportation, and hospitals) have not been well documented. The effectiveness of masks in real-world settings are impacted by multiple factors including the level of adherence, the mask type, and other environmental contexts []. Overall, findings regarding the effectiveness of mask wearing in community settings remain limited to date. Leech et al. [] used a Bayesian hierarchical model approach across 92 regions and found that self-reported mask wearing was associated with a 25% reduction in SARS-CoV-2 transmission, although mask mandates themselves were not associated with transmission rates. In contrast, Bundgaard et al. [] reported no significant difference in SARS-CoV-2 infection rates between participants who wore masks and those who did not. One of the earliest systematic reviews in community settings provided promising preliminary evidence for the effectiveness of mask wearing; however, the evidence was limited due to the small number of studies available at that time []. These mixed results highlight the need for an updated and synthesized review of the effectiveness of mask policies and wearing face masks in non-controlled, real-world settings. The purpose of this review was to evaluate the effectiveness of mask-wearing and masking policies for the prevention of SARS-CoV-2 transmission and COVID-19 in multiple real-world settings.
2. Methods
2.1. Data Sources
A systematic search of electronic databases was conducted in SCOPUS, PubMed, and CINAHL. Gray literature, such as conference abstracts, county data, and government reports, was also identified through ProQuest, MedRxiv, BioRxiv, and Google Scholar. Key terms were used to capture the relevant literature on making policies, mask wearing, and SARS-CoV-2 transmission and COVID-19. Table 1 summarizes the key terms used for this review. The study protocol was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY202460011).

Table 1.
List of key search terms.
2.2. Study Selection
Study eligibility criteria were as follows: (1) written in or translated to English; (2) prospectively assessed incidence of SARS-CoV-2 or COVID-19; (3) assessed the behavior and/or policy of mask wearing; and 4) conducted in community/public settings such as healthcare settings, worksites, and schools. Studies were excluded if (1) they did not parse out data specific to the effect of mask wearing (behavior and/or policy) and subsequent SARS-CoV-2 transmission or COVID-19; or (2) they relied solely on statistical models to estimate the effects of mask wearing on transmission (i.e., no primary data were collected on mask-wearing behavior or transmission). The time span for the literature search included all years available in the databases up to June 2023.
This study followed the structure and recommendations for reporting a systematic literature review as outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines []. Searches were uploaded to the Rayyan platform (Cambridge, MA, USA), which was also used to manage reviewer ratings and remove duplicate studies. Database searches and gray literature searches were conducted by two independent reviewers. After identifying articles from each database, duplicates were identified and removed before screening for inclusion criteria. A total of 2616 studies were screened and evaluated first by title and abstract for meeting inclusion and exclusion criteria by a primary and secondary reviewer. Discrepancies between reviewers were resolved after a discussion following the initial screening. Articles that met criteria in phase 1 (n = 470) underwent full-text review (phase 2) by two independent reviewers. Final inclusion of articles was determined after the full-text review. The included articles were also explored for works cited by using the backward referencing technique to search for additional literature that met the inclusion criteria.
2.3. Data Extraction
For all articles that met the inclusion and exclusion criteria (n = 79), relevant data and study characteristics were extracted by the two independent reviewers following a standardized data abstraction protocol. These included author, year, country, study design, outcome measures, study sample, main finding, adherence, duration, and study limitations.
2.4. Risk of Bias Assessment and Outcome Analysis
Two independent reviewers assessed the quality of included studies using Joanna Briggs Institute (JBI) critical appraisal tools []. A third reviewer was consulted when discrepancies were identified. JBI critical appraisal checklists are considered suitable and the most preferred for scoring quasi-experimental, observational, and cross-sectional study designs, which were the majority of studies included in this review []. Checklists specific to study design were used to evaluate criteria such as description of clinical condition, validity of measurement of disease outcome, appropriateness of statistical approaches, and mitigation of confounders. Each JBI risk of bias criterion for each study was rated as either red = “no”, green = “yes”, or yellow = “unclear.” Risk of bias was ranked as high when the study was rated with ≤49% of “yes” scores, moderate when the study was rated between 50 and 79% of “yes” scores, and low when the study was rated with ≥80% of “yes” scores.
Due to the high heterogeneity of statistical methods and study designs in the included studies, a vote counting methodology was used in lieu of a meta-analysis to summarize the direction of effect for masking behavior and/or masking policies for the prevention of SARS-CoV-2 transmission and COVID-19 disease []. The primary objective of this approach was to compare studies indicating a ‘benefit’ (i.e., prevention of SARS-CoV-2 transmission or COVID-19) with those indicating a potential ‘harm’ (i.e., increased SARS-CoV-2 transmission or COVID-19). Two independent reviewers read through each study to identify the reported effect estimate as well as the observed direction of effect of a masking policy and/or mask wearing to develop a standardized binary metric. The number of effects demonstrating benefit was then compared to the number of effects indicating harm, allowing for a quantitative assessment of the overall effectiveness of mask-wearing behavior and/or policies. The certainty of evidence was graded by classifying SARS-CoV-2 transmission and COVID-19 results and rating the evidence for each outcome in the Gradepro GDT Standard version.
3. Results
Results of the article screening process are presented in the PRISMA flow diagram (Figure 1). A total of 2616 articles and gray literature were identified, and 79 met the final criteria for inclusion and data abstraction. Table 2 summarizes key characteristics for each study included in this review. A greater proportion of studies (47%) were from the United States [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,], followed by China (10%) [,,,,,,,], Germany (8%) [,,,,,], Japan (4%) [,,], Spain (3%) [,], and other countries that had two or less studies (29%) [,,,,,,,,,,,,,,,,,,,,,,]. SARS-CoV-2 infection was primarily identified through lab-verified test results such as polymerase chain reaction rapid (PCR) antigen tests (n = 56) or serological tests (n = 4), followed by self-report (n = 6) and aggregate community-level data reports of COVID-19 cases (n = 13).
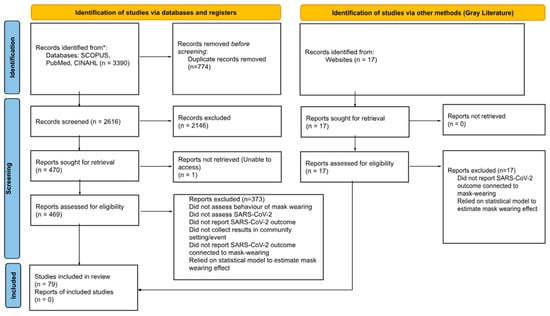
Figure 1.
PRISMA diagram.

Table 2.
Included studies.
3.1. Study Design and Vote Counting Results
Of the 79 studies, 34% (n = 27) were prospective or retrospective cohort studies, 29% (n = 23) were cross-sectional studies, 13% (n = 10) were case–control studies, 14% (n = 11) were case reports, 6% (n = 5) were quasi-experimental studies, and 4% (n = 3) were randomized controlled studies (RCTs). Overall, 77% (n = 61) of studies reported a beneficial association or effect of mask wearing or policy on SARS-CoV-2 transmission or COVID-19 disease (Table 3). Among the cross-sectional studies, 87% (n = 20) reported a beneficial association of mask wearing or policy on SARS-CoV-2 transmission or COVID-19. Ninety percent (n = 9) of case–control studies reported a beneficial effect of mask wearing or policy. Of the prospective cohort studies, 93% (n = 14) reported a benefit from mask wearing or policy, and of the retrospective cohort studies, 67% (n = 8) reported a benefit to mask wearing or policy. Lastly, all the quasi-experimental and RCT studies reported a benefit to mask wearing and preventing the spread of SARS-CoV-2 transmission or COVID-19 disease (n = 8). Most of the case report studies did not report sufficient information to determine whether mask wearing or policy provided any benefits or harm (82%, n = 9).

