Abstract
Background and aim: Ever since the discovery of tumor-associated immune cells, there has been growing interest in the understanding of the mechanisms underlying the crosstalk between these cells and tumor cells. A “seed and soil” approach has been recently introduced to describe the glioblastoma (GBM) landscape: tumor microenvironments act as fertile “soil” and interact with the “seed” (glial and stem cells compartment). In the following article, we provide a systematic review of the current evidence pertaining to the characterization of glioma-associated macrophages and microglia (GAMs) and microglia and macrophage cells in the glioma tumor microenvironment (TME). Methods: An online literature search was launched on PubMed Medline and Scopus using the following research string: “((Glioma associated macrophages OR GAM OR Microglia) AND (glioblastoma tumor microenvironment OR TME))”. The last search for articles pertinent to the topic was conducted in February 2022. Results: The search of the literature yielded a total of 349 results. A total of 235 studies were found to be relevant to our research question and were assessed for eligibility. Upon a full-text review, 58 articles were included in the review. The reviewed papers were further divided into three categories based on their focus: (1) Microglia maintenance of immunological homeostasis and protection against autoimmunity; (2) Microglia crosstalk with dedifferentiated and stem-like glioblastoma cells; (3) Microglia migratory behavior and its activation pattern. Conclusions: Aggressive growth, inevitable recurrence, and scarce response to immunotherapies are driving the necessity to focus on the GBM TME from a different perspective to possibly disentangle its role as a fertile ‘soil’ for tumor progression and identify within it feasible therapeutic targets. Against this background, our systematic review confirmed microglia to play a paramount role in promoting GBM progression and relapse after treatments. The correct and extensive understanding of microglia–glioma crosstalk could help in understanding the physiopathology of this complex disease, possibly opening scenarios for improvement of treatments.
1. Introduction
Ever since the discovery of tumor-associated immune cells, there has been growing interest in the understanding of the mechanisms underlying the crosstalk between these cells and tumor cells, which can range from conferring a growth advantage to the latter to enabling the cancer cells to escape autoimmunity. To achieve this, a significant effort has been made to define the types and characteristics of the cells constituting the tumor microenvironment (TME) and to characterize how these cells assist the tumor cells by producing cytokines, chemokines, growth factors, and triggering the release of inhibitory immune checkpoint proteins from T cells.
Gliomas, with emphasis on glioblastomas (GBMs), are no exception and they present a wide range of glioma-associated macrophage and microglia (GAMs). Extensive literature in this field has been published to gain a better understanding of the composition of the TME and of the role that resident microglia and immune cells from peripheral blood play in ensuring an immunosuppressive environment in which the tumor can thrive undisturbed.
The nature of the TME shapes both therapeutic responses and resistance, justifying the recent impetus to target its components. Despite the growing body of evidence on the topic, many aspects are yet to be explored in the field. Open questions are related to microglia distribution in the peritumoral area, its spatial and molecular interaction with GBM infiltrative margins and stem cell compartment, and the real extension of the so-called TME with respect to the tumoral core. A correct and extensive understanding of microglia–glioma crosstalk could help in understanding the physiopathology of this complex disease, possibly opening scenarios for improvement of treatments. An immunosuppressive pressure acts on the microglia and macrophage towards a polarization to an M2 protumor-immunosuppressive cellular phenotype. However, it is not ultimately clear to what extent an M2 macrophage distribution is capable of maintaining an immunologically downregulated environment.
A “seed and soil” approach has been recently introduced to describe the GBM landscape: the tumor microenvironment acts as fertile “soil” interacting with the “seed” (glial and stem cells compartment). Microenvironmental contribution seems critical to gaining a better understanding of the unique challenges GBM poses and could be pivotal in:
- (a)
- developing new treatments targeting GAMs, thus rendering the tumor once again targetable by host immunity, and slowing its progression and aggressiveness by inhibiting the microglia and tumor cell crosstalk
- (b)
- defining the hystotypes of the tumor and degree of response to treatment based on the GAMs composition and infiltration pattern.
In the following article, we provide a systematic review of the current evidence pertaining to the characterization of GAMs and microglia, and macrophage cells in the glioma TME.
2. Methods
This study was conducted in accordance with the PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) guidelines. An online literature search was launched on PubMed Medline and Scopus using the following research string: “((Glioma associated macrophages OR GAM OR Microglia) AND (glioblastoma tumor microenvironment OR TME))”. The last search for articles pertinent to the topic was conducted in February 2022. Two authors, C.M.D. and G.M., independently conducted the abstract screening for eligibility. Any discordance was solved by consensus with a third, senior author, G.D.P. No restrictions on the date of publication were made. Exclusion criteria were as follows: no comparative study design, studies published in languages other than English, and metaanalysis. A systematic abstract screening of the references (forward search) was performed to identify additional records.
3. Results
The search of the literature yielded a total of 349 results. Duplicate records were then removed (n = 10), via title and abstract screening; 235 studies were found to be relevant to our research question and were assessed for eligibility (Figure 1). Upon a full-text review, 58 articles were included in the review.
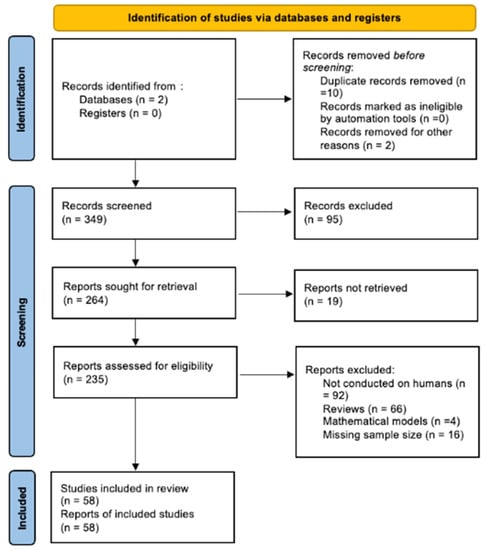
Figure 1.
Prisma diagram showing the research strategy and selection of papers included.
The reviewed papers were further divided into four categories based on their focus:
- (1)
- Microglia maintenance of immunological homeostasis and protection against autoimmunity (Table 1);
 Table 1. Microglia maintenance of immunological homeostasis and protection against autoimmunity.
Table 1. Microglia maintenance of immunological homeostasis and protection against autoimmunity. - (2)
- Microglia crosstalk with dedifferentiated and stem-like glioblastoma cells (Table 2);
 Table 2. Microglia crosstalk with dedifferentiated and stem-like glioblastoma.
Table 2. Microglia crosstalk with dedifferentiated and stem-like glioblastoma. - (3)
- Microglia migratory behavior and its activation pattern (Table 3).
 Table 3. Microglia migratory behavior and its activation pattern.
Table 3. Microglia migratory behavior and its activation pattern.
4. Discussion
GBM is a complex solid tumor with a highly inflammatory tumor environment. Approximately 30–50% of the brain tumor mass is constituted by microglia, monocytes, and macrophages, defined as GAMs []. These cellular populations are the major cerebral immune components [], responsible for maintaining brain homeostasis, producing cytokines, chemokines, and growth factors (which altogether constitute the TME), and regulating tumor progression [] (Figure 2).
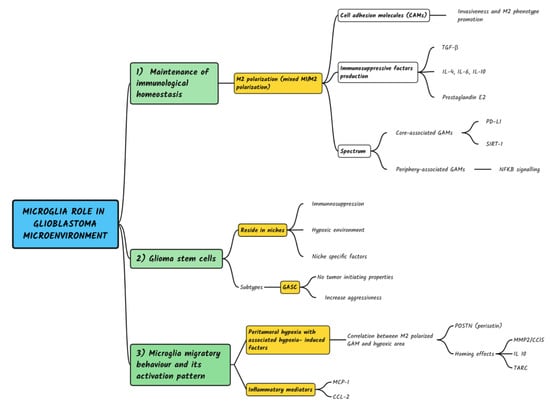
Figure 2.
Schematic representation of multiple roles of microglia in Glioblastoma development, pathogenesis and relapse according a ‘seed and soil’ aproach.
4.1. Microglia Maintenance of Immunological Homeostasis and Protection against Autoimmunity
GBM immune-escape is primarily due to the characteristics of neoplastic cells [,,,,,], which mask tumor antigens with decreased expression of HLA molecules [,,,,,,,] and have the ability to produce immunosuppressive factors [] and proapoptotic signals aimed at infiltrating tumor-specific immune cells [,]. In particular, the produced transforming growth factor-β (TGF-β) inhibits T-cell activation, proliferation, and differentiation, while promoting regulatory T-cells (T-regs) and suppressing both NK-cells and cytotoxic T-cells []. Complementarily, locally produced IL-10 has an inhibitory effect on T-helper (Th) cells, monocytes, macrophages, and dendritic cells (DC), resulting in an immune tolerance condition that favors tumor growth [].
All the relevant findings regarding microglia maintenance of immunological homeostasis and protections against autoimmunity are summarized in Table 1.
