Effectiveness of Telematic Behavioral Techniques to Manage Anxiety, Stress and Depressive Symptoms in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
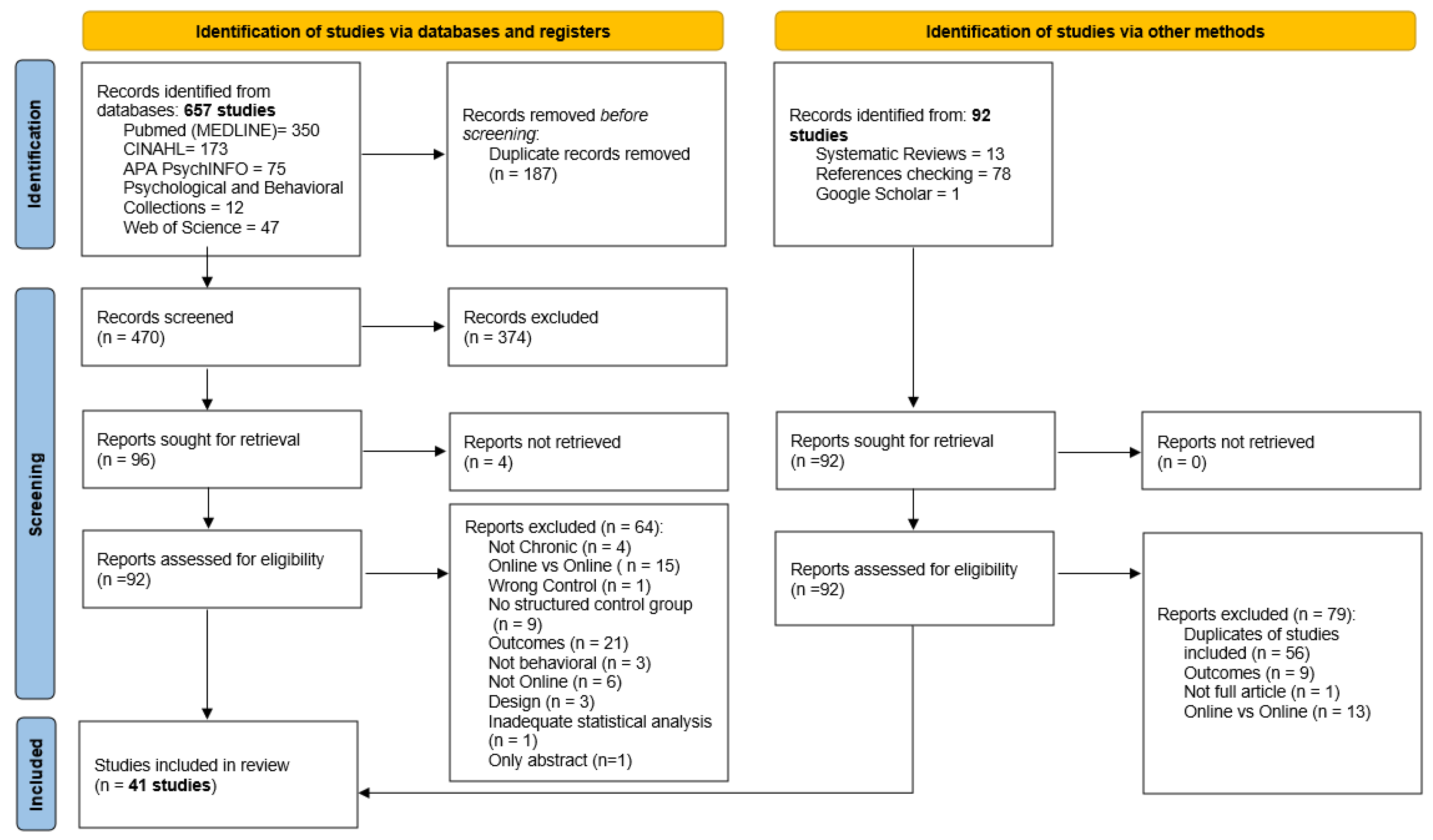
2. Materials and Methods
2.1. Search Strategy
2.2. Study Eligibility Criteria
2.3. Selection Process and Data Extraction
2.4. Risk of Bias and Methodological Quality Assessment
2.5. Quality of Evidence
2.6. Data Synthesis
3. Results
3.1. Descriptions of the Studies
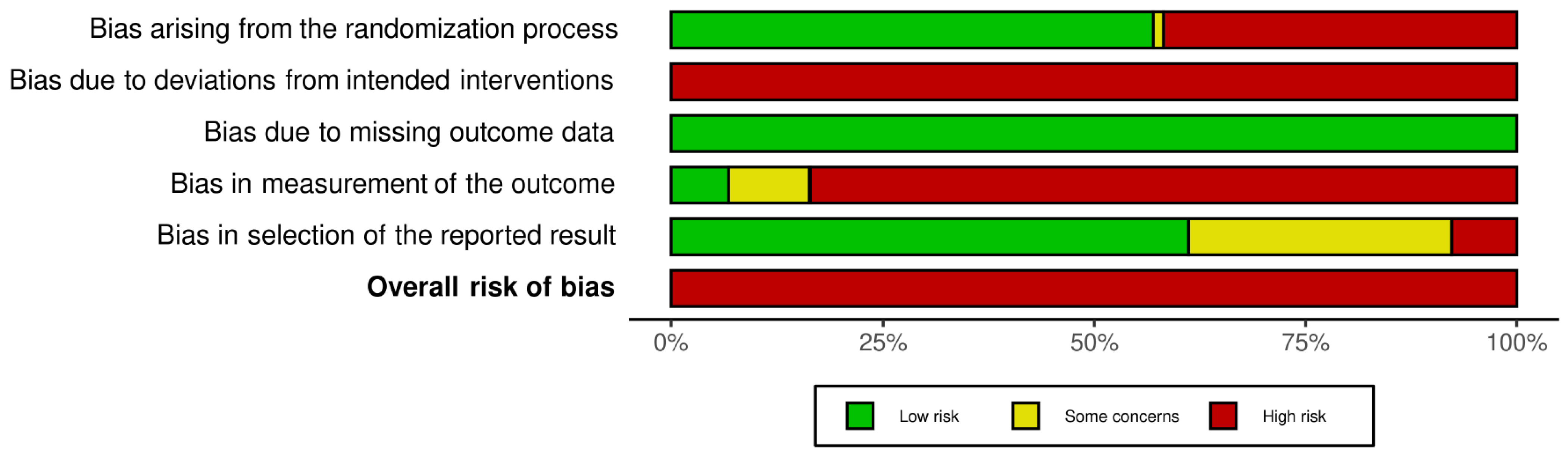
3.2. Methodological Quality and Risk of Bias
3.3. Qualitative Synthesis
3.4. Quantitative Synthesis
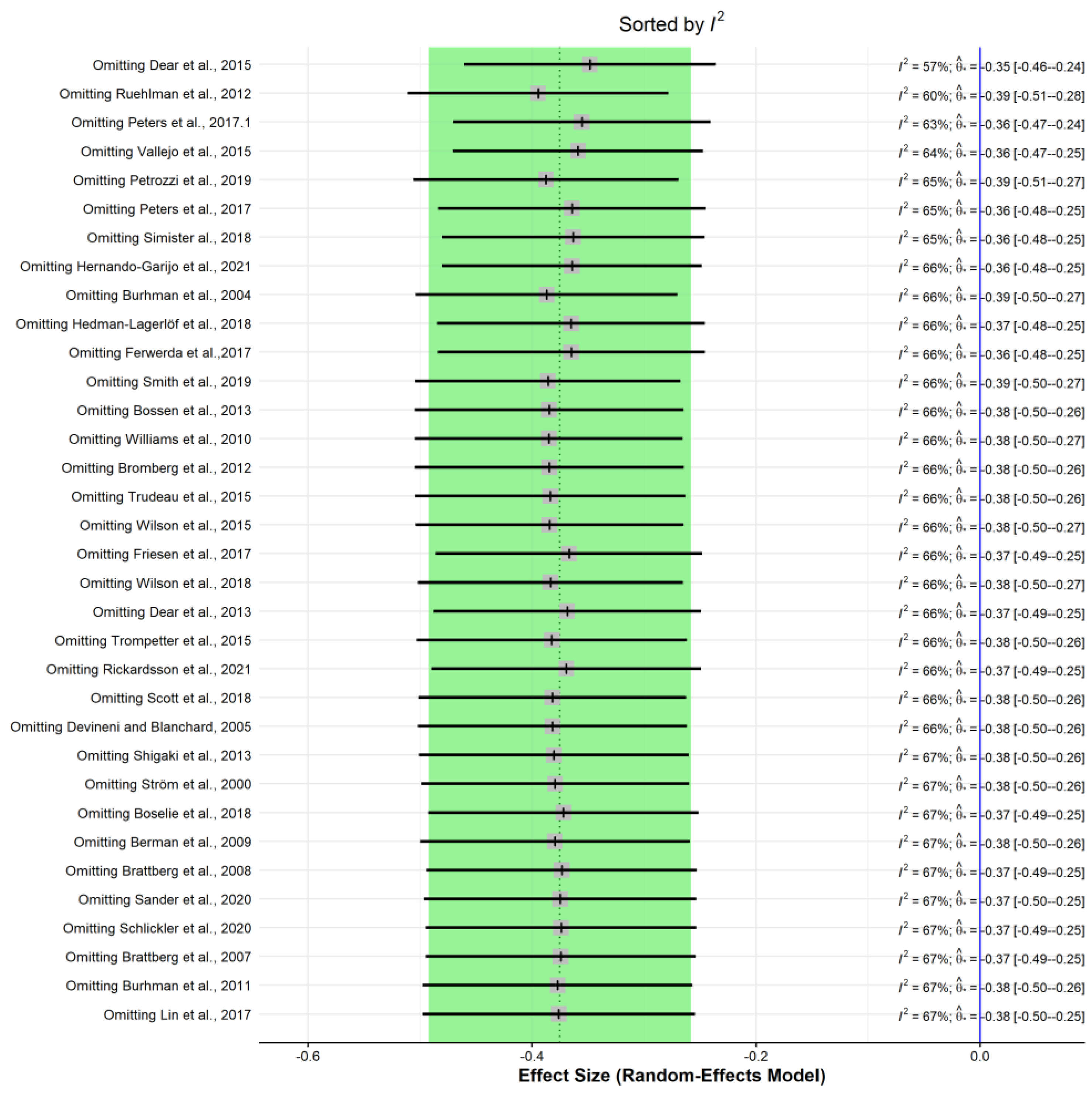
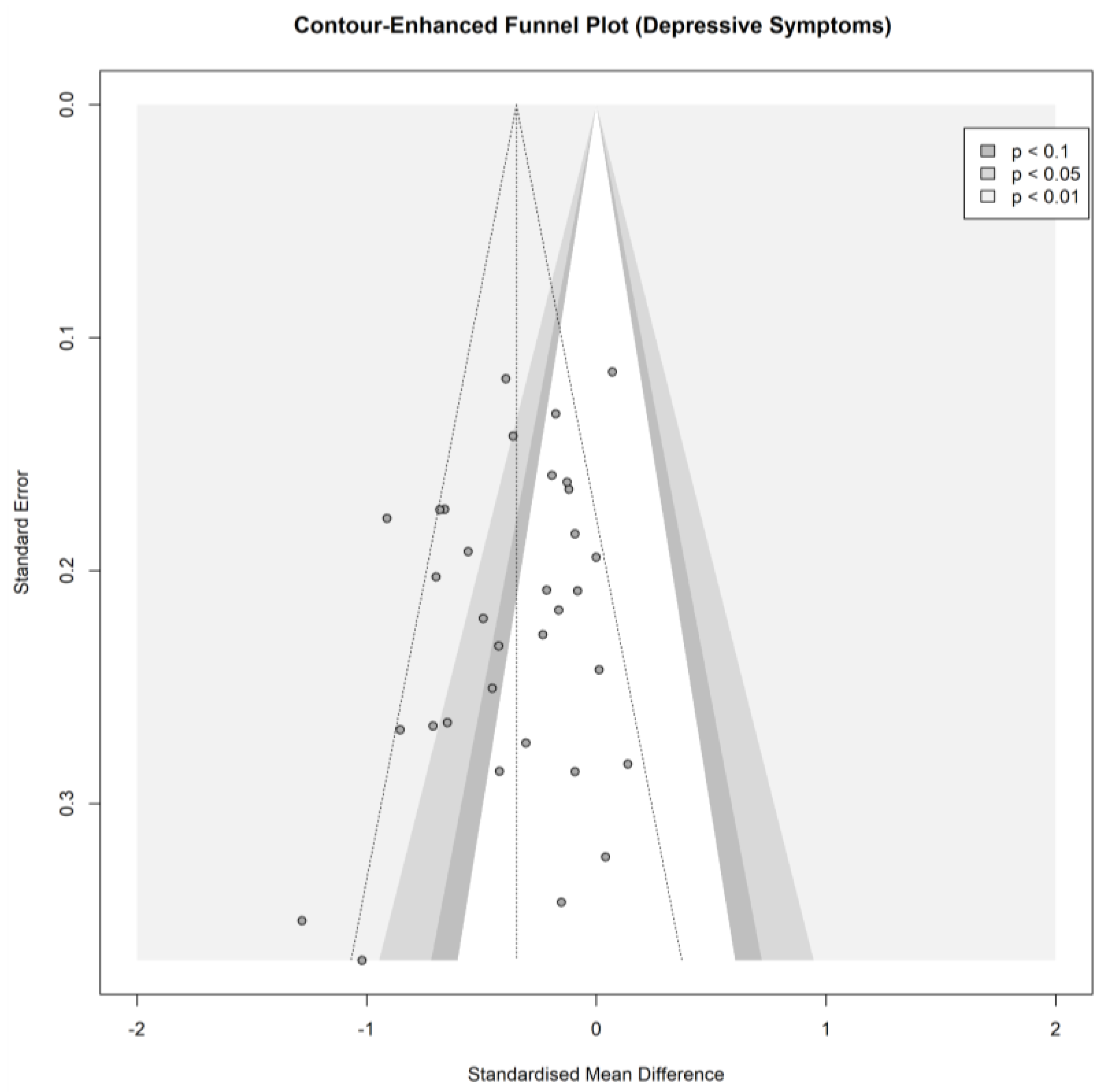
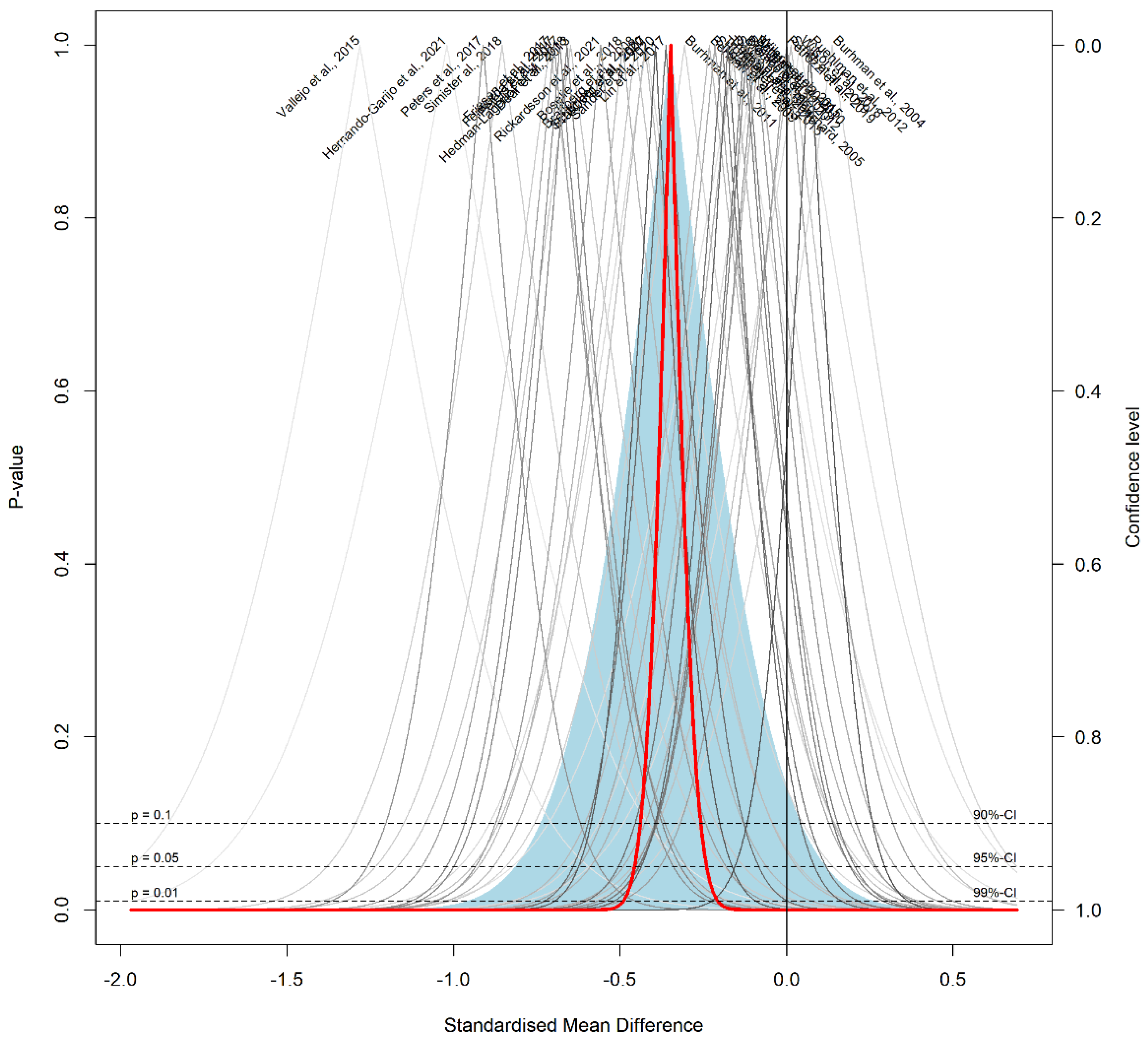
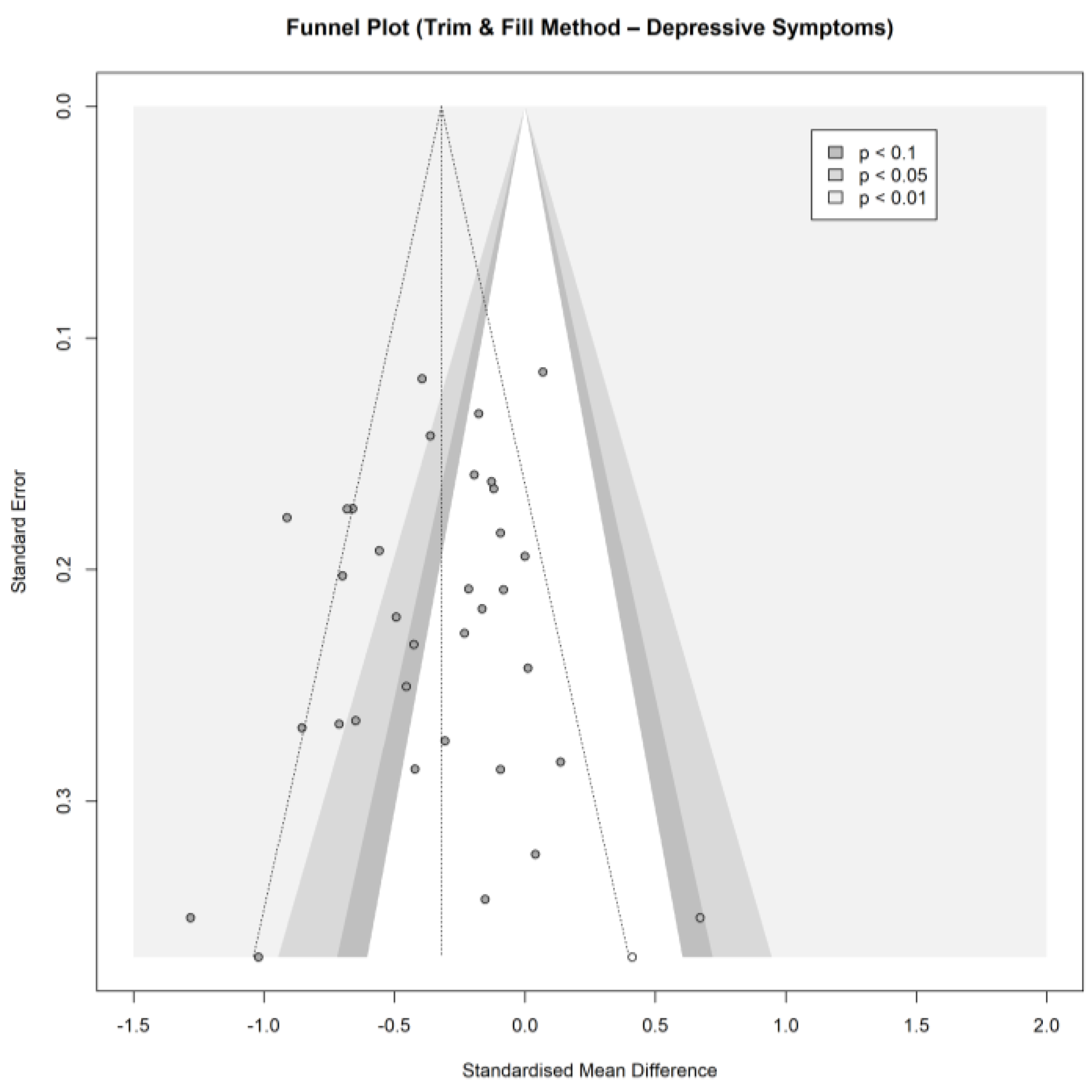
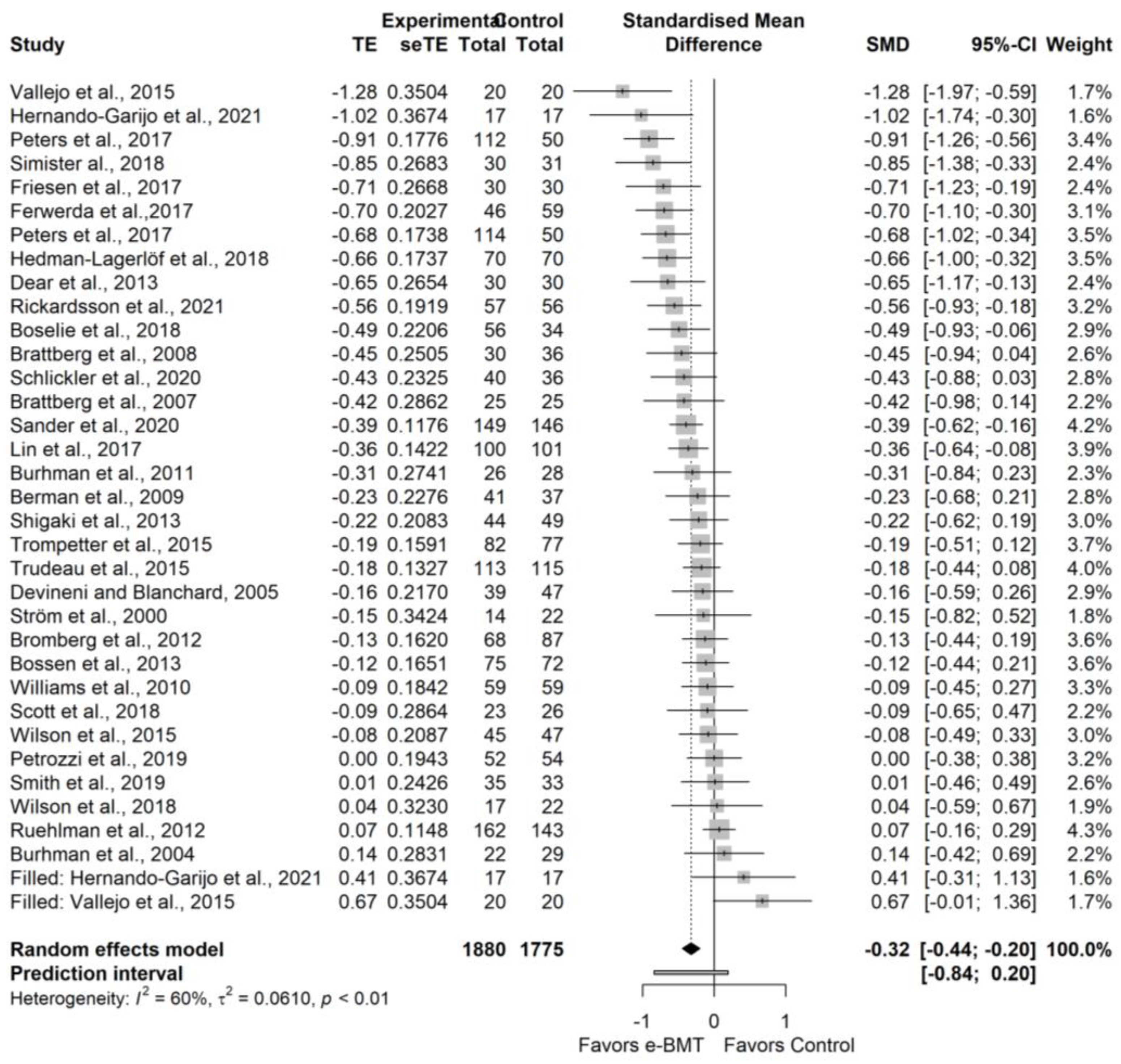
3.4.1. Depressive Symptoms
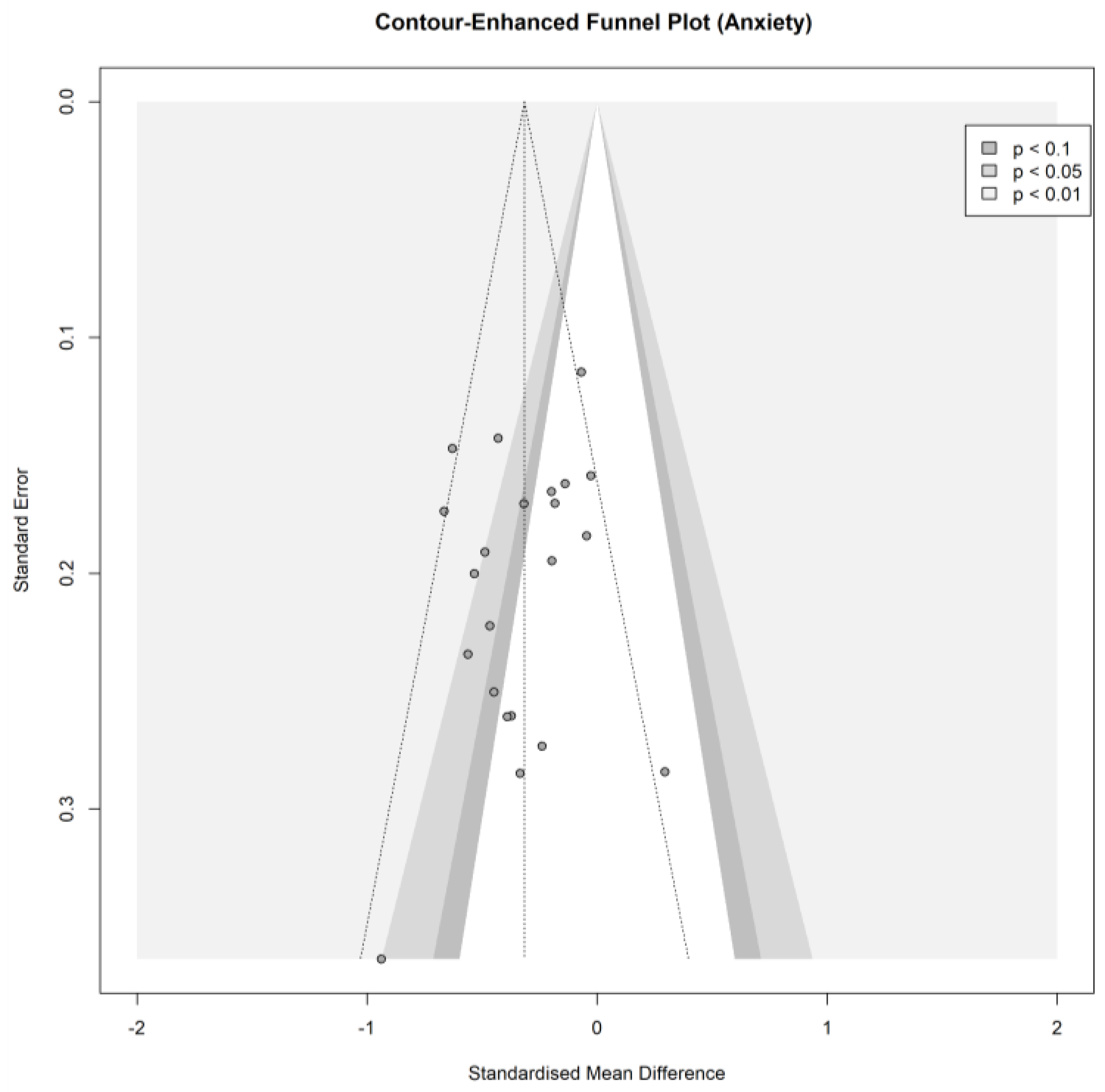
3.4.2. Anxiety
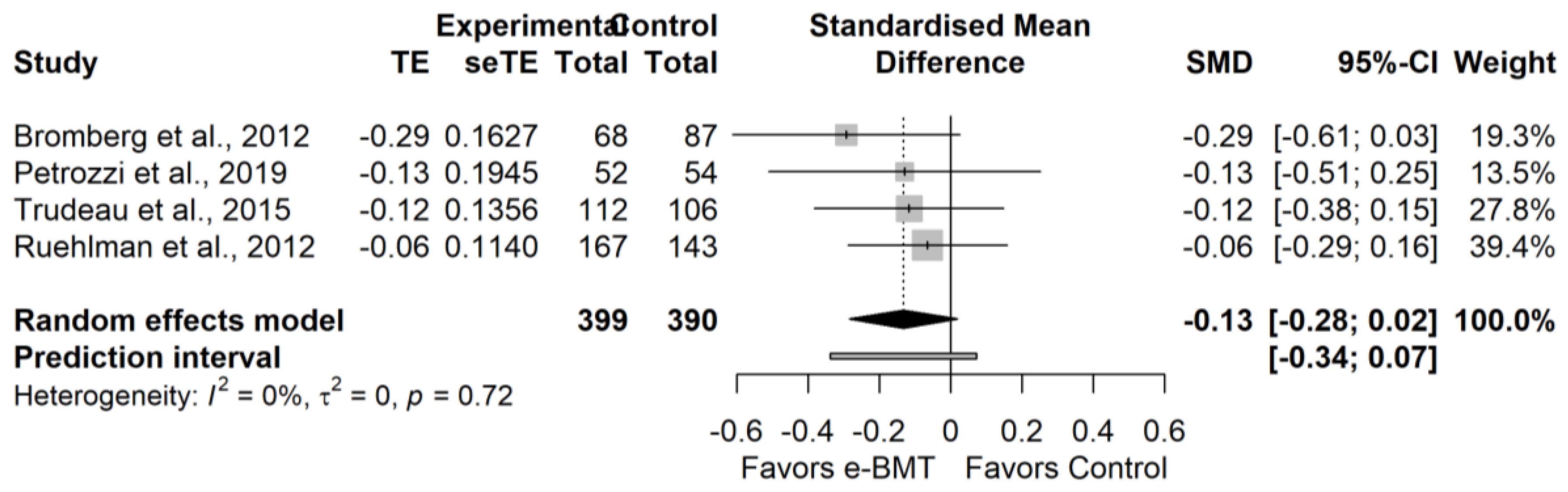
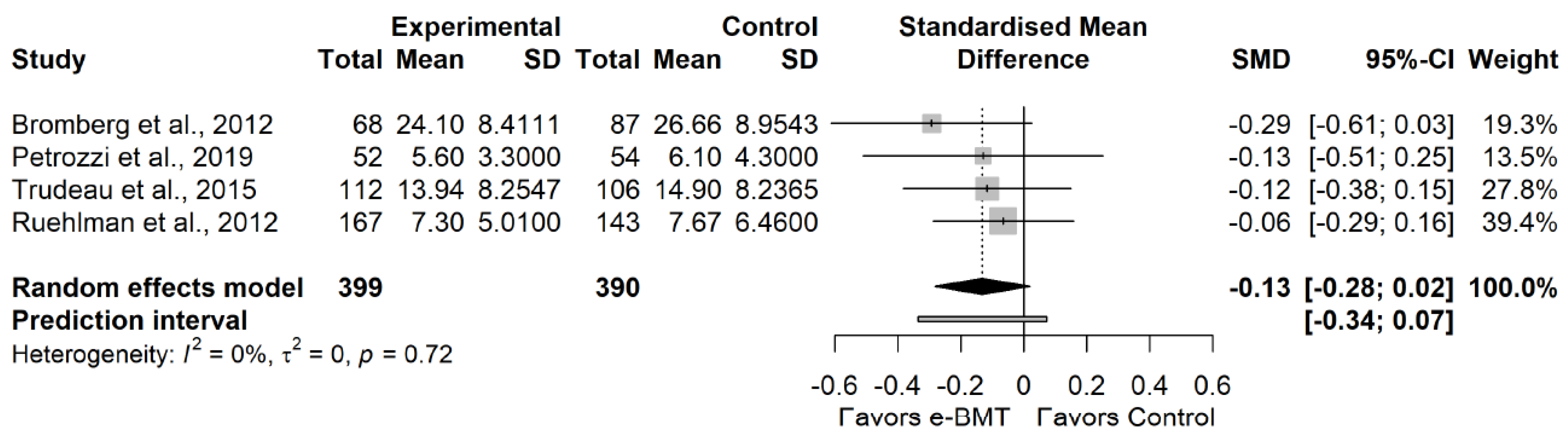
3.4.3. Stress
4. Discussion
4.1. Practical Implication
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
Appendix A.1
Appendix A.2
Appendix A.3. Details of the Studies Included in the Systematic Review
| Authors, Year Design Country | Participants Sample Size (n) Age (Mean (SD)) Gender Condition | Intervention Modality Format | Comparator | Outcomes | Results |
|---|---|---|---|---|---|
| Amorim et al., 2019 Pilot RCT Australia | N = 68 58.3 (13.4) yrs 50%F/50%M Chronic LBP | Activity tracker and monitoring application. + Telephone follow-up Mobile application | Advice to stay active and booklet | Depressive symptoms, anxiety and stress: DASS | No significant differences on the outcomes. |
| Ang et al., 2010 RCT USA | N = 32 48.9 (10.9) yrs 100%F Fibromyalgia | CBT + Usual care Telephone | Usual care | Depressive symptoms: PHQ-8 | Non-significant difference on depressive symptoms (p = 0.8). |
| Berman et al., 2009 RCT USA | N = 89 65.8 (N/R) yrs 87%F/13%M Unspecified chronic pain | Self-care intervention Internet-based | No intervention | Depressive symptoms: CES-D 10 | Small non-significant effect on anxiety and depressive symptoms only in self-care group (p > 0.05). |
| Boselie et al., 2018 RCT The Netherlands | N = 33 N/R yrs N/R%F/N/R%M Unspecified chronic pain | Positive psychology Internet-based | Waiting list | Depressive symptoms and anxiety: HADS | Significant main effect of PPI condition on anxiety (p = 0.02) and depressive symptoms (p = 0.01). |
| Bossen et al., 2013 RCT The Netherlands | N = 199 62.0 (5.7) yrs 65%F/35%M Knee and hip OA | Behavior-graded activity program Internet-based | Waiting list | Anxiety and depressive symptoms: HADS | At the end of the intervention, intervention group showed less anxiety (p = 0.007). Other outcomes showed no significant differences. |
| Brattberg, 2007 RCT Sweden | N = 60 47.0 (8.0) yrs 90%F/10%M Unspecified chronic pain | Support/self-help group about pain. Internet-based videos or CDs | Waiting list | Anxiety and Depressive symptoms: HADS | Intervention group showed a higher improvement in depressive symptoms over time (p = 0.04) but not in anxiety (p = 0.4). |
| Brattberg, 2008 RCT Sweden | N = 66 43.8 (8.8) yrs 100%F Fibromyalgia | Emotional freedom techniques Internet-based | Waiting list | Anxiety and Depressive symptoms: HADS | Intervention group showed a statistically significant time*group interaction in depressive symptoms (p = 0.02) and anxiety (p = 0.03). |
| Bromberg et al., 2012 RCT USA | N = 189 42.6 (11.5) yrs 89%F/11%M Chronic migraine | Structured behavior changes program +Usual care Internet-based | Usual care | Depressive symptoms, anxiety and stress: DASS-21 | Intervention group showed a higher improvement in depressive symptoms (p = 0.008) and stress (p = 0.04), but not on anxiety. |
| Buhrman et al., 2004 RCT Sweden | n = 56 44.6 (10.4) yrs 63%F/37%M Chronic back pain | Online CBT + Relaxation with CDs + Telephone calls about goals Internet-based | Waiting list | Anxiety and depressive symptoms: HADS | There was no significant main effects difference on anxiety and depressive symptoms. |
| Buhrman et al., 2011 RCT Sweden | N = 54 43.2 (9.8) yrs 69%F/32%M Chronic back pain | Online CBT Internet-based | Waiting list | Anxiety and depressive symptoms: HADS | There were no significant differences between group for anxiety and depressive symptoms. |
| Dear et al., 2013 RCT Australia | N = 63 49.0 (13) yrs 85%F/15%M Unspecified chronic pain | Online CBT Internet-based | Waiting list | -Depressive symptoms: PHQ-9 -Anxiety: GAD-7 | Intervention had a significantly higher post-treatment improvement in depressive symptoms (p < 0.001), anxiety (p < 0.001). |
| Dear et al., 2015 RCT Australia | N = 490 50 (13) yrs 80%F/20%M Unspecified chronic pain | G1: Online CBT + Regular online contact G2: Online CBT + optimal online contact G3: Online CBT Internet-based | Waiting list | -Depressive symptoms: PHQ-9 -Anxiety: GAD-7 | Intervention groups had significantly lower scores than waiting list for depressive symptoms and anxiety (p < 0.001) post-treatment. |
| Devineni and Blanchard, 2005 RCT USA | N = 86 42.2 (11.9) yrs 62%F/38%M Chronic migraine and/or tension-type headache | Behavioral headache-related intervention Internet-based | Waiting list | Depressive symptoms: CES-D | There was no statistically significant difference for depressive symptoms (p = 0.11) and anxiety (p = 0.20). |
| Ferwerda et al.,2017 RCT The Netherlands | N = 133 56.4(10) yrs 64%F/36%M Rheumatoid arthritis | CBT Internet-based | Usual care | -Depressive symptoms: BDI -Negative mood and Anxiety: IRGL | Intervention group report a larger decrease in anxiety (p < 0.001) and depressed mood (p < 0.001) than control group. |
| Friesen et al., 2017 RCT Canada | N = 60 48.0 (11.0) yrs 95%F/5%M Fibromyalgia | CBT + Telephone calls Internet-based | Waiting list | -Anxiety: GAD-7 -Depressive symptoms: PHQ-9 -Anxiety and depressive symptoms: HADS | Intervention group had a significantly higher improvement in anxiety (p = 0.030) and depressive symptoms (p < 0.001). There were also statistically significant time by group interactions for HADS-depressive symptoms (p = 0.007), and HADS-anxiety (p = 0.001). |
| Heapy et al., 2017 RCT USA | N = 125 57.9 (11.6) yrs 22%F/78%M Chronic back pain | CBT Interactive voice response | Face-to-Face CBT | Depressive symptoms: BDI-II | There were no significant differences between e-CBT and face-to-face CBT in depressive symptoms. |