Table 3.
Vote counting method results.
3.2. Type of Mask
There was high variability in the types of masks used in the studies that were evaluated (e.g., surgical, cloth, N-95, FFP2, and KF94 respirator). Of the total 79 included studies, 82% (n = 65) assessed various combinations of types of masks (e.g., two or more types). Among these studies, 77% (n = 50) found masks to be beneficial in preventing SARS-CoV-2 transmission or COVID-19 disease, 6% (n = 4) found no benefit, and 17% (n = 11) did not report sufficient data to determine the effect (Table 3). The remaining 18% (n = 14) of studies assessed either surgical masks (n = 10), N-95s (n = 3), or FFP2s (n = 1). Of the 10 studies that assessed surgical masks, 80% (n = 8) found this type of mask to be beneficial, one found no benefit, and one did not provide sufficient data to determine the effect (Table 3). All studies assessing N-95 masks (n = 3) and the single study on FFP2 masks reported them to be beneficial in reducing SARS-CoV-2 transmission.
3.3. Settings
3.3.1. Community
A greater proportion of the studies occurred in community settings (n = 34, 43%) (Table 2). Community settings included studies conducted in neighborhood settings (n = 23), aircraft (n = 3), work offices/businesses (n = 2), nightclubs/music festivals (n = 2), sports facilities (n = 1), hair salons (n = 1), community markets (n = 1), or camps (n = 1). Among the 34 community studies, 91% (n = 31) found face masks to be beneficial in preventing SARS-CoV-2 transmission, 6% (n = 2) found no benefit, and 3% (n = 1) did not report sufficient data to determine an association. Of these studies, 28 (82%) examined various types of masks or did not specify the mask type; within this group, 25 (89%) found that mask use reduced transmission. Six studies (18%) specifically assessed surgical, N-95, FFP2, or two-layer cloth masks, and five (83%) demonstrated effectiveness in preventing transmission.
Four different outcome measures were used to assess SARS-CoV-2 infection and COVID-19 in community and neighborhood settings. Symptomatic laboratory-confirmed COVID-19 was the most common method used in 23 (68%) studies, with masks shown to be effective in 21 (91%) of them. Aggregate community transmission was assessed in seven studies (20%), in which five (71%) found masks to be protective. Two studies (6%) relied on participants’ self-reported laboratory-confirmed infection, and all reported a protective effect of mask use. Finally, SARS-CoV-2 seroconversion was evaluated in two studies (6%), with both showing benefit.
3.3.2. Healthcare
A total of 30 studies (38%) took place in a healthcare setting (Table 2). Healthcare settings included public hospitals (n = 23), healthcare networks (n = 2), dental settings (n = 1), residential aged-care facilities (i.e., nursing home) (n = 1), tertiary care medical centers (n = 1), public health centers (n = 1), and Veteran’s Affairs (VA) healthcare centers (n = 1). Among these studies, 70% (n = 21) found facemasks or mask policies to be beneficial in preventing SARS-CoV-2 transmission or COVID-19 disease, whereas one found there to be no benefit. Additionally, 27% (n = 8) of studies did not report sufficient data to determine the association between face mask wearing and COVID-19. Of these studies, 16 (53%) assessed masks that included surgical, N-95, FFP2, FFP2, disposable, and KF94 respirators, and 10 (63%) of these studies reported the masks to prevent the transmission of SARS-CoV-2. Fourteen studies examined various masks or did not specify what kinds of masks were assessed. Twelve (86%) of the various or not specified masks in a community setting helped reduce the transmission of SARS-CoV-2.
Three outcome measures were used to assess SARS-CoV-2 infection and COVID-19 in healthcare settings. The most common was symptomatic laboratory-confirmed COVID-19, reported in 26 studies (74%), with masks shown to be effective in 17 (65%) of them. Two studies (7%) relied on participants’ self-reported laboratory-confirmed infection, and all reported a protective effect of mask use. Finally, SARS-CoV-2 seroconversion was evaluated in two studies (7%), with both showing benefit.
3.3.3. Schools/Universities
Few studies took place in school settings (n = 15; 19%) (Table 2), which included K-12 schools (n = 12), classrooms (n = 1), universities (n = 1), and childcare programs (n = 1). Among these studies, 80% (n = 12) found facemasks to be beneficial in preventing SARS-CoV-2 transmission or COVID-19, 13% (n = 2) found no benefit, and 7% (n = 1) did not report sufficient data to determine an association. Of these studies, 14 (93%) examined various types of masks or did not specify the mask type; within this group, 10 (71%) found that masks reduced transmission. One study (7%) specifically assessed FFP2 masks and found that they demonstrated effectiveness in preventing transmission.
Three different outcome measures were used to assess SARS-CoV-2 and COVID-19 in school and university settings. Symptomatic laboratory-confirmed COVID-19 was used in seven (47%) studies, with masks shown to be effective in four (57%) of them. The second outcome measure was aggregate community transmission, which was used in six studies (40%), of which all found masks to be protective. Finally, two studies (13%) relied on participants’ self-reported laboratory-confirmed infection, and both reported a protective effect of mask use.
3.3.4. Mask Mandates and Policies
Thirteen studies [,,,,,,,,,,,,] specifically assessed the effectiveness of mask mandates and policies on COVID-19 outcomes (e.g., transmission rates, hospitalizations, and deaths) across statewide, county-level, and school settings. Overall, 85% (11 of 13) of studies demonstrated a beneficial effect in the prevention of COVID-19. Approximately 100 days after implementation, U.S. statewide mask mandates were reported to be associated with a 1.1% decrease in county-level COVID-19 cases []. In Kansas, counties that implemented mask mandates observed a decrease (mean decrease = 0.08 cases per 100,000 per day) in COVID-19 incidence, while those without mask mandates observed an increase (mean increase = 0.11 cases per 100,000 per day) []. Multiple studies in the U.S. and Germany found that mask mandates implemented in K-12 schools were associated with lower COVID-19 infection and transmission rates [,,,]. One observation study conducted across 61 U.S. school districts found that those with optional masking policies had a 3.6 times higher rate of secondary COVID-19 transmission []. However, one study did not find an association between the Texas Statewide Mandate (GA-29) and reductions in COVID-19 hospitalization rates or incidence []. Another study analyzed COVID-19 data across 35 European countries and found that countries that complied more with mask mandates did not have lower COVID-19 incidence rates [].
3.4. Risk of Bias Assessment and Quality of Evidence
Table 4, Table 5, Table 6, Table 7, Table 8 and Table 9 show the risk of bias assessment across all studies included. Six separate JBI checklists were used to assess bias based on study design. Risk of bias was classified as high in 3 studies (3.8%), moderate in 31 studies (39.2%), and low in 45 studies (57%). Of the 11 case reports, 55% were classified as low risk of bias, while 45% were classified as moderate risk of bias due to insufficient description of adverse events (Table 4). Most (88%) of the quasi-experimental and RCT studies were classified as moderate or high bias due to unclear allocation procedures, lack of blinding, and the inadequate description of follow-up procedures to minimize dropout (Table 5 and Table 9). Of the case–control studies, 70% were rated as low risk of bias (Table 6). Fifty-six percent of cohort studies were classified as low risk of bias, and most were reliable in the measurement of outcomes, as they were laboratory-confirmed results (Table 7). Thirteen out of twenty-three (57%) cross-sectional studies were rated as low risk of bias (Table 8).

Table 4.
JBI risk of bias quality assessment—case reports.

Table 5.
JBI risk of bias quality assessment—quasi-experimental trial.

Table 6.
