Abstract
Suicidal behavior is an important public health problem often associated with psychological and biological factors. Understanding the role of biochemical markers, such as cholesterol and serotonin levels, may provide insight into the mechanisms underlying suicidal tendencies. This study aimed to investigate the relationship between lipid profile parameters, serotonin levels, and psychological status in individuals who had attempted suicide. Patients with suicidal attempts underwent a psychiatric evaluation and blood samples were taken to measure serotonin levels, total cholesterol, and lipid metabolism parameters. Psychological assessments included measures of depression, stress, and hopelessness; assessments of motivation; suicidal tendencies; and assessments of psychological and physical aspects of fear of death. The study found a significant positive correlation between serotonin and cholesterol levels (r = 0.6883, p < 0.0001). Lower levels of serotonin and cholesterol were associated with higher rates of depression and stress. These findings suggest that dyslipidemia may be associated with reduced serotonin function, which may contribute to the development of suicidal behavior. The study highlights the potential role of cholesterol and serotonin in the development of suicidal behavior, along with the mental status of patients. Evaluating the interaction of neurobiological and social–psychological factors provide an opportunity to search for peripheral biomarkers of suicide risk.
1. Introduction
Suicide and suicidal behavior are the leading causes of mortality and morbidity in healthcare settings and are a global problem. According to the World Health Organization (WHO), approximately 800,000 deaths are recorded annually [1]. The number of people who die by suicide each year is 1.4% of the total number of deaths [2]. Some authors note that the number of suicide attempts has increased by 10–40 times in recent years compared to completed suicides [3].
According to the WHO, self-poisoning in different contexts is considered not only as a potential suicide attempt but also as an act whose purpose may be related to the resolution of difficult psychological situations or the elimination of mental discomfort [4]. In this context, “real” suicide attempts, which may pose a real threat to life, are combined with acts that may be aimed at attracting attention, or manipulative behavior, rather than suicidal intent [5].
Parasuicide (PS) can be defined as an act of self-harm that is not intended to result in death, but rather to achieve a specific social outcome. In contrast to suicide, parasuicide is frequently a manifestation of distress, a form of protest, or a means of escaping a challenging circumstance. The motivation behind parasuicidal behavior can be attributed to a desire to evade suffering, to mete out punishment upon oneself, or to abandon the prospect of life itself [6]. A history of PS is a strong indicator of suicide risk both in the general population and in specific groups. A history of PS may predict future suicide attempts, particularly if the individual experiences a reduction in fear of death and pain, which are usually protective factors. More than 40% of people who commit suicide have a history of repeated self-harm [7]. For example, within five years of a PS with serious medical consequences, one in two people has made either a fatal, or one or more non-fatal, suicide attempts [8]. PS is associated with a variety of medical, social, and sometimes subtle consequences [9].
In the study by May et al. [10], a variety of demographic, psychological, personality, and psychosocial risk factors were assessed using validated questionnaires and structured interviews. The results revealed six significant predictors of future suicide attempts: Cluster A personality disorder, Cluster B personality disorder, lifetime substance abuse, basic anxiety disorder, adverse maternal relationships, and poor social adjustment.
Stressful life events often trigger suicidal behavior, but it is not a normal stress response. It occurs in patients who have a diathesis or predisposition to either recurrent mood disorders or suicidal behavior, often both. Its study requires attention to a variety of psychosocial and psychiatric factors. Research shows that the likelihood of suicide is significantly higher among unmarried, unemployed, and unskilled individuals. These groups are more likely to live alone and to move frequently. An important risk factor is the presence of suicidal behavior and depressive disorders in the family [10]. Critical psychiatric risk factors for suicide are major depressive episodes and emotionally unstable personality disorder. Suicidal ideation and suicide attempts are significantly more common in people with depression, and depression is closely associated with suicidal ideation, which is often the first step to suicidal behavior [11]. Other risk factors include neuroticism, negative life events, and a lack of social belonging [12,13].
In addition, research also identifies protective factors that reduce the risk of suicidal ideation, such as a sense of satisfaction with interpersonal relationships, a sense of usefulness to family and friends, and a desire for a meaningful life. Beliefs in adaptability and survival, which are common in the general population, also play an important role in reducing suicidal ideation [14]. Thus, a comprehensive approach to suicide research and prevention should consider both risk and protective factors related to the psychosocial and psychiatric aspects of individuals’ lives. In addition to the above, research shows the potential role of serotonin, a neurotransmitter, and lipid profile in the development of suicidal behavior.
Serotonin, or 5-hydroxytryptamine (5-HT), is particularly important in determining an individual’s threshold for suicidal impulses because of its association with impulsive/aggressive personality traits. Serotonin is a biogenic amine that functions as a hormone and neurotransmitter in the human body. The physiological functions of serotonin are diverse [15,16]. As a neurotransmitter, serotonin transmits chemical messages to neurons in the central and peripheral nervous systems.
The etiology of suicidal behavior remains uncertain, but a stress–diathesis model has been proposed to explain its occurrence. The diathesis is thought to have a biological basis [17]. Research shows that during periods of stress, serotonin levels change significantly. Thus, the stress–diathesis theory of suicide suggests that there are both predisposing and precipitating risk factors for suicide attempts. The involvement of serotonin in the regulation of human emotional background has been studied in detail [18,19,20].
Lipids, such as cholesterol and triglycerides, are key components of cell membranes and play an important role in physiological functions, neurological processes, and mental health. Alterations in lipid metabolism may affect neuronal function. Alterations in lipid metabolism can affect the neurotransmitter system, affecting mood regulation and emotional well-being. Decreased cholesterol levels in lipid rafts result in decreased viscosity of neuronal membranes. Low viscosity leads to disruption of synaptic transmission, resulting in decreased serotonin influx through serotonin receptors (5-HT1A) [21]. Modulating serotonin balance in the brain by manipulating the lipid composition of cell membranes may open new avenues for therapeutic interventions targeting suicidal behavior. Neurobiological abnormalities found in suicidal behavior, including altered serotonin function, have been associated with features that characterize suicidal diathesis, suggesting a potential etiology for these abnormalities.
Membrane proteins regulate several different aspects of serotonin (5-HT) signaling, including the production, storage, release, activation, and inactivation of the neurotransmitter. The interaction of lipids and proteins within the cell membrane is of critical importance with regard to the transmission of 5-HT signaling. Modifications in the lipid constitution of synaptic membranes can consequently influence the flexibility and adaptability of the 5-HT synapse [22]. There is a robust correlation between dyslipidemia and the pathogenesis of psychiatric disorders, including anxiety and depression. Individuals with such mental health issues frequently exhibit dysregulated cholesterol metabolism. Abnormal cholesterol levels can have adverse effects on neurons, including cell damage, death, and impaired neuronal function [23,24]. As evidenced in the literature, low cholesterol levels may be associated with an increased risk of suicide in both men and women [25]. Other evidence indicates that individuals with high suicide attempt lethality were, in particular, men diagnosed with bipolar disorder, in comparison to those with less lethal attempts or the control group. Individuals with high suicide attempt lethality exhibited lower cholesterol levels and higher inflammatory markers (CRP) than the other groups. Although there were no significant differences in cholesterol levels between individuals who attempted suicide with low lethality and the control group, the control group demonstrated higher triglyceride levels [26].
These findings suggest the need for further research to clarify the complex interactions between psychological status, serotonin level, lipid profile parameters, and suicidal behavior.
This study aimed to investigate the relationship between serotonin levels, blood lipid profiles, and suicide attempts in patients, taking into account the influence of social and psychological factors.
2. Materials and Methods
2.1. Participants
The study included patients hospitalized after suicide attempts in the Toxicology Department of the Astana City Hospital, Republic of Kazakhstan. The comparison group was formed by random sampling and included 93 mentally healthy and psychologically stable individuals with no history of suicidal tendencies. The control group was randomly selected from students, teachers, their partners, and nurses at the hospital where the patients who attempted suicide were recruited. The mental and psychological stability of the control group participants was evaluated based on their medical history, which excluded any suicidal tendencies. The main group consisted of 102 patients who met the following inclusion criteria:
(1) age from 18 to 39 years; (2) at the time of admission did not take drugs, such as antidepressants, sedatives, neuroleptics, lipid-lowering, and other drugs affecting lipid levels; (3) except for smoking, no disorders associated with alcohol or drug use; (4) no pregnancy or lactation; (5) no diabetes mellitus, cancer, and infectious diseases, or disorders of the central nervous system; (6) the atherogenic coefficient was taken into account to exclude coronary heart disease and cardiovascular disease.
2.2. Ethics
The study was conducted following the ethical provisions of the Declaration of Helsinki and the national standard of the Republic of Kazakhstan State Standard of the Republic of Kazakhstan Good Clinical Practice ST RK 1616-2006. The study protocol was reviewed and approved by the Local Ethics Committee of the L.N. Gumilyov Eurasian National University for Conducting Research, Protocol No. 31, dated 11 August 2022. Written informed consent was obtained from all study participants.
