Abstract
Background: The COVID-19 pandemic disrupted global healthcare systems, requiring rapid adaptations. This study evaluates the impact on health systems and services in India during the peak of the first wave and its aftermath. It analyses disruptions, adaptive measures, and challenges faced by healthcare providers and seekers to enhance future preparedness. Methods: Primary studies conducted in India exploring the impact of COVID-19 on health services provision, utilisation, availability, and the well-being of providers and seekers were included. Electronic searches were conducted in six databases: PubMed, MEDLINE, Embase, Global Health, CINAHL, and the WHO database on COVID-19. The results were analysed using narrative synthesis. Results and Conclusion: The review examined 38 articles with 22,502 subjects. Health service provision, utilisation, and availability were significantly impacted, particularly in outpatient departments (n = 19) and elective services (n = 16), while emergency services remained sub-optimal (n = 20). Adaptations were made in precautionary measures, protocols, staff allocation, training, personal protective equipment (PPE), infrastructure, and resources. Providers faced mental health challenges including depression, stress (n = 14), fear of infection (n = 9), stigmatisation (n = 5), and financial repercussions (n = 5). Seekers also encountered notable challenges (n = 13). Future preparedness necessitates improved healthcare infrastructure, resource optimisation, and comprehensive protocols. Lessons should inform strategies to mitigate disruptions and prioritise the well-being of providers and seekers in future outbreaks.
1. Introduction
The World Health Organisation (WHO) declared coronavirus disease 2019 (COVID-19) a public health emergency of international concern on 30 January 2020, and after that declared it a pandemic on 11 March 2020 [1].
This outbreak has placed unprecedented demands on the health systems, health workforce, and communities worldwide [2,3,4,5,6,7,8]. India’s story is no different [9,10]. Given the large population of over 1.3 billion, the government of India declared a total lockdown across the country as a part of its efforts to control the disease spread [11].
The COVID-19 outbreak has placed severe strain on the health services in India at all levels in hospitals, clinics, and health care centres, with large and rapid increases in demand for patient care [10,12,13]. Caring for COVID-19 patients whilst maintaining treatment for patients with other conditions presented a complex planning challenge [14,15,16]. Ensuring safe and timely care to both COVID-19 patients and those with other conditions was a crucial aspect of the health system’s response to this crisis. In order to free up enough capacity to deal with the initial peak of the pandemic, the health system was forced to shut down or significantly reduce many areas of non-COVID-19 care across healthcare facilities during April, May, and June 2020 [17,18,19,20]. This, combined with fewer patients seeking care during the lockdown, meant that there had been a significant drop in elective procedures, urgent referrals, first treatments, and outpatient services [21,22]. A plethora of activities, adaptations, and measures were undertaken and implemented in a myriad of ways to protect lives and avoid a health system collapse [13,22,23,24]. Furthermore, the pandemic had profound mental and physical health implications for healthcare workers [25] and healthcare seekers, including individuals undergoing quarantine, hospitalisation, those who had recovered from the infection, and those managing other health conditions [15,17].
While several primary studies [26,27,28] have examined the impact of COVID-19 on the health system and its stakeholders in the Indian context, there is a need for a systematic appraisal and critique of these studies, particularly focusing on the peak of the outbreak. This review aims to consolidate the existing research to gain a comprehensive understanding of the health system’s response and assess the impact of the pandemic on healthcare services, healthcare providers, and healthcare seekers across various clinical areas and facilities during the peak of the COVID-19 outbreak in India. The review aims to achieve the following objectives in the Indian context:
- A.
- Assess the impact of COVID-19 on the provision, utilisation, and availability of health services;
- B.
- Understand the health system’s response—adaptations, interventions and efforts for continuity and resumption of services;
- C.
- Evaluate the implications of COVID-19 and its response on individuals—healthcare providers and healthcare seekers.
2. Materials and Methods
The review is registered with PROSPERO (International Prospective Register of systematic reviews) at the National Institute for Health Research and Centre for Reviews and Dissemination (CRD) at the University of York, UK (registration number CRD42020227327) (Link in Supplementary Materials). Design and reporting were conducted per the PRISMA Statement [29,30].
2.1. Inclusion Criteria
- ▪
- Studies conducted exclusively within the Indian context, from the onset of COVID-19 to its first peak and in its aftermath until 15 December 2020;
- ▪
- Primary studies of any research design;
- ▪
- Studies evaluating the impact of COVID-19 on the provision, utilisation, and availability of health services;
- ▪
- Studies exploring the health system’s response in terms of adaptations, interventions and efforts made in different types of health facilities for maintaining the continuity of services;
- ▪
- Studies examining the impact of the pandemic on individuals—health care providers, individuals with acute and chronic diseases.
2.2. Exclusion Criteria
- ▪
- Studies on pandemics other than COVID-19;
- ▪
- Studies that are not primary (such as reviews, reports, policy briefs, commentary etc.);
- ▪
- Global/multi-country studies with India just as one of the settings and studies not conducted in the Indian context;
- ▪
- Studies evaluating aetiology, pathophysiology, histopathology, serology or laboratory examination of COVID-19, clinical trials, or vaccine development;
- ▪
- Studies that are not written in English.
2.3. Search Strategy
We utilised the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to conduct a search of electronic databases. We electronically searched six databases, namely PubMed, MEDLINE, Embase, Global Health, CINAHL, and the WHO database on COVID-19, to identify primary studies employing quantitative, qualitative, and mixed methods. The search was limited to primary studies published in English until 15 December 2020. Our search approach employed a combination of Medical Subject Headings (MeSH), free-text terms, and word variants related to COVID-19, the health system, health services, communities, and community facilitators in the Indian context. In addition to the electronic databases, we also conducted a search on Google Scholar for relevant primary studies. Furthermore, we performed a snowball search to identify references from relevant papers. Detailed search strategies were developed for each electronic database. An illustration of the search strategy and search terms is given in Figure 1:
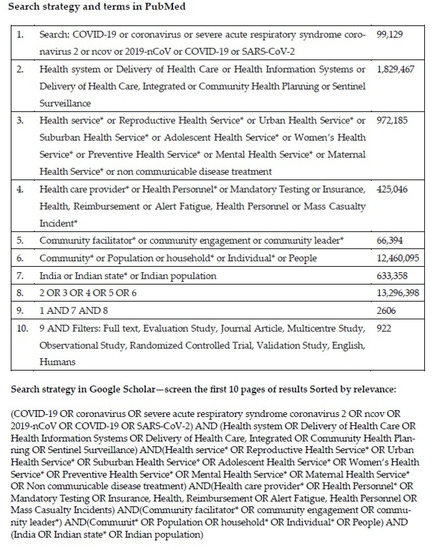
Figure 1.
Search strategy and terms in databases (PubMed and others) and Google Scholar.
2.4. Data Extraction (Selection and Coding)
The literature search results were meticulously organised and stored using the Mendeley reference management software. By importing the results into this software, we were able to seamlessly access full-text articles, annotate important information, remove duplicates, and effortlessly generate citations and a bibliography in the desired format [31,32,33,34,35]. Mendeley played a pivotal role in streamlining these tasks and optimising the management of the literature search results.
To maintain data integrity, we utilised the duplicate identification feature in Mendeley to identify and eliminate any redundant records. This step ensured that we worked with a unique set of unduplicated references. Subsequently, these unique records were imported into Covidence, a web-based systematic review software package developed by Veritas Health Innovation [36]. The two-stage screening process was then conducted in Covidence, facilitating collaboration among authors by providing an adequate platform to discuss and make study selections [37,38,39].
In the first stage of screening, the two authors independently assessed the titles and abstracts of the retrieved records against the predefined inclusion and exclusion criteria. This process helped us narrow down the selection to studies that potentially met the criteria.
Subsequently, all these studies selected in the initial screening stage underwent a thorough full-text screening process conducted independently by the two authors. During this second stage, the study design, relevance of the outcome measures and findings to the specified objectives of the review, and the targeted population were meticulously investigated. Based on this, thorough evaluation, final decisions were made on the inclusion of each study in the review. Studies that did not meet the inclusion criteria after the two-stage screening process were dropped from further consideration.
Any disagreements or uncertainties that arose during the review process were carefully addressed through discussions between the authors. In cases where specific issues required additional expertise, such as determining the exclusion of commentaries or perspectives, or assessing the relevance of outcome measures in the study to the objectives of the review, an independent reviewer was engaged to provide valuable insights and a fresh perspective. Covidence served as a crucial platform for documenting screening decisions, resolving conflicts, and ensuring transparency in our decision making. Its user-friendly interface and collaborative features facilitated effective communication and consensus-building among the authors.
Once the final set of included studies was determined using Covidence, we exported the relevant information required from the studies, including study characteristics and outcomes, into a structured and pre-developed data extraction form within an Excel spreadsheet [38,40,41,42]. This form consisted of columns representing the variables of interest. Two reviewers independently extracted the necessary data from each study and entered them into the corresponding cells of the spreadsheet. Data extraction form in Excel aided in the systematic and structured extraction and management of data from multiple studies, leading to a comprehensive and well-organised review.
2.5. Data Items
We meticulously extracted and structured the following information from the included articles, aligning it with the review’s stated objectives:
- Author name(s);
- Publishing journal;
- Study design;
- Location of the study;
- Targeted population;
- Sample size;
- Outcome measures and findings in the included studies related to the current review objectives:
- ▪
- Availability, provision, and delivery of health services mentioned in the studies: We extracted data on how the included studies discussed the availability and delivery of health services during the COVID-19 pandemic, addressing the first objective of our review.
- ▪
- Adaptations and changes in the health system, along with efforts undertaken: We organised information about the adaptations and changes made within the health system to cope with the pandemic and any efforts undertaken to ensure continued healthcare delivery in relation to the second objective of our review.
- ▪
- Impact on healthcare providers: Data related to the impact of COVID-19 on healthcare providers, including their working conditions, well-being, and any challenges faced, were collected, addressing the third objective of our review that takes into account healthcare providers.
- ▪
- Impact on the health, livelihood, and disease progression among individuals and communities: We documented the impact of COVID-19 on the health and well-being of individuals and communities, including effects on livelihood and disease progression, pertaining to the third objective of our review related to healthcare seekers.
- Limitations and recommendations
By organising the data in this manner, we could effectively analyse how the findings from the included articles related to the stated objectives, providing a comprehensive understanding of the impact of COVID-19 on the health system, healthcare providers, and individuals.
2.6. Outcomes
Considering the anticipated heterogeneity in the widespread impact of COVID-19 on the health system and its various components and stakeholders, attributed to a wide range of settings, medical conditions and specialities, types of health system responses, changes and adaptations, healthcare providers’ experiences, and healthcare seekers’ conditions, our review included studies reporting a broad range of outcomes, addressing the study objectives. Our primary focus was on studies examining the effects on at least one primary or secondary outcomes, listed below:
2.6.1. Primary
- Health services for varied health conditions:
- ▪
- Changes in the provision, utilisation, or availability of:
- ○
- Outpatient department (OPD);
- ○
- Elective health services;
- ○
- Emergency health services
pertaining to reproductive, maternal, and child health services, non-communicable diseases (cancer, cardiovascular diseases, diabetes, etc.), and other general or specific health conditions (orthopaedic, ophthalmic, neurological, etc.).