JBI risk of bias quality assessment—case–control studies.

Table 7.
JBI risk of bias quality assessment—cohort studies.

Table 8.
JBI risk of bias quality assessment—cross-sectional studies.

Table 9.
JBI risk of bias quality assessment—randomized controlled trial.
Table 10 summarizes the quality of evidence for four types of COVID-19 outcomes: (1) symptomatic laboratory-confirmed COVID-19, (2) self-reported laboratory-confirmed COVID-19, (3) SARS-CoV-2 seroconversion, and (4) aggregate community-level incidence (rt-qPCR). For all outcomes, the level of certainty for the evidence was low due to a high number of non-randomized studies and the number of studies with moderate to high risk of bias.

Table 10.
Summary of findings—face masks and masking policies for preventing SARS-CoV-2 transmission and COVID-19 disease.
4. Discussion
Results of this systematic review demonstrate consistent evidence (77% of all studies), supporting that wearing a facemask and masking policies are effective at prevention and reducing the risk of SARS-CoV-2 transmission or COVID-19 disease across various real-world settings. Mask wearing was reported to reduce SARS-CoV-2 transmission across multiple community spaces (e.g., markets, workplaces, and salons), healthcare environments, and schools. These findings provide evidence that masking is an important and practical strategy to reduce transmission outside of controlled laboratory conditions. The results of this review are consistent with previous systematic reviews and meta-analyses [,,,]. One previous meta-analysis demonstrated a pooled relative risk of 0.12 (i.e., risk reduction of 88%), and another study reported an odds ratio of 0.38 for risk of SARS-CoV-2 infection when masking policies were in place [,]. Another review conducted only in cohort and case–control studies found that wearing a cloth mask decreased the odds of COVID-19 regardless of mask type []. The results of the present systematic review builds on these previous studies [] and provides additional evidence for the benefits of face masks and masking policies to reduce SARS-CoV-2 transmission and COVID-19 disease specifically in real-world settings. This is particularly important given that the public’s adherence to wearing masks and the enforcement of mask wearing can vary widely, which would lower the expected effect of the policy. Yet, the results from this review show that 85% (11 of 13) of studies that focused on mask policies demonstrated a beneficial effect in preventing SARS-CoV-2 and COVID-19 disease. Thus, these findings support the external validity and generalizability of previous laboratory-based studies for the benefits of mask wearing to prevent SARS-CoV-2 infection and COVID-19 []. These results can be used to develop and support future public health messaging campaigns to address respiratory disease outbreaks, epidemics, and pandemics. Public health messaging that emphasizes positive framing for mask wearing such as promoting community togetherness and community unity resonate better with the general public compared to messages focused on fear or policies that may be perceived as overly intrusive [].
This systematic review included studies of various designs, types of masks, and community settings to evaluate the evidence of effectiveness of mask wearing and masking policies. The proportion of studies demonstrating a benefit for mask wearing did not vary greatly by study design (67–100%), type of mask (77–100%), or setting (80–91%), while 85% of masking policies specifically reported a benefit. This level of consistent and protective effects of mask wearing and masking policies across study characteristics provides strong empirical evidence for the real-world effectiveness of masking recommendations to reduce the spread of SARS-CoV-2 and COVID-19 disease outside controlled settings. Importantly, the risk of bias ratings were classified as low for 57% of included studies. This suggests that the evidence from this systematic review can be interpreted as mostly reliable with moderate to high validity.
It is important to note that not all studies demonstrate a clear benefit of wearing face masks for the prevention of SARS-CoV-2 infection in community settings. In this systematic literature review, five studies (6%) did not demonstrate a clear protective effect. There are several potential explanations for these results. Sasser et al. [] found no statistically significant association between COVID-19 incidence and face mask use among high school sports participants. This may be partially explained by a relatively low COVID-19 community prevalence during the time of the study. Likewise, April et al. [] did not find that a mask mandate reduced SARS-CoV-2 transmission. It is also possible that mobility-restricting policies (i.e., stay-at-home orders) may have had a larger effect on reducing transmission than wearing masks in community settings. In these studies, data on self-reported mask wearing were not available, which may have limited the ability to evaluate the true effect of masking compared to other mitigation measures. Key study limitations included missing data and variable adherence to mask wearing, which can reduce the ability to detect an intervention effect. Notably, a previous Cochrane review concluded that N95 masks had little impact on the prevention of viral respiratory illness []. However, the studies included in the review demonstrated high variability in methodology and data quality, which can increase the risk of bias towards null findings []. These factors limit the ability to produce reliable estimates of effectiveness in community contexts. In summary, key methodological limitations among studies with null results may partially explain the non-significant findings for the effectiveness of mask wearing on the prevention of SARS-CoV-2 transmission and COVID-19 in community settings. Future research should address these methodological limitations to provide more accurate and reliable estimates of effectiveness.
Strengths and Limitations
This review followed a rigorous and systematic approach using PRISMA guidelines to identify and evaluate relevant studies. Two independent reviewers followed a strict protocol for assessing inclusion/exclusion criteria and subsequently abstracting study data. The Rayyan study management platform and the JBI risk of bias appraisal tools provided standardized methods to manage and evaluate studies. However, a meta-analysis was not conducted due to the high heterogeneity of settings, types of masks, study designs, statistical methods, and outcome measures used (e.g., infection, symptomology) across studies. Meta-analyses are not recommended when there is this level of heterogeneity. Instead, the vote counting method is recommended as an alternative to meta-analysis, which allows for the identification of patterns (direction of results) across different studies. Several studies included in this review lacked information on the community’s adherence to wearing face masks, the specific the type of masks used, and there were inconsistencies in the type of incidence measure (SARS-CoV-2 vs. COVID-19 disease). These limitations make it difficult to more precisely evaluate the effectiveness of masking policies and mask wearing. Furthermore, only three randomized controlled study trials were identified. Although randomized controlled studies can provide stronger evidence of effectiveness and external validity, these study designs can also raise ethical concerns in the context of a new and deadly respiratory disease, such as COVID-19, where randomizing people or communities to not wear face masks may be considered unethical. Lastly, studies written or translated to a language other than English were not included. This may potentially bias results if the excluded studies reported different or contrary results to those studies that were included in this review.
5. Conclusions
Evidence from this systematic literature review supports that masking policies and mask wearing are beneficial to prevent and reduce the risk of SARS-CoV-2 infections and COVID-19 disease in various real-world settings. Importantly, relative to other recommendations (such as limiting travel, limiting group gatherings), wearing a face mask remains one of the most feasible, accessible, and effective non-pharmacologic public health interventions to prevent the spread of SARS-CoV-2. Given the varying adherence to masking from the public, there is a need to improve public health messaging to address misinformation and barriers to wearing masks. Reducing barriers to wearing masks can include providing high quality masks to those who otherwise do not have access to them or would not actively seek to obtain one on their own and by creating positive and supportive social environments that support mask wearing (i.e., depoliticizing and de-stigmatizing mask use).
Author Contributions
N.C.C. conceptualized the current study and made substantial contributions to data acquisition, writing, and revision of the work. S.S. assisted with acquisition of data, risk of bias assessment, and revision of paper drafts. K.K. assisted with acquisition of data, risk of bias assessment, and revision of paper drafts. J.M.F. led the acquisition of data, interpretation, and drafting of the manuscript. P.D. assisted with acquisition of data, risk of bias assessment, and revision of paper drafts. E.T.H. and C.M.-D. interpreted study findings and contributed to revisions of paper drafts. J.G.G., C.B.R. and J.P.E. all interpreted study findings and substantively revised initial and final drafts of the paper. All authors have read and agreed to the published version of the manuscript.
