Clinical Relevance of Mortalin in Ovarian Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients Characteristic and Sample Collection
2.2. Sample Preparation
2.3. Soluble Mortalin Measurement
2.4. Isolation of Cells and Flow Cytometry
2.5. Mortalin Protein Analysis
2.6. Bioinformatics Analysis
2.7. Kaplan–Meier Analysis
2.8. Statistical Analysis
3. Results
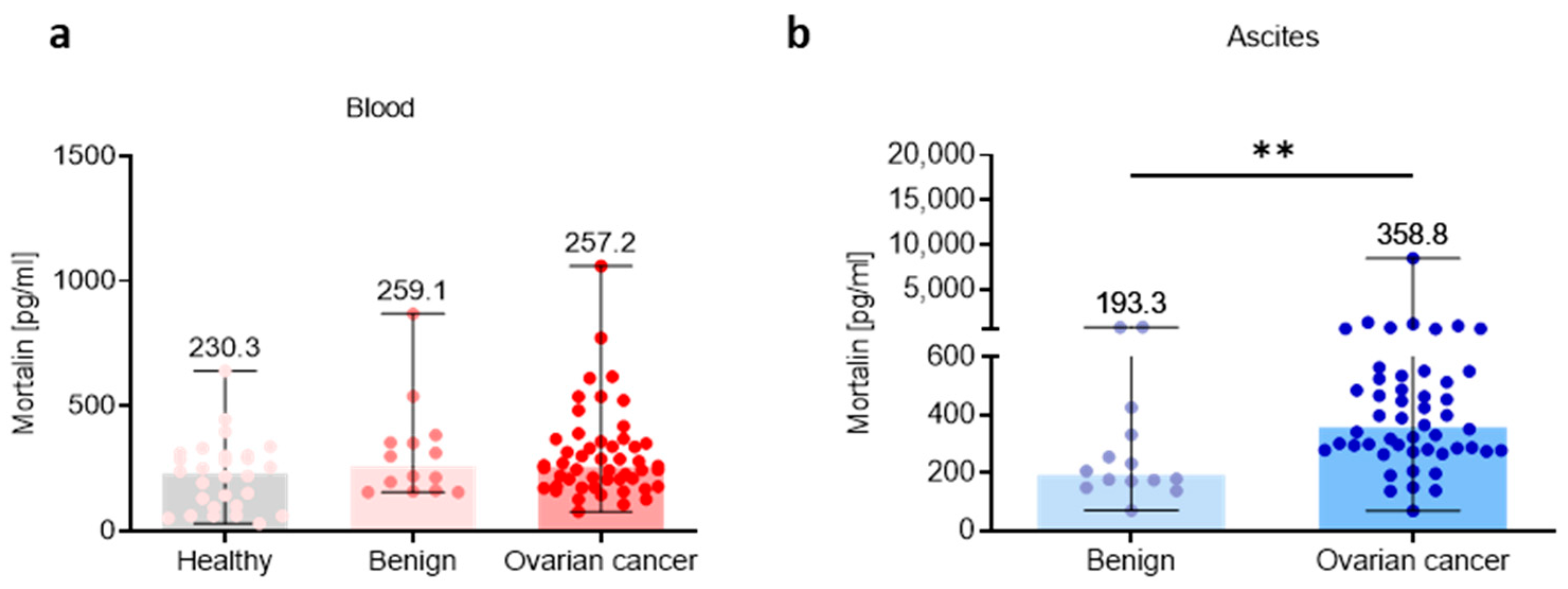
3.1. Mortalin Is Upregulated in Local Tumor Environments in Ovarian Cancer Patients
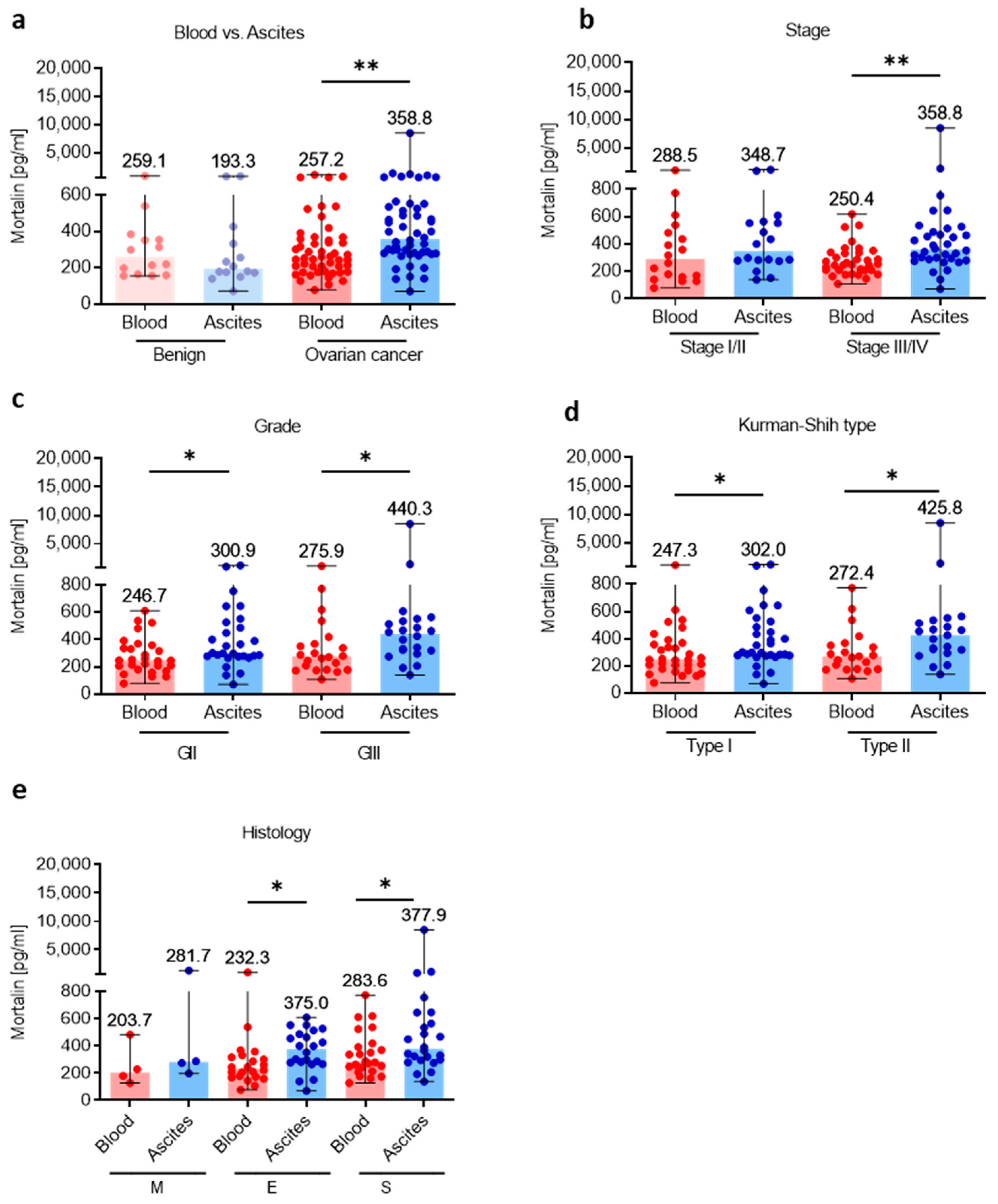
3.2. Mortalin Levels Are Higher in Local Ascites Tumor Environment Compared with Adjacent Peripheral Blood Environment
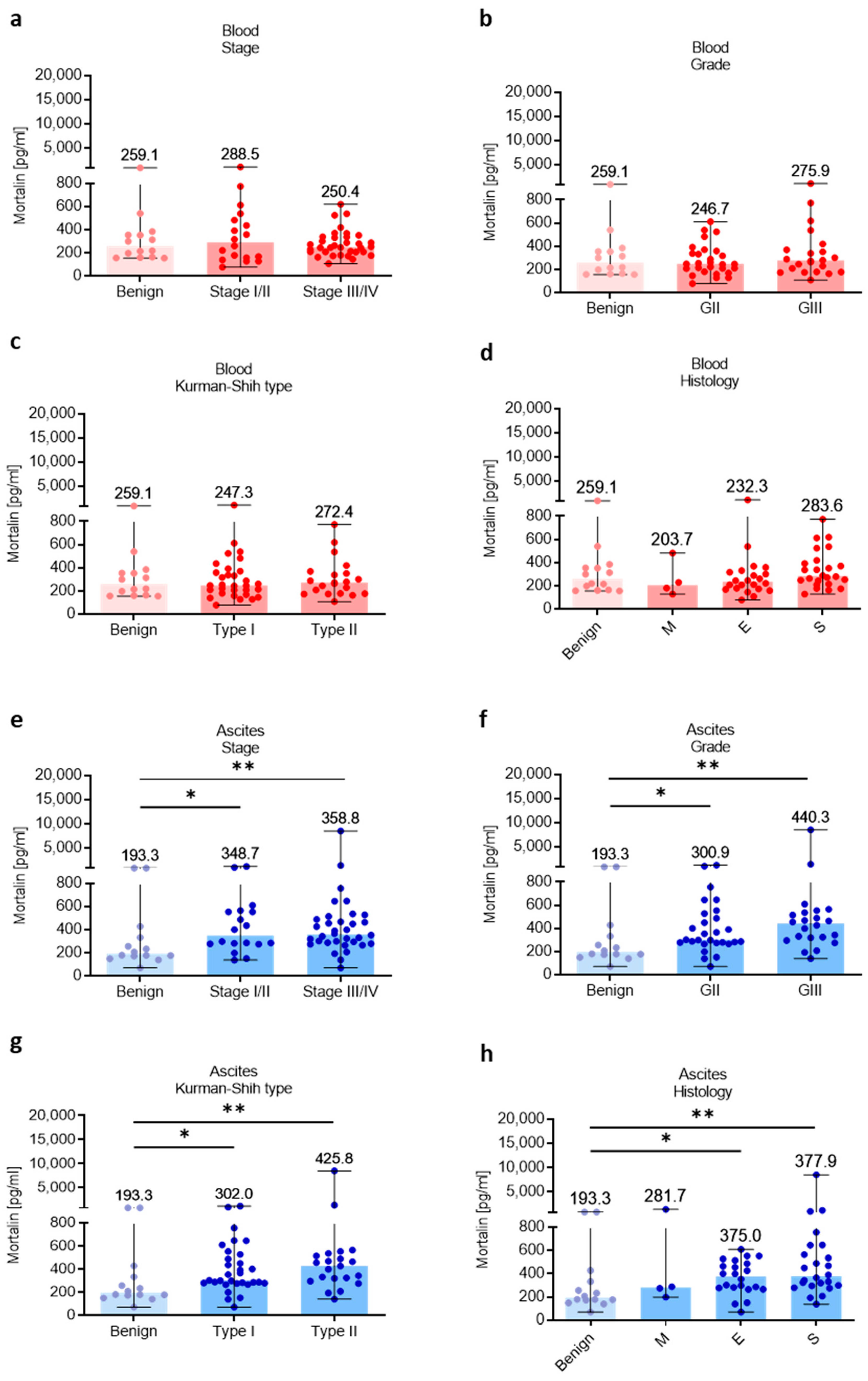
3.3. Association of Mortalin Levels with Clinicopathological Features
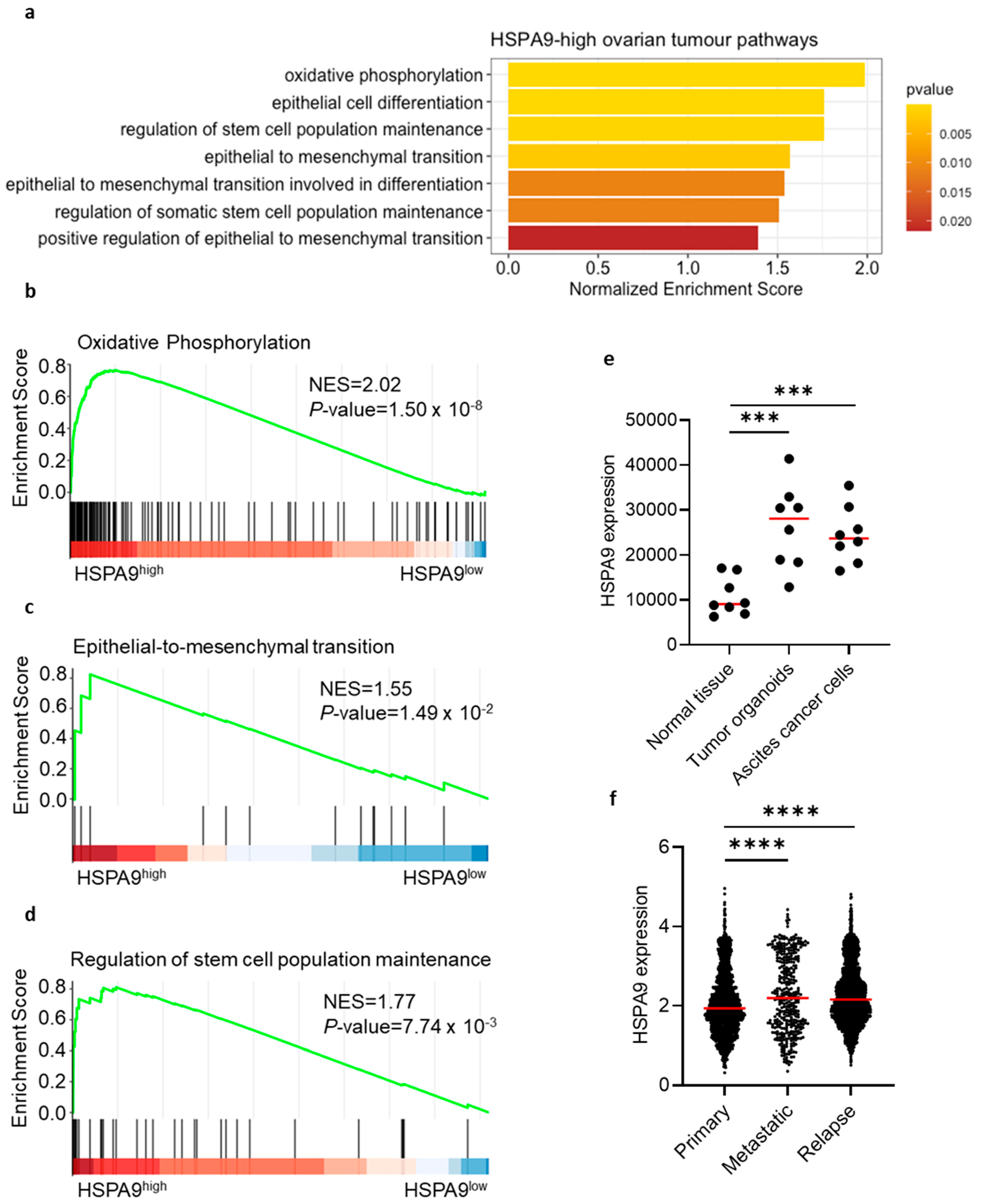
3.4. Mortalin Gene Expression Correlates with Cancer-Driven Gene Signatures and Is Associated with Worse Clinical Outcome
3.5. High Tumor Mortalin Levels Predict Poor Prognosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2019. CA A Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Curtis, M.; Mukherjee, A.; Lengyel, E. The Tumor Microenvironment Takes Center Stage in Ovarian Cancer Metastasis. Trends Cancer 2018, 4, 517–519. [Google Scholar] [CrossRef] [PubMed]
- Okła, K.; Wertel, I.; Polak, G.; Surówka, J.; Wawruszak, A.; Kotarski, J. Tumor-Associated Macrophages and Myeloid-Derived Suppressor Cells as Immunosuppressive Mechanism in Ovarian Cancer Patients: Progress and Challenges. Int. Rev. Immunol. 2016, 35, 372–385. [Google Scholar] [CrossRef] [PubMed]
