Abstract
The purpose of this study is to report a case of idiopathic osteosclerosis of the mandible and to discuss the differential diagnosis of this lesion. A 17-year-old female was referred to the University Hospital of Geneva by her orthodontist following the fortuitous finding of a radio-opaque lesion in the right posterior mandible at the apex of tooth 44. Intraoral clinical examination revealed no abnormalities of the oral mucosa. Tooth 44 was asymptomatic and reacted positively to the sensitivity test. The orthopantomogram revealed a well-defined unilocular radiodense lesion, surrounded by a thin radiolucent border, measuring 10 × 33 mm, located in the IV quadrant, related to the apex of tooth 44. Differential diagnoses mainly included cementoblastoma, focal cemento-osseous dysplasia, ossifying fibroma, condensing osteitis and idiopathic osteosclerosis. The biopsy material allowed a diagnosis of idiopathic osteosclerosis. The proposed treatment was therefore a “wait and see” approach. After 2 years of follow-up, the patient was asymptomatic, and healing was complete without any neurosensory complications. Our case underlines the differential diagnosis complexity of radio-opaque lesions associated with teeth.
1. Introduction
The fortuitous finding of radiopaque or radiolucent images during dental X-ray exams is a frequent occurrence [1,2]. An investigation is then necessary in order to establish a diagnosis and thus be able to guide their management. The differential diagnosis of these lesions sometimes represents a real challenge. Radio-opacities, which are less common than radiolucencies, can have multiple origins: they can be caused by numerous bone pathological conditions, i.e., neoplasms of odontogenic and non-odontogenic origin, but also sometimes by superimposed structures present in the maxillofacial region [2,3]. The radiological signs need to be carefully analysed to guide the diagnosis: location, number of lesions, contour, appearance, content and relationship with the roots and/or impact on the teeth [2,3,4].
Although a precise knowledge of the different bone pathologies and their clinical and radiological appearance generally enables a differential diagnosis to be established, a bone biopsy may be necessary to obtain a precise diagnosis and adopt the appropriate treatment [4,5].
The following case deals with the incidental finding of a radio-opaque lesion of the posterior region of the mandible in a young patient diagnosed with idiopathic osteosclerosis (IO).
IO, also known as a dense bone island or enostosis, is a common finding of radiopacity in the alveolar bone of unknown aetiology [2,3,6,7,8]. It presents as an area of increased density in the cancellous bone of various sizes, which usually appears on X-ray exams to be round, elliptical or irregularly shaped [5,6,7]. It is usually located in the first molar or premolar region of the mandible when compared to the maxilla and is sometimes associated with the roots or completely separated from them [5,6,7]. The lesion is consistently asymptomatic and might remain stable over time or show slow growth with no detectable cortical expansion. Its growth usually ends when the patient reaches skeletal maturity [7,8,9]. Histologically, it is composed of dense lamellar vital bone and lacks inflammatory infiltrate [9,10].
The main differential diagnoses are cementoblastoma, focal cemento-osseous dysplasia (FCOD), ossifying fibroma (OF) and condensing osteitis (CO) [1,2,3].
This study aimed to describe imaging features of an atypical case of IO and provide a short literature review to aid in the differential diagnosis of similar dentomaxillary conditions.
2. Case Presentation
A 17-year-old female patient in good health was referred to the Oral Surgery and Implantology Unit of the University Hospital of Geneva by her orthodontist after detecting a radio-opaque lesion in the right posterior mandible centred on the root apex of tooth 44 on OPG radiological examination.
Clinical examination of the oral cavity was within normal limits. A dental examination revealed good oral hygiene and the absence of carious lesions or restorations. More specifically, tooth 44 was asymptomatic, with a positive sensitivity test and negative percussion.
