Did the COVID-19 Pandemic Disproportionately Affect the Most Socioeconomically Vulnerable Areas of Brazil?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
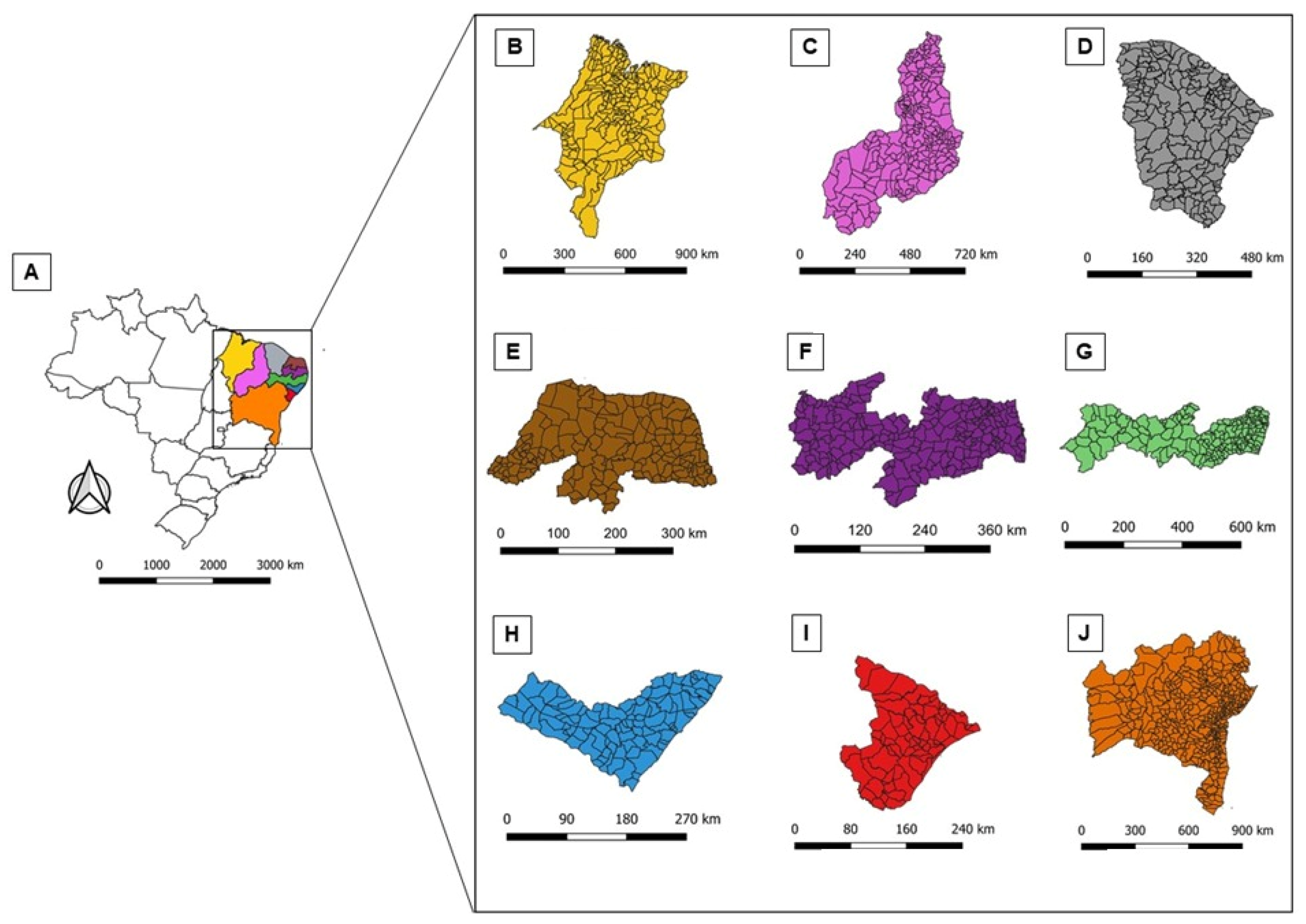
2.2. Study Area
2.3. Study Variables and Data Source
- Epidemiological variables:
- Number of confirmed cases of COVID-19 in the 1794 municipalities of Northeast Brazil.
