Exploring the Impact of Swimming on Body Mass Index and Body Fat in Individuals with Down Syndrome: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
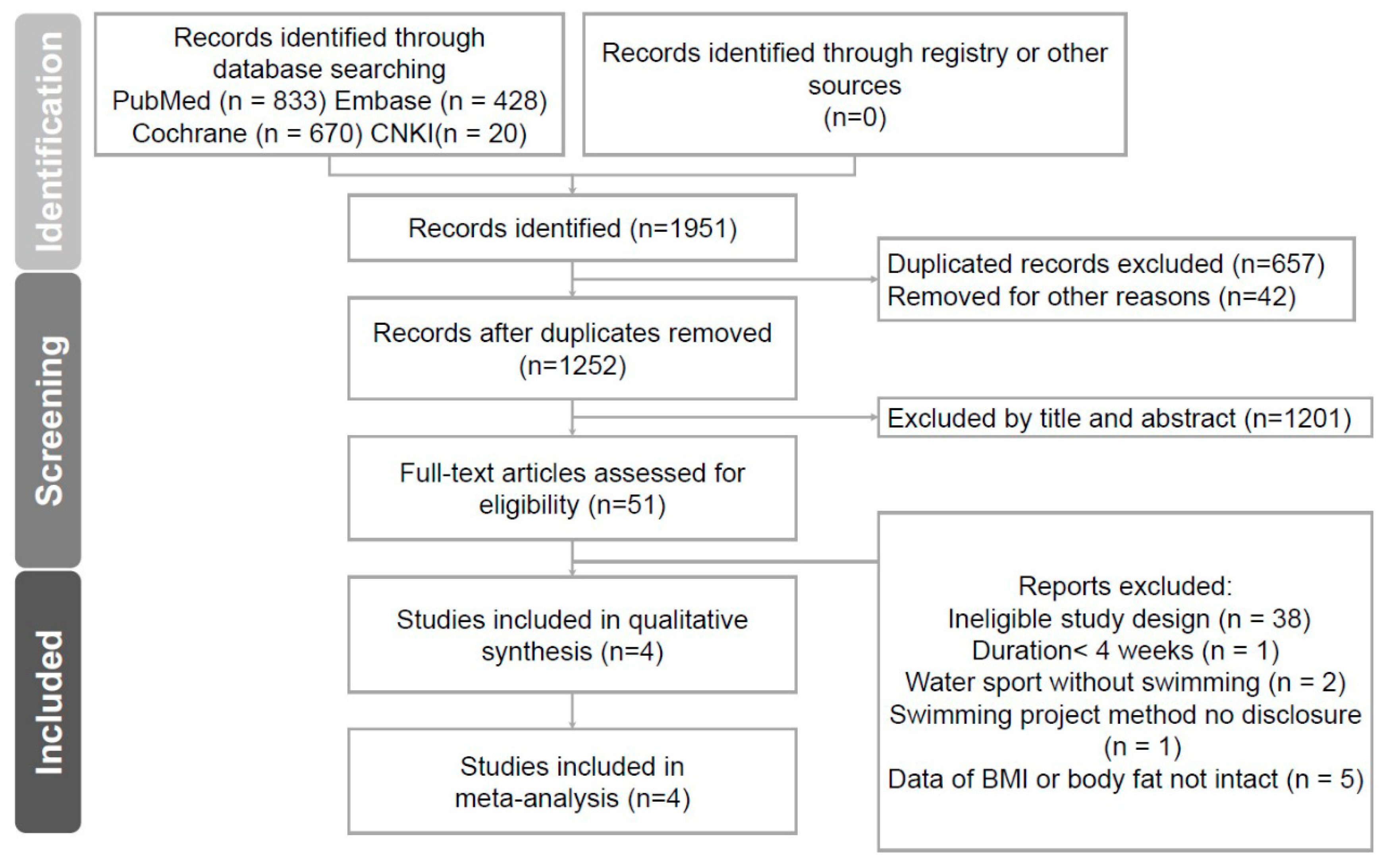
2.3. Study Selection
2.4. Data Collection and Risk of Bias Assessment
2.5. Data Synthesis and Analysis
3. Results
3.1. Study Search and Characteristics of Included Patients
3.2. Quality Assessment and Risk of Bias
3.3. Outcomes
4. Discussion
4.1. Novel Findings
4.2. Clinical Implications
4.3. Comparisons to Other Studies
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Antonarakis, S.E.; Skotko, B.G.; Rafii, M.S.; Strydom, A.; Pape, S.E.; Bianchi, D.W.; Sherman, S.L.; Reeves, R.H. Down syndrome. Nat. Rev. Dis. Primers 2020, 6, 9. [Google Scholar] [CrossRef]
- Hsieh, K.; Rimmer, J.H.; Heller, T. Obesity and associated factors in adults with intellectual disability. J. Intellect. Disabil. Res. 2014, 58, 851–863. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Espinosa, R.M.; Molina Vila, M.D.; Reig García-Galbis, M. Evidences from clinical trials in Down syndrome: Diet, exercise and body composition. Int. J. Environ. Res. Public Health 2020, 17, 4294. [Google Scholar] [CrossRef] [PubMed]
- Bertapelli, F.; Pitetti, K.; Agiovlasitis, S.; Guerra-Junior, G. Overweight and obesity in children and adolescents with Down syndrome-prevalence, determinants, consequences, and interventions: A literature review. Res. Dev. Disabil. 2016, 57, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Cushing, P.; Spear, D.; Novak, P.; Rosenzweig, L.; Wallace, L.S.; Conway, C.; Wittenbrook, W.; Lemons, S.; Medlen, J.G. Academy of Nutrition and Dietetics: Standards of practice and standards of professional performance for registered dietitians (competent, proficient, and expert) in intellectual and developmental disabilities. J. Acad. Nutr. Diet. 2012, 112, 1454–1464.e35. [Google Scholar] [CrossRef]
