Abstract
Human beings around the globe have been suffering from a devastating novel pandemic and public health emergency, coronavirus disease 2019 (COVID-19), for more than one and a half years due to the deadly and highly pathogenic severe acute respiratory coronavirus 2 (SARS-CoV-2) infection worldwide. Notably, no effective treatment strategy has been approved for the complete recovery of COVID-19 patients, though several vaccines have been rolled out around the world upon emergency use authorization. After the emergence of the COVID-19 outbreak globally, plenty of clinical investigations commenced to screen the safety and efficacy of several previously approved drugs to be repurposed against the SARS-CoV-2 pathogen. This concise review aims at exploring the current status of the clinical efficacy and safety profile of several antiviral medications for the treatment of patients with COVID-19 and other respiratory complications caused by SARS-CoV-2 infection. The paper covers all kinds of human studies (January 2020 to June 2021) except case reports/series to highlight the clear conclusion based on the current clinical evidence. Among the promising repositioned antivirals, remdesivir has been recommended in critical conditions to mitigate the fatality rate and improve clinical conditions. In addition, boosting the immune system is believed to be beneficial in treating COVID-19 patients, so interferon type I might exert immunomodulation through its antiviral effects by stimulating interferon-stimulated gene (ISG). However, more extensive clinical studies covering all ethnic groups globally are warranted based on current data to better understand the clinical efficacy of the currently proposed repurposed drugs against COVID-19.
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) has created a lot of burden on the global medical system, public health, and economic and social life of human beings [1,2]. The causative pathogen identified for COVID-19 is called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which emerged from viruses of unknown sources [3,4]. SARS-CoV-2 is a type of ß-coronavirus (β-CoV) that belongs to the coronavirus group. The human coronavirus group causes several outbreaks, including the severe acute respiratory syndrome (SARS-CoV) epidemic from 2002 to 2004 and the Middle East respiratory syndrome (MERS-CoV) outbreak in the Middle East, Africa, and South Asia, and many more countries during 2012 [5,6]. Wuhan, China, was the first city for the occurrence of COVID-19, and after that, it spread all over the world, infecting around 218 million people together with over 4.5 million total deaths, according to the COVID-19 global case dashboard of the World Health Organization (WHO), by 29 August 2021 [7]. Based on the data from January 2020, the WHO declared COVID-19 a Public Health Emergency of International Concern (PHEIC), which was followed by a pandemic on 11 March 2020 [8].
In the meantime, many vaccines have received emergency use authorization, and by 30 August 2021, 5.24 billion doses had been administered globally. Around 40% of the world population has received at least one dose of the COVID-19 vaccine. It is notable that approximately 39 million people are taking the COVID-19 vaccine per day. However, only 1.6% of people from low-income countries have received at least one dose of the vaccine to be inoculated [9]. In addition, the production and equitable distribution of a large number of vaccine doses is challenging for world leaders to achieve within a short time. Another concern is that political and financial matters might be a significant barrier to administering the vaccines to the entire world population for all ethnic and socioeconomic groups. The development and production of the vaccines within a very narrow time frame might have implied insufficient evidence for the safety and efficacy of the vaccines in the long term [10]. Therefore, the world community must develop new effective and safe antiviral drugs or therapeutics to fight against COVID-19.
To date, no effective and approved antiviral treatment is available to fight against COVID-19. However, some recommendations are being practiced concurrently to manage individual patients’ needs, such as antipyretic drugs for fever, oxygen therapy for respiratory distresses, antimicrobial therapy with mechanical ventilation applied in some severe cases depending on the clinical condition of the patient, and so on [11,12]. Meanwhile, the drug repurposing strategy is being continuously used in COVID-19 treatment. Drug repurposing or drug repositioning is tactically a rapid process to identify new pharmacological indications rather than the original purpose of investigational, existing, already marketed or FDA-approved drugs for the treatment of diseases. This advantageous method provides a great benefit in circumventing some de novo drug design and development stages. Thus, the technique decreases scheduled periods of drug development, reduces failure risk, and protects funds from being wasted [13]. In addition, it is crucial for a drug to be effective, proportionally related to clinical efficacy, or to produce desired pharmacological activities for a specified indication in humans. A potential drug must be passed through efficacy trials to fulfill the principal requirements of clinical efficacy, including several human trial phases [14]. In other words, efficacy trials determine the possibility of an intervention to produce expected results under ideal circumstances or the degree of beneficial effects under real-world clinical settings [15,16].
More importantly, SARS-CoV-2 is the seventh member of the genus β-coronavirus and the Coronavirdiae family [17]. Genome sequencing of SARS-CoV-2 demonstrated that the virus is almost 79% and 50% identical with the previous two SARS-CoV and MERS coronaviruses, respectively [18]. So, it might be very convenient and rational to repurpose the currently available antiviral drugs used against the two previous viral pandemics (SARS and MERS CoV) or have evidence of previous experience. Furthermore, it has been perceived that drug repurposing has already become a “universal strategy” to face the challenges of the COVID-19 pandemic because of several advantages it offers. These include fewer clinical trial steps, the availability of the formulation and distribution of the existing pharmaceutical supply, the possibility of more effective treatment of known combination therapy, the discovery of novel mechanisms of actions of old drugs or new classes of medicines, [19] and the elimination of “activation barriers” in the early stages of research, thus ensuring the rapid advancement of any project to disease-oriented research [20].
Several FDA-approved available antiviral drugs, alone or in combination, have been screened clinically for their extended use since the early phase of the current pandemic to find a safe and effective treatment option against COVID-19 [21,22], and many clinical trials of these antiviral drugs are still ongoing. However, an in-depth understanding is required from current clinical literature reports to execute integrated approaches between computational and experimental methods to guarantee high success rates of repositioned drugs. Moreover, multiple challenges associated with repurposed drugs have been identified, including dose adjustments, route of administration, acute/chronic toxicity, appropriate delivery systems, etc. [23,24]. Although many preliminary studies exhibited promising results, several extensive clinical investigations reported contradictory findings with significant adverse effects of these elongated applications of antiviral drugs. However, numerous clinical trials conducted with larger samples/patients have recently disclosed many mixed results, which needs careful study. Therefore, it is essential to review comprehensively the uses of repurposed drugs focusing on the therapeutic strategies, advantages, adverse drug reactions, and respective delivery approaches for instigating an instrumental battle against COVID-19. Likewise, it is also necessary to know the clear disease pathology and critical strategies to identify new drugs capable of protecting against highly contagious viral infections, including the SARS-CoV-2 infection [25]. This article summarizes the current understanding of clinical efficacy and the adverse drug reaction of various antiviral drugs used for SARS-CoV-2-infected patients across the world. Here, we also illustrated Figure 1 to represent the chemical structures of the seven repurposed antivirals drugs for use against COVID-19.
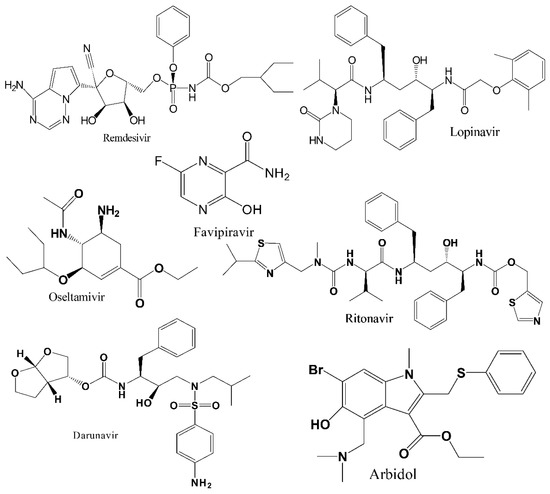
Figure 1.
Chemical structures of the selected most promising antiviral drugs against COVID-19.