- Health system response to COVID-19:
- ▪
- Efforts and adaptations made in:
- ○
- General precautionary and infection prevention measures;
- ○
- Protocols and guidelines;
- ○
- Staff allocation, management, and training;
- ○
- Personal Protective Equipment (PPE);
- ○
- Physical infrastructure and resources.
These outcomes address objectives A and B of our review, which aim to assess the impact of COVID-19 on the provision, utilisation, and availability of health services in the Indian context and understand the health system’s response, including adaptations, interventions, and efforts for continuity and resumption of services.
2.6.2. Secondary
- Mental/psychological health of health care providers:
- ▪
- Depression, anxiety, and burnout;
- ▪
- Fear of infecting themselves and transmitting it to family members;
- ▪
- Financial repercussions.
- General health or disease conditions of health care seekers/individuals:
These outcomes pertain to objective C, focusing on evaluating the impact of COVID-19 and the health system’s response on individuals, encompassing both healthcare providers and healthcare seekers.
2.7. Critical Appraisal—Quality Assessment
Two reviewers (A.S.C., A.N.) appraised the included studies using two tools:
- CASP (Critical appraisal skills programme) checklist for qualitative (observational) studies [43,44,45]. This tool is commonly used for evaluating the quality and methodological rigour of qualitative studies. It helped us assess the appropriateness of the study design, data collection methods, data analysis, and the credibility of study findings in qualitative research studies included in the review.
- AXIS critical appraisal tool for cross sectional studies/surveys [46,47,48,49,50,51]. This tool is designed to assess the quality of cross-sectional studies or surveys. It helped us evaluate such studies included in the review on various aspects, including sampling methods, participant selection, data collection, and statistical analysis.
Both tools have been adapted for use in this review. The reviewers utilised the checklists to evaluate each included study’s design, conduct, and analysis, with a focus on addressing potential biases.
Any discrepancies in ratings on different questions/items between the two reviewers were thoroughly discussed, and consensus was reached for each checklist item. The quality appraisal was not a criterion for study inclusion; therefore, no studies were excluded based on the results of the appraisal.
2.8. Data Analysis
Due to the heterogeneity of the studies, a detailed narrative synthesis was employed to analyse and interpret the data based on the outcome measures. Narrative synthesis [52,53] refers to an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis. It adopts a textual approach to the process of synthesis to “tell the story” of the findings from the included studies. This narrative synthesis approach enabled us to thoroughly examine and comprehend the data, taking into account its diverse nature. It played a crucial role in identifying patterns and trends within the findings, allowing us to gain valuable insights from the varied studies without compromising their heterogeneity.
3. Results
3.1. Screening and Inclusion of Studies
From the screening of five databases—PubMed, MEDLINE, Global Health, EMBASE, CINAHL, and WHO COVID-19 Global literature on coronavirus disease—we identified 1477 records (Figure 2). Additionally, 74 records were retrieved and added from other sources, such as Google Scholar and references in the citations. After eliminating duplicates, we retained 1271 unique records. The duplication mainly occurred because certain articles were indexed in multiple databases. Subsequently, 526 studies were selected based on the initial screening of abstracts. The full text of these 526 articles was assessed in detail for adherence to eligibility criteria, resulting in 121 articles. Of these, 38 articles were included for narrative analysis, while 83 were excluded for not meeting the eligibility criteria.
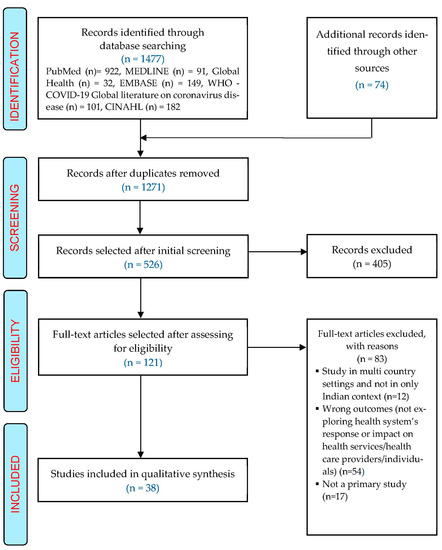
Figure 2.
PRISMA Flow diagram.
3.2. Narrative Analysis
The review comprises a total of 38 primary studies (Table 1) with a collective participant count of 22,502. These studies consist of 21 cross-sectional surveys, 16 observational studies, and one mixed-method study combining survey and observational approaches. They were conducted in diverse settings, including clinics, hospitals, and primary healthcare or community health centres, which might have affected the choice of the study design, targeted population, outcome measures, and, eventually, the findings in these studies.

Table 1.
Characteristics of Included Studies in Review—Authors, Areas of Work, Participant Types and Numbers, Settings/Contexts, Outcome Measures, and Findings from 38 Studies (in relation to review’s objectives).
The participants involved in these studies encompassed healthcare providers, including surgeons, doctors, nurses, and frontline workers as well as healthcare seekers, specifically patients. The findings derived from these studies have been meticulously analysed, interpreted, and categorised based on specific thematic areas.
3.2.1. Impact of COVID-19 and Turn of Events on Provision, Availability, and Utilisation of Health Services
- (a)
- Outpatient department (OPD) services
OPD services were described in 19 studies [54,55,56,57,58,59,61,62,64,65,68,69,72,74,77,79,80,82,86] involving 11,890 healthcare stakeholders. These studies covered various fields, such as oncology, neurosurgery, ophthalmology, maternal health, primary health care, general surgery, orthopaedics, and palliative care. All 19 studies reported a significant reduction in OPD services during the lockdown phase (March–May 2020), which persisted for several months thereafter. On further analysis, the reduction in these OPD services was statistically significant (p < 0.05 or <0.01), as reported in two studies [59,72]. Another study reported a staggering 97% decrease in OPD visits compared to the corresponding period in 2019 [74].
Among the OPD clinics at Primary Health Care sites, the greatest reduction was observed in noncommunicable diseases (NCDs) and immunisation clinics, while antenatal care services (ANCs) experienced lesser disruptions. General OPDs were the least affected [58].
Several included studies also reported the establishment and existence of Screening OPDs [54,55,57,74,77], where incoming patients were assessed for COVID-19-related symptoms and their travel history and underwent thermal screening and subsequent COVID-19 testing.
- (b)
- Elective services
Elective procedures are described in 16 studies [28,54,55,56,59,60,61,62,63,64,65,67,72,73,74,77] involving a total of 9268 subjects. These studies consistently report a significant impact on elective procedures across various areas of healthcare services, with procedures either being completely halted, significantly reduced, or deferred.
For instance, several studies focus on cancer care, all indicating a noteworthy decline, deferral, or even cessation of elective oncological procedures [28,54,62,64,73]. These procedures included radiotherapy [28,62], surgery, chemotherapy [62], tumour boards [28], and nutritionist consultations [28]. In cases where appropriate, such as advanced cases, deferrals were made to manage cancer through neoadjuvant chemotherapy [28,54].
Orthopaedics also experienced a similar trend, with the majority of elective surgeries being halted [63]. Many orthopaedic surgeons limited their practice to performing only essential trauma surgeries (62%) or ceased surgeries altogether (35%) during this period. Likewise, 93% of general surgical practices ceased all elective surgical procedures [59].
There was a significant decrease in vitreoretinal ophthalmological surgeries [67], with many of them being postponed [74]. Neurosurgery also witnessed a sharp decline, with approximately 70% fewer surgeries performed (p = 0.000) [72].
In the realm of maternal health services, a substantial 45% decrease in the number of deliveries was reported compared to pre-COVID-19 times, and this decline was statistically significant (p < 0.001) [61]. Furthermore, there were notable delays in service provision [77].
When it comes to cardiovascular diseases, there was a significant reduction in STEMI (ST-Segment Elevation Myocardial Infarction) admissions by 67% during the lockdown period compared to the pre-COVID-19 period. The reduction in NSTEMI (Non-ST-segment elevated myocardial infarction) cases was even more significant, reaching 93% within the same timeframe [60].
- (c)
- Emergency services
Emergency services are the subject of 20 studies [28,54,55,56,57,59,61,62,64,67,68,72,73,74,77,78,80,81,84,86] involving 12,850 healthcare stakeholders. These services encompass various specialities such as ophthalmology, maternal health, non-communicable diseases (including cardiovascular diseases, diabetes, and kidney diseases), neurosurgery, orthopaedics, injuries/trauma, and general surgical practice.
Overall, the majority of healthcare providers and institutions continued to deliver emergency and urgent services, taking necessary precautions and adapting protocols and techniques accordingly. However, the provision, utilisation, and availability of these services were impacted and altered due to challenges related to accessibility, transportation difficulties, infrastructural changes, resource constraints, and concerns arising from the lockdown. Consequently, these factors resulted in suboptimal medical care in life-threatening emergencies.
The changes and altered patterns of these services are described in several studies in different clinical areas.
In ophthalmological services [56], trauma cases accounted for the majority (51.9%), and a significant portion of doctors (83%) focused solely on emergency cases. Notably, there was a sharp 60% increase in home-related trauma cases during the lockdown, particularly among children. Despite this, the number of immediate surgical interventions among children has reduced (>80%) compared to pre-COVID-19 times, possibly due to difficulty in availing transport and poor access to healthcare facilities. Another study [74] also reported that the overall volume of surgical interventions was reduced, with only a small fraction of emergency interventions continued in cases of imminent risk of visual loss.
In cardiovascular diseases [60], there was an upsurge in acute coronary syndrome (ACS) patients presenting with delayed symptoms and mechanical complications. Similarly, in the context of diabetes [80], overall emergency services were reduced, with only individuals experiencing severe hyperglycaemia and recurrent hypoglycaemia receiving emergency consultations or services. Additionally, renal diseases witnessed a decline in the number of available dialysis stations and patients, and renal transplants both in the public and private sectors [86].
In cancer care also, despite an overall reduction in the patient load for gynaecologic cancers, a significant proportion of healthcare providers (69–92%) continued to provide treatment for emergency cases and advanced-stage emergency gynaecological cancers [64,73]. They adapted their approaches according to institutional protocols [73], shifting from minimal access surgery to conventional surgery, implementing neoadjuvant chemotherapy, and modifying radiotherapy protocols.
In obstetrics, there has been an increase in the volume of maternal and obstetric emergencies due to factors such as the reduced number of antenatal visits, delays in accessing services (due to travel restrictions), and waiting until the last moment due to infection fears [61].
In orthopaedics, approximately 21% had even ceased emergency surgeries entirely, and many surgeons were exclusively performing unavoidable emergency trauma surgeries (62%) [63].
3.2.2. Health System’s Response—Adaptations and Efforts for Resumption of Health Care Services
- (a)
- General precautionary and infection prevention measures
Ten studies [54,57,58,67,69,72,74,76,77,80] involving 5911 healthcare providers/seekers examined general precautionary and infection prevention measures.
There had been widespread implementation of some of the essential general precautionary and infection prevention measures, such as initial screening at entry, mandatory mask-wearing, and limitations on the number of attendants visiting or accompanying the patients [54,57,67,69,74,77].
