Abstract
Introduction: Obstructive sleep apnea syndrome (OSAS) is characterized by intermittent hypoxia, sleep fragmentation, daytime sleepiness, cognitive impairment, and brain cell damage due to brain blood flow reduction, with ischemic damage, increased microvascular reactivity, and brain tissue damage. OSAS is strongly linked to chronic, neurodegenerative, and inflammatory cerebrovascular disease and cognitive impairment. Continuous positive airway pressure (CPAP) is the first-line treatment for OSAS. Objective: This article aims to evaluate the effect of CPAP treatment on neurocognitive performance in OSAS patients with mild cognitive impairment or dementia by reviewing the literature. Methods: We performed a comprehensive review of the Portuguese and English languages without a time limit using the following Mesh terms: dementia, mild cognitive impairment, obstructive sleep apnea, and CPAP. We included randomized controlled trials (RCTs), meta-analyses, and systematic reviews (SRs) where the impact of CPAP on neurocognitive performance was addressed. Results: Five SRs and three RCTs reported significant improvements in neurocognitive performance, especially in verbal, visuospatial, and working memory. Conclusion: CPAP treatment seems to improve cognitive defects associated with OSA.
1. Introduction
Obstructive sleep apnea syndrome (OSAS) is the most common primary sleep disorder in older adults [1], and it is characterized by repetitive episodes of complete or partial collapse of the upper airways during sleep, causing obstruction, chronic intermittent hypoxia, sleep fragmentation, and daytime sleepiness [2].
OSAS is a risk factor not only in several diseases, both in young and older adults, such as hypertension, diabetes, metabolic syndrome, and stroke, but also in cognitive disorders [3], including dementia and Alzheimer’s Disease (AD), which has been linked to neuroinflammation [4], intermittent hypoxemia, reduced sleep quality and continuity, and hypercapnia disruption of the hypothalamic–pituitary–adrenal axis mechanisms [5]. Chronic sleep deprivation might also be associated with increased toxic products that induce neurodegeneration. Asthma is another common respiratory disorder that may complicate the clinical course of OSAS, as the pathology and its treatment may increase the collapsibility of the upper airways, contributing to the development and worsening of OSAS. On the other hand, OSAS modifies asthmatic airway inflammation, worsening asthma symptoms and the frequency of exacerbations [6]. The coexistence of both disorders is common as they are highly prevalent and share genetic background and risk factors, such as allergic rhinitis, gastroesophageal reflux disease, and obesity [6].
Due to brain blood flow reduction, which results in ischemic damage, increased microvascular reactivity, and brain tissue damage, OSAS is strongly linked with chronic cerebrovascular, neurodegenerative, and inflammatory disease and cognitive impairment, affecting attention, executive functioning, motor efficiency, working memory, and long-term episodic memory [5].
Continuous positive airway pressure (CPAP), the gold-standard treatment for OSAS, can improve both OSAS and asthma control in patients suffering from both diseases by preventing episodes of upper airway collapse and maintaining a continuous airflow [7,8].
Furthermore, evidence suggests CPAP might have a positive influence on cognitive performance both in young and cognitively impaired patients and improve daily function providing greater independence, quality of life, lower caregiver burden, and need for medical assistance or social support [9]. This association would have a broad impact regarding these patients’ quality of life.
With this comprehensive review, we aim to evaluate the existing evidence of CPAP’s impact on cognitive function improvement and the prevention of cognitive impairment in OSAS patients with mild cognitive impairment or dementia.
2. Materials and Methods
The present systematic literature review protocol was guided according to the methodological guidelines proposed by the Joanne Briggs Institute (JBI) [10] and registered at PROSPERO with the ID CRD42024622192. We considered the PI(C)O (Population, Intervention, Comparison, and Outcome) framework to formulate the research question [11]: Population—OSAS patients, only adults, diagnosed with mild cognitive impairment or dementia; Intervention—CPAP; Comparison—placebo or CPAP with a low-adherence therapeutic regimen; Outcome—improved neurocognitive performance. In this sense, this review aims to answer the research question: what are the benefits of treating OSAS (I) patients (P) in their cognition (O)?