Funding
Dr. Crespo received support from Family Health Centers of San Diego’s Scientist in Residence Program sponsored by The Conrad Prebys Foundation. Administrative and (or) IT support was provided by the SDSU HealthLINK Endowment (S21 MD010690).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data from the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Scheid, J.L.; Lupien, S.P.; Ford, G.S.; West, S.L. Commentary: Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6655. [Google Scholar] [CrossRef]
- Piroth, L.; Cottenet, J.; Mariet, A.-S.; Bonniaud, P.; Blot, M.; Tubert-Bitter, P.; Quantin, C. Comparison of the Characteristics, Morbidity, and Mortality of COVID-19 and Seasonal Influenza: A Nationwide, Population-Based Retrospective Cohort Study. Lancet Respir. Med. 2021, 9, 251–259. [Google Scholar] [CrossRef]
- World Health Organization COVID-19 Cases|WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 9 October 2025).
- CDC How to Protect Yourself and Others. Available online: https://www.cdc.gov/covid/prevention/index.html (accessed on 9 October 2025).
- Qualls, N.; Levitt, A.; Kanade, N.; Wright-Jegede, N.; Dopson, S.; Biggerstaff, M.; Reed, C.; Uzicanin, A. CDC Community Mitigation Guidelines Work Group Community Mitigation Guidelines to Prevent Pandemic Influenza—United States, 2017. MMWR Recomm. Rep. 2017, 66, 1–34. [Google Scholar] [CrossRef]
- Locke, L.; Dada, O.; Shedd, J.S. Aerosol Transmission of Infectious Disease and the Efficacy of Personal Protective Equipment (PPE): A Systematic Review. J. Occup. Environ. Med. 2021, 63, e783–e791. [Google Scholar] [CrossRef]
- Mele, J.; Rosenstrom, E.; Ivy, J.; Mayorga, M.; Patel, M.D.; Swann, J. Mask Interventions in K12 Schools Can Also Reduce Community Transmission in Fall 2021. medRxiv 2021, 2021.09.11.21263433. [Google Scholar] [CrossRef]
- Ramesh, S.; Govindarajulu, M.; Parise, R.S.; Neel, L.; Shankar, T.; Patel, S.; Lowery, P.; Smith, F.; Dhanasekaran, M.; Moore, T. Emerging SARS-CoV-2 Variants: A Review of Its Mutations, Its Implications and Vaccine Efficacy. Vaccines 2021, 9, 1195. [Google Scholar] [CrossRef]
- Lyu, W.; Wehby, G.L. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US. Health Aff. (Millwood) 2020, 39, 1419–1425. [Google Scholar] [CrossRef]
- He, L.; He, C.; Reynolds, T.L.; Bai, Q.; Huang, Y.; Li, C.; Zheng, K.; Chen, Y. Why Do People Oppose Mask Wearing? A Comprehensive Analysis of U.S. Tweets during the COVID-19 Pandemic. J. Am. Med. Inf. Assoc. 2021, 28, 1564–1573. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An Evidence Review of Face Masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- Asadi, S.; Cappa, C.D.; Barreda, S.; Wexler, A.S.; Bouvier, N.M.; Ristenpart, W.D. Efficacy of Masks and Face Coverings in Controlling Outward Aerosol Particle Emission from Expiratory Activities. Sci. Rep. 2020, 10, 15665. [Google Scholar] [CrossRef] [PubMed]
- Ueki, H.; Furusawa, Y.; Iwatsuki-Horimoto, K.; Imai, M.; Kabata, H.; Nishimura, H.; Kawaoka, Y. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere 2020, 5, e00637-20. [Google Scholar] [CrossRef]
- Chen, C.; Zhou, W.; Qi, J.; Chen, M.; Yuan, Z.; Miao, J.; Yang, M.; Chen, J.; Shen, F.; Cao, K.; et al. Adherence to Mask-Wearing and Its Impact on the Incidence and Deaths of Viral Respiratory Infectious Diseases: A Systematic Review, Meta-Analysis and Modelling Study. BMJ Glob. Health 2025, 10, e017087. [Google Scholar] [CrossRef]
- Leech, G.; Rogers-Smith, C.; Monrad, J.T.; Sandbrink, J.B.; Snodin, B.; Zinkov, R.; Rader, B.; Brownstein, J.S.; Gal, Y.; Bhatt, S.; et al. Mask Wearing in Community Settings Reduces SARS-CoV-2 Transmission. Proc. Natl. Acad. Sci. USA 2022, 119, e2119266119. [Google Scholar] [CrossRef]
- Bundgaard, H.; Bundgaard, J.S.; Raaschou-Pedersen, D.E.T.; von Buchwald, C.; Todsen, T.; Norsk, J.B.; Pries-Heje, M.M.; Vissing, C.R.; Nielsen, P.B.; Winsløw, U.C.; et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Controlled Trial. Ann. Intern. Med. 2021, 174, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Coclite, D.; Napoletano, A.; Gianola, S.; Del Monaco, A.; D’Angelo, D.; Fauci, A.; Iacorossi, L.; Latina, R.; Torre, G.L.; Mastroianni, C.M.; et al. Face Mask Use in the Community for Reducing the Spread of COVID-19: A Systematic Review. Front. Med. (Lausanne) 2020, 7, 594269. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Aromataris, E.; Stern, C.; Lockwood, C.; Barker, T.H.; Klugar, M.; Jadotte, Y.; Evans, C.; Ross-White, A.; Lizarondo, L.; Stephenson, M.; et al. JBI Series Paper 2: Tailored Evidence Synthesis Approaches Are Required to Answer Diverse Questions: A Pragmatic Evidence Synthesis Toolkit from JBI. J. Clin. Epidemiol. 2022, 150, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological Quality (Risk of Bias) Assessment Tools for Primary and Secondary Medical Studies: What Are They and Which Is Better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- McKenzie, J.E.; Brennan, S.E. Synthesizing and Presenting Findings Using Other Methods. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019; pp. 321–347. [Google Scholar]
- Adawee, M.O.; Brum, R.E.; Ellsworth, L.J. Examining Common Characteristics Among Healthcare Personnel Positive for COVID-19 and the Effectiveness of Healthcare Personnel Mask Use in Preventing COVID-19 in a Large Health System in Central Michigan. J. Occup. Environ. Med. 2021, 63, 226–229. [Google Scholar] [CrossRef]
- Andrejko, K.L.; Pry, J.M.; Myers, J.F.; Fukui, N.; DeGuzman, J.L.; Openshaw, J.; Watt, J.P.; Lewnard, J.A.; Jain, S. California COVID-19 Case-Control Study Team Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection—California, February-December 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 212–216. [Google Scholar] [CrossRef]
- Andrejko, K.L.; Pry, J.; Myers, J.F.; Openshaw, J.; Watt, J.; Birkett, N.; DeGuzman, J.L.; Barbaduomo, C.M.; Dong, Z.N.; Fang, A.T.; et al. Predictors of Severe Acute Respiratory Syndrome Coronavirus 2 Infection Following High-Risk Exposure. Clin. Infect. Dis. 2021, 75, e276–e288. [Google Scholar] [CrossRef]