GAMs constitute a crucial component of the TME, together with extracellular matrix (ECM) and other nonmalignant cells, such as endothelial cells, fibroblasts, and T lymphocytes which play a pivotal role in the development, growth, and malignant characteristics of gliomas []. Within this complex cellular multiplicity, different GAM components can be identified []: a first group originating from the embryonic yolk sac and considered central nervous system (CNS) immune tissue residents, and a second group consisting of the CNS-infiltrating leucocytes (e.g., monocytes, T, B, and natural killer cells), normally circulating within the blood vessels except in the case of a blood-brain barrier disruption, as described in inflammatory and neoplastic CNS pathologies []. Although monocytes, macrophages, and microglia have several common markers, such as an ionized calcium-binding adapter molecule 1 (Iba1) and CX3CR1, some studies regarding transcriptome analyses comparing microglia and other myeloid immune cells, have identified a multitude of genes dependent on the TGF-β signaling, codifying for Sall1, TGF-βr1, P2ry12, Fcrls, and Gpr34 that can be considered specific markers for microglia []. GAMs can exhibit a different spectrum of phenotypes. As generally accepted, the activated microglia and macrophages can present an antitumoral immune phenotype, defined as M1, through the secretion of proinflammatory cytokines, such as tumor necrosis factor-alpha, IL-1beta, and inducible nitric oxide synthase []. Alternatively, GAMs have also been reported to play a crucial role in some GBM features, such as growth, invasion, proliferation, and immunosuppression [,]. Particularly, GAMs are forced to switch to the M2 phenotypes in the GBM microenvironment, secreting factors such as IL-10, IL-4, IL-6, macrophage colony-stimulating factor, TGF-β, macrophage inhibitory factor, and prostaglandin E2, which, due to their anti-inflammatory action, facilitate tumoral immune-escape and increase tumor invasiveness, angiogenesis and growth, contributing to the creation of an immunosuppressive tumoral microenvironment []. However, in recent years different studies reported that M1 and M2 phenotypes would represent only extremes of broader and more articulated cell heterogeneity [,]. To reinforce this concept, Landry et al. report significant differences in the GAM populations present in the GBM core, compared to those of the GBM periphery: on one side, core GAMs manifest mainly a proinflammatory phenotype correlated with Programmed cell Death-1 (PD-1) signaling; on the other, peripheral GAMs exhibit an anti-inflammatory phenotype and a strong association with NFkB signaling [].
Among the mechanisms that seem to support the proinflammatory activity of the GBM core, deacetylase Sirtuin 1 (SIRT1), whose gene is deleted in 80% of GBM tumors, seems to play a role. As a result, GBM cells continuously produce cytokines and factors attracting and activating glioma-associated microglia and macrophages, promoting a proinflammatory loop []. Another potential role in modulation and interaction between GBM cells and GAMs might be played by the ERp57/PDIA3 (protein disulfide-isomerase A3), an endoplasmic reticulum protein present both in GAMs and GBM cells, whose expression and activity were found to be directly proportional to the polarization capacity towards the protumor M2 phenotype of microglia []. This complex tumoral microenvironment, which mainly expresses immunosuppressive characteristics, especially in the tumoral periphery, determines a limited migration of T lymphocytes which represent less than 2% of the neoplastic cell mass []. This aspect has a pivotal role in therapeutic strategies, being immunotherapies targeting T cells, such as monoclonal antibodies against programmed cell death 1 (PD-1) or cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), which are not suitable for treating GBM [].
A further significant role in tumor metastasis and invasiveness is played by cell adhesion molecules (CAMs), which are cell surface-proteins that mediate cell–cell adhesion, particularly between immune cells and target tissues. Intercellular CAM (ICAM-1, also known as CD54) and vascular CAM (VCAM-1, also known as CD106), are upregulated by several proinflammatory cytokines, improving the immune-mediated response. Furthermore, ICAM-1 and VCAM-1 play important roles in the adhesion of cancer cells to the endothelium, especially in the context of the inflammatory microenvironment, supported by the high concentration of IL-1b, correlated with higher grade gliomas [,]. Through binding to IL-1R present on the surface of GBM cells, IL-1 can promote the cascade of the MAPK and p65 signaling pathways, resulting in the production of proteins and soluble forms of VCAM-1 and ICAM-1, which enhance monocytes adhesion and secretion of CCL2 and IL-6 through activated macrophages. This would seem to modulate the immunosuppressive activity, increasing the survival of myeloid monocytes recruited to the TME and polarizing their differentiation toward M2-type macrophages. Furthermore, the immunosuppressive microenvironment is not exclusive to GBMs: it has also been demonstrated in IDH mutant anaplastic astrocytomas and in IDH mutant/1p-19q codeleted anaplastic oligodendrogliomas [].
4.2. Microglia Crosstalk with Dedifferentiated and Stem-like Glioblastoma Cells
Glioma stem cells (GCS) are a chemo-resistant population that can drive tumor growth and relapse. The traditional theory of cancer stem cells defines them as a minor subpopulation of self-renewing malignant cells that maintain a low but steady level of unlimited proliferation [,]. The latter maintains the tumor, and these cells’ low mitotic activity protects them from treatment approaches that are directed against actively dividing cells [,]. Therefore, these cells can survive treatment and give rise to recurrences [,,,,,,]. In addition, stem cells interact with the TME, and their interplay is mandatory to develop biological resistance and sustain the tumorigenic process [,]. General features of GSCs are treatment resistance and association with tumor recurrence. They reside within specific anatomic niches, which can be seen as specialized microenvironments ensuring their stemness, proliferation, and apoptosis resistance, analogous to tissue stem cell niches. These niches shield GSC functionally by providing prosurvival cues and anatomically by blocking them from therapy exposure [,,,].
All the relevant findings regarding microglia crosstalk with dedifferentiated and stem-like glioblastoma cells are summarized in Table 2.
Four different niches have been identified, each one with a distinct TME composition and with niche-specific transcriptional and epigenetic signature. These are subarachnoid, perineuronal, perivascular, and perinecrotic [,,,,,,]. Within these niches, GSCs are regulated by several mechanisms other than from the TME, such as [,,,]:
- -
- Host immune system: since immunosuppression is a cardinal feature of malignant tumors.
- -
- Metabolism: GBM is characterized by a hypoxic environment, which in turn increases the need for glycolysis, active in malignant cells, even under aerobic conditions. Hypoxic niches and perivascular niches have been reported both inside and outside of the tumor mass.
- -
- Niche-specific factors: perivascular niches develop along capillaries and arterioles where GASCs are in direct contact with the endothelium. Invasive niches are characterized by perivascular growth of single invasive neoplastic cells along the capillaries, between the endothelium and reactive astrocytes.
Tumor-associated microglia and macrophages accumulate in perivascular and perinecrotic hypoxic niches, where they start a crosstalk with the staminal compartment ultimately promoting disease progression and relapse after treatments [,,,,,]. Mechanisms of crosstalk have only been investigated in a few seminal studies [,,,,,,].
Both clinical outcomes and mathematical modeling show that GSCs are a key mechanism in determining the resistance of the whole tumor to therapy. Isolated cell lines of glioblastoma do not show such a marked resistance as observed in GBM patients. In addition to this, in the brain-mimetic biomaterial platform for the 3D culturing of patient-derived GBM cells, the modulation of hyaluronic acid content and mechanical properties of biomaterials were required to recreate the known resistance to epidermal growth factors receptor (EGFR).
As previously discussed, TME niches play a multifaceted role in regulating GSCs and this motivates further investigation. Additionally, it has been demonstrated that GSCs immune evasion is critical to sustaining the tumorigenic process. GSCs express low levels of molecules involved in the processing and presenting tumor antigens to TCRs, a crucial stimulatory signal to the T-cell response. Consequently, they escape from recognition by antitumor immunity and possibly actively suppress T-cell activation. GSCs express various molecules that deliver either stimulatory or inhibitory signals during direct physical contact with tumor-infiltrating lymphocytes (TILs). The balance of these opposing signals regulates the amplitude and quality of TIL response and the aberrant activation of the inhibitory signals, also known as immune checkpoints, is a mechanism utilized by cancer cells to evade immune attacks [,].
Given the therapeutic potential and the promising therapies targeting the PD-1/PDL1 axis in GBM, the association between GSCs and the PDL1 axis in GBM deserves further analysis and investigation.
Hsu et al. recently demonstrated that epithelial-mesenchymal transition (EMT) enriches PD-L1 in GSCs by the EMT/β-catenin/STT3/PD-L1 signaling axis, in which EMT transcriptionally induces Nglycosyltransferase STT3 through β-catenin, and subsequent STT3-dependent PD-L1 Nglycosylation stabilizes and upregulates PD-L1. The axis is also utilized by the general cancer cell population, but it has a much more profound effect on GASCs as EMT induces more STT3 in CSCs than in nonGASCs. They further identified a noncanonical mesenchymal–epithelial transition (MET) activity of etoposide, which suppresses the EMT/β-catenin/STT3/PD-L1, leading to PD-L1 downregulation and sensitization of cancer cells to anti-Tim-3 therapy. On the one hand, this gives hope, on the other hand, it must be said that the expression of PD-L1 in GASC has never been described and further studies would be necessary to understand the possible potential for research and therapeutics [].
