What Drives the Contemporary Black–White Racial Disparities in Gout in the US? Impact of Social Determinants of Health
Abstract
1. Introduction
2. Are Black Americans at Higher Risk of Gout Than White Americans?
3. What Are the Contemporary National Level Black–White Disparity Figures?
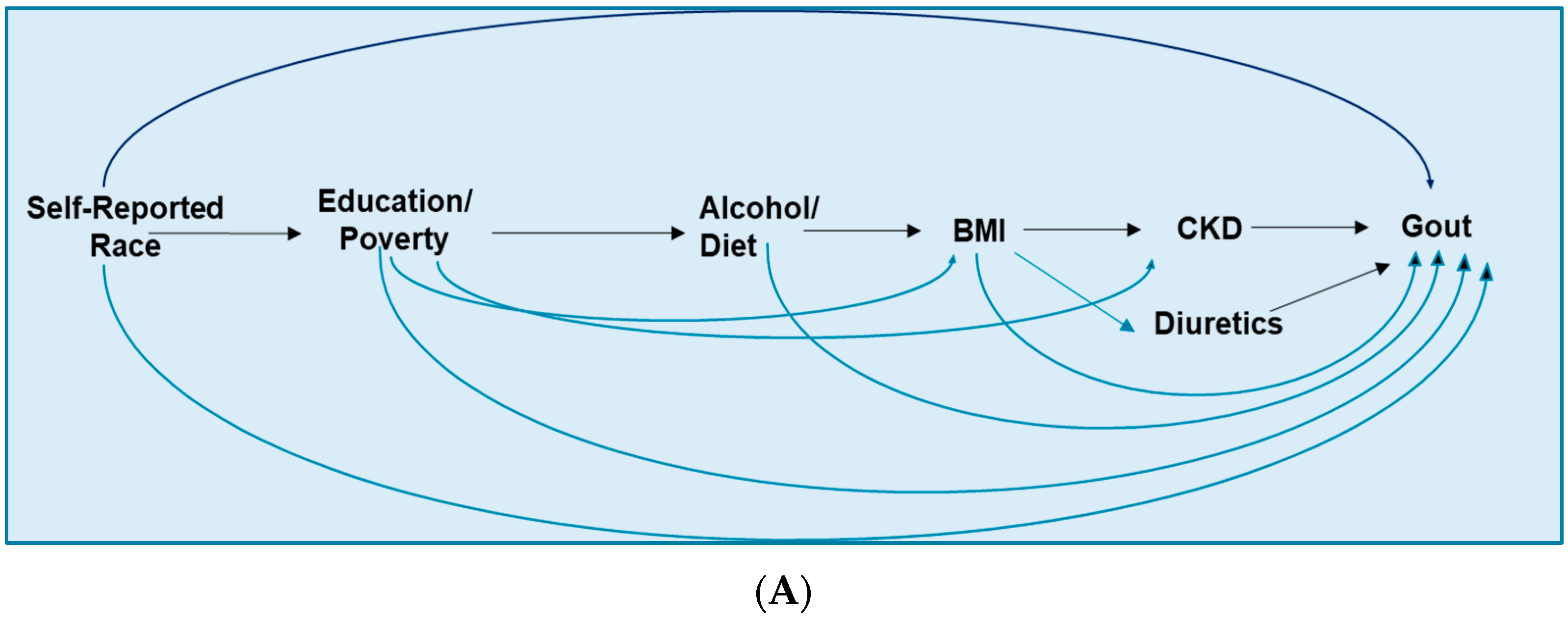
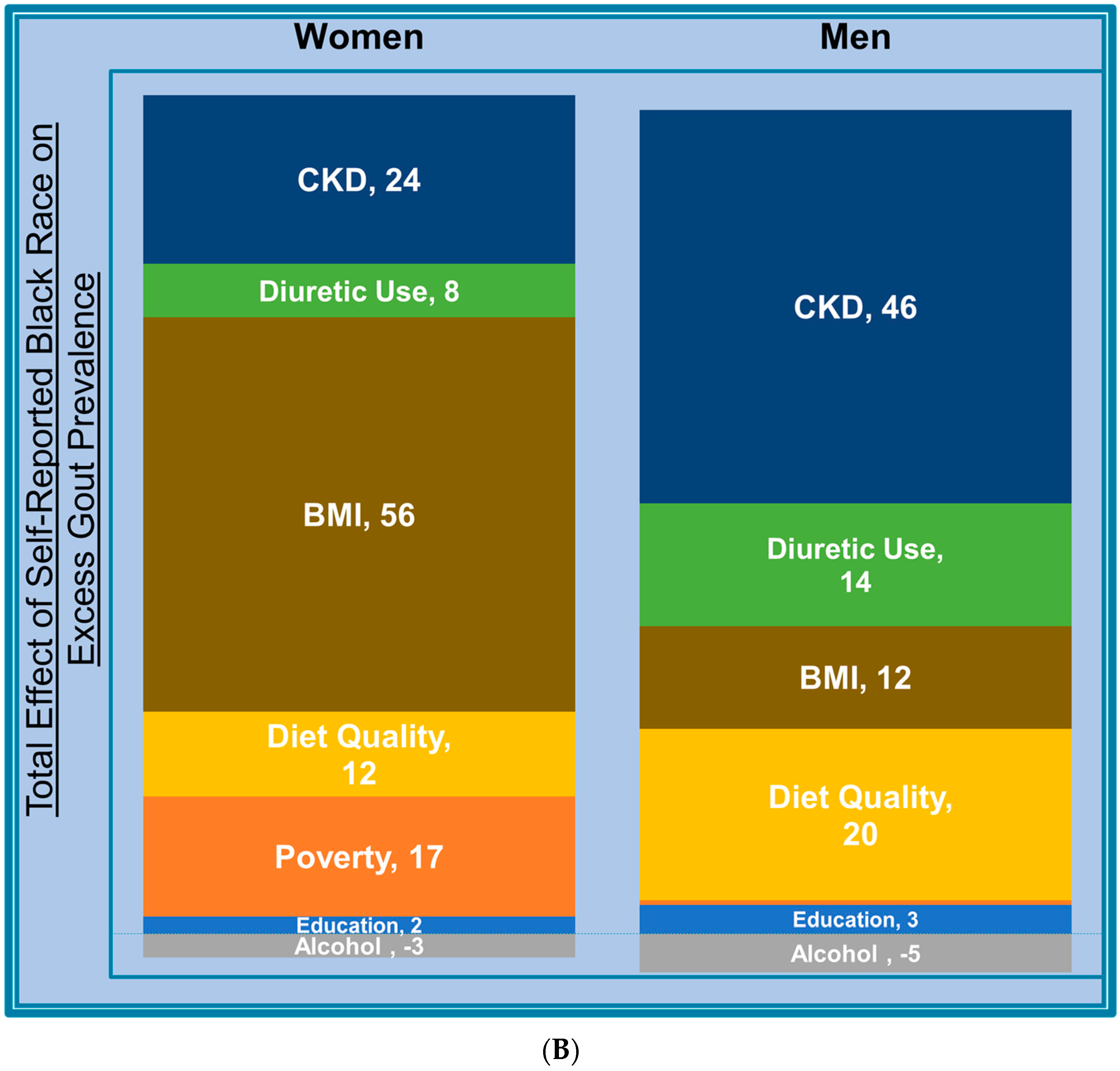
4. What Drives the Contemporary Black–White Racial Disparities in the US?
4.1. Socioeconomic Status
4.2. Diet Quality and Alcohol
4.3. Adiposity
4.4. Diuretic Medications
4.5. Chronic Kidney Disease
5. Are there Black–White Disparities in Gout Care and Outcomes in the US?
5.1. Gout Care Disparity
5.2. Gout Outcomes Disparity
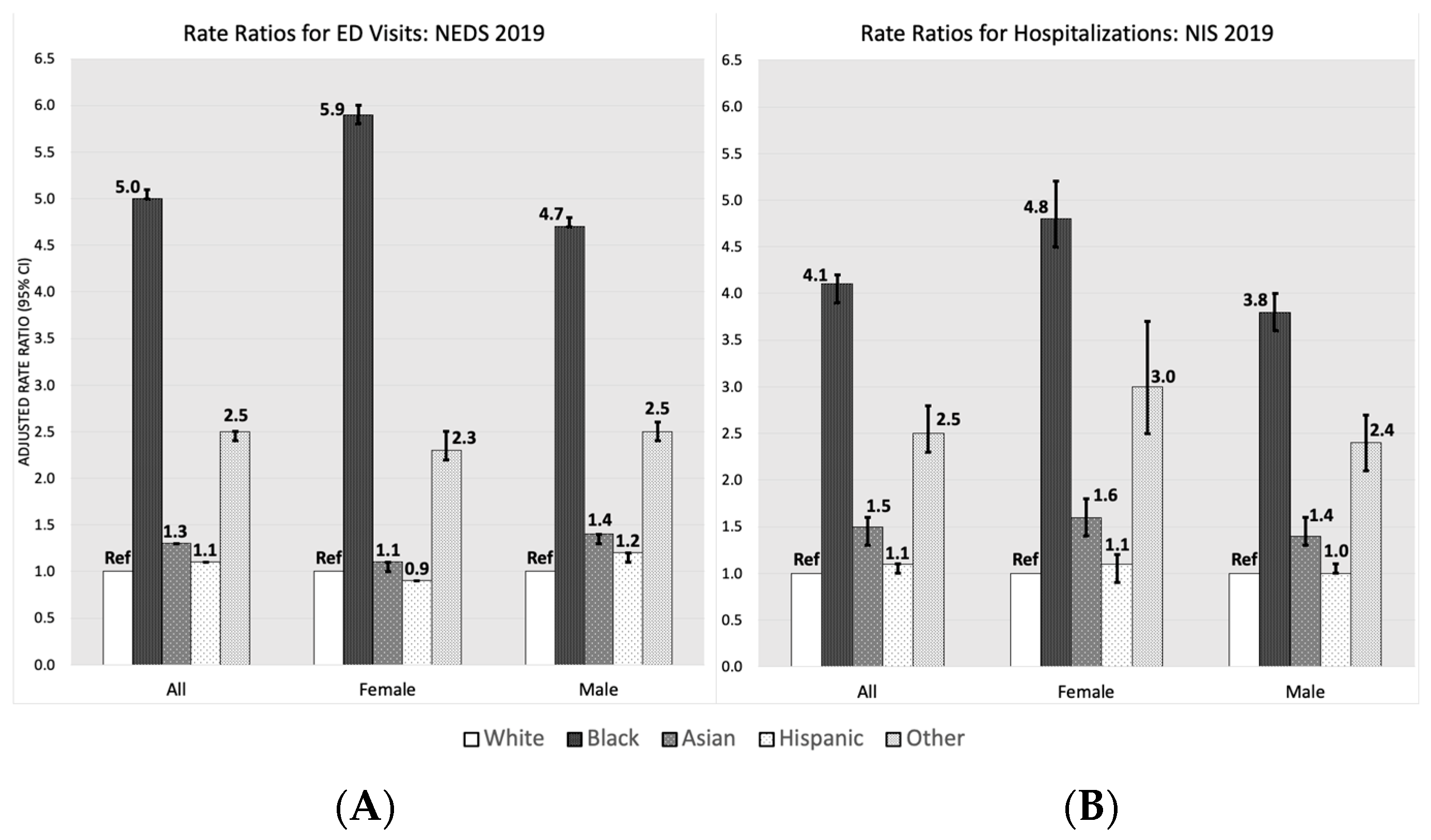
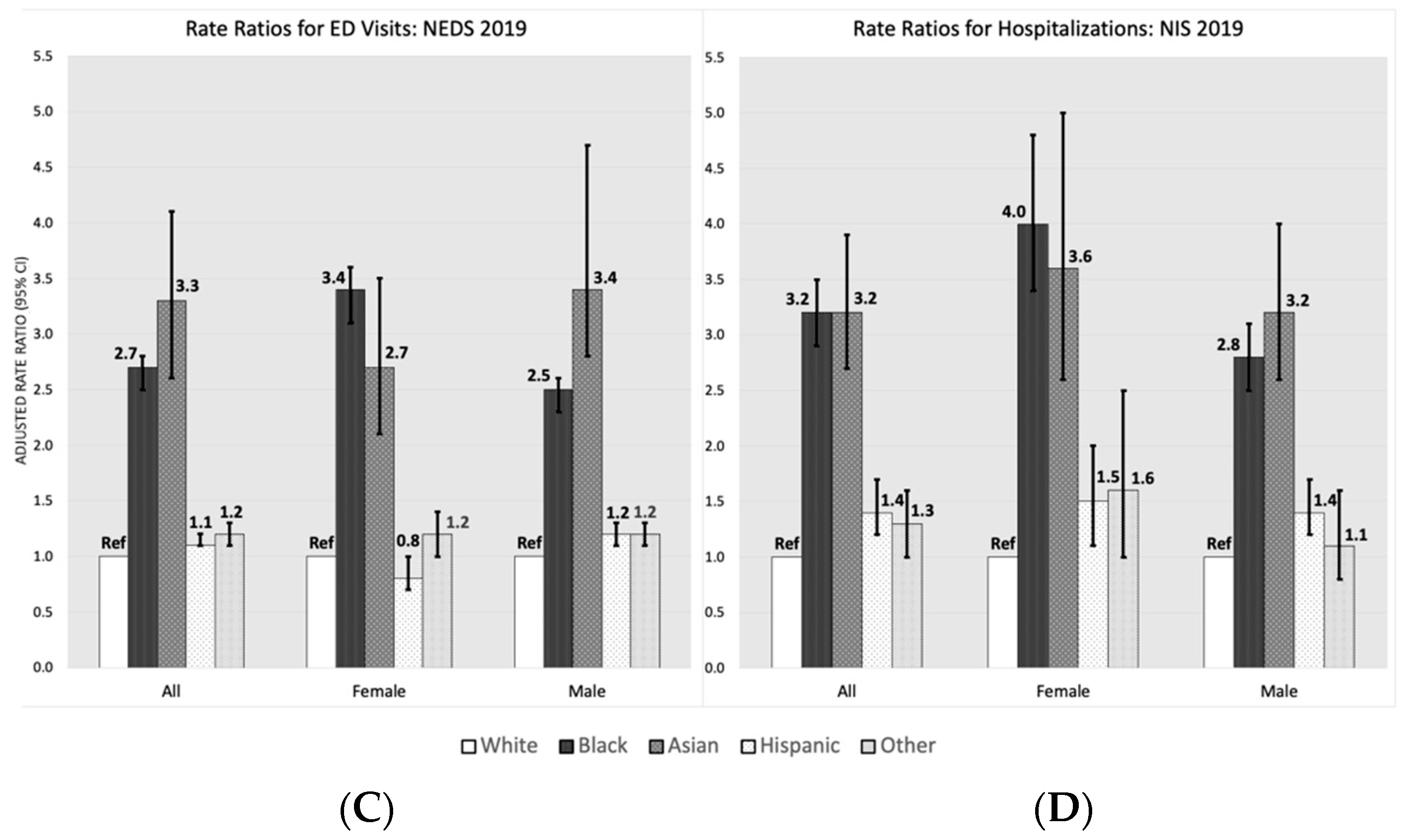
5.3. More Frequent Gout-Primary ED Visits and Hospitalisation among the US Black Population
5.4. Role of Inherent Systematic Health Care Disparities
6. What Research Is Needed to Reduce Black–White Disparities?
