Immediately Placed Single Locking-Taper Implants in the Aesthetic Area of Upper Maxilla: A Short-Term Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
- -
- having had a single-tooth replacement with one single locking-taper plateau-design implant [16] in the aesthetic upper jaw, in the area between the upper right canine and the upper left canine;
- -
- being compliant with a regular maintenance program (professional oral hygiene sessions every 4 months) [16];
- -
- having complete clinical, photographic, and radiographic documentation.
2.3. Implant System
- -
- a plateau root-form design: the absence of micro-gaps and micro-movements confers greater mechanical stability to the implant-crown assembly and allows for minimal bone resorption [24];
- -
- a convergent crest module (Sloping Shoulder®): the implant shoulder gradually slopes inward and coronally toward the IAI, creating space for crestal bone even in the presence of narrow ridges or areas with limited restorative space;
- -
- a locking-taper screwless implant-abutment connection (IAI) [16]: when the conical shape abutment (1.5° angle) is activated by gentle tapping, a locking-taper occurs; specifically, the 2 surfaces of the same metal (Ti V 6 A14) rub together in such a way that the metals enter in intimate contact [25] to create a hermetic seal (cold fusion) that provides a frictional bacterial seal against microbial penetration or infiltration [26,27].
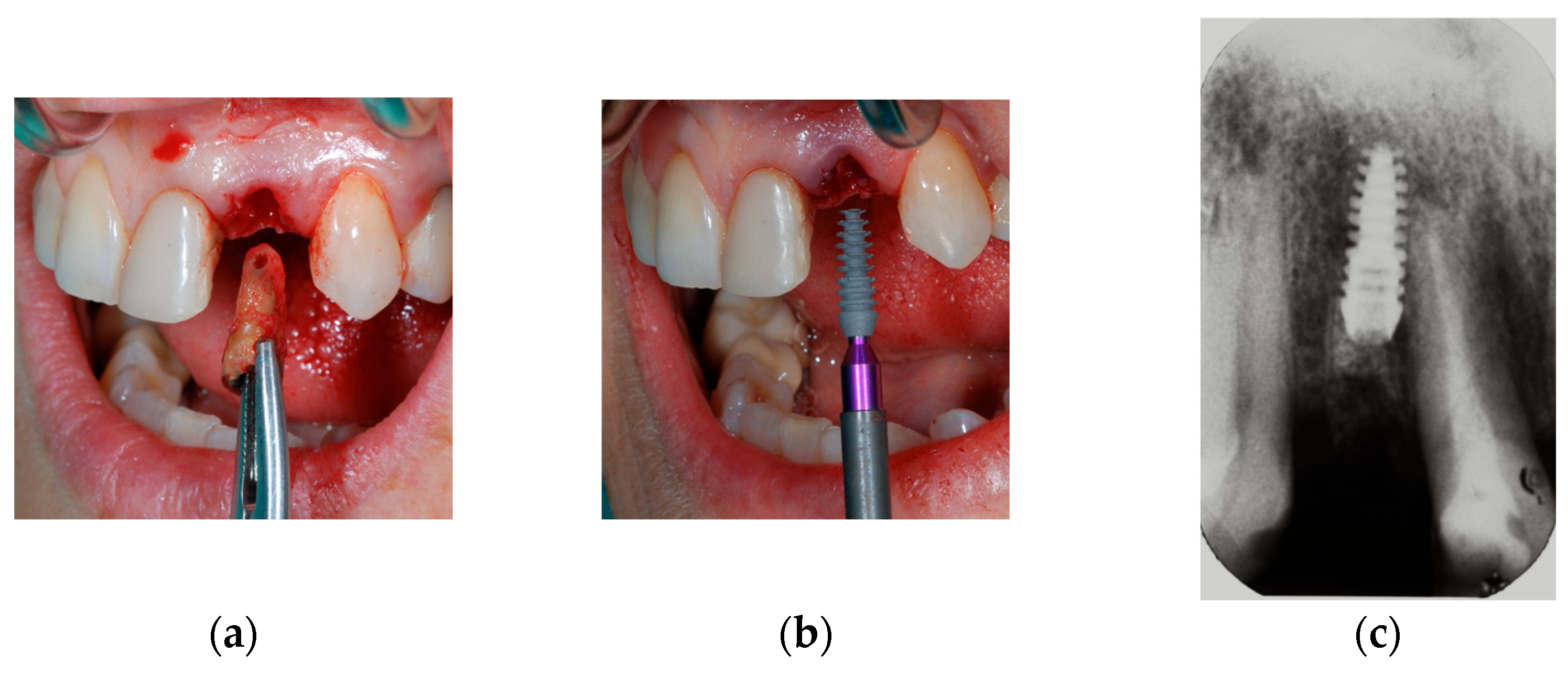
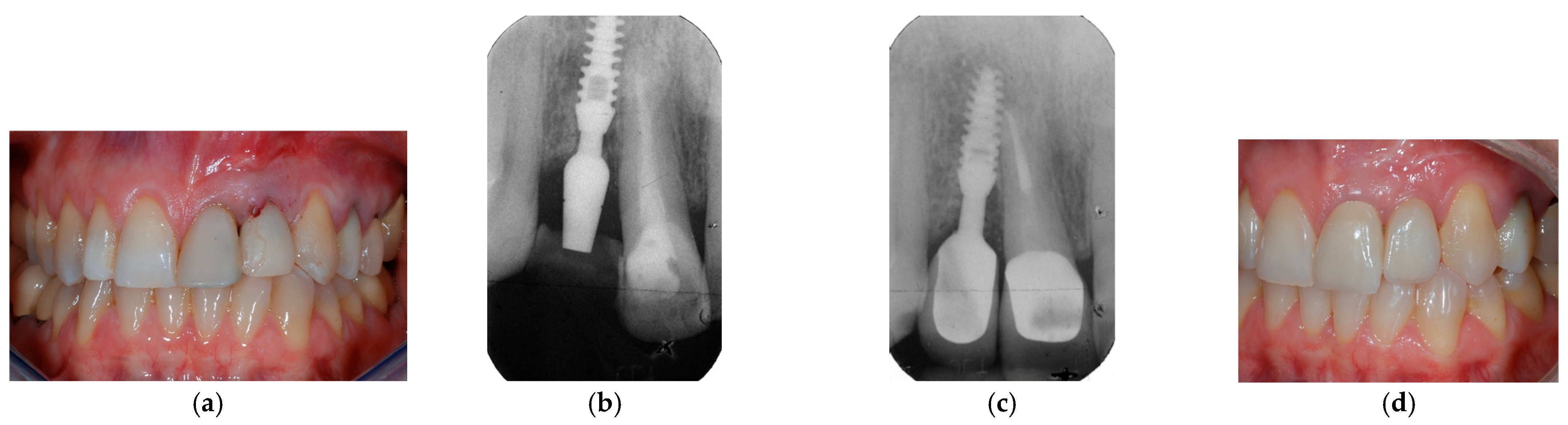
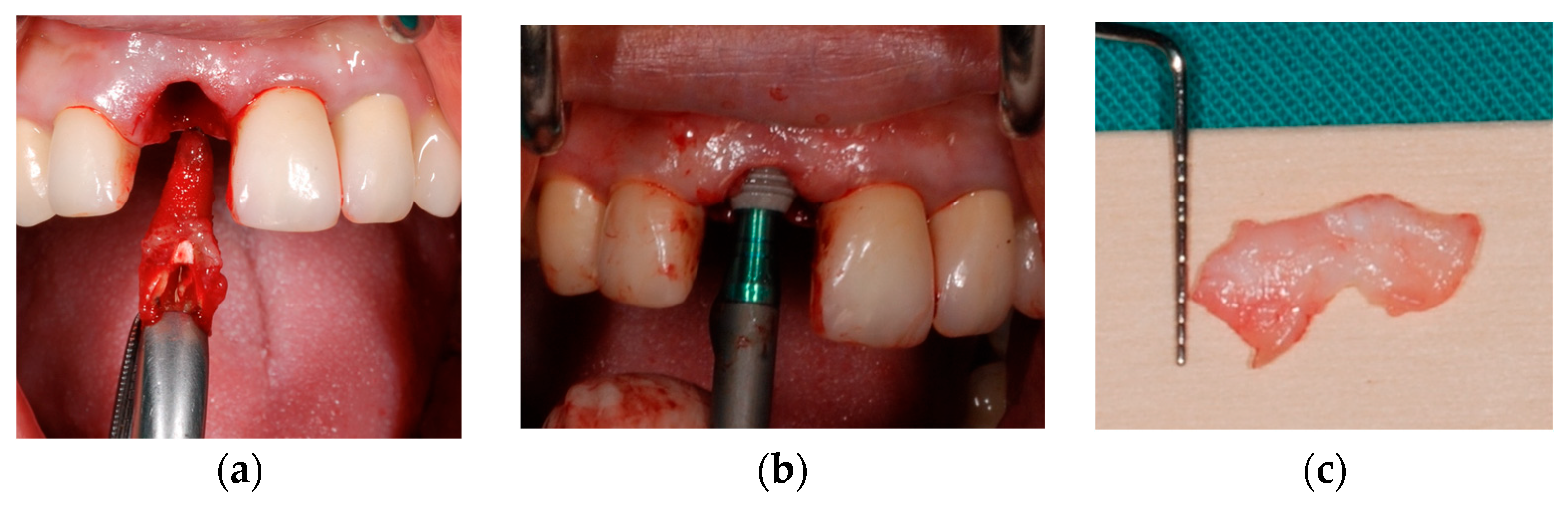
2.4. Surgical Protocol
2.5. Prosthetic Protocol
2.6. Photographic Measurements of Variations in (i) Papillae Height and (ii) Gingival Margin Position
- -
- Mesial papilla height: the distance of MP from RL;
- -
- Distal papilla height: the distance of DP from RL;
- -
- Recession (REC): the difference between the distance of GM from RL at T0 or at T1;
- -
- Keratinized tissue (KT) width: the distance of GM from MGJ.
2.7. Aesthetic Outcomes in Relation to the Use of CTG and Patient’s Phenotype
- -
- thin: thin phenotype without CTG;
- -
- thin + CTG: thin phenotype with CTG;
- -
- thick: thick phenotype without CTG;
- -
- thick + CTG: a thick phenotype with CTG.