- April, M.D.; Naylor, J.F.; Long, B. Analysis of the Effects of a Texas State-Wide Mask Mandate (Executive Order GA-29) on Case Load, Hospitalizations, and Mortality. South. Med. J. 2022, 115, 175–180. [Google Scholar] [CrossRef]
- Badri, S.; Sardá, V.; Moncada, J.S.; Merçon, M.; Rezai, K.; Weinstein, R.A.; Trick, W.E. Disparities and Temporal Trends in COVID-19 Exposures and Mitigating Behaviors Among Black and Hispanic Adults in an Urban Setting. JAMA Netw. Open 2021, 4, e2125187. [Google Scholar] [CrossRef]
- Baker, J.M.; Nakayama, J.Y.; O’Hegarty, M.; McGowan, A.; Teran, R.A.; Bart, S.M.; Mosack, K.; Roberts, N.; Campos, B.; Paegle, A.; et al. SARS-CoV-2 B.1.1.529 (Omicron) Variant Transmission Within Households—Four U.S. Jurisdictions, November 2021-February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 341–346. [Google Scholar] [CrossRef]
- Boutzoukas, A.E.; Zimmerman, K.O.; Inkelas, M.; Brookhart, M.A.; Benjamin, D.K.; Butteris, S.; Koval, S.; DeMuri, G.P.; Manuel, V.G.; Smith, M.J.; et al. School Masking Policies and Secondary SARS-CoV-2 Transmission. Pediatrics 2022, 149, e2022056687. [Google Scholar] [CrossRef]
- Bruckhaus, A.; Martinez, A.; Garner, R.; La Rocca, M.; Duncan, D. Post-Lockdown Infection Rates of COVID-19 Following the Reopening of Public Businesses. J. Public Health 2022, 44, e51–e58. [Google Scholar] [CrossRef] [PubMed]
- Budzyn, S.E.; Panaggio, M.J.; Parks, S.E.; Papazian, M.; Magid, J.; Eng, M.; Barrios, L.C. Pediatric COVID-19 Cases in Counties with and Without School Mask Requirements—United States, 1 July–4 September 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1377–1378. [Google Scholar] [CrossRef] [PubMed]
- Donovan, C.V. SARS-CoV-2 Incidence in K–12 School Districts with Mask-Required Versus Mask-Optional Policies—Arkansas, August–October 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.B.; Adrien, N.; Silguero, J.J.; Hopper, J.J.; Chowdhury, A.I.; Werler, M.M. Mask Adherence and Rate of COVID-19 across the United States. PLoS ONE 2021, 16, e0249891. [Google Scholar] [CrossRef]
- Gettings, J.; Czarnik, M.; Morris, E.; Haller, E.; Thompson-Paul, A.M.; Rasberry, C.; Lanzieri, T.M.; Smith-Grant, J.; Aholou, T.M.; Thomas, E.; et al. Mask Use and Ventilation Improvements to Reduce COVID-19 Incidence in Elementary Schools—Georgia, 16 November–11 December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 779–784. [Google Scholar] [CrossRef]
- Guy, G.P.; Lee, F.C.; Sunshine, G.; McCord, R.; Howard-Williams, M.; Kompaniyets, L.; Dunphy, C.; Gakh, M.; Weber, R.; Sauber-Schatz, E.; et al. Association of State-Issued Mask Mandates and Allowing On-Premises Restaurant Dining with County-Level COVID-19 Case and Death Growth Rates—United States, 1 March–31 December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 350–354. [Google Scholar] [CrossRef]
- Hast, M.; Swanson, M.; Scott, C.; Oraka, E.; Espinosa, C.; Burnett, E.; Kukielka, E.A.; Rice, M.E.; Mehari, L.; McCloud, J.; et al. Prevalence of Risk Behaviors and Correlates of SARS-CoV-2 Positivity among in-School Contacts of Confirmed Cases in a Georgia School District in the Pre-Vaccine Era, December 2020–January 2021. BMC Public Health 2022, 22, 101. [Google Scholar] [CrossRef]
- Hendrix, M.J.; Walde, C.; Findley, K.; Trotman, R. Absence of Apparent Transmission of SARS-CoV-2 from Two Stylists After Exposure at a Hair Salon with a Universal Face Covering Policy—Springfield, Missouri, May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 930–932. [Google Scholar] [CrossRef]
- Jehn, M.; McCullough, J.M.; Dale, A.P.; Gue, M.; Eller, B.; Cullen, T.; Scott, S.E. Association Between K-12 School Mask Policies and School-Associated COVID-19 Outbreaks—Maricopa and Pima Counties, Arizona, July–August 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1372–1373. [Google Scholar] [CrossRef] [PubMed]
- Klompas, M.; Baker, M.A.; Griesbach, D.; Tucker, R.; Gallagher, G.R.; Lang, A.S.; Fink, T.; Cumming, M.; Smole, S.; Madoff, L.C.; et al. Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From Asymptomatic and Presymptomatic Individuals in Healthcare Settings Despite Medical Masks and Eye Protection. Clin. Infect. Dis. 2021, 73, 1693–1695. [Google Scholar] [CrossRef]
- Liu, P.Y.; Gragnani, C.M.; Timmerman, J.; Newhouse, C.N.; Soto, G.; Lopez, L.; Spronz, R.; Mhaskar, A.; Yeganeh, N.; Fernandes, P.; et al. Pediatric Household Transmission of Severe Acute Respiratory Coronavirus-2 Infection-Los Angeles County, December 2020 to February 2021. Pediatr Infect. Dis. J. 2021, 40, e379–e381. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, G.S.; Mann, T.K.; Boutzoukas, A.E.; Blakemore, A.; Brookhart, M.A.; Edwards, L.; Jackman, J.G.; Panayotti, G.M.M.; Warren, T.; Pendleton, J.; et al. Masking Adherence in K-12 Schools and SARS-CoV-2 Secondary Transmission. Pediatrics 2022, 149, e2021054268l. [Google Scholar] [CrossRef] [PubMed]
- Murray, T.S.; Malik, A.A.; Shafiq, M.; Lee, A.; Harris, C.; Klotz, M.; Humphries, J.E.; Patel, K.M.; Wilkinson, D.; Yildirim, I.; et al. Association of Child Masking with COVID-19-Related Closures in US Childcare Programs. JAMA Netw. Open 2022, 5, e2141227. [Google Scholar] [CrossRef]
- Rebeiro, P.F.; Aronoff, D.M.; Smith, M.K. The Impact of State Mask-Wearing Requirements on the Growth of Coronavirus Disease 2019 Cases, Hospitalizations, and Deaths in the United States. Clin. Infect. Dis. 2021, 73, 1703–1706. [Google Scholar] [CrossRef]
- Rebmann, T.; Loux, T.M.; Arnold, L.D.; Charney, R.; Horton, D.; Gomel, A. SARS-CoV-2 Transmission to Masked and Unmasked Close Contacts of University Students with COVID-19—St. Louis, Missouri, January–May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1245–1248. [Google Scholar] [CrossRef]
- Riley, J.; Huntley, J.M.; Miller, J.A.; Slaichert, A.L.B.; Brown, G.D. Mask Effectiveness for Preventing Secondary Cases of COVID-19, Johnson County, Iowa, USA. Emerg. Infect. Dis. 2022, 28, 69–75. [Google Scholar] [CrossRef]
