Simple Summary
Active breathing control (ABC), voluntary deep inspiration breath hold (vDIBH), and surface-guided radiation therapy (SGRT) are three breath-hold techniques that can be used in the treatment of left-sided breast cancer. Their quality-of-life impact was compared to each other using the European Organization for Research and Treatment of Cancer QoL questionnaire (EORTC QLQ-C30) at baseline, last fraction and 6–8 weeks follow-up. Although vDIBH was found to have the worst pain compared to ABC and the worst social function compared to SGRT at 6–8 weeks, all breath-hold techniques were comparable in quality-of-life impact when accounting for the limitations of this study.
Abstract
Purpose: This study aimed to compare QoL outcomes among patients undergoing active breathing control (ABC), voluntary deep inspiration breath hold (vDIBH), and surface-guided radiation therapy (SGRT). Methods: This was a non-randomized, three-arm clinical trial in which 55 patients were sequentially allocated to ABC (n = 19), SGRT (n = 20), or vDIBH (n = 16). QoL was assessed using the European Organization for Research and Treatment of Cancer QoL questionnaire (EORTC QLQ-C30) at baseline, treatment completion, and 6–8 weeks post-treatment. Linear regression was used to compare changed scales in QoL domains across groups. A p-value of <0.05 was considered statistically significant. Results: Baseline QoL scores were high across all groups, with physical functioning being the highest-rated domain and global health status the lowest. Fatigue, pain, and insomnia were the most highly reported symptoms at all time points. At 6–8 weeks, social functioning improved significantly in SGRT compared to vDIBH (16.67 vs. −12.50, p = 0.0053). Patients in the vDIBH group reported significantly increased pain compared to ABC at 6–8 weeks (p = 0.0240). No other significant differences were observed in QoL changes between the groups. Conclusions: The three breath-hold techniques maintained overall QoL with no differences between the groups, except for pain between vDIBH and ABC and social functioning for vDIBH and SGRT both at 6–8 weeks of follow-up. Despite the limitations of this study, each breath-hold technique has demonstrated comparable impact on QoL in patients with left-sided breast cancer and each could be used as a viable option with respect to QoL.
1. Introduction
Radiation therapy following breast-conserving surgery or mastectomy achieves excellent local control and survival [1,2]. However, it is associated with increased risk of cardiovascular disease, especially for patients undergoing treatment for left-sided breast cancer [3,4]. Darby et al. reported a significantly higher cardiac mortality ratio in patients with left-sided tumours compared to right-sided tumours [3].
Breath-holding techniques have emerged as effective strategies to reduce cardiac radiation dose by increasing the separation between the heart and the chest wall [5]. Among these, active breathing control (ABC) and voluntary deep inspiration breath hold (vDIBH) have demonstrated reductions in cardiac toxicity [4,6,7]. ABC uses a device to maintain a controlled breath hold, while vDIBH allows patients to hold their breath voluntarily, with imaging ensuring consistent positioning during treatment. Both methods are comparable in positional reproducibility and normal tissue sparing [8].
Consistent positioning and inter-fraction reproducibility are crucial for delivering cardiac-sparing treatments. Surface-guided radiation therapy (SGRT), which tracks the position of a portion of the skin surface, has emerged as an effective tool to enhance accuracy and reproducibility [9]. SGRT has been shown to avoid early radiation-associated cardiac perfusion defects, even in patients receiving radiation to the internal mammary lymph nodes [10].
While patients are instructed to take a deep breath in both vDIBH and SGRT, vDIBH uses visual confirmation by placing skin marks on patients when in SGRT; a system called AlignRT tracks the patient’s position with a 3D camera—avoiding the use of skin marks. On the other hand, ABC involves using a spirometer that forcibly holds one’s breath. The differences in set up for each of the breath-hold techniques may cause quality-of-life (QoL) impact among patients who use the different devices. A technique demonstrating better QoL would be preferred in clinical practice if the cardiac sparing in each is equivalent. However, a study comparing the QoL between different breath-hold groups has not been conducted.