Furthermore, additional infection prevention measures were implemented at various study sites [54,57,67,69,74,80]. These included providing hand sanitizers at accessible locations and displaying audio-visual notices at regular intervals to promote hand washing, mask usage, and adherence to social distancing norms. Furthermore, standing spaces were marked to maintain physical distance, adequately spaced sitting areas were designated, and surfaces were regularly sanitized.
Healthcare providers were reported to diligently implement infection prevention measures and take necessary precautions while delivering services. For instance, they frequently practiced hand sanitization using alcohol-based sanitizers, wore N95 masks, face shields, or safety goggles, utilised disposable gowns and gloves, employed double gowns when necessary, and set up dedicated ICUs for suspected COVID-19 cases [54,57,69,72,76,80].
While these precautionary measures were generally adhered to in most hospitals, they were significantly compromised at numerous primary healthcare centres [58]. For example, 76% of the sites lacked airborne infection control measures, 24% lacked adequate handwashing facilities for patients, and patient queuing averaged 14.1 individuals at many centres. Nevertheless, chemical disinfection of the PHCs was being undertaken at most (82%) sites with daily, alternate day, and less frequent disinfection reportedly conducted in 53%, 14%, and 20% of the sites, respectively.
- (b)
- Protocol and guidelines
To guide the operations, healthcare centres, hospitals, and clinics implemented various guidelines and protocols. The adoption and adherence to these diverse protocols and guidelines are discussed in thirteen studies [28,54,59,62,64,67,72,73,74,77,80,81,86], encompassing 8697 participants. Some institutions formulated or modified their guidelines based on existing literature and guidelines, while others followed state, national, or international guidelines.
For example, in two oncological studies [64,73], it was found that a significant majority of institutes and surgeons (69–75%) followed institutional or national guidelines, while the remaining (25% to 31%) adhered to international or alternative guidelines. This heterogeneity in the adoption and adherence to guidelines and protocols was further confirmed by a survey [86] conducted in 19 major hospitals, which reported variations among facilities in terms of adhering to the guidelines for testing SARS-CoV-2 issued by the Ministry of Health and Family Welfare (MoHFW) and the Indian Council of Medical Research (ICMR), with some institutions using their own protocols.
In another two oncological studies, cancer care hospitals [54,62] developed and implemented their own comprehensive protocols for all areas of work—general hospital, staff, preoperative, OT, postoperative, and emergency procedures—based on the limited available literature at the beginning of the pandemic. Similarly, a tertiary care centre formalised a diabetes treatment protocol for therapy modifications (escalations, de-escalations) and subsequently distributed it to all team members [80].
In obstetrics, a hospital formulated inpatient management protocols for both antenatal and intrapartum patients based on the national and international guidelines from organisations such as the International Federation of Gynaecology and Obstetrics (FIGO), the Centres for Disease Control and Prevention (CDC), and the World Health Organisation (WHO) [77]. These protocols encompassed various aspects, including communication pathways and transport protocols in the operating theatre. Many others modified or adapted the guidelines and protocols in different areas in an effort to continue operations [28,67,81]. On the other hand, in an ophthalmological study, surgeons kept adhering to the guidelines and precautions advised by The All India Ophthalmological Society (AIOS) [74].
After the initial phase, within 3–4 months of the pandemic (May–June 2020), the majority of healthcare facilities had implemented protocols for reopening services in the “new normal” situation. However, despite the availability of these protocols and guidelines, a significant proportion (60%) of healthcare providers expressed a lack of scientific evidence supporting the guidelines [54,62,72,73,86]. This absence of specific protocols also contributed to the stress experienced by healthcare workers, highlighting the urgent need for evidence-based protocols [54,72]. For example, a significant majority (71.5%) of surgeons expressed the explicit need for guidelines addressing safety measures for future surgical practices and providing solutions to mitigate the aftereffects of the pandemic [59].
- (c)
- Staff allocation, management, and training
Sixteen (n = 16) studies [54,55,57,58,62,66,67,68,70,72,74,76,77,80,82,86] involving 11,408 healthcare stakeholders provide valuable insights into staff allocation, training, and management during the peak of the pandemic. These studies shed light on the various measures implemented to enhance the efficiency of human resources and prevent the transmission of infection.
To effectively respond to the crisis, healthcare facilities established initiatives such as creating a dedicated COVID-19 action group, implementing staff rotation with different teams working in shifts, and dividing the workforce into separate groups for COVID-19 and non-COVID-19 patients [54,62,67,82]. Some studies also highlighted the adoption of reduced staffing strategies to preserve the workforce and prevent fatigue in hospitals and clinics [55,67,72,74]. A study in neurosurgical department revealed that all out-station leaves of healthcare workers were suspended to prevent community spread and ensure the maximum availability of the workforce [55]. Physical meetings in the hospitals were either cancelled or replaced by virtual meetings [54,55] and remote work was authorised for clinical, resident, and support staff [55]. Staff members arriving from areas declared as containment zones were granted paid leaves to mitigate the risk of cross-infection [54]. Furthermore, operation theatres were observed to operate with minimal staff, organised into teams or shifts [67].
Despite these measures, there have been instances of human resource constraints reported to have weighed heavily on the teams when vulnerable (older, pregnant) staff were relieved from high-risk duties [66]. The existing staff faced the challenge of balancing their time between designing and implementing new interventions and providing essential care.
Furthermore, quarantining staff as per infection prevention guidelines also contributed to the availability of lesser staff at any given point. Both private and public healthcare providers underwent adequate quarantine measures in cases of incidental exposure or if they were working in isolation wards or had any form of exposure to COVID-19 [54,62,67,68,76,77,80,82,86]. One study [62] explains that all the staff was divided into two groups, working at different times, and strict precautions were taken to ensure no overlap between these two groups. If any staff or patient turned positive for COVID-19, the entire group was quarantined and tested.
Training and workshops played an integral role in enhancing staff efficiency, ensuring adherence to protocols, preventing COVID-19 infections among personnel, and delivering comprehensive care to both COVID-19 and non-COVID-19 patients.
As underscored in several studies [55,57,58,62,66,77,80], the training related to infection control, sanitization, PPE Kit, donning and doffing of PPE, and the management of COVID-19 patients as per protocols were made mandatory for all staff and doctors at institutions. Even in primary health centres, the training related to the safe and effective management of patients with presumptive COVID-19 had been provided at approximately 78% of the sites to the health staff [58].
In several instances, the training and meetings were conducted online, including webinars [55,70,80], and information about guidelines and management protocols for COVID-19 widely disseminated in closed groups formed, aided by social media [77].
Furthermore, a study [80] demonstrated the practical and effective approach of training and engaging para-clinical doctors in providing diabetes care and COVID-19 information through underused telemedicine. The study further recommends extending similar efforts to address other chronic conditions like hypertension and asthma by training and building the capacity of more such teams of doctors. Also, this strategy can be adapted at other resource-limited centres facing challenges in delivering patient care services for non-COVID-19 illnesses such as diabetes, cardiovascular diseases, and more during the pandemic [80].
Another study [70] reporting burnout among HCPs stresses that HCPs should be provided information, instructions, training, and technical updates on COVID-19 through frequent communication to curb fear and burnout.
- (d)
- Personal Protective Equipment (PPE)
This analysis encompasses 22 studies involving 15,144 participants [27,54,55,56,57,58,59,61,62,64,65,66,68,69,70,72,73,74,76,77,78,86], which delve into the use and challenges of Personal Protective Equipment (PPE) among healthcare providers (HCPs) during consultations, surgeries, and other healthcare services. While the adoption of PPE became widespread, specific instances, predicaments, and challenges have been identified.
A common-sense, rationed approach to using resources like PPE during a pandemic of this magnitude is being followed cautiously in India and worldwide. Most practitioners felt that complete PPE needed to be reserved for workers dealing with high-risk patients [58]. While this seems to be a reasonable approach, many argue that primary care providers are also known to be at an increased risk, especially during epidemics. If the allocation of PPE limits the provision of N95 masks to only those HCPs directly involved in the management of confirmed COVID-19 cases, HCPs in resource-constrained settings working in enclosed small spaces without adequate ventilation and likely overcrowded are rendered highly vulnerable to COVID-19 in the absence of adequate PPE provision. Unfortunately, only half of the medical colleges and institutions provided N95 masks to healthcare providers at their primary health care facilities. PPE suits, N-95 masks, and surgical masks were available at only 27%, 50% and 39% of primary health care sites, respectively [58].
Furthermore, the unavailability and short supply of adequate quality PPE were widespread concerns reported in a plethora of included studies [27,54,58,64,68,72,76,77,78,86]. Supply chain disruptions and increased demand contributed to these shortages of PPE [78,86]. In response, a major tertiary care COVID-19 hospital resorted to procuring maximum PPE kits using administrative funds or donor liaison to address the heightened demand [77].
While the health system grappled with supply and demand issues, several studies highlighted the need for better quality and additional quantities of PPE. For instance, studies involving ophthalmologists, oncologists, and neurologists indicated a preference for wearing additional PPE during surgeries [28,56,62,72] to ensure adequate protection. However, even with full PPE, medical personnel were not always spared from infections [65], raising concerns about the quality of PPE. A survey of neurosurgeons revealed that nearly 40% were dissatisfied with the available PPE’s quality [78]. Another study [54] emphasised the increased need for better protective equipment, particularly amongst surgeons during operations. Additionally, an alarming 34% of surveyed neurosurgeons [72] had not operated in PPE, and among those who did, most (42%) felt it negatively impacted their surgical performance, underscoring the vital need for comfortable and high-quality PPE during complex neurosurgeries that demand significant finesse, concentration, and time. This predicament left surgeons grappling with the dilemma of either risking infection or compromising their surgical performance due to inadequate PPE [72]. Despite these quality concerns, ensuring quality control was challenging due to variations in suppliers and excessive demand [78].
Several other studies shed light on the challenges associated with donning PPE, especially during surgical procedures. Operating in PPE resulted in constant misting of eyewear/face shields [77], extreme heat/dehydration [66,77] and difficulty in breathing [78]. Respondents in different studies indicated limited tolerance periods for wearing PPE, ranging from 2 to 4 h at most [66,76,78]. In some slum clinics, health workers were provided with reusable water-resistant PPE. However, disinfecting these PPEs in the confined space of the slum clinics posed additional challenges [66].
- (e)
- Preoperative/OT/post-operative measures
Twelve studies [28,54,55,56,59,62,64,67,72,73,78,82,83] provide insights into preoperative, intraoperative, and postoperative measures, involving a total of 3814 participants. Several studies consistently emphasised the necessity of COVID-19 testing for all preoperative patients, ensuring that only those testing negative for the virus proceeded with surgeries [55,78,82]. However, at the onset of the pandemic, there was significant uncertainty and scepticism surrounding preoperative procedures. For instance, an early study [56] revealed that the majority of clinicians (63%) were uncertain about the appropriate course of action and were eagerly awaiting guidelines regarding preoperative screening. Another study [64] highlighted a similar predicament during the initial phase, as the recommendations by the Government of India did not initially allow for preoperative COVID-19 testing, making it challenging to make decisions regarding surgery based on COVID-19 status.
