Rapid Ovarian Reserve Decline in a Woman with Pericentric Inv(9) Variant
Abstract
1. Introduction
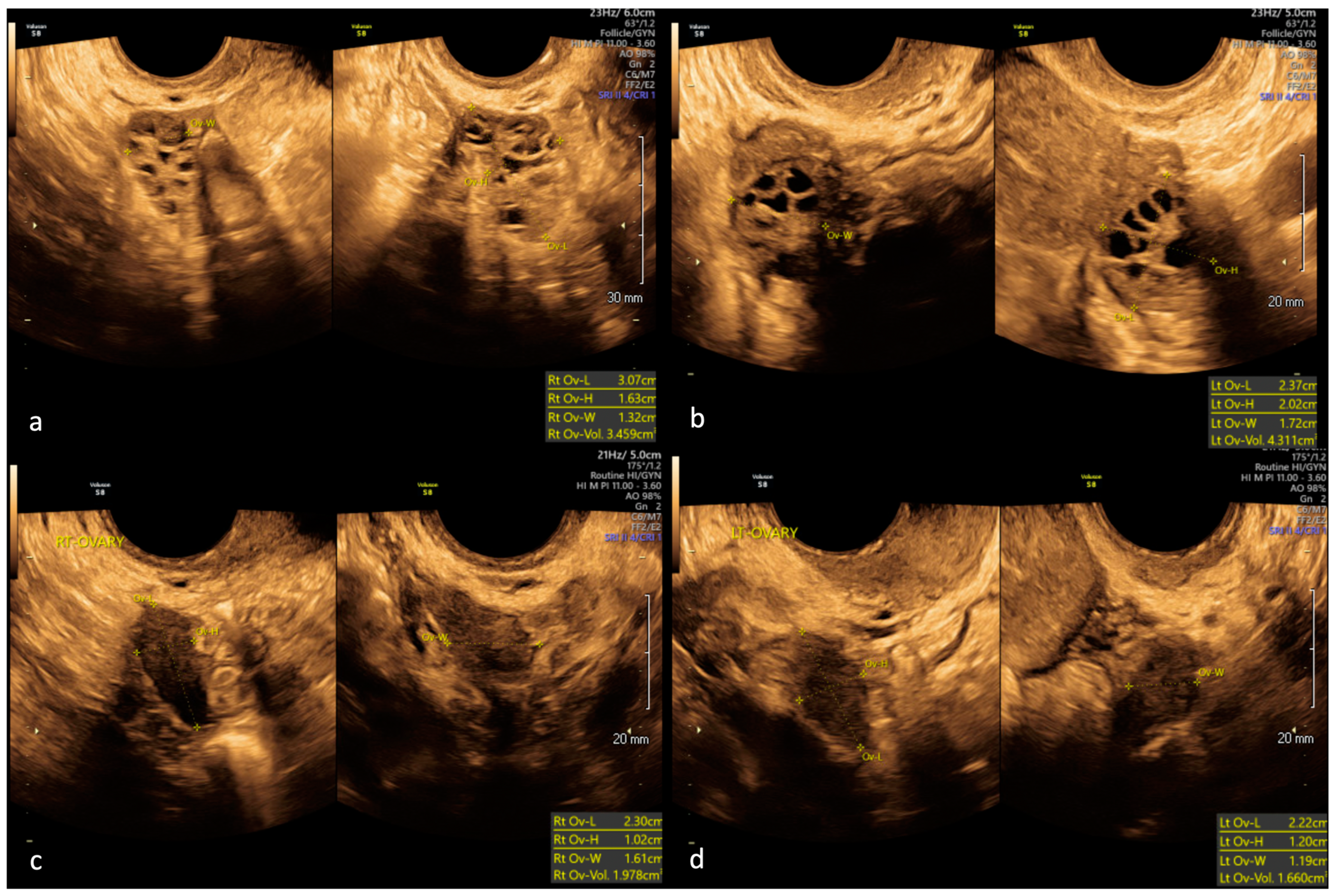
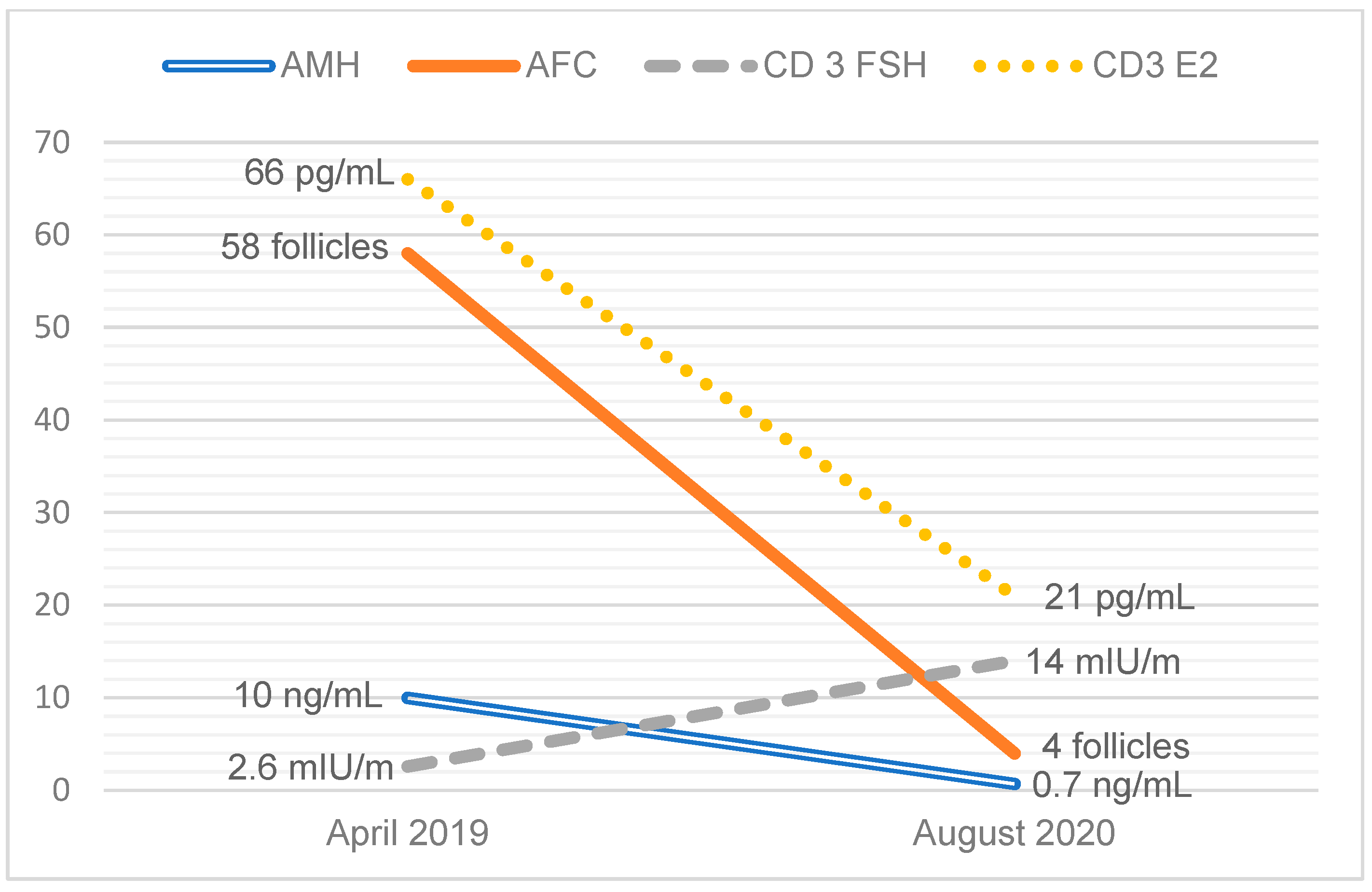
2. Case Report
3. Literature Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carson, S.A.; Kallen, A.N. Diagnosis and Management of Infertility: A Review. JAMA 2021, 326, 65–76. [Google Scholar] [CrossRef]
- Practice Committee of the American Society for Reproductive Medicine. Testing and Interpreting Measures of Ovarian Reserve: A Committee Opinion. Fertil. Steril. 2020, 114, 1151–1157. [Google Scholar] [CrossRef]
- Younis, J.S.; Ben-Ami, M.; Ben-Shlomo, I. The Bologna Criteria for Poor Ovarian Response: A Contemporary Critical Appraisal. J. Ovarian Res. 2015, 8, 76. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Primary Ovarian Insufficiency in Adolescents and Young Women: Committee Opinion No. 605. Obs. Gynecol 2014, 124, 193–197. [Google Scholar] [CrossRef]
- Moiseeva, A.V.; Kudryavtseva, V.A.; Nikolenko, V.N.; Gevorgyan, M.M.; Unanyan, A.L.; Bakhmet, A.A.; Sinelnikov, M.Y. Genetic Determination of the Ovarian Reserve: A Literature Review. J. Ovarian Res. 2021, 14, 102. [Google Scholar] [CrossRef] [PubMed]
- The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 Consensus on Diagnostic Criteria and Long-Term Health Risks Related to Polycystic Ovary Syndrome. Fertil. Steril. 2004, 81, 19–25. [Google Scholar] [CrossRef]
- Cheng, R.; Ma, Y.; Nie, Y.; Qiao, X.; Yang, Z.; Zeng, R.; Xu, L. Chromosomal Polymorphisms Are Associated with Female Infertility and Adverse Reproductive Outcomes after Infertility Treatment: A 7-Year Retrospective Study. Reprod. Biomed. Online 2017, 35, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Dana, M.; Stoian, V. Association of Pericentric Inversion of Chromosome 9 and Infertility in Romanian Population. Maedica 2012, 7, 25–29. [Google Scholar] [PubMed]
- Kumar, M.; Chapadgaonkar, S. Homozygosity and Heterozygosity of Pericentric Inversion of Chromosome 9 and Its Clinical Impact. J. Clin. Diagn. Res. 2012, 6, 816–820. [Google Scholar]
- Minocherhomji, S.; Athalye, A.S.; Madon, P.F.; Kulkarni, D.; Uttamchandani, S.A.; Parikh, F.R. A Case-Control Study Identifying Chromosomal Polymorphic Variations as Forms of Epigenetic Alterations Associated with the Infertility Phenotype. Fertil. Steril. 2009, 92, 88–95. [Google Scholar] [CrossRef]