The OPG radiological examination (Figure 1a) revealed a solitary unilocular, well-defined radiodense lesion measuring 10 × 33 mm, surrounded by a thin radiolucent border, located in the posterior IV quadrant, centred at the apex of tooth 44. The complementary Cone Beam Computer Tomography (CBCT) (Newtom Go, Newtom Cefla, Imola, Italy) examination (Figure 1b–d) allowed for the better localisation of this radiodense lesion and appreciation of its size (12 mm mesio-distally, 8 mm vestibulo-lingually and 9 mm in height) as well as its appearance: hyperdense with ground-glass areas at the centre of the lesion and a thin peripheral radiolucent border, more visible than on the OPG. CBCT also showed that the lesion involved the vestibular cortex with a slight expansion of the lingual cortex. The distal side of the lesion was in contact with the mental foramen and was displacing the mandibular incisive canal.

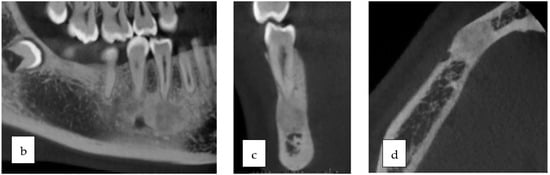
Figure 1.
(a–d). OPG (a) and CBCT in transverse, frontal and sagittal sections (b–d).
Based on clinical and radiological findings, the differential diagnosis most likely included cementoblastoma but also FCOD, CO and IO.
To establish the diagnosis, after discussion with the patient, it was decided to perform a biopsy of the lesion. Two biopsies were taken under local anaesthesia. A full-thickness triangular flap was raised following the intra-sulcular incisions of teeth 43 to 46 and the releasing incision opposite to tooth 43; the mental nerve was thus exposed, and two bone cores were taken from the vestibular cortex (Figure 2a,b). Core biopsies measuring 3.8 × 6 mm were retrieved at the future implant positions using a Ø 4.1 mm trephine explantation bur under constant irrigation with sterile saline (500 rpm): the one from the periphery and the other from the centre of the lesion.
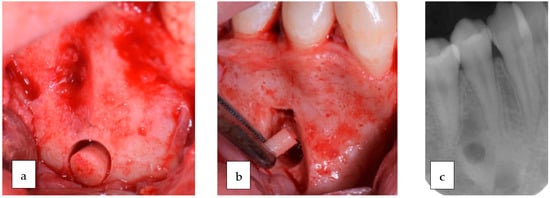
Figure 2.
(a–c). Clinical views during surgery (a,b) and post-operative intra-oral radiograph (c).
The specimens were sent for histopathological analysis, and a diagnosis of benign IO was made (Figure 3).
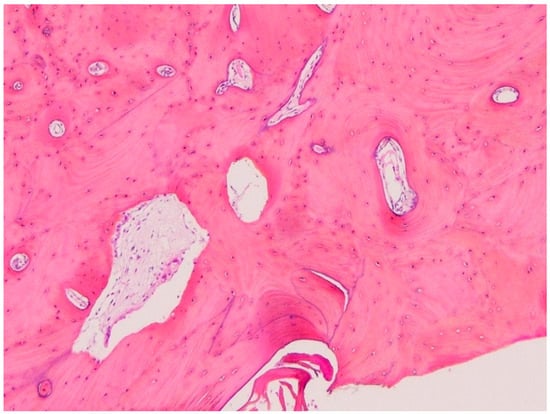
Figure 3.
Histopathology showing vital compact lamellar bone with sparse channels containing loose fibrovascular tissue (H&E, ×20).
The proposed treatment was therefore a “wait and see approach”.
The patient was regularly followed. At 3-year follow-up appointment the patient was asymptomatic, and healing was satisfactory without any neurosensory complications (Figure 4).

Figure 4.
OPG at 3-year follow-up recall appointment.
3. Discussion
When dealing with the radiological detection of a solitary radio-opaque lesion in the posterior mandibular region, a large number of pathological entities comes into play in the differential diagnosis spectrum. The main differential diagnoses are shortly discussed below.
Idiopathic osteosclerosis is a frequent asymptomatic intramaxillary lesion, with a prevalence ranging from 2.3 to 9.7% depending on the study [1] and the population [2]. It seems to be more frequent in Black and Asian than in Caucasian populations. These lesions appear in young patients, aged between 12 and 20, with no known gender predominance.