Furthermore, the literature currently shows contrasting findings regarding QoL for breath-hold techniques. Two studies investigating anxiety with ABC found contradictory results, with one describing over half of their participants having high anxiety during the treatment related to the device [11], while another reported low anxiety throughout treatment with no device-related distress [12]. A qualitative study examining the experiences of patients undergoing SGRT found that patients had anxiety and physical discomfort with the breath-hold technique [13].
While the current literature shows contrasting results for patient anxiety with breath-hold techniques, it fails to expand on other domains of QoL. Thus, this study aimed to compare the QoL of patients who underwent three different breath-hold techniques—ABC, vDIBH, and SGRT—during left-sided breast radiation therapy.
2. Methods
2.1. Study Design
The inclusion criteria, radiotherapy and breath-hold techniques have been previously described in publications by our group [14,15]. This was a non-randomized 3-armed clinical trial (NCT03459898) [16], where patients were sequentially allocated in groups of 20 from May 2018–February 2021 to the three breath-hold techniques in the following order: vDIBH, ABC, and SGRT. Patients were included if they (1) were 18 or above, (2) required adjuvant left chest wall or breast irradiation after mastectomy or lumpectomy for breast cancer, (3) had Eastern Cooperative Oncology Group performance status < 3, and (4) were able to maintain a breath-hold of 15 s or longer. Exclusion criteria were (1) partial breast irradiation and (2) the need for bolus, as it makes surface tracking difficult. The study was approved by the local Research Ethics Board.
2.2. Breath-Hold Techniques
A previous study by our group reported the techniques in detail [14,15]. To summarize, the vDIBH group had a high-resolution camera in the treatment bunker to visualize the marks for breath-hold reproduction. The ABC group had the Elekta apparatus, which included a spirometer to regulate each breath-hold for a specific duration. The SGRT group used the AlignRT® (Vision RT, Dallas, TX, USA) system, which is a surface-imaging system [14,15].
2.3. QOL Tools
The QoL was assessed with the European Organization for Research and Treatment of Cancer (EORTC) core QoL questionnaire (QLQ-C30), which is a well-validated and widely used QoL questionnaire available in multiple languages [17,18]. The QLQ-C30 is composed of 30 questions that represent 5 functional scales (physical, role, cognitive, emotional and social), 3 symptom scales (fatigue, nausea and vomiting, and pain), and a global health/QoL scale. For the QLQ-C30 functioning scales and global health score, higher values indicated better QoL. With the symptom scales, lower values depict better QoL. The patients completed the QLQ-C30 at the time of radiation simulation at baseline, at completion of their radiation and at the 6–8 weeks follow-up appointment.
2.4. Statistical Analysis
Descriptive analysis of each breath-hold group was summarized by mean, standard deviation (SD), median (interquartiles) and range for each functional, symptom and global health scale of the EORTC QLQ-C30. The change in QoL over time was calculated from the last fraction and 6–8 weeks follow-up minus the baseline. Negative change indicated that the score decreased from baseline. To compare changes in EORTC QLQ-C30 scores between the 3 breath-hold techniques, 2-sample independent t-tests were performed to compare the changes in each QoL domain between the techniques in a pairwise fashion, first for the last fraction time point and then for the 6–8 weeks follow-up time point. A p-value of <0.05 was considered significant. All analyses were conducted by Statistical Analysis Software (SAS version 9.4, Cary, NC, USA) and R package (v4.3.0).
3. Results
Of the 60 patients recruited for the study, 5 withdrew, giving a total of 55 at baseline divided into the three breath-hold groups: 19 ABC, 20 SGRT, and 16 vDIBH. Due to non-compliance or missed appointments, the number of patients at the last review and 6–8 weeks follow-up was mainly reduced from baseline (Figure 1). The amount included in the changed-scales analysis are representative of the number of patients at the last review and 6–8 weeks follow-up, except for vDIBH. In this group, there was one participant who lacked baseline data for all but the physical functioning scale and thus, the number of patients included in the last review and 6–8 weeks changed-scales analysis for the remaining domains were 12 and 8, respectively.