2.3. Methodological Basis
Patients with failed suicide attempts and control subjects were interviewed using 7 psycho-diagnostic questionnaires. The general methodological basis consisted of the following seven psycho-diagnostic tests, proposed for written and oral completion in Russian and Kazakh: Beck Hopelessness Scale (1974) by A.T. Beck [27]; Reasons for Living Inventory by M.M. Linehan, J.L. Goodstein et al. [14], adapted by T.V. Zhuravleva, S.N. Enikolopova, and K.A. Chistopolskaya [28]; Fear of Personal Death Scale by V. Florian and S. Kravetz [29], adapted by K.A. Chistopolskaya and S.N. Enikolopova [30]; The Questionnaire Meaning of Suicide Attempt (RASQ) by D. Jones and R.R. Holden, modified by R.R. Holden and P.S. Kerr [31] and adapted by T.V. Zhuravleva, S.N. Enikolopov, and K.A. Chistopolskaya) [28], the Depression, Anxiety, and Stress Scale (DASS) by S. Lovibond and P. Lovibond [32]; the Method for Identifying the Tendency to Suicidal Reactions (Sr-45), by P.I. Yunatskevich (1998) [33]; and the Columbia-Suicide Severity Rating Scale (C-SSRS) [34], in Kazakh, adapted by R. Tatayeva (2022).
The Beck Hopelessness Scale [27] measures the level of hopelessness. The Cronbach’s alpha coefficient for the Beck Hopelessness Scale was found 0.91. It includes questions assessing attitudes toward the future, negative attitudes, and belief in the possibility of positive change. Higher scores may indicate severe depression. The interpretation of the questionnaire is as follows: 0–9—no depressive symptoms; 10–15—mild depression (sub-depression); 16–19—moderate depression; 20–29—major depression (moderate); 30–63—major depression.
The Reasons for Life questionnaire [14] is used to assess motivation and the reasons why a person sees meaning and purpose in life. These are based on the idea that suicidal tendencies are formed in the process of socialization and are determined by the free will, moral qualities, and inner meaning of each individual. The results demonstrate that the scales exhibit moderately high internal reliability, as indicated by Cronbach’s alpha scores that range from 0.72 to 0.89. The Reasons for Living Inventory method not only evaluates the factors that prevent the implementation of suicidal intentions but also makes it possible to predict the risk of recurrence of a suicidal act. The Questionnaire is a multidimensional inventory consisting of 48 items with six dimensions: survival and coping beliefs, responsibility to family, concerns related to children, fear of suicide, fear of social disapproval, and moral objections [35].
DASS (Depressive Anxiety and Stress Scale) [32] is used to measure an individual’s level of depression, anxiety, and stress. DASS has three subscales: Depression: questions are designed to identify symptoms of depression, such as insomnia, lack of pleasure, fatigue, and low mood. Anxiety: the physical effects of nervousness, tension, and worry. Stress: Questions are designed to identify factors that cause stress and assess its impact on psychological state. Scoring: Each of the three subscales (depression, anxiety, stress) is scored separately. Results are usually interpreted based on scores: higher scores indicate more severe symptoms. There is a special rating scale, which helps to classify the level of depression, anxiety, and stress. Overall Cronbach’s alpha coefficient for the DASS-21 scale was 0.74. Interpretation of Depression, Anxiety, and Stress Scale (DASS-21) scores [36] are as follows:
Depression scale: Low level (0 points): No depressive experiences. Intermediate level (1–8 points): Symptoms of depression range from mild (sub-depression) to moderate depression. Apathy, anhedonia, and decreased interest in life are possible. High level (over 8 points): Severe depression characterized by feelings of hopelessness, the meaninglessness of life, the tendency toward self-destruction and suicidal thoughts, irritability, sleep, and appetite disturbances.
Anxiety scale: Low level (0 points): No anxious experiences. Intermediate level (1–7 points): Anxiety symptoms ranging from mild to clinically expressed anxiety. High level (over 7 points): High level of anxiety, characterized by intense arousal, overexertion, and anticipation of negative events.
Stress scale: Low level (less than 2 points): No stress symptoms. Intermediate level (2–10 points): Mild to intense stress. High level (over 10 points): Severe stress accompanied by nervousness, irritability, increased tension, and inability to relax.
The method Tendency to suicidal reactions (Sr-45, P.I. Yunatskevich) [33] is designed to determine the tendency towards suicidal reactions. The use of questions as motivational material during the examination makes it possible to identify people with a tendency to have suicidal reactions and to create a risk group. When interpreting the results of the method, it should be taken into account that it assesses only the initial level of a person’s suicidal tendency during the examination period. The results of the Suicidality Scale (S) are interpreted according to the following levels: a low level; a below-average level; an average level; an above-average level; and finally, a high level of suicidal tendency. The Cronbach alpha coefficient for the Cr-45 questionnaire is 0.98.
The Reasons for Attempting Suicide questionnaire [31] is designed to explore the reasons that lead to suicidal actions. In this way, it is possible to differentiate between people who attempt suicide in a demonstrative and blackmailing way and people who have a sincere intention to commit suicide. Descriptive statistics of the suicide questionnaire have a possible range of values: internal confusion from 6 to 30 points; manipulative motivation from 5 to 25 points. The attributable motives assessed by the questionnaire appear to be reliable, valid indicators of suicidal behavior, and may improve the prediction of suicide criteria (e.g., past suicide attempts, current suicidal ideation, self-rated likelihood of future suicide) beyond that of previously identified psychological constructs.
The Columbia-Suicide Severity Rating Scale (C-SSRS) is a tool for assessing and classifying suicidal behavior and ideation, i.e., suicide risk [34]. The reliability of the questionnaire is 0.814, as indicated by Cronbach’s alpha. The main components of the C-SSRS include the following: Wanting to die: assesses the presence and strength of the desire to die, the presence of suicidal plans, and assesses accuracy; Actions (suicidal behavior): to determine the presence and severity of suicidal actions; Support (lethality in case of suicide attempt): assesses the severity of the suicide attempt; Safety (rescue factors): identifies factors that help prevent suicidal behavior.
The C-SSRS has four modules:
- Suicidal ideation;
- Intensity of suicidal ideation;
- Suicidal Behavior Module, consisting of six items;
- The module of the actual and potential risk of suicidal actions, consists of two items: “actual risk”, i.e., harm to health, and “potential risk”.
The Fear of Personal Death Scale [29] was developed in 1983. The Russian version was published in 2012 in an adaptation by K.A. Chistopolskaya and her co-authors [30]. The scale is designed to measure the degree of fear of death at the individual level. Questionnaires can address the emotional and cognitive aspects associated with fear of death. The Fear of Personal Death Scale is designed to assess the psychological and physical aspects of fear of death, as well as the mental rejection of the topic of death and the analysis of possible reasons for its internal rejection. The initial pool of items was formulated concerning previous empirical and theoretical research. Moreover, students from the Department of Social Sciences at SO were requested to provide a list of the reasons for their fear of death. As a consequence of these procedures, the SO items were devised and submitted to a panel of three psychologists with a proven track record of reliability. The objective was to ascertain whether each item satisfied the criteria set out in the theoretical model underpinning this study.
Each of these questionnaires is a tool for a deeper understanding of the psychological aspects related to emotional state, anxiety, motivation, and attitude toward death in the subjects under study. However, it is important to remember the need for ethical use of survey data and correct interpretation of the results.
2.4. Blood Sample Testing
Triglycerides (TC), total cholesterol (TG), low-density lipoprotein cholesterol (LDL), and high-density lipoprotein cholesterol (HDL) were measured in all patients. TC, TG, HDL, and LDL levels were measured using a Roche reagent kit designed for quantitative determination by spectrophotometric analysis in serum and plasma. Plasma serotonin concentration was measured by high-performance liquid chromatography (HPLC) at the Olymp Clinical Diagnostic Laboratory in Astana. All patients and control subjects fasted overnight. Blood samples were taken from the antecubital vein between 7 and 10 a.m. For suicidal patients, blood was taken within 3 days of the suicide attempt. Five milliliters of blood were collected in Vacutainer tubes for cholesterol and platelet 5-HT determination. Serum was separated by centrifugation at 3000× g for 5 min at room temperature and stored at −80 °C until analysis.