- Ranjan, S.; Nasser, J.A.; Fisher, K. Prevalence and potential factors associated with overweight and obesity status in adults with intellectual developmental disorders. J. Appl. Res. Intellect. Disabil. 2018, 31 (Suppl. S1), 29–38. [Google Scholar] [CrossRef]
- Meredith-Jones, K.; Waters, D.; Legge, M.; Jones, L. Upright water-based exercise to improve cardiovascular and metabolic health: A qualitative review. Complement. Ther. Med. 2011, 19, 93–103. [Google Scholar] [CrossRef]
- Ondrak, K.S.; Thorpe, D.E. Physiologic responses of adolescents with CP when walking on land and in water: A case series. J. Aquat. Phys. Ther. 2007, 15, 10–15. [Google Scholar]
- Querido, A.; Costa, M.J.; Araújo, D.; Sampaio, A.R.; Vilas-Boas, J.P.; Corredeira, R.; Daly, D.J.; Fernandes, R.J. Swimmers with Down Syndrome Are Healthier and Physically Fit than Their Untrained Peers. Healthcare 2023, 11, 482. [Google Scholar] [CrossRef]
- Ergu, N.; Konukman, F.; Zorba, E.; Cimen, Z.; Agbuğa, B.; Yılmaz, I. The Effects of Water Exercises and Swimming on Physical Fitness of Children with Mental Retardation. J. Hum. Kinet. 2009, 21, 105–111. [Google Scholar]
- Fragala-Pinkham, M.; Haley, S.M.; O’Neil, M.E. Group aquatic aerobic exercise for children with disabilities. Dev. Med. Child Neurol. 2008, 50, 822–827. [Google Scholar] [CrossRef]
- Kamińska, K.; Ciołek, M.; Krysta, K.; Krzystanek, M. Benefits of Treadmill Training for Patients with Down Syndrome: A Systematic Review. Brain Sci. 2023, 13, 808. [Google Scholar] [CrossRef]
