Dear Editors: Pityriasis lichenoides-like mycosis fungoides (MF) is a rare variant of MF, presenting clinical findings of pityriasis lichenoides (PL) but histological features of MF [1,2,3,4,5,6]. This is a case report, in the form of a letter to the editor, presenting an elderly patient with pityriasis lichenoides-like CD8+ mycosis fungoides, which is an uncommon variant of MF. It is stressed that the PL clinical characteristics resembled in the case of a PL-like MF, are of diagnostic and prognostic relevance.
A 67-year-old female presented to our department with a 2-month history of multiple slightly itchy scaly pinkish maculopapular lesions on the extremities (Figure 1).
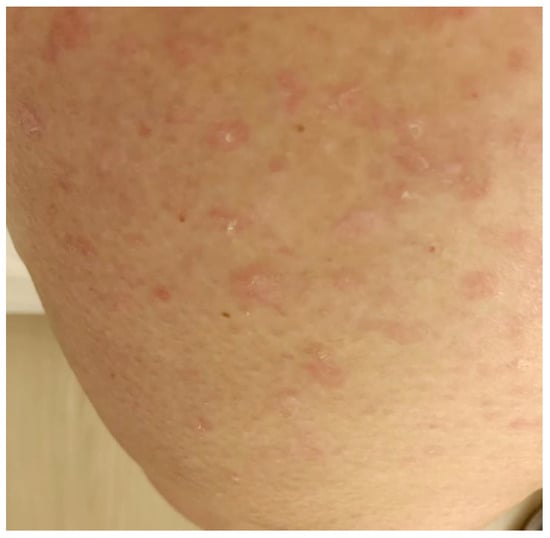
Figure 1.
A female patient with scaly reddish-pinkish maculopapules on the right thigh.
Clinically, we suspected PL chronica. However, histopathology revealed hyperparakeratosis and prominent epidermotropism of atypical lymphocytes forming Pautrier’s microabscesses (Figure 2). Immunohistochemically, the infiltrating lymphocytes were mainly positive for CD8 (Figure 3) with the coexpression of CD3 and CD5 and an almost complete loss of CD7 expression. CD20 and CD30 were not expressed.
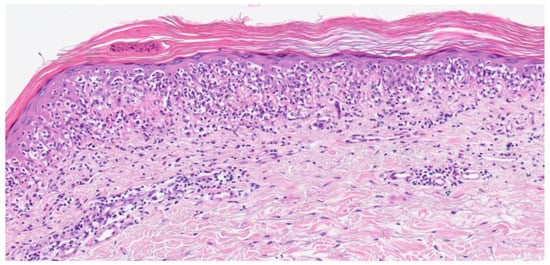
Figure 2.
Hematoxylin-eosin stain revealed hyperparakeratosis and prominent epidermotropism of atypical lymphocytes also forming Pautrier’s microabscesses (×200).
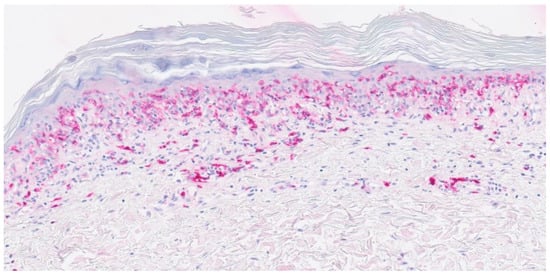
Figure 3.
The infiltrating lymphocytes of the epidermis were mainly positive for CD8 on immunohistochemistry (×200).
T-cell receptor gene rearrangement analysis (multiplex-PCR, BIOMED-2) demonstrated the rearrangement of the gamma chain (tube A: 219 bp; tube B: 177 bp, 176 bp). Complete work-up including lymph node ultrasound, abdominal and thoracic computed tomography, cranial magnetic resonance imaging, blood smear, and bone marrow biopsy did not reveal evidence for the spread of lymphoma spread. Flow cytometry of peripheral blood revealed a decreased CD4/CD8 ratio with an increase in CD8+ CD7-cells and decrease in CD4+ cells. PL-like CD8+ MF was diagnosed. For staging purposes, we adopted the ISCL/EORTC classification for MF and Sezary syndrome (T2aN0M0B1b stage IB) [7]. The patient was started on tapered systemic prednisolone (starting dose: 150 mg) and narrowband ultraviolet B (NBUVB) phototherapy thrice weekly using a Waldmann UV7002-K cabin (Waldmann GmbH & Co. KG, Villingen-Schwenningen, Germany). The initial NBUVB of 0.1 J/cm2 was increased every second procedure by 0.1 J/cm2. Complete clearance of skin lesions was observed after 12 weeks of treatment (cumulative NBUVB dose: 6.8 J/cm2). Due to the the involvement of peripheral blood, we planned extracorporeal photopheresis (ECP), starting with two procedures every other week [8].
