Abstract
(1) Background: Patients who experience acute traumatic injury requiring hospitalisation represent a vulnerable population. The trauma patient often experiences multi-system injuries and complex physiology. Additionally, there are complex socio-ecological issues that impact the care and outcomes of trauma patients. Of interest, culturally and linguistically diverse populations with language barriers experience worse outcomes in trauma settings. This scoping review evaluates the current evidence on language barriers in this population and the influences on outcomes for trauma patients. (2) Methods: A scoping review was performed following a computer-assisted search of the Medline, Embase and Cochrane Central databases. Papers that evaluated the impact of the language barrier in culturally and linguistically diverse populations and outcomes in acute trauma settings were included. (3) Results: A literature search identified eight articles that were eligible for inclusion. Overall, there was no robust evidence to suggest that such populations were disadvantaged in terms of length of hospital stay and overall mortality. However, studies did identify that these populations were at higher risk of disability and poor mental health outcomes, experienced communication barriers more often and had lower social functioning. (4) Conclusions: This scoping review demonstrates that individuals admitted due to trauma who are from culturally and linguistically diverse backgrounds experience more significant disadvantages concerning psychological and functional outcomes. It is posited this is due to their inability to communicate their complex needs in trauma, however more robust and rigorous research is required to better characterise this effect.
1. Introduction
Patients who sustain traumatic injuries requiring hospital admission represent a unique vulnerable population. Specifically, the trauma patient often experiences multi-system injuries that require multidisciplinary care. Additionally, they exhibit well characterised complex physiological responses that stem from the systemic immune response to trauma including perturbations to homeostasis and impairment of essential processes such as wound healing, response to infection, coagulation and immune function [1,2,3]. Such findings have led to significant advancements in the care of the modern trauma patient, influencing aspects of management including resuscitation guidelines, trauma triaging systems and trauma surgery.
An area of interest in trauma care has also been to consider the underlying socio-ecological factors that can influence outcomes in trauma patients and therefore allow trauma clinicians to identify additional avenues for improvement in terms of delivering safe and quality care for these patients. Observational studies have shown clear evidence that ethnicity and minority status affect outcomes in trauma patients including worse mental health and poorer quality of life [4,5,6]. In Australia, 26% of the population are born overseas and 21% of those born overseas speak a language other than English [7]. Studies exploring the social determinants of health have proven that such individuals from culturally and linguistically diverse backgrounds (CALD) have poorer health outcomes attributable to language barriers that hinder access to healthcare services, altered beliefs related to injury and illness that can hinder the types of healthcare received or how healthcare is conceptualised, as well as fear of stigma or discrimination [8,9,10,11,12,13].
Interestingly, when CALD patients are matched for socioeconomic status, they continue to experience worse outcomes in trauma settings [14,15,16]. From an intuitive stand point, one reason that could explain these findings is the language barrier and therefore the difficulties of the trauma patient in communicating their mechanisms of injury, concerns, areas they experience pain, and the other vital medical or relevant information to clinicians. Despite this, the impact of the language barrier on trauma outcomes for CALD patients remains poorly characterised, with a lack of rigorous data in this space. This scoping review therefore looks to evaluate the current evidence around the influence of the language barrier on outcomes following traumatic injury in CALD patients. A further understanding of these impacts may help identify avenues for stakeholders including clinicians, allied health staff and policy makers to further improve the care of trauma patients.
2. Materials and Methods
2.1. Literature Search
A scoping review was conducted in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the Arksey and O’Malley framework for scoping reviews [17,18]. A computer-assisted search of the Medline, Embase and Cochrane Central databases was performed on 19 December 2023. The search combined keywords and relevant medical subject heading (MeSH) terms related to cultural and linguistic diversity, non-English speaking backgrounds, ethnic diversity and outcomes following traumatic injury. The search strategy is presented in Appendix A. Additional articles were hand searched from reference lists of relevant articles where possible.
2.2. Eligibility Criteria
Peer-reviewed full-text articles available in the English language that evaluated the role of linguistic diversity and outcomes following trauma were considered in this review. Specifically, inclusion criteria included papers that assessed the following: (1) adults (age ≥ 18) who are from cultural and linguistically diverse or non-English speaking background who have suffered a traumatic accident and been admitted for same; (2) outcomes including post-admission complications, functional outcomes, mental health outcomes and quality of life outcomes for the population of interest; and (3) were of the following study designs—randomised clinical trials, prospective cohort studies, observational retrospective or cohort studies or cross-sectional studies, case series, abstracts, and qualitative studies. Articles were excluded if they assessed the following: (1) paediatric (age ≤ 17) patients; (2) outcomes not relevant to acute hospital admission such as outcomes associated with community-based rehabilitation programs; (3) psychological trauma and similar presentations without an element of acute traumatic injury; and (4) outcomes that were not of interest.