Figure 1.
Flow diagram of participants included in each breath-hold technique for the baseline, last fraction, and 6–8 weeks follow-up. Abbreviations: ABC = active breathing control, SGRT = surface-guided radiation therapy, vDIBH = voluntary deep inspiration breath-hold.
The demographics of the included participants are described in our previous publications [14,15]. The mean (IQR) age was 55 (46–64) years (Table 1). The majority of patients had breast-conserving surgery in all three breast hold groups (ABC: 78.9%, SGRT: 60%, vDIBH: 93.7%). The most common fractionation was 42.56 Gy/15 fractions (81.8%), followed by 50 Gy/25 fractions (12.7%) and 40.05 Gy/15 fractions (5.5%). Forty-nine percent had tangents only, and 51% were treated with 3–4 fields. The distribution of each demographic amongst the three groups can be seen in Table 1.

Table 1.
Baseline characteristics amongst the three breath-hold groups. Abbreviations: ABC = active breathing control, SGRT = surface-guided radiation therapy, vDIBH = voluntary deep inspiration breath-hold.
3.1. Descriptive Analysis of EORTC QLQ-C30 Scales
The baseline scores demonstrated high QoL amongst the participants with scores over 70 in all breath-hold groups for physical functioning, role functioning, emotional functioning, cognitive functioning and social functioning (Figure 2). The highest functioning scale at baseline was physical functioning across the three groups. Likewise, global health status had the lowest QoL at baseline for the three groups. Graphs of the mean change quality of life are presented in Figure 2.
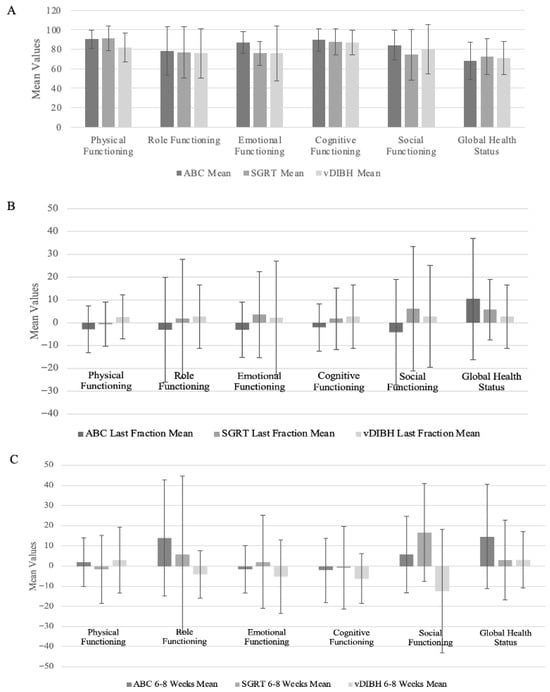
Figure 2.
(A) Bar graph of baseline mean values for the functioning and global health scales of the EORTC QLQ-C30 between the three breath-hold groups. Error bars represent the standard deviation for each mean. Higher scores indicate better quality of life. (B,C) Bar graph of mean change in quality of life for the functioning and global health scales of the EORTC QLQ-C30 between the three breath-hold groups at the last fraction (B) and 6–8 weeks follow-up (C). Error bars represent the standard deviation for each mean. Positive values indicate improved quality of life. Abbreviations: ABC = active breathing control, SGRT = surface-guided radiation therapy, vDIBH = voluntary deep inspiration breath-hold.
At baseline, the most prominent symptoms were fatigue, pain, and insomnia with mean scores over 15 in each breath-hold group (Figure 3). The symptom with the highest baseline QoL was insomnia in all three groups. Nausea/vomiting had the lowest QoL for the symptom scale in ABC, diarrhea had the mean lowest mean QoL in SGRT, and both were the lowest in vDIBH. The mean changed scales in symptoms are presented in Figure 3.