2. Methods
Search and Data Collection
The scientific articles published from January 2020 to June 2021 on several repurposed antiviral drugs that had potentiality against COVID-19 were downloaded from various databases such as Google Scholar, Semantic Scholar, PubMed, Scopus, Europe PMC, ScienceDirect Journals, SpringerLink, Wiley, Taylor & Francis, and so on, with several preprint servers. We utilized several suitable keywords and used those words individually or in combination to find the data regarding the target topic. The keywords included “COVID-19”, “coronavirus diseases 2019”, “SARS-CoV-2”, “clinical trials”, “observational study”, “cohort study”, “safety and efficacy”, “remdesivir”, “favipiravir”, “lopinavir/ritonavir”, “interferons”, “arbidol”, “umifenovir”, “oseltamivir”, “darunavir”, and so on. We included the human studies designed as randomized or non-randomized, open-label, controlled clinical trials, and observational or cohort studies to find a clear understanding of the safety and efficacy of repurposed antiviral drugs against mild, moderate, and severe cases of COVID-19. However, we excluded case reports or case series in this review paper. In addition, the current review rejected the data containing a limited number of subjects, weak statistical analysis, or vague conclusions.
4. Discussion and Concluding Remarks
The new emergence of such a deadly virus needs potential agents to control it. It can be noted that mass vaccination is not easily affordable in many developing and underdeveloped countries immediately or before 2024 [141]. Additionally, over-populated countries might face some critical situations to ensure vaccines for all people due to vaccine insufficiency, and it might take longer to eradicate the outbreak. Moreover, the delta variant of concern has shown to be several times more resistant against vaccine-induced immunity [142]. This crucial situation calls for effective treatment tools/antiviral agents to fight against the deadly infectious disease. This review mainly focuses on the efficiency and adverse effects of repurposing antiviral drugs potentially used to treat COVID-19.
Various drugs are being used as repurposing drugs, as there is no drug or effective treatment strategy against COVID-19. Therefore, the most promising seven antiviral drugs were taken under consideration to evaluate their efficacy and also their adverse effects in various levels of COVID-19 patients.
The very first drug and most widely used one was RDV. Though several studies mentioned above showed reduced mortality, shorter hospital stay, and better improvement of symptoms, several studies have been reported it to be insignificant in the case of COVID-19 patients’ recovery. Notably, the Macaque experiment stated that RDV was only efficient in viral clearance from the lower respiratory tract, not the upper one [143]. Another randomized controlled study conducted by Wang et al. [37] suggested no efficacy of RDV on the respiratory tract, neither upper nor lower. We can conclude by evaluating the above data that RDV might be effective for severe patients in mitigating the fatality rate and improvement of clinical conditions. The WHO has recommended RDV against in non-severe patients, which might match with the current findings.
FPV has shown great efficacy in this crucial situation, yet it is not patient-friendly due to its high dose. The studies discussed above revealed that FPV is a potential cure for COVID-19, both in severe and mild cases. Chen et al. [44] reported a positive effect of FPV compared to ARB, as the former showed better improvement of symptoms like cough, pyrexia, and difficulty breathing. The drug is beneficial in alleviating symptoms, reducing viral load and hospital stay, but still, it is considered risky due to severe side effects like teratogenicity and embryotoxicity [144]. This drug was very effective against H1N1 virus, which is also an RNA virus and has shown potential antiviral effects, perhaps most efficient in viral clearance. There has been no toxicity detected for its huge loading dose, but some adverse effects have been reported; cardiovascular complications, nausea, vomiting, diarrhea, and kidney injuries are the common ones. Several studies also compared the efficacy among FPV, hydroxychloroquine, chloroquine, and IFN, which had minimal significant difference. LPV/RTV combination was also a drug of choice for COVID-19 in the early stages of the pandemic. However, this combination proved to be insignificant in most of the cases studied, with some exceptions. The combination rather became the reason behind serious complications like diarrhea, gastrointestinal disturbance, electrolyte imbalance, and severe acute kidney injury in patients with both severe and mild COVID-19.
INF therapy is one of the promising treatments for COVID-19 now. Several subcategories of INF are known, such as IFN-alpha 1a, IFN-alpha 1b, IFN-beta 1a, IFN-beta 1b, IFN-gamma, and IFN-lambda. All have shown a variety of efficacy without severe side effects. They have worked to the betterment of patients’ condition and reduced the fatality rate among severe patients. Several studies were also carried out to evaluate and compare the potentials of these variants. Recombinant IFN has proven to be more potent than traditional ones. An efficient therapy known as triple therapy is a combination of IFN/LPV/r/RBV that has shown amazing results. Type I interferons (IFN-I, IFN-α, and IFN-ß) are immunomodulatory drugs that can induce antiviral effects and may induce pro-inflammatory activity, which has turned out to be beneficial for early treatment of COVID-19 [145]. Combination with other antiviral agents may mitigate the adverse effects as well as improve the clinical condition of the patients.
ARB has shown noteworthy effects in alleviating symptoms of COVID-19 and shortening the time for converting the PCR result from positive to negative. The potential antiviral agent works well both alone and in combination with various other agents like HCQ, RBV, and IFN. Antibiotic therapy alongside ARB is just the icing on the cake, showing prompt activity in quick recovery and reduction of fatality rate. It has proved to be more efficacious than other drugs like LPV/RTV and HCQ. All these have made it a potential agent in this pandemic situation. We can add oseltamivir to this list, but the drug showed great positive effects in severe patients when used early. Darunavir is emerging as a potent antiviral drug by lowering the mortality rate and hospital stay, but more studies are required to extensively verify its safety profile.
HCQ, LPV/RTV, and many other drugs, which were thought to be a treatment option earlier, are already banned by the WHO. FPV, ARB, and oseltamivir are in the pool of acceptable drugs for COVID-19, but there are still many randomized trials going on to assess their safety profiles. RDV is recommended in severe conditions considering its adverse effects that require limited use of the drug. Boosting the immune system is believed to be beneficial, so IFN type I might exert immunomodulation through its antiviral effects by stimulating interferon-stimulated gene (ISG).
As patients with COVID-19 might face multiple pathological dysfunctions, they must be prescribed multi-drug therapies [146]. Moreover, several pieces of evidence have demonstrated that combination therapy is superior to monotherapy, as the multiple drugs might heal by acting on multiple receptors [147]. Particularly, combination therapy in COVID-19 has become an excellent choice to wrestle against the disease. Several diagnoses revealed that secondary infections have become of paramount importance as an after-effect of COVID-19, and have some saddening consequences. A combination of potential antivirals with antibiotics is used to fight the secondary infections produced due to lessened immunity, along with the viral infection [148]. Interferon uses an immunomodulator that has served well for COVID-19, and its combination with antiviral agents gives the best results. Moreover, the combination lowers the time taken to reduce viral shedding significantly [149]. The mechanism could be the dual action of antivirals and immunomodulatory agents; one weakens the virus, and the latter strengthens the immunity so the body can recover faster, through confirmation or justification of this mechanism is yet to be provided. However, to define the exact mechanism and efficacy profile of the stated combinations in the current review, more precise investigation with larger data and evidence might be required.
Author Contributions
Conceptualization, M.J.H.; methodology, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; software, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; validation, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; formal analysis, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; investigation, M.J.H. and T.B.E.; resources, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; data curation, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; writing—original draft preparation, M.J.H., T.J., S.R.B., U.R. and S.M.; writing—review and editing, M.J.H., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; visualization, M.J.H., T.J., S.R.B., U.R., S.M., M.O.R., M.R.I., M.L.N., M.A.I. and T.B.E.; supervision, M.J.H. and T.B.E.; project administration, M.J.H. and T.B.E.; funding acquisition, T.B.E. All authors have read and agreed to the published version of the manuscript.
