Abstract
The COVID-19 pandemic disrupted dental education significantly, forcing adaptations in both didactic and clinical curricula. This study evaluates the impact of COVID-19 on dental students’ mental health and perceptions of the SARS-CoV-2 vaccine. An anonymous online survey was administered to dental students at Roseman University of Health Sciences, focusing on health experiences and vaccination perceptions. Results showed 56.8% of students were concerned about their emotional health, 82.1% felt stressed, and 60.6% felt depressed. About 81.9% received the vaccine, with 75.5% believing it effective, though only 55.3% supported mandatory vaccination. The pandemic negatively impacted students’ emotional health, indicating a need for institutional mental health support. This study was conducted during the COVID-19 pandemic, and findings relate specifically to that period. Further research can focus on investigation of reasonings behind the sentiments.
1. Introduction
COVID-19 is an infectious disease of varying severity caused by the SARS-CoV-2 virus. Transmission primarily occurs through respiratory droplets and fomites [1]. The virus can survive for hours in aerosols and days on surfaces [2,3]. Patients who are pre-symptomatic or asymptomatic can also spread the virus, which facilitates transmission [4,5].
The first human case of COVID-19 was diagnosed and recognized as a serious respiratory disease in December 2019 [1]. Several scientific task forces have been assembled since then to gather information on the disease [6]. Studies have identified the virus’ biological mechanism, transmission modes, diagnostic tests, and vaccines.
COVID-19 was declared a global pandemic by the World Health Organization (WHO) on 11 March 2020 due to the rapid and abrupt worldwide transmission pattern of the virus [7]. Although global efforts are being made to stem COVID-19’s spread, it remains a significant public health concern as of 2024 [8,9]. On 15 May 2023, the WHO director general accepted the recommendation to no longer classify COVID-19 as a global emergency, but this decision did not signify the end of the pandemic, and a review committee formed to create long-term guidelines for countries on how to manage COVID-19 continuously [10]. As of June 2024, there were 103 million cumulative confirmed cases of COVID-19 reported in the US, with over 1.2 million deaths attributed to COVID-19 [11].
The COVID-19 lockdowns in the US began in March 2020 when states implemented various stay-at-home orders to curb the spread of the virus. These orders varied in length and strictness across different states [12]. For example, California issued one of the earliest statewide lockdowns on 19 March 2020 [12,13], while states like Arkansas, Iowa, Nebraska, North Dakota, South Dakota, Utah, and Wyoming never issued a statewide order [12,14,15]. Most of these lockdowns lasted until late May or June 2020 [14,16,17], with some states extending or modifying restrictions through the summer and fall of 2020 [18]. By mid-2021, many states had lifted their stay-at-home orders, although some public health emergency declarations continued into 2022 to manage ongoing mitigation efforts [19]. Lockdowns and social isolation can reduce COVID-19 spread but also cause psychological distress, anxiety, and depression [12].
Since the COVID-19 pandemic began, more studies have been conducted on students’ mental health. Hung et al. [20] reported students’ challenges in maintaining focus and motivation during their studies. Students experienced restless sleep, stress, and anxiety due to the pandemic’s uncertainty. A recent meta-analysis found that 34% and 32% of students experience depressive and anxiety symptoms, respectively [21]. In the healthcare field, students in medicine, dentistry, nursing, and pharmacy play a unique role as both students and caregivers. Before the pandemic, medical and dental students already suffered from high stress levels, and these worsened during the pandemic [22].
The COVID-19 pandemic has significantly disrupted dental education. It has disturbed all aspects of life, with dental education being no exception. Dental schools were one of the most severely impacted institutions during the early stages of the pandemic [23]. Dental schools had to manage lockdown by adjusting didactic and clinical curricula [24]. The Centers for Disease Control and Prevention (CDC) asked dentists to provide only essential care in order help preserve personal protective equipment for frontline providers [25], resulting in disruption to academic dental clinics and research endeavors. This kept students from practicing their clinical skills and learning necessary for their graduation requirement and future success in their career [26]. Schools also moved from in-person didactic to virtual learning, causing significant changes that likely caused worry and stress for students [27].