2.3. Literature Screening
Initial screening by title and abstract with reference to eligibility criteria was performed by two independent investigators (KDRL, KL). Studies that were eligible based on this screening progressed to full-text analysis. Similarly, studies where a decision could not be made during title and abstract screening also progressed to full-text analysis. The same investigators independently undertook full-text analysis of articles for final inclusion in this scoping review. Disagreement at all stages of the literature screening process was resolved by discussion and consensus. A third independent investigator (SL) provided oversight and validation of this process to ensure minimal risk of bias.
2.4. Data Extraction and Synthesis
Relevant data, including demographic data of study populations of included articles and outcomes of interest following trauma admission, were collected where possible. Outcome data were organised into themes for synthesis of results.
2.5. Quality and Risk of Bias Assessment
The methodological quality of included studies was evaluated utilising the Newcastle–Ottawa Scale (NOS) by two independent investigators (KDRL, KL) [19]. Disagreements during this process were resolved by discussion and consensus. A third independent investigator (SL) provided oversight and validation of this process to ensure minimal risk of bias. Quality was classified by total score into the following categories: low quality (NOS < 5), fair quality (NOS 6–7) and good quality (NOS 8–9).
3. Results
3.1. Literature Search Results
A total of 3770 publications were retrieved following a computer-assisted search (Figure 1). Following the removal of duplicate publications, 3333 articles underwent screening by title and abstract according to the eligibility criteria, resulting in 3041 articles being excluded. The remaining 292 articles progressed to full-text analysis. During this process, 107 articles were excluded due to incorrect study design, 163 articles were excluded due to incorrect comparator, 4 were excluded due to incorrect setting, 2 were excluded due to incorrect patient population, 2 were excluded due to incorrect intervention and 6 were excluded due to incorrect outcomes. A total of eight articles met the eligibility criteria and were included in the analysis of this scoping review [14,20,21,22,23,24,25,26].
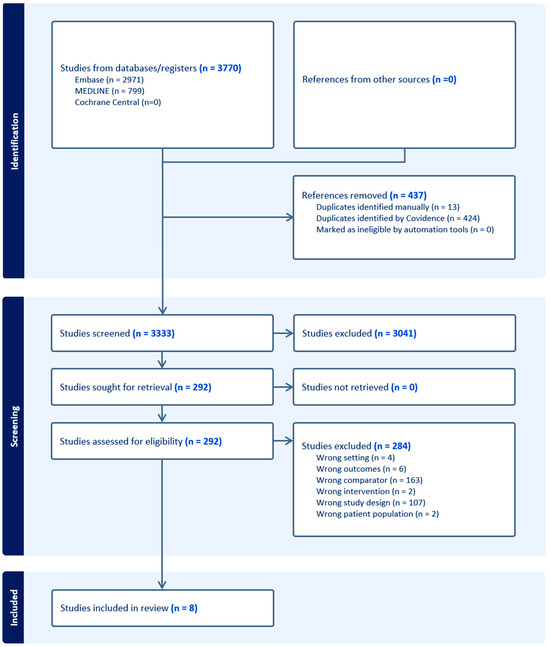
Figure 1.
Search strategy and workflow reported in accordance with the PRISMA guidelines.
3.2. Overview of Studies
The overview of included studies is presented in Table 1. Of the included studies, one was a reflexive thematic analysis, one was a prospective, cross-sectional cohort study and six were retrospective cohort studies. Included articles are represented in Table 1. With the exception of one study published in Australia, the remainder were derived from the United States of America. All but one study were published in the last decade (n = 7, 87.5%). Overall, there was a high proportion of Spanish-speaking individuals in the included studies which was likely a mirror of the Hispanic population of the American studies. With respect to the study populations, non-English speaking CALD patients varied in proportion from 2.39% to 50.70% of the study population.

Table 1.
Overview of studies.