- Sarti, D.; Campanelli, T.; Rondina, T.; Gasperini, B. COVID-19 in Workplaces: Secondary Transmission. Ann. Work. Expo. Health 2021, 65, 1145–1151. [Google Scholar] [CrossRef]
- Sasser, P.; McGuine, T.A.; Haraldsdottir, K.; Biese, K.M.; Goodavish, L.; Stevens, B.; Watson, A.M. Reported COVID-19 Incidence in Wisconsin High School Athletes in Fall 2020. J. Athl. Train. 2022, 57, 59–64. [Google Scholar] [CrossRef]
- Seidelman, J.L.; Lewis, S.S.; Advani, S.D.; Akinboyo, I.C.; Epling, C.; Case, M.; Said, K.; Yancey, W.; Stiegel, M.; Schwartz, A.; et al. Universal Masking Is an Effective Strategy to Flatten the Severe Acute Respiratory Coronavirus Virus 2 (SARS-CoV-2) Healthcare Worker Epidemiologic Curve. Infect. Control Hosp. Epidemiol. 2020, 41, 1466–1467. [Google Scholar] [CrossRef] [PubMed]
- Shah, V.P.; Breeher, L.E.; Hainy, C.M.; Swift, M.D. Evaluation of Healthcare Personnel Exposures to Patients with Severe Acute Respiratory Coronavirus Virus 2 (SARS-CoV-2) Associated with Personal Protective Equipment. Infect. Control Hosp. Epidemiol. 2022, 43, 770–774. [Google Scholar] [CrossRef]
- Shah, M.; Shah, M.; Hollingsworth, J.W. Relation of Masking Policy to COVID-19 Positivity Rate in Texas School Districts. Bayl. Univ. Med. Cent. Proc. 2022, 35, 466–467. [Google Scholar] [CrossRef] [PubMed]
- Suh, H.H.; Meehan, J.; Blaisdell, L.; Browne, L. Non-Pharmaceutical Interventions and COVID-19 Cases in US Summer Camps: Results from an American Camp Association Survey. J. Epidemiol. Community Health 2022, 76, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, P.V.; Zimmerman, K.O.; Benjamin, D.K.; Kalu, I.C. SARS-CoV-2 Infections and Incidence at a North Carolina Pre-Kindergarten-12 School During In-Person Education: August 2020 to January 2021. J. Sch. Health 2022, 92, 461–468. [Google Scholar] [CrossRef]
- Thompson, E.R.; Williams, F.S.; Giacin, P.A.; Drummond, S.; Brown, E.; Nalick, M.; Wang, Q.; McDonald, J.R.; Carlson, A.L. Universal Masking to Control Healthcare-Associated Transmission of Severe Acute Respiratory Coronavirus Virus 2 (SARS-CoV-2). Infect. Control Hosp. Epidemiol. 2022, 43, 344–350. [Google Scholar] [CrossRef]
- Tjaden, A.H.; Edelstein, S.L.; Ahmed, N.; Calamari, L.; Dantuluri, K.L.; Gibbs, M.; Hinkelman, A.; Mongraw-Chaffin, M.; Sanders, J.W.; Saydah, S.; et al. Association between COVID-19 and Consistent Mask Wearing during Contact with Others Outside the Household-A Nested Case-Control Analysis, November 2020-October 2021. Influenza Other Respir Viruses 2023, 17, e13080. [Google Scholar] [CrossRef]
- Tjaden, A.H.; Gibbs, M.; Runyon, M.; Weintraub, W.S.; Taylor, Y.J.; Edelstein, S.L. COVID-19 Community Research Partnership Study Group Association between Self-Reported Masking Behavior and SARS-CoV-2 Infection Wanes from Pre-Delta to Omicron-Predominant Periods-North Carolina COVID-19 Community Research Partnership (NC-CCRP). Am. J. Infect. Control 2023, 51, 261–267. [Google Scholar] [CrossRef]
- Van Dyke, M.E.; Rogers, T.M.; Pevzner, E.; Satterwhite, C.L.; Shah, H.B.; Beckman, W.J.; Ahmed, F.; Hunt, D.C.; Rule, J. Trends in County-Level COVID-19 Incidence in Counties with and Without a Mask Mandate—Kansas, 1 June–23 August 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1777–1781. [Google Scholar] [CrossRef]
- Walker, J.; Fleece, M.E.; Griffin, R.L.; Leal, S.M.; Alsip, J.A.; Stigler, W.S.; Nafziger, S.D.; Marrazzo, J.M.; Lee, R.A. Decreasing High-Risk Exposures for Healthcare Workers Through Universal Masking and Universal Severe Acute Respiratory Syndrome Coronavirus 2 Testing on Entry to a Tertiary Care Facility. Clin. Infect. Dis. 2021, 73, e3113–e3115. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ferro, E.G.; Zhou, G.; Hashimoto, D.; Bhatt, D.L. Association Between Universal Masking in a Health Care System and SARS-CoV-2 Positivity Among Health Care Workers. JAMA 2020, 324, 703–704. [Google Scholar] [CrossRef]
- Williams, V.R.; Maze Dit Mieusement, L.; Tomiczek, N.; Chan, A.K.; Salt, N.; Leis, J.A. Risk of SARS-CoV-2 Transmission from Universally Masked Healthcare Workers to Patients or Residents: A Prospective Cohort Study. Am. J. Infect. Control 2021, 49, 1429–1431. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Tong, X.; Wang, J.; Huang, W.; Yin, S.; Huang, R.; Yang, H.; Chen, Y.; Huang, A.; Liu, Y.; et al. High SARS-CoV-2 Antibody Prevalence among Healthcare Workers Exposed to COVID-19 Patients. J. Infect. 2020, 81, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.-C.; Wong, S.-C.; Chuang, V.W.-M.; So, S.Y.-C.; Chen, J.H.-K.; Sridhar, S.; To, K.K.-W.; Chan, J.F.-W.; Hung, I.F.-N.; Ho, P.-L.; et al. The Role of Community-Wide Wearing of Face Mask for Control of Coronavirus Disease 2019 (COVID-19) Epidemic Due to SARS-CoV-2. J. Infect. 2020, 81, 107–114. [Google Scholar] [CrossRef]
- Guo, X.; Wang, J.; Hu, D.; Wu, L.; Gu, L.; Wang, Y.; Zhao, J.; Zeng, L.; Zhang, J.; Wu, Y. Survey of COVID-19 Disease Among Orthopaedic Surgeons in Wuhan, People’s Republic of China. J. Bone Jt. Surg. Am. 2020, 102, 847–854. [Google Scholar] [CrossRef]
- Hong, L.-X.; Lin, A.; He, Z.-B.; Zhao, H.-H.; Zhang, J.-G.; Zhang, C.; Ying, L.-J.; Ge, Z.-M.; Zhang, X.; Han, Q.-Y.; et al. Mask Wearing in Pre-Symptomatic Patients Prevents SARS-CoV-2 Transmission: An Epidemiological Analysis. Travel. Med. Infect. Dis. 2020, 36, 101803. [Google Scholar] [CrossRef]
- Lio, C.F.; Cheong, H.H.; Lei, C.I.; Lo, I.L.; Yao, L.; Lam, C.; Leong, I.H. Effectiveness of Personal Protective Health Behaviour against COVID-19. BMC Public Health 2021, 21, 827. [Google Scholar] [CrossRef]
- Martín-Sánchez, M.; Lim, W.W.; Yeung, A.; Adam, D.C.; Ali, S.T.; Lau, E.H.Y.; Wu, P.; Yuen, K.-Y.; Leung, G.M.; Cowling, B.J. COVID-19 Transmission in Hong Kong despite Universal Masking. J. Infect. 2021, 83, 92–95. [Google Scholar] [CrossRef]