Furthermore, there was no consensus among practitioners regarding the number of negative COVID-19 tests required preoperatively [72]. Before emergency surgery, 63% did not perform any testing, 35% performed 1 test, and 2% performed 2 tests. For elective surgery, 65% required one negative test, while 23% needed two negative tests [72]. This ambiguity surrounding preoperative testing and procedures was widely observed during the early stages of the pandemic.
At some institutions/clinics however, testing became an essential prerequisite criterion [55,78,82]. As a result, delays in surgeries were common, with an average delay of 3.22 days (±0.26) reported in one study [82]. Hospitals without dedicated COVID-19 operation theatres allowed surgeries only for patients with negative test results, especially those from containment zones. In another study [78], 54% of institutions performed pre-admission testing, and over 85% of respondents believed preoperative testing and screening of asymptomatic individuals were crucial to reduce in-hospital transmission among healthcare workers.
In addition to preoperative testing, certain institutions implemented changes in their surgical strategies and techniques. For instance, an ophthalmological study reported modifications in their operation theatre (OT) sterilisation protocol [67]. Furthermore, some surgeons adopted the use of a “heads-up” 3D visualisation system during vitreoretinal surgery to increase the distance between the surgeon and the patient, thereby minimising the risk of exposure. Additionally, in several settings, strict precautions were taken upon admitting patients, allowing only one attendant [54,72,82].
In the field of oncology, studies highlighted the adoption of neoadjuvant chemotherapy as an alternative to upfront surgery, deviating from the standard of care but serving as a viable option during resource-constrained times of the pandemic [28,54,62,73,83]. For instance, in one of these studies, elderly and frail patients with operable lesions, who were at a higher risk at COVID-19 infection were advised to either wait or undergo neoadjuvant therapy [62]. Furthermore, surgeries for pre-invasive lesions and slow-growing cancers were postponed, and only life-saving procedures were performed at most healthcare facilities. Other cases were either kept under observation or considered for neoadjuvant therapy, specifically for carefully selected eligible cases [28,54,62,73,83].
In the realm of neurosurgical procedures, certain adaptations were made to minimise exposure risk. Some surgeons avoided craniotomy whenever possible, while others opted not to use drills and adopted the practice of wearing two gowns, removing the outer gown after 20 min following craniotomy to minimise contamination [72]. In general surgical practice also [59], various adaptations were implemented to reduce the risk of infection, including the use of Hydroxychloroquine (HCQ) for chemoprophylaxis, considering open surgery, and using filters for desufflation.
- (f)
- Physical infrastructure and resources
Twenty studies [54,55,56,57,58,59,61,62,63,64,66,69,72,73,74,77,80,82,84,86] involving 12,409 subjects have documented various modifications made to infrastructure and resources. The primary objective of these changes was to create COVID-safe environments in buildings, wards, operating rooms (ORs), and other facilities. For instance, several studies emphasise the allocation of separate buildings, units, or wards exclusively dedicated to managing or treating COVID-19 patients [54,72,77,86]. Additionally, engineering controls, such as physical barriers, curtains, or partitions [72,77], were put in place to reduce exposure risk and contamination. Healthcare facilities also established distinct and regulated entry and exit points for both patients and healthcare providers [54,58,77], set up special screening areas near the entrance of the hospital [54,58,62,77], and designated separate areas for donning and doffing personal protective equipment (PPE) [62,77].
Efforts were also made to ensure physical distancing, with sitting and standing areas properly marked and spaced [54,58]. In addition, a minimum distance of 1.5–1.8 m was maintained between beds [62,77], and the number of patients in waiting areas, common spaces, elevators, wards, and operating rooms was limited and regulated to prevent overcrowding [54,62]. Healthcare facilities prioritised environmental cleaning, proper ventilation, air conditioning, and air filtration in areas such as wards, ICUs, and operating rooms [54,77]. For example, one study reported the maintenance of adequate air exchange rates in ORs, with the use of high-efficiency particulate air filters for ultra-filtration, strict fumigation after each case, and suction to evacuate smoke and ensure clean air and ventilation.
A health care clinic in slums [66] also improved ventilation by relocating consultation rooms to open spaces to reduce the risk of viral transmission. However, challenges persisted as patient registration, laboratory work, and dental procedures were still conducted in rooms with compromised ventilation, leading to long queues and waiting times. Another study [58] assessing primary health facilities also highlighted inadequate ventilation, suboptimal infrastructural capacity and a lack of separate entries, hindering physical distancing efforts at most PHCs.
Besides these adaptations, several changes were made in the processes. For instance, surgical procedures in operating rooms were spaced out with sufficient time intervals to ensure proper sterilisation [54,62]. Solutions were implemented to cohort COVID-positive patients or suspected cases, including the creation of isolation rooms, dedicated machines and dedicated shifts [72]. Furthermore, adjustments were made to resources, such as increasing the hospital’s oxygen capacity and arranging more beds with oxygen ports and supply in response to the increased demand for oxygen during the COVID-19 pandemic [77]. Further efforts were increased for procuring ventilators, non-invasive options (HFNO and BiPAP) and other respiratory support devices [77].
Furthermore, telemedicine experienced widespread and varied adoption, enabling healthcare providers to extend their reach to patients in diverse medical specialities [55,56,57,59,61,63,64,66,69,72,73,74,80,82,84,86]. It facilitated remote consultations, follow-ups, and monitoring, minimising the need for in-person visits and reducing the risk of exposure in varied healthcare settings. It proved to be a valuable tool in ensuring continuity of care for patients while adhering to safety measures during the pandemic.
3.2.3. Impact of Pandemic on Healthcare Providers and Individuals/Communities
- (a)
- Impact on health care providers (HCPs)
- ▪
- Depression, stress, anxiety, and burnout in health care providers (HCPs)
Fourteen studies [27,54,56,58,62,65,66,68,70,71,72,75,76,78] involving 8568 participants examined the mental health status of HCPs during the pandemic, revealing a significant prevalence of pandemic-related stress and burnout among them.
Approximately 33% to 35% of HCPs [75,76] experienced depression, surpassing the prevalence of 10% for common mental disorders in the general population of India [89]. The mean score of pandemic-related burnout in HCPs [68] was significantly higher than both personal and work-related scores (51.37 vs. 49.7 and 39.7, respectively, p < 0.05). Additionally, HCPs working in high-risk hospital environments demonstrated a significantly greater prevalence of work-related (27.8% vs. 21.2%, p < 0.01) and pandemic-related burnout (53.9% vs. 45.6%, p < 0.01). Other studies have also documented varying degrees of depression, stress, anxiety, and burnout among HCPs working in different specialities [27,58,66,78].
Among front-line COVID-19 doctors [71], the prevalence of depression and stress symptoms was much higher, with rates reaching 64% and 45%, respectively. Another study [66], which focused on front-line health workers in slums, highlighted the enormous emotional and physical toll they experienced. These workers not only put in long hours fully clad in PPE but also faced additional challenges, such as clashes and violence due to limited economic activity among slum dwellers during the pandemic. Furthermore, the population’s resistance to adhering to safety measures like wearing masks and following clinic protocols added to the difficulties faced by them.
Numerous factors contributed to stress and anxiety among HCPs [27,54,56,58,62,66,68,70,71,72,75,76,78,86] to varying degrees, including the fear of contracting COVID-19 due to extreme proximity during treatment, anxieties regarding the availability of sufficient PPE, and the physical strain of working long hours in protective gear. Loneliness during quarantine, difficulties in maintaining social connections, and the challenges associated with routine tasks (OR, OPD, and IPD works) also took a heavy toll on their well-being. Additionally, insufficient guidelines and knowledge gaps, limited administrative support, financial losses, and staff shortages further exacerbated the burden they experienced.
- ▪
- Fear of contracting infection and carrying it at home
The fear of contracting and transmitting the infection has been addressed in nine studies [27,54,56,62,66,70,75,78,86], involving 9490 participants. Among HCPs caring for COVID-19 patients, approximately 55% expressed fear of contracting the infection themselves, while an even higher percentage (67%) feared transmitting it to their families [70].
A separate study [27] conducted across ten states and one union territory revealed that a significant majority of HCPs (78%) experienced serious apprehensions about infecting their friends or family members. Likewise, healthcare workers in the community health division of a hospital serving a large slum area [66] emphasised their primary concern of transmitting the infection to vulnerable family members, including the elderly, immune-compromised individuals, and those with chronic medical conditions.
Notably, this fear of transmitting the infection to families and close ones was even identified as a cause of depression among HCPs in some studies [27,75]. Furthermore, certain specialities [56,78], such as ophthalmology and neurology, perceived a higher risk of contracting COVID-19 while examining and treating patients, leading to the requirement for additional protective gear compared to other specialities.
- ▪
- Stigmatisation
Stigmatisation targeting healthcare providers (HCPs) has been documented in five studies [62,66,70,75,76], involving 5173 participants. A significant proportion of HCPs in a comprehensive survey (26.6%) reported feeling unwelcome in their communities [70]. The studies conducted in both community and hospital settings [62,66,76] highlighted that healthcare workers were perceived as carriers of infection and often faced ostracisation from friends, neighbours, and society as a self-protective measure. This stigmatisation had negative impacts on the mental well-being of HCPs, leading to feelings of depression, stress, and anxiety [70,75,76].
- ▪
- Financial impact
The financial impact of the pandemic on healthcare practitioners is documented in five studies [27,54,59,63,75], involving 3489 participants. A survey revealed that a significant majority (82%) of healthcare providers experienced financial harm due to the pandemic [72]. In another study [59] over 50% of the healthcare providers reported a decrease of more than 75% in their monthly income, while 22% faced a 50–75% reduction.
The financial burden was particularly pronounced among private practitioners and those with multiple affiliations compared to those in government jobs (p = 0.000) [59,63,72].
Notably, approximately 28% and 33% of respondents who owned hospitals expected their income to decline by more than 90% [63] and anticipated a monthly financial liability of $30,000 [59], respectively. Surgeons with more years of practice, specifically those with 20 to 30 years or more than 30 years of experience, were particularly affected compared to their younger counterparts [63].
Some other studies [54,63,75] revealed that the decreased income from practice poses significant implications on their financial sustainability, career, and quality of training, prompting many to consider changing their financial strategies in response to the challenges posed by the pandemic.
- (b)
- Effect of pandemic on healthcare seekers
Thirteen studies [26,57,61,62,69,74,79,82,83,85,86,87,88] involving 11,371 participants examined the effects of the pandemic on the physical and mental health of individuals. These studies highlighted various impacts on disease progression, disease status, lifestyle factors such as physical activity and diet, and medication adherence.
Specifically, among diabetic patients, there was an observed increase in missed insulin doses (27%) [79], irregular blood glucose monitoring (28–39%) [79,85], reduced engagement in regular physical activities (37%) [79], and decreased compliance with dietary guidelines (17%) [79]. The unavailability of insulin injections [79] and Self-Monitoring Blood Glucose (SMBG) machines/strips [85] during the lockdown was reported to have contributed to missed insulin doses and irregular blood glucose monitoring. As a result, average blood glucose and HbA1c levels were elevated, hyperglycaemic episodes increased (37%), and there was a higher incidence of Diabetic ketoacidosis (DKA) and hospitalisations (8%) [79] among these patients. Besides, an increased risk of type 2 diabetes was also observed among non-diabetic people [87] owing to weight gain and an elevated diabetes risk score.