- Incidence rate of COVID-19. For the calculation, the number of confirmed cases of COVID-19 in each state and municipality was used as a numerator, and the corresponding populations were multiplied by the constant of 100,000 inhabitants.
- SDH:
2.4. Statistical Analysis
- a.
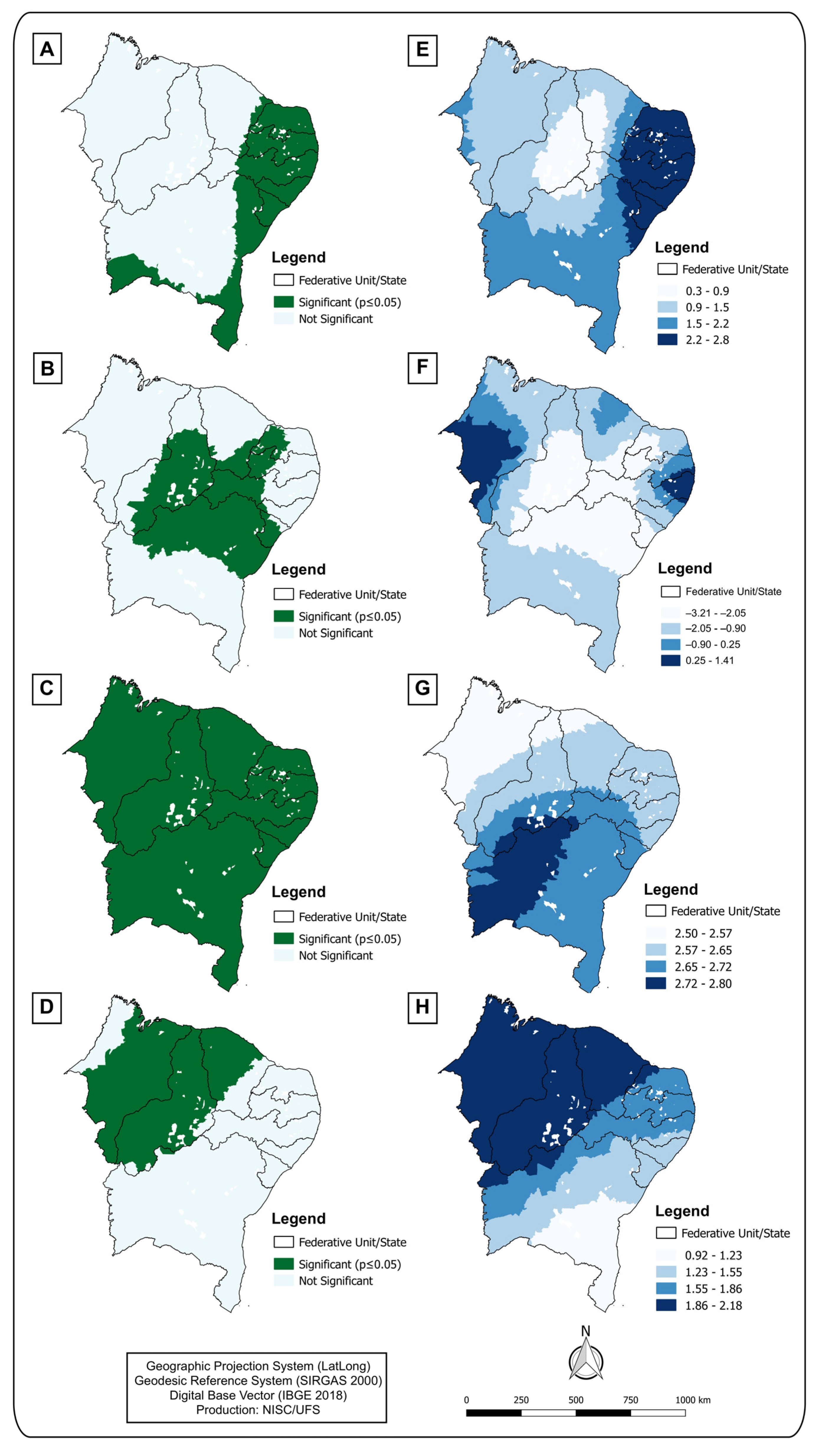
- Spatial analysis
- b.