Funding
This work was conducted with the individual funding of all authors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Available data are presented in the manuscript and reference list.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Abbreviations
| RDV | remdesivir |
| FPV | favipiravir |
| LPV-RTV | lopinavir-ritonavir |
| INF | interferon |
| rhIFN-α | recombinant human interferon alpha |
| rSIFN | recombinant super compound interferon |
| TFF2 | trefoil factor 2 |
| ARB | arbidol |
| DRV | darunavir |
| DRV/c | darunavir/cobicisitat |
| HCQ | hydroxychloroquine |
| CQ | chloroquine |
| RCT | randomized controlled trial |
| LHQW | Lianhuaqingwen |
| LQ | Lianhua Qingwen |
| CP | convalescent plasma |
| BCN | baricitinib |
| RBV | ribavirin |
| SFV/DCV | sofosbuvir/daclatasvir |
| N | number |
| T | treatment (group) |
| C | control (group) |
| SOC | standard of care |
| CT | computed tomography |
| IV | intravenous |
| NA | not available |
| SC | subcutaneous |
| GI | gastrointestinal |
| 95% CI | 95% confidence interval |
| HR | hazard ratio |
| OR | odds ratio |
| RR | relative risk |
| ROA | route of administration |
| ADR | adverse drug reaction |
| ADRS | acute respiratory distress syndrome |
| ALT | alanine aminotransferase |
| RdRp | RNA-dependent RNA polymerase |
| IQR | interquartile range |
| PCR | polymerase chain reaction |
| ECG | electrocardiogram |
References
- Ashraf, B.N. Economic impact of government interventions during the COVID-19 pandemic: International evidence from financial markets. J. Behav. Exp. Financ. 2020, 27, 100371. [Google Scholar] [CrossRef]
- Hossain, M.J.; Ahmmed, F.; Rahman, S.; Sanam, S.; Emran, T.B.; Mitra, S. Impact of online education on fear of academic delay and psychological distress among university students following one year of COVID-19 outbreak in Bangladesh. Heliyon 2021, 7, e07388. [Google Scholar] [CrossRef]
- Gollakner, R.; Capua, I. Is COVID-19 the first pandemic that evolves into a panzootic? Vet. Ital. 2020, 56, 11–12. [Google Scholar] [CrossRef]
- Yoo, H.S.; Yoo, D. COVID-19 and veterinarians for one health, zoonotic- and reverse-zoonotic transmissions. J. Vet. Sci. 2020, 21, e51. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Singhai, M.; Garg, S.; Shah, D.; Sood, V.; Singh, S.K. The missing pieces in the jigsaw and need for cohesive research amidst coronavirus infectious disease 2019 global response. Med. J. Armed Forces India 2020, 76, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Decaro, N.; Lorusso, A. Novel human coronavirus (SARS-CoV-2): A lesson from animal coronaviruses. Vet. Microbiol. 2020, 244, 108693. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Weekly Operational Update on COVID-19—20 July 2021; World Health Organization: Geneva, Switzerland, 2021; pp. 1–13. [Google Scholar]
- Hossain, M.J.; Kuddus, M.R.; Rahman, S.M.A. Knowledge, attitudes, and behavioral responses toward COVID-19 during early phase in bangladesh: A questionnaire-based study. Asia Pac. J. Public Health 2021, 33, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Statistics and Research. Coronavirus Disease 2019 (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 30 August 2021).
- Forni, G.; Mantovani, A.; COVID-19 Commission of Accademia Nazionale dei Lincei, Rome. COVID-19 vaccines: Where we stand and challenges ahead. Cell Death Differ. 2021, 28, 626–639. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). Available online: https://stacks.cdc.gov/view/cdc/88624 (accessed on 30 August 2021).
- Hossain, M.J. Is Bangladesh moving toward herd immunity? Current COVID-19 perspective. Bangladesh J. Infect. Dis. 2020, 7 (Suppl. S2), S63–S66. [Google Scholar] [CrossRef]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2019, 18, 41–58. [Google Scholar] [CrossRef]
- Hossain, M.J.; Kuddus, M.R.; Rashid, M.A.; Sultan, M.Z. Understanding and dealing the SARS-CoV-2 infection: An updated concise review. Bangladesh Pharm. J. 2021, 24, 61–75. [Google Scholar] [CrossRef]
- Godwin, M.; Ruhland, L.; Casson, I.; MacDonald, S.; Delva, D.; Birtwhistle, R.; Lam, M.; Seguin, R. Pragmatic controlled clinical trials in primary care: The struggle between external and internal validity. BMC Med. Res. Methodol. 2003, 3, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viveiros Rosa, S.G.; Santos, W.C. Clinical trials on drug repositioning for COVID-19 treatment. Rev. Panam. Salud Publica Pan Am. J. Public Health 2020, 44, e40. [Google Scholar] [CrossRef]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Oprea, T.I.; Bauman, J.E.; Bologa, C.G.; Buranda, T.; Chigaev, A.; Edwards, B.S.; Jarvik, J.W.; Gresham, H.D.; Haynes, M.K.; Hjelle, B.; et al. Drug repurposing from an academic perspective. Drug Discov. Today Ther. Strateg. 2011, 8, 61–69. [Google Scholar] [CrossRef] [Green Version]
- Senanayake, S.L. Drug repurposing strategies for COVID-19. Future Drug Discov. 2020, 2, FDD40. [Google Scholar] [CrossRef]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.-T.; Marimuthu, K.; Ang, L.W.; Mak, T.M.; et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA 2020, 323, 1488–1494. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Parvathaneni, V.; Gupta, V. Utilizing drug repurposing against COVID-19—Efficacy, limitations, and challenges. Life Sci. 2020, 259, 118275. [Google Scholar] [CrossRef]
- Marra, F.; Smolders, E.J.; El-Sherif, O.; Boyle, A.; Davidson, K.; Sommerville, A.J.; Marzolini, C.; Siccardi, M.; Burger, D.; Gibbons, S.; et al. Recommendations for Dosing of Repurposed COVID-19 Medications in Patients with Renal and Hepatic Impairment. Drugs R&D 2021, 21, 9–27. [Google Scholar] [CrossRef]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, F.; Tang, J.; Nussinov, R.; Cheng, F. Artificial intelligence in COVID-19 drug repurposing. Lancet Digit. Health 2020, 2, e667–e676. [Google Scholar] [CrossRef]
- Sheahan, T.P.; Sims, A.C.; Leist, S.R.; Schäfer, A.; Won, J.; Brown, A.J.; Montgomery, S.A.; Hogg, A.; Babusis, D.; Clarke, M.O.; et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat. Commun. 2020, 11, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of Covid-19—Final Report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef]
- Grein, J.; Ohmagari, N.; Shin, D.; Diaz, G.; Asperges, E.; Castagna, A.; Feldt, T.; Green, G.; Green, M.L.; Lescure, F.-X.; et al. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N. Engl. J. Med. 2020, 382, 2327–2336. [Google Scholar] [CrossRef]