- Scholes, S.; Fat, L.N.; Mindell, J.S. Trends in cardiovascular disease risk factors by BMI category among adults in England, 2003–2018. Obesity 2021, 29, 1347–1362. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K.; Ryoo, J.H.; Oh, C.M.; Choi, J.M.; Chung, P.W.; Jung, J.Y. Body fat percentage, obesity, and their relation to the incidental risk of hypertension. J. Clin. Hypertens. 2019, 21, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Suarez-Villadat, B.; Luna-Oliva, L.; Acebes, C.; Villagra, A. The effect of swimming program on body composition levels in adolescents with Down syndrome. Res. Dev. Disabil. 2020, 102, 103643. [Google Scholar] [CrossRef]
- Naczk, A.; Gajewska, E.; Naczk, M. Effectiveness of Swimming Program in Adolescents with Down Syndrome. Int. J. Environ. Res. Public Health 2021, 18, 7441. [Google Scholar] [CrossRef]
- Boer, P.H. The effect of 8 weeks of freestyle swim training on the functional fitness of adults with Down syndrome. J. Intellect. Disabil. Res. 2020, 64, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Riyahi Malayeri, S.; Zeinali, E.; Masoomeh, H.; Jalali, M. Effect of Swimming Training along with Omega-3 Intake on Irisin and Body Composition in Obese Girls with Down Syndrome. Med. J. Mashhad Univ. Med. Sci. 2020, 63, 2342–2349. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Escobedo-de la Peña, J.; Ramírez-Hernández, J.A.; Fernández-Ramos, M.T.; González-Figueroa, E.; Champagne, B. Body fat percentage Rather than body mass index related to the high occurrence of Type 2 diabetes. Arch. Med. Res. 2020, 51, 564–571. [Google Scholar] [CrossRef]
- Charmas, M.; Gromisz, W. Effect of 12-week swimming training on body composition in young women. Int. J. Environ. Res. Public Health 2019, 16, 346. [Google Scholar] [CrossRef] [PubMed]
- King, J.A.; Wasse, L.K.; Stensel, D.J. The acute effects of swimming on appetite, food intake, and plasma acylated ghrelin. J. Obes. 2011, 2011, 351628. [Google Scholar] [CrossRef] [PubMed]