2.5. Statistical Analysis
GraphPad Prism version 10.2.1 was used for statistical analysis of data and assessment of suicide attempt lethality risk. The arithmetic mean and standard error (SE) were calculated for each scale of the questionnaires and lipid profile parameters. To identify differences in psychological factors in suicidal behavior between the groups of individuals who committed suicidal acts, they were individually grouped by the number of primary and repeated suicidal acts committed. Since there was no significant difference in the distribution of lipid content between the group of individuals with single suicide attempts and the group of individuals with multiple suicide attempts, these two subgroups were combined into one suicide attempt group. The participants were 18–39 years old for the study of lipid profile parameters, serum serotonin levels, and psychological status. Pearson’s correlation coefficient was calculated to determine the linear relationship between lipid profile and psychological status in suicide attempters. The reliability of the differences between the mean values of the scales and the lipid profile was determined by the Student’s t-test, and the differences were considered significant at p < 0.05, p < 0.01, p < 0.001, p < 0.0001.
3. Results
3.1. Demographic and Clinical Background of Participants
A total of 102 patients participated in the study, 87 of whom had committed a single suicidal act, and the remaining 15 multiple suicide attempts (2 attempts), as well as 93 controls. In our study, we focused on the 18–39 age group for the following reasons: individuals aged 18–39 often face unique stressors, such as the onset of adulthood, the transition from school to work, starting a family, and financial independence. These stressors may increase the risk of suicidal behavior in this age group. It is also important to note that metabolic processes and levels of biomarkers, such as lipid profile and serotonin, can vary significantly across age groups. Establishing relationships between these biomarkers and suicide attempts in young people may provide more accurate and specific results that can be used to develop preventive and therapeutic interventions. Sociodemographic data, mental status, lipid metabolism parameters, and blood serotonin levels of the subjects were analyzed. In the groups studied, significantly more females (70%) attempted suicide than males (30%) (Table 1).

Table 1.
Sociodemographic variables of the participants.
Among the patients who attempted suicide, 1.2% had secondary education, 62.5% had specialized secondary education, 5% had incomplete higher education, and 31.3% had higher education. At the same time, 43.9% were married, 5.1% were divorced, and 46.3% had never been married. According to the oral questionnaire, 33.5% of the subjects in this group were employed, 35.6% were unemployed, and 30.9% were students.
The study collected data on the motivations that led the participants to commit suicide (Figure 1). At the same time, 38% of the participants refused to disclose the reasons for their suicide attempts. This high percentage may indicate difficulties with self-expression, embarrassment, fear of judgment, or an inability to accurately identify their motives.
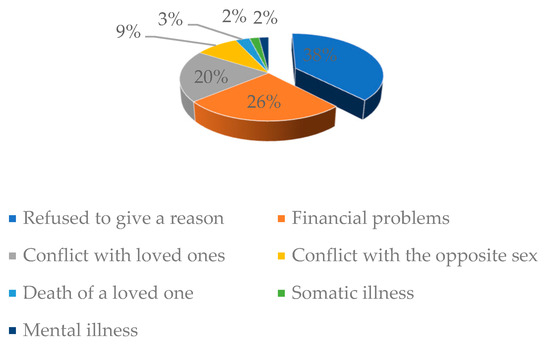
Figure 1.
Reasons given by patients who have attempted suicide.
The second most common reason given by respondents is financial problems, cited by 26% of suicides. Financial difficulties, such as debt, job loss, or significant financial problems, are an important factor that can cause severe stress and lead to suicidal intent. Conflicts with loved ones (parents, brothers, sisters) were present in 20% of cases. A proportion of 9% of respondents cited conflicts with the opposite sex as a reason for suicidal actions. These conflicts included romantic relationships with husbands or wives, breakups, infidelity, or other aspects of personal relationships. A proportion of 3% of respondents cited the death of a loved one. Only 2% of respondents cited health problems as a reason. This includes somatic illnesses that can significantly affect the quality of life and satisfaction. Another 2% cited specific mental illnesses, such as chronic illness, depression, bipolar disorder, and others, which can contribute to the development of suicidal thoughts and actions.
These results highlight the complexity and multifaceted nature of the factors influencing suicidal behavior and the need for an integrated approach to its prediction and prevention.
3.2. Results of Psycho-Diagnostic Tests
In accordance with the methodology proposed by P.I. Yunatskevich [33], the tendency to suicidal reactions (Sr-45) was identified in patients with a mean score of 0.39 ± 0.12 points (Table 2). This indicates the presence of potential tendencies to suicidal reactions, which are not characterized by high stability of mental state. This indicator exhibited a significantly lower value in the control group (0.28 ± 0.03; p < 0.0001).

Table 2.
Results of psycho-diagnostic tests (in points).
The results of measurements on the Beck Hopelessness Scale indicate that the average score in the control group was 2.12 ± 0.22 points, while those who had attempted suicide exhibited a markedly elevated level of hopelessness, with an average score of 4.35 ± 0.51 points (p < 0.0001). The results of the Reasons for Life questionnaire indicated that the Beliefs in Survival and Coping scale for patients with a suicide attempt was 112.6 ± 3.9 points, while in the control group, this indicator was significantly higher at 122.2 ± 9.6 points (p < 0.0145). The indicators of the Fear of Social Disapproval scale in individuals who had attempted suicide exhibited a mean score of 11.76 ± 3.05 points. The results of the DASS questionnaire indicated that patients who had attempted suicide exhibited elevated levels of depression, stress, and anxiety, whereas these indicators were markedly diminished in the control group. The results of the questionnaire, entitled Reasons for Attempting Suicide, indicated that the manipulative motivation indicator for patients with a suicide attempt was 15 ± 0.94 points. In contrast, this indicator was significantly lower in the control group, with a mean of 12.64 ± 2.35 points (p < 0.0141). The results of the Internal confusion scale in individuals with a suicide attempt were 18.6 ± 4.2 points, while in the control group, this indicator was significantly lower at 14.36 ± 1.2 points (p < 0.0006). The aforementioned indicators suggest that individuals who have attempted suicide exhibit particular emotional and motivational characteristics. The mean Columbia-Suicide Severity Rating Scale score for patients with a suicide attempt was 1.19 ± 0.23 points while, in the control group, this score was significantly lower at 0.58 ± 0.61 points (p < 0.0104). This finding underscores the importance of assessing and monitoring suicide risk in patients. In light of the aforementioned factors, it may prove beneficial to consider their potential utility in the development of preventive and therapeutic measures. The Fear of Personal Death Questionnaire and its subscales revealed no statistically significant differences between the main and control groups.
3.3. Results of Lipid Profile Parameters
In consideration of the potential impact of altered lipid metabolism on the neurotransmitter system, including its influence on mood regulation and emotional well-being, we conducted a study to examine the lipid profile of individuals with suicide attempts and a control group aged 18–39 years (Table 3).

Table 3.
Lipid profile levels in individuals with failed suicide attempts and the control group.
The mean total cholesterol level for the cohort of individuals with suicide attempts in the 18–39 age group was 3.37 ± 0.88 mmol/L, which was significantly lower than the mean level observed in the control group (4.62 ± 1.51 mmol/L). The observed difference was highly reliable (p < 0.01). The analysis did not reveal a statistically significant difference in lipid parameters between men and women.
Additionally, the concentration of LDL in the bloodstream is diminished in comparison to the suicide group, as evidenced by statistical analysis (p < 0.05). Consequently, the LDL level in patients was 1.92 ± 0.51 mmol/L, while the control group exhibited a mean LDL level of 2.66 ± 0.88 mmol/L.
No significant differences were observed in other biochemical parameters, including high-density lipoprotein, triglycerides, and very low-density lipoprotein, between the two groups.
3.4. Results of Serotonin Level and Its Correlation with Lipid Profile Parameters
As previously stated, serotonin, a bioamine neurotransmitter, plays a pivotal role in the development of suicidal behavior. The mean serotonin level in the group of individuals who had attempted suicide and were aged between 18 and 39 years was 84.9 ± 54.9 ng/mL. In the control group comprising individuals of the same age range, the serotonin level was higher, with a mean of 147.84 ± 43 ng/mL. Even though the results fall within the reference range of serotonin levels (50–220 ng/mL), the data indicate a notable decline in serotonin levels among individuals with suicide attempts in comparison to the control group (p < 0.05).
An analysis of the correlation between serotonin levels and lipid profile parameters in individuals who have committed suicide attempts and a control group is crucial for identifying biological markers associated with suicidal behavior.
Should a correlation be established between lipid metabolism disorders and suicidal tendencies, it may facilitate the development of novel methods of prevention and treatment, such as dietary modifications or the utilization of pharmacological agents to normalize lipid profile parameters. Furthermore, an understanding of the biological mechanisms underlying suicide attempts facilitates the development of more targeted therapeutic approaches. The integration of biological data with psychological aspects enhances diagnosis and treatment, rendering them more personalized and effective.
We analyzed the correlation between serotonin levels and various lipid profile parameters in individuals who attempted suicide and in the control group (Table 4).

Table 4.
Results of correlation analysis between lipid profile and serotonin levels in individuals with failed suicide attempts and the control group in the age group 18–39 years.