- Sahin, F.I.; Yilmaz, Z.; Yuregir, O.O.; Bulakbasi, T.; Ozer, O.; Zeyneloglu, H.B. Chromosome Heteromorphisms: An Impact on Infertility. J. Assist. Reprod. Genet. 2008, 25, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Li, F.; Tan, W.; Tang, J. Analysis of the Clinical Features of Pericentric Inversion of Chromosome 9. J. Int. Med. Res. 2020, 48, 0300060520957820. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K. Population Studies of Inv(9) Chromosomes in 4300 Japanese: Incidence, Sex Difference and Clinical Significance. Jpn. J. Hum. Genet. 1992, 37, 293–301. [Google Scholar] [CrossRef]
- Azim, M.; Khan, A.H.; Khilji, Z.L.; Pal, J.A.; Khurshid, M. Chromosomal Abnormalities as a Cause of Recurrent Abortions: A Hospital Experience. J. Pak. Med. Assoc. 2003, 53, 117–119. [Google Scholar]
- Cozaru, G.C.; Butnariu, L.I.; Gorduza, E.V. Genetic Counselling in Reproductive Disorders. Procedia-Soc. Behav. Sci. 2012, 33, 213–217. [Google Scholar] [CrossRef]
- Dubey, S.; Chowdhury, M.R.; Prahlad, B.; Kumar, V.; Mathur, R.; Hamilton, S.; Kabra, M.; Menon, P.S.N.; Verma, I.C. Cytogenetic Causes for Recurrent Spontaneous Abortions—An Experience of 742 Couples (1484 Cases). Indian J. Hum. Genet. 2005, 11, 94–98. [Google Scholar] [CrossRef]
- Dutta, U.R.; Rajitha, P.; Pidugu, V.K.; Dalal, A.B. Cytogenetic Abnormalities in 1162 Couples with Recurrent Miscarriages in Southern Region of India: Report and Review. J. Assist. Reprod. Genet. 2011, 28, 145. [Google Scholar] [CrossRef] [PubMed]
- Elkarhat, Z.; Kindil, Z.; Zarouf, L.; Razoki, L.; Aboulfaraj, J.; Elbakay, C.; Nassereddine, S.; Nasser, B.; Barakat, A.; Rouba, H. Chromosomal Abnormalities in Couples with Recurrent Spontaneous Miscarriage: A 21-Year Retrospective Study, a Report of a Novel Insertion, and a Literature Review. J. Assist. Reprod. Genet. 2019, 36, 499–507. [Google Scholar] [CrossRef]
- Flynn, H.; Yan, J.; Saravelos, S.H.; Li, T.C. Comparison of Reproductive Outcome, Including the Pattern of Loss, between Couples with Chromosomal Abnormalities and Those with Unexplained Repeated Miscarriages. J. Obstet. Gynaecol. Res. 2014, 40, 109–116. [Google Scholar] [CrossRef]