This confirms GSCs and their interplay with TMEs to be mandatory for biological resistance.
Against this background, our group previously isolated a subpopulation of stem cells, called glioma-associated stem cells (GASCs). Indeed, GASCs are devoid of tumor-initiating properties, but show stem cell properties and the ability to support, in vitro, the biological aggressiveness of tumor cells [].
In the infiltrating front of the tumor, transcriptomic suggested the presence of a GASC population possibly responsible for tumor recurrence. As already mentioned, even when GBM resection is performed beyond the tumor edge, there is no assurance that all tumor cells can be located and resected: infiltrating tumor cells are enriched with GASC, which in turn interacts with the TME, thus promoting tumor growth; in turn, the TME, by favoring hypoxic conditions, contributes to GASC generation.
4.3. Microglia Migratory Behavior and Its Activation Pattern
Despite a growing body of evidence, many aspects are yet to be explored regarding the migratory behavior of microglia with respect to tumoral margins. Open questions are related to microglia distribution in the peritumoral area, its spatial and molecular interaction with glioma infiltrative margins, and stem cell compartment []. Seminal studies showed how microglia move in a rather random way, whereas glioma cells exhibit a “committed” migratory behavior with significantly increased directionality compared to microglia []. However, it is unclear if glioma cells and microglia are responding to different migratory cues or are responding to the same cues but in different ways. GAMs polarization is influenced by both macrophage localization and tumor microenvironment signaling, resulting in a more complex scenario than the simple M1 and M2 activation status. Macrophage polarization in GBM has not yet been fully elucidated, and most results have been obtained in experimental nonhuman settings [,,,,,].
All the relevant findings regarding microglia migratory behavior and its activation pattern are summarized in Table 3.
Glioma cell–GAM crosstalking is fundamental to understanding microglia migratory behavior and its activation pattern in the center of the tumor and the surrounding periphery. Several studies have confirmed the central role of this crosstalk, highlighting a strong correlation between the local density of glioma cells and the rapidity of GAM migration and polarization [,]. Glioma cells stimulate the motility of microglial cells at the peritumoral infiltrative margins and after activation in a short period, microglia may enable more contact with cells via this random migration, resembling a surveillance function. However, microglia accumulation and polarization should not be regarded as a mere nonspecific reaction to tissue injury with consequent cytokine gradients, as it ultimately reflects their active participation in supporting and promoting the invasive phenotype of astrocytoma cells [,,,,].
Recent evidence highlights that the migration of tumoral and microglia compartments is ‘driven’ by, (a) a condition of peritumoral hypoxia with associated hypoxia-induced factors and, (b) inflammatory mediators produced by immune cells in the TME.
Hypoxia probably is the strongest determinant in shaping glioma and GAM migration. Indeed, it is well known that gliomas contain large hypoxic areas, and that a correlation between the density of M2-polarized GAMs and hypoxic areas exists. This suggests hypoxia plays a supportive role during GAM recruitment and M2 induction. Recent literature demonstrated perivascular niches in hypoxic areas and that hypoxia can affect chemotactic factors expression in such niches [,,,]. This mechanism underlies hypoxia-induced GAM recruitment and polarization, even if a clear description of M1- and M2-polarized cells distribution in a “topographic fashion” is still lacking in literature [].
To date, in normal brains, the macrophage population is mainly located in perivascular (Virchow–Robin) spaces of cerebral microvessels. These are continuously repopulated by blood-derived monocytes and macrophages, and more rarely by resident brain microglia []. A considerable amount of M2 macrophages can be identified in perinecrotic and perivascular areas, which are indicators of an advanced stage of the tumor. The accumulation of GAMs in avascular and necrotic areas strongly accounts for their exposure to hypoxia, recognized as a key stimulus for alternative macrophage activation. Altogether, these data further support the notion that the macrophage phenotype could be a result of glioma progression owing to an interactive network involving glioma stem cells, proinflammatory-activated glioma cells, GAMs, and other components of the perivascular niche []. Recent studies confirmed a high prevalence of M2-polarized macrophages mainly disposed around the clusters of proliferating vessels. However, it must be acknowledged that whereas ‘quantitative’ information on GAM has been quite widely investigated, little is known about GAM spatial distribution within and around tumor mass and if a possible ‘gradient of activation status’ at the tumor periphery exists.
Furthermore, Guo et al. showed how hypoxia-increased periostin (POSTN) expression in glioma cells actively promotes the recruitment of macrophages and that hypoxia-inducible POSTN expression was increased by TGF-α via the RTK/PI3K pathway [].
Other studies have shed light on the mechanisms that underlie GAM recruitment and M2 polarization under hypoxic conditions in gliomas. Specific chemokine or metalloproteinase upregulation has shown a distinct ‘homing effect’ with regards to GAMs. As shown in the seminal study by Yu-Ju et al., chemokine C-C ligand 5 (CCL5) modulates the migratory and invasive activities of glioma cells in association with metalloproteinase 2 (MMP2) expression. In response to CCL5, glioma cells undergo a synchronized increase in intracellular calcium levels and glioma cells tend to migrate toward GAM-conditioned media activated by a granulocyte-macrophage colony-stimulating factor (GM-CSF) in which CCL5 is abundant. Moreover, an association between CCL5 and GAM activation has been demonstrated []. Authors suggest that modulation of glioma calcium levels may restrict the effect of CCL5 on glioma invasion and could be a potential therapeutic target for alleviating glioma growth. Indeed, GBM expresses a plethora of macrophage chemoattractants, such as IL-10, macrophage migration inhibitory factor (MIF), cytokines of the CSF family (macrophage colony-stimulating factor1, M-CSF, and granulocyte-macrophage colony-stimulating factor, GM-CSF), monocyte chemotactic protein 1 (MCP-1), alternative macrophage activation-associated CC chemokine-1 (AMAC-1), thymus and activation regulated chemokine (TARC) belonging to the CC chemokine family, chemokine (C-X-C motif) ligand 4 (CXCL4), chemokine (C-X3-C motif) ligand 1 (CX3CL1/fractalkine), and stromal cell-derived factor 1 (SDF-1).
Regarding inflammatory mediators, it has been explained in the previous sections how inflammatory cytokines are determinants in GAM polarization and activation []. CC motif chemokine ligand 2 (CCL-2), also known as monocyte chemoattractant protein 1 (MCP-1), is a major chemokine that acts as a glioma cell-derived monocyte chemotactic factor. Indeed, overexpression of CCL-2 results in increased migration. Conversely, stromal cells such as macrophages secrete more CCL-2 into the TME than cancer cells. In a positive feedback loop, GBM cells secrete CCL-2 and attract macrophages and microglia; these cells also secrete CCL-2, and the number of activated cells is increased. Thus, GBM cells, macrophages, and microglia exhibit a robust reciprocal network in proliferation and migration. Other authors showed how chemokine receptor pairs CXCL12/CXCR4/CXCR7, CXCL16/CXCR6, and CX3CL1/CX3CR1 are involved in tumor progression and that GBM-associated macrophages and microglia are also characterized by expression of these chemokine receptor pairs indicating a pivotal role of this expression profile in GAM biology in gliomas [,].
4.4. Targeting the Tumor Microenvironment: The Disillusionment with Current Immunotherapeutic Treatment
Targeting therapeutics to the TME offers promise to improve patient survival and quality of life. Unfortunately, most of the clinically tested GBM-targeted therapies have shown little efficacy so far, such as erlotinib targeting the often overexpressed EGFR. At present, the anti-VEGF bevacizumab is the only drug targeting GBM TMEs that is approved by the US Food and Drug Administration (FDA). In addition, traditional treatments, radiotherapy, and chemotherapy with TMZ have shown to promote TME remodeling [,,,,]:
- -
- Radiotherapy improves the blood-brain barrier (BBB) permeability to chemotherapy; triggers TME remodeling via increased GAM infiltrates and improved GSC radiation resistance by activating DNA damage checkpoints to repair DNA damage.
- -
- Temozolomide (TMZ) triggers a proinvasive TME phenotype by altering proteoglycans and glycosaminoglycans (GAGs) content.
These observations confirm that the TME acts as a “plastic soil” and can change its functions based on environmental stimuli [,,,,,,,,].
As already stressed, TME niches play a multifaceted role in regulating GSCs and GSC immune evasion is critical to sustaining the tumorigenic process. GSCs express low levels of molecules involved in the processing and presenting of tumor antigens to TCRs, a crucial stimulatory signal to the T-cell response. Consequently, they escape from recognition by antitumor immunity and possibly actively suppress T-cell activation. GSCs express various molecules that deliver either stimulatory or inhibitory signals during direct physical contact with TILs. The balance of these opposing signals regulates the amplitude and quality of TIL response, and aberrant activation of the inhibitory signals, also known as immune checkpoints, is a mechanism utilized by cancer cells to evade immune attacks.