Cholesterol plays a pivotal role in the formation of lipid rafts, which are lipid-rich microregions present in neuronal membranes. It is established that cholesterol-rich lipid rafts and adapter proteins regulate the function and signaling of serotonin receptors [37]. The results demonstrated a statistically significant positive correlation between serotonin levels and total cholesterol levels (r = 0.6883, p < 0.0001). A negative correlation was observed between serum serotonin levels and cholesterol levels. Lipid rafts play a pivotal role in modulating the function of receptors, including those involved in serotonin signaling (e.g., 5-HT1A and 5-HT2A) and transport proteins, such as the serotonin transporter (SERT). A cholesterol deficiency may impair the integrity and functionality of these rafts, which may in turn reduce the efficiency of serotonin signaling. Concurrently, a weak negative correlation was identified between serotonin content and both HDL and VLDL levels. The correlation between serotonin content and LDL level, as well as triglyceride level, was found to be weakly positive.
Therefore, a clear relationship was identified between the serotonin level and cholesterol content in individuals who had attempted suicide, although this relationship was less dependent on other lipids.
In this study, we focused on determining cholesterol levels in individuals between the ages of 18 and 39. The data obtained will serve as a basis for further comparative analysis and identification of possible differences in lipid profiles between different age groups, taking into account the known increase in cholesterol levels in older age groups.
3.5. Results of Correlation Between the Levels of Serotonin, Lipid Profile Parameters, and the Indicators of Various Psycho-Diagnostic Tests
The correlation between the levels of serotonin, lipid profile parameters, and the indicators of various psycho-diagnostic tests in patients who attempted suicide was analyzed during the study (Table 5). The results demonstrated a significant correlation between serotonin levels and certain psychological state indicators, indicating a complex relationship between biological and psychological factors associated with suicidal behavior.

Table 5.
Correlation between serotonin levels, lipid parameters, and psycho-diagnostic test scores in patients who attempted suicide.
The results of the analysis indicated a moderate negative correlation between the scores on the Survival copying beliefs scale and serotonin levels (r = −0.468, p < 0.01). This finding suggests that lower serotonin levels are associated with weaker survival beliefs. Depression scores demonstrated a robust negative correlation (r = −0.895, p < 0.0001), indicating a substantial association between low serotonin levels and elevated depression scores. Similarly, lower serotonin levels were found to be associated with higher stress levels (p < 0.01), which underscores the role of serotonin in regulating the hypothalamic–pituitary–adrenal (HPA) axis [38]. Additionally, lower serotonin levels were linked to heightened concerns about the loss of self-fulfillment (p < 0.05) and a stronger tendency towards fear of loss of social identity (p < 0.001). A positive correlation was observed between low serotonin levels and an increased fear of consequences for the body (p < 0.01).
Subsequently, the correlation between lipid metabolism parameters and the indicators of various psycho-diagnostic questionnaires was analyzed. A significant positive correlation was identified between cholesterol levels and moral objections to suicide (r = 0.405, p < 0.05). Furthermore, a robust negative correlation was identified between cholesterol levels and depression indicators (r = −0.852, p <0.0001). A negative correlation was identified between cholesterol levels and stress scale parameters (r = −0.344, p < 0.05). The analysis also revealed a significant negative correlation between cholesterol levels and Columbia-Suicide Severity Rating Scale scores (r = −0.479, p < 0.001), indicating that low cholesterol levels are associated with higher scores on the C-SSRS, which measures the severity of suicidal thoughts and behaviors. Finally, a negative correlation was identified between cholesterol levels and fear of transcendental consequences (r = −0.290, p < 0.05), indicating that low cholesterol levels are associated with elevated fear of transcendental consequences.
Significant results were found for triglyceride levels and survival copying beliefs (r = −0.279, p < 0.05), indicating that higher triglyceride levels are associated with lower levels of survival beliefs. Similarly, a negative correlation was identified between triglyceride levels and fear of social disapproval (r = −0.279, p < 0.05).
Correlations between high-density lipoprotein (HDL) levels and psycho-diagnostic questionnaires yielded intriguing associations. A positive correlation was identified between HDL levels and measures of fear of consequences for family and friends (r = 0.2840, p < 0.05), indicating that higher HDL levels are associated with increased concern about the impact of one’s actions on loved ones. Furthermore, a more robust positive correlation was observed between HDL levels and fear of transcendental consequences (r = 0.3902, p < 0.01), suggesting that individuals with elevated HDL levels tend to apprehend the spiritual or existential implications of mortality.
Therefore, the observed variability in the significant correlations between serotonin levels, lipid profile parameters, and psycho-diagnostic test results can be attributed to the complex and multifaceted role of lipids and serotonin in brain function and psychological processes. However, it is important to consider that psycho-diagnostic tests are limited by the patient’s willingness to share information and the potential for a high number of false-positive results.
4. Discussion
The present study examined the relationships between lipid profile parameters, blood serotonin levels, and psychological status parameters among patients who had attempted suicide and a control group.
When studying the mental state of patients with parasuicidal behavior, the tendency to suicidal reactions of the patients showed significantly higher values compared to the control group, which indicates low stability of the mental state in the main group (Table 1), requiring further targeted work with a psychotherapist as a potential risk group.
The concept of hopelessness, as measured by the Beck Hopelessness Inventory, includes negative cognitive schemas about oneself, current life situations, and prospects [27]. The results of this study show that hopelessness, as measured by the Beck Hopelessness Inventory, is a highly sensitive marker of suicide risk. Statistically significant differences between the mean scores in the experimental and control groups (p < 0.0001) (Table 1) indicate that elevated levels of hopelessness are a reliable predictor of suicidal behavior. The data obtained emphasize the importance of assessing the level of hopelessness in clinical practice for the timely identification of patients in need of intensive psychotherapeutic care and suicide prevention measures. The results of other studies indicate the existence of gender differences in the relationship between initial hopelessness and suicidal ideation [39]. In women, there was a more stable relationship between depression and hopelessness throughout the treatment period, regardless of the dynamics of depressive symptoms. This suggests that hopelessness may play a more important role in the pathogenesis of suicidal behavior in women, which may be a prospect for future studies of our detailed gender differences in this context.
The results of the current study showed that people with suicidal thoughts and ideation have significantly lower confidence in their ability to cope with life’s challenges and to survive compared to those without such thoughts. The data suggest that attention should be paid to increasing self-confidence and the ability to cope with life’s challenges in order to prevent suicide attempts. The extant literature indicates that individuals with suicidal tendencies may exhibit a proclivity for specific personality traits, including impulsivity, low self-esteem, a tendency to self-blame [40], an inability to regulate emotions, and difficulties in coping with stress [41]. These findings are consistent with the results of our study. Additionally, individuals with a history of suicide attempts exhibit elevated levels of neuroticism [42]. Fear of being judged by others plays an important role in the emotional state of patients with suicide attempts and is one of the factors that can, to some extent, deter suicide attempts. Support in the form of reducing stigma and negative public opinion can be an important aspect of working with patients and prevention.
The DASS-21 is a reliable and valid cross-cultural measure of depression, anxiety, and stress [43]. The results of this study, using the DASS questionnaire, indicate that depression, stress, and anxiety are common and prominent symptoms in individuals who have attempted suicide. Statistically significant differences between groups emphasize the importance of careful assessment of the emotional state of patients at risk for suicide (Table 1). The identified differences indicate the need to develop and implement comprehensive psychotherapeutic programs aimed at reducing the level of negative emotions and preventing repeated suicide attempts.
The results of the questionnaire Reasons for Suicide Attempts show that some patients may use suicide attempts as a means of influencing others and developing manipulative strategies around suicidal behavior.
It is also common for patients with suicidal ideation to hold negative and unrealistic ideas about themselves, the world, and the future. It has been demonstrated that interpersonal conflicts, whether familial, social, or professional, can act as a significant stressor, contributing to the development of suicidal ideation and behaviors [44]. This finding aligns with the identified causes of suicide attempts in our study. The fear of being judged for suicidal thoughts or attempts can act as a deterrent to individuals seeking help. Our study revealed deterrent factors, such as family and fear of death. As evidenced in the literature, the factors that initially precipitated suicidal ideation may persist after a suicide attempt, thereby increasing the risk of repeated attempts [45]. Results from a systematic review [46] indicate that a significant number of people with suicidal tendencies do not seek professional help due to barriers, such as high autonomy, lack of perceived need for treatment, and stigmatizing attitudes toward suicide and mental health problems.