The scope of PL presentations is delineated along a continuum of several variants, including PL et varioliformis acuta, PL chronica, and febrile ulceronecrotic Mucha-Habermann disease [1]. Patients previously reporting with PL-like MF exhibited some features distinct from classic MF, including a higher incidence in male children and predominantly CD8+ T cell infiltration. However, in most previous reports, it was not mentioned which PL variant was clinically observed, although this may be of diagnostic as well as prognostic relevance [2,3]. A good response to phototherapy and a favourable prognosis may be expected. Based on previous cases, most patients received NBUVB phototherapy or psoralen combined with ultraviolet A, and demonstrated either a complete or partial response with late recurrences in only two cases [6]. The early involvement of blood in the present case may indicate a more unfavourable prognosis requiring systemic directed therapies such as ECP [8]. Indeed, the most important differential diagnosis of PL-like CD8+ MF is primary cutaneous aggressive epidermotropic CD8+ cytotoxic T cell lymphoma (CTCL) which has a much more rapid and aggressive clinical course with early ulcerating and necrotising papules, plaques, and tumours [9]. PL-like CD8+ MF and primary cutaneous aggressive epidermotropic CD8+ CTCL share common histological features, the distinction between both conditions must be made predominantly based on clinical features; therefore, disease history, and complete work-up results. In the present case, the PL chronica-like appearance of skin lesions did not suggest a diagnosis of epidermotropic CD8+ CTCL. Importantly however, PL et varioliformis acuta-like or febrile ulceronecrotic Mucha-Habermann disease-like appearance would have been a clinical challenge in this setting since epidermotropic CD8+ CTCL may present in a similar clinical picture [1,2,3,4,5,6]. Another differential diagnosis represents type D lymphomatoid papulosis which is typically composed of CD8+ lymphocytes. However, CD30 expression is often reserved, and the clinical picture differs from PL [10].
In conclusion, PL-like CD8+ MF is usually associated with an indolent course and, in most patients, skin-directed therapies were found to be efficient in controlling the disease. Clinicians should be aware of this rare presentation of MF that may be misdiagnosed as some other skin conditions.
Author Contributions
Conceptualization, T.G.; methodology, T.G., C.H. and N.D.; investigation, T.G., E.H., C.H., N.D. and S.B.; writing—original draft preparation, T.G.; visualization, T.G, C.H. and N.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Khachemoune, A.; Blyumin, M.L. Pityriasis lichenoides: Pathophysiology, classification, and treatment. Am. J. Clin. Dermatol. 2007, 8, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.B.; Youn, S.H.; Park, E.J.; Kwon, I.H.; Kim, K.J. CD8-positive pityriasis lichenoides-like mycosis fungoides. Eur. J. Dermatol. 2012, 22, 415–416. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.S.; Kang, D.Y.; Bin Park, J.; Kim, J.H.; Park, K.A.; Rim, H.; Suh, K.S. Pityriasis Lichenoides-like Mycosis Fungoides: Clinical and Histologic Features and Response to Phototherapy. Ann. Dermatol. 2016, 28, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Mohd Amin, S.N.; Muhamad, R.; Wan Abdullah, W.N.H.; Mohd Zulkifli, M.; Bakrin, I.H.; Tangam, T. A Case Report of Pityriasis Lichenoides-Like Mycosis Fungoides in Children: A Challenging Diagnosis. Korean J. Fam. Med. 2021, 42, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-H.; Hsiao, C.-H.; Hsiao, P.-F.; Chu, C.-Y. Adult pityriasis lichenoides-like mycosis fungoides with high density of CD8-positive T-lymphocytic infiltration. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 401–402. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.L.; Chen, Y.J.; Weng, Y.C.; Yang, C.S.; Juan, I.K. Pityriasis Lichenoid-like Mycosis Fungoides in a 9-year-old Boy: A Case Report. Acta Dermatovenerol. Croat. 2019, 27, 37–39. [Google Scholar] [PubMed]
- Olsen, E.; Vonderheid, E.; Pimpinelli, N.; Willemze, R.; Kim, Y.; Knobler, R.; Zackheim, H.; Duvic, M.; Estrach, T.; Lamberg, S.; et al. Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: A proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC). Blood 2007, 110, 1713–1722. [Google Scholar] [PubMed]
- Gambichler, T.; Späth, J.; Said, S.; Scheel, C.H.; Susok, L.; Stranzenbach, R. Outcome of extracorporeal photopheresis in mycosis fungoides patients is not predicted by quotients of systemic immune-inflammatory biomarkers. J. Clin. Apher. 2022, 37, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Robson, A.; Assaf, C.; Bagot, M.; Burg, G.; Calonje, E.; Castillo, C.; Cerroni, L.; Chimenti, N.; Dechelotte, P.; Franck, F.; et al. Aggressive epidermotropic cutaneous CD8+ lymphoma: A cutaneous lymphoma with distinct clinical and pathological features. Report of an EORTC Cutaneous Lymphoma Task Force Workshop. Histopathology 2015, 67, 425–441. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.N.; Blessing, M.M.; Marcogliese, A.N.; Vega, F.; Prose, N.; Metry, D. Childhood lymphomatoid papulosis Type D, a rare and challenging diagnosis. Pediatr. Dermatol. 2022. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).