- Ghazaey, S.; Keify, F.; Mirzaei, F.; Maleki, M.; Tootian, S.; Ahadian, M.; Abbaszadegan, M.R. Chromosomal Analysis of Couples with Repeated Abortions in Northeastern Iran. Int. J. Fertil. Steril. 2015, 9, 47. [Google Scholar] [CrossRef]
- Makino, T.; Tabuchi, T.; Nakada, K.; Iwasaki, K.; Tamura, S.; Iizuka, R. Chromosomal Analysis in Japanese Couples with Repeated Spontaneous Abortions. Int. J. Fertil. 1990, 35, 266–270. [Google Scholar] [PubMed]
- Mozdarani, H.; Mohseni Meybodi, A.; Karimi, H. Impact of Pericentric Inversion of Chromosome 9 [Inv (9) (P11q12)] on Infertility. Indian J. Hum. Genet. 2007, 13, 26–29. [Google Scholar] [CrossRef][Green Version]
- Nonaka, T.; Takahashi, M.; Nonaka, C.; Enomoto, T.; Takakuwa, K. The Analysis of Chromosomal Abnormalities in Patients with Recurrent Pregnancy Loss, Focusing on the Prognosis of Patients with Inversion of Chromosome (9). Reprod. Med. Biol. 2019, 18, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Rawal, L.; Kumar, S.; Mishra, S.R.; Lal, V.; Bhattacharya, S.K. Clinical Manifestations of Chromosomal Anomalies and Polymorphic Variations in Patients Suffering from Reproductive Failure. J. Hum. Reprod. Sci. 2020, 13, 209–215. [Google Scholar] [CrossRef]
- Yuce, H. A Rare Seen Case with Homozygosity for Pericentric Inversion of Chromosome 9 and Primary Infertility. Am. J. Case Rep. 2008, 9, 385–388. [Google Scholar]
- Šípek, A.J.; Panczak, A.; Mihalová, R.; Hrčková, L.; Suttrová, E.; Sobotka, V.; Lonský, P.; Kaspříková, N.; Gregor, V. Pericentric Inversion of Human Chromosome 9 Epidemiology Study in Czech Males and Females. Folia Biol 2015, 61, 140–146. [Google Scholar]
- Demirhan, O.; Pazarbasi, A.; Suleymanova-Karahan, D.; Tanriverdi, N.; Kilinç, Y. Correlation of Clinical Phenotype with a Pericentric Inversion of Chromosome 9 and Genetic Counseling: A Report of 157 Carriers. Saudi Med. J. 2008, 29, 946–951. [Google Scholar]
- Yuksel, S.; Savaci, S.; Ekici, C.; Kurtoglu, E.L.; Korkmaz, S.; Yesilada, E. Prevalence of Pericentric Inversion of Chromosome 9 in Eastern Anatolia Region and Relationship to Reproductive Efficiency. EJMO 2018, 2, 40–42. [Google Scholar]
- Teo, S.H.; Tan, M.; Knight, L.; Yeo, S.H.; Ng, I. Pericentric Inversion 9—Incidence and Clinical Significance. Ann. Acad. Med. Singap. 1995, 24, 302–304. [Google Scholar]