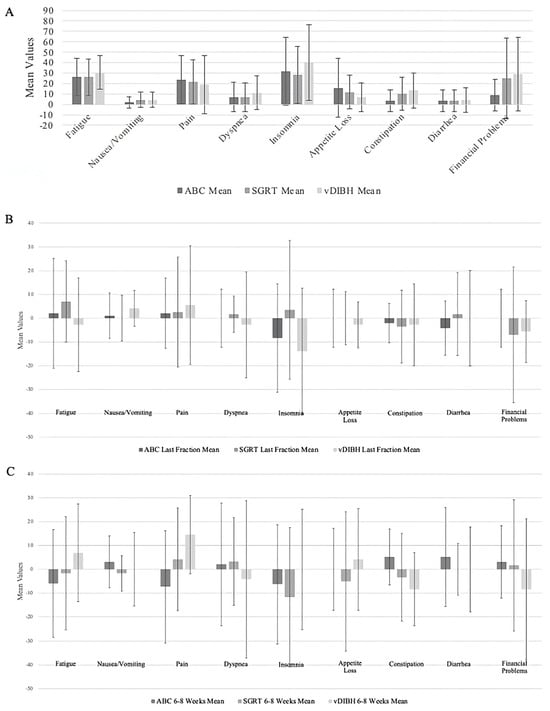
Figure 3.
(A) Bar graph of baseline mean values for the symptom scales of the EORTC QLQ-C30 between the three breath-hold groups. Error bars represent the standard deviation for each mean. Lower scores indicate better quality of life. (B,C) Bar graph of mean change in quality of life for the symptom scales of the EORTC QLQ-C30 between the three breath-hold groups at last fraction (B) and 6–8 weeks follow-up (C). Error bars represent the standard deviation for each mean. Negative values indicate improved quality of life. Abbreviations: ABC = active breathing control, SGRT = surface-guided radiation therapy, vDIBH = voluntary deep inspiration breath-hold.
3.2. Comparison of the Breath-Hold Techniques at Last Fraction Compared to Baseline
There were no significant differences with change in QoL from baseline to last fraction between the three breath-hold techniques for the EORTC C30 functioning, symptoms and global health status (Table 2) on pairwise testing.

Table 2.
Comparison of the three breath-hold techniques for EORTC QLQ-C30 changed scales from baseline. Significant values are indicated with an asterisk. Abbreviations: ABC = active breathing control, SGRT = surface-guided radiation therapy, vDIBH = voluntary deep inspiration breath-hold.
3.3. Comparison of the Breath-Hold Techniques at 6–8 Weeks Follow-Up Compared to Baseline
Patients with vDIBH were more likely to have increased pain symptoms at 6–8 weeks follow-up from baseline when compared with ABC (p = 0.0240). There was no significant difference in the pain-changed scales between ABC vs. SGRT and vDIBH vs. SGRT (Table 2).
There was also a significant difference for the social functioning domain between SGRT and vDIBH. Patients with SGRT were more likely to have increased social functioning compared to those with vDIBH after 6–8weeks of follow-up from baseline (p = 0.0053). There was no significant difference between ABC vs. vDIBH or SGRT vs. ABC for social functioning (Table 2).
With the other domains, symptoms and global health status, there was no significant difference between the three breath-hold techniques at 6–8 weeks follow-up compared to baseline (Table 2).
4. Discussion
This is the first study to report on QoL outcomes regarding different breath-hold techniques for left-sided breast cancer radiation. Each breath-hold technique was shown to be well-tolerated from baseline to completion of radiation. There were no significant differences between the breath-hold techniques, except for pain between vDIBH and ABC at 6–8 weeks of follow-up and social functioning for vDIBH and SGRT, also at 6–8 weeks of follow-up.