Several studies have indicated that the COVID-19 pandemic affected dental education and practice [28]. A lack of clinical skills caused by the pandemic stressed dental students, who worried about their competency after graduation [29]. Online education decreased the quality of life for dental students [30]. Indeed, studies showed significant anxiety and depression among dental students during the COVID-19 pandemic [31,32].
After extensive research, COVID-19 vaccines were introduced in December 2020 to control its rapid spread and were approved by the WHO [33,34]. As the vaccines became more available in March 2021, the University required students to receive it. Although many accepted the vaccines, some resisted due to lack of understanding [35].
Vaccination significantly impacted dental students [36]. It reduced COVID-19 cases and hospitalizations in the US [37]. Many schools allowed students to return to campus with a weekly negative COVID-19 test or proof of vaccination, reducing the need for social distancing and masks [38,39,40]. As transmission rates dropped, life returned to a new normal [41,42]. The US population showed varying levels of hesitancy towards the new vaccine, including healthcare workers, with 23% of correctional healthcare workers and 17% of general healthcare workers refusing vaccination [43]. The American Dental Association (ADA) strongly encouraged dental professionals to get vaccinated [44]. However, the ADA only provides guidelines and defers to CDC recommendations [44].
Although much has been written on the stress experienced by dental school students [45,46,47], little is known about how pandemic-related changes to dental curricula affected their stress and the mental health. This study uniquely addresses the combined effect of curriculum changes and personal health concerns on dental students during the COVID-19 pandemic, providing insights not covered in previous studies. While prior research explored general impacts on dental education [20,48,49], this study focuses specifically on the mental health and vaccination perceptions in a unique institutional context. Furthermore, this research examines detailed demographic differences, such as race and ethnicity, and their specific impacts on mental health and vaccination attitudes, which have not been extensively studied.
Thus, this study aims to evaluate the impact of COVID-19 on dental students’ stress and mental health, in addition to assessing student perception and hesitancy toward the SARS-CoV-2 vaccine, along with perception of its effectiveness.
2. Materials and Methods
2.1. Setting and Participants
The survey project was conducted at Roseman University of Health Sciences (RUHS) College of Dental Medicine (CODM). RUHS is a private, nonprofit health sciences university offering a dental medicine doctoral (DMD) degree and residency training in orthodontics. The DMD program is located in Utah. The orthodontic program is located in Nevada. Dental clinics at both the Utah and Nevada campuses maintained clinical operations for urgent care services during the pandemic. Both dental programs are accredited by the Commission on Dental Accreditation in the United States.
The study team sent an email to students and residents (collectively referred to as dental students) asking them to complete a survey on “Student Perceptions of COVID-19”. The email included a brief description of the survey, assured dental students that participation was voluntary, and assured that responses would be kept anonymous. The window for survey completion was 16 weeks (from 26 April 2021 to 25 August 2021), with reminder emails sent to the students at the end of the second week, sixth week, and twelfth week. The study received approval from Roseman University of Health Sciences Institutional Review Board. Students provided their informed consent by responding to the survey questions, with the act of completing the survey indicating their agreement to participate in the study.
2.2. Survey Instrument
This is a cross-sectional survey study aimed at assessing the impact of COVID-19 on dental students via the SurveyMonkey [50] online platform. The study team developed a survey to evaluate how the COVID-19 pandemic impacted dental students at Roseman CODM and to see how COVID-19 influenced student perceptions of the 2020–2021 school year. Survey items were adapted from a validated instrument in the literature [20], drafted, and reviewed by the study team. They were designed to start with “In light of COVID-19” to ensure that responses focused on the pandemic and not pre-pandemic events. The survey allowed students to express how they felt RUHS responded to the pandemic. Students were asked to express concerns that they had for their emotional health in light of COVID-19, and how often they felt stressed or depressed. Also considered was whether students’ family members or roommates tested positive for COVID-19, and their level of concern for contracting COVID-19 on campus.