In the course of this study, no significant differences were found in the Fear of Personal Death Questionnaire and its subscales between the main group (patients with suicide attempts) and the control group (psychologically stable participants). This lack of differences may be due to several factors. First, the fear of personal death itself, as an existential phenomenon, may be present in people regardless of their mental state or suicidal behavior. As shown in previous studies [47], fear of death is a general human characteristic and may not depend on the presence of suicidal tendencies. However, another study showed that people with suicidal ideation exhibit a paradoxical phenomenon: on the one hand, they show a reduced emotional response to their mortality, which is manifested by a decrease in anxiety or fear of death during self-reflection. On the other hand, their response to death in an abstract context (e.g., when thinking about death in general or the death of other people) does not differ from that of people without suicidal thoughts [48]. Psychologically stable individuals and patients with suicide attempts may experience similar levels of fear of personal death and its subscales (e.g., fear of consequences for the body or for loved ones).
Second, the sample of participants (age group 18–39 years) may also play a role in the results obtained. In this age group, the fear of death associated with personal identity and oblivion may be less pronounced than in older age groups, for whom such issues become more relevant [49].
Finally, the influence of cultural factors may be a possible explanation. In a society where social and family ties play an important role, people may experience similar levels of fear of forgetting and social condemnation, as reflected in the lack of significant differences in these indicators between groups.
A potential correlation has been identified between cholesterol levels and suicidal behavior [50]. Lipid metabolism disorders may contribute to the development of mental disorders, including depression and anxiety, which are often precursors to suicidal ideation [51]. In this study, suicide attempters aged 18–39 years had statistically significantly lower total cholesterol levels than controls (Table 3). Cholesterol and LDL levels were also significantly lower in suicide attempters than in controls, p < 0.001. Agugliya et al. also found that the high-mortality suicide attempt group had significantly lower total cholesterol levels [26]. Our findings on LDL are also consistent with those of Gonzalez-Castro et al., who found a decrease in low-density lipoprotein (LDL) levels in people with a history of suicide [52]. One possible mechanism is that changes in brain cholesterol levels alter central nervous system function, and a decrease in cholesterol and LDL levels at the neuronal level leads to changes in neurotransmitters and synaptic degeneration. As shown by De Berardis et al., low cholesterol levels are associated with a strong fear of transcendental consequences [53]. The results of this study, as well as similar studies, support the hypothesis that a decrease in serum cholesterol and LDL concentrations is associated with suicidal behavior. In the literature, low serum levels of total cholesterol, LDL, and C-reactive protein have been associated with repeated suicide attempts. The authors of this paper suggest that dyslipidemia contributes to changes in the membranes of serotonergic neurons, which may contribute to the emergence of suicidal ideation. Cholesterol depletion reduces the transport capacity of serotonin by reducing the number of turns of the serotonin transporter [54].
Other biochemical parameters, such as high-density lipoprotein (HDL), triglycerides, and very low-density lipoprotein (VLDL) levels, did not show significant differences between groups in the current study. Loas et al. (2016) and Shaker et al. (2020) found that high suicidal ideation was associated with low HDL levels [55,56]. Su et al. (2019) came to different conclusions; in their study patients with suicidal ideation had higher HDL levels compared to the control group [57].
Triglycerides are the main source of energy for cells, and their levels can affect brain metabolism [58]. Although the patients’ blood triglyceride levels were within normal limits, these indicators were correlated with low survival belief scores in psycho-diagnostic tests. This influence may manifest as a decrease in survival beliefs and an increase in fear of social disapproval. In addition, changes in metabolism and lipid levels can lead to inflammatory processes and hormonal imbalances.
We found that individuals with elevated high-density lipoprotein (HDL) levels were more likely to experience death anxiety, particularly in a spiritual or existential sense (Table 5). Several mechanisms could explain these findings. First, high HDL levels are known to be associated with improved cardiovascular health, which may reflect a general concern for health and well-being [59]. In this context, increased concern about the consequences of one’s actions on others may be associated with an increased focus on maintaining one’s health and preventing negative consequences, which also affects emotional and mental well-being. Thus, high HDL levels may be a marker of a more generally caring and mindful approach to life [60]. Individuals with higher HDL levels may show increased attention to the possible spiritual and existential consequences of their actions, which may manifest as increased anxiety about transcendental consequences.
The correlation between HDL and these psycho-diagnostic tests shows that, in people predisposed to suicidal behavior, higher HDL levels are moderately associated with greater fears about the impact on family and friends and about transcendental consequences.
The results showed that lower cholesterol levels are associated with greater moral objections to suicide, higher levels of depression and stress, higher levels of suicidal ideation and behavior, and greater fear of transcendental consequences. These findings suggest a complex interaction between biological and psychological factors in suicidal behavior and suggest that cholesterol levels may be an important biomarker and may play an important role in the prevention of suicide attempts.
The influence of serotonin and its association with total cholesterol in suicidal behavior demonstrated a statistically significant positive correlation between serotonin levels and total cholesterol levels (r = 0.6883, p < 0.0001), indicating that lower serotonin levels are associated with lower blood cholesterol levels (Table 4). A reduction in cholesterol and LDL levels within the CNS results in a decline in cell membrane viscosity, which subsequently leads to a reduction in the number of 5-HT1A (serotonin) receptors. This, in turn, gives rise to impulsivity and violent suicidal behavior as a consequence of low cholesterol and LDL levels [61,62]. As early as 1992, Engelberg [63] put forth a hypothesis that posits a link between cholesterol and the serotonergic system. He proposed that a reduction in serum cholesterol levels may be associated with alterations in the viscosity and functionality of serotonin receptors and transporters, as well as a decline in the concentration of serotonin precursors, which may contribute to an increase in suicidal ideation. Modifications in lipid micro-viscosity within neural membranes may result in diminished exposure of serotonin receptors on the membrane surface, which may subsequently lead to hypofunction of these receptors [64]. The results of our study indicated a positive correlation between cholesterol levels and moral objections to suicide.
The serotonergic system, which has been linked to suicidal thoughts, impulsivity, and aggressive behavior, has been associated with lower cerebrospinal fluid 5-hydroxyindoleacetic acid (5-HIAA) concentrations in individuals who have attempted suicide [65,66]. Prior research has also identified a positive correlation between serum total cholesterol levels and cerebrospinal fluid 5-HIAA levels in individuals who have attempted suicide [67]. This relationship may be bidirectional, whereby alterations in cholesterol levels may impact the serotonergic system, and vice versa [68]. Individuals who exhibit traits, such as aggression, impulsivity, pessimism, hopelessness, cognitive impairment, and poor affect regulation are more likely to engage in suicidal behaviors. These traits have been identified as risk factors for suicidal ideation and attempts [38,69,70].
In the present study, we sought to ascertain the correlation between serotonin levels and the parameters of various psycho-diagnostic questionnaires (Table 5). The data enable the correlation of biomarkers with psychological characteristics associated with suicidal behavior. The influence of serotonin levels on psychological constructs may be direct, as evidenced by their impact on depression and stress, or indirect, as observed in the context of moral objections and the responsibility to the family. In our study, constructs with a more pronounced biochemical basis, such as depression and stress, demonstrated stronger correlations with serotonin levels. Concurrently, the fears associated with suicide, social disapproval, and self-destruction may be influenced by a multitude of neurotransmitters and psychological processes, thereby attenuating the specific effect of serotonin.
The results of our study demonstrated a robust negative correlation between depression and low serotonin levels in the blood (r = −0.8954, p < 0.0001). This suggests a notable correlation between reduced serotonin levels and elevated depressive symptoms. Some studies have focused on disturbances in serotonin neural signaling, which can lead to endogenous depression [71,72]. In the existing literature, there is an association between lower serotonin levels and weaker survival beliefs [73].
These correlations indicate that lower serotonin levels are associated with higher levels of depression, stress, and various fears related to self-identity and existential issues (Table 5). The data substantiate the hypothesis that the neurotransmitter serotonin plays a pivotal role in the psychological profile of patients with suicidal tendencies. While other neurotransmitters, such as norepinephrine and dopamine, are also utilized, drugs that act on serotonin are typically regarded as the primary avenue of pharmacological intervention, complemented by other modalities, such as lifestyle modifications, exercise, and psychotherapy [74,75]. As posited by Kim and colleagues, reduced cholesterol levels may serve as a potential biological marker for depression [76].
In this study, we examined the interaction between psychological states (depression, stress, emotional, and motivational factors) and biochemical parameters (serotonin levels and lipid profile parameters). The findings indicate that diminished serotonin levels are linked to poorer psychological well-being in patients, including elevated rates of depression and stress, as well as heightened anxiety about social condemnation and internal distress. This finding corroborates the hypothesis that serotonin plays a role in the development of suicidal behavior.
Furthermore, our study revealed a correlation between decreased total cholesterol and low-density lipoprotein levels and decreased serotonin levels. This interaction may have a deleterious effect on the function of neuronal membranes and serotonin receptors, thereby increasing the risk of suicidal behavior. It is becoming increasingly evident that alterations in lipid parameters may have a profound impact on neurobiological processes that regulate mental health. This underscores the crucial importance of monitoring lipid profiles to assess the risk of suicidal behavior.