- Okła, K.; Surówka, J.; Frąszczak, K.; Czerwonka, A.; Kaławaj, K.; Wawruszak, A.; Kotarski, J.; Wertel, I. Assessment of the Clinicopathological Relevance of Mesothelin Level in Plasma, Peritoneal Fluid, and Tumor Tissue of Epithelial Ovarian Cancer Patients. Tumour Biol. 2018, 40, 1010428318804937. [Google Scholar] [CrossRef]
- Okła, K.; Czerwonka, A.; Wawruszak, A.; Bobiński, M.; Bilska, M.; Tarkowski, R.; Bednarek, W.; Wertel, I.; Kotarski, J. Clinical Relevance and Immunosuppressive Pattern of Circulating and Infiltrating Subsets of Myeloid-Derived Suppressor Cells (MDSCs) in Epithelial Ovarian Cancer. Front. Immunol. 2019, 10, 691. [Google Scholar] [CrossRef]
- Want, M.Y.; Lugade, A.A.; Battaglia, S.; Odunsi, K. Nature of Tumour Rejection Antigens in Ovarian Cancer. Immunology 2018, 155, 202–210. [Google Scholar] [CrossRef]
- Colombo, N.; Lorusso, D.; Scollo, P. Impact of Recurrence of Ovarian Cancer on Quality of Life and Outlook for the Future. Int. J. Gynecol. Cancer 2017, 27, 1134–1140. [Google Scholar] [CrossRef]
- Coleman, R.L.; Monk, B.J.; Sood, A.K.; Herzog, T.J. Latest Research and Clinical Treatment of Advanced-Stage Epithelial Ovarian Cancer. Nat. Rev. Clin. Oncol. 2013, 10, 211–224. [Google Scholar] [CrossRef]
- Marth, C.; Wieser, V.; Tsibulak, I.; Zeimet, A.G. Immunotherapy in Ovarian Cancer: Fake News or the Real Deal? Int. J. Gynecol. Cancer 2019, 29, 201–211. [Google Scholar] [CrossRef]
- Binnewies, M.; Roberts, E.W.; Kersten, K.; Chan, V.; Fearon, D.F.; Merad, M.; Coussens, L.M.; Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Hedrick, C.C.; et al. Understanding the Tumor Immune Microenvironment (TIME) for Effective Therapy. Nat. Med. 2018, 24, 541–550. [Google Scholar] [CrossRef]