At the time of the survey, Roseman University CODM did not require students to receive the COVID-19 vaccine but did recommend weekly COVID-19 tests for unvaccinated students. This study assessed students’ beliefs on whether their school should require students, faculty, and staff to receive the COVID-19 vaccine, students’ beliefs on the rapid testing of patients for COVID-19 before they could receive treatment, and which COVID-19 vaccine students had received. Perceptions of the effectiveness of vaccine in protecting individuals from getting the COVID-19 infection were also evaluated.
2.3. Data Analyses
Descriptive statistics were computed to examine the distribution of the survey responses. The proportions of dental students having concerns related to their mental health as well as their perceptions about the COVID-19 vaccine were examined, with the study stratifying by respondents who knew of a family member or friend who had tested positive for COVID-19 versus those who did not know. All data analyses were calculated utilizing SPSS version 28.0. This software, which has been used by others to conduct COVID-19 research, was chosen for its robustness in handling survey data [51].
3. Results
3.1. Demographics
A total of 95 dental students responded to the survey, representing a 22% response rate. The respondents consisted of 92.6% of DMD students and 7.4% of orthodontic residents. The age range was 22 to 47 years old (mean = 27.7 years; SD = 4.0 years; 95% CI = 26.8–28.5 years). The study sample consisted of 51.1% female, 62.4% White, and 94.6% non-Hispanic/non-Latino respondents. Furthermore, 60.2% of the sample were single, and 69.6% were non-Utah residents (Table 1).

Table 1.
Demographic characteristics.
3.2. Assessment of Mental Health Concerns and Perceptions of COVID-19 Vaccine
Figure 1 summarizes dental students’ self-reported mental health concerns associated with COVID-19. There were 56.8% of dental students who felt concerned about their emotional health, and 82.1% felt that they were stressed, while 60.6% felt depressed. Most dental students (75.5%) believed that the COVID-19 vaccine provided effective protection against contracting the COVID-19 infection. Over half of them (55.3%) thought that the school should require all students or faculty to receive the COVID-19 vaccine (Figure 1).
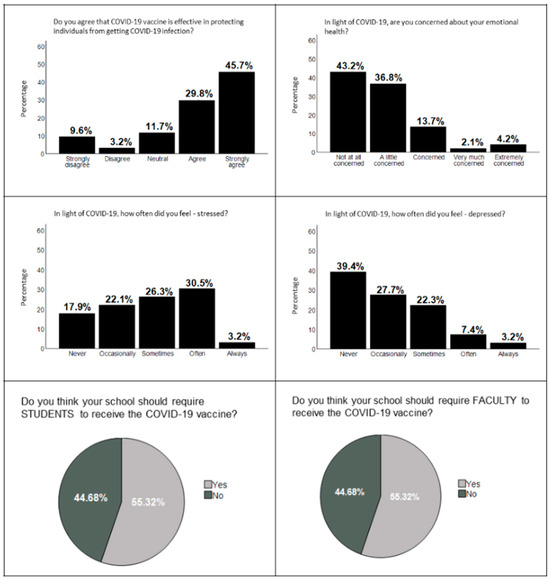
Figure 1.
Assessment of mental health concerns and perceptions of COVID-19 vaccines. Top left looks at perception of vaccine effectiveness. Top right looks at emotional health. Middle left looks at frequency of stress. Middle right looks at frequency of depression. Bottom left looks at whether the school should require students to receive the vaccine. Bottom right looks at whether the school should require faculty to receive the vaccine.
3.3. Assessments of Differences between Students with and without Family Members or Friends Who Had COVID-19
When asked whether the school should require students to receive the COVID-19 vaccine, 59.0% of the dental students without COVID-19-infected family members or friends indicated yes, whereas 52.7% of those with COVID-19-infected family members or friends indicated yes. Similarly, the percentage of students who thought the school should require faculty to receive the COVID-19 vaccine was higher among those without COVID-19-positive family members or friends than students with family members or friends who had COVID-19 (60% vs. 51.9%, respectively) (Table 2). Additionally, students who had family members or friends with COVID-19 were more likely to say that the COVID-19 vaccine offered adequate protection against COVID-19 infection than students who did not. Students who had family members or friends with COVID-19 were more concerned about their emotional health than those who did not. Those who had family members or friends with COVID-19 reported feeling more stressed than those who did not. Students who did not have COVID-19-affected family members or friends reported feeling more depressed than those who did (Figure 2).