In conclusion, our study illuminates the intricate interplay between psychological states, the serotonergic system, and lipid metabolism, demonstrating how biochemical and psychological factors collectively influence suicidal behavior. In the future, we intend to expand these studies and consider additional variables to gain a more comprehensive understanding of the mechanisms underlying these relationships.
While our study offers valuable insights into the relationship between suicidal behavior and a range of psychological and biological factors, including serotonin levels and lipid profile, it is important to consider the limitations of the findings when generalizing to broader populations.
Firstly, the sample of participants was limited to the age category of 18–39 years, which may limit the applicability of the results to other age groups where factors influencing suicidal behavior may differ. Future research should explore these factors across a wider age range to understand how these factors may influence suicidal behavior in different age groups.
Secondly, the study was conducted in the Republic of Kazakhstan, which may limit its generalizability to other cultural and ethnic groups, since social, cultural, and economic factors may play an important role in suicidal behavior.
In addition, the selection of patients taking into account strict criteria (exclusion of individuals with alcohol and drug addiction, and patients with somatic diseases that can affect lipid and serotonin metabolism) may also limit the generalizability of the results to more heterogeneous populations. For example, in clinical practice, there may be patients with suicide attempts and comorbid conditions, which requires additional research to identify possible variations in biomarkers and psychological characteristics. Future research should explore the relationship between lipid parameters, serotonin levels, and psycho-diagnostic tests in individuals with comorbid conditions, such as alcohol and drug addiction, to understand how these factors may influence the association between variables. By investigating a broader range of populations, we can gain a more comprehensive understanding of the factors involved in suicidal behavior. Factors such as stress associated with professional activity or individual psychological characteristics of the participants could remain as uncontrolled variables. We also acknowledge that correlation analysis methods, such as Pearson correlation, may not always accurately reflect complex causal relationships between variables and, in future studies, we plan to use more advanced statistical methods, such as regression analysis or path analysis to account for the influence of multiple factors. We acknowledge the importance of confirmatory factor analysis for assessing the psychometric validity of the measures we used. In future studies, we plan to conduct CFA to further validate the scales and ensure their reliability and construct validity. It is also possible that differences in sociodemographic characteristics between groups (such as education and occupation) may have influenced psychological status and the assessment of suicidal risk.
Therefore, although the study yielded valuable findings, its focus on a specific subgroup of patients and controls may limit its applicability to broader populations. It is recommended that these results be considered as part of a larger picture and that further research be conducted in different age, cultural, and clinical contexts to confirm and extend the findings presented here.
5. Conclusions
This specific type of research was conducted for the first time in the Republic of Kazakhstan, which represents a significant component of the study.
Those who have attempted suicide often display a constellation of psychological factors, including persistent suicidal ideation, hopelessness, low self-esteem, difficulty coping, social anxiety, elevated levels of depression, stress, and anxiety. Additionally, they may exhibit manipulative motivations and internal turmoil.
In the study, we examined the interaction between psychological states (depression, stress, emotional and motivational factors) and biochemical indicators (serotonin levels and lipid profile parameters). The results demonstrate that a reduction in serotonin levels is associated with a decline in the psychological state of patients, including elevated levels of depression and stress, as well as fear of social condemnation and internal turmoil. This lends further support to the hypothesis that serotonin plays a role in the formation of suicidal behavior.
Furthermore, our study revealed a correlation between decreased total cholesterol and low-density lipoprotein (LDL) levels and decreased serotonin levels. This interaction may have a deleterious effect on the function of neuronal membranes and serotonin receptors, thereby increasing the risk of suicidal behavior. The monitoring of lipid profiles is of particular importance in the assessment of suicidal risk, as alterations in lipid metabolism parameters have the potential to influence neurobiological processes that regulate mental health.
The study corroborated the existence of a correlation between low serotonin levels and elevated rates of depression, stress, and specific emotional and motivational factors, including inner turmoil and fear of social condemnation. These findings suggest that serotonin plays a pivotal role in the etiology of suicidal behavior and depression, thereby supporting the hypothesis that lipid metabolism is a key regulator of the serotonergic system. Furthermore, lower levels of total cholesterol and LDL were found to be associated with an increased risk of suicide attempts, which is consistent with the findings of previous studies. This underscores the necessity of monitoring lipid profiles as a potential biomarker for evaluating suicide risk and depression.
These findings underscore the necessity for further investigation into the correlation between serotonin, lipid metabolism, and suicidal behavior. This may contribute to the development of more effective diagnostic and treatment methods aimed at improving mental health and preventing suicide attempts. Such models could serve as the foundation for more efficacious prevention and intervention strategies. The study underscores the necessity for the development of targeted prevention programs that address both the biological and psychological aspects of suicidal behavior. It is recommended that these programs prioritize the enhancement of mental health and the strengthening of familial relationships. It would be beneficial for future studies to include participants of varying ages in order to identify age-related differences in biological and psychological markers of suicidal behavior. This is particularly crucial given that the risks and underlying causes of suicidal behavior may differ across different life stages.
Author Contributions
Conceptualization, R.T.; methodology, A.T. and S.S.; software, B.A.; validation, A.S., R.T. and A.T.; formal analysis, A.T.; investigation, B.A.; editing, A.S. and S.K.; data curation, A.T.; writing—original draft preparation, A.T. and S.S.; writing—review and editing, R.T. and A.S.; visualization, S.S., B.A. and S.K.; supervision, R.T.; funding acquisition, R.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research work was carried out with the support of the targeted funding program—BR18574196—Study of genetic mechanisms in the formation of suicidal behavior to develop strategies for predicting and preventing suicide, Ministry of Science and Higher Education of the Republic of Kazakhstan.
Institutional Review Board Statement
The study was conducted in accordance with the ethical provisions of the Declaration of Helsinki and the National Standard of the Republic of Kazakhstan State Standard of the Republic of Kazakhstan Good Clinical Practice GOST ST RK 1616-2006. The research protocol was examined and approved by the local ethical commission of the L.N. Gumilyov Eurasian National University for conducting research work, protocol No. 31, dated 11 August 2022. All subjects were informed about the study and all provided informed consent.
Informed Consent Statement
Written informed consent has been obtained from the patients before publishing this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Acknowledgments
We would like to thank all study participants.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Suicide Worldwide in 2019. Available online: https://www.who.int/publications/i/item/9789240026643 (accessed on 18 July 2024).
- Bilsen, J. Suicide and Youth: Risk Factors. Front. Psychiatry 2018, 9, 540. [Google Scholar] [CrossRef]
- Khademi, N.; Zangeneh, A.; Ziapour, A.; Saeidi, S.; Teimouri, R.; Yenneti, K.; Moghadam, S.; Almasi, A.; Golanbari, S.Z. Exploring the Epidemiology of Suicide Attempts: Risk Modeling in Kermanshah-Iran. Front. Public Health 2022, 10, 924907. [Google Scholar] [CrossRef]
- Preventing Suicide: A Global Imperative. Available online: https://www.who.int/publications/i/item/9789241564779 (accessed on 18 July 2024).