| Hedman-Lagerlöf et al., 2018 RCT Sweden | N = 140 50.8 (24--77) yrs 98%F/2%M Fibromyalgia | Online exposure therapy Internet-based | Waiting list | -Depressive symptoms: PHQ-9 -Anxiety: GAD-7 | There were statistically significant interactions in favor of intervention group for depressive symptoms and anxiety (all, p < 0.001). |
| Herbert et al., 2017 RCT USA | N = 128 18%F/82%M 52.0 (13.3) yrs Unspecific chronic pain | ACT Video teleconferencing | Face-to-face ACT | -Depressive symptoms: PHQ-9 -Pain-related anxiety: PASS-20 | There were no significant differences for any outcomes. |
| Hernando-Garijo et al., 2021 RCT Spain | N = 34 53.4 (8.8) yrs 100%F Fibromyalgia | Video-guided aerobic training + usual medical prescription Videoconferencing | Usual medical prescription | Anxiety and depressive symptoms: HADS | There was a statistically significant higher improvement in psychological distress (p = 0.002) according to HADS than control group. |
| Juhlin et al., 2021 RCT Sweden | N = 139 47.6 (10.1) yrs 90%F/10%M Chronic widespread pain | Person-centered intervention supported by online platform Internet-based | Person-centered intervention | Stress: SCI-93 | No statistically significant differences between groups for stress (p = 0.21). |
| Lin et al., 2017 RCT Germany | N = 201 51.0 (12.4) yrs 86%F/14%M Unspecific chronic pain | Online guided ACT Internet-based | Waiting list | Depressive symptoms: PHQ-9 Anxiety: GAD-7 | There was a significant interaction effect for group x time on depressive symptoms (p < 0.05) in favor of intervention group. |
| Moessner et al., 2012 RCT Germany | N = 75 45.9 (9.1) yrs 56%F/44%M Chronic back pain | Self-monitoring + Online guided chat Internet-based | Usual care | Anxiety and depressive symptoms: HADS | There were no significant differences in other outcomes. |
| Peters et al., 2017 RCT Sweden | N = 284 48.6 (12.0) yrs 85%F/15%M Chronic back, neck or shoulder pain | G1: Online Positive psychology G2: Online CBT Internet-based | Waiting list | Depressive symptoms and Anxiety: HADS | Both intervention groups showed significant differences with the waiting list group for depressive symptoms (p < 0.001). There were also significant differences for anxiety. |
| Petrozzi et al., 2019 RCT New Zealand | N = 108 50.4 (13.6) yrs 50%F/50%M Chronic LBP | Online CBT+ Usual care Internet-based | Usual care | Depressive symptoms, anxiety and stress: DASS-21 | There were no statistically significant differences between the two groups for depressive symptoms (0.98), anxiety (p = 0.19) or stress (p = 0.41) at any time-points. |
| Rickardsson et al., 2021 RCT Sweden | N = 113 49.5 (12.1) yrs 75%F/25%M Unspecific chronic pain | Online ACT Internet-based | Waiting list | Anxiety: GAD-7 Depressive symptoms: PHQ-9 | The intervention group showed significant interaction effects of time x group for anxiety (p = 0.03) and depressive symptoms (p = 0.001). |
| Ruehlman et al., 2012 RCT USA | N = 305 44.9 (N/R) yrs 64%F/36%M Unspecific chronic pain | Online self-management Internet-based | Usual care | -Depressive symptoms: CES-D -Depressive symptoms, anxiety and stress: DASS | Intervention group showed a significant group x time interaction in depressive symptoms (p = 0.03 and p = 0.04), stress (p = 0.00) and anxiety (p = 0.05) |
| Sander et al., 2020 | N = 295 52.8 (7.7) yrs 62%F/38%M Unspecific chronic pain | Online CBT + Usual care Internet-based | Usual Care | Depressive symptoms: HamD, QIDS score and PHQ-9 | Intervention group had a statistically significant greater improvement of all the outcomes compared with control group. |
| Schlickler et al., 2020 RCT Germany | N = 76 50.8 (7.9) yrs 55%F/45%M Chronic back pain | Online CBT-based intervention Internet-based and mobile-based | Waiting list | -Depressive symptoms: CES-D and QIDS-SR16 -Anxiety: HamADS | There was a significant reduction in both treatment in depressive symptoms according to CES-D (p < 0.001) with a significant difference in favor of the intervention group post-treatment (p = 0.03). Intervention group also showed a significant greater reduction in anxiety (p = 0.001). |
| Scott et al., 2018 RCT UK | N = 63 45.5 (14.0) yrs 64%F/36%M Unspecific chronic pain | Online ACT + Usual care Internet-based | Usual care | Depressive symptoms: PHQ-9 | Intervention group showed medium effects on depressive symptoms. |
| Shigaki et al., 2013 RCT USA | N = 108 49.8 (11.9) yrs 94%F/6%M Rheumatoid arthritis | Education and social network website about Rheumatoid arthritis + Telephone calls Internet-based | Waiting list | Depressive symptoms: CES-D | No statistically significant differences in depressive symptoms (p = 0.14). |
| Simister al., 2018 RCT | N = 67 39.7 (9.4) yrs 95%F/5%M Fibromyalgia | Online ACT + Usual care Internet-based | Usual care | Depressive symptoms: CES-D | Intervention group significantly improved, relative to control group, on depressive symptoms (p = 0.02). |
| Smith et al., 2019 RCT Australia | N = 80 45.0 (13.9) yrs 88%F/12%M Unspecific chronic pain | Online self-management and CBT-based intervention Internet-based | Usual care | Depressive symptoms: PHQ-9 | There was no statistically significant interaction for depressive symptoms. |
| Ström et al., 2000 RCT Sweden | N = 45 36.7 (N/R) yrs 69%F/31%M Recurrent headache sufferers | Online relaxation and problem-solving intervention Internet-based | Wait-list | Depressive symptoms: BDI | There were no significant differences for depressive symptoms. |
| Tavallaei et al., 2018 RCT Iran | N = 30 33.7 (9.0) yrs 100%F Migraine and tension-type headache | Mindfulness-based Stress Reduction Bibliotherapy Internet-based | Usual care | Depressive symptoms, anxiety and stress: DASS-21 | N/R |
| Trompetter et al., 2015 RCT The Netherlands | N = 238 52.7 (12.4) yrs 76%F/24%M Unspecific chronic pain | Online ACT Internet-based | Waiting list | Depressive symptoms and Anxiety: HADS | There was a statistically significant difference in depressive symptoms (p = 0.006). |
| Trudeau et al., 2015 RCT USA | N = 228 49.9 (11.6) 68%F/32%M Arthritis | Online self-management intervention Internet-based | Waiting List | Depressive symptoms, anxiety, and stress: DASS-21 | No statistically significant condition-by-time effect on the three subscales of the DASS-21. |