The questions in the EORTC QLQ-C30 that pertain to social functioning discuss treatment interfering with family or social activities. It is plausible that SGRT reduced the overall treatment time, allowing patients to better engage in their social activities, when compared to vDIBH [19]. However, it is unlikely that the magnitude of the difference was this large and it is more probable that this significant difference was due to other confounding factors. The vDIBH group had the smallest patient sample size at the 6–8 weeks follow-up, with only 8 patients being included for the social functioning analysis compared to 20 for the SGRT group, which may have skewed the results. Likewise, the difference in pain may have been due to factors other than the breath-hold techniques, such as type of surgery, adverse events from radiation and differences in patient healing [20].
Overall, the three breath-hold techniques are broadly equivalent with respect to QoL. Across the three treatment groups, the EORTC QLQ-C30 scores at baseline showed similar patterns to other patients with breast cancer as well as the general population [21,22]. With minimal changes detected across the scales, each breath-hold technique demonstrated preserved quality of life for the breast cancer patients after their radiation treatment. Furthermore, unlike previous studies that have reported increased anxiety with ABC and SGRT [11,13], the scores for the emotional functioning scale of the EORTC QLQ-C30, which includes an item on worry, had minimal changes at the completion of treatment for each breath-hold group in this study.
Cashell et al. and Dower et al., two studies that found increased anxiety with ABC and SGRT, respectively, both prepared questionnaires specific to the breath-hold experience [11,13]. It is possible that their specific questions and inclusion of more open-ended questions were able to elucidate the anxiety provoked from the breath-hold techniques more than the EORTC QLQ-C30. However, Beaton et al. also employed a breath-hold specific questionnaire and found that patients reported little to no anxiety with ABC throughout three time points: planning, second week of treatment and third week of treatment, which coincides with the results of this study [12]. It is possible that the differences in anxiety seen across these studies may be related to differences in age—as younger patients reported increased anxiety—and institutional practices, such as having practice sessions with the device [11].
Limitations
A limitation of this study includes the attrition of the participants. Fifty-five patients were included, but this was further diminished through follow-up attrition with 45–46 remaining at the 6–8 weeks follow-up. The vDIBH group especially was affected by this, with 9 of the 16 completing the 6–8 weeks follow-up. This may have influenced the significant differences seen. Additionally, confounding factors, such as type of breast cancer treatment and co-morbidities, may have affected the interpretation of the results. The type of systemic treatment patients were on that were not recorded in this study could have had an impact on their quality of life; for example, feeling uncomfortable from the hot flashes or musculoskeletal pain caused by hormonal treatment or tiredness from neoadjuvant chemotherapy.
Limitations within the study design also exist. Firstly, this study was non-blinded, which could lead to potential participant bias. The small sample size of 55 with less than or equal to 20 participants in each breath-hold group was another limitation. This prevented using more robust statistical analysis, including a mixed-effect model or including confounding factors into the comparisons. Lastly, the EORTC QLQ C30 is general and not breast-specific. It included many items that were unlikely to be affected by breast radiation therapy, such as cognition, constipation, diarrhea and nausea/vomiting. Although breast-specific QoL questionnaires, like the EORTC QLQ-BR42, exist, they also ask questions that are specific to other aspects of breast oncology—hormone therapy, chemotherapy and surgery [23]. Since many questions were not related to radiation, the general questionnaire of EORTC QLQ C30 was chosen for the study but created the limitation of not asking breast-specific questions for the three breath-hold groups.
5. Conclusions
Each breath-hold technique demonstrated comparable impact on QoL in patients with left-sided breast cancer. The differences observed in the study are more likely to be due to the limitations in the study itself than the differences between the groups. Any of the investigated breath-hold techniques could be used as a viable option with respect to QoL and patient education around the various breath-hold techniques could include their comparable QoL impact.