2.8. Statistical Analysis
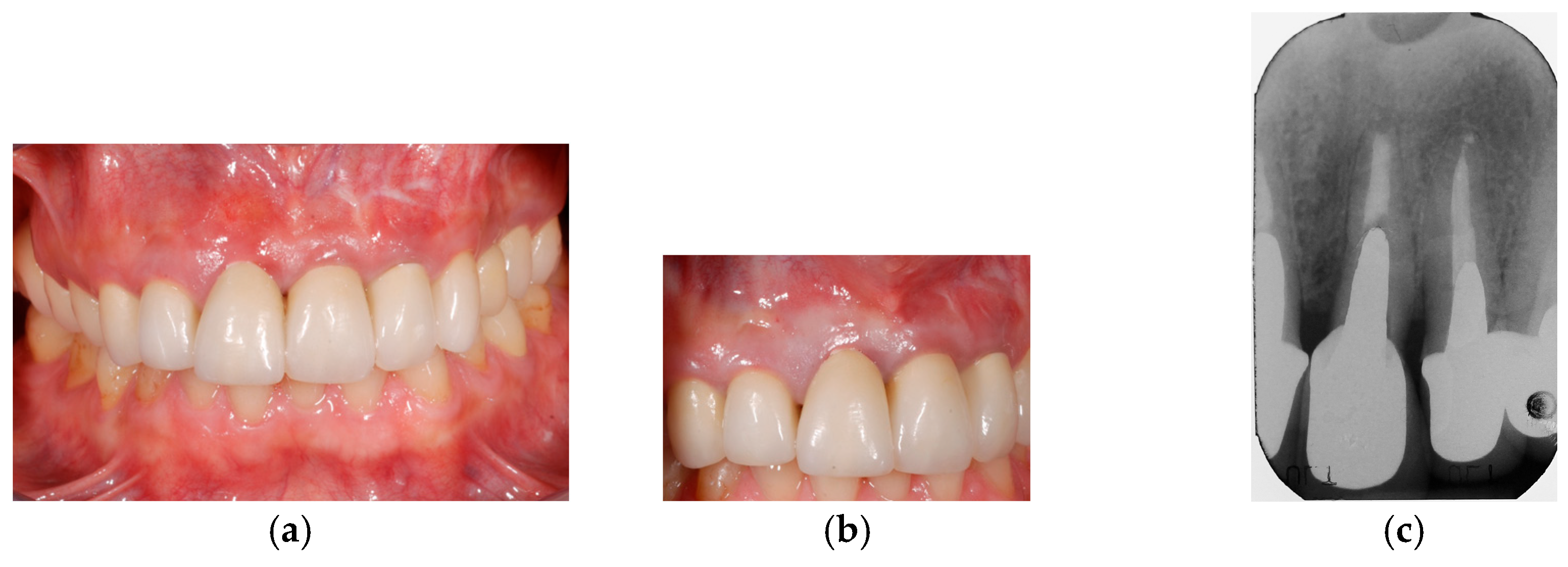
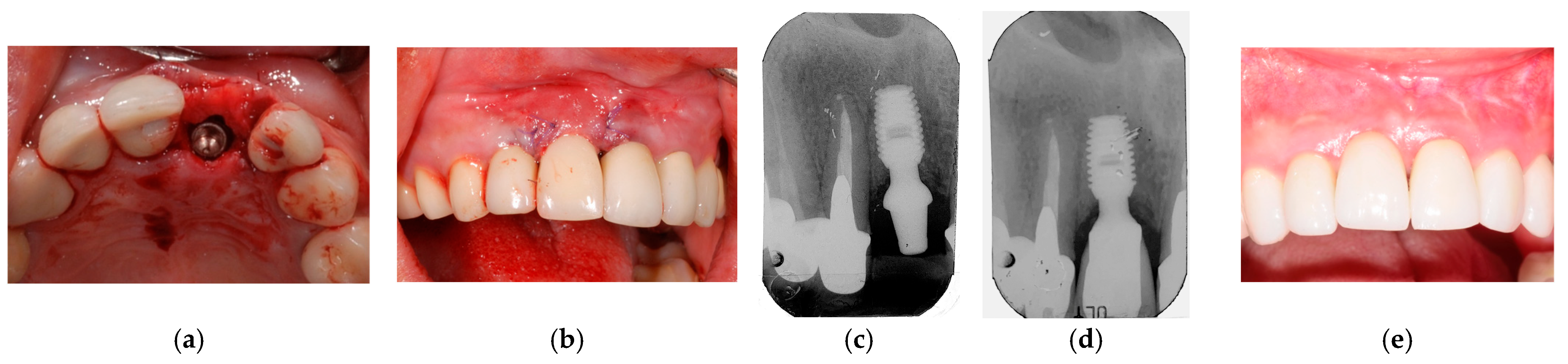
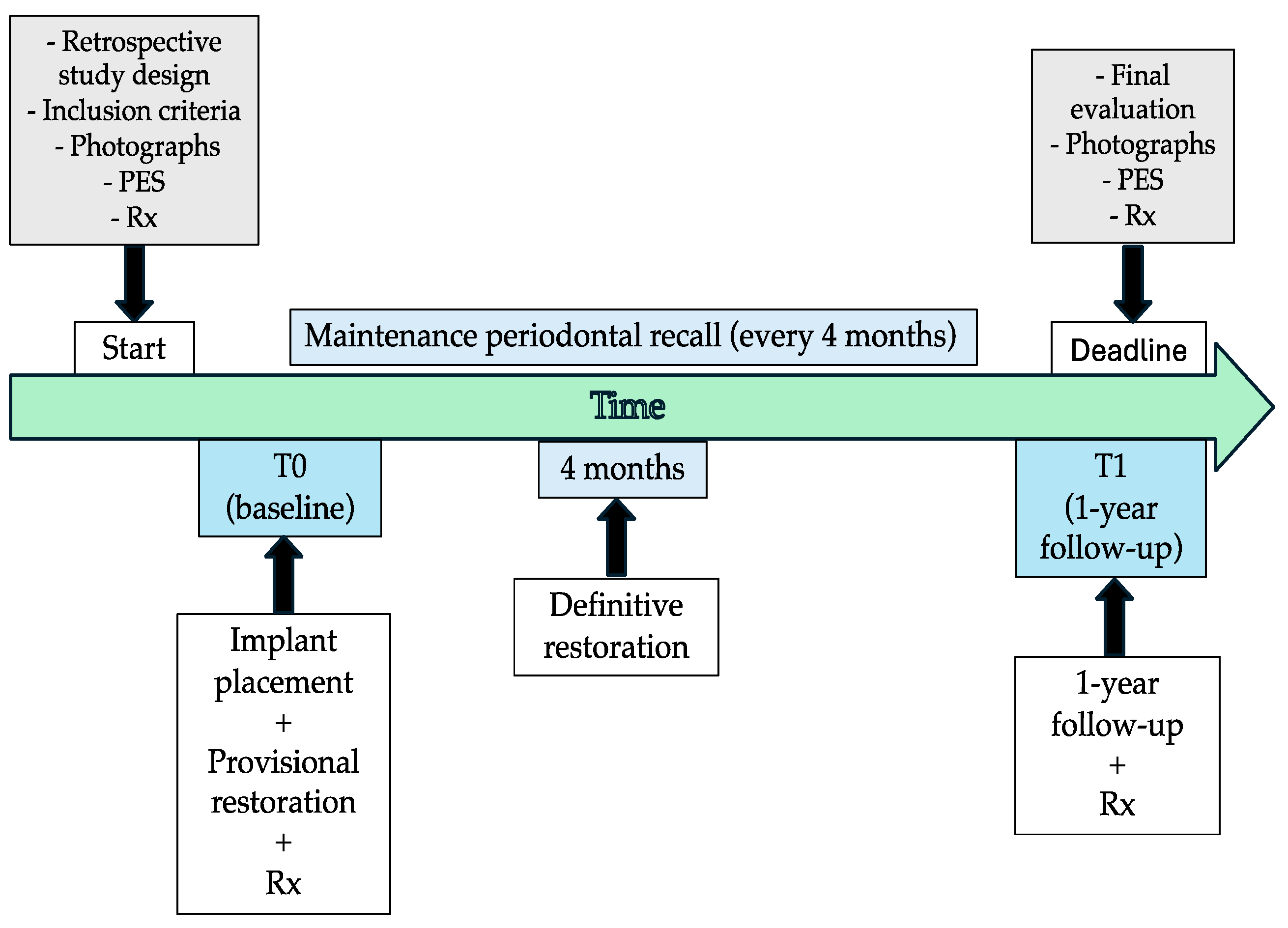
2.9. Clinical Cases and Study Diagram
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Pink Esthetic Score | PES |
| connective tissue graft | CTG |
| implant-abutment connection | IAI |
| mucogingival line | MGJ |
| mesial papilla | MP |
| distal papilla | DP |
| gingival/mucosal margin | GM |
| reference line | RL |
| recession | REC |
| keratinized tissue | KT |
References
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Araújo, M.G.; Silva, C.O.; Souza, A.B.; Sukekava, F. Socket healing with and without immediate implant placement. Periodontol. 2000 2019, 79, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.D.; Chen, S.T. Esthetic outcomes of immediate implant placements. Clin. Oral Implant. Res. 2008, 19, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Lozada, J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int. J. Oral Maxillofac. Implant. 2003, 18, 31–39. [Google Scholar]
- Rosenquist, B.; Grenthe, B. Immediate placement of implants into extraction sockets: Implant survival. Int. J. Oral Maxillofac. Implant. 1996, 11, 205–209. [Google Scholar] [CrossRef]
- Chen, S.T.; Wilson, T.G., Jr.; Hämmerle, C.H. Immediate or early placement of implants following tooth extraction: Review of biologic basis, clinical procedures, and outcomes. Int. J. Oral Maxillofac. Implant. 2004, 19, 12–25. [Google Scholar]
- Kan, J.Y.K.; Yin, S.; Rungcharassaeng, K.; Zucchelli, G.; Urban, I.; Lozada, J. Facial implant gingival level and thickness changes following maxillary anterior immediate tooth replacement with scarf-connective tissue graft: A 4–13-year retrospective study. J. Esthet. Restor. Dent. 2023, 35, 138–147. [Google Scholar] [CrossRef]
- Belser, U.C.; Bernard, J.P.; Buser, D. Implant-supported restorations in the anterior region: Prosthetic considerations. Pract. Periodontics Aesthet. Dent. 1996, 8, 875–883. [Google Scholar]
- Belser, U.C.; Buser, D.; Hess, D.; Schmid, B.; Bernard, J.P.; Lang, N.P. Aesthetic implant restorations in partially edentulous patients—A critical appraisal. Periodontol. 2000 1998, 17, 132–150. [Google Scholar] [CrossRef]
- Grunder, U.; Gracis, S.; Capelli, M. Influence of the 3-D bone-to-implant relationship on esthetics. Int. J. Periodontics Restor. Dent. 2005, 25, 113–119. [Google Scholar]
- Juodzbalys, G.; Wang, H.L. Soft and hard tissue assessment of immediate implant placement: A case series. Clin. Oral Implant. Res. 2007, 18, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Darby, I.B.; Adams, G.G.; Reynolds, E.C. A prospective clinical study of bone augmentation techniques at immediate implants. Clin. Oral Implant. Res. 2005, 16, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Meijndert, L.; Meijer, H.J.; Stellingsma, K.; Stegenga, B.; Raghoebar, G.M. Evaluation of aesthetics of implant-supported single-tooth replacements using different bone augmentation procedures: A prospective randomized clinical study. Clin. Oral Implant. Res. 2007, 18, 715–719. [Google Scholar] [CrossRef]