| Vallejo et al., 2015 RCT Spain | N = 60 51.6 (9.9) yrs 100%F Fibromyalgia | Online CBT + Usual care Internet-based | G1: Face-to-face CBT + Usual care G2: Usual care | Depressive symptoms and anxiety: HADS Depressive symptoms: BDI | Both groups improved depressive symptoms (both, p < 0.01) and HADS scores. |
| Westenberg et al., 2018 RCT USA | N = 126 54.5 (15.0) yrs 50%F/50%M Upper limb disorders | Online Mindfulness Internet-based | Attention control | -Depressive symptoms: N/R -Anxiety: N/R | Intervention group had statistically significant improvements in depressive symptoms (p = 0.004) and anxiety (p = 0.024). |
| Williams et al., 2010 RCT USA | N = 118 50.5 (11.5) yrs 95%F/5%M Fibromyalgia | Online CBT + Usual care Internet-based | Usual care | -Depressive symptoms: CES-D -Anxious mood: STPI—state anxiety | There were no statistically significant differences in anxiety and depressive symptoms. |
| Wilson et al., 2015 RCT USA | N = 114 49.3 (11.6) yrs 78%F/12%M Unspecific chronic pain | Online pain management program Internet-based | Waiting list | Depressive symptoms: PHQ-9 | There were no statistically significant interactions for group-by-time on depressive symptoms. |
| Wilson et al., 2018 RCT USA | N = 60 44.3 (12.0) yrs 44%F/56%M Unspecific chronic pain | Online self-management program Internet-based | Waiting list | Depressive symptoms: PHQ-8 | Intervention group had higher depressive symptoms score at the end of the intervention (p = 0.001). |
Appendix A.4. Details of the Interventions
| Authors, Year | Intervention | Comparator | ||||
|---|---|---|---|---|---|---|
| Format Equipment and Contact Form | Modality and Content | Duration and Frequency, Follow-Up | Format Equipment | Modality and Content | Duration and Frequency, Follow-Up | |
| Amorim et al., 2019 | Mobile application Written, pedometer Telephone call, message | Physical exercise, activity tracker, lessons
| 6 months 1 face-to-face interview and 2 calls/month Follow-up: N/A | Recommendations Written, brief advice |
| 6 months N/A Follow-up: N/A |
| Ang et al., 2010 | Telephone call + usual care Written Telephone call | CBT. Lessons, relaxation
| 6 weeks 1 session/week Follow-up: 12 weeks | Usual care |
| 6 weeks N/A Follow-up: 12 weeks |
| Berman et al., 2009 | Internet-based Images, audio | Self-care. Mind–body exercises and lessons
| 6 weeks ≥1 session/week Follow-up: N/A | No intervention N/A | N/A | N/A N/A Follow-up: N/A |
| Boselie et al., 2018 | Internet-based Online platform Telephone call, email | Positive psychology exercises
| 8 weeks Call: weeks 1, 3, 5,7 Email: weeks 2, 4, 6, 8 Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Bossen et al., 2013 | Internet-based Written, video | Behavior-graded activity and exercises
| 9 weeks ≥1 session/week Follow-up: 12 weeks | Waiting list N/A | N/A | N/A N/A Follow-up: 12 weeks |
| Brattberg, 2007 | Internet-based Written, video Internet guided chat | Self-help about pain.
| 20 weeks 1 video/week Follow-up: 12 months | Waiting list | Maintain pharmacotherapy | 20 weeks N/A Follow-up: 12 months |
| Brattberg, 2008 | Internet-based Written Telephone call, email | Self-management. Emotional Freedom TechniquesSelf-monitoring of outcome of behavior | 8 weeks 1 time/day Follow-up: N/A | Waiting list | N/A | N/A N/A Follow-up: N/A |
| Bromberg et al., 2012 | Internet-based +usual care Written | Behavior change, physical activity, lessons
| 6 months ≥2 sessions/week (first 4 weeks) ≥1 sessions/month (final 5 month) Follow-up: N/A | Usual care N/A | Maintain the routine care and self-management effort | N/A N/A Follow-up: N/A |
| Buhrman et al., 2004 | Internet-based Slideshow, audio Telephone call | CBT. Physical and psychological exercises, relaxation
| 6 weeks 1 call/week Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Buhrman et al., 2011 | Internet-based Written | CBT. Physical exercise, relaxation, cognitive skills
| 8 weeks N/R Follow-up: 12 weeks | Waiting list N/A | N/A | N/A N/A Follow-up: 12 weeks |
| Dear et al., 2013 | Internet-based Written Telephone call | CBT. Lessons, homework
| 8 weeks 1 lesson/7–10 days 1 call/week Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Dear et al., 2015 | Internet-based
Slideshow Telephone call, email | CBT. Lessons, homework
| 8 weeks 1 lesson/7–10 days G1: 1 call/week G2: as-needed calls G3: no contact Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Devineni and Blanchard, 2005 | Internet-based Written, audio, web pages | Lessons, exercises, relaxation, Behavioral headache-related intervention Autogenic training
| 4 weeks N/R Follow-up: 2 months | Waiting list | N/A | N/A N/A Follow-up: 2 months |
| Ferwerda et al., 2017 | Internet-based Written | CBT. Lessons, homework
| 17 to 32 weeks 1 email/1–2 weeks Follow-up: 12 months | Usual care N/R | Rheumatological care | N/R N/R Follow-up: 12 months |
| Friesen et al., 2017 | Internet-based Slideshow Telephone call, email | CBT. Lessons, homework
| 8 weeks 1 email and call/week Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow up: N/A |
| Heapy et al., 2017 | Interactive voice response Written, images, audio, pedometer Telephone call | CTB. Lessons, relaxation
| 10 weeks 1 call/day Follow-up: 9 months | Face-to-face Written, images, audio, pedometer | CBT. Lessons, relaxation
| 10 weeks 1 session/week Follow-up: 9 months |
| Hedman-Lagerlöf et al., 2018 | Internet-based Written Telephone call, message | Lessons, homework, mindfulness
| 10 weeks 1–3 contact/week Follow-up: 12 months | Waiting list N/A | N/A | N/A N/A Follow-up: 12 months |
| Herbert et al., 2017 | Videoconferencing Written N/R | ACT. Mindfulness, lessons
| 8 weeks 1 session/week Follow-up: 6 months | Face-to-face Written | ACT. Mindfulness, lessons
| 8 weeks 1 session/week Follow-up: 6 months |
| Hernando-Garijo et al., 2021 | Videoconferencing + usual care Video Video call | Aerobic exercise
| 15 weeks 2 session/week Follow-up: N/A | Usual care N/A |
| 15 weeks N/A Follow-up: NA |
| Juhlin et al., 2021 | Internet-based Digital platform Message | Person-centered intervention. Physical and psychological exercises
| 6 months 1 contact/week Follow-up: N/A | Face-to-face (1 session) N/A |
| 6 months N/A Follow-up: N/A |