The literature search was carried out on the electronic PUBMED, Cochrane Library, and NICE evidence databases in July 2024 without a time limit. We used the Medical Subject Heading (MeSH) terms “dementia”, “mild cognitive impairment”, “obstructive sleep apnea”, and “CPAP” and the booleans “AND” and “OR”. The inclusion and exclusion criteria adopted are presented in Table 1.

Table 1.
Inclusion and exclusion criteria.
Articles published in Portuguese and English were considered, with no time limit.
All identified citations were uploaded into Zotero 6.0.37 for MacOS, and duplicates were removed. Afterward, titles and abstracts were screened by two independent reviewers for assessment against the inclusion criteria for the review.
The full text of the selected studies was assessed in detail by two independent reviewers, including the quality, quantity, and consistency of evidence using the SORT (Strength of Recommendation Taxonomy) scale [12].
The results of the inclusion process are presented as a PRISMA flow diagram [13] in Figure 1.
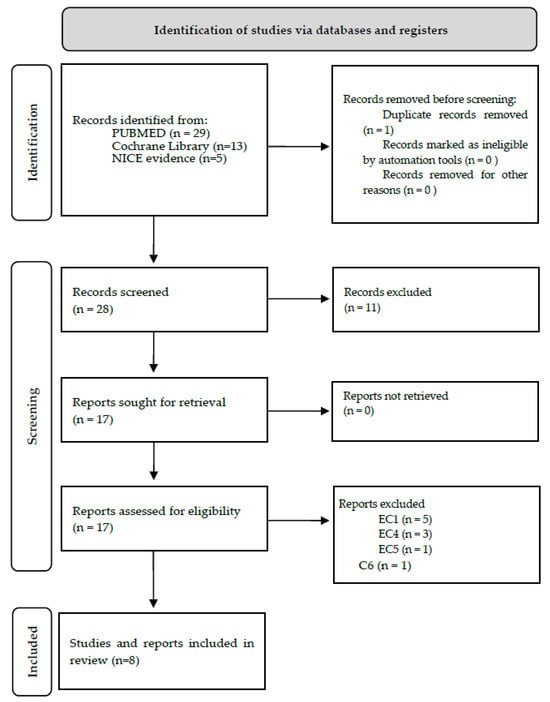
Figure 1.
Preferred reporting items for systematic reviews and meta-analysis diagrams.
The articles included in the present review were summarized and presented in a table prepared by the authors.
3. Results
Of the eight selected articles, five were reviews, two were clinical trials, and one was a secondary analysis of a clinical trial. All the articles are from Europe and the United States of America. Table 2 summarizes the data collected from each article, including objectives, participants, evidence level, and key findings regarding our research.

Table 2.
Presentation of the studies included in the review.
Table 3 summarizes the design and evidence of each clinical trial included in the present review. In every trial, the intervention group showed improved results when compared to the control group.

Table 3.
Randomized control trials included in the review.
4. Discussion
Using the VOSviewr version 1.6.20 software for MacOS, we analyzed biometric networks between all included studies. Figure 2 presents the network visual map obtained by VOSviewr.
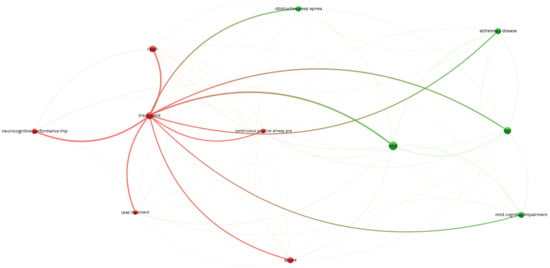
Figure 2.
Visual map of included studies cluster analysis.
The cluster analysis focusing on the “treatment” concept connects it to OSAS, CPAP, MCI, AD, and neurocognitive performance impairment.