No clear aetiology for the genesis of these lesions has been identified, although several hypotheses have been considered and studied. Some local stimuli could be related to and precede the appearance of IO, such as occlusal overloads [3] or the persistence of root remnants. The aetiology therefore remains unknown, but unlike SO, local irritation of inflammatory origin is not the cause [4]. Generally asymptomatic, these lesions are often detected in young patients during dental X-ray examinations, with no abnormalities on clinical examination, and the teeth associated with the lesions are vital. Sites of IO can also be found throughout the skeleton. The maxillae are the bones of the skull most frequently affected, with a preferential location in the periapical region of the mandibular first premolars (44%) and first molars (43%) [1] and, more rarely, the mandibular canines.
Radiologically, the lesions appear as radio-opaque foci, often round but sometimes irregular, varying in size from a few millimetres to 2 or more cm. Some studies have shown a tendency for foci present in patients under 20 years of age to increase in size compared with those present in patients over 20 years of age, which remain more stable [1]. In the majority of cases, these lesions are solitary, but rare cases of multiple and sometimes bilateral and symmetrical cases have been reported [10]. The density of osteosclerosis may vary, and its appearance is generally uniform in some ground-glass areas [11].
Complications associated with the presence of IO, such as tooth movement and even root resorption following ectopic tooth eruption, have been described but remain very uncommon [12].
Histological examination shows vital trabecular bone devoid of inflammatory cells, with dense trabeculae, obliterating the bone marrow without any other pathological alterations.
Following the detection of a radiopaque lesion, a precise diagnosis must be made in order to determine whether or not treatment is required. A biopsy should be performed if the diagnosis is not obvious, as in the case we have described above. Although IO does not require treatment, annual follow-up with X-rays is recommended.
Condensing osteitis (or focal sclerosing osteitis) is the most common radio-opaque lesion, with a prevalence of 4 to 7% [13] and a sex ratio of 3 men to 2 women. These lesions are also seen in young people, with 50% of affected patients aged under 30. The vast majority of these lesions are located in the mandible (85%), more precisely opposite to the molars and premolars and, more rarely, at an extraction site.
Unlike IO, the aetiology is well known: These lesions are the consequence of inflammation or infection and are therefore related to teeth that are generally necrotic, endodontically treated, decayed or restored. These lesions appear as a reaction of the bone marrow to a long-term, low-intensity aggression such as chronic pulpitis or pulpal necrosis [8] and are thought to represent the result of excessive osteoblast activity during periapical bone remodelling, which locally fills the marrow spaces [13]. Clinically, these lesions are generally asymptomatic but can sometimes cause pain on palpation or percussion. Radiologically, like IO, these lesions appear as radiopaque foci, rounded in shape and varying in size, opposite to tooth apices, but in this case, the teeth in relation to the lesion are not healthy and show enlargement of the periodontal ligament and loss of the lamina dura [14].
Histological examination shows densification of the trabeculae but a sparse chronic inflammatory infiltrate [13].
The treatment of CO is therefore the elimination of the cause of the inflammation. Endodontic treatment of the opposing teeth is therefore recommended and, in the majority of cases, leads to the total disappearance of the lesion (85%) [15]. Otherwise, no treatment is recommended if the size of the lesion remains stable. As the diagnosis is often obvious, a confirmatory biopsy is generally not necessary.
Cementoblastoma (previously described in the literature as cementomas, true cementomas, sclerosing cementomas, periapical fibro-osteoma and periapical fibrous dysplasia) is a rare benign odontogenic tumour of mesenchymal origin [16]. It is diagnosed in young female patients, predominantly between 20 and 30 years of age, with a slight male predominance [17]. These lesions are typically solitary, located in the posterior mandible (70%), associated with and attached to the roots of teeth apices (usually second premolars and first molars and, exceptionally, the apices of deciduous teeth).
This lesion determines the rapid proliferation of cementoblasts, which then produce a disorganised calcified tissue or acellular cementum.
Clinically, most patients are asymptomatic, and the teeth concerned are vital. The most frequent sign is the appearance of a painful swelling opposite the lesion [18].
More rarely, complications may arise following significant growth of the lesion. Mandibular fractures and lower labial paresthesia have been described [19].