- Cordaro, L. Implants for restoration of single tooth spaces in areas of high esthetic risk. In The SAC Classification in Implant Dentistry, 2nd ed.; Dawson, A., Martin, W., Polido, W.D., Eds.; Quintessence Publishing: Berlin, Germany, 2009; pp. 50–56. [Google Scholar]
- King, G.N.; Hermann, J.S.; Schoolfield, J.D.; Buser, D.; Cochran, D.L. Influence of the size of the microgap on crestal bone levels in non-submerged dental implants: A radiographic study in the canine mandible. J. Periodontol. 2002, 73, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Liboni, P.; Bonfante, E.A.; Nocini, P.F. Survival rates of ultra-short (<6 mm) compared with short locking-taper implants supporting single crowns in posterior areas: A 5-year retrospective study. Clin. Implant. Dent. Relat. Res. 2021, 23, 904–919. [Google Scholar]
- Lombardo, G.; Corrocher, G.; Pighi, J.; Mascellaro, A.; Marincola, M.; Nocini, P.F. Esthetic Outcomes of Immediately Loaded Locking Taper Implants in the Anterior Maxilla: A Case Series Study. J. Oral Implantol. 2016, 42, 258–264. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Bornstein, M.M.; Wittneben, J.G.; Frei, M.; Belser, U.C. Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: A prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up. J. Periodontol. 2013, 84, 1517–1527. [Google Scholar] [CrossRef]
- Belser, U.C.; Grütter, L.; Vailati, F.; Bornstein, M.M.; Weber, H.P.; Buser, D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J. Periodontol. 2009, 80, 140–151. [Google Scholar] [CrossRef]
- Fürhauser, R.; Florescu, D.; Benesch, T.; Haas, R.; Mailath, G.; Watzek, G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin. Oral Implant. Res. 2005, 16, 639–644. [Google Scholar] [CrossRef]
- Dursun, E.; Lin, G.H.; Taheri, S.; Chu, S.J.; Wang, H.L.; Tözüm, T.F. A Comparison of Esthetic Features of Pre-existing Natural Tooth Versus Post-Implant Restoration in the Esthetic Zone: A Retrospective 12-month Follow-up. Int. J. Oral Maxillofac. Implant. 2018, 33, 919–928. [Google Scholar] [CrossRef]
- Hartlev, J.; Kohberg, P.; Ahlmann, S.; Andersen, N.T.; Schou, S.; Isidor, F. Patient satisfaction and esthetic outcome after immediate placement and provisionalization of single-tooth implants involving a definitive individual abutment. Clin. Oral Implant. Res. 2014, 25, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Hämmerle, C.H.; Chen, S.T.; Wilson, T.G., Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int. J. Oral Maxillofac. Implant. 2004, 19, 26–28. [Google Scholar]
- Chou, H.Y.; Romanas, G.; Müftü, A.; Müftü, S. Peri-implant bone remodeling around an extraction socket: Predictions of bone maintenance by finite element method. Int. J. Oral Maxillofac. Implant. 2012, 27, 39–48. [Google Scholar]