3.3. Comparison of Injury Severity
Four papers compared injury severity between CALD and non-CALD trauma patients, utilising the injury severity score (ISS) system. Three retrospective cohort studies reported no significant difference in ISS between CALD and non-CALD patients [21,23,26]. Alternatively, Meyer et al. documented lower mean ISS scores in CALD patients (10.43; n = 257) compared to non-CALD patients (12.35; n = 10,478) (p = 0.002) in a retrospective cohort study [24]. Interestingly, no papers reported higher ISS from CALD patients. Despite this, it is essential to note that Garduno-Ortega et al. highlighted greater mean periods of post-traumatic amnesia experienced by CALD patients (days = 23.57 ± 25.74) in comparison to non-CALD patients (days = 16.62 ± 18.35) (adjusted difference = 6.7 days SD 3.24, p = 0.04; adjusted for age, sex and cause of trauma) [21].
3.4. Discrepancy in Outcomes of Inpatient Care
Reported outcomes measuring inpatient trauma care differences for CALD and non-CALD patients primarily involved the duration of stay in intensive care unit (ICU), total hospital stay and mortality rates. Two retrospective cohort studies explored differences in durations of hospital stay in CALD and non-CALD cohorts [14,24]. Meyer et al. showed that the CALD cohort (days = 1.75, n = 257) compared to the non-CALD group (days = 2.5, n = 10,478) had shorter stays in the ICU (p = 0.02). Despite this, there were no significant differences in total length of hospital stay between CALD and non-CALD groups [24]. Aligning with this is evidence from Ponsford et al., which similarly reported a lack of significant differences in days spent at the hospital by CALD (n = 100) and non-CALD patients (n = 100) [14]. In terms of mortality rates, three retrospective cohort studies reported quite disparate outcomes. Kinney et al. documented lower survival rates in CALD (82.8%, n = 261) compared to non-CALD (91.9%, n = 5201) cohorts (p < 0.001) [26]. However, Hines et al. reported no significant differences in mortality rates between CALD and non-CALD cohorts, with the sole exception of higher risk-adjusted inpatient mortality rates (per 1000 admissions) in obstetrics-related trauma found in CALD cohorts (specifically persons from Asia and Pacific Islands; API), both following instrument-assisted (API 159.05, n = 71,495; non-API 119.94, n = 3,211,939; p < 0.01) and unassisted (API 34.76, n = 71,495; non-API 22.42, n = 3,211,939; p < 0.01) procedures [22]. In contrast, Meyer et al. highlighted lower rates of mortality in CALD cohorts (2.0%; n = 257) compared to non-CALD groups (6.1%; n = 10,478) (p = 0.008) [24].
3.5. Discrepancy in Functional Outcomes upon Follow-Up Evaluation
Functional outcomes of trauma patients upon follow-up evaluations can be separated into lasting disabilities, morbidities and extent of social participation. Two retrospective cohort studies explored subsequent disability and morbidity after traumatic injuries within CALD and non-CALD cohorts [14,23]. De la Plata et al. found significantly higher rates of severe disability in a 6-month follow-up evaluation of trauma patients with CALD backgrounds (50%; n = 42) compared to non-CALD (29%; n = 377) (p < 0.05) using the Glasgow Outcome Scale-Extended (GOSE) questionnaire [23]. Statistically, this study further revealed that CALD patients had a 15-fold greater likelihood of experiencing severe disability at a 6-month follow-up evaluation after post-traumatic injury compared to non-CALD patients (OR 15.093; 95% CI 1.632–139.617; p = 0.017) [23]. Using the Craig Handicap Assessment and Reporting Technique (CHART), Ponsford et al., demonstrated that CALD patients reported lower scores for cognitive independence (CALD 75.60 ± 26.16, n = 101; non-CALD 85.67 ± 17.30, n = 103; p = 0.031), mobility (CALD 83.04 ± 18.74 n = 101; non-CALD 94.43 ± 12.36, n = 101; p < 0.001) and total CHART scores (CALD 388.42 ± 87.56, n = 97; non-CALD 435.61 ± 58.23, n = 101; p < 0.001), all of which indicates a greater handicap burden experienced by CALD cohorts [14]. Mental health outcomes were additionally evaluated in this study using the Hospital Anxiety and Depression Scale (HADS). Both anxiety (U = 580.5, p = 0.042, Cohen’s d = 0.49) and depression (U = 573, p = 0.035, Cohen’s d = 0.53) were reported to be higher in CALD cohorts compared to non-CALD cohorts on a follow-up evaluation 6 months after [14]. It is important to note that the time of follow-up evaluation was variable in this study, with a mean time of 22.26 months.