| Lin et al., 2017 | Internet-based Written, audio, video Email, message | ACT. Lessons, mindfulness
| 9 weeks 1 session/week Follow-up: 6 months | Waiting list N/A |
| N/A N/A Follow-up: 6 months |
| Moessner et al., 2012 | Internet-based N/R Internet guided chat | Self-monitoring. Lessons
| 12–15 weeks 1 session/week Follow-up: 6 months | Usual care N/A | N/R | 12–15 weeks 1 session/week Follow-up: 6 months |
| Peters et al., 2017 | Internet-based Written Telephone call, email | G1: Positive psychology. Psychological exercises
| 8 weeks 1 lesson/week Call: weeks 1, 3, 5, 7 Email: weeks: 2, 4, 6, 8 Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Petrozzi et al., 2019 | Internet-based + usual care Written Telephone call | CBT. Lessons, homework
| 8 weeks 1 lesson/week 1 call/week Follow-up: 12 months | Usual care N/A |
| 8 weeks 12 sessions (variable frequency) Follow-up: 12 months |
| Rickardsson et al., 2021 | Internet-based Written, image, audio Telephone call, message | ACT. Lessons
| 8 weeks 7 sessions/week ≥2 messages/week Follow-up: 12 months | Waiting list N/A |
| N/A N/A Follow-up: 12 months |
| Ruehlman et al., 2012 | Internet-based Written, image Email, message | Self-management + e-community. Physical exercise, lessons, homework, relaxation
| 6 weeks N/R Follow-up: 14 weeks | Usual care N/A | N/R | 6 weeks N/A Follow-up: 14 weeks |
| Sander et al., 2020 | Internet-based + usual care Written, audio, video Telephone call, email, message | CBT. Lessons, homework, relaxation
| 9 weeks 7 sessions/week Follow-up: 12 months | Usual care N/A | Medical or psychological treatment | 9 weeks N/R Follow-up: 12 months |
| Schlickler et al., 2020 | Internet-based + mobile-based N/R Email, message | CBT. Lessons, mindfulness, relaxation
| 9 weeks 7 lessons/week Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Scott et al., 2018 | Internet-based + usual care Video Telephone call, email | ACT. Lessons
| 5 weeks 2 lesson/week (first 3 weeks), 1 lesson/week (final 2 weeks) Follow-up: 9 months | Usual care N/A |
| 5 weeks N/A Follow-up: 9 months |
| Shigaki et al., 2013 | Internet-based Slideshow Telephone call, message, online chat | Lessons, homework
| 10 weeks 1 lesson/week 1 call/week Follow-up: N/A | Waiting list |
| N/A N/A Follow-up: N/A |
| Simister al., 2018 | Internet-based + usual care Written, audio, video | ACT. Lessons, homeworkFeedback on behaviorNon-specific reward | 8 weeks N/R Follow-up: 3 months | Usual care N/A |
| 8 weeks N/A Follow-up: 3 months |
| Smith et al., 2019 | Internet-based Written, image, audio, video Telephone call, email | CBT and self-management. Multidisciplinary program with physical exercise, lessons, homework, relaxation
| 4 months 2 lessons/month Follow-up: 7 months | Usual care N/A |
| 4 months N/A Follow-up: 7 months |
| Ström et al., 2000 | Internet-based Written | Lessons, relaxation
| 6 weeks 1 lesson/week Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Tavallaei et al., 2018 | Internet-based Written N/R | Mindfulness-based stress reduction bibliotherapy
| 8 weeks 1 lesson/week Follow-up: N/A | Usual care N/A |
| 8 weeks N/A Follow-up: N/A |
| Trompetter et al., 2015 | Internet-based Written | ACT. Lessons, mindfulness
| 3 months ≥3 h/week Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Trudeau et al., 2015 | Internet-based Multimedia materials Telephone call, email | Self-management. Lessons
| 6 months ≥2 sessions/week (1 month) 1 session/month (5 months) Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Vallejo et al., 2015 | Internet-based + usual care Written, images, audio Message | CBT. Lessons, homework, relaxation
| 10 weeks 1 session/week Follow-up: 12 months | G1: Face-to-face + usual care Written, images, audio G2: Usual care N/A | G1: CBT. Lessons, homework, relaxation
| 10 weeks G1: 1 session/week G2: N/A Follow-up (only G1): 12 months |
| Westenberg et al., 2018 | Internet-based Written, video N/R | Mindfulness
| 60-s video N/R Follow-up: N/A | Attention control Written |
| 60-s read N/R Follow-up: N/A |
| Williams et al., 2010 | Internet-based + usual care Written, audio, video No contact | Self-management. Lessons, homework, relaxation
| 6 months N/R Follow-up: N/A | Usual care |
| 6 months N/A Follow-up: N/A |
| Wilson et al., 2015 | Internet-based N/R N/R | Self-management. Lessons, exercises, relaxation
| 8 weeks N/R Follow-up: N/A | Usual care N/A | N/A | 8 weeks N/R Follow-up: N/A |
| Wilson et al., 2018 | Internet-based Written Interactive activity | Self-management. Lessons, homework
| 8 weeks N/R Follow-up: N/A | Waiting list Written |
| 8 weeks 1 email/week Follow-up: N/A |
Appendix A.5. Assessment of the Quality of the Studies Based on the PEDro Scale
| Items | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Articles | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
| Amorim et al., 2019 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Ang et al., 2010 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Berman et al., 2009 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Boselie et al., 2018 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Bossen et al., 2013 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 |
| Brattberg, 2007 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Brattberg, 2008 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Bromberg et al., 2012 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Buhrman et al., 2004 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Buhrman et al., 2011 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Dear et al., 2013 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Dear et al., 2015 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Devineni and Blanchard, 2005 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Ferwerda et al., 2017 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Friesen et al., 2017 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Heapy et al., 2017 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 |
| Hedman-Lagerlöf et al., 2018 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Herbert et al., 2017 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Hernando-Garijo et al., 2021 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Juhlin et al., 2021 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 |