- Antinori, S.; Cossu, M.V.; Ridolfo, A.L.; Rech, R.; Bonazzetti, C.; Pagani, G.; Gubertini, G.; Coen, M.; Magni, C.; Castelli, A.; et al. Compassionate remdesivir treatment of severe Covid-19 pneumonia in intensive care unit (ICU) and Non-ICU patients: Clinical outcome and differences in post-treatment hospitalisation status. Pharmacol. Res. 2020, 158, 104899. [Google Scholar] [CrossRef]
- Pasquini, Z.; Montalti, R.; Temperoni, C.; Canovari, B.; Mancini, M.; Tempesta, M.; Pimpini, D.; Zallocco, N.; Barchiesi, F. Effectiveness of remdesivir in patients with COVID-19 under mechanical ventilation in an Italian ICU. J. Antimicrob. Chemother. 2020, 75, 3359–3365. [Google Scholar] [CrossRef] [PubMed]
- Aiswarya, D.; Arumugam, V.; Dineshkumar, T.; Gopalakrishnan, N.; Lamech, T.M.; Nithya, G.; Sastry, B.V.R.H.; Vathsalyan, P.; Dhanapriya, J.; Sakthirajan, R. Use of Remdesivir in Patients With COVID-19 on Hemodialysis: A Study of Safety and Tolerance. Kidney Int. Rep. 2021, 6, 586–593. [Google Scholar] [CrossRef]
- Olender, S.A.; Perez, K.K.; Go, A.S.; Balani, B.; Price-Haywood, E.G.; Shah, N.S.; Wang, S.; Walunas, T.L.; Swaminathan, S.; Slim, J.; et al. Remdesivir for Severe Coronavirus Disease 2019 (COVID-19) Versus a Cohort Receiving Standard of Care. Clin. Infect. Dis. 2020, ciaa1041. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.D.; Lye, D.C.B.; Hui, D.S.; Marks, K.M.; Bruno, R.; Montejano, R.; Spinner, C.D.; Galli, M.; Ahn, M.-Y.; Nahass, R.G.; et al. Remdesivir for 5 or 10 Days in Patients with Severe Covid-19. N. Engl. J. Med. 2020, 383, 1827–1837. [Google Scholar] [CrossRef]
- Garibaldi, B.T.; Wang, K.; Robinson, M.L.; Zeger, S.L.; Roche, K.B.; Wang, M.-C.; Alexander, G.C.; Gupta, A.; Bollinger, R.; Xu, Y. Effectiveness of remdesivir with and without dexamethasone in hospitalized patients with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Tsuzuki, S.; Hayakawa, K.; Matsunaga, N.; Terada, M.; Suzuki, S.; Ohtsu, H.; Asai, Y.; Kitajima, K.; Saito, S.; Uemura, Y.; et al. Efficacy of remdesivir in Japanese patients hospitalised with COVID-19: A large observational study using the COVID-19 Registry Japan. medRxiv 2021. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, D.; Du, G.; Du, R.; Zhao, J.; Jin, Y.; Fu, S.; Gao, L.; Cheng, Z.; Lu, Q.; et al. Remdesivir in adults with severe COVID-19: A randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2020, 395, 1569–1578. [Google Scholar] [CrossRef]
- Spinner, C.D.; Gottlieb, R.L.; Criner, G.J.; López, J.R.A.; Cattelan, A.M.; Viladomiu, A.S.; Ogbuagu, O.; Malhotra, P.; Mullane, K.M.; Castagna, A.; et al. Effect of Remdesivir vs. Standard Care on Clinical Status at 11 Days in Patients With Moderate COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 1048–1057. [Google Scholar] [CrossRef]
- Kalil, A.C.; Patterson, T.F.; Mehta, A.K.; Tomashek, K.M.; Wolfe, C.R.; Ghazaryan, V.; Marconi, V.C.; Ruiz-Palacios, G.M.; Hsieh, L.; Kline, S.; et al. Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N. Engl. J. Med. 2020, 384, 795–807. [Google Scholar] [CrossRef]
- Falcão, F.; Viegas, E.; Carmo, I.; Soares, J.; Falcao, M.; Solano, M.; Cavaco, P.; Mendes, D.; Rijo, J.; Povoa, P.; et al. A prospective, observational study to evaluate adverse drug reactions in patients with COVID-19 treated with remdesivir or hydroxychloroquine: A preliminary report. Eur. J. Hosp. Pharm. 2021, 28, 248–253. [Google Scholar] [CrossRef]
- Goldberg, E.; Zvi, H.B.; Sheena, L.; Sofer, S.; Krause, I.; Sklan, E.H.; Shlomai, A. A real-life setting evaluation of the effect of remdesivir on viral load in COVID-19 patients admitted to a large tertiary centre in Israel. Clin. Microbiol. Infect. 2021, 27, 917.e1–917.e4. [Google Scholar] [CrossRef]
- Padilla, R.; Arquiette, J.; Mai, Y.; Singh, G.; Galang, K.; Liang, E. Clinical Outcomes of COVID-19 Patients Treated with Convalescent Plasma or Remdesivir Alone and in Combination at a Community Hospital in California’s Central Valley. J. Pharm. Pharm. Sci. 2021, 24, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Yang, M.; Liu, D.; Chen, J.; Shu, D.; Xia, J.; Liao, X.; Gu, Y.; Cai, Q.; Yang, Y.; et al. Experimental Treatment with FPVipiravir for COVID-19: An Open-Label Control Study. Engineering 2020, 6, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhang, Y.; Huang, J.; Yin, P.; Cheng, Z.; Wu, J.; Chen, S.; Zhang, Y.; Chen, B.; Lu, M.; et al. Favipiravir versus Arbidol for COVID-19: A Randomized Clinical Trial. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Lou, Y.; Liu, L.; Yao, H.; Hu, X.; Su, J.; Xu, K.; Luo, R.; Yang, X.; He, L.; Lu, X.; et al. Clinical Outcomes and Plasma Concentrations of Baloxavir Marboxil and FPVipiravir in COVID-19 Patients: An Exploratory Randomized, Controlled Trial. Eur. J. Pharm. Sci. 2021, 157, 105631. [Google Scholar] [CrossRef]
- The Indian Express. COVID-19: Glenmark’s FPVipiravir Shows Encouraging Results in Phase 3 Clinical Trial. Available online: https://www.newindianexpress.com/nation/2020/jul/23/covid-19-glenmarks-FPVipiravir-shows-encouraging-results-in-phase-3-clinical-trial-2173500.html (accessed on 14 July 2021).
- The Daily Star. Covid-19 Patients: Favipiravir Effective in Dhaka Trial. Available online: https://www.thedailystar.net/backpage/news/covid-19-patients-FPVipiravir-effective-dhaka-trial-1927321 (accessed on 14 July 2021).
- Ucan, A.; Cerci, P.; Efe, S.; Akgun, H.; Ozmen, A.; Yagmuroglu, A.; Bilgin, M.; Avci, D. Benefits of treatment with Favipiravir in hospitalized patients for COVID-19: A retrospective observational case–control study. Virol. J. 2021, 18, 102. [Google Scholar] [CrossRef] [PubMed]
- Alamer, A.; Alrashed, A.A.; Alfaifi, M.; Alosaimi, B.; AlHassar, F.; Almutairi, M.; Howaidi, J.; Almutairi, W.; Mohzari, Y.; Sulaiman, T.; et al. Effectiveness and safety of Favipiravir compared to supportive care in moderately to critically ill COVID-19 patients: A retrospective study with propensity score matching sensitivity analysis. Curr. Med. Res. Opin. 2021, 37, 1085–1097. [Google Scholar] [CrossRef]
- Zhao, H.; Zhang, C.; Zhu, Q.; Chen, X.; Chen, G.; Sun, W.; Xiao, Z.; Du, W.; Yao, J.; Li, G.; et al. Favipiravir in the treatment of patients with SARS-CoV-2 RNA recurrent positive after discharge: A multicenter, open-label, randomized trial. Int. Immunopharmacol. 2021, 97, 107702. [Google Scholar] [CrossRef]
- Udwadia, Z.F.; Singh, P.; Barkate, H.; Patil, S.; Rangwala, S.; Pendse, A.; Kadam, J.; Wu, W.; Caracta, C.F.; Tandon, M. Efficacy and safety of Favipiravir, an oral RNA-dependent RNA polymerase inhibitor, in mild-to-moderate COVID-19: A randomized, comparative, open-label, multicenter, phase 3 clinical trial. Int. J. Infect. Dis. 2021, 103, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Meng, Z.; Wang, T.; Chen, L.; Chen, X.; Li, L.; Qin, X.; Li, H.; Luo, J. The Effect of Recombinant Human Interferon Alpha Nasal Drops to Prevent COVID-19 Pneumonia for Medical Staff in an Epidemic Area. Curr. Top. Med. Chem. 2021, 21, 920–927. [Google Scholar] [CrossRef]