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Choi, H.K.; McCormick, N.; Yokose, C. Excess comorbidities in gout: The causal paradigm and pleiotropic approaches to care. Nat. Rev. Rheumatol. 2022, 18, 97–111. [Google Scholar] [CrossRef]
- Fisher, M.C.; Rai, S.K.; Lu, N.; Zhang, Y.; Choi, H.K. The unclosing premature mortality gap in gout: A general population-based study. Ann. Rheum. Dis. 2017, 76, 1289–1294. [Google Scholar] [CrossRef]
- Major, T.J.; Dalbeth, N.; Stahl, E.A.; Merriman, T.R. An update on the genetics of hyperuricaemia and gout. Nat. Rev. Rheumatol. 2018, 14, 341–353. [Google Scholar] [CrossRef]
- Choi, H.K.; McCormick, N.; Lu, N.; Rai, S.K.; Yokose, C.; Zhang, Y. Population Impact Attributable to Modifiable Risk Factors for Hyperuricemia. Arthritis Rheumatol. 2020, 72, 157–165. [Google Scholar] [CrossRef] [PubMed]
- McCormick, N.; Rai, S.K.; Lu, N.; Yokose, C.; Curhan, G.C.; Choi, H.K. Estimation of Primary Prevention of Gout in Men Through Modification of Obesity and Other Key Lifestyle Factors. JAMA Netw. Open 2020, 3, e2027421. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, L.A.; Kim, S.C. Gout: A review of nonmodifiable and modifiable risk factors. Rheum. Dis. Clin. N. Am. 2014, 40, 581–604. [Google Scholar] [CrossRef]
- McCormick, N.; Yokose, C.; Lu, N.; Joshi, A.D.; Curhan, G.C.; Choi, H.K. Impact of adiposity on risk of female gout among those genetically predisposed: Sex-specific prospective cohort study findings over >32 years. Ann. Rheum. Dis. 2022, 81, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; McCormick, N.; Yokose, C.; Joshi, A.D.; Lu, N.; Curhan, G.C.; Merriman, T.R.; Saag, K.G.; Ridker, P.M.; Buring, J.E.; et al. Interactions Between Genetic Risk and Diet Influencing Risk of Incident Female Gout: Discovery and Replication Analysis of Four Prospective Cohorts. Arthritis Rheumatol. 2022, 75, 1028–1038. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. NCHHSTP Social Determinants of Health. 2023. Available online: https://www.cdc.gov/nchhstp/socialdeterminants/faq.html (accessed on 4 February 2023).
- U.S. Department of Health & Human Services. Minority Health and Health Disparities Research. Available online: https://www.nih.gov/ending-structural-racism/minority-health-health-disparities-research (accessed on 4 February 2023).