Radiologically, these lesions appear as rounded, well-defined radiopaque masses attached to a dental apex. Unlike CO, this lesion presents the loss of the desmodontal space and a thin radiolucent border. Depending on the stage of maturity of the lesion, the central density may be more or less uniform. It can also lead to the resorption of adjacent teeth and the displacement of the mandibular canal.
Histologically, two zones can be distinguished. A central zone composed of acellular cementum containing cementocytes and cementoclasts, and a peripheral zone with non-mineralised connective tissue containing cementoblasts.
The recommended treatment for cementoblastoma is surgical removal because even a small lesion will usually continue to grow slowly. Curettage, or even osteotomy, should follow removal to avoid the risk of recurrence. The tooth concerned, fused to the lesion, will therefore be sacrificed [20].
Cemento-osseous dysplasia (COD) is a benign fibro-osseous lesion of the jaws that can present in three different clinical forms: periapical (in the periapical region of the anterior mandibular teeth), focal (usually a single lesion in the posterior mandibular region), and florid (with multifocal distribution in the maxilla and mandible, often bilaterally and symmetrically). These lesions are characterised by the replacement of normal maxillary or mandibular bone by fibrous tissue, followed by cemento-osseous tissue that becomes increasingly calcified, depending on the stage of evolution.
Three radiological and histological stages can be identified depending on the amount of mineralised tissue: firstly, the osteolytic stage, which appears as a radiolucent lesion. This is followed by the cementoblastic stage, in which the tissue begins to calcify, revealing radiopaque centres within the lesion. Finally, the mature stage where, following total calcification of the tissues, the lesion appears totally radiopaque, dense, rounded and well-defined, with a radiolucent border around the periphery [21,22].
It is therefore the focal form of COD, which presents itself like the lesions in our patient: in the form of a solitary radio-opaque focus, located in the periapical region of the posterior mandibular teeth (86%). This form predominantly affects Afro-American women between the 3rd and 5th decades of life.
Clinically, patients are generally asymptomatic, and the teeth associated with the lesion are vital. Rarely, bone expansion may occur.
No treatment is therefore indicated for asymptomatic patients, but monitoring of the lesion’s progress is recommended.
The classic ossifying fibroma, a rare benign fibro-osseous tumour, can also present as a radio-opaque lesion localised in the posterior region of the mandible. There is a more aggressive juvenile form of this tumour, which is more often located in the maxilla and can therefore cause nasal obstruction, epistaxis and exophthalmos [23].
The classic form is diagnosed in young patients after adolescence, between the 2nd and 3rd decade, with a predominance of women. Periodontal ligament cells are thought to be responsible for the formation of osteoid and/or cementoid calcified tissue within the lesion, leading to its expansion. Clinically, the lesions are asymptomatic in their early stages, but the first symptoms are associated with the expansion of the lesion. Swelling followed by pain and tooth movement may appear [24]. Radiologically, OF is initially radiolucent, and then, as it evolves and accumulates deposits of calcified tissue, it features a radiodense appearance with ground-glass opacities [25]. A radiolucent border persists around the periphery of the lesion, even at an advanced stage, making it possible to differentiate it from a lesion with very similar histological characteristics, i.e., fibrous dysplasia.
The treatment for FO is total enucleation of the lesion followed by curettage until all particles have been removed from the lesion, thereby reducing the risk of recurrence. In the case of very extensive lesions, radical surgical resection may be necessary. The risk of recurrence remains low, but cases of malignant degeneration have been observed. Long-term follow-up of patients is therefore recommended.
Osteoblastoma is another very rare benign bone tumour: it accounts for less than 1% of all bone tumours and only involves the cranio-facial bones in 10% of cases. It mainly affects children and young adults, with a male predominance ratio of 2:1. Its preferred location in the maxilla is in the posterior mandible [26].
This tumour represents a proliferation of osteoblasts and therefore tends to grow following the deposition of bone tissue. Clinically, at an advanced stage, this can be seen as a swelling which can subsequently cause pain.
Radiologically, the lesion appears rounded, well-defined, radiolucent at first, mixed and finally radiodense following calcification of the tissue. It remains surrounded by a radiolucent halo [26]. Unlike cementoblastoma, the lesion is not fused to a dental apex.