| Lin et al., 2017 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 |
| Moessner et al., 2012 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Peters et al., 2017 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Petrozzi et al., 2019 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Rickardsson et al., 2020 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Ruehlman et al., 2012 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Sander et al., 2020 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Schlicker et al., 2021 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Scott et al., 2018 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Shigaki et al., 2013 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Simister et al., 2018 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Smith et al., 2019 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 6 |
| Ström et al., 2000 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Tavallaei et al., 2018 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Trompetter et al., 2014 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Trudeau et al., 2015 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Vallejo et al., 2015 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Westenberg et al., 2018 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Williams et al., 2010 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Wilson et al., 2015 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Wilson et al., 2018 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
Appendix A.6. Risk of Bias 2

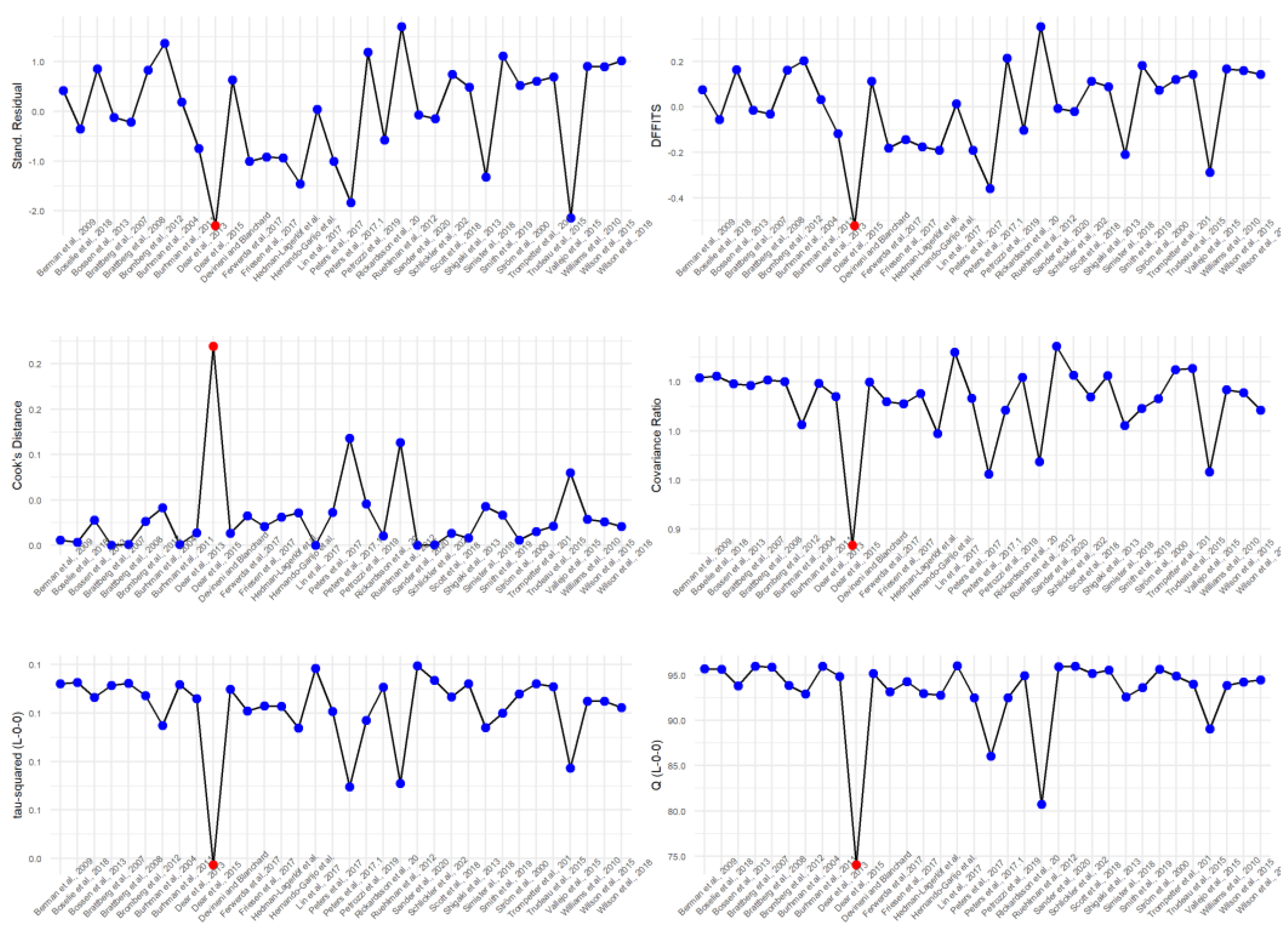
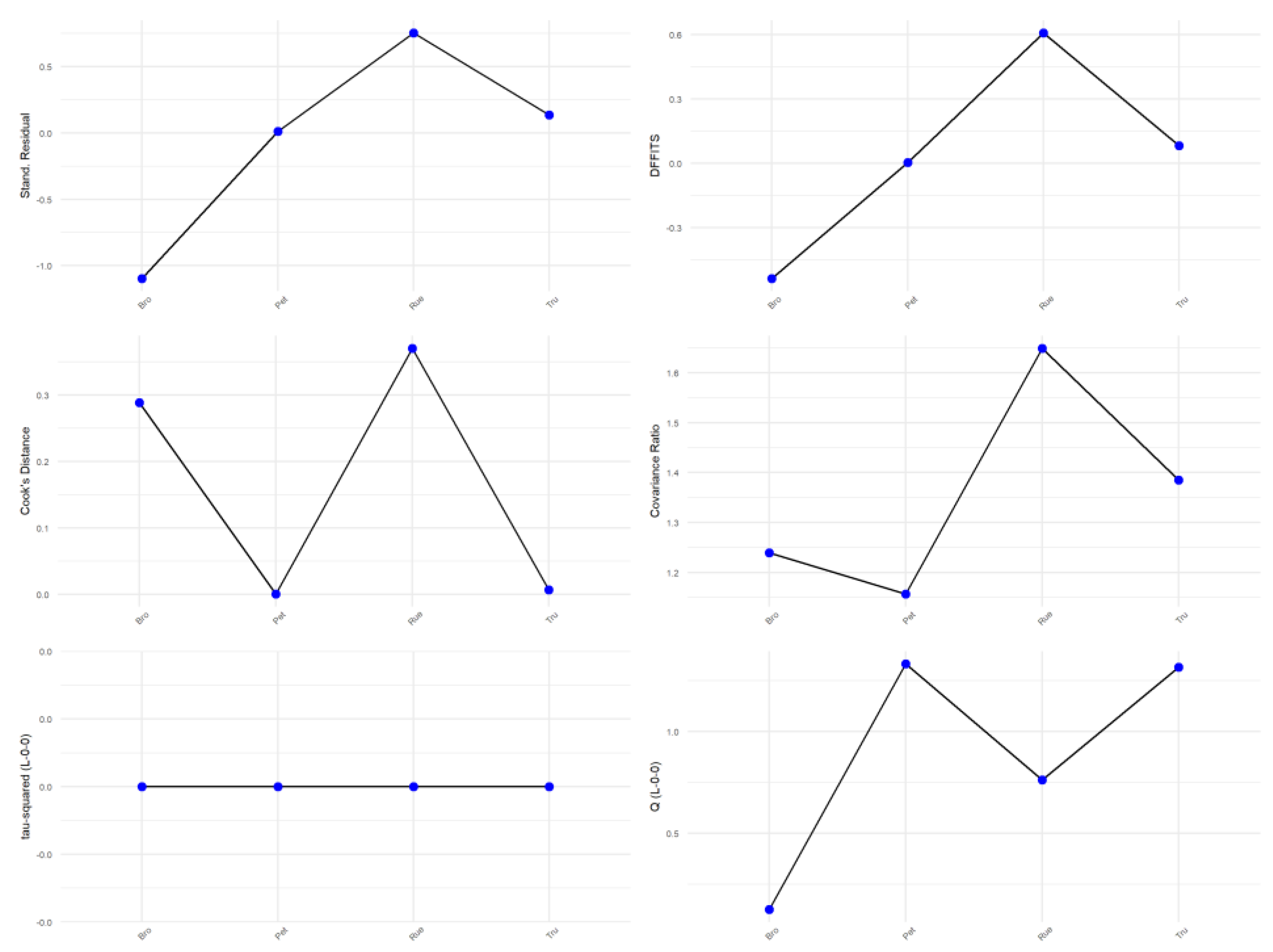
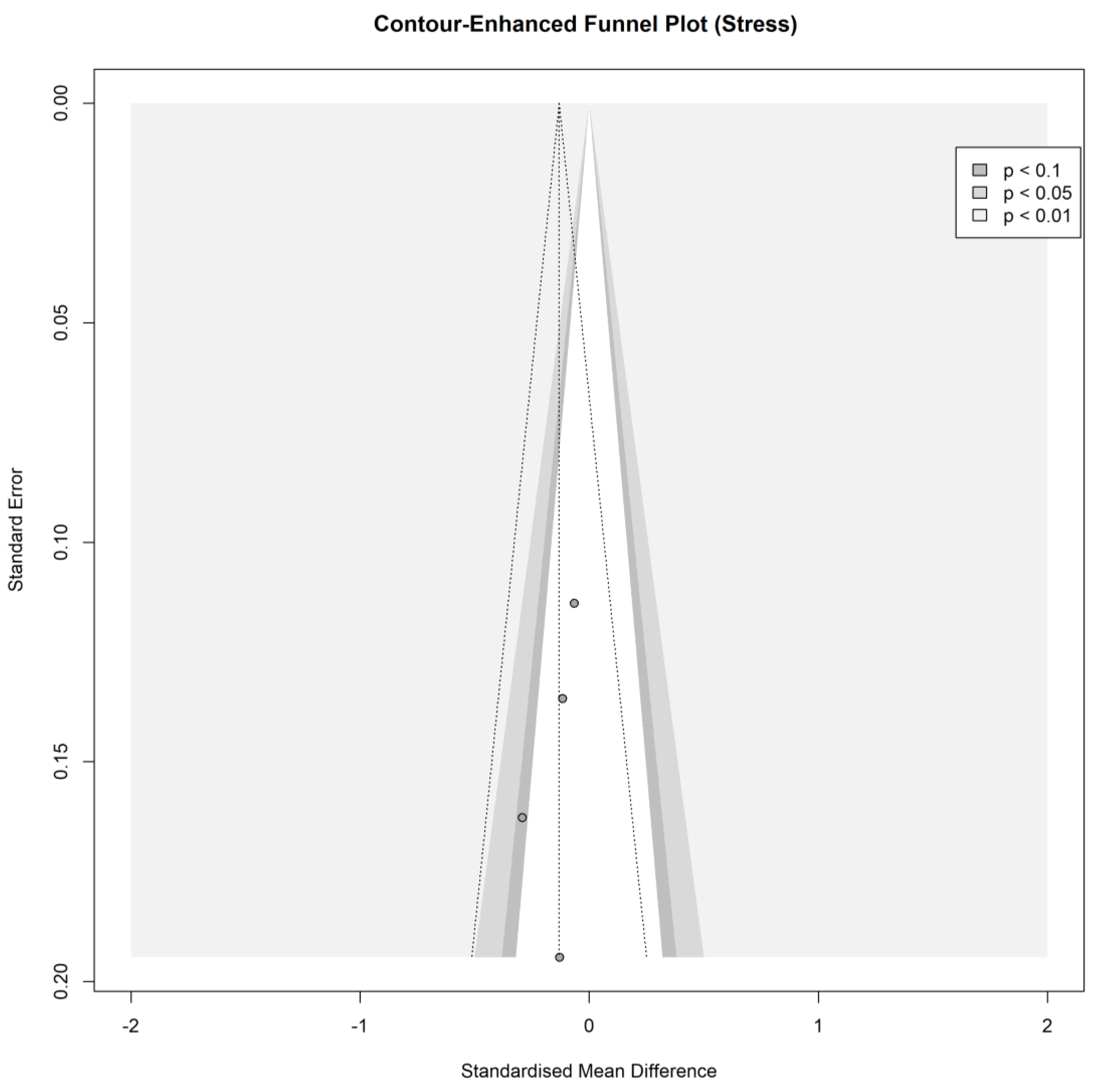
Appendix A.7. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Depressive Symptoms Variable


Appendix A.8. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Anxiety Variable



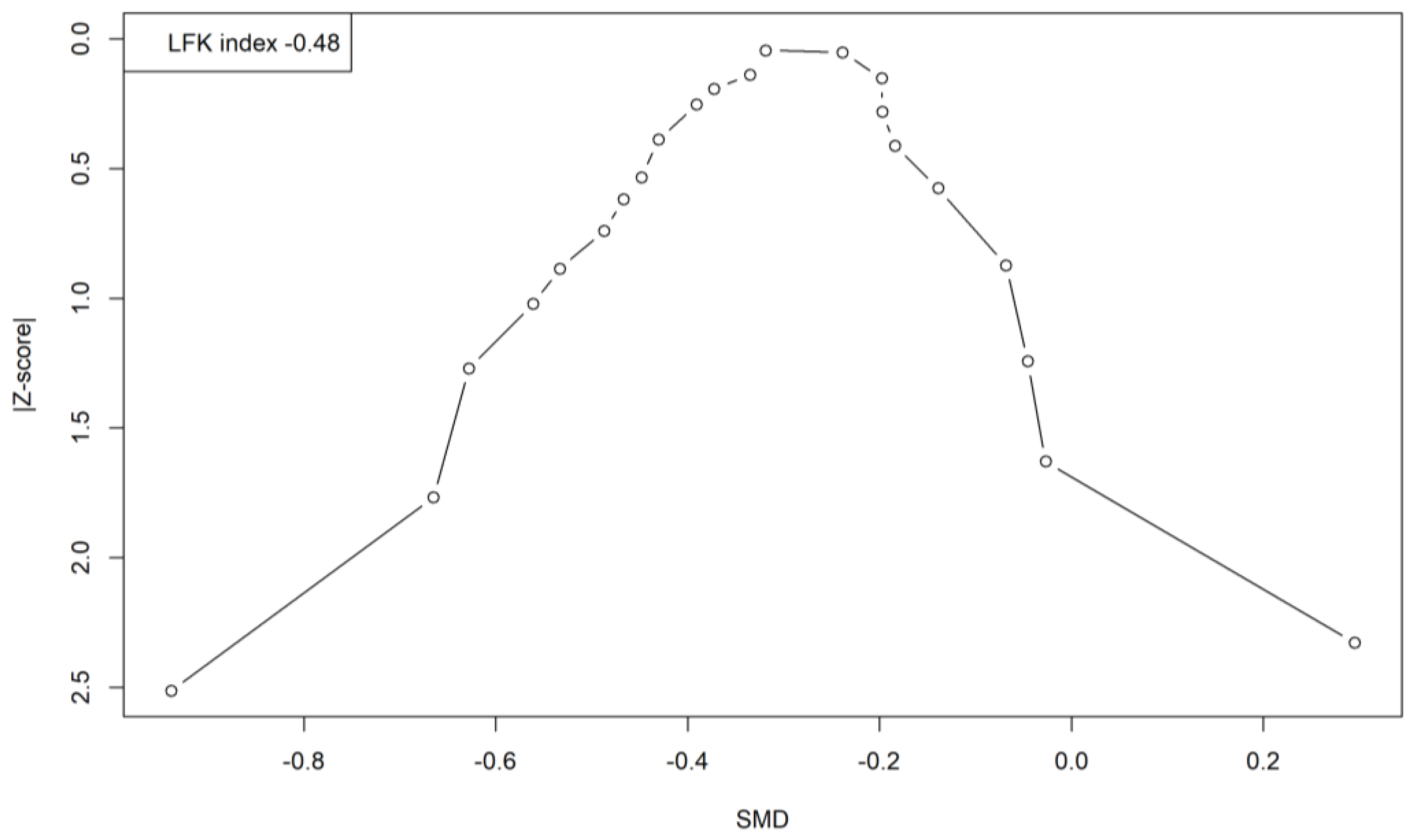
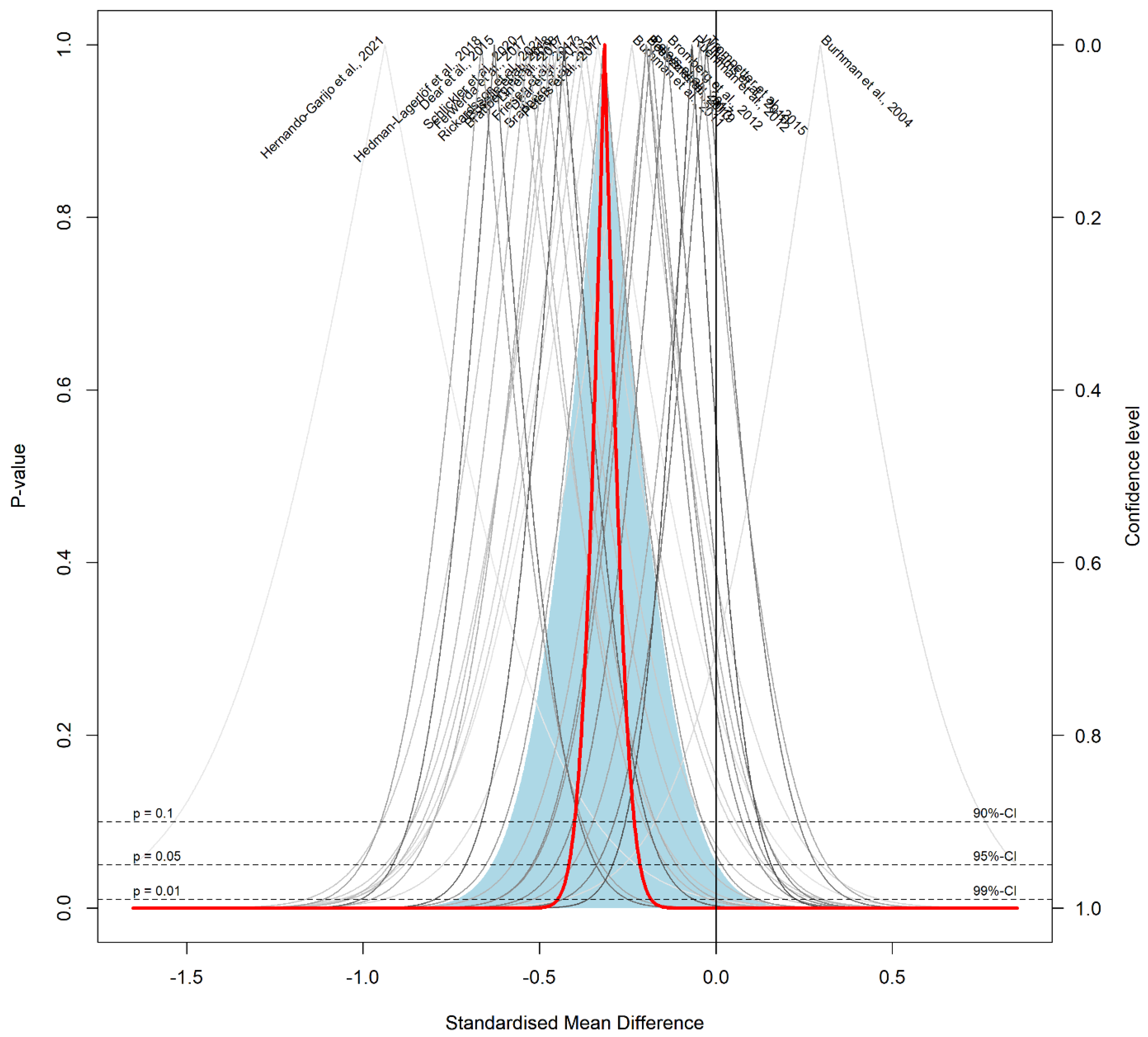
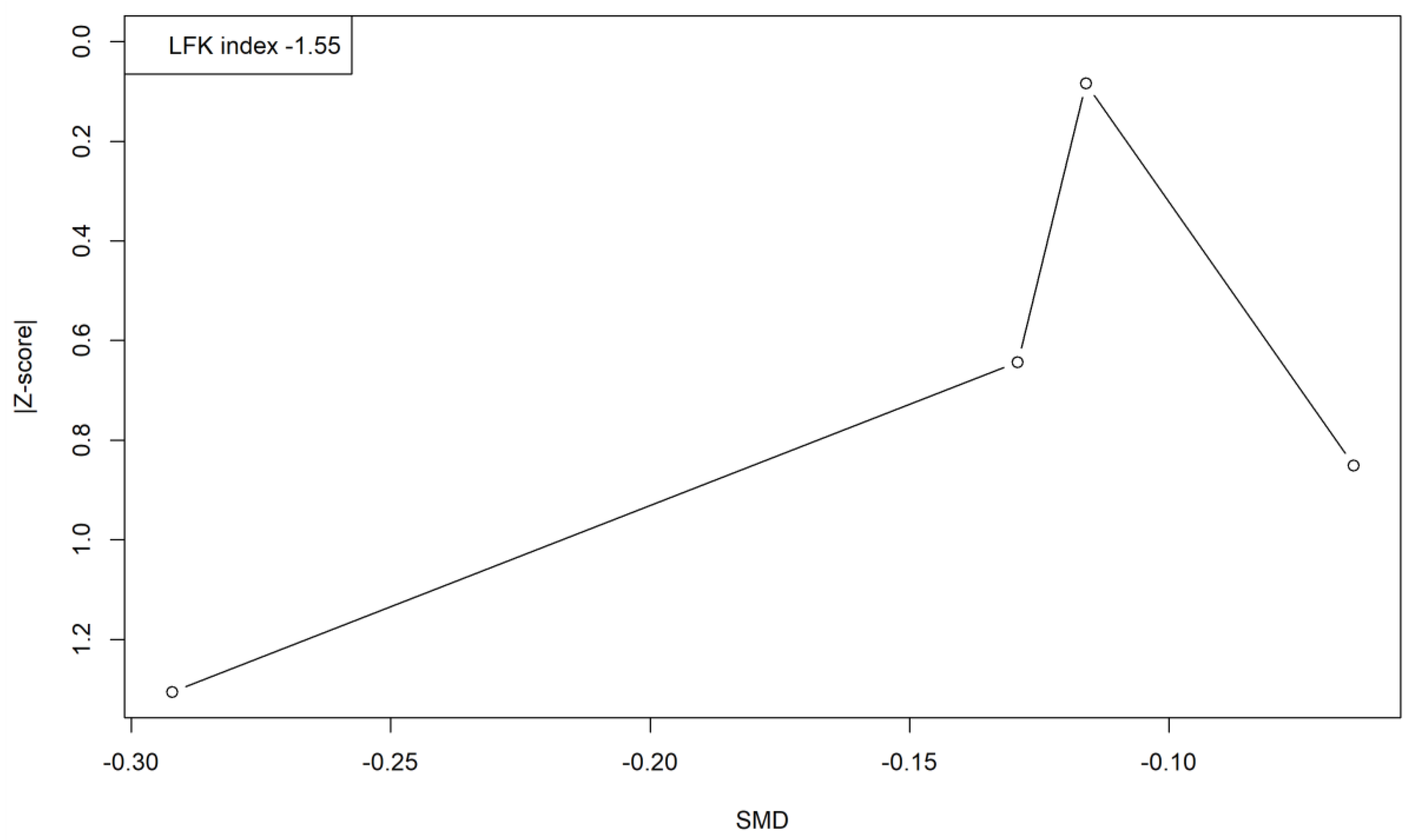
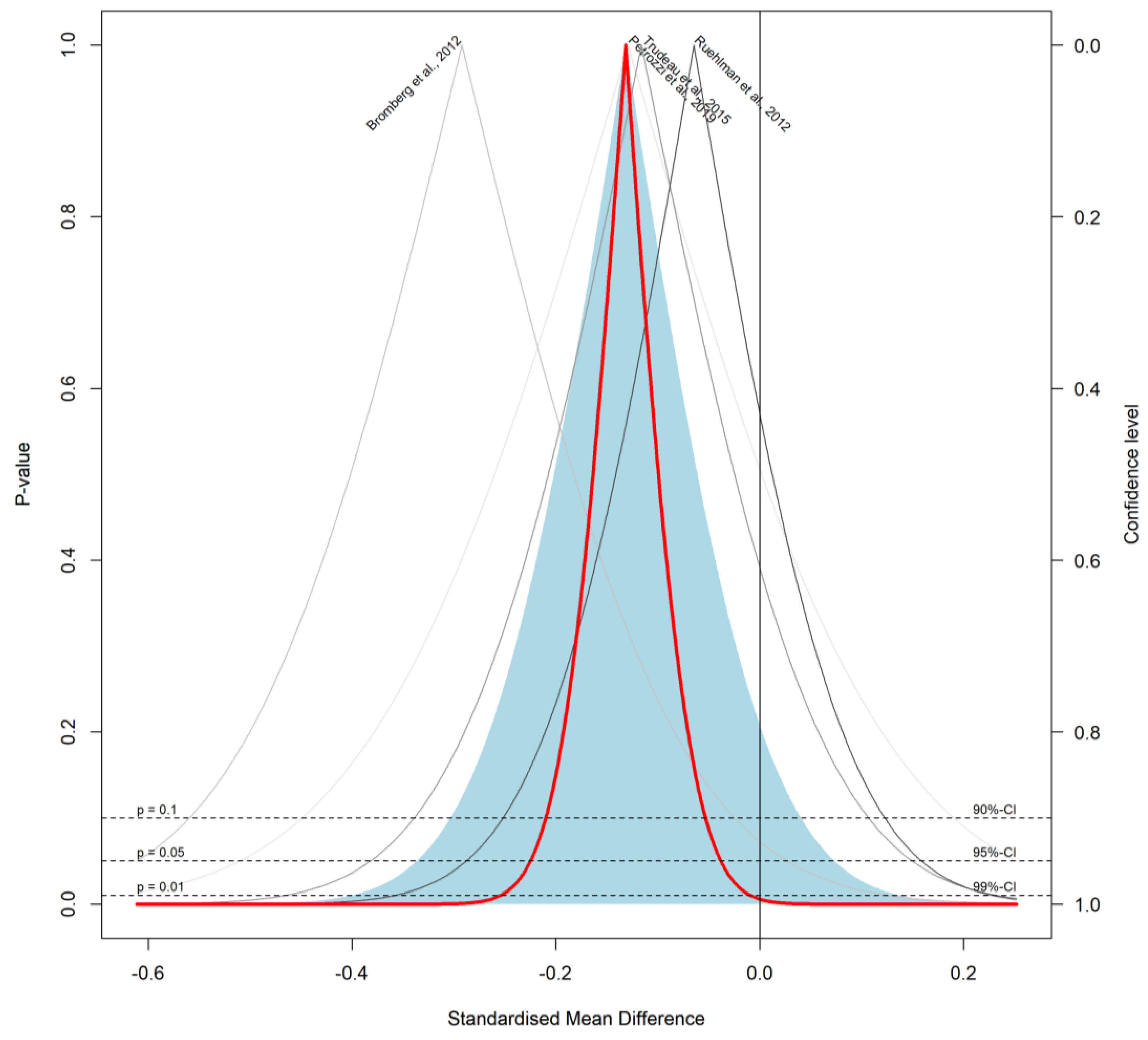
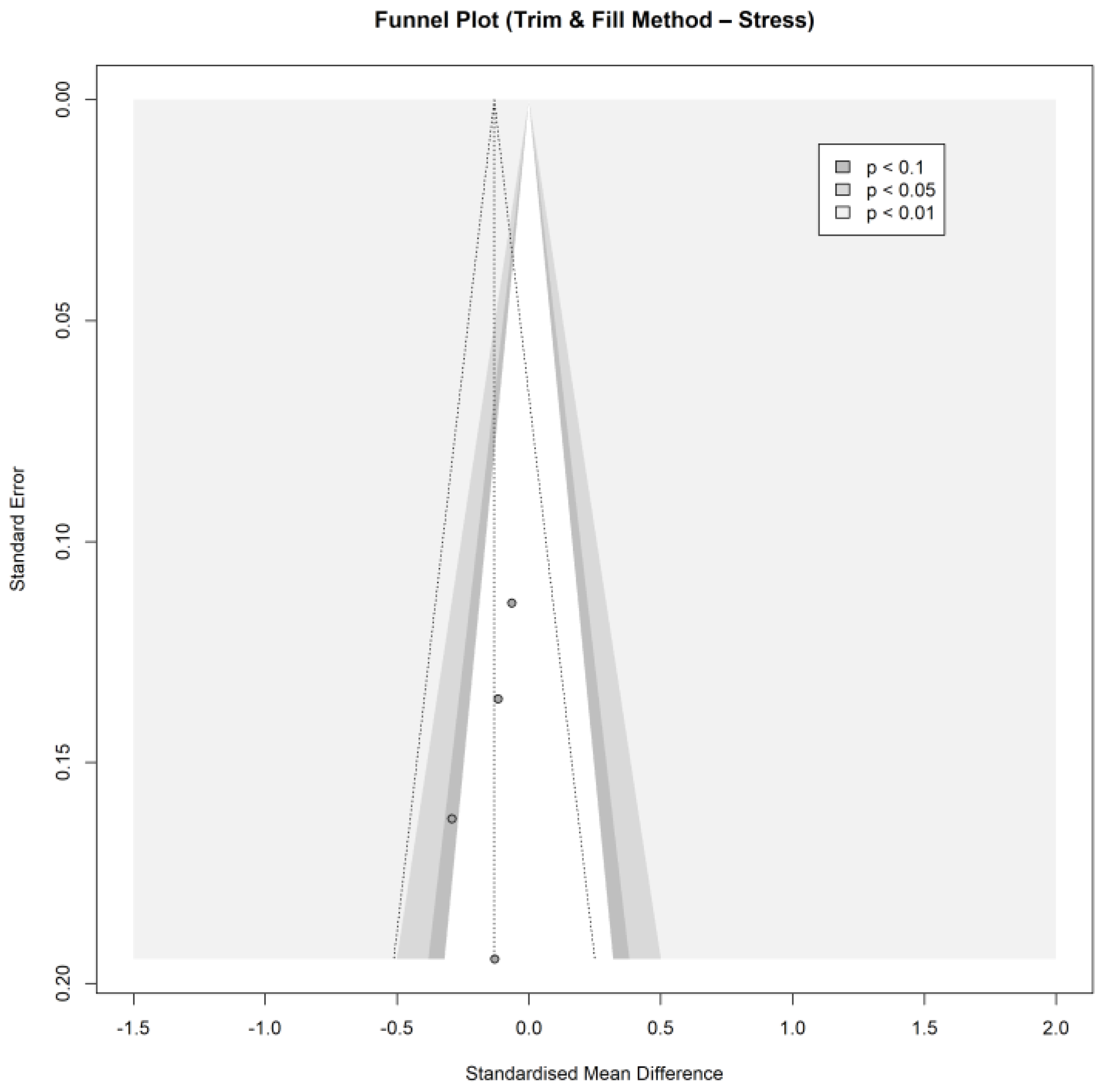
Appendix A.9. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Stress Variable

References
- Clauw, D.J.; Häuser, W.; Cohen, S.P.; Fitzcharles, M.A. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain 2020, 161, 1694–1697. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; Williams, A.C.d.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Fallon, N.; Brown, C.; Twiddy, H.; Brian, E.; Frank, B.; Nurmikko, T.; Stancak, A. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Br. J. Pain 2021, 15, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Pagé, M.G.; Lacasse, A.; Dassieu, L.; Hudspith, M.; Moor, G.; Sutton, K.; Thompson, J.M.; Dorais, M.; Montcalm, A.J.; Sourial, N.; et al. A cross-sectional study of pain status and psychological distress among individuals living with chronic pain: The chronic pain & COVID-19 pan-canadian study. Health Promot. Chronic Dis. Prev. Can. 2021, 41, 141–152. [Google Scholar]
- Arteta, J.; Cobos, B.; Hu, Y.; Jordan, K.; Howard, K. Evaluation of how depression and anxiety mediate the relationship between pain catastrophizing and prescription opioid misuse in a chronic pain population. Pain Med. 2016, 17, 295–303. [Google Scholar] [CrossRef] [Green Version]
- Curtin, K.B.; Norris, D. The relationship between chronic musculoskeletal pain, anxiety and mindfulness: Adjustments to the Fear-Avoidance Model of Chronic Pain. Scand. J. Pain 2017, 17, 156–166. [Google Scholar] [CrossRef]
- Veehof, M.M.; Oskam, M.J.; Schreurs, K.M.G.; Bohlmeijer, E.T. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain 2011, 152, 533–542. [Google Scholar] [CrossRef] [Green Version]
- Williams, A.C.d.C.; Fisher, E.; Hearn, L.; Eccleston, C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2020, 12, CD007407. [Google Scholar] [CrossRef]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-management program for chronic low back pain: A systematic review and meta-analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef]
- Ariza-Mateos, M.J.; Cabrera-Martos, I.; Prados-Román, E.; Granados-Santiago, M.; Rodríguez-Torres, J.; Carmen Valenza, M. A systematic review of internet-based interventions for women with chronic pain. Br. J. Occup. Ther. 2020, 84, 6–14. [Google Scholar] [CrossRef]
- White, V.; Linardon, J.; Stone, J.E.; Holmes-Truscott, E.; Olive, L.; Mikocka-Walus, A.; Hendrieckx, C.; Evans, S.; Speight, J. Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2020, 52, 1–26. [Google Scholar] [CrossRef]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The Role of Google Scholar in Evidence Reviews and Its Applicability to Grey Literature Searching. PLoS ONE 2015, 10, e0138237. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0[M]; Wiley-Blackwell: Hoboken, NJ, USA, 2008. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Hariohm, K.; Prakash, V.; Saravankumar, J. Quantity and quality of randomized controlled trials published by Indian physiotherapists. Perspect. Clin. Res. 2015, 6, 91. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. An Application of Hierarchical Kappa-type Statistics in the Assessment of Majority Agreement among Multiple Observers. Biometrics 1977, 33, 363. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE Working Group GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [Green Version]
- Andrews, J.; Guyatt, G.; Oxman, A.D.; Alderson, P.; Dahm, P.; Falck-Ytter, Y.; Nasser, M.; Meerpohl, J.; Post, P.N.; Kunz, R.; et al. GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. J. Clin. Epidemiol. 2013, 66, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- RStudio Team RStudio: Integrated Development Environment for R. 2021. Available online: https://support.rstudio.com/hc/en-us/articles/206212048-Citing-RStudio (accessed on 10 February 2022).
- R Core Team R: A Language and Environment for Statistical Computing. 2021. Available online: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006 (accessed on 10 February 2022).
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Li, T.; Deeks, J.J. 6.5.2.3 Obtaining Standard Deviations from Standard Errors, Confidence Intervals, T Statistics and p Values for Differences in Means. Available online: https://training.cochrane.org/handbook/current/chapter-06 (accessed on 10 February 2022).