- Guillen, A.G.; Te Karu, L.; Singh, J.A.; Dalbeth, N. Gender and Ethnic Inequities in Gout Burden and Management. Rheum. Dis. Clin. N. Am. 2020, 46, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.J.; Rideout, B.A. Uric acid and diet—Insights into the epidemic of cardiovascular disease. N. Engl. J. Med. 2004, 350, 1071–1073. [Google Scholar] [CrossRef]
- Cassim, B.; Mody, G.M.; Deenadayalu, V.K.; Hammond, M.G. Gout in black South Africans: A clinical and genetic study. Ann. Rheum. Dis. 1994, 53, 759–762. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.C.; Thomas, J.; Thomas, D.J.; Mead, L.; Levine, D.M.; Klag, M.J. Racial differences in the incidence of gout. The role of hypertension. Arthritis Rheum. 1995, 38, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Wu, Y.Y.; Cooney, R.V.; Wilkens, L.R.; Haiman, C.A.; Pirkle, C.M. Modifiable Factors and Incident Gout across Ethnicity within a Large Multiethnic Cohort of Older Adults. J. Rheumatol. 2022, 49, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Puig, J.G.; Michan, A.D.; Jimenez, M.L.; Perez de Ayala, C.; Mateos, F.A.; Capitan, C.F.; de Miguel, E.; Gijon, J.B. Female gout. Clinical spectrum and uric acid metabolism. Arch. Intern. Med. 1991, 151, 726–732. [Google Scholar] [CrossRef]
- Harrold, L.R.; Yood, R.A.; Mikuls, T.R.; Andrade, S.E.; Davis, J.; Fuller, J.; Chan, K.A.; Roblin, D.; Raebel, M.A.; Von Worley, A.; et al. Sex differences in gout epidemiology: Evaluation and treatment. Ann. Rheum. Dis. 2006, 65, 1368–1372. [Google Scholar] [CrossRef]
- Harrold, L.R.; Etzel, C.J.; Gibofsky, A.; Kremer, J.M.; Pillinger, M.H.; Saag, K.G.; Schlesinger, N.; Terkeltaub, R.; Cox, V.; Greenberg, J.D. Sex differences in gout characteristics: Tailoring care for women and men. BMC Musculoskelet. Disord. 2017, 18, 108. [Google Scholar] [CrossRef]
- Te Kampe, R.; Janssen, M.; van Durme, C.; Jansen, T.L.; Boonen, A. Sex Differences in the Clinical Profile Among Patients With Gout: Cross-sectional Analyses of an Observational Study. J. Rheumatol. 2021, 48, 286–292. [Google Scholar] [CrossRef]
- Flegal, K.M.; Carroll, M.D.; Ogden, C.L.; Johnson, C.L. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002, 288, 1723–1727. [Google Scholar] [CrossRef]
- Liu, B.; Du, Y.; Wu, Y.; Snetselaar, L.G.; Wallace, R.B.; Bao, W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: Population based study. BMJ 2021, 372, n365. [Google Scholar] [CrossRef]
- Helget, L.N.; England, B.R.; Roul, P.; Sayles, H.; Petro, A.D.; Michaud, K.; Mikuls, T.R. Incidence, Prevalence, and Burden of Gout in the Veterans Health Administration. Arthritis Care Res. 2021, 73, 1363–1371. [Google Scholar] [CrossRef]
- McCormick, N.; Lu, N.; Yokose, C.; Joshi, A.D.; Sheehy, S.; Rosenberg, L.; Warner, E.T.; Dalbeth, N.; Merriman, T.R.; Saag, K.G.; et al. Racial and Sex Disparities in Gout in US Adults. JAMA Netw. Open 2022, 5, e2226804. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, E. Gout in African Americans. Am. J. Med. 2014, 127, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Maynard, J.W.; McAdams-DeMarco, M.A.; Law, A.; Kao, L.; Gelber, A.C.; Coresh, J.; Baer, A.N. Racial differences in gout incidence in a population-based cohort: Atherosclerosis Risk in Communities Study. Am. J. Epidemiol. 2014, 179, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Gaffo, A.L.; Jacobs, D.R., Jr.; Lewis, C.E.; Mikuls, T.R.; Saag, K.G. Association between being African-American, serum urate levels and the risk of developing hyperuricemia: Findings from the Coronary Artery Risk Development in Young Adults cohort. Arthritis Res. Ther. 2012, 14, R4. [Google Scholar] [CrossRef] [PubMed]
- McAdams-DeMarco, M.A.; Law, A.; Maynard, J.W.; Coresh, J.; Baer, A.N. Risk factors for incident hyperuricemia during mid-adulthood in African American and white men and women enrolled in the ARIC cohort study. BMC Musculoskelet. Disord. 2013, 14, 347. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Guo, C.Y.; Cupples, L.A.; Levy, D.; Wilson, P.W.; Fox, C.S. Genome-wide search for genes affecting serum uric acid levels: The Framingham Heart Study. Metabolism 2005, 54, 1435–1441. [Google Scholar] [CrossRef]
- Krishnan, E.; Lessov-Schlaggar, C.N.; Krasnow, R.E.; Swan, G.E. Nature versus nurture in gout: A twin study. Am. J. Med. 2012, 125, 499–504. [Google Scholar] [CrossRef]
- Roman, Y.M. Moving the Needle in Gout Management: The Role of Culture, Diet, Genetics, and Personalized Patient Care Practices. Nutrients 2022, 14, 3590. [Google Scholar] [CrossRef]
- Banda, Y.; Kvale, M.N.; Hoffmann, T.J.; Hesselson, S.E.; Ranatunga, D.; Tang, H.; Sabatti, C.; Croen, L.A.; Dispensa, B.P.; Henderson, M.; et al. Characterizing Race/Ethnicity and Genetic Ancestry for 100,000 Subjects in the Genetic Epidemiology Research on Adult Health and Aging (GERA) Cohort. Genetics 2015, 200, 1285–1295. [Google Scholar] [CrossRef]
- Tin, A.; Marten, J.; Halperin Kuhns, V.L.; Li, Y.; Wuttke, M.; Kirsten, H.; Sieber, K.B.; Qiu, C.; Gorski, M.; Yu, Z.; et al. Target genes, variants, tissues and transcriptional pathways influencing human serum urate levels. Nat. Genet. 2019, 51, 1459–1474. [Google Scholar] [CrossRef]
- Howard, G.; Cushman, M.; Moy, C.S.; Oparil, S.; Muntner, P.; Lackland, D.T.; Manly, J.J.; Flaherty, M.L.; Judd, S.E.; Wadley, V.G.; et al. Association of Clinical and Social Factors With Excess Hypertension Risk in Black Compared With White US Adults. JAMA 2018, 320, 1338–1348. [Google Scholar] [CrossRef]
- McCormick, N.; Lu, N.; Yokose, C.; Joshi, A.D.; Merriman, T.R.; Saag, K.; Zhang, Y.; Choi, H.K. What drives racial disparities in gout in the US?—Population-based, sex-specific, casual mediation analysis. Ann. Rheum. Dis. 2022, 81, 305–306. [Google Scholar] [CrossRef]
- Valeri, L.; Vanderweele, T.J. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychol. Methods 2013, 18, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Steen, J.; Loeys, T.; Moerkerke, B.; Vansteelandt, S. Flexible Mediation Analysis With Multiple Mediators. Am. J. Epidemiol. 2017, 186, 184–193. [Google Scholar] [CrossRef]
- Derksen, C.; Murdoch, R.; Petrie, K.J.; Dalbeth, N. “An apple pie a day does not keep the doctor away”: Fictional depictions of gout in contemporary film and television. BMC Rheumatol. 2021, 5, 4. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Huang, M.; Fang, M.; Xie, X.; Huang, Z. Socioeconomic differences in hyperuricemia and gout: A systematic review and meta-analysis. Endocrine 2020, 69, 286–293. [Google Scholar] [CrossRef]
- Kapetanovic, M.C.; Hameed, M.; Turkiewicz, A.; Neogi, T.; Saxne, T.; Jacobsson, L.; Englund, M. Prevalence and incidence of gout in southern Sweden from the socioeconomic perspective. RMD Open 2016, 2, e000326. [Google Scholar] [CrossRef]
- US Department of Agriculture. SNAP Eligibility. Available online: https://www.fns.usda.gov/snap/recipient/eligibility (accessed on 4 February 2023).