- Apter, A. Clinical Aspects of Suicidal Behavior Relevant to Genetics. Eur. Psychiatry 2010, 25, 257–259. [Google Scholar] [CrossRef]
- Kreitman, N.; Philip, A.; Greer, S.; Bagley, C. ‘Parasuicide. ’ Br. J. Psychiatry 1970, 116, 460–461. [Google Scholar] [CrossRef]
- Lyubov, E.B.; Zotov, P.B. Diagnosis of Suicidal Behavior and Assessment of the Degree of Suicidal Risk. Message I. Suicidology 2018, 9, 23–35. [Google Scholar]
- Beautrais, A.L. Further Suicidal Behavior among Medically Serious Suicide Attempters. Suicide Life Threat. Behav. 2004, 34, 27772. [Google Scholar] [CrossRef]
- Lyubov, E.B.; Parshin, A.N. Clinical and Economic Studies of Suicidal Behavior. Suicidology 2016, 7, 11–28. [Google Scholar]
- Cheng, A.; Chen, T.; Chen, C.-C.; Jenkins, R. Psychosocial and Psychiatric Risk Factors for Suicide: Case-Control Psychological Autopsy Study. Br. J. Psychiatry 2000, 177, 360–365. [Google Scholar] [CrossRef]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.; Selby, E.A.; Joiner, T.E. The Interpersonal Theory of Suicide. Psychol. Rev. 2010, 117, 575–600. [Google Scholar] [CrossRef]
- Hartley, E.L.; Stritzke, W.G.K.; Page, A.C.; Blades, C.A.; Parentich, K.T. Neuroticism Confers Vulnerability in Response to Experimentally Induced Feelings of Thwarted Belongingness and Perceived Burdensomeness: Implications for Suicide Risk. J. Personal. 2019, 87, 566–578. [Google Scholar] [CrossRef]
- Fisher, L.B.; Overholser, J.C.; Ridley, J.; Braden, A.; Rosoff, C. From the Outside Looking In: Sense of Belonging, Depression, and Suicide Risk. Psychiatry 2015, 78, 29–41. [Google Scholar] [CrossRef]
- Linehan, M.M.; Goodstein, J.L.; Nielsen, S.L.; Chiles, J.A. Reasons for Staying Alive When You Are Thinking of Killing Yourself: The Reasons for Living Inventory. J. Consult. Clin. Psychol. 1983, 51, 276–286. [Google Scholar] [CrossRef]
- Shajib, M.S.; Khan, W.I. The Role of Serotonin and Its Receptors in Activation of Immune Responses and Inflammation. Acta Physiol. 2015, 213, 561–574. [Google Scholar] [CrossRef]
- Kanova, M.; Kohout, P. Serotonin—Its Synthesis and Roles in the Healthy and the Critically Ill. IJMS 2021, 22, 4837. [Google Scholar] [CrossRef]
- van Heeringen, K.; Mann, J.J. The Neurobiology of Suicide. Lancet Psychiatry 2014, 1, 63–72. [Google Scholar] [CrossRef]
- Müller, C.P.; Jacobs, B.L. Handbook of the Behavioral Neurobiology of Serotonin; Elsevier: Amsterdam, The Netherlands, 2009; ISBN 978-0-12-374634-4. [Google Scholar]
- Sargin, D.; Jeoung, H.-S.; Goodfellow, N.M.; Lambe, E.K. Serotonin Regulation of the Prefrontal Cortex: Cognitive Relevance and the Impact of Developmental Perturbation. ACS Chem. Neurosci. 2019, 10, 3078–3093. [Google Scholar] [CrossRef]
- Puig Pérez, S. Serotonin and Emotional Decision-Making. In Serotonin; IntechOpen: Rijeka, Croatia, 2019. [Google Scholar] [CrossRef]
- De Berardis, D.; Marini, S.; Piersanti, M.; Cavuto, M.; Perna, G.; Valchera, A.; Mazza, M.; Fornaro, M.; Iasevoli, F.; Martinotti, G.; et al. The Relationships between Cholesterol and Suicide: An Update. ISRN Psychiatry 2012, 2012, 387901. [Google Scholar] [CrossRef]
- Kalinichenko, L.S.; Kornhuber, J.; Sinning, S.; Haase, J.; Müller, C.P. Serotonin Signaling through Lipid Membranes. ACS Chem. Neurosci. 2024, 15, 1298–1320. [Google Scholar] [CrossRef]
- Cheon, S.Y. Impaired Cholesterol Metabolism, Neurons, and Neuropsychiatric Disorders. Exp. Neurobiol. 2023, 32, 57–67. [Google Scholar] [CrossRef]
- Cartocci, V.; Catallo, M.; Tempestilli, M.; Segatto, M.; Pfrieger, F.; Bronzuoli, M.; Scuderi, C.; Servadio, M.; Trezza, V.; Pallottini, V. Altered Brain Cholesterol/Isoprenoid Metabolism in a Rat Model of Autism Spectrum Disorders. Neuroscience 2018, 372, 53. [Google Scholar] [CrossRef]
- Sublette, M.E. Lipids and Suicide Risk. In Current topics in Behavioral Neurosciences; Springer: Berlin/Heidelberg, Germany, 2020; Volume 46, ISBN 978-3-030-57573-1. [Google Scholar]
- Aguglia, A.; Solano, P.; Giacomini, G.; Caprino, M.; Conigliaro, C.; Romano, M.; Aguglia, E.; Serafini, G.; Amore, M. The Association Between Dyslipidemia and Lethality of Suicide Attempts: A Case-Control Study. Front. Psychiatry 2019, 10, 70. [Google Scholar] [CrossRef]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The Measurement of Pessimism: The Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef]
- Chistopolskaya, K.A.; Zhuravleva, T.V.; Enikolopov, S.N.; Nikolyaev, E.L. Adaptation of Methods for Studying Suicidal Aspects of Personality. Psychol. J. High. Sch. Econ. 2017, 14, 61–87. [Google Scholar]
- Florian, V.; Kravetz, S. Fear of Personal Death: Attribution, Structure, and Relation to Religious Belief. J. Personal. Soc. Psychol. 1983, 44, 600–607. [Google Scholar] [CrossRef]
- Chistopolskaya, K.A.; Enikolopov, S.N.; Nikolyaev, E.L.; Semikin, G.I.; Khramelashvili, V.V.; Nikolayevna, K.V.; Kazantseva, V.N. Adaptation of the Questionnaires “Attitude towards Death” and “Fear of Personal Death” on a Russian-Speaking Sample. Suicidology 2014, 5, 60–69. [Google Scholar]
- Holden, R.; DeLisle, M. Factor Structure of the Reasons for Attempting Suicide Questionnaire (RASQ) with Suicide Attempters. J. Psychopathol. Behav. Assess. 2006, 28, 1–8. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Yunatskevich, P.I. Fundamentals of Psychological and Pedagogical Diagnostics and Correction of Suicidal Behavior. VIKA im. A.F. Mozhaisky: St. Petersburg, Russia, 1998; pp. 165–172. [Google Scholar]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S.; et al. The Columbia–Suicide Severity Rating Scale: Initial Validity and Internal Consistency Findings from Three Multisite Studies With Adolescents and Adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef]
- Pirani, S.; Kulhanek, C.; Wainwright, K.; Osman, A. The Reasons for Living Inventory for Young Adults (RFL-YA-II). Assessment 2021, 28, 942–954. [Google Scholar] [CrossRef]
- Basha, E.; Kaya, M. Depression, Anxiety and Stress Scale (DASS): The Study of Validity and Reliability. Univers. J. Educ. Res. 2016, 4, 2701–2705. [Google Scholar] [CrossRef]
- Björk, K.; Sjögren, B.; Svenningsson, P. Regulation of Serotonin Receptor Function in the Nervous System by Lipid Rafts and Adaptor Proteins. Exp. Cell Res. 2010, 316, 1351–1356. [Google Scholar] [CrossRef]
- Mann, J.J. Neurobiology of Suicidal Behaviour. Nat. Rev. Neurosci. 2003, 4, 819–828. [Google Scholar] [CrossRef]
- Wolfe, K.L.; Nakonezny, P.A.; Owen, V.J.; Rial, K.V.; Moorehead, A.P.; Kennard, B.D.; Emslie, G.J. Hopelessness as a Predictor of Suicide Ideation in Depressed Male and Female Adolescent Youth. Suicide Life-Threat. Behav. 2019, 49, 253–263. [Google Scholar] [CrossRef]
- Beautrais, A.L.; Joyce, P.R.; Mulder, R.T. Personality Traits and Cognitive Styles as Risk Factors for Serious Suicide Attempts among Young People. Suicide Life Threat. Behav. 1999, 29, 37–47. [Google Scholar] [CrossRef]
- Nordström, P.; Schalling, D.; Asberg, M. Temperamental Vulnerability in Attempted Suicide. Acta Psychiatr. Scand. 1995, 92, 155–160. [Google Scholar] [CrossRef]
- Özdemir, P.G.; Kefeli, M.C.; Özcan, H. Emotion Regulation Difficulties, Personality Traits and Coping Styles in First-Time Suicide Attempters. J. Psychol. Psychother.Res. 2017, 4, 27–34. [Google Scholar] [CrossRef]
- Zolotareva, A.A. Systematic Review of the Psychometric Properties of the Depression Anxiety and Stress Scale-21 (DASS-21). V.M. Bekhterev Rev. Psychiatry Med. Psychol. 2020, 2, 26–37. [Google Scholar] [CrossRef]