In the case of cancer patients, they encountered numerous challenges, such as limited availability of chemotherapy slots (56%), long waiting hours despite scheduled appointments (22%), postponed surgeries (14%) and tumour board meetings (20%) [57,82,83]. Teleconsultations and nutritionist advice were also significantly delayed (42% and 89%, respectively), and there was a concerning shortage of chemotherapy medications (22%) [57,82,83]. Most of the patients (68%) wanted their chemotherapy to continue despite the pandemic, emphasising their deep concerns about cancer progression, outweighing their fear of contracting SARS-CoV-2 [83].
In obstetric complications [61], a surge in the number of high-risk pregnancies (by 7.2% points) and aggravation in one or more complications (44.7%) was observed owing to the delay in seeking health care. The reason for the delay in health-seeking was either the strict lockdown and lack of transportation or avoidance of visits due to the fear of catching infections. Anaemia was overlooked in most women, followed by pregnancy-induced hypertension. Many women opted to wait at home for labour or choose home deliveries, contributing to adverse outcomes such as eclampsia, acute renal failure, sepsis, and pneumonia.
Patients across multiple studies [61,62,79,82,83,88] expressed widespread fear due to the increased risk of infection associated with their existing conditions. They were concerned about the potential deterioration of their underlying diseases as a result of delayed or suboptimal treatment. Apart from the fear of adverse outcomes, patients also reported challenges such as limited guidance from healthcare professionals [82], shortages of essential medications and donors [69,74,79,82], escalating costs of planned medical procedures [58], higher expenses for hospital visits [57,62], and the need to travel long distances to access medical care, putting their immunocompromised state at risk [57]. These factors contributed to heightened anxiety and stress among the patients.
Furthermore, transportation and travel issues significantly impacted patients seeking treatment during the lockdown period [57,61,62,69,74]. The unavailability of public transport, limited access to fuelling stations, and the need for permissions under strict lockdown measures compounded the difficulties patients faced in reaching hospitals. Moreover, the conversion of public hospitals into COVID-19 care centres further hindered access to treatment, especially for individuals from low to middle socioeconomic backgrounds who depend on the public sector for healthcare services [86].
The fear of job loss and financial hardships [57,79,82,88], feelings of loneliness and boredom [88], the worsening COVID-19 situation, adherence to strict lockdown measures [26,62,85], and the increasing reach of television and online news and media [62] all contributed to the heightened concerns and had a significant impact on the mental well-being of the patients. Furthermore, the unavailability of peer group support services and psychological counselling sessions [82] and the restrictions on visitors/attendants exacerbated their challenges [82].
Physical activity levels [69,87,89] were found to decrease during the pandemic due to various factors such as lack of motivation, limited time availability, and restricted access to parks, dance studios, and fitness centres. However, some individuals adapted by incorporating physical activities within their homes. In terms of dietary habits, there were observed improvements or maintenance [85,88] driven by concerns related to COVID-19. Many individuals developed a preference for home-cooked food and reduced eating out and socialising, aiming to minimise the risk of exposure to the virus.
3.3. Quality Appraisal of Included Studies
Among the 16 observational studies, the overall quality ranges from high to low. Specifically, 13 studies are rated as high quality, 3 studies are considered to be of moderate quality, and 1 study is assessed as low quality. Similarly, among the 21 cross-sectional surveys, the overall quality varies from high to low (Appendix A.1). Of these surveys, 11 are classified as high quality, 9 are deemed to be of moderate quality, and 2 are evaluated as low quality (Appendix A.2). In addition, there is 1 mixed-method qualitative study that incorporates both observational methodology and cross-sectional survey components. This study undergoes assessment using both tools and is determined to be of high quality.
4. Discussion
This review examines the impact of COVID-19 on health services and the health system’s response in India during the first wave and its aftermath. It explores the initial stumbling and disruption of the system, highlighting sudden and urgent instances of imbalance, resource strain, and coordination challenges as the first objective of the study. It also sheds light on subsequent adaptations and efforts that were made with a sense of urgency to effectively address COVID-19 while at the same time striving to maintain and deliver essential health services, addressing the second objective of the study. It also reflects upon the challenges faced by healthcare providers and seekers, in relation to the third objective of the study. The review offers valuable lessons for future preparedness and identifies areas for improvement in building a resilient healthcare system capable of managing similar sudden and unprecedented crises.
This review is based on primary studies conducted in different Indian health care settings to keep the analysis based on robust research and first-hand evidence.
Highlighting the impact on the provision, utilisation, and availability of health services, consistent findings across multiple studies included in this review indicate a significant reduction in outpatient department (OPD) services [54,55,56,57,58,59,61,62,64,65,68,69,72,74,77,79,80,82,86] during the initial lockdown phase and subsequent months. Notably, among the OPD clinics at the Primary Health Care sites, noncommunicable diseases (NCDs) and immunisation clinics were particularly affected, while ANC services and general OPDs experienced relatively fewer disruptions [58]. Elective procedures across diverse healthcare areas were either completely halted or significantly scaled back, leading to delays and postponements in treatment [28,54,55,56,59,60,61,62,63,64,65,67,72,73,74,77]. Despite these challenges, emergency services persevered, albeit with difficulties in accessibility, transport, and resource constraints [28,54,55,56,57,59,61,62,64,67,68,72,73,74,77,78,80,81,84,86].
These findings align with a comprehensive survey conducted by the World Health Organisation (WHO) across 155 countries during a similar time frame, which highlighted severe interruptions in prevention and treatment services for non-communicable diseases (NCDs) as countries transitioned from sporadic cases to community transmission of the coronavirus [90].
A comprehensive systematic review conducted in multi-country settings [91] during that time further substantiates our findings, revealing a significant reduction in healthcare utilisation across various populations and countries. This reduction was particularly pronounced among individuals with less severe illnesses, in line with our observation of disrupted elective and essential services for less severe conditions, which experienced substantial declines. Conversely, emergency services for severe illnesses persisted, albeit with necessary adaptations. Furthermore, a study [92] conducted in the United States provides additional support for these findings, demonstrating a marked decrease in medical admissions during the COVID-19 outbreak in March and April 2020 across diverse patient groups. The study also emphasises the significance of long-term research to fully understand the implications of avoiding hospitalisation during the pandemic on patients’ mortality, morbidity, and quality of life, a consideration extensively discussed and observed in the included studies of this review.
In addition to evaluating the impact on health services, our study sheds light on the level of preparedness and various adaptations undertaken by healthcare facilities, addressing the second objective of the study. These adaptations encompassed changes made in precautionary and infection prevention measures [54,57,58,67,69,72,74,76,77,80], protocols and guidelines [54,59,62,64,72,73,74,77,81,86], staff and resource management [54,55,58,62,66,67,68,70,72,74,76,77,80,82,86], PPE [27,54,55,56,57,58,59,61,62,64,65,66,68,69,70,72,73,74,76,78,86], preoperative/OT/post-operative measures [28,54,55,56,59,62,64,67,72,73,78,82,83] and infrastructure [54,58,62,66,72,77,86], demonstrating the proactive measures taken to respond to the challenges posed by the COVID-19 pandemic. These findings from our review are consistent with studies conducted in different settings and geographies during this phase of the pandemic. For instance, a study in Ireland found that healthcare infrastructures were reconfigured to facilitate the pandemic response, including the construction of structures to separate patients and the strengthening of triage systems [93]. Similarly, an analysis of datasets and literature reviews in England showed that hospitals implemented interventions to manage patient admissions and increase resource availability, including the cancellation of elective surgeries and the deployment of additional medical personnel [94]. Likewise, a National Survey conducted in the US reported comparable adaptations such as the establishment of dedicated respiratory isolation units, expanded use of inpatient telehealth, and strategies to minimise room entry [95]. These consistent findings highlight the similar efforts made to address the challenges posed by the pandemic across various healthcare settings.
Furthermore, the aforementioned survey [95], a large-scale study conducted in nursing homes across the US [96], and a prospective observational cohort study [97] conducted in both the UK and the US focusing on frontline healthcare workers, all highlighted the concerning insufficiency of personal protective equipment (PPE) and the widespread practice of reusing PPE. These findings closely align with the conclusions drawn from our review, emphasising the critical shortage of PPE and the desperate need to reuse it.
Addressing the third objective, which focuses on the impact on healthcare providers [27,54,56,58,62,65,66,68,70,71,72,75,76,78], a significant finding of our study is the prevalence of pandemic-related stress and burnout among healthcare providers (HCPs). HCPs, (including doctors, nurses, paramedics, and administrative staff), who cared for COVID-19 patients, feared contracting and transmitting the infection to their families. Similar findings have emerged in other studies conducted in diverse multi-country settings. For instance, an observational cohort multicentre study in acute hospital settings in the South-East of Ireland [98] highlighted the scarcity of research focusing on mental health issues during the pandemic and found a notable prevalence of psychological distress among HCPs in those settings. On similar lines, a systematic review during the time in selected Asian countries [99] examined viral epidemic outbreak studies and concluded that the prevalence of anxiety, depression, acute and PTSD, and burnout was high during and after outbreaks; with problems having a long-lasting effect on the mental health of HCPs.
Furthermore, our study observed instances of stigmatisation against HCPs, which is consistent with the statement released by the International Committee of the Red Cross (ICRC) [100], reporting over 600 incidents of violence, harassment, or stigmatisation targeting healthcare providers, patients, and medical infrastructure in relation to the COVID-19 pandemic.
While the review highlights the research and evidence-based picture of the challenges posed by the pandemic and the response to it, it is crucial to acknowledge the inherent limitations within the primary studies included. These studies were conducted during the early stages of the pandemic, necessitating careful consideration of the spatial and temporal aspects of the findings. Extrapolating the review’s findings to a different time period or phase of the pandemic may contradict them and limit their generalisability. Furthermore, the contextual nature of the findings within Indian settings prevents their direct applicability to other countries.
The majority of the studies aimed to assess changes in the status of health services across different health conditions and levels, considering the immense and sudden pressures faced by the health system. Due to the rapidly evolving situation, limited attention was given to meticulous sample selection methods and research study design. Consequently, all the studies relied on cross-sectional surveys with purposefully selected samples. While this approach may have compromised the robustness of the evidence collected, it effectively captured the sudden impact of the pandemic on various health services, especially when timely evidence was crucial for interventions. Additionally, the study faced other limitations, including the inability to conduct a meta-analysis due to significant heterogeneity in the included studies, the potential exclusion of important data sources such as studies with smaller sample sizes, reports, and subjectivity in our outcome assessments.
5. Conclusions
In conclusion, this study sheds light on the profound and sudden impact of COVID-19 on health services during the initial wave, resulting in disruptive effects on OPD and elective services and raising concerns about suboptimal emergency care. The healthcare system promptly responded by implementing quick and possible adaptations in staff management, resource allocation, and infection prevention. These valuable findings and insights provide essential knowledge to enhance our understanding of the necessary measures, approaches, and level of preparedness required to build resilient health systems. Incorporating these insights into future strategies will ensure that the health system is well-prepared and resilient in effectively addressing similar crises proactively.