- Bozkaya, D.; Muftu, S. Mechanics of the tapered interference fit in dental implants. J. Biomech. 2003, 36, 1649–1658. [Google Scholar] [CrossRef]
- Dibart, S.; Warbington, M.; Su, M.F.; Skobe, Z. In vitro evaluation of the implant-abutment bacterial seal: The locking taper system. Int. J. Oral Maxillofac. Implant. 2005, 20, 732–737. [Google Scholar]
- Aloise, J.P.; Curcio, R.; Laporta, M.Z.; Rossi, L.; da Silva, A.M.; Rapoport, A. Microbial leakage through the implant-abutment interface of Morse taper implants in vitro. Clin. Oral Implant. Res. 2010, 21, 328–335. [Google Scholar] [CrossRef]
- Seyssens, L.; De Lat, L.; Cosyn, J. Immediate implant placement with or without connective tissue graft: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 48, 284–301. [Google Scholar] [CrossRef]
- Urdaneta, R.A.; Marincola, M. The Integrated Abutment Crownt, a screwless and cementless restoration for single-tooth implants: A report on a new technique. J. Prosthodont. 2007, 16, 311–318. [Google Scholar] [CrossRef]
- De Rouck, T.; Eghbali, R.; Collys, K.; De Bruyn, H.; Cosyn, J. The gingival biotype revisited: Transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J. Clin. Periodontol. 2009, 36, 428–433. [Google Scholar] [CrossRef]
- Levine, R.A.; Ganeles, J.; Gonzaga, L.; Kan, J.K.; Randel, H.; Evans, C.D.; Chen, S.T. 10 Keys for Successful Esthetic-Zone Single Immediate Implants. Compend. Contin. Educ. Dent. 2017, 38, 248–260. [Google Scholar]
- Choquet, V.; Hermans, M.; Adriaenssens, P.; Daelemans, P.; Tarnow, D.P.; Malevez, C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J. Periodontol. 2001, 72, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Kois, J.C.; Kan, J.Y. Predictable peri-implant gingival aesthetics: Surgical and prosthodontic rationales. Pract. Proced. Aesthet. Dent. 2001, 13, 691–698. [Google Scholar] [PubMed]
- Chang, M.; Wennström, J.L.; Odman, P.; Andersson, B. Implant supported single-tooth replacements compared to contralateral natural teeth. Crown and soft tissue dimensions. Clin. Oral Implant. Res. 1999, 10, 185–194. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral Implant. Res. 2013, 24, 1179–1184. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Nocini, P.F. Assessment of Peri-Implant Soft Tissues Conditions around Short and Ultra-Short Implant-Supported Single Crowns: A 3-Year Retrospective Study on Periodontally Healthy Patients and Patients with a History of Periodontal Disease. Int. J. Environ. Res. Public. Health 2020, 17, 9354. [Google Scholar] [CrossRef] [PubMed]