- Global and local spatial regression models
2.5. Software
2.6. Ethical Aspects
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde (BR). Ministério da Saúde Declara Transmissão Comunitária Nacional. Brasil: Ministério da Saúde. 2020. Available online: https://www.gov.br/saude/pt-br/assuntos/noticias/ministerio-da-saude-declara-transmissao-comunitaria-nacional (accessed on 10 March 2022).
- Johns Hopkins University (JHU). Coronavirus Resource Center. United States: JHU. 2021. Available online: https://coronavirus.jhu.edu/ (accessed on 10 March 2022).
- Ministério da Saúde (BR). Coronavírus Brasil. Brasil: Ministério da Saúde. 2021. Available online: https://covid.saude.gov.br/ (accessed on 10 March 2022).
- Almeida Andrade, L.; Silva da Paz, W.; Fontes Lima, A.G.C.; da Conceição Araújo, D.; Duque, A.M.; Peixoto, M.V.S.; Góes, M.A.O.; Freire de Souza, C.D.; Nunes Ribeiro, C.J.; Almeida Lima, S.V.M.; et al. Spatiotemporal Pattern of COVID-19–Related Mortality during the First Year of the Pandemic in Brazil: A Population-Based Study in a Region of High Social Vulnerability. Am. J. Trop. Med. Hyg. 2022, 106, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Mansouritorghabeh, H.; Bagherimoghaddam, A.; Eslami, S.; Raouf-Rahmati, A.; Hamer, D.H.; Kiani, B.; MohammadEbrahimi, S. Spatial Epidemiology of COVID-19 Infection through the First Outbreak in the City of Mashhad, Iran. Spat. Inf. Res. 2022, 30, 585–595. [Google Scholar] [CrossRef]
- Hohl, A.; Delmelle, E.M.; Desjardins, M.R.; Lan, Y. Daily Surveillance of COVID-19 Using the Prospective Space-Time Scan Statistic in the United States. Spat. Spatiotemporal. Epidemiol. 2020, 34, 100354. [Google Scholar] [CrossRef] [PubMed]
- Gravlee, C.C. Systemic Racism, Chronic Health Inequities, and COVID-19: A Syndemic in the Making? Am. J. Hum. Biol. 2020, 32, e23482. [Google Scholar] [CrossRef] [PubMed]
- Rafael, R.d.M.R.; Neto, M.; Depret, D.G.; Gil, A.C.; Fonseca, M.H.S.; Souza-Santos, R. Effect of Income on the Cumulative Incidence of COVID-19: An Ecological Study. Rev. Lat. Am. Enferm. 2020, 28, e3344. [Google Scholar] [CrossRef] [PubMed]
- de Souza, C.D.F.; Machado, M.F.; do Carmo, R.F. Human Development, Social Vulnerability and COVID-19 in Brazil: A Study of the Social Determinants of Health. Infect. Dis. Poverty 2020, 9, 124. [Google Scholar] [CrossRef] [PubMed]
- Baggio, J.A.O.; Machado, M.F.; Carmo, R.F.d.; Armstrong, A.d.C.; Santos, A.D.d.; Souza, C.D.F.d. COVID-19 in Brazil: Spatial Risk, Social Vulnerability, Human Development, Clinical Manifestations and Predictors of Mortality—A Retrospective Study with Data from 59 695 Individuals. Epidemiol. Infect. 2021, 149, e100. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Portal Cidades. Rio de Janeiro: IBGE. 2021. Available online: https://cidades.ibge.gov.br (accessed on 10 March 2022).
- Programa das Nações Unidas para o Desenvolvimento (PNUD). Atlas do Desenvolvimento Humano. Brasil: PNUD. 2010. Available online: https://www.br.undp.org/ (accessed on 12 March 2022).