PD-1 belongs to the family of immunoglobulins and is expressed predominantly by activated T lymphocytes. It is often activated by PD-L1, one of the ligands known to be expressed by antigen-presenting cells (APCs), B lymphocytes, and parenchymal cells. Importantly, the expression of PD-L1 has been detected in glioma. In normal conditions, PD-1/PD-L1 engagement occurs controlling a prolonged activation of the immune system, often avoiding autoimmunity processes. Therefore, the PD-1/PD-L1 pathway has been appropriated by tumor cells to resist antitumor responses and facilitate tumor survival. Early immunotherapeutic attempts were focused on targeting PD-1 expression in the general cancer cell population. However, failure of anti-PD1 therapy has been seen in Checkmate 143, 498, and 548 clinical trials [,,].
Thus, the focus has been shifted to PD-L1. In the TME, PD-L1 is regulated mainly by cytokine, while receptor antigen signaling is influenced by hypoxia, cytokines, and oncogenes. GBM cells express PD-L1, which engages with the PD-1 receptor primarily on T cells and attenuates its functions, effectively reducing the antitumor activity of these cells. Nevertheless, studies have shown heterogeneity of PD-L1 expression in tumor mass; a greater expression was observed at the edges of the tumor than in the core. Several phase I and II trials are focusing on PD-L1 in gliomas. Current evidence demonstrates that:
- (1)
- PD-L1 quantitative expression has an impact on survival, independently of gender and age [].
- (2)
- PD-L1 overexpression is significantly associated with poor OS for patients from Asia and America, while no significant association for the survival of patients from Europe. This “ethnic bias” of PD-L1 has been observed in several clinical studies for patients with other solid tumors, such as KEYNOTE-161 in esophageal squamous cell carcinoma and KEYNOTE-063 in advanced gastric or gastro-esophageal junction cancer [].
- (3)
- IDH1-wildtype status in glioblastoma was PD-L1 expression positive, suggesting PD-L1/IDH1-wildtype association. From a molecular point of view, it could be that IDH1 mutation results in PD-L1 promoter hypermethylation, thus downregulating the expression of PD-L1. Therefore, PD-L1 immune checkpoint inhibitors analysis might not be advisable because of the globally low PD-L1 expression in patients with IDH1-mutant glioblastomas.
To sum up, higher expression of PD-L1 (both at protein and mRNA levels) is linked to a worse outcome. PD-L1 may expand and maintain immunosuppressive Tregs, which are associated with decreased survival in glioma patients. Beyond the direct impact on effector cells, the blockade of the PD-L1/PD-1 axis may reduce Treg expansion and further improve T cell function [].
5. Conclusions
Microenvironmental contribution seems therefore critical to gaining a better understanding of the unique challenges GBM poses. Aggressive growth, inevitable recurrence, and scarce response to immunotherapies are driving the necessity to focus on GBM TMEs from a different perspective to possibly disentangle its role as a fertile ‘soil’ for tumor progression and identify in it feasible therapeutic targets. Against this background, our systematic review confirmed:
- (1)
- Microglia play a paramount role in the maintenance of immunological homeostasis and protection against autoimmunity and its activation pattern at the TME level, polarized toward an M2 phenotype as selected by environmental pressure. This suggests that further investigation of microglia phenotypic characterization at the microenvironment level (M1 vs. M2 phenotype) is needed.
- (2)
- Microglia crosstalk with dedifferentiated and stem-like glioblastoma cells in perivascular and perinecrotic hypoxic niches, where they start crosstalk with the staminal compartment ultimately promoting disease progression and relapse after treatments.
- (3)
- Microglia demonstrate migratory behavior with respect to infiltrative margins of tumor cells. However, there are still many issues to be investigated. While the classification of macrophages or microglial cells into the M1 or M2 polarized state is a well-established approach in most preclinical models, the same is not true in the clinical research setting, because of the high degree of diversity and plasticity shown by these cell types. Therefore, dichotomizing GAMS into M1 and M2 activation status might be over simplistic as, indeed, a clear distinction between these phenotypes cannot be clearly distinguished. The resulting definitions of transcriptomic-based functional phenotypes of GAMs from human and experimental rodent gliomas are conflicting and indicate a mixture of M1 and M2 phenotypes. Cells within the tumor often display a complex pattern of phenotypes, upregulating both M1 and M2 molecular markers, and the prevalence of one phenotype on the other might also depend on the stage of disease [].
In addition, the danger of ‘oversimplification’ goes along with the lack of universally recognized markers of the functional phenotype of GAMs. Although the association of GAM subtypes and patient overall survival has been observed in several papers still no consensus exists on reliable gene expression-based markers [].
To further confound the research scenario on the topic it should also take into account that it is hard to define realistic research models as significant differences between human and mice models exists in terms of microglia polarization and inconsistency between rodent and human GAMs, regarding markers, has been reported. Despite some similarities, the mouse and rat models represent different pathways of GAM activation; comparative analysis of GAM transcriptomics across different in vivo models of human, mouse, and rat, failed to reproduce consistent microglia phenotypes that could be classified according to previously reported gene signatures and showed remarkably low similarity between models [].
Despite the growing body of evidence on the topic reported in this paper, many aspects are yet to be explored in the field [,,,,,,]. The correct and extensive understanding of microglia–glioma crosstalk could help in understanding the physiopathology of this complex disease, possibly opening scenarios for improvement of surgical strategies and medical treatments.
Author Contributions
Conceptualization, G.M., G.M.D.P. and P.P.M.; methodology, G.M.D.P.; data curation, G.M., P.P.M. and C.M.D.; writing—original draft preparation, G.M., P.P.M., C.M.D. and G.M.D.P.; writing—review and editing, G.M.D.P. and L.L.; visualization, G.M., L.L. and G.M.D.P.; supervision, G.M.D.P. and A.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| APCs | Antigen presenting cells |
| BBB | Blood brain barrier |
| CAMs | cell adhesion molecules |
| CNS | Central nervous system |
| ECM | Extracellular matrix |
| EMT | Epithelial–mesenchymal transition |
| EGFR | epidermal growth factors receptor |
| FDA | Food and Drug Administration |
| GAG | Glycosaminoglycans |
| GAM | Glioma-associated macrophage and microglia |
| GASC | Glioma Associated Stem cells |
| GBM | Glioblastoma |
| GCS | Glioma stem cells |
| MET | mesenchymal–epithelial transition |
| PD1 | Programmed cell Death-1 |