- Viechtbauer, W. Bias and Efficiency of Meta-Analytic Variance Estimators in the Random-Effects Model. J. Educ. Behav. Stat. 2005, 30, 261–293. [Google Scholar] [CrossRef]
- Veroniki, A.A.; Jackson, D.; Viechtbauer, W.; Bender, R.; Bowden, J.; Knapp, G.; Kuss, O.; Higgins, J.P.T.; Langan, D.; Salanti, G. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res. Synth. Methods 2016, 7, 55–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knapp, G.; Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 2003, 22, 2693–2710. [Google Scholar] [CrossRef]
- Sidik, K.; Jonkman, J.N. A simple confidence interval for meta-analysis. Stat. Med. 2002, 21, 3153–3159. [Google Scholar] [CrossRef]
- Hoaglin, D. Misunderstandings about Q and “Cochran’s Q test” in meta-analysis. Stat. Med. 2016, 35, 485–495. [Google Scholar] [CrossRef]
- Borenstein, M.; Higgins, J.P.T.; Hedges, L.V.; Rothstein, H.R. Basics of meta-analysis: I(2) is not an absolute measure of heterogeneity. Res. Synth. Methods 2017, 8, 5–18. [Google Scholar] [CrossRef] [Green Version]
- IntHout, J.; Ioannidis, J.P.A.; Rovers, M.M.; Goeman, J.J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 2016, 6, e010247. [Google Scholar] [CrossRef] [Green Version]
- Viechtbauer, W.; Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 2010, 1, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Rücker, G.; Schwarzer, G. Beyond the forest plot: The drapery plot. Res. Synth. Methods 2021, 12, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Doi, S.A. Rendering the Doi plot properly in meta-analysis. Int. J. Evid. Based. Healthc. 2018, 16, 242–243. [Google Scholar] [CrossRef] [PubMed]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based. Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis With R: A Hands-On Guide, 1st ed.; Chapman & Hall: Boca Raton, FL, USA; CRC Press: London, UK, 2021; ISBN 978-0-367-61007-4. [Google Scholar]
- Amorim, A.B.; Pappas, E.; Simic, M.; Ferreira, M.L.; Jennings, M.; Tiedemann, A.; Carvalho-E-Silva, A.P.; Caputo, E.; Kongsted, A.; Ferreira, P.H. Integrating Mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): A pilot randomised controlled trial. BMC Musculoskelet. Disord. 2019, 20, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Ang, D.C.; Chakr, R.; Mazzuca, S.; France, C.R.; Steiner, J.; Stump, T. Cognitive-behavioral therapy attenuates nociceptive responding in patients with fibromyalgia: A pilot study. Arthritis Care Res. 2010, 62, 618–623. [Google Scholar] [CrossRef]
- Dear, B.F.; Gandy, M.; Karin, E.; Staples, L.G.; Johnston, L.; Fogliati, V.J.; Wootton, B.M.; Terides, M.D.; Kayrouz, R.; Perry, K.N.; et al. The Pain Course: A randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain 2015, 156, 1920–1935. [Google Scholar] [CrossRef]
- Devineni, T.; Blanchard, E.B. A randomized controlled trial of an internet-based treatment for chronic headache. Behav. Res. Ther. 2005, 43, 277–292. [Google Scholar] [CrossRef]
- Ferwerda, M.; Van Beugen, S.; Van Middendorp, H.; Spillekom-Van Koulil, S.; Donders, A.R.T.; Visser, H.; Taal, E.; Creemers, M.C.W.; Van Riel, P.C.L.M.; Evers, A.W.M. A tailored-guided internet-based cognitive-behavioral intervention for patients with rheumatoid arthritis as an adjunct to standard rheumatological care: Results of a randomized controlled trial. Pain 2017, 158, 868–878. [Google Scholar] [CrossRef]
- Friesen, L.N.; Hadjistavropoulos, H.D.; Schneider, L.H.; Alberts, N.M.; Titov, N.; Dear, B.F. Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: A randomized controlled trial. Pain 2017, 158, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Heapy, A.A.; Higgins, D.M.; Goulet, J.L.; La Chappelle, K.M.; Driscoll, M.A.; Czlapinski, R.A.; Buta, E.; Piette, J.D.; Krein, S.L.; Kerns, R.D. Interactive voice response-based self-management for chronic back Pain: The Copes noninferiority randomized trial. JAMA Intern. Med. 2017, 177, 765–773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedman-Lagerlöf, M.; Hedman-Lagerlöf, E.; Axelsson, E.; Ljotsson, B.; Engelbrektsson, J.; Hultkrantz, S.; Lundbäck, K.; Björkander, D.; Wicksell, R.K.; Flink, I.; et al. Internet-Delivered Exposure Therapy for Fibromyalgia A Randomized Controlled Trial. Clin. J. Pain 2018, 34, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Hernando-Garijo, I.; Ceballos-Laita, L.; Mingo-Gómez, M.T.; Medrano-De-la-fuente, R.; Estébanez-De-miguel, E.; Martínez-Pérez, M.N.; Jiménez-Del-barrio, S. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int. J. Environ. Res. Public Health 2021, 18, 2075. [Google Scholar]
- Juhlin, S.; Bergenheim, A.; Gjertsson, I.; Larsson, A.; Mannerkorpi, K. Physical activity with person-centred guidance supported by a digital platform for persons with chronic widespread pain: A randomized controlled trial. J. Rehabil. Med. 2021, 53, jrm00175. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Paganini, S.; Sander, L.; Lüking, M.; Daniel Ebert, D.; Buhrman, M.; Andersson, G.; Baumeister, H. An Internet-based intervention for chronic pain—A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Dtsch. Arztebl. Int. 2017, 114, 681–688. [Google Scholar] [PubMed] [Green Version]
- Moessner, M.; Schiltenwolf, M.; Neubauer, E. Internet-based aftercare for patients with back pain-A pilot study. Telemed. e-Health 2012, 18, 413–419. [Google Scholar] [CrossRef]
- Berman, R.L.H.; Iris, M.A.; Bode, R.; Drengenberg, C. The Effectiveness of an Online Mind-Body Intervention for Older Adults with Chronic Pain. J. Pain 2009, 10, 68–79. [Google Scholar] [CrossRef]
- Peters, M.L.; Smeets, E.; Feijge, M.; Van Breukelen, G.; Andersson, G.; Buhrman, M.; Linton, S.J. Happy Despite Pain: A Randomized Controlled Trial of an 8-Week Internet-delivered Positive Psychology Intervention for Enhancing Well-being in Patients with Chronic Pain. Clin. J. Pain 2017, 33, 962–975. [Google Scholar] [CrossRef] [Green Version]
- Petrozzi, M.J.; Leaver, A.; Ferreira, P.H.; Rubinstein, S.M.; Jones, M.K.; Mackey, M.G. Addition of MoodGYM to physical treatments for chronic low back pain: A randomized controlled trial. Chiropr. Man. Ther. 2019, 27, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Rickardsson, J.; Gentili, C.; Holmström, L.; Zetterqvist, V.; Andersson, E.; Persson, J.; Lekander, M.; Ljótsson, B.; Wicksell, R.K. Internet-delivered acceptance and commitment therapy as microlearning for chronic pain: A randomized controlled trial with 1-year follow-up. Eur. J. Pain 2021, 25, 1012–1030. [Google Scholar] [CrossRef] [PubMed]