Two papers examined social integration and participation in follow-up evaluations with trauma patients [14,25]. Ponsford et al. reported CALD patients had lower mean scores related to occupational performance (CALD 51.80 ± 36.26, n = 97; non-CALD 66.18 ± 30.84, n = 102; p = 0.003), based on the CHART measure [14]. Additionally, in a prospective, cross-sectional cohort study, Sander et al. reported lower rates of social functioning following trauma incidences upon a 1-year follow-up evaluation using the Participation Assessment with Recombined Tools-Objective (PART-O) score [25]. This study found that CALD cohorts (n = 506) had lower scores in comparison to non-CALD cohorts (n = 492) for productivity (CALD 0.90 ± 0.92; non-CALD 1.19 ± 1.02; CI 0.061 (0.16–0.41), p < 0.0001); social relations (CALD 1.90 ± 1.01; non-CALD 2.12 ± 1.00; CI 0.064 (0.09–0.34), p = 0.0007); being ‘out and about’ (CALD 1.38 ± 0.77; non-CALD 1.52 ± 0.84; CI 0.051 (0.04–0.24), p = 0.0065) and total PART-O scores (CALD 0.62 ± 0.7; non-CALD 0.87 ± 0.79; CI 0.047 (0.15–0.34), p < 0.0001), indicating lower social functioning [25]. Interestingly, when adjusted for participant characteristics (including sex; marital status; education level at 1-year follow-up; productivity level at injury; age at injury; post-traumatic amnesia and functional independence measure at 1-year follow-up), significant differences were only evident in social relations (mean score difference 0.117; CI 0.058 (0.002–0.103), p = 0.0461) and total PART-O score (mean score difference 0.088; CI 0.042 (0.006–0.17), p = 0.0361) [25].
3.6. Communication Barriers
Two papers reported existing communication barriers faced by CALD trauma patients in inpatient treatment [14,20]. Using the Illness Perception Questionnaire—Revised (IPQ-R) score, Ponsford et al. highlighted that CALD patients had less understanding (CALD 16.83 ± 5.60, n = 102; non-CALD 18.68 ± 4.45, n = 103; p = 0.017) and feeling of control (CALD 19.86 ± 4.49, n = 101; non-CALD 22.07 ± 4.47, n = 102; p < 0.001) of their condition [14]. In addition, Costello et al. conducted semi-structured interviews for trauma patients and their families of CALD background (n = 15) to explore current issues and barriers faced in linguistically challenging situations [20]. Documented responses revolved around some patients/family members of CALD background finding difficulty communicating with medical professionals and dissatisfaction with current interpreter services (including dialect issues) [20]. Alternatively, in cases where staff from similar cultural backgrounds were available, patients/family members of CALD background reported positively to their given care, with noticeable satisfaction in areas including helpful terminology clarifications and overall feeling of support [20].
3.7. Risk of Bias
A quality and risk of bias assessment was performed utilising the Newcastle–Ottawa Scale (Table 2). Scores ranged from 5 to 8. The median score was 7 with an interquartile range of 1.5 indicating fair quality of the included studies.

Table 2.
Quality and risk of bias assessment of included studies using Newcastle–Ottawa Score.
4. Discussion
Patients who sustain traumatic injuries navigate a complex environment of care. Physiologically, they experience significant challenges to normal homeostatic mechanisms including response to infection, coagulation and wound healing [1,2,3]. This occurs against a background of the need for multidisciplinary care coordination, including management of injuries by multiple specialist medical and surgical consulting teams, engagement of various specialties of allied health and the need to pay attention to the complexities behind mental ill health and the psychology of trauma. It is therefore unsurprising that observational studies demonstrate CALD patients who face language-specific communication barriers are disadvantaged with respect to outcomes following traumatic injury. Despite this, there is a paucity of evidence in this area and no robust data as to the true effect the language barrier has on trauma outcomes. To our knowledge, this scoping review is the first to systematically explore the impact of the language barrier experienced by CALD patients in trauma.