The gold standard for treating OSAS is CPAP [7,8,14,15,16,17,18,19,20], which is consistent in the studies included in this review and in the evidence from the literature. CPAP is proven to prolong N3 sleep and increase the power and amplitude of slow electroencephalographic waves during N3 sleep, indicating improved sleep quality [21]. Additionally, CPAP can improve sleep-related symptoms, the apnea–hypopnea index, and quality of life [7,8], although poor adherence can compromise its results [22]. People with allergic rhinitis, moderate to severe nasal congestion at bedtime, rhinorrhoea, sinus opacification, and high nasal septum deviation have higher rates of CPAP initial adherence problems, leading to treatment discontinuation unless adequately treated before CPAP initiation [23,24]. A systematic review regarding CPAP adherence suggests home calls, phone calls, CPAP therapist support, patient education, motivational interviews, and follow-up visits as CPAP adherence interventions [22]. Also, nurses can play an important role in managing respiratory diseases and treatment compliance [25]. In some countries, adherence is continuously monitored with devices attached to the CPAP system, and its non-use can lead to the removal of the device from the national health system or the insurance company.
It is well established that OSAS is strongly associated with cerebrovascular and neurodegenerative diseases, which may aggravate cognitive dysfunction such as dementia, AD, psychomotor speed, memory, attention, and daytime sleepiness [14,16,17,20,22]. Evidence from analyzed studies in this review supports that treating OSAS seems to have a positive impact on MCI [14,15,16,17,18,19,20], improving cognition, protecting against MCI, and slowing its progression. In this sense, some of the MCI improvements mentioned were (i) memory (including long-term verbal memory and short-term visuospatial memory) [4,14,16,18,19,20], (ii) attention [15,16,18,19,20], (iii) daytime sleepiness [15,16,17,18,20], and (iv) language [16,19]. Corroborating this evidence, a clinical trial conducted by Hong et al. (2000) revealed that OSAS patients treated with CPAP for two months showed significant improvements in daytime sleepiness, logical memory, and face memory compared to those patients without CPAP treatment [21]. A study from Malik and Patrik (2001) also concluded that good CPAP adherence improves cognitive memory and attention [26]. Many patients with OSAS experience excessive daytime sleepiness, which can improve with CPAP treatment [27], although a substantial proportion of patients may continue to experience this symptom despite receiving optimized primary OSA therapy [28]. OSAS may affect language abilities, especially those that involve efficient retrieval of lexical–semantic representations [29], but the evidence is not clear about this.
On the other hand, we could also find studies that did not find MCI improvements over OSAS treatment [30], suggesting the correlation is not linear and that more studies should be conducted. In a systematic review, Bubu et al. (2020) suggest that decreased neural plasticity and neural loss and atrophy seen in AD patients may explain the lack of significant results on some cognitive dysfunction improvements with CPAP therapy [16]. In return, the same author stated that in young and middle-aged OSAS patients, CPAP treatment played a significant role in cognitive function improvement, suggesting potential benefits on brain tissue damage prevention and AD, as significant improvements in memory, attention, and executive function paralleled white matter changes after 12-month treatment, found in middle-aged patients.
According to the studies analyzed, treating OSAS also seems to have a positive impact on neurocognitive performance in areas such as (i) executive function [4,14,15,16,17,18,19,20], (ii) psychomotor speed [14,15,16,18], (iii) cognitive process speed [4,14,15,16,18], and (iv) reaction time [16,19,20]. A study by Malik and Patrick (2021) found significant executive performance differences between patients with OSAS, improved by correct compliance with CPAP treatment [26]. Evidence is divided concerning psychomotor speed and reaction time improvement with OSAS treatment. OSAS patients reveal impaired results in minimum single-task solving time in the speed of solving simple arithmetic operations [31], where CPAP treatment appears to mitigate and slow the rate of cognitive decline and may improve information processing speed [9]. On the other hand, a study conducted by Vanek et al. (2020) stated that, in contrast to other cognitive areas, psychomotor speed and fine coordination do not significantly improve after CPAP treatment [32]. However, all authors agree that treating OSAS is necessary to prevent neurocognitive and psychomotor performance declination.
Education, prevention, and early diagnosis are the most effective ways to mitigate the impact of OSAS both on patients and the health system, whereas CPAP adherence can be treated as a secondary prevention measure that aims to reduce the overall impact of OSAS [33]. Furthermore, OSAS prevention includes physical activity, obesity treatment, reducing the frequency of supine sleep, reducing alcohol consumption, treating dental and maxillofacial pathology, and reducing the use of sedatives such as opioids and benzodiazepines [33]. All these aspects should be addressed in treating OSAS in order to achieve better results in cognition, not forgetting to treat comorbidities and MCI accordingly.