- Hayward, R.A.; Rathod, T.; Roddy, E.; Muller, S.; Hider, S.L.; Mallen, C.D. The association of gout with socioeconomic status in primary care: A cross-sectional observational study. Rheumatology 2013, 52, 2004–2008. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Fakhouri, T.H.; Carroll, M.D.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Adults, by Household Income and Education—United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1369–1373. [Google Scholar] [CrossRef]
- Myers, C.A.; Mire, E.F.; Katzmarzyk, P.T. Trends in Adiposity and Food Insecurity Among US Adults. JAMA Netw. Open 2020, 3, e2012767. [Google Scholar] [CrossRef]
- Juraschek, S.P.; Gelber, A.C.; Choi, H.K.; Appel, L.J.; Miller, E.R., 3rd. Effects of the Dietary Approaches To Stop Hypertension (DASH) Diet and Sodium Intake on Serum Uric Acid. Arthritis Rheumatol. 2016, 68, 3002–3009. [Google Scholar] [CrossRef] [PubMed]
- Juraschek, S.P.; Yokose, C.; McCormick, N.; Miller, E.R., 3rd; Appel, L.J.; Choi, H.K. Effects of Dietary Patterns on Serum Urate: Results From a Randomized Trial of the Effects of Diet on Hypertension. Arthritis Rheumatol. 2021, 73, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Yokose, C.; McCormick, N.; Lu, N.; Joshi, A.D.; Curhan, G.; Choi, H.K. Adherence to 2020 to 2025 Dietary Guidelines for Americans and the Risk of New-Onset Female Gout. JAMA Intern. Med. 2022, 182, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Rai, S.K.; Fung, T.T.; Lu, N.; Keller, S.F.; Curhan, G.C.; Choi, H.K. The Dietary Approaches to Stop Hypertension (DASH) diet, Western diet, and risk of gout in men: Prospective cohort study. BMJ 2017, 357, j1794. [Google Scholar] [CrossRef] [PubMed]
- Emmerson, B. Hyperlipidaemia in hyperuricaemia and gout. Ann. Rheum. Dis. 1998, 57, 509–510. [Google Scholar] [CrossRef] [PubMed]
- Fam, A.G. Gout, diet, and the insulin resistance syndrome. J. Rheumatol. 2002, 29, 1350–1355. [Google Scholar]
- Quinones Galvan, A.; Natali, A.; Baldi, S.; Frascerra, S.; Sanna, G.; Ciociaro, D.; Ferrannini, E. Effect of insulin on uric acid excretion in humans. Am. J. Physiol. 1995, 268, E1–E5. [Google Scholar] [CrossRef]
- Solomon, D.H.; Glynn, R.J.; MacFadyen, J.G.; Libby, P.; Thuren, T.; Everett, B.M.; Ridker, P.M. Relationship of Interleukin-1beta Blockade With Incident Gout and Serum Uric Acid Levels: Exploratory Analysis of a Randomized Controlled Trial. Ann. Intern. Med. 2018, 169, 535–542. [Google Scholar] [CrossRef]
- Hart, M.J.; Torres, S.J.; McNaughton, S.A.; Milte, C.M. Dietary patterns and associations with biomarkers of inflammation in adults: A systematic review of observational studies. Nutr. J. 2021, 20, 24. [Google Scholar] [CrossRef]
- Monsivais, P.; Rehm, C.D.; Drewnowski, A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern. Med. 2013, 173, 1922–1924. [Google Scholar] [CrossRef]
- Mackenbach, J.D.; Burgoine, T.; Lakerveld, J.; Forouhi, N.G.; Griffin, S.J.; Wareham, N.J.; Monsivais, P. Accessibility and Affordability of Supermarkets: Associations With the DASH Diet. Am. J. Prev. Med. 2017, 53, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Crews, D.C.; Kuczmarski, M.F.; Miller, E.R., 3rd; Zonderman, A.B.; Evans, M.K.; Powe, N.R. Dietary habits, poverty, and chronic kidney disease in an urban population. J. Ren. Nutr. 2015, 25, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Curhan, G. Beer, Liquor, Wine, and Serum Uric Acid Level—The Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2004, 51, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Willett, W.C.; Curhan, G. Alcohol Intake and Risk of Incident Gout in Men—A Prospective Study. Lancet 2004, 363, 1277–1281. [Google Scholar] [CrossRef]
- Neogi, T.; Chen, C.; Niu, J.; Chaisson, C.; Hunter, D.J.; Zhang, Y. Alcohol quantity and type on risk of recurrent gout attacks: An internet-based case-crossover study. Am. J. Med. 2014, 127, 311–318. [Google Scholar] [CrossRef]
- Zhang, Y.; Woods, R.; Chaisson, C.E.; Neogi, T.; Niu, J.; McAlindon, T.E.; Hunter, D. Alcohol consumption as a trigger of recurrent gout attacks. Am. J. Med. 2006, 119, 800.e11–800.e16. [Google Scholar] [CrossRef]
- Sa, J.; Russell, M.; Weintruab, M.R.; Seo, D.C.; Chaput, J.P.; Habib, M. Gender and Racial/Ethnic Differences in the Association Between Alcohol Drinking Patterns and Body Mass Index-the National Health and Nutrition Examination Survey, 1999–2010. J. Racial Ethn. Health Disparit. 2019, 6, 301–311. [Google Scholar] [CrossRef]
- Aune, D.; Norat, T.; Vatten, L.J. Body mass index and the risk of gout: A systematic review and dose-response meta-analysis of prospective studies. Eur. J. Nutr. 2014, 53, 1591–1601. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015, 41, 311–330. [Google Scholar] [CrossRef]