Table 2.
Group differences in mindsets related to COVID-19 vaccine.
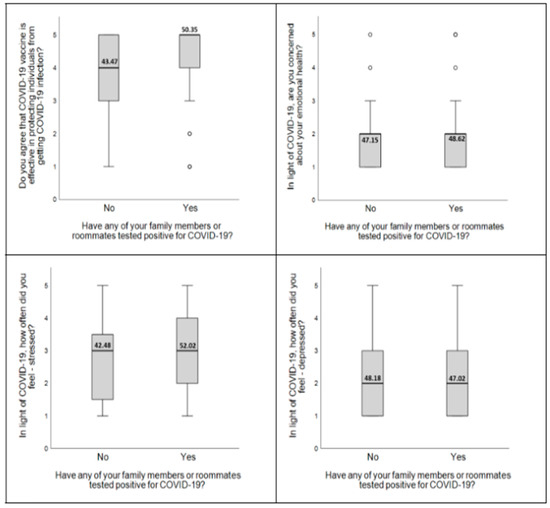
Figure 2.
Differences in perceptions of COVID-19 between students with and without COVID-19-positive family members or friends. Top left looks at the difference in perception of vaccine effectiveness between students with and without families or friends with COVID-19. Top right looks at the difference in concerns relating to emotional health between students with and without families or friends with COVID-19. Bottom left looks at the difference in the frequency of stress between students with and without families or friends with COVID-19. Bottom right looks at the difference in the frequency of depression between students with and without families or friends with COVID-19.
4. Discussion
Not only do dental students suffer from daily stress due to the everyday workload faced in school, but now an added constituent of the COVID-19 pandemic has also negatively contributed to the lives of these students. This study showed that many dental students expressed some feeling of depression and anxiety since the start of the COVID-19 pandemic. These elevated feelings of anxiety and depression could also cause these dental providers to not want to render emergency treatment, or may even prevent dentists from treating patients with their best care [52]. Worldwide, the COVID-19 pandemic may have even caused many patients to develop a “dental phobia” due to the high transmission risk in a dental office [53]. Because of this, many patients commonly avoid or delay their regularly scheduled appointments, causing them to mainly only come into the office when they are in an emergency situation [54]. Due to the significant reduction in patient visits in the dental office, dentists’ relationship with their patient was more affected during the pandemic compared to other healthcare professionals’ [54]. These work-related stress levels for dentists considerably contribute to dental professionals’ tendency to experience burnout, depression, and anxiety more so than other healthcare professionals [53]. The uncertainty of possible future pandemics and how they will affect the dental world present other reasons for anxiety and depression in current dental students.
The analysis showed significant differences in stress and depression levels among dental students of different races and ethnicities, highlighting the necessity for targeted mental health interventions. Research has indicated that racial and ethnic minorities often face unique stressors, including discrimination, cultural stigma around mental health, and a lack of culturally competent care, which can exacerbate mental health issues [55,56]. Within this study, non-White dental students reported higher levels of stress and depression compared to their White counterparts. This disparity underscores the critical need for mental health programs that are tailored to address the specific challenges faced by minority groups. Implementing culturally sensitive counseling services, fostering an inclusive educational environment, and providing stress management resources can help mitigate these disparities [57,58]. Ensuring that mental health interventions are equitable and accessible to all students, regardless of their racial or ethnic background, is essential for fostering a supportive educational environment.
This study also delved into dental students’ expectations regarding the SARS-CoV-2 vaccination, examining their views on its efficacy and the institutional vaccination policies. The majority of students expressed confidence in the vaccine’s effectiveness in preventing COVID-19 infection, with 75.5% believing in its protective benefits. However, the support for mandatory vaccination policies was more divided, with only 55.3% in favor of such measures. These findings reflect broader trends observed in healthcare settings, where vaccine hesitancy remains a concern despite high levels of vaccine acceptance [35]. Personal experiences with COVID-19, such as having family members or friends who contracted the virus, appeared to influence students’ views on mandatory vaccination. Those with direct exposure to COVID-19 were more likely to support vaccination mandates for both students and faculty. This suggests that personal experiences and perceived vulnerability play significant roles in shaping attitudes towards vaccination policies. As dental students are frontline healthcare workers in training, their vaccination status is crucial for both their safety and the safety of their patients. Thus, understanding and addressing the factors that influence vaccine hesitancy in this group are vital for developing effective public health strategies and ensuring high vaccination rates among future dental professionals.
