Dear Editors: Giant congenital melanocytic naevus (GCMN)-associated melanoma in adults is very rare [1]. We here report an adult male with fatal GCMN-associated melanoma despite the initiation of combined immunotherapy (Figure 1).

Figure 1.
An adult male with congenital giant melanocytic nevus presenting as huge brownish-black partly hairy bathing trunk nevus including several tumorous nodules (arrow head, (a,b)). Moreover, there were countless satellite nevi on the entire body.
A 28-year-old male refugee from Syria presented with increasing abdominal pain over a three-week period. The patient as well as his family had no history of cancers. Dermatological examination revealed a huge CGMN presenting as huge brownish black, partly hairy bathing trunk nevus including several tumorous nodules. There were countless satellite nevi on the entire body. Moreover, there were huge skin folds with neurofibromatosis-like appearance (Figure 2) [1].

Figure 2.
A closer look at a congenital giant melanocytic nevus (bathing trunk subtype) showing huge skin folds with neurofibromatosis-like appearance.
Abdominal and thoracic computed tomography revealed a partly necrotic abdominal/retroperitoneal tumor conglomerate with displacement of the urinary bladder. Evidence for metastatic disease was also detected intrapulmonal, mediastinal bihilar, hepatic, and osseal. Cranial magnetic resonance imaging, including axial pre- and post-contrast T1-weighted images, did not reveal signs for neurocutaneous melanosis or metastatic disease. However, serum lactate dehydrogenase and S100B were significantly elevated with 486 U/L (135–225) and 2.66 µg/L (<0.15).
Histopathology of two nodules excised from the lower back and right buttock revealed similar findings, including dermal monomorphic small epithelioid and spindle cell shaped melanocytes and melanophages, reaching down to the subcutaneous tissue. Underneath there was a partly necrotic nodule including large melanocytes with atypia, prominent nucleoli, and increased and atypical mitoses (Figure 3a–c).
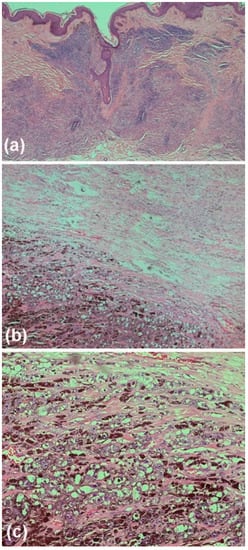
Figure 3.
Histopathology of two nodules excised from the lower back and right buttock revealed similar findings, including dermal monomorphic small epithelioid and spindle cell shaped melanocytes and melanophages, reaching down to the subcutaneous tissue (a). Underneath there was a partly necrotic nodule including large melanocytes with atypia, prominent nucleoli, and increased and atypical mitoses (b,c).
The entire lesion was strongly positive for S100B and Melan-A, whereas the deep atypical part also showed in Ki-67 positive melanocytes loss of 5-hydroxymethylcytosine and H3K27me3 expression (Figure 4).
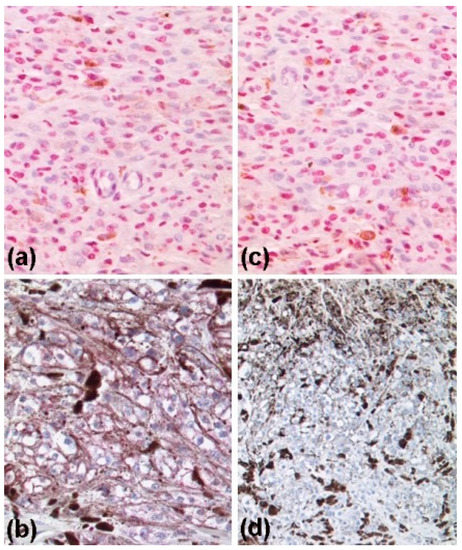
Figure 4.
Immunohistochemitry of a tumor nodule revealing almost complete loss of H3K27me3 (a,b) and 5-hydroxymethylcytosine (c,d) expression in the malignant deep part (b,d) of the tumor when compared to the upper benign part of the melanocytic tumor (a,c).
PD-L1 expression was <1%. Mutation analysis did reveal wildtypes for BRAF, NRAS, and KIT genes. Immunotherapy with ipilimumab (3 mg/kg body weight) and nivolumab (1 mg/kg body weight) every three weeks was recommended. However, 14 days following the first immunotherapy cycle the patient deceased from rapid tumor progression and septic complications.