- De Santis, D.; Sinigaglia, S.; Pancera, P.; Faccioni, P.; Portelli, M.; Luciano, U.; Cosola, S.; Penarrocha, D.; Bertossi, D.; Nocini, R.; et al. An overview of socket preservation. J. Biol. Regul. Homeost. Agents 2019, 33, 55–59. [Google Scholar]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Jung, R.E.; Becker, K.; Bienz, S.P.; Dahlin, C.; Donos, N.; Hammächer, C.; Iglhaut, G.; Liñares, A.; Ortiz-Vigón, A.; Sanchez, N.; et al. Effect of peri-implant mucosal thickness on esthetic outcomes and the efficacy of soft tissue augmentation procedures: Consensus report of group 2 of the SEPA/DGI/OF workshop. Clin. Oral Implant. Res. 2022, 33, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Tavelli, L.; Barootchi, S.; Avila-Ortiz, G.; Urban, I.A.; Giannobile, W.V.; Wang, H.L. Peri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis. J. Periodontol. 2021, 92, 21–44. [Google Scholar] [CrossRef]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J. Periodontol. 2018, 89, 237–248. [Google Scholar] [CrossRef]
- Barootchi, S.; Tavelli, L.; Zucchelli, G.; Giannobile, W.V.; Wang, H.L. Gingival phenotype modification therapies on natural teeth: A network meta-analysis. J. Periodontol. 2020, 91, 1386–1399. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Bissada, N.F. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018, 89, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Lozada, J.L.; Zimmerman, G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: A 2- to 8-year follow-up. Int. J. Oral Maxillofac. Implant. 2011, 26, 179–187. [Google Scholar]
- Mailoa, J.; Arnett, M.; Chan, H.L.; George, F.M.; Kaigler, D.; Wang, H.L. The Association Between Buccal Mucosa Thickness and Periimplant Bone Loss and Attachment Loss: A Cross-Sectional Study. Implant. Dent. 2018, 27, 575–581. [Google Scholar] [CrossRef]
- Chen, S.T.; Darby, I.B.; Reynolds, E.C.; Clement, J.G. Immediate implant placement postextraction without flap elevation. J. Periodontol. 2009, 80, 163–172. [Google Scholar] [CrossRef]
- van Nimwegen, W.G.; Raghoebar, G.M.; Zuiderveld, E.G.; Jung, R.E.; Meijer, H.J.A.; Mühlemann, S. Immediate placement and provisionalization of implants in the aesthetic zone with or without a connective tissue graft: A 1-year randomized controlled trial and volumetric study. Clin. Oral Implants Res. 2018, 29, 671–678. [Google Scholar] [CrossRef]
- Ferrantino, L.; Camurati, A.; Gambino, P.; Marzolo, M.; Trisciuoglio, D.; Santoro, G.; Farina, V.; Fontana, F.; Asa’ad, F.; Simion, M. Aesthetic outcomes of nonfunctional immediately restored single post-extraction implants with and without connective tissue graft: A multicenter randomized controlled trial. Clin. Oral Implant. Res. 2021, 32, 684–694. [Google Scholar] [CrossRef] [PubMed]
- Zuiderveld, E.G.; Meijer, H.J.A.; den Hartog, L.; Vissink, A.; Raghoebar, G.M. Effect of connective tissue grafting on periimplant tissue in single immediate implant sites: A RCT. J. Clin. Periodontol. 2018, 45, 253–264. [Google Scholar] [CrossRef]
- Chung, S.; Rungcharassaeng, K.; Kan, J.Y.; Roe, P.; Lozada, J.L. Immediate single tooth replacement with subepithelial connective tissue graft using platform switching implants: A case series. J. Oral Implantol. 2011, 37, 559–569. [Google Scholar] [CrossRef]