- Rodriguez, G.M.; Galpin, K.J.C.; McCloskey, C.W.; Vanderhyden, B.C. The Tumor Microenvironment of Epithelial Ovarian Cancer and Its Influence on Response to Immunotherapy. Cancers 2018, 10, 242. [Google Scholar] [CrossRef] [PubMed]
- Drakes, M.L.; Stiff, P.J. Regulation of Ovarian Cancer Prognosis by Immune Cells in the Tumor Microenvironment. Cancers 2018, 10, 302. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, R.; Takano, S.; Kaur, K.; Deocaris, C.C.; Pereira-Smith, O.M.; Reddel, R.R.; Kaul, S.C. Upregulation of Mortalin/Mthsp70/Grp75 Contributes to Human Carcinogenesis. Int. J. Cancer 2006, 118, 2973–2980. [Google Scholar] [CrossRef]
- Yun, C.W.; Kim, H.J.; Lim, J.H.; Lee, S.H. Heat Shock Proteins: Agents of Cancer Development and Therapeutic Targets in Anti-Cancer Therapy. Cells 2019, 9, 60. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Xiong, X.; Ren, X.; Yang, J.-M.; Song, J. Heat Shock Proteins in Cancer Immunotherapy. J. Oncol. 2019, 2019, 3267207. [Google Scholar] [CrossRef] [PubMed]
- Asea, A.; Kraeft, S.-K.; Kurt-Jones, E.A.; Stevenson, M.A.; Chen, L.B.; Finberg, R.W.; Koo, G.C.; Calderwood, S.K. HSP70 Stimulates Cytokine Production through a CD14-Dependant Pathway, Demonstrating Its Dual Role as a Chaperone and Cytokine. Nat. Med. 2000, 6, 435–442. [Google Scholar] [CrossRef]
- Rozenberg, P.; Kocsis, J.; Saar, M.; Prohászka, Z.; Füst, G.; Fishelson, Z. Elevated Levels of Mitochondrial Mortalin and Cytosolic HSP70 in Blood as Risk Factors in Patients with Colorectal Cancer. Int. J. Cancer 2013, 133, 514–518. [Google Scholar] [CrossRef]