This scoping review has revealed an unexpected finding. Specifically, when comparing CALD patients with language barriers to patients without language barriers, there was no significant robust discrepancy in length of hospital stay or mortality. This finding may be attributable to modern trauma care, which is highly protocolised and standardised across many jurisdictions. Despite this, this scoping review identifies areas in which there are disadvantages for CALD communities including duration of post-traumatic amnesia, functional outcomes including the experience of severe disability and reduced mobility, poor psychological health and reduced cognitive independence and social function. It is likely these outcomes arise from an inability to communicate, and therefore the lower likelihood of tailored care with respect to rehabilitation, counselling and psychological support. More nuanced challenges also exist due to these communication barriers, with studies from this scoping review suggesting that affected patients also experience loss of control, poorer understanding and a reduced ability to explore complex issues during their hospitalisation. In the landscape of holistic trauma care, these perspectives are highly valuable and indicate an unmet need for higher-quality research to drive policies that aim to improve the experience and delivery of trauma care for patients [27].
The accessibility of modern technologies, such as translation tools and open-access generative artificial intelligence tools in addition to in-house or mobile translation services, has allowed health services to navigate the challenge of a language barrier in all settings, inclusive of trauma. Importantly, these generally occur in an ad hoc manner, with no clear guidelines, frameworks or policy to drive the holistic care of the linguistically diverse trauma patient. Intuitively, the presence of modern tools and translation services perhaps is an argument that the care for such patients does not deviate from the norm, however, the results of our scoping review suggests that this may not hold true in a clinical setting. It is likely that these resources are not without their limitations, including impaired niche language access as well as the implications of access to the relevant technology and human resources required in the context of healthcare funding and rurality or remoteness. The advancement and application of generative and conversational artificial intelligence has already been applied diversely within the medical field. Currently, however, it is a constrained resource as there are ongoing risks of bias, misinformation, liability and coercion that could negatively impact patient care. Although these technologies may reduce barriers to care for those who experience difficulties communicating, thereby reducing poorer health outcomes, they need to be further refined to be reliably and safely implemented in clinical practice [28]. This remains a significant area of promise that requires multisectoral collaboration, judicious regulation and reform before widespread implementation. Lastly, trauma teams are often met with competing demands for time, attention and care of acute trauma admissions that inevitably present at all hours of the day. These factors are likely additional confounders that result in disparate outcomes for CALD populations with language barriers who are admitted because of traumatic injury.
4.1. Limitations
Limitations of this review relate primarily to the level of evidence of the included studies. Specifically, our scoping review was performed in light of the paucity of robust evidence that explores the outcomes and effect of the language barrier in these settings. Additionally, there was significant heterogeneity in the included studies that prevented meta-analyses or pooled analyses of the respective trauma cohorts. This also occurs against a background of fair to moderate risk of the bias of included studies, which may hinder analysis of the true effect of the language barrier in trauma populations. Overall, these factors impair the generalisability and validity of these results to diverse trauma populations worldwide. In this way, the results presented must be considered with caution.
4.2. Future Directions
It is clear that for more targeted policy, frameworks and guidelines to be developed for contemporary trauma care, more attention has to be placed in this area. Trauma-based registries are becoming increasingly common and the quality of evidence from these registries, particularly in health services with access to advanced electronic medical records, are avenues to explore in developing the research to inform better practice in this space.
5. Conclusions
This scoping review demonstrates that trauma patients from CALD backgrounds who experience language barriers in the course of their care experience greater disadvantages with respect to psychological and functional outcomes than their English-speaking counterparts. This, however, is drawn from a collection of included studies of fair quality. More robust research is required to interrogate the true effect of the language barrier in such populations to better inform holistic trauma guidelines in the care of minority populations.
Author Contributions
Conceptualization, K.D.R.L.; methodology, K.D.R.L., K.L. and S.J.L.; validation, K.D.R.L., K.L., A.S. and S.J.L.; formal analysis, K.D.R.L., K.L., A.S. and S.J.L.; investigation, K.D.R.L., K.L., A.S. and S.J.L.; resources, K.D.R.L. and K.L.; data curation, K.D.R.L. and K.L.; writing—original draft preparation, K.D.R.L. and K.L.; writing—review and editing, K.D.R.L., K.L., A.S. and S.J.L.; visualization, K.D.R.L., K.L. and S.J.L.; supervision, K.D.R.L.; project administration, K.D.R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data collected for generation of this manuscript was from peer-reviewed open-access peer-reviewed journals available on online medical journal databases.
Conflicts of Interest
The authors declare no conflicts of interest.
Correction Statement
This article has been republished with a minor correction to the readability of Figure 1, and a typo was corrected in the Section 3.1. This change does not affect the scientific content of the article.