- Pandit, A.; Bhalani, N.; Bhushan, B.L.S.; Koradia, P.; Gargiya, S.; Bhomia, V.; Kansagra, K. Efficacy and safety of pegylated interferon alfa-2b in moderate COVID-19: A phase II, randomized, controlled, open-label study. Int. J. Infect. Dis. 2021, 105, 516–521. [Google Scholar] [CrossRef]
- Yu, J.; Lu, X.; Tong, L.; Shi, X.; Ma, J.; Lv, F.; Wu, J.; Pan, Q.; Yang, J.; Cao, H.; et al. Interferon-α-2b aerosol inhalation is associated with improved clinical outcomes in patients with coronavirus disease-2019. Br. J. Clin. Pharmacol. 2021, 2021, 1–10. [Google Scholar] [CrossRef]
- Feld, J.J.; Kandel, C.; Biondi, M.J.; Kozak, R.A.; Zahoor, M.A.; Lemieux, C.; Borgia, S.M.; Boggild, A.K.; Powis, J.; McCready, J.; et al. Peginterferon lambda for the treatment of outpatients with COVID-19: A phase 2, placebo-controlled randomised trial. Lancet Respir. Med. 2021, 9, 498–510. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, B.; Li, Q.; Wen, L.; Zhang, R. Clinical Features of 69 Cases With Coronavirus Disease 2019 in Wuhan, China. Clin. Infect. Dis. 2020, 71, 769–777. [Google Scholar] [CrossRef] [Green Version]
- Lian, N.; Xie, H.; Lin, S.; Huang, J.; Zhao, J.; Lin, Q. Umifenovir treatment is not associated with improved outcomes in patients with coronavirus disease 2019: A retrospective study. Clin. Microbiol. Infect. 2020, 26, 917–921. [Google Scholar] [CrossRef]
- Zhu, Z.; Lu, Z.; Xu, T.; Chen, C.; Yang, G.; Zha, T.; Lu, J.; Xue, Y. Arbidol monotherapy is superior to lopinavir/ritonavir in treating COVID-19. J. Infect. 2020, 81, e21–e23. [Google Scholar] [CrossRef]
- Chen, W.; Yao, M.; Fang, Z.; Lv, X.; Deng, M.; Wu, Z. A study on clinical effect of Arbidol combined with adjuvant therapy on COVID-19. J. Med. Virol. 2020, 92, 2702–2708. [Google Scholar] [CrossRef]
- Liu, Q.; Fang, X.; Tian, L.; Vankadari, N.; Chen, X.; Wang, K.; Li, D.; Dai, X.; Xu, F.; Shen, L.; et al. Arbidol treatment with reduced mortality of adult patients with COVID-19 in Wuhan, China: A retrospective cohort study. medRxiv 2021. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.; Ke, C.; Yue, D.; Li, W.; Hu, Z.; Liu, W.; Hu, S.; Wang, S.; Liu, J. Effectiveness of Arbidol for COVID-19 Prevention in Health Professionals. Front. Public Health 2020, 8, 249. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; He, X.; Liu, W.; Kan, J.; He, L.; Zhao, J.; Chen, C.; Zhang, J.; Chen, S. Antiviral Abidol is Associated with the Reduction of In-Hospital Mortality in COVID-19 Patients. Cardiol. Discov. 2021, 1, 37–43. [Google Scholar]
- Tan, J.; Yuan, Y.; Xu, C.; Song, C.; Liu, D.; Ma, D.; Gao, Q. A retrospective comparison of drugs against COVID-19. Virus Res. 2021, 294, 198262. [Google Scholar] [CrossRef]
- Moreno, G.; Rodríguez, A.; Sole-Violán, J.; Martín-Loeches, I.; Díaz, E.; Bodí, M.; Reyes, L.F.; Gómez, J.; Guardiola, J.; Trefler, S.; et al. Early oseltamivir treatment improves survival in critically ill patients with influenza pneumonia. ERJ Open Res. 2021, 7, 00888–2020. [Google Scholar] [CrossRef]
- Deng, L.; Xiong, Y.; Chen, T.; Zhang, Y.; Luo, M.; Gao, S.; Mo, P.; Hospital, Z.; Song, S.; Hospital Zhiyong, Z.; et al. Role of Darunavir/cobicisitat in the Treatment of COVID-19: Initial Virological and Clinical Findings. Res. Sq. 2021, 2021, 1–23. [Google Scholar] [CrossRef]
- Kim, E.J.; Choi, S.H.; Park, J.S.; Kwon, Y.S.; Lee, J.; Kim, Y.; Lee, S.Y.; Choi, E.Y. Use of Darunavir-Cobicistat as a Treatment Option for Critically Ill Patients with SARS-CoV-2 Infection. Yonsei Med. J. 2020, 61, 826–830. [Google Scholar] [CrossRef]
- Chen, J.; Xia, L.; Liu, L.; Xu, Q.; Ling, Y.; Huang, D.; Huang, W.; Song, S.; Xu, S.; Shen, Y.; et al. Antiviral Activity and Safety of Darunavir/Cobicistat for the Treatment of COVID-19. Open Forum Infect. Dis. 2020, 7, ofaa241. [Google Scholar] [CrossRef]
- Guner, R.; Hasanoglu, I.; Kayaaslan, B.; Aypak, A.; Akinci, E.; Bodur, H.; Eser, F.; Kaya Kalem, A.; Kucuksahin, O.; Ates, I.; et al. Comparing ICU admission rates of mild/moderate COVID-19 patients treated with hydroxychloroquine, FPVipiravir, and hydroxychloroquine plus FPVipiravir. J. Infect. Public Health 2021, 14, 365–370. [Google Scholar] [CrossRef]
- Dabbous, H.M.; Abd-Elsalam, S.; El-Sayed, M.H.; Sherief, A.F.; Ebeid, F.F.S.; El Ghafar, M.S.A.; Soliman, S.; Elbahnasawy, M.; Badawi, R.; Tageldin, M.A. Efficacy of Favipiravir in COVID-19 treatment: A multi-center randomized study. Arch. Virol. 2021, 166, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Kocayiğit, H.; Süner, K.Ö.; Tomak, Y.; Demir, G.; Yaylacı, S.; Dheir, H.; Güçlü, E.; Erdem, A.F. Observational study of the effects of FPVipiravir vs. Lopinavir/Ritonavir on clinical outcomes in critically Ill patients with COVID-19. J. Clin. Pharm. Ther. 2021, 46, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Dabbous, H.M.; El-Sayed, M.H.; El Assal, G.; Elghazaly, H.; Ebeid, F.F.S.; Sherief, A.F.; Elgaafary, M.; Fawzy, E.; Hassany, S.M.; Riad, A.R.; et al. Safety and efficacy of Favipiravir versus hydroxychloroquine in management of COVID-19: A randomised controlled trial. Sci. Rep. 2021, 11, 7282. [Google Scholar] [CrossRef]
- Khamis, F.; Al Naabi, H.; Al Lawati, A.; Ambusaidi, Z.; Al Sharji, M.; Al Barwani, U.; Pandak, N.; Al Balushi, Z.; Al Bahrani, M.; Al Salmi, I.; et al. Randomized controlled open label trial on the use of FPVipiravir combined with inhaled interferon beta-1b in hospitalized patients with moderate to severe COVID-19 pneumonia. Int. J. Infect. Dis. 2021, 102, 538–543. [Google Scholar] [CrossRef]
- Kim, J.-W.; Kim, E.J.; Kwon, H.H.; Jung, C.Y.; Kim, K.C.; Choe, J.-Y.; Hong, H.-L. Lopinavir-ritonavir versus hydroxychloroquine for viral clearance and clinical improvement in patients with mild to moderate coronavirus disease 2019. Korean J. Intern. Med. 2020, 36, S253–S263. [Google Scholar] [CrossRef]
- Lee, J.E.; Lee, S.O.; Heo, J.; Kim, D.W.; Park, M.R.; Son, H.; Kim, D.; Kim, K.-H.; Lee, S.; Lee, S.H. Comparative outcomes of lopinavir/ritonavir and hydroxychloroquine for the treatment of coronavirus disease 2019 with mild to moderate severity. Res. Sq. 2020, 2020, 1–20. [Google Scholar] [CrossRef]
- Yu, C.; Zhang, Z.; Guo, Y.; Shi, J.; Pei, G.; Yao, Y.; Liao, W.; Zeng, R. Lopinavir/ritonavir is associated with pneumonia resolution in COVID-19 patients with influenza coinfection: A retrospective matched-pair cohort study. J. Med. Virol. 2021, 93, 472–480. [Google Scholar] [CrossRef]