The treatment for osteoblastoma is enucleation followed by curettage or resection. The risk of recurrence is low and may be due to incomplete treatment. There is a risk of malignant transformation, which is why it is important to remove the entire lesion and ensure long-term follow-up.
4. Conclusions
The incidental finding of intraosseous lesions of the jaws during dental radiography is frequent. In some cases, the signs are obvious and clinical and radiological data allow setting an accurate diagnosis. In other cases, such as the one we described herein, the aspect of the lesion is atypical and may correspond to many other lesions, which are very different in nature, and require either monitoring or more or less aggressive surgical treatment. For such reasons, a biopsy is sometimes necessary in order to establish a definitive diagnosis and carry out an appropriate treatment.
Author Contributions
Draft of the manuscript, A.P. and A.M.; patient treatment, A.P.; radiological interpretation, preparation of images, A.P. and T.L.; conception, diagnosis, and critical review of the manuscript, A.P. and T.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The presented study adhered to the Helsinki Declaration of ethical principles by the World Medical Association. The study did not require approval of the Ethics Commission on Human Research of Geneva (CCER-Geneva) according to the Federal Human Research Act (Art.3al.a) since the study involved less than five patients.
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
Data are contained within the article.
Acknowledgments
We wish to thank D. Baumhoer (Bone Tumour Reference Center, Basel) for having confirmed the diagnosis. We would like to express our gratitude to V. Lenoir (Geneva University Hospitals) for his expertise and assistance in shaping this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gamba, T.O.; Maciel, N.A.P.; Rados, P.V.; Da Silveira, H.L.D.; Arús, N.A.; Flores, I.L. The imaging role for diagnosis of idiopathic osteosclerosis: A retrospective approach based on records of 33,550 cases. Clin. Oral Investig. 2021, 25, 1755–1765. [Google Scholar] [CrossRef] [PubMed]
- Hlongwa, P.; Moshaoa, M.A.L.; Musemwa, C.; Khammissa, R.A.G. Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs. Int. J. Environ. Res. Public Health 2023, 20, 3479. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.; Yu, W. Incidental findings in a consecutive series of digital panoramic radiographs. Imaging Sci. Dent. 2020, 50, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, R.; Arias, A.; Astete, N.; Farfán, C.; Garay, I.; Dias, F. Prevalence and morphometric analysis of idiopathic osteosclerosis in a Chilean population. Folia Morphol. 2018, 77, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xu, L.; Cai, C.; Liu, Z.; Zhang, L.; Wang, C.; Xu, J. Longitudinal investigation of idiopathic osteosclerosis lesions of the jaws in a group of Chinese orthodontically-treated patients using digital panoramic radiography. J. Dent. Sci. 2022, 17, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Al-Habib, M.A. Prevalence and Pattern of Idiopathic Osteosclerosis and Condensing Osteitis in a Saudi Subpopulation. Cureus 2022, 14, e22234. [Google Scholar] [CrossRef]
- Geist, J.R.; Katz, J.O. The frequency and distribution of idiopathic osteosclerosis. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 388–393. [Google Scholar] [CrossRef]
- Ledesma-Montes, C.; Jiménez-Farfán, M.D.; Hernández-Guerrero, J.C. Idiopathic osteosclerosis in the maxillomandibular area. Radiol. Medica 2019, 124, 27–33. [Google Scholar] [CrossRef]