- Instituto de Pesquisa Econômica Aplicada (IPEA). Atlas da Vulnerabilidade Social. Brasil: IPEA. 2021. Available online: http://www.atlasbrasil.org.br/ (accessed on 10 March 2022).
- Ministério da Saúde (MS). Painel Coronavírus. Brasília: MS. 2021. Available online: https://covid.saude.gov.br/ (accessed on 10 March 2022).
- Assunção, R.M.; Barreto, S.M.; Guerra, H.L.; Sakurai, E. Mapas de taxas epidemiológicas: Uma abordagem Bayesiana. Cad. Saude Publica 1998, 14, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Anselin, L.; Florax, R.J.G.M. Small Sample Properties of Tests for Spatial Dependence in Regression Models: Some Further Results; Springer: Berlin/Heidelberg, Germany, 1995; pp. 21–74. [Google Scholar] [CrossRef]
- Zuur, A.F.; Ieno, E.N.; Smith, G.M. Analysing Ecological Data; Springer: New York, NY, USA, 2007. [Google Scholar] [CrossRef]
- Magalhães, M.d.A.F.M.; Medronho, R.d.A. Análise Espacial Da Tuberculose No Rio de Janeiro No Período de 2005 a 2008 e Fatores Socioeconômicos Associados Utilizando Microdado e Modelos de Regressão Espaciais Globais. Cien. Saude Colet. 2017, 22, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Anselin, L. Exploring Spatial Data with GeoDa: A Workbook; Centre for Spatially Integrated Social Science: Santa Barbara, CA, USA, 2005. [Google Scholar]
- Charlton, M.; Fotheringham, S.; Brunsdon, C. Geographically Weighted Regression; ESRC National Centre for Research Methods: Maynooth, UK, 2005. [Google Scholar]
- Oshan, T.; Li, Z.; Kang, W.; Wolf, L.; Fotheringham, A. Mgwr: A Python Implementation of Multiscale Geographically Weighted Regression for Investigating Process Spatial Heterogeneity and Scale. ISPRS Int. J. Geo-Inf. 2019, 8, 269. [Google Scholar] [CrossRef]
- QGIS Team Development. QGIS: A free and Open Source Geographic Information System. 2021. Available online: https://qgis.org/pt_BR/site/, (accessed on 10 March 2022).
- Burström, B.; Tao, W. Social Determinants of Health and Inequalities in COVID-19. Eur. J. Public Health 2020, 30, 617–618. [Google Scholar] [CrossRef] [PubMed]
- Raymundo, C.E.; Oliveira, M.C.; Eleuterio, T.d.A.; André, S.R.; da Silva, M.G.; Queiroz, E.R.d.S.; Medronho, R.d.A. Spatial Analysis of COVID-19 Incidence and the Sociodemographic Context in Brazil. PLoS ONE 2021, 16, e0247794. [Google Scholar] [CrossRef] [PubMed]
- Baqui, P.; Bica, I.; Marra, V.; Ercole, A.; van der Schaar, M. Ethnic and Regional Variations in Hospital Mortality from COVID-19 in Brazil: A Cross-Sectional Observational Study. Lancet Glob. Health 2020, 8, e1018–e1026. [Google Scholar] [CrossRef] [PubMed]
- Gomes, D.S.; Andrade, L.A.; Ribeiro, C.J.N.; Peixoto, M.V.S.; Lima, S.V.M.A.; Duque, A.M.; Cirilo, T.M.; Góes, M.A.O.; Lima, A.G.C.F.; Santos, M.B.; et al. Risk Clusters of COVID-19 Transmission in Northeastern Brazil: Prospective Space–Time Modelling. Epidemiol. Infect. 2020, 148, e188. [Google Scholar] [CrossRef] [PubMed]
- Maciel, J.A.C.; Castro-Silva, I.I.; Farias, M.R.d. Análise Inicial Da Correlação Espacial Entre a Incidência de COVID-19 e o Desenvolvimento Humano Nos Municípios Do Estado Do Ceará No Brasil. Rev. Bras. Epidemiol. 2020, 23, e200057. [Google Scholar] [CrossRef] [PubMed]
- Daspett Mendonça, F.; Soares Rocha, S.; Pimenta Pinheiro, D.L.; Vilges de Oliveira, S. Região Norte Do Brasil e a Pandemia de COVID-19: Análise Socioeconômica e Epidemiológica. J. Health NPEPS 2020, 5, 20–37. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional por Amostra de Domicílios Contínua COVID-19. Rio de Janeiro: IBGE. 2020. Available online: https://www.ibge.gov.br/estatisticas/sociais/rendimento-despesa-e-consumo/9171-pesquisa-nacional-por-amostra-de-domicilios-continua-mensal.html (accessed on 10 March 2022).