| PRISMA-P | Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols |
| SIRT1 | Sirtuin 1 |
| TCR | T cell receptors |
| TGF-β | Transforming growth factor-β |
| TIL | Tumor-infiltrating lymphocytes |
| TME | Tumor Microenvironment |
| TMZ | Temozolomide |
References
- Prosniak, M.; Harshyne, L.A.; Andrews, D.W.; Kenyon, L.; Bedelbaeva, K.; Apanasovich, T.V.; Heber-Katz, E.; Curtis, M.T.; Cotzia, P.; Hooper, D. Glioma Grade Is Associated with the Accumulation and Activity of Cells Bearing M2 Monocyte Markers. Clin. Cancer Res. 2013, 19, 3776–3786. [Google Scholar] [CrossRef] [PubMed]
- Hattermann, K.; Sebens, S.; Helm, O.; Schmitt, A.D.; Mentlein, R.; Mehdorn, H.M.; Held-Feindt, J. Chemokine expression profile of freshly isolated human glioblastoma-associated macrophages/microglia. Oncol. Rep. 2014, 32, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Zeiner, P.S.; Preusse, C.; Blank, A.-E.; Zachskorn, C.; Baumgarten, P.; Caspary, L.; Braczynski, A.K.; Weissenberger, J.; Bratzke, H.; Reiß, S.; et al. MIF Receptor CD74 is Restricted to Microglia/Macrophages, Associated with a M1-Polarized Immune Milieu and Prolonged Patient Survival in Gliomas. Brain Pathol. 2014, 25, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, M.D.; Dahlrot, R.H.; Boldt, H.B.; Hansen, S.; Kristensen, B.W. Tumour-associated microglia/macrophages predict poor prognosis in high-grade gliomas and correlate with an aggressive tumour subtype. Neuropathol. Appl. Neurobiol. 2018, 44, 185–206. [Google Scholar] [CrossRef] [PubMed]
- Zeiner, P.S.; Preusse, C.; Golebiewska, A.; Zinke, J.; Iriondo, A.; Muller, A.; Kaoma, T.; Filipski, K.; Müller-Eschner, M.; Bernatz, S.; et al. Distribution and prognostic impact of microglia/macrophage subpopulations in gliomas. Brain Pathol. 2018, 29, 513–529. [Google Scholar] [CrossRef]
- Lin, G.L.; Nagaraja, S.; Filbin, M.G.; Suvà, M.L.; Vogel, H.; Monje, M. Non-inflammatory tumor microenvironment of diffuse intrinsic pontine glioma. Acta Neuropathol. Commun. 2018, 6, 51. [Google Scholar] [CrossRef]
- Waters, M.R.; Gupta, A.S.; Mockenhaupt, K.; Brown, L.N.; Biswas, D.D.; Kordula, T. RelB acts as a molecular switch driving chronic inflammation in glioblastoma multiforme. Oncogenesis 2019, 8, 37. [Google Scholar] [CrossRef]
- Martinez-Lage, M.; Lynch, T.M.; Bi, Y.; Cocito, C.; Way, G.P.; Pal, S.; Haller, J.; Yan, R.E.; Ziober, A.; Nguyen, A.; et al. Immune landscapes associated with different glioblastoma molecular subtypes. Acta Neuropathol. Commun. 2019, 7, 203. [Google Scholar] [CrossRef]
- González-Tablas Pimenta, M.; Otero, Á.; Arandia Guzman, D.A.; Pascual-Argente, D.; Ruíz Martín, L.; Sousa-Casasnovas, P.; García-Martin, A.; Roa Montes de Oca, J.C.; Villaseñor-Ledezma, J.; Torres Carretero, L.; et al. Tumor cell and immune cell profiles in primary human glioblastoma: Impact on patient outcome. Brain Pathol. 2021, 31, 365–380. [Google Scholar] [CrossRef]
- Fu, W.; Wang, W.; Li, H.; Jiao, Y.; Weng, J.; Huo, R.; Yan, Z.; Wang, J.; Xu, H.; Wang, S.; et al. High Dimensional Mass Cytometry Analysis Reveals Characteristics of the Immunosuppressive Microenvironment in Diffuse Astrocytomas. Front. Oncol. 2020, 10, 78. [Google Scholar] [CrossRef]
- Klemm, F.; Maas, R.R.; Bowman, R.L.; Kornete, M.; Soukup, K.; Nassiri, S.; Brouland, J.-P.; Iacobuzio-Donahue, C.A.; Brennan, C.; Tabar, V.; et al. Interrogation of the Microenvironmental Landscape in Brain Tumors Reveals Disease-Specific Alterations of Immune Cells. Cell 2020, 181, 1643–1660.e17. [Google Scholar] [CrossRef] [PubMed]
- Zinnhardt, B.; Müther, M.; Roll, W.; Backhaus, P.; Jeibmann, A.; Foray, C.; Barca, C.; Döring, C.; Tavitian, B.; Dollé, F.; et al. TSPO imaging-guided characterization of the immunosuppressive myeloid tumor microenvironment in patients with malignant glioma. Neuro-Oncology 2020, 22, 1030–1043. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Wang, W.; Li, H.; Jiao, Y.; Weng, J.; Huo, R.; Yan, Z.; Wang, J.; Xu, H.; Wang, S.; et al. CyTOF Analysis Reveals a Distinct Immunosuppressive Microenvironment in IDH Mutant Anaplastic Gliomas. Front. Oncol. 2021, 10, 560211. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Yuan, F.; Zhu, J.; Yang, J.; Tang, C.; Cong, Z.; Ma, C. Glioma-Associated Stromal Cells Stimulate Glioma Malignancy by Regulating the Tumor Immune Microenvironment. Front. Oncol. 2021, 11, 672928. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, W.; Fan, W.; Ren, C.; Xu, J.; Zeng, F.; Bao, Z.; Jiang, T.; Zhao, Z. Comprehensive transcriptomic characterization reveals core genes and module associated with immunological changes via 1619 samples of brain glioma. Cell Death Dis. 2021, 12, 1140. [Google Scholar] [CrossRef]
- Cui, X.; Wang, Q.; Zhou, J.; Wang, Y.; Xu, C.; Tong, F.; Wang, H.; Kang, C. Single-Cell Transcriptomics of Glioblastoma Reveals a Unique Tumor Microenvironment and Potential Immunotherapeutic Target Against Tumor-Associated Macrophage. Front. Oncol. 2021, 11, 710695. [Google Scholar] [CrossRef]
- Shen, C.-K.; Huang, B.-R.; Yeh, W.-L.; Chen, C.-W.; Liu, Y.-S.; Lai, S.-W.; Tseng, W.-P.; Lu, D.-Y.; Tsai, C.-F. Regulatory effects of IL-1β in the interaction of GBM and tumor-associated monocyte through VCAM-1 and ICAM-1. Eur. J. Pharmacol. 2021, 905, 174216. [Google Scholar] [CrossRef]
- Fries, G.; Perneczky, A.; Kempski, O. Glioblastoma-associated circulating monocytes and the release of epidermal growth factor. J. Neurosurg. 1996, 85, 642–647. [Google Scholar] [CrossRef]
- Dziurzynski, K.; Wei, J.; Qiao, W.; Hatiboglu, M.A.; Kong, L.-Y.; Wu, A.; Wang, Y.; Cahill, D.; Levine, N.; Prabhu, S.; et al. Glioma-Associated Cytomegalovirus Mediates Subversion of the Monocyte Lineage to a Tumor Propagating Phenotype. Clin. Cancer Res. 2011, 17, 4642–4649. [Google Scholar] [CrossRef]
- Kmiecik, J.; Poli, A.; Brons, N.H.C.; Waha, A.; Eide, G.E.; Enger, P.Ø.; Zimmer, J.; Chekenya, M. Elevated CD3+ and CD8+ tumor-infiltrating immune cells correlate with prolonged survival in glioblastoma patients despite integrated immunosuppressive mechanisms in the tumor microenvironment and at the systemic level. J. Neuroimmunol. 2013, 264, 71–83. [Google Scholar] [CrossRef]
- Shimato, S.; Anderson, L.M.; Asslaber, M.; Bruce, J.N.; Canoll, P.; Anderson, D.E.; Anderson, R.C.E. Inhibition of Caveolin-1 Restores Myeloid Cell Function in Human Glioblastoma. PLoS ONE 2013, 8, e77397. [Google Scholar] [CrossRef] [PubMed]
- Silver, D.J.; Siebzehnrubl, F.; Schildts, M.J.; Yachnis, A.T.; Smith, G.M.; Smith, A.A.; Scheffler, B.; Reynolds, B.A.; Silver, J.; Steindler, D.A. Chondroitin Sulfate Proteoglycans Potently Inhibit Invasion and Serve as a Central Organizer of the Brain Tumor Microenvironment. J. Neurosci. 2013, 33, 15603–15617. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Roncaroli, F.; Durrenberger, P.F.; Coope, D.J.; Karabatsou, K.; Hinz, R.; Thompson, G.; Turkheimer, F.E.; Janczar, K.; Du Plessis, D.; et al. The 18-kDa Mitochondrial Translocator Protein in Human Gliomas: An 11C-(R)PK11195 PET Imaging and Neuropathology Study. J. Nucl. Med. 2015, 56, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Stradmann-Bellinghausen, B.; Savaskan, N.; Regnier-Vigouroux, A. Human Monocyte-Derived Macrophages Exposed to Glioblastoma Cells and Tumor-Associated Microglia/Macrophages Differ in Glutamatergic Gene Expressions. In Glia; Wiley-Blackwell: Hoboken, NJ, USA, 2015; Volume 63, p. E466. [Google Scholar]