- Yesiltepe, S.; Bayrakdar, I.S.; Orhan, K.; Çelik, Ö.; Bilgir, E.; Aslan, A.F.; Odabaş, A.; Costa, A.L.F.; Jagtap, R. A deep learning Model for Idiopathic Osteosclerosis Detection on Panoramic Radiographs. Med. Princ. Pract. 2022, 6, 555–561. [Google Scholar] [CrossRef]
- Schulz, M.; Reichart, P.A.; Dula, K.; Bornstein, M. Focal osteosclerotic lesions of the jaws—A review focusing on diagnostic and therpeutic aspects. Schweiz. Monatsschrift Zahnmed. 2010, 120, 325–339. [Google Scholar]
- Ledesma-Montes, C.; Jiménez-Farfán, M.D.; Hernández-Guerrero, J.C. Maxillomandibular giant osteosclerotic lesions. J. Appl. Oral Sci. 2018, 26, e20170535. [Google Scholar] [CrossRef] [PubMed]
- Marques Silva, L.; Guimaraes, A.L.; Dilascio, M.L.; Castro, W.H.; Gomez, R.S. A rare complication of idiopathic osteosclerosis. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E233–E234. [Google Scholar] [PubMed]
- Green, T.L.; Walton, R.E.; Clark, J.M.; Maixner, D. Histologic examination of condensing osteitis in cadaver specimens. J. Endod. 2013, 39, 977–979. [Google Scholar] [CrossRef] [PubMed]
- Kosti, E.; Lambrianidis, T.; Chatzisavvas, P.; Molyvdas, I. Healing of a radiolucent periradicular lesion with periradicular radiopacity. J. Endod. 2004, 30, 548–550. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.S.F.; Bueno, M.R.; Yamamoto-Silva, F.P.; Gomez, R.S.; Peters, O.A.; Estrela, C. Differential diagnosis and clinical management of periapical radiopaque/hyperdense jaw lesions. Braz. Oral Res. 2017, 31, e52. [Google Scholar] [CrossRef]
- Alfahad, S.; Alostad, M.; Dunkley, S.; Anand, P.; Harvey, S.; Monteiro, J. Dense bone islands in pediatric patients: A case series study. Eur. Arch. Paediatr. Dent. 2021, 22, 751–757. [Google Scholar] [CrossRef]
- Takata, T.; Slootweg, P.J. Odontogenic and maxillofacial bone tumours. In WHO Classification of Head and Neck Tumours, 4th ed.; El-Naggar, A.K., Chan, J.K., Grandis, J.R., Takata, T., Slootweg, P.J., Eds.; IARC: Lyon, France, 2017. [Google Scholar]
- Barnes, L.; Everson, J.W.; Reichart, P.; Sidransky, D. (Eds.) Pathology and Genetics of Head and Neck Tumours; World Ahealth Organization Classification of Tumours; IARC: Lyon, France, 2005. [Google Scholar]
- Xu, L.; Liu, Y.; Luo, J.; Jiang, M.; Guo, W.; Zheng, G. Analysis of clinical and imaging findings in cementoblastoma. Hua Xi Kou Qiang Yi Xue Za Zhi 2015, 33, 419–422. (In Chinese) [Google Scholar] [CrossRef]
- Pathak, J.; Hosalkar, R.M.; Sidana, S.; Swain, N.; Patel, S. Benign cementoblastoma involving left deciduous first molar: A case report and review of literature. J. Oral Maxillofac. Pathol. 2019, 23, 422–428. [Google Scholar] [CrossRef]
- Brannon, R.B.; Fowler, C.B.; Carpenter, W.M.; Corio, R.L. Cementoblastoma: An innocuous neoplasm? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 311–320. [Google Scholar] [CrossRef]
- Brad, W.N.; Douglas, D.D.; Carl, M.A. Chir-Oral and Maxillofacial Pathology-Saunders, 4th ed.; Saunders: London, UK, 2015. [Google Scholar]
- Kawai, T.; Hiranuma, H.; Kishino, M.; Jikko, A.; Sakuda, M. Cemento-osseous dysplasia of the jaws in 54 Japanese patients: A radiographic study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 87, 107–114. [Google Scholar] [CrossRef]
- Hentati, H.; Njim, L. Fibrome ossifiant mandibulaire associé à une canine incluse. Médecine Buccale Chir. Buccale 2013, 19, 127–130. [Google Scholar] [CrossRef][Green Version]
- Pérez-García, S.; Berini-Aytés, L.; Gay-Escoda, C. Ossifying fibroma of the upper jaw: Report of a case and review of the literature. Med. Oral. 2004, 9, 333–339, (In English, Spanish). [Google Scholar] [PubMed]
- Kaplan, I.; Nicolaou, Z.; Hatuel, D.; Calderon, S. Solitary central osteoma of the jaws: A diagnostic dilemma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, e22–e29. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).