- Pan, Z.; Zhang, H.; Yang, J.; Tang, S.; Cheng, Z.; Wu, K.; Liu, B. Surgical Masks for Protection of Health Care Personnel Against COVID-19: Results from an Observational Study. Clin. Investig. Med. 2021, 44, E48–E54. [Google Scholar] [CrossRef]
- Wang, Y.; Tian, H.; Zhang, L.; Zhang, M.; Guo, D.; Wu, W.; Zhang, X.; Kan, G.L.; Jia, L.; Huo, D.; et al. Reduction of Secondary Transmission of SARS-CoV-2 in Households by Face Mask Use, Disinfection and Social Distancing: A Cohort Study in Beijing, China. BMJ Glob. Health 2020, 5, e002794. [Google Scholar] [CrossRef] [PubMed]
- Ambrosch, A.; Rockmann, F.; Klawonn, F.; Lampl, B. Effect of a Strict Hygiene Bundle for the Prevention of Nosocomial Transmission of SARS-CoV-2 in the Hospital: A Practical Approach from the Field. J. Infect. Public Health 2020, 13, 1862–1867. [Google Scholar] [CrossRef]
- Baumkötter, R.; Yilmaz, S.; Zahn, D.; Fenzl, K.; Prochaska, J.H.; Rossmann, H.; Schmidtmann, I.; Schuster, A.K.; Beutel, M.E.; Lackner, K.J.; et al. Protective Behavior and SARS-CoV-2 Infection Risk in the Population—Results from the Gutenberg COVID-19 Study. BMC Public Health 2022, 22, 1993. [Google Scholar] [CrossRef] [PubMed]
- Brandt, M.P.; Jäger, W.; Epple, S.; Haferkamp, A.; Schröder, A. SARS-CoV-2 Outbreak in Medical Employees in a Large Urologic Department: Spread, Containment and Outcome. Am. J. Infect. Control 2021, 49, 674–677. [Google Scholar] [CrossRef]
- Heinsohn, T.; Lange, B.; Vanella, P.; Rodiah, I.; Glöckner, S.; Joachim, A.; Becker, D.; Brändle, T.; Dhein, S.; Ehehalt, S.; et al. Infection and Transmission Risks of COVID-19 in Schools and Their Contribution to Population Infections in Germany: A Retrospective Observational Study Using Nationwide and Regional Health and Education Agency Notification Data. PLoS Med. 2022, 19, e1003913. [Google Scholar] [CrossRef]
- Pauser, J.; Schwarz, C.; Morgan, J.; Jantsch, J.; Brem, M. SARS-CoV-2 Transmission during an Indoor Professional Sporting Event. Sci. Rep. 2021, 11, 20723. [Google Scholar] [CrossRef]
- Wendt, R.; Nagel, S.; Nickel, O.; Wolf, J.; Kalbitz, S.; Kaiser, T.; Borte, S.; Lübbert, C. Comprehensive Investigation of an In-Hospital Transmission Cluster of a Symptomatic SARS-CoV-2-Positive Physician among Patients and Healthcare Workers in Germany. Infect. Control Hosp. Epidemiol. 2020, 41, 1209–1211. [Google Scholar] [CrossRef] [PubMed]
- Chano, T.; Morita, S.-Y.; Suzuki, T.; Yamashita, T.; Fujimura, H.; Yuri, T.; Menju, M.; Tanaka, M.; Kakuno, F. Serology Suggests Adequate Safety Measures to Protect Healthcare Workers from COVID-19 in Shiga Prefecture, Japan. PLoS ONE 2022, 17, e0270334. [Google Scholar] [CrossRef] [PubMed]
- Sugimura, M.; Chimed-Ochir, O.; Yumiya, Y.; Ohge, H.; Shime, N.; Sakaguchi, T.; Tanaka, J.; Takafuta, T.; Mimori, M.; Kuwabara, M.; et al. The Association between Wearing a Mask and COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 9131. [Google Scholar] [CrossRef]
- Toyokawa, T.; Shimada, T.; Hayamizu, T.; Sekizuka, T.; Zukeyama, Y.; Yasuda, M.; Nakamura, Y.; Okano, S.; Kudaka, J.; Kakita, T.; et al. Transmission of SARS-CoV-2 during a 2-h Domestic Flight to Okinawa, Japan, March 2020. Influenza Other Respir Viruses 2022, 16, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Gras-Valentí, P.; Mora-Muriel, J.G.; Chico-Sánchez, P.; Algado-Sellés, N.; Soler-Molina, V.M.; Hernández-Maldonado, M.; Lameiras-Azevedo, A.S.; Jiménez Sepúlveda, N.J.; Gómez Sotero, I.L.; Villanueva-Ruiz, C.O.; et al. Effectivity of a Program for the Control and Prevention of COVID-19 Healthcare-Associated Infections in a Spanish Academic Hospital. J. Patient Saf. 2021, 17, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Suñer, C.; Coma, E.; Ouchi, D.; Hermosilla, E.; Baro, B.; Rodríguez-Arias, M.À.; Puig, J.; Clotet, B.; Medina, M.; Mitjà, O. Association between Two Mass-Gathering Outdoor Events and Incidence of SARS-CoV-2 Infections during the Fifth Wave of COVID-19 in North-East Spain: A Population-Based Control-Matched Analysis. Lancet Reg. Health Eur. 2022, 15, 100337. [Google Scholar] [CrossRef]
- Abaluck, J.; Kwong, L.H.; Styczynski, A.; Haque, A.; Kabir, M.A.; Bates-Jefferys, E.; Crawford, E.; Benjamin-Chung, J.; Raihan, S.; Rahman, S.; et al. Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh. Science 2022, 375, eabi9069. [Google Scholar] [CrossRef]
- Sertcelik, A.; Cakir, B.; Metan, G. Evaluation of Risk Factors for Developing COVID-19 in Healthcare Professionals Working at Two University Hospitals in Turkey. Work 2023, 74, 799–809. [Google Scholar] [CrossRef]
- Collatuzzo, G.; Mansour, I.; Ciocan, C.; Ditano, G.; Godono, A.; Rossello, P.; Coggiola, M.; Pira, E.; Boffetta, P. Working Group On Sars-Cov-Prevention, null Effectiveness of Prevention of SARS-CoV-2 Transmission among Unvaccinated Italian Healthcare Workers. Med. Lav. 2022, 113, e2022050. [Google Scholar] [CrossRef] [PubMed]
- Coma, E.; Català, M.; Méndez-Boo, L.; Alonso, S.; Hermosilla, E.; Alvarez-Lacalle, E.; Pino, D.; Medina, M.; Asso, L.; Gatell, A.; et al. Unravelling the Role of the Mandatory Use of Face Covering Masks for the Control of SARS-CoV-2 in Schools: A Quasi-Experimental Study Nested in a Population-Based Cohort in Catalonia (Spain). Arch. Dis. Child. 2023, 108, 131–136. [Google Scholar] [CrossRef]
- Dörr, T.; Haller, S.; Müller, M.F.; Friedl, A.; Vuichard, D.; Kahlert, C.R.; Kohler, P. Risk of SARS-CoV-2 Acquisition in Health Care Workers According to Cumulative Patient Exposure and Preferred Mask Type. JAMA Netw. Open 2022, 5, e2226816. [Google Scholar] [CrossRef]
- Doung-Ngern, P.; Suphanchaimat, R.; Panjangampatthana, A.; Janekrongtham, C.; Ruampoom, D.; Daochaeng, N.; Eungkanit, N.; Pisitpayat, N.; Srisong, N.; Yasopa, O.; et al. Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. Emerg. Infect. Dis. 2020, 26, 2607–2616. [Google Scholar] [CrossRef]
- Jarnig, G.; Kerbl, R.; van Poppel, M.N.M. Effects of Wearing FFP2 Masks on SARS-CoV-2 Infection Rates in Classrooms. Int. J. Environ. Res. Public Health 2022, 19, 13511. [Google Scholar] [CrossRef]