- Kosyakova, N.; Grigorian, A.; Liehr, T.; Manvelyan, M.; Simonyan, I.; Mkrtchyan, H.; Aroutiounian, R.; Polityko, A.D.; Kulpanovich, A.I.; Egorova, T.; et al. Heteromorphic Variants of Chromosome 9. Mol. Cytogenet. 2013, 6, 14. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chiang, C.; Jacobsen, J.C.; Ernst, C.; Hanscom, C.; Heilbut, A.; Blumenthal, I.; Mills, R.E.; Kirby, A.; Lindgren, A.M.; Rudiger, S.R.; et al. Complex Reorganization and Predominant Non-Homologous Repair Following Chromosomal Breakage in Karyotypically Balanced Germline Rearrangements and Transgenic Integration. Nat. Genet. 2012, 44, 390–397. [Google Scholar] [CrossRef]
- Stephens, P.J.; Greenman, C.D.; Fu, B.; Yang, F.; Bignell, G.R.; Mudie, L.J.; Pleasance, E.D.; Lau, K.W.; Beare, D.; Stebbings, L.A.; et al. Massive Genomic Rearrangement Acquired in a Single Catastrophic Event during Cancer Development. Cell 2011, 144, 27–40. [Google Scholar] [CrossRef]
- Kloosterman, W.P.; Hoogstraat, M.; Paling, O.; Tavakoli-Yaraki, M.; Renkens, I.; Vermaat, J.S.; van Roosmalen, M.J.; van Lieshout, S.; Nijman, I.J.; Roessingh, W.; et al. Chromothripsis Is a Common Mechanism Driving Genomic Rearrangements in Primary and Metastatic Colorectal Cancer. Genome Biol. 2011, 12, R103. [Google Scholar] [CrossRef] [PubMed]
- Shorokhova, M.; Nikolsky, N.; Grinchuk, T. Chromothripsis-Explosion in Genetic Science. Cells 2021, 10, 1102. [Google Scholar] [CrossRef] [PubMed]
- de Pagter, M.S.; van Roosmalen, M.J.; Baas, A.F.; Renkens, I.; Duran, K.J.; van Binsbergen, E.; Tavakoli-Yaraki, M.; Hochstenbach, R.; van der Veken, L.T.; Cuppen, E.; et al. Chromothripsis in Healthy Individuals Affects Multiple Protein-Coding Genes and Can Result in Severe Congenital Abnormalities in Offspring. Am. J. Hum. Genet. 2015, 96, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Starke, H.; Seidel, J.; Henn, W.; Reichardt, S.; Volleth, M.; Stumm, M.; Behrend, C.; Sandig, K.R.; Kelbova, C.; Senger, G.; et al. Homologous Sequences at Human Chromosome 9 Bands P12 and Q13-21.1 Are Involved in Different Patterns of Pericentric Rearrangements. Eur. J. Hum. Genet. 2002, 10, 790–800. [Google Scholar] [CrossRef]
- Dong, Z.; Yan, J.; Xu, F.; Yuan, J.; Jiang, H.; Wang, H.; Chen, H.; Zhang, L.; Ye, L.; Xu, J.; et al. Genome Sequencing Explores Complexity of Chromosomal Abnormalities in Recurrent Miscarriage. Am. J. Hum. Genet. 2019, 105, 1102–1111. [Google Scholar] [CrossRef]