- Horton, R. Offline: COVID-19 Is Not a Pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A.; Judd, J. COVID-19: Vulnerability and the Power of Privilege in a Pandemic. Health Promot. J. Aust. 2020, 31, 158–160. [Google Scholar] [CrossRef] [PubMed]

| State | Confirmed Cases | Population | Incidence Rate (per 100,000 Inhabitants) |
|---|---|---|---|
| Alagoas | 150,364 | 3,351,543 | 4486.41 |
| Sergipe | 170,413 | 2,318,822 | 7349.12 |
| Rio Grande do Norte | 191,752 | 3,534,165 | 5425.67 |
| Piauí | 198,664 | 3,281,480 | 6054.10 |
| Maranhão | 239,077 | 7,114,598 | 3360.37 |
| Paraíba | 252,889 | 4,039,277 | 6260.75 |
| Pernambuco | 341,249 | 9,616,621 | 3548.53 |
| Ceará | 508,832 | 9,187,103 | 5538.55 |
| Bahia | 778,617 | 14,930,634 | 5214.90 |
| Total | 2,831,857 | 57,347,243 | 4938.09 |
| Social Determinants of Health | Rho | p |
|---|---|---|
| Percentage of poverty | 0.65 | <0.01 |
| Gini index | −0.57 | <0.01 |
| Percentage of people living in households vulnerable to poverty and who spend more than one hour commuting to work | 0.50 | <0.01 |
| Activity rate—25 to 29 years of age | 0.50 | 0.02 |
| Municipal Human Development Index (MHDI) income | −0.50 | 0.01 |
| Percentage of people who are employed without income | −0.50 | 0.02 |
| Ratio of the richest 10% to the poorest 40% | 0.49 | 0.05 |
| Percentage of people in households vulnerable to poverty and dependent on elderly adults | 0.48 | 0.01 |
| Dependency ratio | −0.47 | 0.02 |
| Illiteracy rate | 0.35 | 0.01 |
| Percentage of employed persons with complete secondary education | 0.33 | 0.01 |
| Municipal Human Development Index Education (MHDI Education): school attendance sub-index | −0.29 | 0.01 |
| Percentage of people in households with inadequate water supply and sanitation | 0.28 | 0.02 |
| Social Determinants of Health | OLS Model | Spatial Lag Model | ||
|---|---|---|---|---|
| Coefficient | p | Coefficient | p | |
| Gini index | −0.93 | <0.01 | −0.78 | <0.01 |
| Percentage of people in households that are vulnerable to poverty and who spend more than 1 h commuting to work | 0.70 | <0.01 | 0.69 | <0.01 |
| Dependency ratio | −0.67 | 0.04 | −0.60 | 0.03 |
| Percentage of poverty | 0.55 | <0.01 | 0.48 | 0.03 |
| Activity rate—25 to 29 years of age | 0.50 | 0.01 | 0.46 | 0.01 |
| MHDI Income | −0.48 | <0.01 | 0.12 | 0.06 |
| Ratio of the richest 10% to the poorest 40% | 0.44 | 0.04 | 0.07 | 0.08 |
| Percentage of people employed without income | −0.40 | 0.02 | −0.31 | 0.04 |
| Illiteracy rate | 0.25 | <0.01 | 0.18 | <0.01 |
| Percentage of employed people with a complete secondary education | 0.23 | <0.01 | 0.19 | <0.01 |
| Percentage of people in households vulnerable to poverty and dependent on elderly adults | 0.22 | <0.01 | 0.19 | 0.01 |
| MHDI Education: school attendance sub-index | −0.19 | 0.01 | −0.90 | 0.02 |
| Percentage of people in households with inadequate water supply and sanitation | 0.18 | 0.03 | −0.21 | 0.03 |
| Criteria for evaluating the model | ||||
| AIC | 2629.79 | 2319.71 | ||