- Aggarwal, R.; Chiu, N.; Wadhera, R.K.; Moran, A.E.; Raber, I.; Shen, C.; Yeh, R.W.; Kazi, D.S. Racial/Ethnic Disparities in Hypertension Prevalence, Awareness, Treatment, and Control in the United States, 2013 to 2018. Hypertension 2021, 78, 1719–1726. [Google Scholar] [CrossRef]
- Sehgal, A.R. Overlap between whites and blacks in response to antihypertensive drugs. Hypertension 2004, 43, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Soriano, L.C.; Zhang, Y.; Rodriguez, L.A. Antihypertensive drugs and risk of incident gout among patients with hypertension: Population based case-control study. BMJ 2012, 344, d8190. [Google Scholar] [CrossRef] [PubMed]
- Juraschek, S.P.; Simpson, L.M.; Davis, B.R.; Shmerling, R.H.; Beach, J.L.; Ishak, A.; Mukamal, K.J. The effects of antihypertensive class on gout in older adults: Secondary analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. J. Hypertens. 2020, 38, 954–960. [Google Scholar] [CrossRef]
- Bruderer, S.; Bodmer, M.; Jick, S.S.; Meier, C.R. Use of diuretics and risk of incident gout: A population-based case-control study. Arthritis Rheumatol. 2014, 66, 185–196. [Google Scholar] [CrossRef]
- Murphy, D.; McCulloch, C.E.; Lin, F.; Banerjee, T.; Bragg-Gresham, J.L.; Eberhardt, M.S.; Morgenstern, H.; Pavkov, M.E.; Saran, R.; Powe, N.R.; et al. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann. Intern. Med. 2016, 165, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Foster, M.C.; Coresh, J.; Fornage, M.; Astor, B.C.; Grams, M.; Franceschini, N.; Boerwinkle, E.; Parekh, R.S.; Kao, W.H. APOL1 variants associate with increased risk of CKD among African Americans. J. Am. Soc. Nephrol. 2013, 24, 1484–1491. [Google Scholar] [CrossRef]
- Chen, T.K.; Coresh, J.; Daya, N.; Ballew, S.H.; Tin, A.; Crews, D.C.; Grams, M.E. Race, APOL1 Risk Variants, and Clinical Outcomes among Older Adults: The ARIC Study. J. Am. Geriatr. Soc. 2021, 69, 155–163. [Google Scholar] [CrossRef]
- Norton, J.M.; Moxey-Mims, M.M.; Eggers, P.W.; Narva, A.S.; Star, R.A.; Kimmel, P.L.; Rodgers, G.P. Social Determinants of Racial Disparities in CKD. J. Am. Soc. Nephrol. 2016, 27, 2576–2595. [Google Scholar] [CrossRef]
- Tarver-Carr, M.E.; Powe, N.R.; Eberhardt, M.S.; LaVeist, T.A.; Kington, R.S.; Coresh, J.; Brancati, F.L. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: A population-based study of potential explanatory factors. J. Am. Soc. Nephrol. 2002, 13, 2363–2370. [Google Scholar] [CrossRef]
- Evans, K.; Coresh, J.; Bash, L.D.; Gary-Webb, T.; Kottgen, A.; Carson, K.; Boulware, L.E. Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol. Dial. Transplant. 2011, 26, 899–908. [Google Scholar] [CrossRef]
- Krishnan, E.; Lienesch, D.; Kwoh, C.K. Gout in ambulatory care settings in the United States. J. Rheumatol. 2008, 35, 498–501. [Google Scholar] [PubMed]
- Chen-Xu, M.; Yokose, C.; Rai, S.K.; Pillinger, M.H.; Choi, H.K. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis Rheumatol. 2019, 71, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.H.; Avorn, J.; Levin, R.; Brookhart, M.A. Uric acid lowering therapy: Prescribing patterns in a large cohort of older adults. Ann. Rheum. Dis. 2008, 67, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Richman, J.; Yang, S.; Bridges, S.L.; Saag, K. Allopurinol adherence and its predictors in gout: A national cohort study in US veterans. Lancet Rheumatol. 2020, 2, e281–e291. [Google Scholar] [CrossRef] [PubMed]
- Rashid, N.; Coburn, B.W.; Wu, Y.L.; Cheetham, T.C.; Curtis, J.R.; Saag, K.G.; Mikuls, T.R. Modifiable factors associated with allopurinol adherence and outcomes among patients with gout in an integrated healthcare system. J. Rheumatol. 2015, 42, 504–512. [Google Scholar] [CrossRef]
- Singh, J.A.; Yang, S.; Saag, K.G. Factors Influencing the Effectiveness of Allopurinol in Achieving and Sustaining Target Serum Urate in a US Veterans Affairs Gout Cohort. J. Rheumatol. 2020, 47, 449–460. [Google Scholar] [CrossRef]
- Singh, J.A.; Bharat, A.; Khanna, D.; Aquino-Beaton, C.; Persselin, J.E.; Duffy, E.; Elashoff, D.; Khanna, P.P. Racial differences in health-related quality of life and functional ability in patients with gout. Rheumatology 2017, 56, 103–112. [Google Scholar] [CrossRef]
- Burke, B.T.; Kottgen, A.; Law, A.; Windham, B.G.; Segev, D.; Baer, A.N.; Coresh, J.; McAdams-DeMarco, M.A. Physical Function, Hyperuricemia, and Gout in Older Adults. Arthritis Care Res. 2015, 67, 1730–1738. [Google Scholar] [CrossRef]
- Jackson, R.; Shiozawa, A.; Buysman, E.K.; Altan, A.; Korrer, S.; Choi, H. Flare frequency, healthcare resource utilisation and costs among patients with gout in a managed care setting: A retrospective medical claims-based analysis. BMJ Open 2015, 5, e007214. [Google Scholar] [CrossRef]
- Yokose, C.; McCormick, N.; Lu, N.; Joshi, A.D.; Jackson, L.; Kohler, M.J.; Yinh, J.; Zhang, Y.; Hsu, J.; Dalbeth, N.; et al. Nationwide racial/ethnic disparities in US emergency department visits and hospitalizations for gout. Rheumatology 2022, 62, 2247–2251. [Google Scholar] [CrossRef]