- Merrion, K.; Maisenbacher, M. Pericentric Inversion (Inv) 9 Variant—Reproductive Risk Factor or Benign Finding? J. Assist. Reprod. Genet. 2019, 36, 2557–2561. [Google Scholar] [CrossRef]
- McAllister, J.M.; Legro, R.S.; Modi, B.P.; Strauss, J.F. Functional Genomics of PCOS: From GWAS to Molecular Mechanisms. Trends Endocrinol. Metab. 2015, 26, 118. [Google Scholar] [CrossRef]
| Author, Year | Country | Population | Control Group | Outcome | Results |
|---|---|---|---|---|---|
| Studies comparing the prevalence of Inv(9) in individuals with infertility or RPL to controls | |||||
| Cheng et al., 2017 [7] | China | Women ages 20–44 years with infertility. (N = 16,285 including N = 2175 with unexplained infertility) Women with chromosome aneuploidy were excluded. | Women in the same age group seeking preconception genetic testing for RPL or stillbirth, advanced maternal age, or history of a child with a prior genetic condition or birth defect. (N = 3665). | Prevalence of Inv(9) | Infertile cases: N = 195 (1.2%) Subset of women with unexplained infertility: N = 45 (2.1%) Fertile controls: N = 29 (0.79%) p < 0.05 for comparisons to controls |
| Dana et al., 2012 [8] | Romania | Men and women with infertility (N = 1800). | Amniocentesis from fetuses considered to be a sample of fertile population (spontaneous pregnancy) (N = 1116) | Prevalence of Inv(9) (p11q12), (p11q13) | Infertile cases: N = 41 (2.28%) Fertile controls: N = 44 (3.94%) N.S. |
| Kumar et al., 2012 [9] | India | Men and women with unexplained infertility (N = 1000). | Individuals of Indian origin in the general population (unpublished data) (N = 4500) | Prevalence of Inv(9) | Infertile cases: N = 26 (2.6%) General population: N = 33 (0.73) p < 0.001 compared to controls |
| Minocherhomji et al., 2009 [10] | India | Men and women with infertility (N = 760). | Age and geographically matched individuals without a history of infertility (N = 555) | Prevalence of Inv(9) | Infertile cases: N = 7 (0.9%) Fertile controls: N = 1 (0.2%) N.S. |
| Sahin et al., 2008 [11] | Turkey | Men and women with infertility (N = 276). | Amniocentesis from fetuses considered to be a sample of fertile population (spontaneous pregnancy) (N = 1130) | Prevalence of Inv(9) | Infertile cases: N = 4 (1.45%) Fertile controls: N = 8 (0.71%) N.S. |