Appendix A. Literature Search
- “Wounds and Injuries”/or accidental injuries/or exp amputation, traumatic/or exp multiple trauma/or BrainInjuries, Traumatic/or Brain Injuries/or exp Wounds, Nonpenetrating/or exp Wounds, Penetrating/or Trauma Centers/
- ((trauma* adj3 (injur* or admission* or surger*)) or trauma care or ((major or multiple or serious) adj trauma*)).tw,kf.
- 1 or 2
- Racial Groups/or Ethnicity/or Cross-Cultural Comparison/or Cultural Diversity/
- exp black people/or “black or african american”/or “native hawaiian or other pacific islander”/or “australianaboriginal and torres strait islander peoples”/
- ((cultur* or linguistic* or ethnic* or race or racial or socioethnic* or multicultural) adj2 (divers* or minorit*or group* or population* or background* or difference* or disparit* or variation*)).tw,kf.
- (((indigenous or aboriginal or first nation*) adj3 Australia*) or (Torres Strait Islander* or Maori)).tw.
- 4 or 5 or 6 or 7
- Disability Evaluation/or Outcome Assessment, Health Care/or Survival Rate/or Treatment Outcome/or Recovery ofFunction/or “Patient Discharge”/or exp postoperative complications/
- Stress Disorders, Post-Traumatic/or Depression/or Anxiety Disorders/or Anxiety/
- exp morbidity/or mortality/or hospital mortality/or survival rate/
- (outcome* or survival* or disabilit* or mortality or morbidity).ti,kf.
- (postoperative complication* or post-operative complication*).tw,kf.
- (((posttraumatic or post-traumatic) adj (stress or symptom*)) or anxiety or depression or mental health).ti,kf.
- 9 or 10 or 11 or 12 or 13 or 14)
- 3 and 8 and 15
- ((exp child/or adolescent/) not adult/) or (p?ediatric or child* or infan* or juvenile or adolescen* or teen*).ti.
- 16 not 17
References
- Lord, J.M.; Midwinter, M.J.; Chen, Y.-F.; Belli, A.; Brohi, K.; Kovacs, E.J.; Koenderman, L.; Kubes, P.; Lilford, R.J. The systemic immune response to trauma: An overview of pathophysiology and treatment. Lancet 2014, 384, 1455–1465. [Google Scholar] [CrossRef] [PubMed]
- Osuka, A.; Ogura, H.; Ueyama, M.; Shimazu, T.; Lederer, J.A. Immune response to traumatic injury: Harmony and discordance of immune system homeostasis. Acute Med. Surg. 2014, 1, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Gando, S.; Otomo, Y. Local hemostasis, immunothrombosis, and systemic disseminated intravascular coagulation in trauma and traumatic shock. Crit. Care 2015, 19, 72. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lasprilla, J.C.; Rosenthal, M.; Deluca, J.; Komaroff, E.; Sherer, M.; Cifu, D.; Hanks, R. Traumatic brain injury and functional outcomes: Does minority status matter? Brain Inj. 2007, 21, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lasprilla, J.C.; Kreutzer, J.S. Racial and ethnic disparities in functional, psychosocial, and neurobehavioral outcomes after brain injury. J. Head Trauma Rehabil. 2010, 25, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Perrin, P.B.; Krch, D.; Sutter, M.; Snipes, D.J.; Arango-Lasprilla, J.C.; Kolakowsky-Hayner, S.A.; Wright, J.; Lequerica, A. Racial/ethnic disparities in mental health over the first 2 years after traumatic brain injury: A model systems study. Arch. Phys. Med. Rehabil. 2014, 95, 2288–2295. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Cultural Diversity in Australia, 2016; Australian Bureau of Statistics: Canberra, Australia, 2017.