The relationship between vaccination expectations and mental health status during the COVID-19 pandemic is multifaceted. Students who believed in the efficacy of the COVID-19 vaccine and supported vaccination mandates reported lower levels of stress and anxiety. This can be attributed to a heightened sense of protection and security against the virus, which alleviates some of the pandemic-related stressors. Conversely, those who were skeptical about the vaccine’s effectiveness or opposed mandatory vaccination policies often experienced higher levels of anxiety and uncertainty, likely due to fears of infection and concerns about vaccine safety and efficacy. This dichotomy highlights the critical role of clear communication and education about vaccine benefits and safety in reducing anxiety and promoting mental well-being among dental students [59]. Ensuring that students have access to reliable information and support can help mitigate the mental health impact of the pandemic and improve overall well-being.
4.1. Limitations
Despite the valuable insights provided by this study, several limitations must be acknowledged. First, the data collected during the COVID-19 pandemic may not fully capture the long-term effects and evolving nature of the crisis, limiting the ability to generalize findings over an extended period. Second, the reliance on self-reported data may introduce bias, as participants’ recollections and perceptions can be influenced by their experiences and current circumstances. Third, the study’s geographic focus may not account for regional variations in pandemic responses and outcomes, potentially limiting the applicability of the results to different contexts. Finally, the rapid pace of the pandemic’s progression necessitated quick decision-making, which may have resulted in incomplete data collection or analysis under certain circumstances.
4.2. Future Research Directions
Building on the findings of this study, several avenues for future research are recommended. One key area is the longitudinal analysis of the long-term impacts of the pandemic on various aspects of society, including mental health, economic stability, and healthcare systems. Additionally, comparative studies across different regions and countries could provide a more comprehensive understanding of the effectiveness of diverse pandemic response strategies. Research exploring the role of technology and digital innovation in enhancing pandemic preparedness and response is also crucial given the increasing reliance on digital tools during crises. Finally, investigating the integration of interdisciplinary approaches in pandemic management, combining insights from public health, economics, sociology, and technology, can yield more holistic and effective strategies for future health emergencies.
5. Conclusions
This study highlights significant mental health concerns and varying perceptions of the COVID-19 vaccine among dental students, emphasizing the impact of personal experiences with the disease on attitudes toward vaccination mandates. By addressing these issues, policymakers and educational leaders can strengthen public health frameworks and improve preparedness and resilience against future health emergencies.
Author Contributions
Conceptualization, M.H.; methodology, N.H., S.S. and M.H.; software, M.H.; validation, M.H.; formal analysis, M.H. and A.M.; investigation, M.H.; resources, M.H.; data curation, N.H., S.S., M.H. and A.M.; writing—original draft preparation, M.H., N.H., S.M. and A.M.; writing—review and editing, M.H., S.S., N.H., S.M. and A.M.; visualization, M.H. and A.M.; supervision, M.H.; project administration, M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by Roseman University of Health Sciences (IRB #2021-05) on 14 April 2021.
Informed Consent Statement
Informed consent was waived by all subjects involved in the study.
Data Availability Statement
Data can be made available with Principal Investigator and IRB approval.
Acknowledgments
The authors thank the Clinical Outcomes Research and Education at Roseman University of Health Sciences College of Dental Medicine and the Analytic Galaxy for the support for this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Holshue, M.L.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 2020, 382, 929–936. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral. Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.-Y.; Chen, L.; Wang, M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.-C.; Liu, Y.H.; Wang, C.-Y.; Wang, Y.-H.; Hsueh, S.-C.; Yen, M.-Y.; Ko, W.-C.; Hsueh, P.-R. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J. Microbiol. Immunol. Infect. 2020, 53, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Aziz, T.M.; Stockand, J.D. Recent progress and challenges in drug development against COVID-19 coronavirus (SARS-CoV-2)—an update on the status. Infect. Genet. Evol. 2020, 83, 104327. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19). Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 2 July 2024).