- Sun, J.; Che, S.-L.; Piao, J.-J.; Xu, M.; Chen, L.-Y.; Lin, Z.-H. Mortalin Overexpression Predicts Poor Prognosis in Early Stage of Non-Small Cell Lung Cancer. Tumour Biol. 2017, 39, 1010428317695918. [Google Scholar] [CrossRef]
- Cui, X.; Li, Z.; Piao, J.; Li, J.; Li, L.; Lin, Z.; Jin, A. Mortalin Expression in Pancreatic Cancer and Its Clinical and Prognostic Significance. Hum. Pathol. 2017, 64, 171–178. [Google Scholar] [CrossRef]
- Na, Y.; Kaul, S.C.; Ryu, J.; Lee, J.-S.; Ahn, H.M.; Kaul, Z.; Kalra, R.S.; Li, L.; Widodo, N.; Yun, C.-O.; et al. Stress Chaperone Mortalin Contributes to Epithelial-to-Mesenchymal Transition and Cancer Metastasis. Cancer Res. 2016, 76, 2754–2765. [Google Scholar] [CrossRef]
- Yun, C.-O.; Bhargava, P.; Na, Y.; Lee, J.-S.; Ryu, J.; Kaul, S.C.; Wadhwa, R. Relevance of Mortalin to Cancer Cell Stemness and Cancer Therapy. Sci. Rep. 2017, 7, 42016. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Li, H.; Jiang, Y.; Zuo, J.; Liu, W. Inhibition of Mortalin Expression Reverses Cisplatin Resistance and Attenuates Growth of Ovarian Cancer Cells. Cancer Lett. 2013, 336, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Jubran, R.; Kocsis, J.; Garam, N.; Maláti, É.; Gombos, T.; Barabás, L.; Gráf, L.; Prohászka, Z.; Fishelson, Z. Circulating Mitochondrial Stress 70 Protein/Mortalin and Cytosolic Hsp70 in Blood: Risk Indicators in Colorectal Cancer. Int. J. Cancer 2017, 141, 2329–2335. [Google Scholar] [CrossRef]
- Kurman, R.J.; Shih, I.-M. The Dualistic Model of Ovarian Carcinogenesis. Am. J. Pathol. 2016, 186, 733–747. [Google Scholar] [CrossRef]