Author Contributions
Guarantor of integrity of entire study, all authors. Study concepts and design, all authors. Literature research, A.W.C., A.H., M.W. and I.K. Clinical studies, A.H., H.C., M.M., D.V., M.W. and I.K. Experiment studies/data analysis, all authors. Statistical analysis, L.Z. Manuscript preparation, C.H., A.W.C. and I.K. Manuscript editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Sunnybrook Research Ethics Board. All participants provided informed consent regarding the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
Hanbo Chen received an honorarium from Novartis. Irene Karam received an honorarium for the EMD Serono advisory board on locally advanced head and neck cancers in November 2023. There are no other conflicts of interest.
References
- EBCTCG (Early Breast Cancer Trialists’ Collaborative Group); McGale, P.; Taylor, C.; Correa, C.; Cutter, D.; Duane, F.; Ewertz, M.; Gray, R.; Mannu, G.; Peto, R.; et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: Meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 2014, 383, 2127–2135. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005, 366, 2087–2106. [Google Scholar] [CrossRef]
- Darby, S.C.; McGale, P.; Taylor, C.W.; Peto, R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005, 6, 557–565. [Google Scholar] [CrossRef]
- Smyth, L.M.; Knight, K.A.; Aarons, Y.K.; Wasiak, J. The cardiac dose-sparing benefits of deep inspiration breath-hold in left breast irradiation: A systematic review. J. Med. Radiat. Sci. 2015, 62, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Aznar, M.C.; Carrasco de Fez, P.; Corradini, S.; Mast, M.; McNair, H.; Meattini, I.; Persson, G.; van Haaren, P. ESTRO-ACROP guideline: Recommendations on implementation of breath-hold techniques in radiotherapy. Radiother. Oncol. 2023, 185, 109734. [Google Scholar] [CrossRef]
- Remouchamps, V.M.; Vicini, F.A.; Sharpe, M.B.; Kestin, L.L.; Martinez, A.A.; Wong, J.W. Significant reductions in heart and lung doses using deep inspiration breath hold with active breathing control and intensity-modulated radiation therapy for patients treated with locoregional breast irradiation. Int. J. Radiat. Oncol. 2003, 55, 392–406. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, F.R.; Donovan, E.M.; McNair, H.A.; Corsini, L.A.; Colgan, R.M.; Evans, P.M.; Maynard, L.; Griffin, C.; Haviland, J.S.; Yarnold, J.R.; et al. The UK HeartSpare Study (Stage II): Multicentre Evaluation of a Voluntary Breath-Hold Technique in Patients Receiving Breast Radiotherapy. Clin. Oncol. 2017, 29, e51–e56. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, F.R.; Colgan, R.M.; Carr, K.; Donovan, E.M.; McNair, H.A.; Locke, I.; Evans, P.M.; Haviland, J.S.; Yarnold, J.R.; Kirby, A.M. The UK HeartSpare Study: Randomised evaluation of voluntary deep-inspiratory breath-hold in women undergoing breast radiotherapy. Radiother. Oncol. 2013, 108, 242–247. [Google Scholar] [CrossRef]
- Naidoo, W.; Leech, M. Feasibility of surface guided radiotherapy for patient positioning in breast radiotherapy versus conventional tattoo-based setups- a systematic review. Tech. Innov. Patient Support Radiat. Oncol. 2022, 22, 39–49. [Google Scholar] [CrossRef]
- Zagar, T.M.; Kaidar-Person, O.; Tang, X.; Jones, E.E.; Matney, J.; Das, S.K.; Green, R.L.; Sheikh, A.; Khandani, A.H.; McCartney, W.H.; et al. Utility of Deep Inspiration Breath Hold for Left-Sided Breast Radiation Therapy in Preventing Early Cardiac Perfusion Defects: A Prospective Study. Int. J. Radiat. Oncol. 2017, 97, 903–909. [Google Scholar] [CrossRef]