- Dietz, W.H. Childhood weight affects adult morbidity and mortality. J. Nutr. 1998, 128, 411S–414S. [Google Scholar] [CrossRef]
- Andriolo, R.B.; El Dib, R.P.; Ramos, L.; Atallah, A.N.; da Silva, E.M. Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome. Cochrane Database Syst. Rev. 2010, 5, CD005176. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Baek, S.S. Effects of 24-week basketball programme on body composition and functional fitness on adults with Down syndrome. J. Intellect. Disabil. Res. 2022, 66, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Ordonez, F.J.; Fornieles, G.; Rosety, M.A.; Rosety, I.; Diaz, A.J.; Camacho, A.; Rosety, M.; Garcia, N.; Rosety-Rodriguez, M. A short training program reduced fat mass and abdominal distribution in obese women with intellectual disability. Int. J. Morphol. 2013, 31, 570–574. [Google Scholar] [CrossRef]
- Boer, P.H.; Moss, S.J. Effect of continuous aerobic vs. interval training on selected anthropometrical, physiological and functional parameters of adults with Down syndrome. J. Intellect. Disabil. Res. 2016, 60, 322–334. [Google Scholar] [CrossRef]
- Casey, A.F.; Rasmussen, R.; Mackenzie, S.J.; Glenn, J. Dual-energy x-ray absorptiometry to measure the influence of a 16-week community-based swim training program on body fat in children and adolescents with intellectual disabilities. Arch. Phys. Med. Rehabil. 2010, 91, 1064–1069. [Google Scholar] [CrossRef]
- Top, E. The effect of swimming exercise on motor development level in adolescents with intellectual disabilities. Am. J. Sports Sci. Med. 2015, 3, 85–89. [Google Scholar]