- World Health Organization. WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/cases?n=c (accessed on 2 July 2024).
- Idris, I.; Adesola, R.O. Emergence and spread of JN.1 COVID-19 variant. Bull. Natl. Res. Cent. 2024, 48, 27. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/europe/emergencies/situations/covid-19 (accessed on 2 July 2024).
- World Health Organization. Data. Available online: https://data.who.int/dashboards/covid19/deaths?n=o (accessed on 2 July 2024).
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C.; Poovey, J.; Werner, A.K.; Jones, C.D.; Fulmer, E.B.; et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement—United States. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- ALEC. COVID-19 Executive Orders Tracker for the 50 States. Available online: https://alec.org/article/covid-19-executive-orders-tracker-for-the-50-states/ (accessed on 2 July 2024).
- AARP. List of Coronavirus-Related Restrictions in Every State. Available online: https://www.aarp.org/politics-society/government-elections/info-2020/coronavirus-state-restrictions.html (accessed on 2 July 2024).
- American Institute for Economic Research. A Closer Look at the States That Stayed Open. Available online: https://www.aier.org/article/a-closer-look-at-the-states-that-stayed-open/ (accessed on 2 July 2024).
- Governor Gavin Newsom. As California Fully Reopens, Governor Newsom Announces Plans to Lift Pandemic Executive Orders. Available online: https://www.gov.ca.gov/2021/06/11/as-california-fully-reopens-governor-newsom-announces-plans-to-lift-pandemic-executive-orders/ (accessed on 2 July 2024).
- NC Chamber. State of NC Updates. Available online: https://ncchamber.com/coronavirus-resource-guide-nc-business/state-of-nc-updates/ (accessed on 2 July 2024).
- Mynorthwest. Timeline: A Look Back at Washington State’s COVID-19 Response. Available online: https://mynorthwest.com/2974047/timeline-washington-states-covid-19-response/ (accessed on 2 July 2024).
- National Academy for State Health Policy. States’ COVID-19 Public Health Emergency Declarations. Available online: https://nashp.org/state-tracker/states-covid-19-public-health-emergency-declarations/ (accessed on 2 July 2024).
- Hung, M.; Licari, F.W.; Hon, E.S.; Lauren, E.; Su, S.; Birmingham, W.C.; Wadsworth, L.L.; Lassetter, J.H.; Graff, T.C.; Harman, W.; et al. In an era of uncertainty: Impact of COVID-19 on dental education. J. Dent. Educ. 2021, 85, 148–156. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res 2021, 301, 113863. [Google Scholar] [CrossRef]
- Chandratre, S. Medical Students and COVID-19: Challenges and Supportive Strategies. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520935059. [Google Scholar] [CrossRef] [PubMed]
- Escontrías, O.A.; Istrate, E.C.; Flores, S.; Stewart, D.C.L. Operational and financial impact of the COVID-19 pandemic on U.S. dental school clinics. J. Dent. Educ. 2021, 85, 1863–1869. [Google Scholar] [CrossRef]
- Harvard School of Dental Medicine. Dental Education in a Time of COVID-19. Available online: https://hsdm.harvard.edu/news/dental-education-time-covid-19 (accessed on 2 July 2024).
- Centers for Disease Control and Prevention. Guidance for Dental Settings during the COVID-19 Response. Available online: https://emergency.cdc.gov/coca/calls/2020/callinfo_060320.asp (accessed on 15 July 2024).
- Ilić, J.; Radović, K.; Savić-Stanković, T.; Popovac, A.; Miletić, V.; Milić Lemić, A. The effect of COVID-19 pandemic on final year dental students’ self-confidence level in performing clinical procedures. PLoS ONE 2021, 16, e0257359. [Google Scholar] [CrossRef]
- ADEA. Response of the Dental Education Community to Novel Coronavirus (COVID-19). Available online: https://www.adea.org/COVID19-Update/ (accessed on 2 July 2024).