| Xie et al., 2020 [12] | China | Men and women with infertility or RPL (N = 2816). | Adult patients without infertility were sent for karyotyping during the same time (N = 172) | Prevalence of Inv(9) | Infertile cases: N = 31 (2.1%) Fertile controls: N = 5 (2.91%) N.S. |
| Yamada et al., 1992 [13] | Japan | Men and women with more than two first-trimester pregnancy losses (N = 752). | Healthy volunteers (N = 1513) | Prevalence of Inv(9) | Infertile cases: N = 24 (3.2%) Fertile controls: N = 25 (1.7%) p = 0.02 |
| Studies reporting the prevalence of Inv(9) in individuals with infertility or RPL, no control group | |||||
| Azim, 2003 [14] | Pakistan | Men and women with RPL (N = 600). | None | Prevalence of Inv(9) | N = 4 (0.67%) |
| Cozaru et al., 2012 [15] | Romania | Men and women with RPL (N = 298) or primary infertility (N = 160). | None | Prevalence of Inv(9) | RPL: N = 2 (0.67%) Primary infertility; N = 4 (2.5%) |
| Dubey et al., 2005 [16] | India | Men and women with RPL (N = 1484). | None | Prevalence of Inv(9) | N = 3 (0.2%) |
| Dutta et al., 2011 [17] | India | Men and women with RPL (N = 2324). | None | Prevalence of Inv(9) | N = 14 (0.6%) |
| Elkarhart et al., 2019 [18] | Morroco | Men and women with RPL (N = 1254). | None | Prevalence of Inv(9) | N = 26 (2.1%) |
| Flynn et al., 2013 [19] | UK | Men and women with RPL (N = 1590). | None | Prevalence of Inv(9) | N = 1 (0.01%) |
| Ghazaey et al., 2015 [20] | India | Men and women with RPL (N = 1456). | None | Prevalence of Inv(9) | N = 20 (1.4%) |
| Makino et al., 1990 [21] | Japan | Men and women with RPL (N = 1278). | None | Prevalence of Inv(9) | N = 15 (1.2%) |
| Mozdarani et al., 2007 [22] | Iran | Men and women with at least 3 years of infertility (N = 601). | None | Prevalence of Inv(9) | N = 15 (2.5%) |
| Nonaka et al., 2019 [23] | Japan | Men and women with RPL (N = 4012). | None | Prevalence of Inv(9) | N = 52 (1.3%) |
| Rawal et al., 2020 [24] | India | Men and women with infertility, RPL, or IVF failure (N = 1276). | None | Prevalence of Inv(9) | N = 47 (3.7%) |
| Yuce et al., 2008 [25] | Turkey | Men and women with infertility (N = 2876). | None | Prevalence of Inv(9) | N = 41 (1.4%) |
| Studies comparing the prevalence of infertility or RPL in individuals with Inv(9) to controls | |||||