- Ballini, A.; Di Cosola, M.; Saini, R.; Benincasa, C.; Aiello, E.; Marrelli, B.; Rajiv Saini, S.; Ceruso, F.M.; Nocini, R.; Topi, S.; et al. A Comparison of Manual Nylon Bristle Toothbrushes versus Thermoplastic Elastomer Toothbrushes in Terms of Cleaning Efficacy and the Biological Potential Role on Gingival Health. Appl. Sci. 2021, 11, 7180. [Google Scholar] [CrossRef]

| n | % | C.I. | |
|---|---|---|---|
| Sex | |||
| male | 7 | 22 | 0.13–0.49 |
| female | 18 | 72 | 0.50–0.86 |
| Implant position | |||
| 11 | 6 | 24 | 0.10–0.45 |
| 12 | 7 | 28 | 0.13–0.49 |
| 13 | 1 | 4 | 0.01–0.26 |
| 21 | 5 | 20 | 0.08–0.41 |
| 22 | 6 | 24 | 0.10–0.45 |
| Connective tissue graft (CTG) | |||
| no | 15 | 60 | 0.38–0.77 |
| yes | 10 | 40 | 0.22–0.61 |
| Gingival phenotype | |||
| thin | 10 | 40 | 0.22–0.61 |
| thick | 15 | 60 | 0.38–0.77 |
| Gingival phenotype combined with CTG | |||
| thin | 6 | 24 | 0.10–0.45 |
| thick | 9 | 36 | 0.18–0.57 |
| thin + CTG | 4 | 16 | 0.05–0.37 |
| thick + CTG | 6 | 24 | 0.10–0.45 |
| Aetiology for tooth loss | |||
| agenesis | 1 | 4 | 0.01–0.26 |
| root fracture | 12 | 48 | 0.30–0.69 |
| caries | 6 | 24 | 0.10–0.45 |
| non-treatable endodontic lesions | 5 | 20 | 0.08–0.41 |
| root resorption | 1 | 4 | 0.01–0.26 |
| Mesial Papilla | Distal Papilla | Gingival Level | Gingival Contour | Alveolar Process | Color | Texture | Total PES | KT | GM | |
|---|---|---|---|---|---|---|---|---|---|---|
| T0 | 1.12 ± 0.72 | 1.08 ± 0.70 | 1.32 ± 0.74 | 1.32 ± 0.69 | 1.32 ± 0.55 | 1.6 ± 0.57 | 1.48 ± 0.58 | 9.24 ± 2.36 | 3.82 ± 0.92 | 11.08 ± 2.03 |
| T1 | 1.00 ± 0.64 | 0.88 ± 0.66 | 1.20 ± 0.64 | 1.52 ± 0.58 | 1.60 ± 0.50 | 1.72 ± 0.45 | 1.68 ± 0.47 | 9.60 ± 1.70 | 3.76 ± 1.26 | 11.48 ± 1.58 |
| p value | 0.41 | 0.06 | 0.44 | 0.25 | 0.06 | 0.41 | 0.13 | 0.39 | 0.8 | 0.06 |
| ΔMesial Papilla | ΔDistal Papilla | ΔGingival Level | ΔGingival Contour | ΔAlveolar Process | ΔColor | ΔTexture | ΔTotal PES | ΔKT | REC | |
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | (-)0.12 (0.72) | (-)0.20 (0.50) | (-)0.12 (0.78) | 0.2 (0.86) | 0.28 (0.73) | 0.12 (0.72) | 0.20 (0.64) | 0.36 (2.07) | (-)0.06 (1.17) | 0.40 (1.00) |
| thin | (-)0.33 (0.51) | (-)0.33 (0.51) | (-)0.33 (1.03) | 0.16 (0.98) | (-)0.16 (0.75) | (-)0.16 (0.75) | (-)0.16 (0.75) | (-)1.33 (2.16) | (-)0.50 (0.54) | 0.33 (1.36) |
| thick | 0.00 (0.86) | 0.00 (0.50) | 0.00 (0.70) | 0.33 (1.00) | 0.22 (0.66) | 0.22 (0.83) | 0.22 (0.66) | 1.00 (1.93) | 0.11 (1.53) | 0.33 (1.11) |
| thin + CTG | 0.25 (0.50) | (-)0.25 (0.50) | 0.00 (0.81) | 0.50 (0.57) | 0.75 (0.95) | 0.50 (0.57) | 0.50 (0.57) | 2.25 (1.70) | 0.62 (0.47) | 0.50 (1.00) |
| thick + CTG | (-)0.33 (0.81) | (-)0.33 (0.51) | (-)0.16 (0.75) | (-)0.16 (0.75) | 0.50 (0.54) | 0.00 (0.63) | 0.33 (0.51) | (-)0.16 (0.98) | 0.50 (1.22) | 0.50 (0.54) |
| p value | 0.43 | 0.53 | 0.92 | 0.61 | 0.28 | 0.45 | 0.43 | 0.04 * | 0.31 | 0.95 |
| Mesial Papilla | Distal Papilla | Gingival Level | Gingival Contour | Alveolar Process | Color | Texture | Total PES | KT | GM | |
|---|---|---|---|---|---|---|---|---|---|---|