- Ellis, M.J.; Gillette, M.; Carr, S.A.; Paulovich, A.G.; Smith, R.D.; Rodland, K.K.; Townsend, R.R.; Kinsinger, C.; Mesri, M.; Rodriguez, H.; et al. Connecting Genomic Alterations to Cancer Biology with Proteomics: The NCI Clinical Proteomic Tumor Analysis Consortium. Cancer Discov. 2013, 3, 1108–1112. [Google Scholar] [CrossRef]
- McDermott, J.E.; Arshad, O.A.; Petyuk, V.A.; Fu, Y.; Gritsenko, M.A.; Clauss, T.R.; Moore, R.J.; Schepmoes, A.A.; Zhao, R.; Monroe, M.E.; et al. Proteogenomic Characterization of Ovarian HGSC Implicates Mitotic Kinases, Replication Stress in Observed Chromosomal Instability. Cell Rep. Med. 2020, 1, 100004. [Google Scholar] [CrossRef]
- Huang, D.; Chowdhury, S.; Wang, H.; Savage, S.R.; Ivey, R.G.; Kennedy, J.J.; Whiteaker, J.R.; Lin, C.; Hou, X.; Oberg, A.L.; et al. Multiomic Analysis Identifies CPT1A as a Potential Therapeutic Target in Platinum-Refractory, High-Grade Serous Ovarian Cancer. Cell Rep. Med. 2021, 2, 100471. [Google Scholar] [CrossRef]
- Carvalho, R.F.; do Canto, L.M.; Abildgaard, C.; Aagaard, M.M.; Tronhjem, M.S.; Waldstrøm, M.; Jensen, L.H.; Steffensen, K.D.; Rogatto, S.R. Single-Cell and Bulk RNA Sequencing Reveal Ligands and Receptors Associated with Worse Overall Survival in Serous Ovarian Cancer. Cell Commun. Signal. 2022, 20, 176. [Google Scholar] [CrossRef]
- Gyorffy, B.; Lánczky, A.; Szállási, Z. Implementing an Online Tool for Genome-Wide Validation of Survival-Associated Biomarkers in Ovarian-Cancer Using Microarray Data from 1287 Patients. Endocr. Relat. Cancer 2012, 19, 197–208. [Google Scholar] [CrossRef]
- Rickard, B.P.; Conrad, C.; Sorrin, A.J.; Ruhi, M.K.; Reader, J.C.; Huang, S.A.; Franco, W.; Scarcelli, G.; Polacheck, W.J.; Roque, D.M.; et al. Malignant Ascites in Ovarian Cancer: Cellular, Acellular, and Biophysical Determinants of Molecular Characteristics and Therapy Response. Cancers 2021, 13, 4318. [Google Scholar] [CrossRef] [PubMed]