| BIC | 2729.78 | 2444.93 | ||
| Log-likelihood | −1292.89 | −1136.66 | ||
| Coefficient of determination (R2) | 0.25 (p = 0.01) | 0.41 (p = 0.01) | ||
| Global Moran’s index of the regression residual | 0.29 (p = 0.00) | −0.25 (p = 0.34) | ||
| Social Determinants of Health | VIF |
|---|---|
| Gini index | 1.227 |
| Percentage of people in households vulnerable to poverty and those who spend more than one hour commuting to work | 1.222 |
| Dependency ratio | 1.127 |
| Percentage of poverty | 1.017 |
| Activity rate—25 to 29 years of age | 1.345 |
| MHDI Income | 2.019 |
| Ratio of the richest 10% to the poorest 40% | 1.217 |
| Percentage of people employed without income | 1.014 |
| Illiteracy rate | 2.001 |
| Percentage of employed people with a complete secondary education | 1.037 |
| Percentage of people in households vulnerable to poverty and dependent on elderly adults | 1.004 |
| MHDI Education: school attendance sub-index | 1.421 |
| Percentage of people in households with inadequate water supply and sanitation | 2.567 |
| Social Determinants of Health | GWMR |
|---|---|
| Mean Z Score Estimates | |
| Gini index | <0.01 |
| Percentage of poverty | 0.01 |
| Illiteracy rate | 0.03 |
| Percentage of people in households vulnerable to poverty and dependent on elderly adults | 0.02 |
| Criteria for evaluating the model | |
| AICc | 2000.87 |
| BIC | 2234.70 |
| Coefficient of determination (R2) | 0.59 (p = 0.01) |
| Global Moran’s index of the regression residual | 0.09 (p = 0.09) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos Alves, J.C.; Ribeiro, C.J.N.; Lima, S.V.M.A.; Morato, G.S.; Andrade, L.A.; Santos, M.B.; Lopes de Sousa, Á.F.; Nogales Crespo, K.A.; Araújo, D.d.C.; dos Santos, A.D. Did the COVID-19 Pandemic Disproportionately Affect the Most Socioeconomically Vulnerable Areas of Brazil? COVID 2023, 3, 924-936. https://doi.org/10.3390/covid3060067
dos Santos Alves JC, Ribeiro CJN, Lima SVMA, Morato GS, Andrade LA, Santos MB, Lopes de Sousa ÁF, Nogales Crespo KA, Araújo DdC, dos Santos AD. Did the COVID-19 Pandemic Disproportionately Affect the Most Socioeconomically Vulnerable Areas of Brazil? COVID. 2023; 3(6):924-936. https://doi.org/10.3390/covid3060067
Chicago/Turabian Styledos Santos Alves, Jonatha C., Caíque J. N. Ribeiro, Shirley V. M. A. Lima, Gabriel S. Morato, Lucas A. Andrade, Márcio B. Santos, Álvaro F. Lopes de Sousa, Katya A. Nogales Crespo, Damião da C. Araújo, and Allan D. dos Santos. 2023. "Did the COVID-19 Pandemic Disproportionately Affect the Most Socioeconomically Vulnerable Areas of Brazil?" COVID 3, no. 6: 924-936. https://doi.org/10.3390/covid3060067
APA Styledos Santos Alves, J. C., Ribeiro, C. J. N., Lima, S. V. M. A., Morato, G. S., Andrade, L. A., Santos, M. B., Lopes de Sousa, Á. F., Nogales Crespo, K. A., Araújo, D. d. C., & dos Santos, A. D. (2023). Did the COVID-19 Pandemic Disproportionately Affect the Most Socioeconomically Vulnerable Areas of Brazil? COVID, 3(6), 924-936. https://doi.org/10.3390/covid3060067