- Cashell, A.; Qadeer, J.; Rosewall, T. Exploring the Experiences of Left-Sided Breast Cancer Patients Receiving Radiation Therapy Using the Active Breathing Coordinator. J. Med. Imaging Radiat. Sci. 2016, 47, 323–328. [Google Scholar] [CrossRef]
- Beaton, N.; Watson, S.; Browne, P.; Sharma, H.; Mai, G.T.; Harvey, J.; Bernard, A.; Brown, E.; Hargrave, C.; Lehman, M. Deep inspiration breath hold in breast cancer: Development and analysis of a patient experience questionnaire. J. Med. Imaging Radiat. Oncol. 2018, 62, 854–860. [Google Scholar] [CrossRef]
- Dower, K.; Halkett, G.K.B.; Dhillon, H.; Naehrig, D.; O’Connor, M. Eliciting the views of left breast cancer patients’ receiving deep inspiration breath hold radiation therapy to inform the design of multimedia education and improve patient-centred care for prospective patients. J. Med. Radiat. Sci. 2024, 71, 384–395. [Google Scholar] [CrossRef]
- Chan, A.W.; Hoang, A.; Chen, H.; McGuffin, M.; Sheikh, A.; Vesprini, D.; Zhang, L.; Wronski, M.; Karam, I. Comparing Interfractional Stability of Heart Dose Among Three Breath-Hold Radiotherapy Techniques in Breast Cancer. Clin. Oncol. 2025, 38, 103699. [Google Scholar] [CrossRef]
- Chan, A.W.; Hoang, A.; Chen, H.; McGuffin, M.; Vesprini, D.; Zhang, L.; Wronski, M.; Karam, I. Prospective Trial on the Impact of Weekly Cone Beam Computed Tomography-Guided Correction on Mean Heart Dose in Breast Cancer Breath-Hold Radiation Therapy. Adv. Radiat. Oncol. 2024, 9, 101651. [Google Scholar] [CrossRef]
- Karam, D.I. Assessment of Left-Sided Cardiac Sparing Through the Use of 3-Dimensional Surface Matching-Based Deep Inspiration Breath Hold and Active Breathing Control. Clinicaltrials.Gov. 2022. Available online: https://clinicaltrials.gov/study/NCT03459898 (accessed on 3 December 2024).
- Osoba, D.; Aaronson, N.; Zee, B.; Sprangers, M.; Te Velde, A. Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. The Study Group on Quality of Life of the EORTC and the Symptom Control and Quality of Life Committees of the NCI of Canada Clinical Trials Group. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 1997, 6, 103–108. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Freislederer, P.; Kügele, M.; Öllers, M.; Swinnen, A.; Sauer, T.-O.; Bert, C.; Giantsoudi, D.; Corradini, S.; Batista, V. Recent Advances in Surface Guided Radiation Therapy. Radiat. Oncol. 2020, 15, 187. [Google Scholar] [CrossRef] [PubMed]
- Andersen, K.G.; Kehlet, H. Persistent Pain After Breast Cancer Treatment: A Critical Review of Risk Factors and Strategies for Prevention. J. Pain. 2011, 12, 725–746. [Google Scholar] [CrossRef]
- Mosconi, P.; Apolone, G.; Barni, S.; Secondino, S.; Sbanotto, A.; Filiberti, A. Quality of Life in Breast and Colon Cancer Long-term Survivors: An Assessment with the Eortc Qlq-c30 and Sf-36 Questionnaires. Tumori J. 2002, 88, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Nolte, S.; Liegl, G.; Petersen, M.A.; Aaronson, N.K.; Costantini, A.; Fayers, P.M.; Groenvold, M.; Holzner, B.; Johnson, C.D.; Kemmler, G.; et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur. J. Cancer. 2019, 107, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Bjelic-Radisic, V.; Cardoso, F.; Weis, J.; Pogoda, K.; Arraras, J.I.; Greimel, E.; Bottomley, A.; Cameron, D.; Brain, E.; Hartup, S.; et al. An international phase IV field study—Psychometric properties of the updated module on assessing quality of life of patients with breast cancer EORTC QLQ-BR42. Breast 2025, 80, 103890. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).