- Kim, D.; Ko, J.-H.; Peck, K.R.; Baek, J.Y.; Moon, H.-W.; Ki, H.K.; Yoon, J.H.; Kim, H.J.; Choi, J.H.; Park, G.E. A COVID-19 Exposure at a Dental Clinic Where Healthcare Workers Routinely Use Particulate Filtering Respirators. Int. J. Environ. Res. Public Health 2021, 18, 6481. [Google Scholar] [CrossRef]
- Malik, T. COVID-19 and the Efficacy of Different Types of Respiratory Protective Equipment Used by Health Care Providers in a Health Care Setting. Cureus 2020, 12, e7621. [Google Scholar] [CrossRef]
- Meylan, S.; Dafni, U.; Lamoth, F.; Tsourti, Z.; Lobritz, M.A.; Regina, J.; Bressin, P.; Senn, L.; Grandbastien, B.; Andre, C.; et al. SARS-CoV-2 Seroprevalence in Healthcare Workers of a Swiss Tertiary Care Centre at the End of the First Wave: A Cross-Sectional Study. BMJ Open 2021, 11, e049232. [Google Scholar] [CrossRef]
- Nir-Paz, R.; Grotto, I.; Strolov, I.; Salmon, A.; Mandelboim, M.; Mendelson, E.; Regev-Yochay, G. Absence of In-Flight Transmission of SARS-CoV-2 Likely Due to Use of Face Masks on Board. J. Travel. Med. 2020, 27, taaa117. [Google Scholar] [CrossRef]
- Ranjan, P.; Bhattacharya, A.; Chakrawarty, A.; Das, R.; Kumar, A.; Pandey, S.; Chowdhury, S.; Mittal, A.; Baitha, U.; Wig, N. Association Between Self-Reported Adherence to Preventive Practices and Probability of Turning COVID-19 Positive: A Cross-Sectional Analytical Study. Cureus 2020, 12, e11815. [Google Scholar] [CrossRef]
- Reyné, B.; Selinger, C.; Sofonea, M.T.; Miot, S.; Pisoni, A.; Tuaillon, E.; Bousquet, J.; Blain, H.; Alizon, S. Analysing Different Exposures Identifies That Wearing Masks and Establishing COVID-19 Areas Reduce Secondary-Attack Risk in Aged-Care Facilities. Int. J. Epidemiol. 2022, 50, 1788–1794. [Google Scholar] [CrossRef]
- Russell, L.B.; Santos da Silva, L.L.; Fracalossi de Moraes, R.; Gidwani, R.; Luz, P.M.; Toscano, C.M. Effect Of Nonpharmaceutical Interventions On COVID-19 Cases And Deaths In Brazil. Health Aff. (Millwood) 2022, 41, 1005–1012. [Google Scholar] [CrossRef]
- Sharif, N.; Alzahrani, K.J.; Ahmed, S.N.; Opu, R.R.; Ahmed, N.; Talukder, A.; Nunia, R.; Chowdhury, M.S.; Nodi, I.J.; Saha, T.; et al. Protective Measures Are Associated with the Reduction of Transmission of COVID-19 in Bangladesh: A Nationwide Cross-Sectional Study. PLoS ONE 2021, 16, e0260287. [Google Scholar] [CrossRef]
- Shaweno, T.; Abdulhamid, I.; Bezabih, L.; Teshome, D.; Derese, B.; Tafesse, H.; Shaweno, D. Seroprevalence of SARS-CoV-2 Antibody among Individuals Aged above 15 Years and Residing in Congregate Settings in Dire Dawa City Administration, Ethiopia. Trop. Med. Health 2021, 49, 55. [Google Scholar] [CrossRef]
- Spira, B. Correlation Between Mask Compliance and COVID-19 Outcomes in Europe. Cureus 2022, 14, e24268. [Google Scholar] [CrossRef]
- Sun, K.; Loria, V.; Aparicio, A.; Porras, C.; Vanegas, J.C.; Zúñiga, M.; Morera, M.; Avila, C.; Abdelnour, A.; Gail, M.H.; et al. Behavioral Factors and SARS-CoV-2 Transmission Heterogeneity within a Household Cohort in Costa Rica. Commun. Med. (Lond) 2023, 3, 102. [Google Scholar] [CrossRef]
- Varela, A.R.; Gurruchaga, A.P.; Restrepo, S.R.; Martin, J.D.; Landazabal, Y.D.C.; Tamayo-Cabeza, G.; Contreras-Arrieta, S.; Caballero-Díaz, Y.; Florez, L.J.H.; González, J.M.; et al. Effectiveness and Adherence to Closed Face Shields in the Prevention of COVID-19 Transmission: A Non-Inferiority Randomized Controlled Trial in a Middle-Income Setting (COVPROSHIELD). Trials 2022, 23, 698. [Google Scholar] [CrossRef]
- Williamson, K.M.; Butler, M.; Elton, B.; Taylor, J.; Islam, F.; Douglas, M.P.; Kirk, M.D.; Durrheim, D.N. Transmission of SARS-CoV-2 Delta Variant from an Infected Aircrew Member on a Short-Haul Domestic Flight, Australia 2021. J. Travel Med. 2022, 29, taac144. [Google Scholar] [CrossRef]
- Wilson, S.; Mouet, A.; Jeanne-Leroyer, C.; Borgey, F.; Odinet-Raulin, E.; Humbert, X.; Le Hello, S.; Thibon, P. Professional Practice for COVID-19 Risk Reduction among Health Care Workers: A Cross-Sectional Study with Matched Case-Control Comparison. PLoS ONE 2022, 17, e0264232. [Google Scholar] [CrossRef]
- Xinias, I.; Mavroudi, A.; Kirvassilis, F.; Antachopoulos, C.; Roilides, E. COVID-19: Face Mask Protection in the Pediatric Setting. Maedica 2021, 16, 149–151. [Google Scholar] [CrossRef]
- SeyedAlinaghi, S.; Karimi, A.; Afsahi, A.M.; Mirzapour, P.; Varshochi, S.; Mojdeganlou, H.; Mojdeganlou, P.; Razi, A.; Alilou, S.; Dashti, M.; et al. The Effectiveness of Face Masks in Preventing COVID-19 Transmission: A Systematic Review. Infect. Disord. Drug Targets 2023, 23, 19–29. [Google Scholar] [CrossRef]
- Tabatabaeizadeh, S.-A. Airborne Transmission of COVID-19 and the Role of Face Mask to Prevent It: A Systematic Review and Meta-Analysis. Eur. J. Med. Res. 2021, 26, 1. [Google Scholar] [CrossRef]
- Li, Y.; Liang, M.; Gao, L.; Ayaz Ahmed, M.; Uy, J.P.; Cheng, C.; Zhou, Q.; Sun, C. Face Masks to Prevent Transmission of COVID-19: A Systematic Review and Meta-Analysis. Am. J. Infect. Control 2021, 49, 900–906. [Google Scholar] [CrossRef]
- Floriano, I.; Silvinato, A.; Bacha, H.A.; Barbosa, A.N.; Tanni, S.; Bernardo, W.M. Effectiveness of Wearing Masks during the COVID-19 Outbreak in Cohort and Case-Control Studies: A Systematic Review and Meta-Analysis. J. Bras. Pneumol. 2024, 49, e20230003. [Google Scholar] [CrossRef]
- Shelus, V.S.; Frank, S.C.; Lazard, A.J.; Higgins, I.C.A.; Pulido, M.; Richter, A.P.C.; Vandegrift, S.M.; Vereen, R.N.; Ribisl, K.M.; Hall, M.G. Motivations and Barriers for the Use of Face Coverings during the COVID-19 Pandemic: Messaging Insights from Focus Groups. Int. J. Environ. Res. Public Health 2020, 17, 9298. [Google Scholar] [CrossRef]
- Jefferson, T.; Foxlee, R.; Del Mar, C.; Dooley, L.; Ferroni, E.; Hewak, B.; Prabhala, A.; Nair, S.; Rivetti, A. Cochrane Review: Interventions for the Interruption or Reduction of the Spread of Respiratory Viruses. Evid. Based Child. Health 2008, 3, 951–1013. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).