- Hur, J.-W.; Choi, K.-Y.; Lee, B.-H.; Shim, S.-H.; Yang, J.-C.; Kim, Y.-K. The Psychosocial Factors Affecting Suicide Attempt. J. Korean Neuropsychiatr. Assoc. 2007, 46, 129–135. [Google Scholar]
- Bhatt, M.; Perera, S.; Zielinski, L.; Eisen, R.B.; Yeung, S.; El-Sheikh, W.; DeJesus, J.; Rangarajan, S.; Sholer, H.; Iordan, E.; et al. Profile of Suicide Attempts and Risk Factors among Psychiatric Patients: A Case-Control Study. PLoS ONE 2018, 13, e0192998. [Google Scholar] [CrossRef]
- Han, J.; Batterham, P.J.; Calear, A.L.; Randall, R. Factors Influencing Professional Help-Seeking for Suicidality: A Systematic Review. Crisis 2018, 39, 175–196. [Google Scholar] [CrossRef]
- Iverach, L.; Menzies, R.G.; Menzies, R.E. Death Anxiety and Its Role in Psychopathology: Reviewing the Status of a Transdiagnostic Construct. Clin. Psychol. Rev. 2014, 34, 580–593. [Google Scholar] [CrossRef]
- Hussey, I.; Barnes-Holmes, D.; Booth, R. Individuals with Current Suicidal Ideation Demonstrate Implicit “Fearlessness of Death”. J. Behav. Ther. Exp. Psychiatry 2016, 51, 3. [Google Scholar] [CrossRef]
- Thorson, J.A.; Powell, F.C. Death Anxiety in Younger and Older Adults; Brunner-Routledge: New York, NY, USA, 2018; pp. 123–136. [Google Scholar] [CrossRef]
- Makhanova, A.M.; Ponamareva, O.A.; Tatayeva, R.K. The Relationship between Blood Cholesterol and Suicidal Behaviour. Bull. L.N. Gumilyov Eurasian Natl. Univ. Biosci. Ser. 2023, 144, 95–114. [Google Scholar] [CrossRef]
- Russell, D.W.; Halford, R.W.; Ramirez, D.M.O.; Shah, R.; Kotti, T. Cholesterol 24-Hydroxylase: An Enzyme of Cholesterol Turnover in the Brain. Annu. Rev. Biochem. 2009, 78, 1017–1040. [Google Scholar] [CrossRef]
- González-Castro, T.B.; Genis-Mendoza, A.D.; León-Escalante, D.I.; Hernández-Díaz, Y.; Juárez-Rojop, I.E.; Tovilla-Zárate, C.A.; López-Narváez, M.L.; Marín-Medina, A.; Nicolini, H.; Castillo-Avila, R.G.; et al. Possible Association of Cholesterol as a Biomarker in Suicide Behavior. Biomedicines 2021, 9, 1559. [Google Scholar] [CrossRef]
- De Berardis, D.; Conti, C.M.V.; Serroni, N.; Moschetta, F.S.; Carano, A.; Salerno, R.M.; Cavuto, M.; Farina, B.; Alessandrini, M.; Janiri, L.; et al. The Role of Cholesterol Levels in Mood Disorders and Suicide. J. Biol. Regul. Homeost. Agents 2009, 23, 133–140. [Google Scholar]
- Magnani, F.; Tate, C.G.; Wynne, S.; Williams, C.; Haase, J. Partitioning of the Serotonin Transporter into Lipid Microdomains Modulates Transport of Serotonin. J. Biol. Chem. 2004, 279, 38770–38778. [Google Scholar] [CrossRef]
- Loas, G.; Dalleau, E.; Lecointe, H.; Yon, V. Relationships between Anhedonia, Alexithymia, Impulsivity, Suicidal Ideation, Recent Suicide Attempt, C-Reactive Protein and Serum Lipid Levels among 122 Inpatients with Mood or Anxious Disorders. Psychiatry Res. 2016, 246, 296–302. [Google Scholar] [CrossRef]
- Shaker, N.M.; Sultan, M.; Mohamed, M.Y.; Helal, S.A.; Abd El Moneam, M.H.E.-D. Lipid Profile and Impulsivity in Suicidal Patients with Major Depressive Disorder. Arch. Suicide Res. 2021, 25, 641–656. [Google Scholar] [CrossRef]
- Su, M.; Li, E.; Tang, C.; Zhao, Y.; Liu, R.; Gao, K. Comparison of Blood Lipid Profile/Thyroid Function Markers between Unipolar and Bipolar Depressed Patients and in Depressed Patients with Anhedonia or Suicidal Thoughts. Mol. Med. 2019, 25, 51. [Google Scholar] [CrossRef]
- Dimache, A.M.; Șalaru, D.L.; Sascău, R.; Stătescu, C. The Role of High Triglycerides Level in Predicting Cognitive Impairment: A Review of Current Evidence. Nutrients 2021, 13, 2118. [Google Scholar] [CrossRef]
- Soo, J.; Kubzansky, L.D.; Chen, Y.; Zevon, E.S.; Boehm, J.K. Psychological Well-Being and Restorative Biological Processes: HDL-C in Older English Adults. Soc. Sci. Med. 2018, 209, 59–66. [Google Scholar] [CrossRef]
- Radler, B.T.; Rigotti, A.; Ryff, C.D. Persistently High Psychological Well-Being Predicts Better HDL Cholesterol and Triglyceride Levels: Findings from the Midlife in the U.S. (MIDUS) Longitudinal Study. Lipids Health Dis. 2018, 17, 1. [Google Scholar] [CrossRef]
- Da Graça Cantarelli, M.; Tramontina, A.C.; Leite, M.C.; Gonçalves, C.-A. Potential Neurochemical Links between Cholesterol and Suicidal Behavior. Psychiatry Res. 2014, 220, 745–751. [Google Scholar] [CrossRef]
- Tomson-Johanson, K.; Harro, J. Low Cholesterol, Impulsivity and Violence Revisited. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 103–107. [Google Scholar] [CrossRef]
- Engelberg, H. Low Serum Cholesterol and Suicide. Lancet 1992, 339, 727–729. [Google Scholar] [CrossRef]
- Kalipatnapu, S.; Chattopadhyay, A. Membrane Organization and Function of the Serotonin(1A) Receptor. Cell Mol. Neurobiol. 2007, 27, 1097–1116. [Google Scholar] [CrossRef]
- Jokinen, J.; Nordström, A.-L.; Nordström, P. Cholesterol, CSF 5-HIAA, Violence and Intent in Suicidal Men. Psychiatry Res. 2010, 178, 217–219. [Google Scholar] [CrossRef]
- Troister, T.; Holden, R.R. Comparing Psychache, Depression, and Hopelessness in Their Associations with Suicidality: A Test of Shneidman’s Theory of Suicide. Personal. Individ. Differ. 2010, 49, 689–693. [Google Scholar] [CrossRef]
- Hibbeln, J.R.; Umhau, J.C.; George, D.T.; Shoaf, S.E.; Linnoila, M.; Salem, N. Plasma Total Cholesterol Concentrations Do Not Predict Cerebrospinal Fluid Neurotransmitter Metabolites: Implications for the Biophysical Role of Highly Unsaturated Fatty Acids. Am. J. Clin. Nutr. 2000, 71, 331S–338S. [Google Scholar] [CrossRef]
- Fischer, P.; Gruenblatt, E.; Pietschmann, P.; Tragl, K.-H. Serotonin Transporter Polymorphism and LDL-Cholesterol. Mol. Psychiatry 2006, 11, 707–709. [Google Scholar] [CrossRef]
- Calati, R.; Nemeroff, C.B.; Lopez-Castroman, J.; Cohen, L.J.; Galynker, I. Candidate Biomarkers of Suicide Crisis Syndrome: What to Test Next? A Concept Paper. Int. J. Neuropsychopharmacol. 2019, 23, 192–205. [Google Scholar] [CrossRef]
- Jimenez-Trevino, L.; Gonzalez-Blanco, L.; Alvarez-Vazquez, C.; Rodriguez-Revuelta, J.; Saiz Martinez, P.A. Glutamine and New Pharmacological Targets to Treat Suicidal Ideation. Curr. Top. Behav. Neurosci. 2020, 46, 179–196. [Google Scholar] [CrossRef]
- Albert, P.R.; Benkelfat, C.; Descarries, L. The Neurobiology of Depression—Revisiting the Serotonin Hypothesis. I. Cellular and Molecular Mechanisms. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2012, 367, 2378–2381. [Google Scholar] [CrossRef]
- Sakai, K. Sleep-Waking Discharge Profiles of Dorsal Raphe Nucleus Neurons in Mice. Neuroscience 2011, 197, 200–224. [Google Scholar] [CrossRef]
- Manfredini, R.; Caracciolo, S.; Salmi, R.; Boari, B.; Tomelli, A.; Gallerani, M. The Association of Low Serum Cholesterol with Depression and Suicidal Behaviours: New Hypotheses for the Missing Link. J. Int. Med. Res. 2000, 28, 247–257. [Google Scholar] [CrossRef]
- Micheli, L.; Ceccarelli, M.; D’Andrea, G.; Tirone, F. Depression and Adult Neurogenesis: Positive Effects of the Antidepressant Fluoxetine and of Physical Exercise. Brain Res. Bull. 2018, 143, 181–193. [Google Scholar] [CrossRef]
- Strawn, J.R.; Geracioti, L.; Rajdev, N.; Clemenza, K.; Levine, A. Pharmacotherapy for Generalized Anxiety Disorder in Adult and Pediatric Patients: An Evidence-Based Treatment Review. Expert. Opin. Pharmacother. 2018, 19, 1057–1070. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Myint, A.-M. Clinical Application of Low Serum Cholesterol as an Indicator for Suicide Risk in Major Depression. J. Affect. Disord. 2004, 81, 161–166. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).