- Shigaki, C.L.; Smarr, K.L.; Siva, C.; Ge, B.; Musser, D.; Johnson, R. RAHelp: An online intervention for individuals with rheumatoid arthritis. Arthritis Care Res. 2013, 65, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Simister, H.D.; Tkachuk, G.A.; Shay, B.L.; Vincent, N.; Pear, J.J.; Skrabek, R.Q. Randomized Controlled Trial of Online Acceptance and Commitment Therapy for Fibromyalgia. J. Pain 2018, 19, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Faux, S.G.; Gardner, T.; Hobbs, M.J.; James, M.A.; Joubert, A.E.; Kladnitski, N.; Newby, J.M.; Schultz, R.; Shiner, C.T.; et al. Reboot Online: A Randomized Controlled Trial Comparing an Online Multidisciplinary Pain Management Program with Usual Care for Chronic Pain. Pain Med. 2019, 20, 2385–2396. [Google Scholar] [CrossRef] [PubMed]
- Ström, L.; Pettersson, R.; Andersson, G. A controlled trial of self-help treatment of recurrent headache conducted via the Internet. J. Consult. Clin. Psychol. 2000, 68, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Tavallaei, V.; Rezapour-Mirsaleh, Y.; Rezaiemaram, P.; Saadat, S.H. Mindfulness for female outpatients with chronic primary headaches: An internet-based bibliotherapy. Eur. J. Transl. Myol. 2018, 28, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Trudeau, K.J.; Pujol, L.A.; DasMahapatra, P.; Wall, R.; Black, R.A.; Zacharoff, K. A randomized controlled trial of an online self-management program for adults with arthritis pain. J. Behav. Med. 2015, 38, 483–496. [Google Scholar] [CrossRef] [Green Version]
- Vallejo, M.A.; Ortega, J.; Rivera, J.; Comeche, M.I.; Vallejo-Slocker, L. Internet versus face-to-face group cognitive-behavioral therapy for fibromyalgia: A randomized control trial. J. Psychiatr. Res. 2015, 68, 106–113. [Google Scholar] [CrossRef]
- Bossen, D.; Veenhof, C.; van Beek, K.E.; Spreeuwenberg, P.M.; Dekker, J.; de Bakker, D.H. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e257. [Google Scholar] [CrossRef]
- Westenberg, R.F.; Zale, E.L.; Heinhuis, T.J.; Ozkan, S.; Nazzal, A.; Lee, S.G.; Chen, N.C.; Vranceanu, A.M. Does a brief mindfulness exercise improve outcomes in upper extremity patients? A randomized controlled trial. Clin. Orthop. Relat. Res. 2018, 476, 790–798. [Google Scholar] [CrossRef]
- Williams, D.A.; Kuper, D.; Segar, M.; Mohan, N.; Sheth, M.; Clauw, D.J. Internet-enhanced management of fibromyalgia: A randomized controlled trial. Pain 2010, 151, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.; Roll, J.M.; Corbett, C.; Barbosa-Leiker, C. Empowering Patients with Persistent Pain Using an Internet-based Self-Management Program. Pain Manag. Nurs. 2015, 16, 503–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, M.; Finlay, M.; Orr, M.; Barbosa-Leiker, C.; Sherazi, N.; Roberts, M.L.A.; Layton, M.; Roll, J.M. Engagement in online pain self-management improves pain in adults on medication-assisted behavioral treatment for opioid use disorders. Addict. Behav. 2018, 86, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Ruehlman, L.S.; Karoly, P.; Enders, C. A randomized controlled evaluation of an online chronic pain self management program. Pain 2012, 153, 319–330. [Google Scholar] [CrossRef] [Green Version]
- Sander, L.B.; Paganini, S.; Terhorst, Y.; Schlicker, S.; Lin, J.; Spanhel, K.; Buntrock, C.; Ebert, D.D.; Baumeister, H. Effectiveness of a Guided Web-Based Self-help Intervention to Prevent Depression in Patients with Persistent Back Pain: The PROD-BP Randomized Clinical Trial. JAMA Psychiatry 2020, 77, 1001–1011. [Google Scholar] [CrossRef]
- Trompetter, H.R.; Bohlmeijer, E.T.; Veehof, M.M.; Schreurs, K.M.G. Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: A randomized controlled trial. J. Behav. Med. 2015, 38, 66–80. [Google Scholar] [CrossRef]
- Schlicker, S.; Baumeister, H.; Buntrock, C.; Sander, L.; Paganini, S.; Lin, J.; Berking, M.; Lehr, D.; Ebert, D.D. A web- and mobile-based intervention for comorbid, recurrent depression in patients with chronic back pain on sick leave (get.back): Pilot randomized controlled trial on feasibility, user satisfaction, and effectiveness. JMIR Ment. Health 2020, 7, e16398. [Google Scholar] [CrossRef] [Green Version]
- Scott, W.; Chilcot, J.; Guildford, B.; Daly-Eichenhardt, A.; McCracken, L.M. Feasibility randomized-controlled trial of online Acceptance and Commitment Therapy for patients with complex chronic pain in the United Kingdom. Eur. J. Pain 2018, 22, 1473–1484. [Google Scholar] [CrossRef]
- Boselie, J.J.L.M.; Vancleef, L.M.G.; Peters, M.L. Filling the glass: Effects of a positive psychology intervention on executive task performance in chronic pain patients. Eur. J. Pain 2018, 22, 1268–1280. [Google Scholar] [CrossRef] [Green Version]
- Brattberg, G. Internet-based rehabilitation for individuals with chronic pain and burnout II: A long-term follow-up. Int. J. Rehabil. Res. 2007, 30, 231–234. [Google Scholar] [CrossRef]
- Herbert, M.S.; Afari, N.; Liu, L.; Heppner, P.; Rutledge, T.; Williams, K.; Eraly, S.; VanBuskirk, K.; Nguyen, C.; Bondi, M.; et al. Telehealth Versus In-Person Acceptance and Commitment Therapy for Chronic Pain: A Randomized Noninferiority Trial. J. Pain 2017, 18, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Brattberg, G. Self-administered EFT (Emotional Freedom Techniques) in individuals with fibromyalgia: A randomized trial. Integr. Med. 2008, 7, 30–35. [Google Scholar]
- Bromberg, J.; Wood, M.E.; Black, R.A.; Surette, D.A.; Zacharoff, K.L.; Chiauzzi, E.J. A randomized trial of a web-based intervention to improve migraine self-management and coping. Headache 2012, 52, 244–261. [Google Scholar] [CrossRef] [PubMed]
- Buhrman, M.; Fältenhag, S.; Ström, L.; Andersson, G. Controlled trial of Internet-based treatment with telephone support for chronic back pain. Pain 2004, 111, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Buhrman, M.; Nilsson-Ihrfelt, E.; Jannert, M.; Ström, L.; Andersson, G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: A randomized controlled trial. J. Rehabil. Med. 2011, 43, 500–505. [Google Scholar] [PubMed] [Green Version]