- Dijksterhuis, J.P.; Arthofer, E.; Marinescu, V.D.; Nelander, S.; Uhlén, M.; Pontén, F.; Mulder, J.; Schulte, G. High levels of WNT-5A in human glioma correlate with increased presence of tumor-associated microglia/monocytes. Exp. Cell Res. 2015, 339, 280–288. [Google Scholar] [CrossRef]
- Chen, J.E.; Lumibao, J.; Leary, S.; Sarkaria, J.N.; Steelman, A.J.; Gaskins, H.R.; Harley, B.A.C. Crosstalk between microglia and patient-derived glioblastoma cells inhibit invasion in a three-dimensional gelatin hydrogel model. J. Neuroinflamm. 2020, 17, 346. [Google Scholar] [CrossRef]
- Zhu, C.; Mustafa, D.; Zheng, P.-P.; Van Der Weiden, M.; Sacchetti, A.; Brandt, M.; Chrifi, I.; Tempel, D.; Leenen, P.J.M.; Duncker, D.J.; et al. Activation of CECR1 in M2-like TAMs promotes paracrine stimulation-mediated glial tumor progression. Neuro-Oncology 2017, 19, 648–659. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, C.; Liu, X.; Wang, Z.; Sun, L.; Li, G.; Liang, J.; Hu, H.; Liu, Y.; Zhang, W.; et al. Molecular and clinical characterization of PD-L1 expression at transcriptional level via 976 samples of brain glioma. OncoImmunology 2016, 5, e1196310. [Google Scholar] [CrossRef]
- Leite, D.M.; Zvar Baskovic, B.; Civita, P.; Neto, C.; Gumbleton, M.; Pilkington, G.J. A human co-culture cell model incorporating microglia supports glioblastoma growth and migration, and confers resistance to cytotoxics. FASEB J. 2020, 34, 1710–1727. [Google Scholar] [CrossRef]
- Caponegro, M.D.; Oh, K.; Madeira, M.M.; Radin, D.; Sterge, N.; Tayyab, M.; Moffitt, R.A.; Tsirka, S.E. A distinct microglial subset at the tumor–stroma interface of glioma. Glia 2021, 69, 1767–1781. [Google Scholar] [CrossRef]
- Sadahiro, H.; Kang, K.-D.; Gibson, J.T.; Minata, M.; Yu, H.; Shi, J.; Chhipa, R.R.; Chen, Z.; Lu, S.; Simoni, Y.; et al. Activation of the Receptor Tyrosine Kinase AXL Regulates the Immune Microenvironment in Glioblastoma. Cancer Res. 2018, 78, 3002–3013. [Google Scholar] [CrossRef]
- Couto, M.; Coelho-Santos, V.; Santos, L.; Fontes-Ribeiro, C.; Silva, A.P.; Gomes, C.M.F. The interplay between glioblastoma and microglia cells leads to endothelial cell monolayer dysfunction via the interleukin-6-induced JAK2/STAT3 pathway. J. Cell Physiol. 2019, 234, 19750–19760. [Google Scholar] [CrossRef] [PubMed]
- Gjorgjevski, M.; Hannen, R.; Carl, B.; Li, Y.; Landmann, E.; Buchholz, M.; Bartsch, J.W.; Nimsky, C. Molecular profiling of the tumor microenvironment in glioblastoma patients: Correlation of microglia/macrophage polarization state with metalloprotease expression profiles and survival. Biosci. Rep. 2019, 39, BSR20182361. [Google Scholar] [CrossRef] [PubMed]
- Lisi, L.; Ciotti, G.M.P.; Chiavari, M.; Pizzoferrato, M.; Mangiola, A.; Kalinin, S.; Feinstein, D.L.; Navarra, P. Phospho-mTOR expression in human glioblastoma microglia-macrophage cells. Neurochem. Int. 2019, 129, 104485. [Google Scholar] [CrossRef] [PubMed]
- Chiavari, M.; Ciotti, G.; Canonico, F.; Altieri, F.; Lacal, P.; Graziani, G.; Navarra, P.; Lisi, L. PDIA3 Expression in Glioblastoma Modulates Macrophage/Microglia Pro-Tumor Activation. Int. J. Mol. Sci. 2020, 21, 8214. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Wang, W.; Li, H.; Jiao, Y.; Huo, R.; Yan, Z.; Wang, J.; Wang, S.; Wang, J.; Chen, D.; et al. Single-Cell Atlas Reveals Complexity of the Immunosuppressive Microenvironment of Initial and Recurrent Glioblastoma. Front. Immunol. 2020, 11, 835. [Google Scholar] [CrossRef]
- Tan, Y.Q.; Li, Y.T.; Yan, T.F.; Xu, Y.; Liu, B.H.; Yang, J.A.; Yang, X.; Chen, Q.X.; Zhang, H.B. Six Immune Associated Genes Construct Prognostic Model Evaluate Low-Grade Glioma. Front. Immunol. 2020, 11, 3326. [Google Scholar] [CrossRef]
- Wei, J.; Gabrusiewicz, K.; Heimberger, A. The Controversial Role of Microglia in Malignant Gliomas. Clin. Dev. Immunol. 2013, 2013, 285246. [Google Scholar] [CrossRef]
- Senjor, E.; Perišić Nanut, M.; Breznik, B.; Mitrović, A.; Mlakar, J.; Rotter, A.; Porčnik, A.; Lah Turnšek, T.; Kos, J. Cystatin F acts as a mediator of immune suppression in glioblastoma. Cell. Oncol. 2021, 44, 1051–1063. [Google Scholar] [CrossRef]
- Tanaka, S.; Ohgidani, M.; Hata, N.; Inamine, S.; Sagata, N.; Shirouzu, N.; Mukae, N.; Suzuki, S.O.; Hamasaki, H.; Hatae, R.; et al. CD206 Expression in Induced Microglia-Like Cells from Peripheral Blood as a Surrogate Biomarker for the Specific Immune Microenvironment of Neurosurgical Diseases Including Glioma. Front. Immunol. 2021, 12, 670131. [Google Scholar] [CrossRef]
- Nuñez, R.E.; del Valle, M.M.; Ortiz, K.; Almodovar, L.; Kucheryavykh, L. Microglial Cytokines Induce Invasiveness and Proliferation of Human Glioblastoma through Pyk2 and FAK Activation. Cancers 2021, 13, 6160. [Google Scholar] [CrossRef]
- Li, Y.; Dong, X.; Cai, J.; Yin, S.; Sun, Y.; Yang, D.; Jiang, C. SERPINA3 induced by astroglia/microglia co-culture facilitates glioblastoma stem-like cell invasion. Oncol. Lett. 2017, 15, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Urbantat, R.M.; Jelgersma, C.; Brandenburg, S.; Nieminen-Kelhä, M.; Kremenetskaia, I.; Zollfrank, J.; Mueller, S.; Rubarth, K.; Koch, A.; Vajkoczy, P.; et al. Tumor-Associated Microglia/Macrophages as a Predictor for Survival in Glioblastoma and Temozolomide-Induced Changes in CXCR2 Signaling with New Resistance Overcoming Strategy by Combination Therapy. Int. J. Mol. Sci. 2021, 22, 11180. [Google Scholar] [CrossRef] [PubMed]
- Parney, I.F.; Waldron, J.S.; Parsa, A.T. Flow cytometry and in vitro analysis of human glioma-associated macrophages: Laboratory investigation. J. Neurosurg. 2009, 110, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Della Pepa, G.M.; Menna, G. In Reply to the Letter to the Editor Regarding “5-Aminolevulinic Acid False Positives in Cerebral Neuro-Oncology: Not All That Is Fluorescent Is Tumor. A Case-Based Update and Literature Review”. World Neurosurg. 2022, 161, 218–219. [Google Scholar] [CrossRef]
- Guo, X.; Xue, H.; Shao, Q.; Wang, J.; Guo, X.; Chen, X.; Zhang, J.; Xu, S.; Li, T.; Zhang, P.; et al. Hypoxia promotes glioma-associated macrophage infiltration via periostin and subsequent M2 polarization by upregulating TGF-βeta and M-CSFR. Oncotarget 2016, 7, 80521–80542. [Google Scholar] [CrossRef]
- Mignogna, C.; Signorelli, F.; Vismara, M.F.M.; Zeppa, P.; Camastra, C.; Barni, T.; Donato, G.; Di Vito, A. A reappraisal of macrophage polarization in glioblastoma: Histopathological and immunohistochemical findings and review of the literature. Pathol.-Res. Pract. 2016, 212, 491–499. [Google Scholar] [CrossRef]
- Lisi, L.; Ciotti, G.; Braun, D.; Kalinin, S.; Currò, D.; Russo, C.D.; Coli, A.; Mangiola, A.; Anile, C.; Feinstein, D.; et al. Expression of iNOS, CD163 and ARG-1 taken as M1 and M2 markers of microglial polarization in human glioblastoma and the surrounding normal parenchyma. Neurosci. Lett. 2017, 645, 106–112. [Google Scholar] [CrossRef]
- Annovazzi, L.; Mellai, M.; Bovio, E.; Mazzetti, S.; Pollo, B.; Schiffer, D. Microglia immunophenotyping in gliomas. Oncol. Lett. 2017, 15, 998–1006. [Google Scholar] [CrossRef]