| Sipek et al., 2015 [26] | Czech Republic | Men and women with Inv(9) (N = 170) were identified from a large database of individuals referred for cytogenetic testing (N = 26,597). | Individuals with normal karyotypes were identified from the same overall cohort using the systemic sampling method (N = 661). | Prevalence of idiopathic reproductive failure | Inv(9): N = 63 (37.1%)Control: N = 214 (32.4%)p = 0.27 |
| Studies comparing the prevalence of infertility or RPL in individuals with Inv(9), no control group | |||||
| Demirhan et al., 2008 [27] | Turkey | Individuals with Inv(9) (N = 157) were identified from a large database of individuals referred for cytogenetic testing (N = 15,528). | None | Prevalence of RPL, primary amenorrhea, and infertility | Infertility: N = 2 (1.3%) RPL: N = 48 (29.9%) Primary amenorrhea: N= 4 (2.5%) |
| Yuksel et al., 2019 [28] | Turkey | Men and women with Inv(9) (N = 71) were identified from a large database of individuals referred for cytogenetic testing (N = 4168). | None | Prevalence of infertility and RPL | Infertility: N= 32 (45.1%) RPL: N = 4 (5.6%) |
| Teo et al., 1995 [29] | Singapore | Men and women with Inv(9) (N = 33) were identified from a large database of individuals referred for cytogenetic testing (N = 2448). | None | Prevalence of subfertility | Subfertility: N = 12 (36%) |
| Kosyakova et al., 2013 [30] | Multiple countries in Eastern + Western Europe | Individuals with Inv(9) were identified during routine diagnostic testing (N = 209). | None | Prevalence of infertility | Infertility: N = 79 (37.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bui, L.M.; Cooney, L.G.; Stanic, A.K. Rapid Ovarian Reserve Decline in a Woman with Pericentric Inv(9) Variant. Women 2023, 3, 421-431. https://doi.org/10.3390/women3030032
Bui LM, Cooney LG, Stanic AK. Rapid Ovarian Reserve Decline in a Woman with Pericentric Inv(9) Variant. Women. 2023; 3(3):421-431. https://doi.org/10.3390/women3030032
Chicago/Turabian StyleBui, Leeann M., Laura G. Cooney, and Aleksandar K. Stanic. 2023. "Rapid Ovarian Reserve Decline in a Woman with Pericentric Inv(9) Variant" Women 3, no. 3: 421-431. https://doi.org/10.3390/women3030032
APA StyleBui, L. M., Cooney, L. G., & Stanic, A. K. (2023). Rapid Ovarian Reserve Decline in a Woman with Pericentric Inv(9) Variant. Women, 3(3), 421-431. https://doi.org/10.3390/women3030032