- Clark, A.; Gilbert, A.; Rao, D.; Kerr, L. ‘Excuse me, do any of you ladies speak English?’ Perspectives of refugee women living in South Australia: Barriers to accessing primary health care and achieving the Quality Use of Medicines. Aust. J. Prim. Health 2014, 20, 92–97. [Google Scholar] [PubMed]
- Hadgkiss, E.J.; Renzaho, A.M. The physical health status, service utilisation and barriers to accessing care for asylum seekers residing in the community: A systematic review of the literature. Aust. Health Rev. 2014, 38, 142–159. [Google Scholar] [CrossRef] [PubMed]
- Hannah, C.T.; Le, Q. Factors affecting access to healthcare services by intermarried Filipino women in rural Tasmania: A qualitative study. Rural Remote Health 2012, 12, 1–9. [Google Scholar] [CrossRef]
- Taylor, J.; Haintz, G.L. Influence of the social determinants of health on access to healthcare services among refugees in Australia. Aust. J. Prim. Health 2018, 24, 14–28. [Google Scholar] [CrossRef]
- Mead, N.; Roland, M. Understanding why some ethnic minority patients evaluate medical care more negatively than white patients: A cross sectional analysis of a routine patient survey in English general practices. Bmj 2009, 339, b3450. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, L.M.; Jacquez, F.; Bakar, R.C. Cultural health attributions, beliefs, and practices: Effects on healthcare and medical education. Open Med. Educ. J. 2009, 2, 64–74. [Google Scholar]
- Ponsford, J.; Downing, M.; Pechlivanidis, H. The impact of cultural background on outcome following traumatic brain injury. Neuropsychol. Rehabil. 2020, 30, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Saltapidas, H.; Ponsford, J. The influence of cultural background on motivation for and participation in rehabilitation and outcome following traumatic brain injury. J. Head Trauma Rehabil. 2007, 22, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Saltapidas, H.; Ponsford, J. The influence of cultural background on experiences and beliefs about traumatic brain injury and their association with outcome. Brain Impair. 2008, 9, 1–13. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2000. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 19 December 2023).
- Costello, R.S.; Downing, M.G.; Ponsford, J. The experience of traumatic brain injury in a culturally and linguistically diverse sample in Australia. Disabil. Rehabil. 2023, 1–10. [Google Scholar] [CrossRef]
- Garduño-Ortega, O.; Li, H.; Smith, M.; Yao, L.; Wilson, J.; Zarate, A.; Bushnik, T. Assessment of the individual and compounding effects of marginalization factors on injury severity, discharge location, recovery, and employment outcomes at 1 year after traumatic brain injury. Front. Neurol. 2022, 13, 942001. [Google Scholar] [CrossRef]
- Hines, A.L.; Andrews, R.M.; Moy, E.; Barrett, M.L.; Coffey, R.M. Disparities in rates of inpatient mortality and adverse events: Race/ethnicity and language as independent contributors. Int. J. Environ. Res. Public Health 2014, 11, 13017–13034. [Google Scholar] [CrossRef]
- de la Plata, C.M.; Hewlitt, M.; de Oliveira, A.; Hudak, A.; Harper, C.; Shafi, S.; Diaz-Arrastia, R. Ethnic differences in rehabilitation placement and outcome after TBI. J. Head Trauma Rehabil. 2007, 22, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Zeidan, A.; Beshara, G.; Cortes, J.; Tibbetts, C.; Tracy, B.M.; Muralidharan, V.J.; Sola Jr, R.; Irizarry, R.H.; Williams, K. Characterizing injury patterns and outcomes in hospitalized trauma patients with non-English Language Preferences. Am. J. Surg. 2023, 225, 948–952. [Google Scholar] [CrossRef] [PubMed]
- Sander, A.M.; Ketchum, J.M.; Lequerica, A.H.; Pappadis, M.R.; Bushnik, T.; Hammond, F.M.; Sevigny, M. Primary language and participation outcomes in hispanics with traumatic brain injury: A traumatic brain injury model systems study. J. Head Trauma Rehabil. 2021, 36, E218. [Google Scholar] [CrossRef] [PubMed]
- Kinney, A.R.; Bahrani, N.H.; Brenner, L.A.; Starosta, A.J.; Mata-Greve, F.; Humbert, A.; Zheng, Z.; Prado, M.G.; Au, M.A.; Mollis, B. Intersectionality of systemic disadvantage on mortality and care following TBI. J. Head Trauma Rehabil. 2023, 38, 137–146. [Google Scholar]
- Kellezi, B.; Earthy, S.; Sleney, J.; Beckett, K.; Barnes, J.; Christie, N.; Horsley, D.; Jones, T.; Kendrick, D. What can trauma patients’ experiences and perspectives tell us about the perceived quality of trauma care? A qualitative study set within the UK National Health Service. Injury 2020, 51, 1231–1237. [Google Scholar]
- Miner, A.S.; Shah, N.; Bullock, K.D.; Bailenson, J. Key considerations for incorporating conversational AI in psychotherapy. Front. Psychiatry 2019, 10, 441761. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).