- Hide, T.; Shibahara, I.; Kumabe, T. Novel concept of the border niche: Glioblastoma cells use oligodendrocytes progenitor cells (GAOs) and microglia to acquire stem cell-like features. Brain Tumor Pathol. 2019, 36, 63–73. [Google Scholar] [CrossRef]
- Yu-Ju Wu, C.; Chen, C.H.; Lin, C.Y.; Feng, L.Y.; Lin, Y.C.; Wei, K.C.; Huang, C.Y.; Fang, J.Y.; Chen, P.Y. CCL5 of glioma-associated microglia/macrophages regulates glioma migration and invasion via calcium-dependent matrix metalloproteinase 2. Neuro-Oncol. 2020, 22, 253–266. [Google Scholar] [CrossRef]
- Landry, A.P.; Balas, M.; Alli, S.; Spears, J.; Zador, Z. Distinct regional ontogeny and activation of tumor associated macrophages in human glioblastoma. Sci. Rep. 2020, 10, 19542. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Liu, W.; Xu, Z.; Zhao, J.; Wang, W.; Yu, Z.; Wei, M. Integrated microenvironment-associated genomic profiles identify LRRC15 mediating recurrent glioblastoma-associated macrophages infiltration. J. Cell. Mol. Med. 2021, 25, 5534–5546. [Google Scholar] [CrossRef] [PubMed]
- Kai, K.; Komohara, Y.; Esumi, S.; Fujiwara, Y.; Yamamoto, T.; Uekawa, K.; Ohta, K.; Takezaki, T.; Kuroda, J.; Shinojima, N.; et al. Macrophage/microglia-derived IL-1β induces glioblastoma growth via the STAT3/NF-κB pathway. Hum. Cell 2022, 35, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Sielska, M.; Przanowski, P.; Wylot, B.; Gabrusiewicz, K.; Maleszewska, M.; Kijewska, M.; Zawadzka, M.; Kucharska, J.; Vinnakota, K.; Kettenmann, H.; et al. Distinct roles of CSF family cytokines in macrophage infiltration and activation in glioma progression and injury response. J. Pathol. 2013, 230, 310–321. [Google Scholar] [CrossRef] [PubMed]
- Butts, C.; Socinski, M.A.; Mitchell, P.L.; Thatcher, N.; Havel, L.; Krzakowski, M.; Nawrocki, S.; Ciuleanu, T.E.; Bosquée, L.; Trigo, J.M.; et al. Tecemotide (L-BLP25) versus placebo after chemoradiotherapy for stage III non-small-cell lung cancer (START): A randomised, double-blind, phase 3 trial. Lancet Oncol. 2014, 15, 59–68. [Google Scholar] [CrossRef]
- Shen, X.; Wang, X.; Shen, H.; Feng, M.; Wu, D.; Yang, Y.; Li, Y.; Yang, M.; Ji, W.; Wang, W.; et al. Transcriptomic Analysis Identified Two Subtypes of Brain Tumor Characterized by Distinct Immune Infiltration and Prognosis. Front. Oncol. 2021, 11, 734407. [Google Scholar] [CrossRef]
- Di Ianni, N.; Maffezzini, M.; Eoli, M.; Pellegatta, S. Revisiting the Immunological Aspects of Temozolomide Considering the Genetic Landscape and the Immune Microenvironment Composition of Glioblastoma. Front. Oncol. 2021, 11, 1–7. [Google Scholar] [CrossRef]
- Anghileri, E.; Patanè, M.; Di Ianni, N.; Sambruni, I.; Maffezzini, M.; Milani, M.; Maddaloni, L.; Pollo, B.; Eoli, M.; Pellegatta, S. Deciphering the Labyrinthine System of the Immune Microenvironment in Recurrent Glioblastoma: Recent Original Advances and Lessons from Clinical Immunotherapeutic Approaches. Cancers 2021, 13, 6156. [Google Scholar] [CrossRef]
- Pyonteck, S.M.; Akkari, L.; Schuhmacher, A.J.; Bowman, R.L.; Sevenich, L.; Quail, D.F.; Olson, O.C.; Quick, M.L.; Huse, J.T.; Teijeiro, V.; et al. CSF-1R inhibition alters macrophage polarization and blocks glioma progression. Nat. Med. 2013, 19, 1264–1272. [Google Scholar] [CrossRef]
- Butovsky, O.; Jedrychowski, M.P.; Moore, C.S.; Cialic, R.; Lanser, A.J.; Gabriely, G.; Koeglsperger, T.; Dake, B.; Wu, P.M.; Doykan, C.E. Erratum: Identification of a unique TGF-β-dependent molecular and functional signature in microglia. Nat. Neurosci. 2014, 17, 1286. [Google Scholar] [CrossRef]
- Pan, Y.; Smithson, L.J.; Ma, Y.; Hambardzumyan, D.; Gutmann, D.H. Ccl5 establishes an autocrine high-grade glioma growth regulatory circuit critical for mesenchymal glioblastoma survival. Oncotarget 2017, 8, 32977–32989. [Google Scholar] [CrossRef]
- Qian, J.; Luo, F.; Yang, J.; Liu, J.; Liu, R.; Wang, L.; Wang, C.; Deng, Y.; Lu, Z.; Wang, Y.; et al. TLR2 Promotes Glioma Immune Evasion by Downregulating MHC Class II Molecules in Microglia. Cancer Immunol. Res. 2018, 6, 1220–1233. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Hu, B.; Hu, X.; Kim, H.; Squatrito, M.; Scarpace, L.; DeCarvalho, A.C.; Lyu, S.; Li, P.; Li, Y.; et al. Tumor Evolution of Glioma-Intrinsic Gene Expression Subtypes Associates with Immunological Changes in the Microenvironment. Cancer Cell 2017, 32, 42–56.e6. [Google Scholar] [CrossRef]
- Feng, X.; Szulzewsky, F.; Yerevanian, A.; Chen, Z.; Heinzmann, D.; Rasmussen, R.D.; Alvarez-Garcia, V.; Kim, Y.; Wang, B.; Tamagno, I.; et al. Loss of CX3CR1 increases accumulation of inflammatory monocytes and promotes gliomagenesis. Oncotarget 2015, 6, 15077–15094. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, W.; Sanchez-Perez, L.; Gajewski, T.F.; Sampson, J.H. Brain Tumor Microenvironment and Host State: Implications for Immunotherapy. Clin. Cancer Res. 2019, 25, 4202–4210. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Dube, C.; Gibert, M.; Cruickshanks, N.; Wang, B.; Coughlan, M.; Yang, Y.; Setiady, I.; Deveau, C.; Saoud, K.; et al. The p53 Pathway in Glioblastoma. Cancers 2018, 10, 297. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Sun, Y.; Zhang, Q.; Jin, W.; Gordon, R.E.; Zhang, Y.; Wang, J.; Sun, C.; Wang, Z.J.; Qi, X.; et al. Pro-inflammatory and proliferative microglia drive progression of glioblastoma. Cell Rep. 2021, 36, 109718. [Google Scholar] [CrossRef]
- Silver, D.J.; Lathia, J.D. Therapeutic Injury and Tumor Regrowth: Tumor Resection and Radiation Establish the Recurrent Glioblastoma Microenvironment. EBioMedicine 2018, 31, 13–14. [Google Scholar] [CrossRef]
- Zhang, H.; Du, J.; Wang, H.; Wang, H.; Jiang, J.; Zhao, J.; Lu, H. Comparison of diagnostic values of ultrasound micro-flow imaging and contrast-enhanced ultrasound for neovascularization in carotid plaques. Exp. Ther. Med. 2017, 14, 680–688. [Google Scholar] [CrossRef]
- Caponegro, M.D.; Moffitt, R.A.; Tsirka, S.E. Expression of neuropilin-1 is linked to glioma associated microglia and macrophages and correlates with unfavorable prognosis in high grade gliomas. Oncotarget 2018, 9, 35655–35665. [Google Scholar] [CrossRef]
- Yang, C.; Lee, D.-H.; Mangraviti, A.; Su, L.; Zhang, K.; Zhang, Y.; Zhang, B.; Li, W.; Tyler, B.; Wong, J.; et al. Quantitative correlational study of microbubble-enhanced ultrasound imaging and magnetic resonance imaging of glioma and early response to radiotherapy in a rat model. Med. Phys. 2015, 42, 4762–4772. [Google Scholar] [CrossRef]
- Wei, Q.; Singh, O.; Ekinci, C.; Gill, J.; Li, M.; Mamatjan, Y.; Karimi, S.; Bunda, S.; Mansouri, S.; Aldape, K.; et al. TNFα secreted by glioma associated macrophages promotes endothelial activation and resistance against anti-angiogenic therapy. Acta Neuropathol. Commun. 2021, 9, 67. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.-M.; Xia, W.; Hsu, Y.-H.; Chan, L.-C.; Yu, W.-H.; Cha, J.-H.; Chen, C.-T.; Liao, H.-W.; Kuo, C.-W.; Khoo, K.-H.; et al. STT3-dependent PD-L1 accumulation on cancer stem cells promotes immune evasion. Nat. Commun. 2018, 9, 1908. [Google Scholar] [CrossRef] [PubMed]
- Manini, I.; Caponnetto, F.; Dalla, E.; Ius, T.; Pepa, G.; Pegolo, E.; Bartolini, A.; Rocca, G.; Menna, G.; Loreto, C.; et al. Heterogeneity Matters: Different Regions of Glioblastoma Are Characterized by Distinctive Tumor-Supporting Pathways. Cancers 2020, 12, 2960. [Google Scholar] [CrossRef] [PubMed]