- Kim, K.H.; Lee, B.A.; Oh, D.J. Effects of aquatic exercise on health-related physical fitness, blood fat, and immune functions of children with disabilities. J. Exerc. Rehabil. 2018, 14, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Pérez, C.A.; Carral, J.M.C.; Costas, A.Á.; Martínez, S.V.; Martínez-Lemos, R.I. Water-based exercise for adults with Down syndrome: Findings from a preliminary study. Int. J. Ther. Rehabil. 2018, 25, 20–28. [Google Scholar] [CrossRef]
- Jacinto, M.; Vitorino, A.S.; Palmeira, D.; Antunes, R.; Matos, R.; Ferreira, J.P.; Bento, T. Perceived Barriers of Physical Activity Participation in Individuals with Intellectual Disability-A Systematic Review. Healthcare 2021, 9, 1521. [Google Scholar] [CrossRef] [PubMed]
- Ptomey, L.T.; Szabo, A.N.; Willis, E.A.; Gorczyca, A.M.; Greene, J.L.; Danon, J.C.; Donnelly, J.E. Changes in cognitive function after a 12-week exercise intervention in adults with Down syndrome. Disabil. Health J. 2018, 11, 486–490. [Google Scholar] [CrossRef]
- Gupta, S.; Rao, B.K.; Kumaran, S.D. Effect of strength and balance training in children with Down’s syndrome: A randomized controlled trial. Clin. Rehabil. 2011, 25, 425–432. [Google Scholar] [CrossRef]
- Barbosa, T.M.; Fernandes, R.; Keskinen, K.L.; Colaço, P.; Cardoso, C.; Silva, J.; Vilas-Boas, J.P. Evaluation of the energy expenditure in competitive swimming strokes. Int. J. Sports Med. 2006, 27, 894–899. [Google Scholar] [CrossRef]

| First Author | Country | Population | Study Design | Duration | Patients | Mean Age a | Outcome | Training Program |
|---|---|---|---|---|---|---|---|---|
| Suarez-Villadat, 2020 [16] | Spain | Adolescents | RCT | 36 weeks | 15 | 13.93 (1.23) | BMI, body fat | Total 50 min, HR b 110–180, twice a week |
| Naczk, 2021 [17] | Poland | Adolescents | RCT | 33 weeks | 11 | 14.9 (2.35) | BMI, body fat | Total 70–90 min, three times a week |
| Boer, 2020 [18] | South Africa | Adult | RCT | 8 weeks | 13 | 34.2 (5) | BMI | Total 30–40 min, three times a week |