- Okła, K.; Rajtak, A.; Czerwonka, A.; Bobiński, M.; Wawruszak, A.; Tarkowski, R.; Bednarek, W.; Szumiło, J.; Kotarski, J. Accumulation of Blood-Circulating PD-L1-Expressing M-MDSCs and Monocytes/Macrophages in Pretreatment Ovarian Cancer Patients Is Associated with Soluble PD-L1. J. Transl. Med. 2020, 18, 220. [Google Scholar] [CrossRef] [PubMed]
- Kocsis, J.; Madaras, B.; Tóth, É.K.; Füst, G.; Prohászka, Z. Serum Level of Soluble 70-KD Heat Shock Protein Is Associated with High Mortality in Patients with Colorectal Cancer without Distant Metastasis. Cell Stress Chaperones 2010, 15, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Sriramkumar, S.; Sood, R.; Huntington, T.D.; Ghobashi, A.H.; Vuong, T.T.; Metcalfe, T.X.; Wang, W.; Nephew, K.P.; O’Hagan, H.M. Platinum-Induced Mitochondrial OXPHOS Contributes to Cancer Stem Cell Enrichment in Ovarian Cancer. J. Transl. Med. 2022, 20, 246. [Google Scholar] [CrossRef] [PubMed]
- Dar, S.; Chhina, J.; Mert, I.; Chitale, D.; Buekers, T.; Kaur, H.; Giri, S.; Munkarah, A.; Rattan, R. Bioenergetic Adaptations in Chemoresistant Ovarian Cancer Cells. Sci. Rep. 2017, 7, 8760. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Yang, L.; Yang, Y.; Han, Y.; Wang, Y.; Liu, W.; Zuo, J. Oncogenic Role of Mortalin Contributes to Ovarian Tumorigenesis by Activating the MAPK–ERK Pathway. J. Cell. Mol. Med. 2016, 20, 2111–2121. [Google Scholar] [CrossRef] [PubMed]