- Lecronier, M.; Beurton, A.; Burrel, S.; Haudebourg, L.; Deleris, R.; Le Marec, J.; Virolle, S.; Nemlaghi, S.; Bureau, C.; Mora, P.; et al. Comparison of hydroxychloroquine, lopinavir/ritonavir, and standard of care in critically ill patients with SARS-CoV-2 pneumonia: An opportunistic retrospective analysis. Crit. Care 2020, 24, 1–9. [Google Scholar] [CrossRef]
- Lan, X.; Shao, C.; Zeng, X.; Wu, Z.; Xu, Y. Lopinavir-ritonavir alone or combined with arbidol in the treatment of 73 hospitalized patients with COVID-19: A pilot retrospective study. Int. J. Clin. Pharmacol. Ther. 2021, 59, 378–385. [Google Scholar] [CrossRef]
- Gao, G.; Wang, A.; Wang, S.; Qian, F.; Chen, M.; Yu, F.; Zhang, J.; Wang, X.; Ma, X.; Zhao, T.; et al. Brief Report: Retrospective Evaluation on the Efficacy of Lopinavir/Ritonavir and Chloroquine to Treat Nonsevere COVID-19 Patients. J. Acquir. Immune Defic. Syndr. 2020, 85, 239–243. [Google Scholar] [CrossRef]
- Karolyi, M.; Pawelka, E.; Mader, T.; Omid, S.; Kelani, H.; Ely, S.; Jilma, B.; Baumgartner, S.; Laferl, H.; Ott, C.; et al. Hydroxychloroquine versus lopinavir/ritonavir in severe COVID-19 patients: Results from a real-life patient cohort. Wien. Klin. Wochenschr. 2020, 133, 284–291. [Google Scholar] [CrossRef]
- Shi, N.; Guo, L.; Liu, B.; Bian, Y.; Chen, R.; Chen, S.; Chen, Y.; Chen, Y.; Cong, X.; Dong, G.; et al. Efficacy and safety of Chinese herbal medicine versus Lopinavir-Ritonavir in adult patients with coronavirus disease 2019: A non-randomized controlled trial. Phytomedicine 2021, 81, 153367. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Wang, Y.; Wen, D.; Liu, W.; Wang, J.; Fan, G.; Ruan, L.; Song, B.; Cai, Y.; Wei, M.; et al. A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19. N. Engl. J. Med. 2020, 382, 1787–1799. [Google Scholar] [CrossRef]
- Li, Y.; Xie, Z.; Lin, W.; Cai, W.; Wen, C.; Guan, Y.; Mo, X.; Wang, J.; Wang, Y.; Peng, P.; et al. Efficacy and Safety of Lopinavir/Ritonavir or Arbidol in Adult Patients with Mild/Moderate COVID-19: An Exploratory Randomized Controlled Trial. Med 2020, 1, 105–113.e4. [Google Scholar] [CrossRef]
- Hung, I.F.-N.; Lung, K.-C.; Tso, E.Y.-K.; Liu, R.; Chung, T.W.-H.; Chu, M.-Y.; Ng, Y.-Y.; Lo, J.; Chan, J.; Tam, A.R.; et al. Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: An open-label, randomised, phase 2 trial. Lancet 2020, 395, 1695–1704. [Google Scholar] [CrossRef]
- Huang, Y.-Q.; Tang, S.-Q.; Xu, X.-L.; Zeng, Y.-M.; He, X.-Q.; Li, Y.; Harypursat, V.; Lu, Y.-Q.; Wan, Y.; Zhang, L.; et al. No Statistically Apparent Difference in Antiviral Effectiveness Observed Among Ribavirin Plus Interferon-Alpha, Lopinavir/Ritonavir Plus Interferon-Alpha, and Ribavirin Plus Lopinavir/Ritonavir Plus Interferon-Alpha in Patients With Mild to Moderate Coronavirus Disease 2019: Results of a Randomized, Open-Labeled Prospective Study. Front. Pharmacol. 2020, 11, 1071. [Google Scholar] [CrossRef]
- Horby, P.W.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Emberson, J.; Palfreeman, A.; Raw, J.; Elmahi, E.; Prudon, B.; et al. Lopinavir–ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2020, 396, 1345–1352. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Asiri, A.Y.; Assiri, A.M.; Balkhy, H.H.; Al Bshabshe, A.; Al Jeraisy, M.; Mandourah, Y.; Azzam, M.H.A.; Bin Eshaq, A.M.; Al Johani, S.; et al. Interferon Beta-1b and Lopinavir–Ritonavir for Middle East Respiratory Syndrome. N. Engl. J. Med. 2020, 383, 1645–1656. [Google Scholar] [CrossRef]
- Sevilla-Castillo, F.; Roque-Reyes, O.J.; Romero-Lechuga, F.; Gómez-Núñez, M.F.; Castillo-López, M.; Medina-Santos, D.; Román, P.O.; Flores-Hernández, J.R.; Méndez-Coca, J.D.; Montaño-Olmos, D.; et al. Both Chloroquine and Lopinavir/Ritonavir Are Ineffective for COVID-19 Treatment and Combined Worsen the Pathology: A Single-Center Experience with Severely Ill Patients. Biomed. Res. Int. 2021, 2021, 1–12. [Google Scholar] [CrossRef]
- Malhani, A.A.; Enani, M.A.; Sharif-Askari, F.S.; Alghareeb, M.R.; Bin-Brikan, R.T.; AlShahrani, S.A.; Halwani, R.; Tleyjeh, I.M. Combination of (interferon beta-1b, lopinavir/ritonavir and ribavirin) versus FPVipiravir in hospitalized patients with non-critical COVID-19: A cohort study. PLoS ONE 2021, 16, e0252984. [Google Scholar] [CrossRef]
- Lepage, M.-A.; Rozza, N.; Kremer, R.; Grunbaum, A. Safety and effectiveness concerns of lopinavir/ritonavir in COVID-19 affected patients: A retrospective series. Clin. Toxicol. 2021, 59, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.; Jaenigen, B.; Wagner, D.; Rieg, S.; Hornuss, D.; Biever, P.M.; Kern, W.V.; Walz, G. Therapy with lopinavir/ritonavir and hydroxychloroquine is associated with acute kidney injury in COVID-19 patients. PLoS ONE 2021, 16, e0249760. [Google Scholar] [CrossRef]
- Fu, W.; Liu, Y.; Liu, L.; Hu, H.; Cheng, X.; Liu, P.; Song, Z.; Zha, L.; Bai, S.; Xu, T.; et al. An open-label, randomized trial of the combination of IFN-κ plus TFF2 with standard care in the treatment of patients with moderate COVID-19. EClinicalMedicine 2020, 27, 100547. [Google Scholar] [CrossRef]
- Li, C.; Luo, F.; Liu, C.; Xiong, N.; Xu, Z.; Zhang, W.; Yang, M.; Wang, Y.; Liu, D.; Yu, C.; et al. Effect of a genetically engineered interferon-alpha versus traditional interferon-alpha in the treatment of moderate-to-severe COVID-19: A randomised clinical trial. Ann. Med. 2021, 53, 391–401. [Google Scholar] [CrossRef]
- Li, H.; Xiong, N.; Li, C.; Gong, Y.; Liu, L.; Yang, H.; Tan, X.; Jiang, N.; Zong, Q.; Wang, J.; et al. Efficacy of ribavirin and interferon-α therapy for hospitalized patients with COVID-19: A multicenter, retrospective cohort study. Int. J. Infect. Dis. 2021, 104, 641–648. [Google Scholar] [CrossRef]
- Darazam, I.A.; Shokouhi, S.; Pourhoseingholi, M.A.; Irvani, S.S.N.; Mokhtari, M.; Shabani, M.; Amirdosara, M.; Torabinavid, P.; Golmohammadi, M.; Hashemi, S.; et al. Role of interferon therapy in severe COVID-19: The COVIFERON randomized controlled trial. Sci. Rep. 2021, 11, 8059. [Google Scholar] [CrossRef]
- Fang, J.; Li, H.; Du, W.; Yu, P.; Guan, Y.-Y.; Ma, S.-Y.; Liu, D.; Chen, W.; Shi, G.-C.; Bian, X.-L. Efficacy of Early Combination Therapy With Lianhuaqingwen and Arbidol in Moderate and Severe COVID-19 Patients: A Retrospective Cohort Study. Front. Pharmacol. 2020, 11, 560209. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.Y.; Xie, Z.W.; Li, Y.P.; Deng, X.L.; Chen, X.T.; Cao, Y.; Ou, X.; Lin, W.Y.; Li, F.; Cai, W.P.; et al. Real-world efficacy and safety of lopinavir/ritonavir and arbidol in treating with COVID-19: An observational cohort study. Zhonghua Nei Ke Za Zhi 2020, 59, E012. [Google Scholar] [CrossRef]