| thin | 1.66 ± 0.51 | 1.66 ± 0.51 | 1.50 ± 0.54 | 1.33 ± 0.81 | 1.66 ± 0.51 | 1.66 ± 0.51 | 1.83 ± 0.40 | 11.33 ± 2.33 | 4.00 ± 0.89 | 11.33 ± 1.96 |
| thick | 1.00 ± 0.70 | 0.77 ± 0.83 | 0.88 ± 0.92 | 1.22 ± 0.83 | 1.22 ± 0.44 | 1.66 ± 0.70 | 1.66 ± 0.50 | 8.44 ± 2.40 | 3.77 ± 0.66 | 10.88 ± 2.02 |
| thin + CTG | 0.75 ± 0.95 | 1.25 ± 0.50 | 1.50 ± 0.57 | 1.25 ± 0.50 | 1.00 ± 0.81 | 1.00 ± 0.01 | 0.75 ± 0.50 | 7.50 ± 1.91 | 4.00 ± 0.01 | 11.75 ± 2.06 |
| thick + CTG | 1.00 ± 0.63 | 0.83 ± 0.40 | 1.66 ± 0.51 | 1.50 ± 0.54 | 1.33 ± 0.51 | 1.83 ± 0.40 | 1.33 ± 0.51 | 9.50 ± 1.04 | 3.16 ± 1.16 | 10.66 ± 2.50 |
| p value | 0.18 | 0.06 | 0.18 | 0.9 | 0.27 | 0.13 | 0.01 * | 0.03 * | 0.08 | 0.85 |
| Mesial Papilla | Distal Papilla | Gingival Level | Gingival Contour | Alveolar Process | Color | Texture | Total PES | KT | GM | |
|---|---|---|---|---|---|---|---|---|---|---|
| thin | 1.33 ± 0.81 | 1.33 ± 0.51 | 1.16 ± 0.75 | 1.50 ± 0.54 | 1.50 ± 0.54 | 1.50 ± 0.54 | 1.66 ± 0.51 | 10.00 ± 0.89 | 3.50 ± 0.83 | 11.66 ± 0.81 |
| thick | 1.00 ± 0.50 | 0.77 ± 0.66 | 0.88 ± 0.60 | 1.55 ± 0.72 | 1.44 ± 0.52 | 1.88 ± 0.33 | 1.88 ± 0.33 | 9.44 ± 2.12 | 3.88 ± 1.61 | 11.22 ± 1.48 |
| thin + CTG | 1.00 ± 0.81 | 1.00 ± 0.81 | 1.50 ± 0.57 | 1.75 ± 0.50 | 1.75 ± 0.50 | 1.50 ± 0.57 | 1.25 ± 0.50 | 9.75 ± 2.87 | 4.62 ± 0.47 | 12.25 ± 1.25 |
| thick + CTG | 0.66 ± 0.51 | 0.50 ± 0.54 | 1.50 ± 0.54 | 1.33 ± 0.51 | 1.83 ± 0.40 | 1.83 ± 0.40 | 1.66 ± 0.51 | 9.33 ± 0.81 | 3.66 ± 1.63 | 11.16 ± 2.48 |
| p value | 0.38 | 0.16 | 0.24 | 0.76 | 0.45 | 0.28 | 0.17 | 0.91 | 0.92 | 0.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lombardo, G.; Signoriello, A.; Zangani, A.; Pardo, A.; Marincola, M.; Messina, E.; Gualtieri, M.; Corrocher, G.; Albanese, M.; Faccioni, P. Immediately Placed Single Locking-Taper Implants in the Aesthetic Area of Upper Maxilla: A Short-Term Pilot Study. Prosthesis 2025, 7, 60. https://doi.org/10.3390/prosthesis7030060
Lombardo G, Signoriello A, Zangani A, Pardo A, Marincola M, Messina E, Gualtieri M, Corrocher G, Albanese M, Faccioni P. Immediately Placed Single Locking-Taper Implants in the Aesthetic Area of Upper Maxilla: A Short-Term Pilot Study. Prosthesis. 2025; 7(3):60. https://doi.org/10.3390/prosthesis7030060
Chicago/Turabian StyleLombardo, Giorgio, Annarita Signoriello, Alessandro Zangani, Alessia Pardo, Mauro Marincola, Elena Messina, Miriana Gualtieri, Giovanni Corrocher, Massimo Albanese, and Paolo Faccioni. 2025. "Immediately Placed Single Locking-Taper Implants in the Aesthetic Area of Upper Maxilla: A Short-Term Pilot Study" Prosthesis 7, no. 3: 60. https://doi.org/10.3390/prosthesis7030060
APA StyleLombardo, G., Signoriello, A., Zangani, A., Pardo, A., Marincola, M., Messina, E., Gualtieri, M., Corrocher, G., Albanese, M., & Faccioni, P. (2025). Immediately Placed Single Locking-Taper Implants in the Aesthetic Area of Upper Maxilla: A Short-Term Pilot Study. Prosthesis, 7(3), 60. https://doi.org/10.3390/prosthesis7030060