- Santegoets, S.J.A.M.; de Groot, A.F.; Dijkgraaf, E.M.; Simões, A.M.C.; van der Noord, V.E.; van Ham, J.J.; Welters, M.J.P.; Kroep, J.R.; van der Burg, S.H. The Blood MMDSC to DC Ratio Is a Sensitive and Easy to Assess Independent Predictive Factor for Epithelial Ovarian Cancer Survival. Oncoimmunology 2018, 7, e1465166. [Google Scholar] [CrossRef]

| Category | Blood | Ascites |
|---|---|---|
| Healthy women, N | 28 | NA |
| Benign, N | 14 | 14 |
| Ovarian cancer, N | 50 | 50 |
| Age at diagnosis, mean (min–max) | ||
| Healthy women | 40.58 (25–66) | NA |
| Benign | 49.71 (23–86) | 49.71 (23–86) |
| Ovarian cancer | 58.56 (20–86) | 58.56 (20–86) |
| Stage, N | ||
| Early I/II | 18 (36.1) | 18 (36.1) |
| Advanced III/IV | 32 (63.9) | 32. (63.9) |
| Grade, N | ||
| II | 28 | 28 |
| III | 22 | 22 |
| Kurman–Shih type, N | ||
| I | 30 | 30 |
| II | 20 | 20 |
| Histology, N | ||
| Mucinous | 4 | 4 |
| Endometrioid | 22 | 22 |
| Serous | 24 | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajtak, A.; Czerwonka, A.; Pitter, M.; Kotarski, J.; Okła, K. Clinical Relevance of Mortalin in Ovarian Cancer Patients. Cells 2023, 12, 701. https://doi.org/10.3390/cells12050701
Rajtak A, Czerwonka A, Pitter M, Kotarski J, Okła K. Clinical Relevance of Mortalin in Ovarian Cancer Patients. Cells. 2023; 12(5):701. https://doi.org/10.3390/cells12050701
Chicago/Turabian StyleRajtak, Alicja, Arkadiusz Czerwonka, Michael Pitter, Jan Kotarski, and Karolina Okła. 2023. "Clinical Relevance of Mortalin in Ovarian Cancer Patients" Cells 12, no. 5: 701. https://doi.org/10.3390/cells12050701
APA StyleRajtak, A., Czerwonka, A., Pitter, M., Kotarski, J., & Okła, K. (2023). Clinical Relevance of Mortalin in Ovarian Cancer Patients. Cells, 12(5), 701. https://doi.org/10.3390/cells12050701