Furthermore, the study underscores the significant toll on the mental health and well-being of healthcare providers, who endured unparalleled challenges and resource constraints. It also illuminates the widespread concerns and fears amongst healthcare seekers, particularly regarding the worsening of their underlying diseases or conditions due to significant delays, formidable barriers, and suboptimal services for diagnosis, treatment, and follow-up.
To mount an effective response to future similar emergencies, it is imperative to prioritise the readiness and preparedness of the health system. This involves adopting agile and efficient strategies to strengthen healthcare infrastructure, optimise resource allocation, and implement comprehensive protocols. Addressing the concerns of healthcare seekers during emergencies and implementing measures to support healthcare providers are vital. By placing emphasis on these aspects, we can proactively enhance the resilience of the health system, ensuring improved outcomes in times of crisis.
Supplementary Materials
The protocol registered on PROSPERO can be downloaded at: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=227327 (accessed on 24 June 2023).
Author Contributions
Conceptualisation, A.S.C., K.S., R.B. and S.K.; methodology, A.S.C., K.S., R.B. and S.K. software, A.S.C. and A.N.; validation, K.S., R.B. and S.K.; formal analysis, A.S.C. and A.N.; investigation, A.S.C. and A.N.; resources, K.S., R.B. and S.K.; data curation, A.S.C. and A.N.; writing—original draft preparation, A.S.C.; writing—review and editing, A.S.C., K.S., R.B. and S.K.; visualisation, A.S.C. and A.N.; supervision, A.S.C., K.S., R.B. and S.K.; project administration, A.S.C., K.S., R.B. and S.K.; funding acquisition, A.S.C. and K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Asian Development Bank (47354-003).
Institutional Review Board Statement
This review is a part of research approved by Human Research Ethics Committee-Ethics committee of Delhi—Sigma-IRB (Institutional Review Board)-IRB Approved date/number—14.12.2020/10044/IRB/D/20-21.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this review are derived from published literature and publicly available sources. No additional data sets were generated or analysed specifically for this review. All references and sources cited in this review are provided for transparency and accessibility.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Appendix A.1. Quality Appraisal of Observational Studies Using Adapted CASP Checklist
| S.No. | Studies | Was There a Clear Statement of the Aims? | Is a Qualitative Methodology Appropriate? | Was the Research Design Appropriate to Address the Research Aims? | Was the Recruitment Strategy/Sampling Appropriate to the Aims of the Research? | Was the Data Collected in a Way That Addressed the Research Issue? | Has the Relationship between Researcher and Participant been Adequately Considered? Research issue? | Have Ethical Issues been Taken into Consideration? | Was the Data Analysis Sufficiently Rigorous? | Is There a Clear Statement of Findings? | Do the Conclusions Drawn in the Research Report Flow form the Analysis or Interpretation of the Data? | Quality Assessment |
| 1 | Goyal N et al. [55] | x | x | x | x | x | x | x | x | x | x | High |
| 2 | Singh M et al. [57] | x | x | x | x | x | x | x | x | Medium | ||
| 3 | Choudhary R et al. [60] | x | x | x | x | x | x | x | x | High | ||
| 4 | Goyal M et al. [61] | x | x | x | x | x | x | x | x | x | x | High |
| 5 | Deshmukh, S [62] | x | x | x | x | x | x | x | x | Medium | ||
| 6 | Gupta A et al. [64] | x | x | x | x | x | x | x | x | x | High | |
| 7 | George CE et al. [66] | x | x | x | x | x | x | x | x | x | x | High |
| 8 | Agarwal D et al. [67] | x | x | x | x | x | x | x | x | x | High | |
| 9 | Khurana DK et al. [69] | x | x | x | x | x | x | x | x | Low | ||
| 10 | Babu N et al. [74] | x | x | x | x | x | x | x | x | x | High | |
| 11 | Mahajan NN et al. [77] | x | x | x | x | x | x | x | x | x | x | High |
| 12 | Verma A et al. [79] | x | x | x | x | x | x | x | x | x | x | High |
| 13 | Jain A et al. [81] | x | x | x | x | x | x | x | x | x | x | High |
| 14 | Ghosh J et al. [83] | x | x | x | x | x | x | x | x | x | x | High |
| 15 | Panda PK et al. [84] | x | x | x | x | x | x | x | x | x | x | High |
| 16 | Ghosal S et al. [87] | x | x | x | x | x | x | x | x | x | x | High |
| 17 | Gautam P et al. [54] | x | x | x | x | Medium |
Appendix A.2. Quality Appraisal of Cross-Sectional Surveys Using Adapted JBI Tool
| S.No. | Were the Aims/Objectives of the Study Clear? | Was the Study Design Appropriate for the Stated Aim(s)? | Was the Sample Size Justified? | Was the Target/Reference Population Clearly Defined? (Is It Clear Who the Research Was About?) | Was the Sample Frame Taken from an Appropriate Population Base So That It Closely Represented the Target/Reference Population under Investigation? | Was the Selection Process Likely to Select Subjects/Participants That Were Representative of the Target/Reference Population under Investigation? | Were Measures Undertaken to Address and Categorise Non-Responders? | Were the Risk Factor and Outcome Variables Measured Appropriate to the Aims of the Study? (e.g. Could You See the Questionnaire?) | Were the Risk Factor and Outcome Variables Measured Correctly Using Instruments/Measurements That Had been Trialled, Piloted or Published previously? | Is It Clear What Was Used to Determined Statistical Significance and/or Precision Estimates? (e.g., p Values, CIs) | Were the Methods (Including Statistical Methods) Sufficiently Described to Enable Them to be Repeated? | Were the Basic Data Adequately Described? | Does the Response Rate Raise Concerns about Non-Response bias? | If Appropriate, Was Information about Non-Responders Described? | Were the Results Internally Consistent? | Were the Results for the Analyses Described in the Methods, Presented? | Were the Authors’ Discussions and Conclusions Justified by the Results? | Were the Limitations of the Study Discussed? | Were There Any Funding Sources or Conflicts of Interest That May Affect the Authors’ Interpretation of the Results? | Was Ethical Approval or Consent of Participants Attained? | Overall Assessment |
| 1 | Nair A et al. [56] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | |||
| 2 | Garg S et al. [58] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | |||
| 3 | Nasta AM et al. [59] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | |||||
| 4 | Keshav K et al. [63] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |||
| 5 | Sahu D et al. [65] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |
| 6 | George CE et al. [66] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |
| 7 | Barik S et al. [68] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |
| 8 | Wilson W et al. [27] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |
| 9 | Khasne RW et al. [70] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | ||
| 10 | Das A et al. [71] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | ||
| 11 | Venkataram T et al. [72] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | ||
| 12 | Bhandoria G et al. [73] | x | x | x | x | x | x | x | x | x | x | x | x | x | Low | ||||||
| 13 | Khanna RC et al. [75] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | ||
| 14 | Chatterjee SS et al. [76] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | ||
| 15 | Subbian A et al. [28] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | ||
| 16 | Moorthy RK et al. [78] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | |||
| 17 | Joshi R et al. [80] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Low | |||
| 18 | Mitra M et al. [82] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | ||
| 19 | Nachimuthu S et al. [85] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | |
| 20 | Prasad N et al. [86] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium | ||
| 21 | Chopra S et al. [88] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | High | ||
| 22 | Nilima N et al. [26] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | Medium |
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 (accessed on 20 March 2020).
- Bong, C.-L.; Brasher, C.; Chikumba, E.; McDougall, R.; Mellin-Olsen, J.; Enright, A. The COVID-19 Pandemic: Effects on Low- and Middle-Income Countries. Anesth. Analg. 2020, 131, 86–92. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 127. Available online: https://apps.who.int/iris/handle/10665/332232 (accessed on 26 May 2020).
- World Health Organization. Attacks on Health Care in the Context of COVID-19. Available online: https://www.who.int/news-room/feature-stories/detail/attacks-on-health-care-in-the-context-of-covid-19 (accessed on 30 July 2020).
- Fontanarosa, P.B.; Bauchner, H. COVID-19—Looking Beyond Tomorrow for Health Care and Society. JAMA 2020, 323, 1907–1908. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.H.; Carrion, D.M.; Rivas, J.G.; Mantica, G.; Mattigk, A.; Pradere, B.; Esperto, F. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur. Urol. 2020, 78, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.G.T.; Whittaker, C.; Watson, O.J.; Baguelin, M.; Winskill, P.; Hamlet, A.; Djafaara, B.A.; Cucunubá, Z.; Olivera Mesa, D.; Green, W.; et al. The Impact of COVID-19 and Strategies for Mitigation and Suppression in Low- and Middle-Income Countries. Science 2020, 369, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Jazieh, A.R.; Akbulut, H.; Curigliano, G.; Rogado, A.; Alsharm, A.A.; Razis, E.D.; Mula-Hussain, L.; Errihani, H.; Khattak, A.; De Guzman, R.B.; et al. Impact of the COVID-19 Pandemic on Cancer Care: A Global Collaborative Study. JCO Glob. Oncol. 2020, 6, 1428–1438. [Google Scholar] [CrossRef]
- Hebbar, P.B.; Sudha, A.; Dsouza, V.; Chilgod, L.; Amin, A. Healthcare Delivery in India amid the Covid-19 Pandemic: Challenges and Opportunities. Indian J. Med. Ethics 2020, 1, 1–4. [Google Scholar] [CrossRef]
- The Lancet. India under COVID-19 Lockdown. Lancet 2020, 395, 1315. [Google Scholar] [CrossRef]
- Chandrashekhar, V. 1.3 Billion People. A 21-Day Lockdown. Can India Curb the Coronavirus? Available online: https://doi.org/10.1126/science.abc0030 (accessed on 31 March 2020).
- Bhardwaj, A. COVID-19: A Bigger Challenge to the Indian Healthcare System. Developing Economics. Available online: https://developingeconomics.org/2020/04/13/covid-19-a-bigger-challenge-to-the-indian-healthcare-system/ (accessed on 1 May 2020).
- Singh, A.; Deedwania, P.; Vinay, K.; Chowdhury, A.R.; Khanna, P. Is India’s Health Care Infrastructure Sufficient for Handling COVID 19 Pandemic? Int. Arch. Public Health Community Med. 2020, 4, 41. [Google Scholar] [CrossRef]
- Jain, P. Heart Attack Patient Denied Treatment in Delhi. India Today. Available online: https://www.indiatoday.in/india/story/heart-attack-patient-denied-treatment-in-delhi-1664652-2020-04-08 (accessed on 8 April 2020).
- Kulkarni, T. Cancer Patients Worried as Hospitals Focus on COVID-19. The Hindu. Available online: https://www.thehindu.com/news/cities/bangalore/cancer-patients-worried-as-hospitals-focus-on-covid-19/article31292061.ece/amp/ (accessed on 8 April 2020).
- Johari, A. India’s Focus on Coronavirus Leave TB and HIV Patients Adrift. Scroll. In. Available online: https://scroll.in/article/958400/invisible-crisis-tb-and-hiv-patients-left-adrift-in-indias-focus-on-coronavirus. (accessed on 7 April 2020).