- Deng, L.; Li, C.; Zeng, Q.; Liu, X.; Li, X.; Zhang, H.; Hong, Z.; Xia, J. Arbidol combined with LPV/r versus LPV/r alone against Corona Virus Disease 2019: A retrospective cohort study. J. Infect. 2020, 81, e1–e5. [Google Scholar] [CrossRef]
- Chen, J.; Lin, S.; Niu, C.; Xiao, Q. Clinical evaluation of Shufeng Jiedu Capsules combined with umifenovir (Arbidol) in the treatment of common-type COVID-19: A retrospective study. Expert Rev. Respir. Med. 2020, 15, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.K.; Hao, S.L.; Ma, J.H.; Wei, G.Y.; Song, K.Y.; Tang, C.; Gao, Y.F.; Liang, S.Q.; Du, W.J. Observation on clinical effect of Shufeng Jiedu Capsule combined with Arbidol Hydrochloride Capsule in treatment of COVID-19. Chin. Tradit. Herb. Drugs 2020, 51, 1167–1170. [Google Scholar] [CrossRef]
- Yu, P.; Li, Y.Z.; Wan, S.B.; Wang, Y. Effects of Lianhua Qingwen Granules Plus Arbidol on Treatment of Mild Corona Virus Disease-19. Chin. Pharm. J. 2020, 55, 1042–1045. [Google Scholar] [CrossRef]
- Xi, W.-N.; Jin, D.; Sun, K.; Yu, R.-Y.; Yao, X.-B.; Zou, B.-S.; Song, Z.-Y.; Yang, A.-Y.; Luo, R.-X.; Liu, Y.; et al. Treatment with Arbidol and Moxifloxacin in Ordinary and Severe Adult Patients Infected with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Huang, H.; Guan, L.; Yang, Y.; Le Grange, J.M.; Tang, G.; Xu, Y.; Yuan, J.; Lin, C.; Xue, M.; Zhang, X.; et al. Chloroquine, arbidol (umifenovir) or lopinavir/ritonavir as the antiviral monotherapy for COVID-19 patients: A retrospective cohort study. Res. Sq. 2020, 2020, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Xu, P.; Huang, J.; Fan, Z.; Huang, W.; Qi, M.; Lin, X.; Song, W.; Yi, L. Arbidol/IFN-α2b therapy for patients with corona virus disease 2019: A retrospective multicenter cohort study. Microbes Infect. 2020, 22, 200–205. [Google Scholar] [CrossRef]
- Nojomi, M.; Yassin, Z.; Keyvani, H.; Makiani, M.J.; Roham, M.; Laali, A.; Dehghan, N.; Navaei, M.; Ranjbar, M. Effect of Arbidol (Umifenovir) on COVID-19: A randomized controlled trial. BMC Infect. Dis. 2020, 20, 954. [Google Scholar] [CrossRef] [PubMed]
- Ghaderkhani, S.; Khaneshan, A.S.; Salami, A.; Alavijeh, P.E.; Kouchak, H.E.; Khalili, H.; Naghi, S.A.A.; Ahmadinejad, Z.; Rasolinejad, M.; Hajiabdolbaghi, M.; et al. Efficacy and Safety of Arbidol in Treatment of Patients with COVID-19 Infection: A Randomized Clinical Trial. Res. Sq. 2020, 2020, 1–13. [Google Scholar] [CrossRef]
- Li, M.; Yu, T.; Zhu, J.; Wang, Y.; Yang, Y.; Zhao, K.; Yi, Y.; He, J.; Li, C.; He, J. Comparison of the antiviral effect of Arbidol and Chloroquine in treating COVID-19. Ann. Palliat. Med. 2021, 10, 3307–3312. [Google Scholar] [CrossRef]
- Chiba, S. Effect of early oseltamivir on outpatients without hypoxia with suspected COVID-19. Wien. Klin. Wochenschr. 2020, 133, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Meriglier, E.; Rivoisy, C.; Hessamfar, M.; Bernard, N.; Aureau, I.; Lapoirie, J.; Contis, A.; Sacher, F.; Sacristan, B.; Lahouati, M.; et al. Safety of hydroxychloroquine and darunavir or lopinavir in COVID-19 infection. J. Antimicrob. Chemother. 2021, 76, 482–486. [Google Scholar] [CrossRef]
- Davoudi-Monfared, E.; Rahmani, H.; Khalili, H.; Hajiabdolbaghi, M.; Salehi, M.; Abbasian, L.; Kazemzadeh, H.; Yekaninejad, M.S. A Randomized Clinical Trial of the Efficacy and Safety of Interferon β-1a in Treatment of Severe COVID-19. Antimicrob. Agents Chemother. 2020, 64, e01061-20. [Google Scholar] [CrossRef]
- Qu, J.; Li, G.-H.; Wang, J.-J.; He, G.-F.; Huang, J.-J.; Chen, Y.; Qu, Q.; Chen, X.-Y.; Lu, Q. Comparative effectiveness of Lopinavir/Ritonavir-based regimens in COVID-19. Clin. Exp. Pharmacol. Physiol. 2021, 48, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Parkar, J.; Ansari, A.; Vora, A.; Talwar, D.; Tiwaskar, M.; Patil, S.; Barkate, H. Role of FPVipiravir in the treatment of COVID-19. Int. J. Infect. Dis. 2021, 102, 501–508. [Google Scholar] [CrossRef]
- Duyan, M.; Ozturan, I.U. Acute Psychosis in COVID-19: Is It Due to FPVipiravir Treatment or Acute Viral Illness? SN Compr. Clin. Med. 2021, 3, 1627–1629. [Google Scholar] [CrossRef]
- Agrawal, U.; Raju, R.; Udwadia, Z.F. FPVipiravir: A new and emerging antiviral option in COVID-19. Med. J. Armed Forces India 2020, 76, 370–376. [Google Scholar] [CrossRef]
- Kaur, R.J.; Charan, J.; Dutta, S.; Sharma, P.; Bhardwaj, P.; Sharma, P.; Lugova, H.; Krishnapillai, A.; Islam, S.; Haque, M.; et al. Favipiravir Use in COVID-19: Analysis of Suspected Adverse Drug Events Reported in the WHO Database. Infect. Drug Resist. 2020, 13, 4427–4438. [Google Scholar] [CrossRef]
- De Andrea, M.; Ravera, R.; Gioia, D.; Gariglio, M.; Landolfo, S. The interferon system: An overview. Eur. J. Paediatr. Neurol. 2002, 6, A41–A46. [Google Scholar] [CrossRef] [Green Version]
- Jakimovski, D.; Kolb, C.; Ramanathan, M.; Zivadinov, R.; Weinstock-Guttman, B. Interferon β for Multiple Sclerosis. Cold Spring Harb. Perspect. Med. 2018, 8, a032003. [Google Scholar] [CrossRef]
- Hasselbalch, H.C.; Skov, V.; Kjær, L.; Ellervik, C.; Poulsen, A.; Poulsen, T.D.; Nielsen, C.H. COVID-19 as a mediator of interferon deficiency and hyperinflammation: Rationale for the use of JAK1/2 inhibitors in combination with interferon. Cytokine Growth Factor Rev. 2021, 60, 28–45. [Google Scholar] [CrossRef]
- Yuan, J.; Zou, R.; Zeng, L.; Kou, S.; Lan, J.; Li, X.; Liang, Y.; Ding, X.; Tan, G.; Tang, S.; et al. The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm. Res. 2020, 69, 599–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Q.; Chen, V.; Shannon, C.P.; Wei, X.-S.; Xiang, X.; Wang, X.; Wang, Z.-H.; Tebbutt, S.J.; Kollmann, T.R.; Fish, E.N. Interferon-α2b Treatment for COVID-19. Front. Immunol. 2020, 11, 1061. [Google Scholar] [CrossRef]
- Wang, N.; Zhan, Y.; Zhu, L.; Hou, Z.; Liu, F.; Song, P.; Qiu, F.; Wang, X.; Zou, X.; Wan, D.; et al. Retrospective Multicenter Cohort Study Shows Early Interferon Therapy Is Associated with FPVorable Clinical Responses in COVID-19 Patients. Cell Host Microbe 2020, 28, 455–464.e2. [Google Scholar] [CrossRef]
- Kaplan, S.S.; Hicks, C.B. Lopinavir/ritonavir in the treatment of human immunodeficiency virus infection. Expert Opin. Pharmacother. 2005, 6, 1573–1585. [Google Scholar] [CrossRef]
- Podzamczer, D.; King, M.S.; Klein, C.E.; Flexner, C.; Katlama, C.; Havlir, D.V.; Letendre, S.L.; Eron, J.J.; Brun, S.C.; Bernstein, B. High-Dose Lopinavir/Ritonavir in Highly Treatment-Experienced HIV-1 Patients: Efficacy, Safety, and Predictors of Response. HIV Clin. Trials 2015, 8, 193–204. [Google Scholar] [CrossRef]