| Malayeri, 2020 [19] | Iran | Adolescents | RCT | 8 weeks | 9 | 12.2 (2) | BMI, body fat | Average 33 min, six times a week |
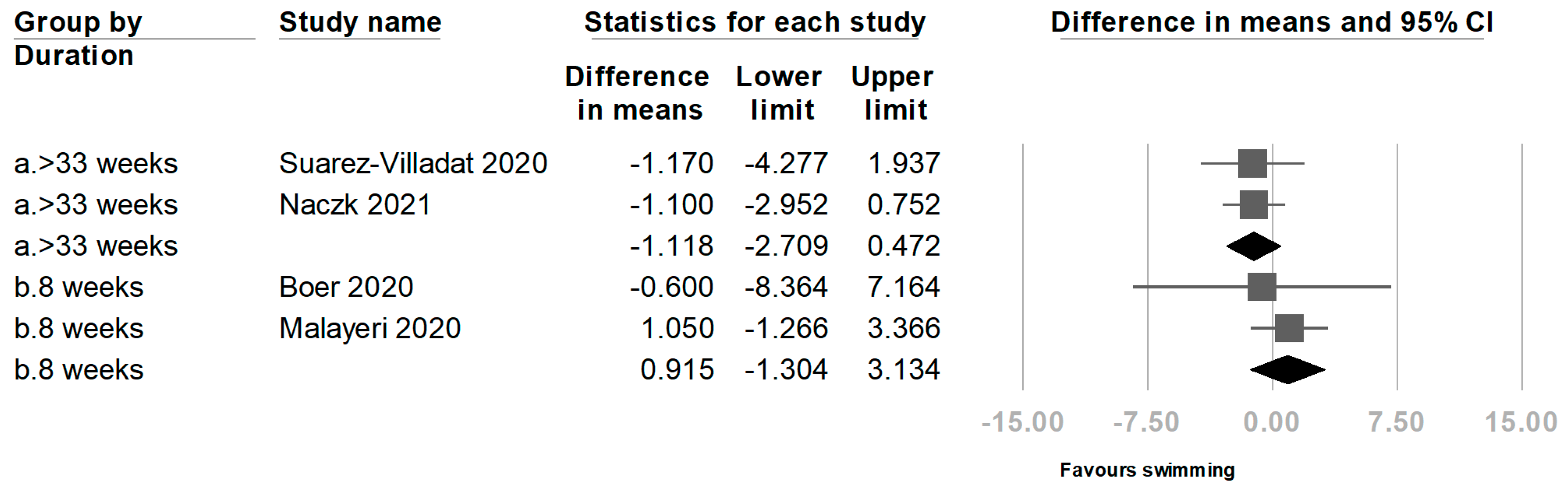
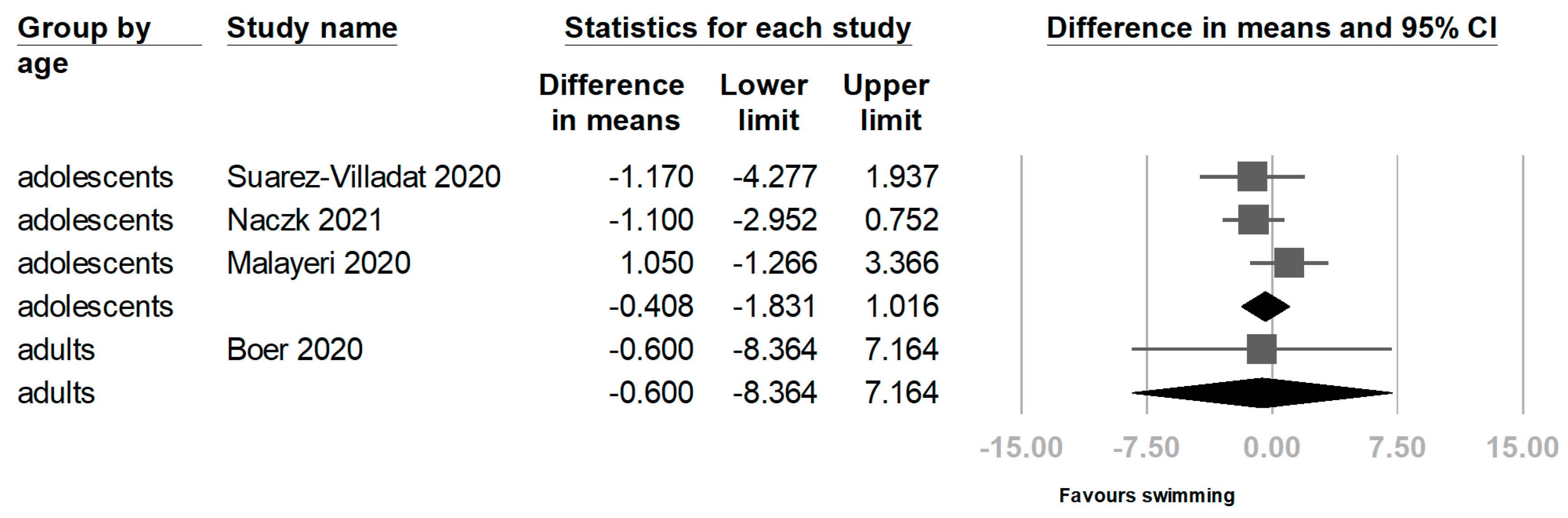
| Subgroup | Weight Mean Difference | 95% Confidence Interval |
|---|---|---|
| BMI: pooled | −0.428 | −1.721 to 0.865 |
| Duration | ||
| 33–36 weeks | −1.118 | −2.709 to 0.472 |
| 8 weeks | 0.915 | −1.304 to 3.134 |
| Age | ||
| Adolescents | −0.408 | −1.831 to 1.016 |
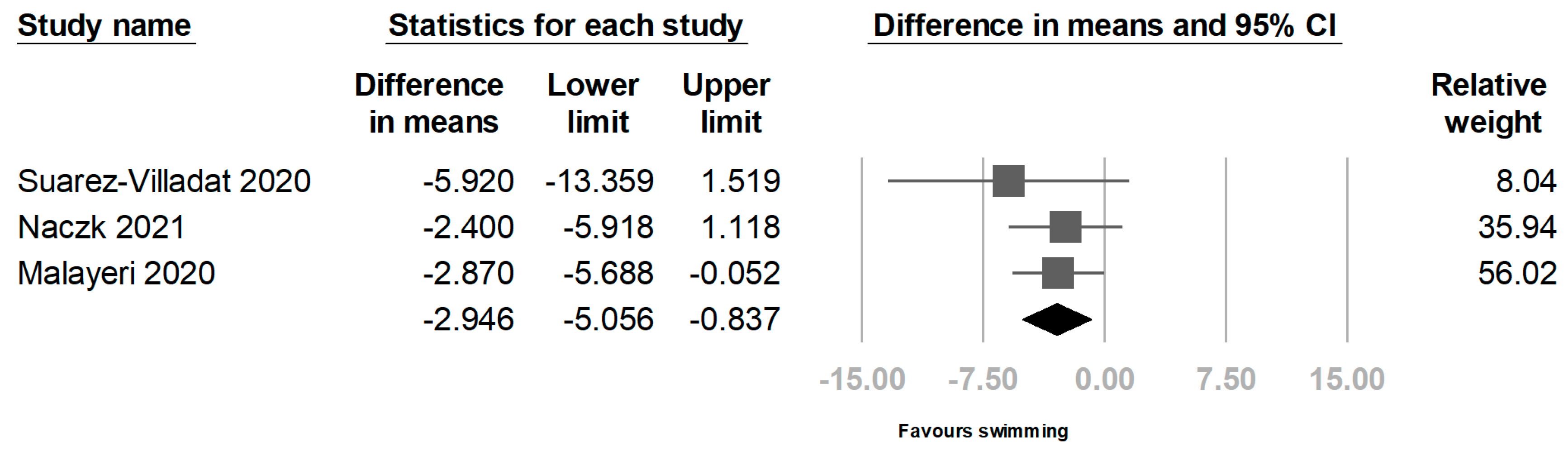
| Body fat (%): pooled | −2.946 | −5.056 to −0.837 |
| Duration | ||
| 33–36 weeks | −0.57 | −1.124 to −0.015 |
| Subgroup | Weight Mean Difference | 95% Confidence Interval |
|---|---|---|
| BMI: pooled, control (3 studies included) | 0.132 | −0.246 to 0.510 |
| Body fat (%): pooled, control (2 studies included) | 0.151 | −0.283 to 0.585 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, H.-T.; Yang, C.-C. Exploring the Impact of Swimming on Body Mass Index and Body Fat in Individuals with Down Syndrome: A Meta-Analysis. Obesities 2024, 4, 341-352. https://doi.org/10.3390/obesities4030027
Kuo H-T, Yang C-C. Exploring the Impact of Swimming on Body Mass Index and Body Fat in Individuals with Down Syndrome: A Meta-Analysis. Obesities. 2024; 4(3):341-352. https://doi.org/10.3390/obesities4030027
Chicago/Turabian StyleKuo, Hou-Ting, and Ciao-Ci Yang. 2024. "Exploring the Impact of Swimming on Body Mass Index and Body Fat in Individuals with Down Syndrome: A Meta-Analysis" Obesities 4, no. 3: 341-352. https://doi.org/10.3390/obesities4030027
APA StyleKuo, H.-T., & Yang, C.-C. (2024). Exploring the Impact of Swimming on Body Mass Index and Body Fat in Individuals with Down Syndrome: A Meta-Analysis. Obesities, 4(3), 341-352. https://doi.org/10.3390/obesities4030027