Our search resulted in only two primary studies, suggesting that the impact of treating OSAS on cognition has not yet been thoroughly explored. Also, most reviews on the subject rely on the same limited clinical trials. In that sense, we cannot assure a high evidence level for the results, and we recommend more primary studies concerning the effect of OSAS treatment on cognition.
5. Conclusions
The literature shows that CPAP treatment in OSAS is associated with significant benefits in neurocognitive performance, such as executive function and cognitive process speed, as well as neural recovery, in the long term. It can also be an important tool in preventing cognitive impairment in OSAS patients, as it can improve memory and attention and reduce daytime sleepiness. Treatment compliance is essential, and certain issues must be addressed, such as allergies, nasal problems, and other comorbidities.
Author Contributions
Conceptualization, J.M.N. and C.A.M.; methodology, J.M.N., C.A.M. and P.A.-S.; software, J.M.N., C.A.M. and P.A.-S.; validation, J.M.N., C.A.M. and P.A.-S.; formal analysis, J.M.N., C.A.M. and P.A.-S.; investigation, J.M.N., C.A.M. and P.A.-S.; resources, J.M.N., C.A.M. and P.A.-S.; data curation, J.M.N., C.A.M. and P.A.-S.; writing—original draft preparation, J.M.N., C.A.M. and P.A.-S.; writing—review and editing, J.M.N., C.A.M. and P.A.-S.; visualization, J.M.N., C.A.M. and P.A.-S.; supervision, P.A.-S.; project administration, J.M.N. and C.A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jaqua, E.E.; Hanna, M.; Labib, W.; Moore, C.; Matossian, V. Common Sleep Disorders Affecting Older Adults. Perm. J. 2023, 27, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Korson, R.; Guilleminault, C. Obstructive Sleep Apnea Syndrome. In Sleep Disorders Medicine; Chokroverty, S., Ed.; Springer: New York, NY, USA, 2017; pp. 567–596. ISBN 978-1-4939-6576-2. [Google Scholar]
- Osman, A.M.; Carter, S.G.; Carberry, J.C.; Eckert, D.J. Obstructive Sleep Apnea: Current Perspectives. Nat. Sci. Sleep 2018, 10, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Cordone, S.; Scarpelli, S.; Alfonsi, V.; De Gennaro, L.; Gorgoni, M. Sleep-Based Interventions in Alzheimer’s Disease: Promising Approaches from Prevention to Treatment along the Disease Trajectory. Pharmaceuticals 2021, 14, 383. [Google Scholar] [CrossRef] [PubMed]
- Devita, M.; Montemurro, S.; Zangrossi, A.; Ramponi, S.; Marvisi, M.; Villani, D.; Raimondi, M.C.; Merlo, P.; Rusconi, M.L.; Mondini, S. Cognitive and Motor Reaction Times in Obstructive Sleep Apnea Syndrome: A Study Based on Computerized Measures. Brain Cogn. 2017, 117, 26–32. [Google Scholar] [CrossRef]
- Khatri, S.B.; Ioachimescu, O.C. The Intersection of Obstructive Lung Disease and Sleep Apnea. Cleve. Clin. J. Med. 2016, 83, 127–140. [Google Scholar] [CrossRef]
- Pavwoski, P.; Shelgikar, A.V. Treatment Options for Obstructive Sleep Apnea. Neur. Clin. Pract. 2017, 7, 77–85. [Google Scholar] [CrossRef]
- Aboussouan, L.S.; Bhat, A.; Coy, T.; Kominsky, A. Treatments for Obstructive Sleep Apnea: CPAP and Beyond. Cleve. Clin. J. Med. 2023, 90, 755–765. [Google Scholar] [CrossRef]
- Seda, G.; Matwiyoff, G.; Parrish, J.S. Effects of Obstructive Sleep Apnea and CPAP on Cognitive Function. Curr. Neurol. Neurosci. Rep. 2021, 21, 32. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. (Eds.) JBI Manual for Evidence Synthesis; JBI. 2020. Available online: https://synthesismanual.jbi.global (accessed on 6 January 2025).