- Prasad, V.; Sri, B.S.; Gaitonde, R. Bridging a False Dichotomy in the COVID-19 Response: A Public Health Approach to the ‘Lockdown’ Debate. BMJ Global Health 2020, 5, e002909. [Google Scholar] [CrossRef]
- SAMA Resource Group for Women and Health. Access to Maternal Health Care: Challenges with Lockdown. Available online: https://samawomenshealth.in/access-to-maternal-health-care-challenges-with-lockdown/ (accessed on 10 May 2020).
- Salve, P. COVID-19 Lockdown Causing Further Shortage at Blood Banks. IndiaSpend. Available online: https://www.indiaspend.com/covid-19-lockdown-causing-further-shortage-at-blood-banks/ (accessed on 1 April 2020).
- Rukmini, S. How Covid-19 Response Disrupted Health Services in Rural India. Livemint. Available online: https://www.livemint.com/news/india/how-covid-19-response-disrupted-health-services-in-rural-india-11587713155817.html (accessed on 25 April 2020).
- Yasmeen, A. COVID-19 Restrictions Hit Other Patients Hard. The Hindu. Available online: https://www.thehindu.com/news/national/karnataka/covid-19-restrictions-hit-other-patients-hard/article31188042.ece (accessed on 28 March 2020).
- Ministry of Health and Family Welfare, Government of India. Enabling Delivery of Essential Health Services during the COVID-19 Outbreak: Guidance Note. Available online: https://www.mohfw.gov.in/pdf/EssentialservicesduringCOVID19updated0411201.pdf (accessed on 15 April 2020).
- Ministry of Health and Family Welfare, Govt. of India. Guidelines on Rational Use of Personal Protective Equipment. Available online: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf (accessed on 4 April 2020).
- Ministry of Health and Family Welfare, Government of India. Telemedicine Practice Guidelines—Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine. Available online: https://www.mohfw.gov.in/pdf/Telemedicine.pdf (accessed on 25 March 2020).
- News18. Day after Honouring Doctors with Claps, Many in India Are Evicting Them Fearing Covid-19. Available online: https://www.news18.com/news/buzz/day-after-honouring-doctors-with-claps-many-in-india-are-evicting-them-fearing-covid-19-2548937.html. (accessed on 28 March 2020).
- Nilima, N.; Kaushik, S.; Tiwary, B.; Pandey, P.K. Psycho-Social Factors Associated with the Nationwide Lockdown in India during COVID-19 Pandemic. Clin. Epidemiol. Glob. Health 2021, 9, 47–52. [Google Scholar] [CrossRef]
- Wilson, W.; Raj, J.P.; Rao, S.; Ghiya, M.; Nedungalaparambil, N.M.; Mundra, H.; Mathew, R. Prevalence and Predictors of Stress, Anxiety, and Depression among Healthcare Workers Managing COVID-19 Pandemic in India: A Nationwide Observational Study. Indian J. Psychol. Med. 2020, 42, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Subbian, A.; Kaur, S.; Patel, V.; Rajanbabu, A. COVID-19 and Its Impact on Gynaecologic Oncology Practice in India-Results of a Nationwide Survey. Ecancermedicalscience 2020, 14, 1067. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Stewart, L.; Moher, D.; Shekelle, P. Why Prospective Registration of Systematic Reviews Makes Sense. Syst. Rev. 2012, 1, 7. [Google Scholar] [CrossRef]
- Beranova, E.; Sykes, C. A Systematic Review of Computer-Based Softwares for Educating Patients with Coronary Heart Disease. Patient Educ. Couns. 2007, 66, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Singh, J. Mendeley: A Free Research Management Tool for Desktop and Web. J. Pharmacol. Pharmacother. 2010, 1, 62–63. [Google Scholar] [CrossRef] [PubMed]
- Murphree, L.; White, M.; Rochen Renner, B. Reference Managers That Support Collaborative Research: Dreaming of the Perfect Fit. Med. Ref. Serv. Q. 2018, 37, 219–233. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.; Pedrosa, M. Using Reference Manager (Mendeley) in Systematic Reviews. In Proceedings of the Abstracts of the Global Evidence Summit, Cape Town, South Africa. Cochrane Database Syst. Rev. 2017, 9 (Suppl. S1), 302–303. [Google Scholar] [CrossRef]
- Lorenzetti, D.L.; Ghali, W.A. Reference Management Software for Systematic Reviews and Meta-Analyses: An Exploration of Usage and Usability. BMC Med. Res. Methodol. 2013, 13, 141. [Google Scholar] [CrossRef]
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 15 December 2020).
- Covidence: Reference Screening. UNC University Libraries. Available online: https://guides.lib.unc.edu/Covidence (accessed on 15 December 2020).
- Lefebvre, C.; Glanville, J.; Briscoe, S.; Featherstone, R.; Littlewood, A.; Marshall, C.; Metzendorf, M.I.; Noel-Storr, A.; Paynter, R.; Rader, T.; et al. Chapter 4: Searching for and Selecting Studies. Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook/current/chapter-04 (accessed on 17 December 2020).
- Mayo Clinic Libraries. Data Extraction Tool for Systematic Reviews. Mayo Library Guides. Available online: https://libraryguides.mayo.edu/systematicreviewprocess/dataextracttools (accessed on 16 December 2020).
- Jonnalagadda, S.R.; Goyal, P.; Huffman, M.D. Automating Data Extraction in Systematic Reviews: A Systematic Review. Syst. Rev. 2015, 4, 78. [Google Scholar] [CrossRef]
- Li, T.; Higgins, J.P.T.; Deeks, J.J. Chapter 5: Collecting Data. Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook/current/chapter-05 (accessed on 17 December 2020).
- UNC Health Sciences Library Systematic Reviews: Step 7: Extract Data from Included Studies. Available online: https://guides.lib.unc.edu/systematic-reviews/extract-data (accessed on 17 December 2020).
- Critical Appraisal Skills Programme. CASP Qualitative Studies Checklist, 2022. Available online: https://casp-uk.net/images/checklist/documents/casp-qualitative-studies-checklist/casp-qualitative-checklist-2018_fillable_form.pdf (accessed on 17 December 2020).
- Long, H.A.; French, D.P.; Brooks, J.M. Optimising the Value of the Critical Appraisal Skills Programme (CASP) Tool for Quality Appraisal in Qualitative Evidence Synthesis. Res. Methods Med. Health Sci. 2020, 1, 31–42. [Google Scholar] [CrossRef]
- Bilardi, D.; Rapa, E.; Bernays, S.; Lang, T. Measuring Research Capacity Development in Healthcare Workers: A Systematic Review. BMJ Open 2021, 11, E046796. [Google Scholar] [CrossRef]
- Hadavi, M.; Ghomian, Z.; Mohammadi, F.; Sahebi, A. Workplace Violence against Health Care Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Safety Res. 2023, 85, 1–7. [Google Scholar] [CrossRef]
- Pimentel, M.M.; Dos Santos, W.H.B.; Rodrigues, E.K.; Fernandes, S.G.G.; de Carvalho, P.F.; Figueiredo, A.T.D.N.S.; Maciel, Á.C.C. Monitoring Sarcopenia with Wearable Devices: A Systematic Review Protocol. BMJ Open 2023, 13, e070507. [Google Scholar] [CrossRef]
- Downes, M. AXIS Critical Appraisal of Cross Sectional Studies. Griffith University. Centre for Applied Health Economics. Available online: http://www.cebm.net/wp-content/uploads/sites/3/2016/06/evidence-live-2016-md.pdf (accessed on 15 January 2021).
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a Critical Appraisal Tool to Assess the Quality of Cross-Sectional Studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [PubMed]
- Schettini, M.A.S.; Passos, R.F.D.N.; Koike, B.D.V. Shift Work and Metabolic Syndrome Updates: A Systematic Review. Sleep Sci. 2023, 16, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Ramamurthy, P.; Jayasree, A.; Solomon, S.; Rudravaram, V.V.; Menon, V.; Thilakan, P. Medication Nonadherence and Its Associated Factors in Psychiatric Patients in India: A Systematic Review and Meta-Analysis. Indian J. Psychiatry 2023, 65, 506–525. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.M.; Hoffmann, M.; Schwarz, P.; Kamolz, L.-P.; Brunner, G.; Sendlhofer, G. A Systematic Literature Review and Narrative Synthesis on the Risks of Medical Discharge Letters for Patients’ Safety. BMC Health Serv. Res. 2019, 19, 158. [Google Scholar] [CrossRef] [PubMed]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Programme. A Prod. ESRC Methods Programme Version 2006, 1, b92. [Google Scholar]
- Gautam, P.; Gandhi, V.; Naik, S.; Mane, A.; Kanitkar, G.; Hegde, S.; Deshmukh, S. Cancer Care in a Western Indian Tertiary Center during the Pandemic: Surgeon’s Perspective. J. Surg. Oncol. 2020, 122, 1525–1533. [Google Scholar] [CrossRef]
- Goyal, N.; Venkataram, T.; Singh, V.; Chaturvedi, J. Collateral Damage Caused by COVID-19: Change in Volume and Spectrum of Neurosurgery Patients. J. Clin. Neurosci. 2020, 80, 156–161. [Google Scholar] [CrossRef]
- Nair, A.G.; Gandhi, R.A.; Natarajan, S. Effect of COVID-19 Related Lockdown on Ophthalmic Practice and Patient Care in India: Results of a Survey. Indian J. Ophthalmol. 2020, 68, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Sanghavi, P.; Patel, B.; Umrania, R.; Chishi, K.; Ghoghari, M. Experience of Palliative Care Services at Tertiary Comprehensive Cancer Center during COVID-19 Lockdown Phase: An Analytical Original Study. Indian J. Palliat. Care 2020, 26, S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Basu, S.; Rustagi, R.; Borle, A. Primary Health Care Facility Preparedness for Outpatient Service Provision During the COVID-19 Pandemic in India: Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e19927. [Google Scholar] [CrossRef] [PubMed]
- Nasta, A.M.; Goel, R.; Kanagavel, M.; Easwaramoorthy, S. Impact of COVID-19 on General Surgical Practice in India. Indian J. Surg. 2020, 82, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, R.; Gautam, D.; Mathur, R.; Choudhary, D. Management of Cardiovascular Emergencies during the COVID-19 Pandemic. Emerg. Med. J. 2020, 37, 778. [Google Scholar] [CrossRef]
- Goyal, M.; Singh, P.; Singh, K.; Shekhar, S.; Agrawal, N.; Misra, S. The Effect of the COVID-19 Pandemic on Maternal Health Due to Delay in Seeking Health Care: Experience from a Tertiary Center. Int. J. Gynaecol. Obstet. 2021, 152, 231–235. [Google Scholar] [CrossRef]