- Loch, C.; Kuan, I.B.J.; Elsalem, L.; Schwass, D.; Brunton, P.A.; Jum’ah, A. COVID-19 and dental clinical practice: Students and clinical staff perceptions of health risks and educational impact. J. Dent. Educ. 2021, 85, 44–52. [Google Scholar] [CrossRef]
- Løset, I.H.; Lægreid, T.; Rodakowska, E. Dental Students’ Experiences during the COVID-19 Pandemic-A Cross-Sectional Study from Norway. Int. J. Environ. Res. Public. Health 2022, 19, 3102. [Google Scholar] [CrossRef] [PubMed]
- Başağaoğlu Demirekin, Z.; Buyukcavus, M.H. Effect of distance learning on the quality of life, anxiety and stress levels of dental students during the COVID-19 pandemic. BMC Med. Educ. 2022, 22, 309. [Google Scholar] [CrossRef]
- Klaassen, H.; Ashida, S.; Comnick, C.L.; Xie, X.J.; Smith, B.M.; Tabrizi, M.; Arsenault, K.; Capin, O.R.; Scully, A.C.; da Mata, C.; et al. COVID-19 pandemic and its impact on dental students: A multi-institutional survey. J. Dent. Educ. 2021, 85, 1280–1286. [Google Scholar] [CrossRef] [PubMed]
- Santabarbara, J.; Idoiaga, N.; Ozamiz-Etxebarria, N.; Bueno-Notivol, J. Prevalence of Anxiety in Dental Students during the COVID-19 Outbreak: A Meta-Analysis. Int J Environ Res Public Health 2021, 18, 10978. [Google Scholar] [CrossRef]
- Cohen, J. Vaccine wagers on coronavirus surface protein pay off. Science 2020, 370, 894–895. [Google Scholar] [CrossRef]
- Karayürek, F.; Çebi, A.T.; Gülses, A.; Ayna, M. The Impact of COVID-19 Vaccination on Anxiety Levels of Turkish Dental Professionals and Their Attitude in Clinical Care: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2021, 18, 10373. [Google Scholar] [CrossRef]
- Fakonti, G.; Kyprianidou, M.; Toumbis, G.; Giannakou, K. Attitudes and Acceptance of COVID-19 Vaccination Among Nurses and Midwives in Cyprus: A Cross-Sectional Survey. Front. Public. Health 2021, 9, 656138. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.S.S.; Lee, H.Y.; Leong, J.Z.; Sulaiman, M.M.; Loo, W.F.; Tan, W.W. COVID-19 vaccination acceptance among dental students and dental practitioners: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0267354. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Huang, H.; Ju, J.; Sun, R.; Zhang, J. Impact of vaccination on the COVID-19 pandemic in U.S. states. Sci. Rep. 2022, 12, 1554. [Google Scholar] [CrossRef]
- University of Wisconsin–Madison. Required COVID Testing; What to Expect this Fall. Available online: https://news.wisc.edu/required-covid-testing-what-to-expect-this-fall/ (accessed on 2 July 2024).
- CCNY. Mask Wearing Indoors. Available online: https://www.ccny.cuny.edu/presidentsoffice/blog/covid-19 (accessed on 2 July 2024).
- Delaware County Community College. COVID-19 Vaccination Requirement Information. Available online: https://www.dccc.edu/vaccine-info (accessed on 2 July 2024).
- NPR Health. A New Normal? 6 Stories about the Evolving U.S. COVID Response in 2023. Available online: https://health.wusf.usf.edu/npr-health/2023-12-19/a-new-normal-6-stories-about-the-evolving-u-s-covid-response-in-2023 (accessed on 2 July 2024).
- University of Utah Health. What Will the “New Normal” of COVID-19 Look Like? Available online: https://uofuhealth.utah.edu/notes/2022/02/what-will-new-normal-of-covid-19-look (accessed on 2 July 2024).