A nevus with a projected adult size greater than 40 cm is classified as GCMN, as in our case. The clinical risk factors associated with the development of melanoma in patients with GCMN include childhood, truncal involvement, numerous satellite nevi, and nevi located over the posterior axis [2]. Scard et al. [3] recently showed in a systematic review that most melanomas in patients with congenital melanocytic nevi occur early in life. In fact, a higher risk of melanoma onset was observed in the first year of life, in the groups defined by small or medium as well as large or GCMN. For the large and giant categories, a higher risk before 3 years of age was already known [2]. Hence, melanoma development in adult patients with GCMN is considered a rarity [2,3]. Moreover, melanomas arising in congenital melanocytic nevi appear as a dermal/deep-seated melanoma with histopathologic features difficult to distinguish from cutaneous melanoma metastasis or proliferative nodules which often represent a diagnostic challenge given a close resemblance to malignant melanoma [3,4]. In the present case, however, it was not difficult to diagnose melanoma in the deep part of the GCMN using routine histopathology. Moreover, the proliferating melanocytes in the deep nevus part showed loss of 5-hydroxymethylcytosine and H3K27me3 expression which is a hallmark for melanoma [5,6,7]. According to recent research, NRAS gene mutation is the main driving factor in GCMN [8]. Due to the absence of druggable mutations and tumoral PD-L1 expression, we initiated combined immunotherapy which could unfortunately not prevent the early fatal outcome in the present case.
Conclusively, we reported this tragic case because of the rarity of adult-onset melanoma in GCMN and to highlight the need for melanoma assessments and rigorous follow-up in adult patients with GCMN as well.
Author Contributions
Conceptualization, T.G.; methodology, T.G.; investigation, T.G., K.N., Y.A., M.N., A.R. and S.B.; writing—original draft preparation, T.G.; visualization, T.G., M.N. and A.R.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from the patient presented.
Data Availability Statement
Not applicable.
Conflicts of Interest
T.G. has received speakers and/or advisory board honoraria from BMS, Sanofi-Genzyme, MSD, Novartis Pharma, Roche, Abbvie, Almirall, Janssen, Lilly, Pfizer, Pierre Fabre, and Merck-Serono, outside the submitted work. The other authors have no conflicts of interest to declare.
References
- Boyers, L.N.; Karimkhani, C.; Stevens, E.; High, W.A. Innumerable nevi with giant congenital melanocytic nevus clinically mimicking neurofibromatosis: A diagnostic challenge. JAAD Case Rep. 2015, 1, 241–243. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.; Shin, H.T.; Choi, Y.; Lee, D.Y. Evolutionary processes of melanomas from giant congenital melanocytic nevi. Pigment. Cell Melanoma Res. 2020, 33, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Scard, C.; Aubert, H.; Wargny, M.; Martin, L.; Barbarot, S. Risk of melanoma in congenital melanocytic nevi of all sizes: A systematic review. J. Eur. Acad. Derm. Venereol. 2023, 37, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ricci, C.; Ambrosi, F.; Grillini, M.; Serra, M.; Melotti, B.; Gruppioni, E.; Altimari, A.; Fiorentino, M.; Dika, E.; Lambertini, M.; et al. Next-generation sequencing revealing TP53 mutation as potential genetic driver in dermal deep-seated melanoma arising in giant congenital nevus in adult patients: A unique case report and review of the literature. J. Cutan. Pathol. 2020, 47, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Busam, K.J.; Shah, K.N.; Gerami, P.; Sitzman, T.; Jungbluth, A.A.; Kinsler, V. Reduced H3K27me3 Expression Is Common in Nodular Melanomas of Childhood Associated with Congenital Melanocytic Nevi but Not in Proliferative Nodules. Am. J. Surg. Pathol. 2017, 41, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Pavlova, O.; Fraitag, S.; Hohl, D. 5-Hydroxymethylcytosine Expression in Proliferative Nodules Arising within Congenital Nevi Allows Differentiation from Malignant Melanoma. J. Investig. Dermatol. 2016, 136, 2453–2461. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Sand, M.; Skrygan, M. Loss of 5-hydroxymethylcytosine and ten-eleven translocation 2 protein expression in malignant melanoma. Melanoma Res. 2013, 23, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Aimaier, R.; Chung, M.; Zhu, H.; Yu, Q. Spatiotemporal expression of NRAS and occurrence of giant congenital melanocytic nevi. Exp. Dermatol. 2022, 31, 582–585. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).