- Singh, J.A.; Bharat, A.; Khanna, D.; Aquino-Beaton, C.; Persselin, J.E.; Duffy, E.; Elashoff, D.; Khanna, P.P. Health care utilization in patients with gout: A prospective multicenter cohort study. BMC Musculoskelet. Disord. 2017, 18, 233. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Mount, D.B.; Reginato, A.M. Pathogenesis of gout. Ann. Intern. Med. 2005, 143, 499–516. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Pandya, B.J.; Choi, H.K. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am. J. Med. 2012, 125, 679–687. [Google Scholar] [CrossRef]
- Choi, H.K.; Curhan, G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation 2007, 116, 894–900. [Google Scholar] [CrossRef]
- Krishnan, E.; Svendsen, K.; Neaton, J.D.; Grandits, G.; Kuller, L.H. Long-term cardiovascular mortality among middle-aged men with gout. Arch. Intern. Med. 2008, 168, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Chandrakumar, H.P.; Puskoor, A.V.; Chillumuntala, S.; Sharif, S.; Mora, D.C.; Gupta, T.; Tadayoni, A.; Zonnoor, S.L.; Celiker, P.; Yakoubovitch, S.; et al. Assessment of Cardiovascular Disease Among Predominantly Black Gout Patients. J. Clin. Rheumatol. 2023, 29, 202–206. [Google Scholar] [CrossRef]
- Johnston, K.J.; Hammond, G.; Meyers, D.J.; Joynt Maddox, K.E. Association of Race and Ethnicity and Medicare Program Type With Ambulatory Care Access and Quality Measures. JAMA 2021, 326, 628–636. [Google Scholar] [CrossRef]
- Wallace, J.; Lollo, A.; Duchowny, K.A.; Lavallee, M.; Ndumele, C.D. Disparities in Health Care Spending and Utilization Among Black and White Medicaid Enrollees. JAMA Health Forum 2022, 3, e221398. [Google Scholar] [CrossRef]
- Bailey, Z.D.; Krieger, N.; Agenor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Alrajeh, K.; Roman, Y. Pharmacogenetic Perspective for Optimal Gout Management. Future Pharmacol. 2022, 2, 135–152. [Google Scholar] [CrossRef]
- Thomas, E.A.; Enduru, N.; Tin, A.; Boerwinkle, E.; Griswold, M.E.; Mosley, T.H.; Gottesman, R.F.; Fornage, M. Polygenic Risk, Midlife Life’s Simple 7, and Lifetime Risk of Stroke. J. Am. Heart Assoc. 2022, 11, e025703. [Google Scholar] [CrossRef] [PubMed]
- Hasbani, N.R.; Ligthart, S.; Brown, M.R.; Heath, A.S.; Bebo, A.; Ashley, K.E.; Boerwinkle, E.; Morrison, A.C.; Folsom, A.R.; Aguilar, D.; et al. American Heart Association’s Life’s Simple 7: Lifestyle Recommendations, Polygenic Risk, and Lifetime Risk of Coronary Heart Disease. Circulation 2022, 145, 808–818. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Rhodes, L.; Young, K.L.; Lilly, A.G.; Raffield, L.M.; Highland, H.M.; Wojcik, G.L.; Agler, C.; Love, S.M.; Okello, S.; Petty, L.E.; et al. Importance of Genetic Studies of Cardiometabolic Disease in Diverse Populations. Circ. Res. 2020, 126, 1816–1840. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.R.; Kanai, M.; Kamatani, Y.; Okada, Y.; Neale, B.M.; Daly, M.J. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 2019, 51, 584–591. [Google Scholar] [CrossRef]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Curhan, G. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: The health professionals follow-up study. Arch. Intern. Med. 2005, 165, 742–748. [Google Scholar] [CrossRef]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Willett, W.C.; Curhan, G. Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men. New. Eng. J. Med. 2004, 350, 1093–1103. [Google Scholar] [CrossRef]
- Choi, H.K.; Curhan, G. Soft drinks, fructose consumption, and the risk of gout in men: Prospective cohort study. BMJ 2008, 336, 309–312. [Google Scholar] [CrossRef]
- Choi, H.K.; Willett, W.; Curhan, G. Fructose-rich beverages and risk of gout in women. JAMA 2010, 304, 2270–2278. [Google Scholar] [CrossRef]
- Choi, H.K.; Willett, W.; Curhan, G. Coffee consumption and risk of incident gout in men: A prospective study. Arthritis Rheum. 2007, 56, 2049–2055. [Google Scholar] [CrossRef]
- Choi, H.K.; Curhan, G. Coffee consumption and risk of incident gout in women: The Nurses’ Health Study. Am. J. Clin. Nutr. 2010, 92, 922–927. [Google Scholar] [CrossRef]
- Choi, H.K.; Gao, X.; Curhan, G. Vitamin C intake and the risk of gout in men: A prospective study. Arch. Intern. Med. 2009, 169, 502–507. [Google Scholar] [CrossRef] [PubMed]

| Study | Years | Black vs. White Disparity | Data Source/Population |
|---|---|---|---|
| Gout Prevalence, % or Odds Ratio | |||
| Helget et al. [22] | 2014 | 7.0% (7.0 to 7.1) vs. 6.0% (5.9 to 6.0) | Veteran’s Affairs (99% male) |
| McCormick et al. [23] | 2007–2016 | Overall: 1.46 (1.22 to 1.74) | NHANES (US general population) |
| Women: 1.81 (1.29 to 2.53) | |||
| Men: 1.26 (1.02 to 1.55) | |||
| Gout Incidence, Relative Risk or Incidence Rate | |||