- Menna, G.; Manini, I.; Cesselli, D.; Skrap, M.; Olivi, A.; Ius, T.; Della Pepa, G.M. Immunoregulatory effects of glioma-associated stem cells on the glioblastoma peritumoral microenvironment: A differential PD-L1 expression from core to periphery? Neurosurg. Focus 2022, 52, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Altieri, R.; Barbagallo, D.; Certo, F.; Broggi, G.; Ragusa, M.; Di Pietro, C.; Caltabiano, R.; Magro, G.; Peschillo, S.; Purrello, M.; et al. Peritumoral Microenvironment in High-Grade Gliomas: From FLAIRectomy to Microglia–Glioma Cross-Talk. Brain Sci. 2021, 11, 200. [Google Scholar] [CrossRef]
- Yuan, J.X.; Bafakih, F.F.; Mandell, J.W.; Horton, B.J.; Munson, J.M. Quantitative Analysis of the Cellular Microenvironment of Glioblastoma to Develop Predictive Statistical Models of Overall Survival. J. Neuropathol. Exp. Neurol. 2016, 75, 1110–1123. [Google Scholar] [CrossRef][Green Version]
- Zhang, Q.; Wang, J.; Yao, X.; Wu, S.; Tian, W.; Gan, C.; Wan, X.; You, C.; Hu, F.; Zhang, S.; et al. Programmed Cell Death 10 Mediated CXCL2-CXCR2 Signaling in Regulating Tumor-Associated Microglia/Macrophages Recruitment in Glioblastoma. Front. Immunol. 2021, 12, 1933. [Google Scholar] [CrossRef]
- Schiffer, D.; Mellai, M.; Bovio, E.; Bisogno, I.; Casalone, C.; Annovazzi, L. Glioblastoma niches: From the concept to the phenotypical reality. Neurol. Sci. 2018, 39, 1161–1168. [Google Scholar] [CrossRef]
- Schiffer, D.; Annovazzi, L.; Casalone, C.; Corona, C.; Mellai, M. Glioblastoma: Microenvironment and Niche Concept. Cancers 2018, 11, 5. [Google Scholar] [CrossRef]
- Hide, T.; Komohara, Y.; Miyasato, Y.; Nakamura, H.; Makino, K.; Takeya, M.; Kuratsu, J.-I.; Mukasa, A.; Yano, S. Oligodendrocyte Progenitor Cells and Macrophages/Microglia Produce Glioma Stem Cell Niches at the Tumor Border. EBioMedicine 2018, 30, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Westphal, M.; Maire, C.L.; Lamszus, K. EGFR as a Target for Glioblastoma Treatment: An Unfulfilled Promise. CNS Drugs 2017, 31, 723–735. [Google Scholar] [CrossRef]
- Wenger, K.J.; Wagner, M.; You, S.-J.; Franz, K.; Harter, P.N.; Burger, M.C.; Voss, M.; Ronellenfitsch, M.W.; Fokas, E.; Steinbach, J.P.; et al. Bevacizumab as a last-line treatment for glioblastoma following failure of radiotherapy, temozolomide and lomustine. Oncol. Lett. 2017, 14, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Rath, B.H.; Wahba, A.; Camphausen, K.; Tofilon, P.J. Coculture with astrocytes reduces the radiosensitivity yof glioblastoma stem-like cells and identifies additional targets for radiosensitization. Cancer Med. 2015, 4, 1705–1716. [Google Scholar] [CrossRef] [PubMed]
- Litak, J.; Mazurek, M.; Grochowski, C.; Kamieniak, P.; Roliński, J. PD-L1/PD-1 Axis in Glioblastoma Multiforme. Int. J. Mol. Sci. 2019, 20, 5347. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Xu, C. Immune checkpoint signaling and cancer immunotherapy. Cell Res. 2020, 30, 660–669. [Google Scholar] [CrossRef]
- Scheffel, T.B.; Grave, N.; Vargas, P.; Diz, F.M.; Rockenbach, L.; Morrone, F.B. Immunosuppression in Gliomas via PD-1/PD-L1 Axis and Adenosine Pathway. Front. Oncol. 2021, 10, 617385. [Google Scholar] [CrossRef]
- Yao, Y.; Tao, R.; Wang, X.; Wang, Y.; Mao, Y.; Zhou, L.F. B7-H1 is correlated with malignancy-grade gliomas but is not expressed exclusively on tumor stem-like cells. Neuro-Oncology 2009, 11, 757–766. [Google Scholar] [CrossRef]
- Wilmotte, R.; Burkhardt, K.; Kindler, V.; Belkouch, M.-C.; Dussex, G.; De Tribolet, N.; Walker, P.R.; Dietrich, P.-Y. B7-homolog 1 expression by human glioma: A new mechanism of immune evasion. Neuro Report 2005, 16, 1081–1085. [Google Scholar] [CrossRef]
- Xue, S.; Hu, M.; Iyer, V.; Yu, J. Blocking the PD-1/PD-L1 pathway in glioma: A potential new treatment strategy. J. Hematol. Oncol. 2017, 10, 81. [Google Scholar] [CrossRef]
- Li, X.; Yan, S.; Yang, J.; Wang, Y.; Lv, C.; Li, S.; Zhao, J.; Yang, Y.; Zhuo, M.; Wu, N. Efficacy and Safety of PD-1/PD-L1 Inhibitors Plus Chemotherapy Versus PD-1/PD-L1 Inhibitors in Advanced Non-Small Cell Lung Cancer: A Network Analysis of Randomized Controlled Trials. Front. Oncol. 2021, 10, 574752. [Google Scholar] [CrossRef] [PubMed]
- Hao, C.; Chen, G.; Zhao, H.; Li, Y.; Chen, J.; Zhang, H.; Li, S.; Zhao, Y.; Chen, F.; Li, W.; et al. PD-L1 Expression in Glioblastoma, the Clinical and Prognostic Significance: A Systematic Literature Review and Meta-Analysis. Front. Oncol. 2020, 10, 1015. [Google Scholar] [CrossRef] [PubMed]
- Nduom, E.K.; Wei, J.; Yaghi, N.K.; Huang, N.; Kong, L.-Y.; Gabrusiewicz, K.; Ling, X.; Zhou, S.; Ivan, C.; Chen, J.Q.; et al. PD-L1 expression and prognostic impact in glioblastoma. Neuro-Oncology 2015, 18, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Kelly, W.J.; Giles, A.J.; Gilbert, M. T lymphocyte-targeted immune checkpoint modulation in glioma. J. Immunother. Cancer 2019, 8, e000379. [Google Scholar] [CrossRef] [PubMed]
- Litak, J.; Grajkowska, W.; Szumiło, J.; Krukow, P.; Maciejewski, R.; Roliński, J.; Grochowski, C. PD-L1 Expression Correlated with p53 Expression in Pediatric Glioblastoma Multiforme. Brain Sci. 2021, 11, 262. [Google Scholar] [CrossRef]
- Alexander, B.M.; Ba, S.; Berger, M.S.; Berry, D.A.; Cavenee, W.K.; Chang, S.M.; Cloughesy, T.F.; Jiang, T.; Khasraw, M.; Li, W. GBMAGILE Network. Adaptive global innovative learning environment for glioblastoma: GBMAGILE. Clin. Cancer Res. 2018, 24, 737–743. [Google Scholar] [CrossRef]
- Alexander, B.M.; Trippa, L.; Gaffey, S.C.; Arrillaga, I.; Lee, E.Q.; Tanguturi, S.K.; Ahluwalia, M.S.; Colman, H.; Galanis, E.; De Groot, J.F. Individualized screening trial of innovative glioblastoma therapy (INSIGhT). J. Clin. Oncol. 2017, 35, TPS2079. [Google Scholar] [CrossRef]
- Walentynowicz, K.A.; Ochocka, N.; Pasierbińska, M.; Wojnicki, K.; Stepniak, K.; Mieczkowski, J.; Ciechomska, I.; Kaminska, B. In Search for Reliable Markers of Glioma-Induced Polarization of Microglia. Front. Immunol. 2018, 9, 1329. [Google Scholar] [CrossRef]
- Szulzewsky, F.; Pelz, A.; Feng, X.; Synowitz, M.; Markovic, D.; Langmann, T.; Holtman, I.R.; Wang, X.; Eggen, B.J.L.; Boddeke, H.W.G.M.; et al. Glioma-Associated Microglia/Macrophages Display an Expression Profile Different from M1 and M2 Polarization and Highly Express Gpnmb and Spp1. PLoS ONE 2015, 10, e0116644. [Google Scholar] [CrossRef]
- La Rocca, G.; Sabatino, G.; Menna, G.; Altieri, R.; Ius, T.; Marchese, E.; Olivi, A.; Barresi, V.; Della Pepa, G.M. 5-Aminolevulinic Acid False Positives in Cerebral Neuro-Oncology: Not All That Is Fluorescent Is Tumor. A Case-Based Update and Literature Review. World Neurosurg. 2020, 137, 187–193. [Google Scholar] [CrossRef]
- Mieczkowski, J.; Kocyk, M.; Nauman, P.; Gabrusiewicz, K.; Sielska, M.; Przanowski, P.; Maleszewska, M.; Rajan, W.D.; Pszczolkowska, D.; Tykocki, T.; et al. Down-regulation of IKKβ expression in glioma-infiltrating microglia/macrophages is associated with defective inflammatory/immune gene responses in glioblastoma. Oncotarget 2015, 6, 33077–33090. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).