- Gu, M.; Taylor, B.; Pollack, H.A.; Schneider, J.A.; Zaller, N. A pilot study on COVID-19 vaccine hesitancy among healthcare workers in the US. PLoS ONE 2022, 17, e0269320. [Google Scholar] [CrossRef]
- American Dental Association. ADA ‘Strongly’ Encouraging Dental Professionals to be Vaccinated. Available online: https://adanews.ada.org/ada-news/2021/july/ada-strongly-encouraging-dental-professionals-to-be-vaccinated (accessed on 15 July 2024).
- Al-Dhubaiban, M.; BinAjian, A.; Al-Shumrani, A.; Al-Thobaiti, A.; Al-Shalan, T. Stress among Dental Students in Saudi Dental Colleges: Cross-Sectional Study. J. Community Med. Public. Health 2023, 7, 387. [Google Scholar] [CrossRef]
- Alhilali, K.; Husni, M.; Almarabheh, A. Frequency of burnout in dental students and its relationship with stress level, depressive, and anxiety state. Middle East. Curr. Psychiatry 2024, 31, 21. [Google Scholar] [CrossRef]
- Lin, X.-J.; Zhang, C.-Y.; Yang, S.; Hsu, M.-L.; Cheng, H.; Chen, J.; Yu, H. Stress and its association with academic performance among dental undergraduate students in Fujian, China: A cross-sectional online questionnaire survey. BMC Med. Educ. 2020, 20, 181. [Google Scholar] [CrossRef] [PubMed]
- Iyer, P.; Aziz, K.; Ojcius, D.M. Impact of COVID-19 on dental education in the United States. J. Dent. Educ. 2020, 84, 718–722. [Google Scholar] [CrossRef] [PubMed]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; Krämer, N.; Schulz-Weidner, N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): A cross-sectional study. BMC Med. Educ. 2020, 20, 354. [Google Scholar] [CrossRef]
- SurveyMonkey. Available online: https://www.surveymonkey.com/ (accessed on 26 April 2021).
- Huo, W.; He, M.; Zeng, Z.; Bao, X.; Lu, Y.; Tian, W.; Feng, J.; Feng, R. Impact Analysis of COVID-19 Pandemic on Hospital Reviews on Dianping Website in Shanghai, China: Empirical Study. J. Med. Internet Res. 2024, 26, e52992. [Google Scholar] [CrossRef]
- Salehiniya, H.; Hatamian, S.; Abbaszadeh, H. Mental health status of dentists during COVID-19 pandemic: A systematic review and meta-analysis. Health Sci. Rep. 2022, 5, e617. [Google Scholar] [CrossRef]
- De Haro, J.C.; Rosel, E.M.; Salcedo-Bellido, I.; Leno-Durán, E.; Requena, P.; Barrios-Rodríguez, R. Psychological Impact of COVID-19 in the Setting of Dentistry: A Review Article. Int. J. Environ. Res. Public. Health 2022, 19, 16216. [Google Scholar] [CrossRef]
- Salgarello, S.; Audino, E.; Bertoletti, P.; Salvadori, M.; Garo, M.L. Dental Patients’ Perspective on COVID-19: A Systematic Review. Encyclopedia 2022, 2, 365–382. [Google Scholar] [CrossRef]
- González, H.M.; Tarraf, W.; Whitfield, K.E.; Vega, W.A. The epidemiology of major depression and ethnicity in the United States. J. Psychiatr. Res. 2010, 44, 1043–1051. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and Health: Evidence and Needed Research. Annu. Rev. Public. Health 2019, 40, 105–125. [Google Scholar] [CrossRef]
- Alvarez, J.; Jason, L.A.; Olson, B.D.; Ferrari, J.R.; Davis, M.I. Substance abuse prevalence and treatment among Latinos and Latinas. J. Ethn. Subst. Abuse 2007, 6, 115–141. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration. Evidence-Based and Culturally Relevant Behavioral Health Interventions in Practice: Strategies and Lessons Learned from NNEDLearn (2011–2020). Available online: https://store.samhsa.gov/sites/default/files/pep21-05-02-001.pdf (accessed on 15 July 2024).
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).