- Vilelas, J. Investigação—O Processo de Construção Do Conhecimento, 3rd ed.; Edições Sílabo: Lisboa, Portugal, 2022; ISBN 978-989-561-097-6. [Google Scholar]
- Ebell, M.H.; Siwek, J.; Weiss, B.D.; Woolf, S.H.; Susman, J.; Ewigman, B.; Bowman, M. Strength of Recommendation Taxonomy (SORT): A Patient-Centered Approach to Grading Evidence in the Medical Literature. J. Am. Board Fam. Med. 2004, 17, 59–67. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Palmer, B.W.; Cooke, J.R.; Corey-Bloom, J.; Fiorentino, L.; Natarajan, L.; Liu, L.; Ayalon, L.; He, F.; Loredo, J.S. Cognitive Effects of Treating Obstructive Sleep Apnea in Alzheimer’s Disease: A Randomized Controlled Study. J. Am. Geriatr. Soc. 2008, 56, 2076–2081. [Google Scholar] [CrossRef] [PubMed]
- Richards, K.C.; Gooneratne, N.; Dicicco, B.; Hanlon, A.; Moelter, S.; Onen, F.; Wang, Y.; Sawyer, A.; Weaver, T.; Lozano, A.; et al. CPAP Adherence May Slow 1-Year Cognitive Decline in Older Adults with Mild Cognitive Impairment and Apnea. J. Am. Geriatr. Soc. 2019, 67, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Bubu, O.M.; Andrade, A.G.; Umasabor-Bubu, O.Q.; Hogan, M.M.; Turner, A.D.; De Leon, M.J.; Ogedegbe, G.; Ayappa, I.; Jean-Louis, G.G.; Jackson, M.L.; et al. Obstructive Sleep Apnea, Cognition and Alzheimer’s Disease: A Systematic Review Integrating Three Decades of Multidisciplinary Research. Sleep Med. Rev. 2020, 50, 101250. [Google Scholar] [CrossRef]
- Siachpazidou, D.I.; Stavrou, V.T.; Astara, K.; Pastaka, C.; Gogou, E.; Hatzoglou, C.; Economou, N.-T.; Gourgoulianis, K.I. Alzheimer’s Disease in Patients with Obstructive Sleep Apnea Syndrome. Tanaffos 2020, 19, 176. [Google Scholar] [PubMed]
- Wang, Y.; Cheng, C.; Moelter, S.; Fuentecilla, J.L.; Kincheloe, K.; Lozano, A.J.; Carter, P.; Gooneratne, N.; Richards, K.C. One Year of Continuous Positive Airway Pressure Adherence Improves Cognition in Older Adults with Mild Apnea and Mild Cognitive Impairment. Nurs. Res. 2020, 69, 157–164. [Google Scholar] [CrossRef]
- Fernandes, M.; Placidi, F.; Mercuri, N.B.; Liguori, C. The Importance of Diagnosing and the Clinical Potential of Treating Obstructive Sleep Apnea to Delay Mild Cognitive Impairment and Alzheimer’s Disease: A Special Focus on Cognitive Performance. J. Alzheimers Dis. Rep. 2021, 5, 515–533. [Google Scholar] [CrossRef]
- Pollicina, I.; Maniaci, A.; Lechien, J.R.; Iannella, G.; Vicini, C.; Cammaroto, G.; Cannavicci, A.; Magliulo, G.; Pace, A.; Cocuzza, S.; et al. Neurocognitive Performance Improvement after Obstructive Sleep Apnea Treatment: State of the Art. Behav. Sci. 2021, 11, 180. [Google Scholar] [CrossRef]
- Li, Y.; Li, Q.; Zou, X.; Zhong, Z.; Ouyang, Q.; Zeng, Q.; Hu, Y.; Wang, M.; Luo, Y.; Yao, D. Effects of CPAP Treatment on Electroencephalographic Activity in Patients with Obstructive Sleep Apnea Syndrome during Deep Sleep: Preliminary Findings of a Cross-Sectional Study. Chron. Respir. Dis. 2023, 20, 14799731231215094. [Google Scholar] [CrossRef]