- Meini, S.; Pagotto, A.; Longo, B.; Vendramin, I.; Pecori, D.; Tascini, C. Role of Lopinavir/Ritonavir in the Treatment of Covid-19: A Review of Current Evidence, Guideline Recommendations, and Perspectives. J. Clin. Med. 2020, 9, 2050. [Google Scholar] [CrossRef]
- Choi, M.J.; Kang, M.; Shin, S.Y.; Noh, J.Y.; Cheong, H.J.; Kim, W.J.; Jung, J.; Song, J.Y. Comparison of antiviral effect for mild-to-moderate COVID-19 cases between lopinavir/ritonavir versus hydroxychloroquine: A nationwide propensity score-matched cohort study. Int. J. Infect. Dis. 2021, 102, 275–281. [Google Scholar] [CrossRef]
- Yadollahzadeh, M.; Eskandari, M.; Roham, M.; Zamani, F.; Laali, A.; Yassin, Z.; Zeiaei, M.T.; Rahimian, N.; Moetamed, N.; Aliakbar, A.; et al. Evaluation of Sovodak (Sofosbuvir/Daclatasvir) Treatment Outcome in COVID-19 Patient’s Compared with Kaletra (Lopinavir/ritonavir): A Randomized Clinical Trial. Res. Sq. 2021, 2021, 1–18. [Google Scholar] [CrossRef]
- Hossain, M.J.; Rahman, S.M.A. Repurposing therapeutic agents against SARS-CoV-2 infection: Most promising and neoteric progress. Expert Rev. Anti. Infect. Ther. 2020, 19, 1009–1027. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cao, R.; Zhang, H.; Liu, J.; Xu, M.; Hu, H.; Li, Y.; Zhao, L.; Li, W.; Sun, X.; et al. The anti-influenza virus drug, arbidol is an efficient inhibitor of SARS-CoV-2 in vitro. Cell Discov. 2020, 6, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, W.; Peng, B.; Peng, W.; Zhang, Y.; Wang, Y.; Wan, Y.; Chang, J.; Mao, L.; Miao, X.; et al. Potential of Arbidol for Post-exposure Prophylaxis of COVID-19 Transmission: A Preliminary Report of a Retrospective Cohort Study. Curr. Med. Sci. 2020, 40, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Chen, Y.; Yuan, J.; Yi, P.; Ding, C.; Wu, W.; Li, Y.; Ni, Q.; Zhou, R.; Li, X.; et al. Clinical Efficacy of Arbidol in Patients with 2019 Novel Coronavirus-Infected Pneumonia: A Retrospective Cohort Study. SSRN Electron. J. 2020, 2020, 1–28. [Google Scholar] [CrossRef]
- Yadegarinia, D.; Tehrani, S.; Abolghasemi, S.; Zarghi, A.; Sali, S.; Zolfaghari, F. Evaluation of the Efficacy of Arbidol in Comparison with the Standard Treatment Regimen of Hospitalized Patients with Covid-19: A Randomized Clinical Trial. Arch. Clin. Infect. Dis. 2020, 15, 1–6. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Y.; Zhu, B.; Zeng, J.; Hong, W.; He, X.; Chen, J.; Zheng, H.; Qiu, S.; Deng, Y.; et al. Associations of clinical characteristics and antiviral drugs with viral RNA clearance in patients with COVID-19 in Guangzhou, China: A retrospective cohort study. medRxiv 2020. [Google Scholar] [CrossRef]
- McClellan, K.; Perry, C. Oseltamivir: A review of its use in influenza. Drugs 2001, 61, 263–283. [Google Scholar] [CrossRef] [PubMed]
- Whitley, R.J.; Hayden, F.G.; Reisinger, K.S.; Young, N.; Dutkowski, R.; Ipe, D.; Mills, R.G.; Ward, P. Oral oseltamivir treatment of influenza in children. Pediatr. Infect. Dis. J. 2001, 20, 127–133. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Sanders, J.M.; Monogue, M.L.; Jodlowski, T.Z.; Cutrell, J.B. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 323, 1824–1836. [Google Scholar] [CrossRef]
- Wu, R.; Wang, L.; Kuo, H.-C.D.; Shannar, A.; Peter, R.; Chou, P.J.; Li, S.; Hudlikar, R.; Liu, X.; Liu, Z.; et al. An Update on Current Therapeutic Drugs Treating COVID-19. Curr. Pharmacol. Rep. 2020, 6, 56–70. [Google Scholar] [CrossRef]
- Mancilla-Galindo, J.; García-Méndez, J.Ó.; Marquéz-Sánchez, J.; Reyes-Casarrubias, R.E.; Aguirre-Aguilar, E.; Rocha-González, H.I.; Kammar-García, A. All-cause mortality among patients treated with repurposed antivirals and antibiotics for COVID-19 in Mexico City: A real-world observational study. EXCLI J. 2021, 20, 199–222. [Google Scholar] [CrossRef]
- Deeks, E.D. Darunavir/Cobicistat/Emtricitabine/Tenofovir Alafenamide: A Review in HIV-1 Infection. Drugs 2018, 78, 1013–1024. [Google Scholar] [CrossRef]
- Chowdhury, K.H.; Chowdhury, R.; Mahmud, S.; Tareq, A.M.; Hanif, N.B.; Banu, N.; Reza, A.S.M.; Emran, T.B.; Simal-Gandara, J. Drug repurposing approach against novel coronavirus disease (COVID-19) through virtual screening targeting SARS-CoV-2 main protease. Biology 2021, 10, 2. [Google Scholar] [CrossRef]
- Halder, U.C. Predicted antiviral drugs Darunavir, Indinavir and Rimantadine can potentially bind to neutralize COVID-19 conserved proteins. Res. Sq. 2020, 2020, 1–21. [Google Scholar] [CrossRef]
- OECD. Policy Responses to Coronavirus (COVID-19). Coronavirus (COVID-19) Vaccines for Developing Countries: An Equal Shot at Recovery. Available online: https://www.oecd.org/coronavirus/policy-responses/coronavirus-covid-19-vaccines-for-developing-countries-an-equal-shot-at-recovery-6b0771e6/ (accessed on 27 July 2021).
- Bari, M.S.; Hossain, M.J.; Akhter, S.; Emran, T.B. Delta variant and black fungal invasion: A bidirectional assault might worsen the massive second/third stream of COVID-19 outbreak in South-Asia. Ethics Med. Public Health 2021, 19, 100722. [Google Scholar] [CrossRef]
- Williamson, B.N.; Feldmann, F.; Schwarz, B.; Meade-White, K.; Porter, D.P.; Schulz, J.; Van Doremalen, N.; Leighton, I.; Yinda, C.K.; Pérez-Pérez, L.; et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Nature 2020, 585, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Nagata, T.; Lefor, A.K.; Hasegawa, M.; Ishii, M. Favipiravir: A new medication for the Ebola virus disease pandemic. Dis. Med. Public Health Prep. 2015, 9, 79–81. [Google Scholar] [CrossRef]
- Sharun, K.; Tiwari, R.; Dhama, K.; Emran, T.B.; Rabban, A.A.; Al Mutair, A. Emerging SARS-CoV-2 variants: Impact on vaccine efficacy and neutralizing antibodies. Hum. Vaccines Immunother. 2021, 17, 1–4. [Google Scholar] [CrossRef]
- Hossain, M.J. Impact of COVID-19 pandemic among health care providers in Bangladesh: A systematic review. Bangladesh J. Infect. Dis. 2020, 7 (Suppl. S2), S8–S15. [Google Scholar] [CrossRef]
- Hossain, M.J.; Islam, M.S.; Shahriar, S.; Sanam, S.; Emran, T.B.; Khatun, C.S.; Islam, M.R.; Mitra, S.; Dhama, K. Comedication of rabeprazole sodium causes potential drug-drug interaction with diabetic drug linagliptin: In-vitro and in-silico approaches. J. Exp. Biol. Agric. Sci. 2021, 9, 528–542. [Google Scholar] [CrossRef]
- Lai, C.C.; Wang, C.Y.; Hsueh, P.R. Coinfections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020, 53, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Liu, Y.; Zhong, Q.; Zhang, K.; Xu, Y.; Wang, Z. Lopinavir/ritonavir and interferon combination therapy may help shorten the duration of viral shedding in patients with COVID-19: A retrospective study in two designated hospitals in Anhui, China. J. Med. Virol. 2020, 92, 2666–2674. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