- Deshmukh, S.; Naik, S.; Zade, B.; Patwa, R.; Gawande, J.; Watgaonkar, R.; Wagh, S.; Deshmukh, S.; Gautam, P.; Gandhi, V.; et al. Impact of the Pandemic on Cancer Care: Lessons Learnt from a Rural Cancer Center in the First 3 Months. J. Surg. Oncol. 2020, 122, 831–838. [Google Scholar] [CrossRef]
- Keshav, K.; Kumar, A.; Sharma, P.; Baghel, A.; Mishra, P.; Huda, N. How Much Has COVID-19 Pandemic Affected Indian Orthopaedic Practice? Results of an Online Survey. Indian J. Orthop. 2020, 54, 358–367. [Google Scholar] [CrossRef]
- Gupta, A.; Arora, V.; Nair, D.; Agrawal, N.; Su, Y.-X.; Holsinger, F.C.; Chan, J.Y.K. Status and Strategies for the Management of Head and Neck Cancer during COVID-19 Pandemic: Indian Scenario. Head Neck 2020, 42, 1460–1465. [Google Scholar] [CrossRef]
- Sahu, D.; Agrawal, T.; Rathod, V.; Bagaria, V. Impact of COVID 19 Lockdown on Orthopaedic Surgeons in India: A Survey. J. Clin. Orthop. Trauma 2020, 11, S283–S290. [Google Scholar] [CrossRef]
- George, C.E.; Inbaraj, L.R.; Rajukutty, S.; de Witte, L.P. Challenges, Experience and Coping of Health Professionals in Delivering Healthcare in an Urban Slum in India during the First 40 Days of COVID-19 Crisis: A Mixed Method Study. BMJ Open 2020, 10, e042171. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, D.; Chawla, R.; Varshney, T.; Shaikh, N.; Chandra, P.; Kumar, A. Managing Vitreoretinal Surgeries during COVID-19 Lockdown in India: Experiences and Future Implications. Indian J. Ophthalmol. 2020, 68, 2126–2130. [Google Scholar] [CrossRef] [PubMed]
- Barik, S.; Paul, S.; Kandwal, P. Insight into the Changing Patterns in Clinical and Academic Activities of the Orthopedic Residents during COVID-19 Pandemic: A Cross-Sectional Survey. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3087–3093. [Google Scholar] [CrossRef]
- Khurana, D.K.; Raheja, S.G.; Dayal, M.; Pande, D.; Ganapathy, U. COVID 19: The New Normal in the Clinic: Overcoming Challenges in Palliative Care. Indian J. Palliat. Care 2020, 26, S81–S85. [Google Scholar] [CrossRef]
- Khasne, R.W.; Dhakulkar, B.S.; Mahajan, H.C.; Kulkarni, A.P. Burnout among Healthcare Workers during COVID-19 Pandemic in India: Results of a Questionnaire-Based Survey. Indian J. Crit. Care Med. 2020, 24, 664–671. [Google Scholar] [CrossRef]
- Das, A.; Sil, A.; Jaiswal, S.; Rajeev, R.; Thole, A.; Jafferany, M.; Ali, S.N. A Study to Evaluate Depression and Perceived Stress Among Frontline Indian Doctors Combating the COVID-19 Pandemic. Prim. Care Companion CNS Disord. 2020, 22, 26168. [Google Scholar] [CrossRef]
- Venkataram, T.; Goyal, N.; Dash, C.; Chandra, P.P.; Chaturvedi, J.; Raheja, A.; Singla, R.; Sardhara, J.; Singh, B.; Gupta, R. Impact of the COVID-19 Pandemic on Neurosurgical Practice in India: Results of an Anonymized National Survey. Neurol. India 2020, 68, 595–602. [Google Scholar] [CrossRef]
- Bhandoria, G.; Shylasree, T.S.; Bhandarkar, P.; Ahuja, V.; Maheshwari, A.; Sekhon, R.; Somashekhar, S.P. Impact of COVID-19 Pandemic on Gynecological Oncology Care: Glimpse into Association of Gynecological Oncologists of India (AGOI) Perspective. Indian J. Gynecol. Oncol. 2020, 18, 71. [Google Scholar] [CrossRef]
- Babu, N.; Kohli, P.; Mishra, C.; Sen, S.; Arthur, D.; Chhablani, D.; Baliga, G.; Ramasamy, K. To Evaluate the Effect of COVID-19 Pandemic and National Lockdown on Patient Care at a Tertiary-Care Ophthalmology Institute. Indian J. Ophthalmol. 2020, 68, 1540–1544. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.C.; Honavar, S.G.; Metla, A.L.; Bhattacharya, A.; Maulik, P.K. Psychological Impact of COVID-19 on Ophthalmologists-in-Training and Practising Ophthalmologists in India. Indian J. Ophthalmol. 2020, 68, 994–998. [Google Scholar] [CrossRef]
- Chatterjee, S.S.; Bhattacharyya, R.; Bhattacharyya, S.; Gupta, S.; Das, S.; Banerjee, B.B. Attitude, Practice, Behavior, and Mental Health Impact of COVID-19 on Doctors. Indian J. Psychiatry 2020, 62, 257–265. [Google Scholar] [CrossRef]
- Mahajan, N.N.; Pednekar, R.; Patil, S.R.; Subramanyam, A.A.; Rathi, S.; Malik, S.; Mohite, S.C.; Shinde, G.; Joshi, M.; Kumbhar, P.; et al. Preparedness, Administrative Challenges for Establishing Obstetric Services, and Experience of Delivering over 400 Women at a Tertiary Care COVID-19 Hospital in India. Int. J. Gynaecol. Obstet. 2020, 151, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, R.K.; Rajshekhar, V. Impact of COVID-19 Pandemic on Neurosurgical Practice in India: A Survey on Personal Protective Equipment Usage, Testing, and Perceptions on Disease Transmission. Neurol. India 2020, 68, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Rajput, R.; Verma, S.; Balania, V.K.B.; Jangra, B. Impact of Lockdown in COVID 19 on Glycemic Control in Patients with Type 1 Diabetes Mellitus. Diabetes Metab. Syndr. 2020, 14, 1213–1216. [Google Scholar] [CrossRef] [PubMed]
- Joshi, R.; Atal, S.; Fatima, Z.; Balakrishnan, S.; Sharma, S.; Joshi, A. Diabetes Care during COVID-19 Lockdown at a Tertiary Care Centre in India. Diabetes Res. Clin. Pract. 2020, 166, 108316. [Google Scholar] [CrossRef]
- Jain, A.; Goyal, V.; Varma, C. Reflection of Epidemiological Impact on Burden of Injury in Tertiary Care Centre, Pre-COVID and COVID Era: “Lockdown, a Good Fortune for Saving Life and Limb”. Indian J. Surg. 2021, 83, 139–143. [Google Scholar] [CrossRef]
- Mitra, M.; Basu, M. A Study on Challenges to Health Care Delivery Faced by Cancer Patients in India During the COVID-19 Pandemic. J. Prim. Care Community Health 2020, 11, 2150132720942705. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, J.; Ganguly, S.; Mondal, D.; Pandey, P.; Dabkara, D.; Biswas, B. Perspective of Oncology Patients During COVID-19 Pandemic: A Prospective Observational Study From India. JCO Glob. Oncol. 2020, 6, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Dawman, L.; Panda, P.; Sharawat, I.K. Feasibility and Effectiveness of Teleconsultation in Children with Epilepsy amidst the Ongoing COVID-19 Pandemic in a Resource-Limited Country. Seizure 2020, 81, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Nachimuthu, S.; Vijayalakshmi, R.; Sudha, M.; Viswanathan, V. Coping with Diabetes during the COVID—19 Lockdown in India: Results of an Online Pilot Survey. Diabetes Metab. Syndr. 2020, 14, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Prasad, N.; Bhatt, M.; Agarwal, S.K.; Kohli, H.S.; Gopalakrishnan, N.; Fernando, E.; Sahay, M.; Rajapurkar, M.; Chowdhary, A.R.; Rathi, M.; et al. The Adverse Effect of COVID Pandemic on the Care of Patients With Kidney Diseases in India. Kidney Int. Rep. 2020, 5, 1545–1550. [Google Scholar] [CrossRef]
- Ghosal, S.; Arora, B.; Dutta, K.; Ghosh, A.; Sinha, B.; Misra, A. Increase in the Risk of Type 2 Diabetes during Lockdown for the COVID-19 Pandemic in India: A Cohort Analysis. Diabetes Metab. Syndr. 2020, 14, 949–952. [Google Scholar] [CrossRef] [PubMed]
- Chopra, S.; Ranjan, P.; Singh, V.; Kumar, S.; Arora, M.; Hasan, M.S.; Kasiraj, R.; Suryansh; Kaur, D.; Vikram, N.K.; et al. Impact of COVID-19 on Lifestyle-Related Behaviours- a Cross-Sectional Audit of Responses from Nine Hundred and Ninety-Five Participants from India. Diabetes Metab. Syndr. 2020, 14, 2021–2030. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Family Welfare National Mental Health Survey of India, 2015–2016. Prevalence, Pattern and Outcomes. Available online: http://indianmhs.nimhans.ac.in/Docs/Report2.pdf (accessed on 18 January 2021).
- World Health Organization. COVID-19 Significantly Impacts Health Services for Noncommunicable Diseases. Available online: https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (accessed on 25 July 2020).
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 Pandemic on Utilisation of Healthcare Services: A Systematic Review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff. 2020, 39, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Conlon, C.; McDonnell, T.; Barrett, M.; Cummins, F.; Deasy, C.; Hensey, C.; McAuliffe, E.; Nicholson, E. The Impact of the COVID-19 Pandemic on Child Health and the Provision of Care in Paediatric Emergency Departments: A Qualitative Study of Frontline Emergency Care Staff. BMC Health Serv. Res. 2021, 21, 279. [Google Scholar] [CrossRef]
- McCabe, R.; Schmit, N.; Christen, P.; D’Aeth, J.C.; Løchen, A.; Rizmie, D.; Nayagam, S.; Miraldo, M.; Aylin, P.; Bottle, A.; et al. Adapting Hospital Capacity to Meet Changing Demands during the COVID-19 Pandemic. BMC Med. 2020, 18, 329. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, A.; O’Leary, K.J.; Greysen, S.R.; Harrison, J.D.; Kripalani, S.; Ruhnke, G.W.; Vasilevskis, E.E.; Maselli, J.; Fang, M.C.; Herzig, S.J.; et al. Hospital Ward Adaptation During the COVID-19 Pandemic: A National Survey of Academic Medical Centers. J. Hosp. Med. 2020, 15, 483–488. [Google Scholar] [CrossRef]
- McGarry, B.E.; Grabowski, D.C.; Barnett, M.L. Severe Staffing And Personal Protective Equipment Shortages Faced By Nursing Homes During The COVID-19 Pandemic. Health Aff. 2020, 39, 1812–1821. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H.; et al. Risk of COVID-19 among Front-Line Health-Care Workers and the General Community: A Prospective Cohort Study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Ali, S.; Maguire, S.; Marks, E.; Doyle, M.; Sheehy, C. Psychological Impact of the COVID-19 Pandemic on Healthcare Workers at Acute Hospital Settings in the South-East of Ireland: An Observational Cohort Multicentre Study. BMJ Open 2020, 10, e042930. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of Viral Epidemic Outbreaks on Mental Health of Healthcare Workers: A Rapid Systematic Review and Meta-Analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Devi, S. COVID-19 Exacerbates Violence against Health Workers. Lancet 2020, 396, 658. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).