| Hochberg et al. [14] | 1957–64 (Hopkins) and 1958–65 (Meharry), to 1988–92 | 1.69 (1.02 to 2.80) | Meharry-Hopkins Study (male physicians) |
| Krishnan et al. [24] | 1973–75 to 1980–82 | 0.95 (0.64 to 1.41) | MR-FIT Study (all males) |
| Helget et al. [22] | 2014 | 7.3 (7.1 to 7.5) vs. 5.9 (5.8 to 6.0) per 1000 PY | Veteran’s Affairs (99% male) |
| Maynard et al. [25] | 1987–89 to 2012 | Women: 2.51 (2.03 to 3.12) | ARIC |
| Men: 1.73 (1.37 to 2.18) | |||
| Thompson et al. [15] | 1999 to 2016 | 1.34 (1.26 to 1.43) | Multiethnic Cohort Study (Medicare beneficiaries) |
| Hyperuricemia Prevalence, Odds Ratio | |||
| McCormick et al. [23] | 2007–2016 | Women: 2.00 (1.62 to 2.47) | NHANES (US general population) |
| Men: 1.39 (1.15 to 1.68) | |||
| Hyperuricemia Incidence, Relative Risk | |||
| Gaffo et al. [26] | 1985–86 to 2005–06 | Women: 2.79 (2.02 to 3.86) | CARDIA |
| Men: 0.87 (0.73 to 1.04) | |||
| McAdams-DeMarco et al. [27] | 1987–89 to 1996–99 | 1.79 (1.37 to 2.33) | ARIC |
| Krishnan et al. [24] | 1973–75 to 1980–82 | 1.10 (0.98 to 1.24) | MR-FIT Study (all males) |
| Study | Black vs. White Disparity | Data Source/Population |
|---|---|---|
| Quality Of Care and Health Outcomes | ||
| Urate-Lowering Therapy Use, Odds Ratio | ||
| Krishnan et al. [74] | 0.18 (0.04 to 0.78) | NACS (US general population) |
| Chen-Xu et al. [75] | 0.84 (0.53 to 1.34) | NHANES (US general population) |
| Adherence to Urate-Lowering Therapy (≥80% of Days Covered), Odds Ratio | ||
| Rashid et al. [78] | 0.68 (0.62 to 0.76) | Managed healthcare plan |
| Solomon et al. [76] | 0.54 (0.44 to 0.66) | US Medicare |
| Singh et al. [77] | 0.74 (0.72 to 0.76) | Veteran’s Affairs (99% male) |
| Achieving Target Serum Urate (<6 mg/dL), Odds Ratio | ||
| Rashid et al. [78] | 0.80 (0.78 to 0.89) | Managed healthcare plan |
| Singh et al. [79] | 0.94 (0.89 to 0.99) | Veteran’s Affairs (99% male) |
| Health-Related Quality of Life, Mean Score or Prevalence Ratio | ||
| Singh et al. [80] | SF-36 Mental Health: 40.8 vs. 46.3 (p < 0.01) 1 | Veteran’s Affairs (98% male) |
| SF-36 Role Emotional: 31.3 vs. 40.6 (p < 0.01) 1 | ||
| SF-36 Social Functioning: 37.3 vs. 41.5 (p = 0.04) 1 | ||
| SF-36 Mental Component: 39.5 vs. 46.2 (p < 0.01) 1 | ||
| GIS Gout Concern: 73.7 vs. 64.3 (p < 0.01) 2 | ||
| GIS Unmet Treatment Need: 41.4 vs. 33.9 (p < 0.01) 2 | ||
| GIS Well-Being During Attacks: 61.7 vs. 51.1 (p < 0.01) 2 | ||
| GIS Concern During Attacks: 60.4 vs. 50.0 (p < 0.01) 2 | ||
| Teevan Burke et al. [81] | Poor SPPB score: 1.35 (1.09 to 1.66) 3 | ARIC |
| Poor walking speed: 1.61 (1.26 to 2.05) | ||
| Flare Frequency, Rate Ratio | ||
| Jackson et al. [82] | 1.17 (1.11 to 1.23) | Managed healthcare plan |
| Healthcare Ulitization and Costs | ||
| Gout-Related Healthcare Costs, Cost Ratio | ||
| Jackson et al. [82] | 1.16 (1.05 to 1.28) | Managed healthcare plan |
| Gout-Primary Inpatient Hospitalisations, Rate Ratio | ||
| Yokose et al., 2022 [83] | All: 4.07 (3.90 to 4.24) | NIS (US general population) |
| Women: 4.80 (4.45 to 5.17) | ||
| Men: 3.76 (3.57 to 3.95) | ||
| Gout-Primary Emergency Department Visits, Rate Ratio | ||
| Yokose et al., 2022 [83] | All: 5.01 (4.96 to 5.06) | NEDS (US general population) |
| Women: 5.91 (5.79 to 6.03) | ||
| Men: 4.73 (4.68 to 4.79) | ||
| Singh et al. [84] | RR 2.68 (1.48 to 4.86) * | Veteran’s Affairs (98% male) |
| Gout-Primary Inpatient Hospitalisations, Mean Excess Cost per Admission | ||
| Yokose et al., 2022 [83] | All: $916.30 ($450.00 to $1382.50) | NIS (US general population) |
| Women: $1530.20 ($671.40 to $2388.90) | ||
| Men: $618.90 ($24.60 to $1213.20) | ||
| Ambulatory Visits for Gout, Rate Ratio | ||
| Singh et al. [84] | 1.80 (1.30 to 2.50) | Veteran’s Affairs (98% male) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCormick, N.; Yokose, C.; Choi, H.K. What Drives the Contemporary Black–White Racial Disparities in Gout in the US? Impact of Social Determinants of Health. Gout Urate Cryst. Depos. Dis. 2023, 1, 99-114. https://doi.org/10.3390/gucdd1020010
McCormick N, Yokose C, Choi HK. What Drives the Contemporary Black–White Racial Disparities in Gout in the US? Impact of Social Determinants of Health. Gout, Urate, and Crystal Deposition Disease. 2023; 1(2):99-114. https://doi.org/10.3390/gucdd1020010
Chicago/Turabian StyleMcCormick, Natalie, Chio Yokose, and Hyon K. Choi. 2023. "What Drives the Contemporary Black–White Racial Disparities in Gout in the US? Impact of Social Determinants of Health" Gout, Urate, and Crystal Deposition Disease 1, no. 2: 99-114. https://doi.org/10.3390/gucdd1020010
APA StyleMcCormick, N., Yokose, C., & Choi, H. K. (2023). What Drives the Contemporary Black–White Racial Disparities in Gout in the US? Impact of Social Determinants of Health. Gout, Urate, and Crystal Deposition Disease, 1(2), 99-114. https://doi.org/10.3390/gucdd1020010