- Dear, B.F.; Titov, N.; Perry, K.N.; Johnston, L.; Wootton, B.M.; Terides, M.D.; Rapee, R.M.; Hudson, J.L. The Pain Course: A randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain 2013, 154, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Varker, T.; Brand, R.; Ward, J.; Terhaag, S.; Phelps, A. Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: A rapid evidence assessment. Psychol. Serv. 2019, 16, 621–635. [Google Scholar] [CrossRef]
- McCall, T.; Bolton, C.S., III; Carlson, R.; Khairat, S. A systematic review of telehealth interventions for managing anxiety and depression in African American adults. mHealth 2021, 7, 31. [Google Scholar] [CrossRef]
- De Boer, M.J.; Versteegen, G.J.; Vermeulen, K.M.; Sanderman, R.; Struys, M.M.R.F. A randomized controlled trial of an Internet-based cognitive-behavioural intervention for non-specific chronic pain: An effectiveness and cost-effectiveness study. Eur. J. Pain 2014, 18, 1440–1451. [Google Scholar] [CrossRef] [Green Version]
- Aspvall, K.; Sampaio, F.; Lenhard, F.; Melin, K.; Norlin, L.; Serlachius, E.; Mataix-Cols, D.; Andersson, E. Cost-effectiveness of Internet-Delivered vs In-Person Cognitive Behavioral Therapy for Children and Adolescents with Obsessive-Compulsive Disorder. JAMA Netw. Open 2021, 4, 1–13. [Google Scholar] [CrossRef] [PubMed]


| Outcomes Sub = Analysis | N Studies | SMD | Lower Limit 95%CI | Upper Limit 95% CI | Q | I2 |
|---|---|---|---|---|---|---|
| (a) Depressive Symptoms—Treatment | ||||||
| ACT | 5 | −0.39 | −0.71 | −0.07 | 6.38 | 37% |
| CBT | 11 | −0.46 | −0.73 | −0.19 | 29.21 | 66% |
| Positive Psychology | 2 | −0.61 | −1.77 | 0.55 | 0.45 | 0% |
| Self-management | 8 | −0.12 | −0.26 | 0.03 | 6.30 | 0% |
| Other types of treatment | 7 | −0.30 | −0.58 | −0.03 | 11.19 | 46% |
| Depressive Symptoms—Chronic Musculoskeletal disorder | ||||||
| Back pain | 5 | −0.24 | −0.53 | 0.05 | 5.58 | 28% |
| Fibromyalgia | 7 | −0.66 | −1.01 | −0.31 | 14.16 | 58% |
| Headache | 3 | −0.14 | −0.19 | −0.09 | 0.02 | 0% |
| Rheumatic disorders | 4 | −0.28 | −0.68 | 0.12 | 5.85 | 49% |
| Unspecified chronic pain | 13 | −0.33 | −0.51 | −0.15 | 36.61 | 65% |
| Depressive Symptoms—Added to usual care treatment? (Y/N) | ||||||
| Only e-BMT | 24 | −0.34 | −0.46 | −0.22 | 52.26 | 54% |
| e-BMT added to usual care | 8 | −0.41 | −0.80 | −0.03 | 21.79 | 68% |
| Depressive Symptoms—Intervention duration | ||||||
| Between 1 and 6 weeks | 6 | −0.02 | −0.17 | 0.12 | 2.44 | 0% |
| Between 7 and 11 weeks | 18 | −0.46 | −0.61 | −0.31 | 36.70 | 51% |
| 12 weeks and more | 8 | −0.26 | −0.50 | −0.03 | 12.54 | 44% |
| Depressive Symptoms—Methodological Quality according to the PEDro scale | ||||||
| Fair methodological quality | 7 | −0.18 | −0.43 | 0.07 | 10.86 | 45% |
| Good methodological quality | 25 | −0.39 | −0.52 | −0.26 | 54.08 | 54% |
| (b) Anxiety—Treatment | ||||||
| ACT | 3 | −0.31 | −0.93 | 0.31 | 4.75 | 58% |
| CBT | 10 | −0.31 | −0.50 | −0.12 | 14.71 | 39% |
| Positive psychology | 2 | −0.37 | -1.28 | 0.53 | 0.28 | 0% |
| Self-Management | 3 | −0.20 | −0.70 | 0.30 | 2.34 | 15% |
| Other types of treatment | 4 | −0.41 | −0.97 | 0.14 | 8.43 | 64% |
| Anxiety—Chronic Musculoskeletal disorder | ||||||
| Unspecific back pain | 3 | −0.09 | −0.75 | 0.58 | 2.43 | 18% |
| Fibromyalgia | 5 | −0.45 | −0.85 | −0.05 | 8.17 | 51% |
| Headache | 1 | −0.14 | −0.85 | 0.18 | N/A | N/A |
| Rheumatic disorders | 2 | −0.35 | -2.47 | 1.77 | 1.67 | 40% |
| Unspecified chronic pain | 10 | −0.33 | −0.47 | −0.19 | 16.12 | 38% |
| Anxiety—Intervention duration | ||||||
| 1 to 6 weeks | 2 | 0.02 | -1.96 | 2.01 | 1.41 | 29% |
| 7 to 11 weeks | 13 | −0.41 | −0.50 | −0.31 | 10.34 | 0% |
| 12 weeks and more | 6 | −0.25 | −0.56 | 0.06 | 9.13 | 45% |
| Anxiety—Added to usual care treatment? (Y/N) | ||||||
| Only e-BMT | 17 | −0.34 | −0.45 | −0.22 | 26.85 | 37% |
| e-BMT added to usual care | 4 | −0.19 | −0.59 | 0.22 | 4.95 | 39% |
| Anxiety—Methodological Quality according to the PEDro scale | ||||||
| Fair methodological quality | 5 | −0.18 | −0.40 | 0.04 | 6.61 | 24% |
| Good methodological quality | 16 | −0.37 | −0.49 | −0.24 | 22.28 | 33% |
| Certainty Assessment | No. of Participants | Effect | Certainty | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome (No. of Studies) | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | e-BMT | Control | Absolute (95% CI) | |
| Depressive symptoms (n = 32) | RCT | Serious | Serious | Not serious | Not serious | Not serious | 1843 | 1688 | −0.35 (−0.46; −0.24) | Low ⊕⊕ |
| Anxiety (n = 21) | RCT | Serious | Not Serious | Not serious | Not serious | Not serious | 1412 | 1166 | −0.32 (−0.42; −0.21) | Moderate ⊕⊕⊕ |
| Stress (n = 4) | RCT | Serious | Not serious | Not serious | Not serious | Not serious | 399 | 390 | −0.13 (−0.28; 0.02) | Moderate ⊕⊕⊕ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuenca-Martínez, F.; Suso-Martí, L.; Herranz-Gómez, A.; Varangot-Reille, C.; Calatayud, J.; Romero-Palau, M.; Blanco-Díaz, M.; Salar-Andreu, C.; Casaña, J. Effectiveness of Telematic Behavioral Techniques to Manage Anxiety, Stress and Depressive Symptoms in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3231. https://doi.org/10.3390/ijerph19063231
Cuenca-Martínez F, Suso-Martí L, Herranz-Gómez A, Varangot-Reille C, Calatayud J, Romero-Palau M, Blanco-Díaz M, Salar-Andreu C, Casaña J. Effectiveness of Telematic Behavioral Techniques to Manage Anxiety, Stress and Depressive Symptoms in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(6):3231. https://doi.org/10.3390/ijerph19063231
Chicago/Turabian StyleCuenca-Martínez, Ferran, Luis Suso-Martí, Aida Herranz-Gómez, Clovis Varangot-Reille, Joaquín Calatayud, Mario Romero-Palau, María Blanco-Díaz, Cristina Salar-Andreu, and Jose Casaña. 2022. "Effectiveness of Telematic Behavioral Techniques to Manage Anxiety, Stress and Depressive Symptoms in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 6: 3231. https://doi.org/10.3390/ijerph19063231
APA StyleCuenca-Martínez, F., Suso-Martí, L., Herranz-Gómez, A., Varangot-Reille, C., Calatayud, J., Romero-Palau, M., Blanco-Díaz, M., Salar-Andreu, C., & Casaña, J. (2022). Effectiveness of Telematic Behavioral Techniques to Manage Anxiety, Stress and Depressive Symptoms in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(6), 3231. https://doi.org/10.3390/ijerph19063231