- Oliver, C.; Li, H.; Biswas, B.; Woodstoke, D.; Blackman, J.; Butters, A.; Drew, C.; Gabb, V.; Harding, S.; Hoyos, C.M.; et al. A Systematic Review on Adherence to Continuous Positive Airway Pressure (CPAP) Treatment for Obstructive Sleep Apnoea (OSA) in Individuals with Mild Cognitive Impairment and Alzheimer’s Disease Dementia. Sleep Med. Rev. 2024, 73, 101869. [Google Scholar] [CrossRef]
- Inoue, A.; Chiba, S.; Matsuura, K.; Osafune, H.; Capasso, R.; Wada, K. Nasal Function and CPAP Compliance. Auris Nasus Larynx 2019, 46, 548–558. [Google Scholar] [CrossRef]
- Chaidas, K.; Lamprou, K.; Munnings, A.; Stradling, J.R.; Nickol, A.H. Nasal Symptoms in Patients with Obstructive Sleep Apnoea and Their Association with Continuous Positive Airway Pressure Usage. Life 2022, 12, 305. [Google Scholar] [CrossRef] [PubMed]
- Alexandre-Sousa, P.; Sousa, N.; Bento, J.; Azevedo, F.; Assis, M.; Mendes, J. Nurses’ Role in the Control and Treatment of Asthma in Adults: A Systematic Literature Review. Adv. Respir. Med. 2024, 92, 175–189. [Google Scholar] [CrossRef] [PubMed]
- Malik, H.; Patrick, R. Examining the Relationship Between CPAP Adherence and Attention/Executive Functioning Among OSA-Diagnosed Older Adults. Am. J. Geriatr. Psychiatry 2021, 29, S81. [Google Scholar] [CrossRef]
- Venkatnarayan, K.; Devaraj, U.; Veluthat, C.; Louis, V.; Ramachandran, P.; D’Souza, G.; Krishnaswamy, U.M. The Effect of CPAP Therapy on Excessive Daytime Sleepiness and Quality of Life in Subjects with Obstructive Sleep Apnoea: An AB Design Study. Sleep Breath 2021, 25, 1351–1357. [Google Scholar] [CrossRef] [PubMed]
- Lal, C.; Weaver, T.E.; Bae, C.J.; Strohl, K.P. Excessive Daytime Sleepiness in Obstructive Sleep Apnea. Mechanisms and Clinical Management. Ann. ATS 2021, 18, 757–768. [Google Scholar] [CrossRef]
- Makanikas, K.; Andreou, G.; Simos, P.; Chartomatsidou, E. Effects of Obstructive Sleep Apnea Syndrome and Medical Comorbidities on Language Abilities. Front. Neurol. 2021, 12, 721334. [Google Scholar] [CrossRef]
- Luz, G.P.; Badke, L.; Nery, L.E.; Silva, L.O.; Guimarães, T.M.; Coelho, G.; Millani, A.; Alves, R.G.; Kase, C.; Tufik, S.; et al. Effect of CPAP vs. Mandibular Advancement Device for Excessive Daytime Sleepiness, Fatigue, Mood, Sustained Attention, and Quality of Life in Patients with Mild OSA. Sleep Breath 2023, 27, 991–1003. [Google Scholar] [CrossRef]
- Lusic Kalcina, L.; Pavlinac Dodig, I.; Pecotic, R.; Valic, M.; Dogas, Z. Psychomotor Performance in Patients with Obstructive Sleep Apnea Syndrome. Nat. Sci. Sleep 2020, 12, 183–195. [Google Scholar] [CrossRef]
- Vanek, J.; Prasko, J.; Genzor, S.; Ociskova, M.; Kantor, K.; Holubova, M.; Slepecky, M.; Nesnidal, V.; Kolek, A.; Sova, M. Obstructive Sleep Apnea, Depression and Cognitive Impairment. Sleep Med. 2020, 72, 50–58. [Google Scholar] [CrossRef]
- Correa, E.; Conti, D.; Gozal, D.; O’Connor-Reina, C. Preventive medicine in obstructive sleep apnea—A systematic review and a call to action. Sleep 2024, 47, zasae164. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).