Abstract
Burn injuries are a constant threat in war. Aspects of the modern battlefield increase the risk of burn injuries and pose challenges for early treatment. The initial resuscitation of a severely burn-injured patient often exceeds the resources available in front-line medical facilities. This stems mostly from the weight and volume of the intravenous fluids required. One promising solution to this problem is enteral resuscitation with an oral rehydration solution. In addition to being logistically easier to manage, enteral resuscitation may be able to mitigate secondary injuries to the gut related to burn shock and systemic immunoinflammatory activation. This has been previously studied in burn patients, primarily using electrolyte solutions, with promising results. Modern ORS containing sodium, potassium, and glucose in ratios that maximize gut absorption may provide additional benefits as a resuscitation strategy, both in terms of plasma volume expansion and protection of the barrier and immune functions of the gut mucosa. While enteral resuscitation is promising and should be used when other options are not available, further research is needed to refine an optimal implementation strategy.
1. Introduction
Major burn injuries that occur during war and disaster represent a significant challenge for low-resource and/or disrupted health systems. The resources needed to adequately resuscitate and care for burn-injured patients can quickly overwhelm those available in austere settings. In addition to a lack of burn care expertise, the large cube (i.e., weight, volume, size) of sterile intravenous (IV) fluids required for burn-injured patients in field units and far-forward settings remains a major limiting factor of austere burn care. Military medicine has sought innovative technical solutions to this in the form of various man-portable IV fluid makers and alternate resuscitation fluids, including colloids (e.g., starches, lyophilized plasma) or hypertonic saline, with only partial success. One strategy for alleviating IV fluid requirements is enteral resuscitation (EResus) with oral rehydration solution (ORS). The use of ORS in the treatment of another disease characterized by massive fluid losses, cholera, is already considered one of the greatest public health advances in modern times. While the evidence base is small, it has also shown success when applied to the resuscitation of burn-injured patients.
2. Battlefield Burn History and Epidemiology
Burn injuries are a ubiquitous threat on the battlefield, occurring in 5–20% of all casualties in conventional warfare [1]. The incidence of military burn injuries varies based on the setting and types of units involved in a conflict. Mechanized warfare between armored units and naval warfare in particular result in high rates of burn injuries. This is evident when comparing the rate of burn injuries from the Vietnam War (4.6%), fought largely by infantry, to the heavily mechanized 1973 Arab–Israeli War (10.5%) and the 1982 Lebanon War (8.6%) [2,3]. In the Falklands War, 34% of British naval casualties suffered burn injuries [4].
Advances in military clothing and vehicle technology have resulted in fewer and less severe burns among military personnel. This is evidenced by the reduced rate of burn injuries in Iraq and Afghanistan after the introduction of fire-resistant clothing and mine-resistant, ambush-protected vehicles to US forces in 2007 [5,6,7]. However, a large conflict between mechanized forces is estimated to generate thousands of moderate-to-severe (20–90% total body surface area (TBSA)) burn casualties requiring resuscitation [8,9].
Moreover, advances in protective equipment do not mitigate civilian harm in conflict settings. Civilians living in war zones also suffer from burn injuries caused by mechanisms including the use of explosive weapons in populated areas, incendiary weapons, and explosive ordnance. Increasingly, civilians are targeted by hostilities and now comprise up to 80% of those killed during war [10,11,12]. In addition to direct attacks on civilians and injuries caused by explosive ordnance, injuries also result from the deterioration of infrastructure and public safety [13]. In Baghdad during the Global War on Terror, the majority of burn injuries were not directly conflict-related but rather due to the degradation of infrastructure (e.g., electrical wires, unsafe cooking devices) and breakdown in usual safe behaviors [14]. Damage to the healthcare system, which is increasingly intentional, further compounds the challenges that civilians face during conflict [15].
3. Logistical Constraints
One of the main differences between being wounded on the battlefield and during peacetime is the delay in both stabilization and definitive care. It frequently takes hours to days to reach a specialized medical unit during prolonged-field-care scenarios or shipboard incidents, and days to weeks to evacuate a casualty from the point of injury to a burn center [16]. During this period, casualties are cared for with extremely limited resources, often only with the items the provider is able to carry in an aid bag. The fluid requirements for even a moderate-size burn cannot be transported by person for use in these scenarios.
Further, it can be difficult to obtain the IV or durable intraosseous access necessary to safely administer large volumes of fluids. A retrospective review of prehospital interventions performed for casualties during Operation Iraqi Freedom found that 40% of casualties arrived at combat support hospitals without IV access [17]. Only 50% of casualties with major burn injuries (i.e., >20% TBSA) had prehospital IV access, and only 85% of those with IV access had resuscitation initiated prior to arrival [18]. This delay in resuscitation is alarming, particularly for casualties with large burns, since time to resuscitation is a major predictor of mortality and even long-term health-related quality of life [19].
EResus can mitigate some of these logistical challenges. First, EResus can be accomplished with sachets of oral rehydration solution reconstituted with locally sourced potable (not sterile) water. Therefore, large volumes of sterile crystalloid solutions are not required. A 10 lb package of ORS is about the size of five bags of IV fluid but yields 125 L of fluid. The equivalent amount of IV fluid would weigh 287.5 lbs. Second, EResus does not require IV access. Fluids can be administered by drinking with or without buddy support. Lastly, if a patient is incapacitated or unable to drink, EResus can be administered via a nasogastric tube placed without advanced equipment.
4. History and Physiology of Enteral Resuscitation
EResus relies on the efficient enteral absorption of fluids and dissolved solutes (e.g., sodium, potassium, glucose). Under normal physiologic conditions, the bioavailability of water and electrolytes approaches near 100%, with only minimal amounts excreted in stool and a large reserve of excess absorptive capacity [20]. This excess absorptive capacity can be leveraged for the treatment of various disease states that cause dehydration.
The classic example of the lifesaving treatment potential of EResus is seen during acute watery diarrhea (e.g., cholera). During the 1831 European cholera epidemic, O’Shaughnessy and Latta developed a method of treating the profound dehydration caused by cholera with intravenous fluids [21]. Intravenous fluid resuscitation remained the mainstay of treatment for cholera until the 1970s, when enteral resuscitation with ORS came to prominence in South Asia.
The science behind enteral resuscitation rests on two physiological phenomena: (i) the independence of the absorptive and secretory functions of the gastrointestinal tract, and (ii) the cotransport of sodium and glucose by the sodium–glucose cotransporter (SGLT1) [22]. The discovery of sodium–glucose cotransport has been touted as “the most important medical advance of [the 20th] century” [23]. These findings, which were discovered in the 1950s, were not initially known to the physicians who would eventually develop ORS in the 1960s [24]. Early studies on EResus for people with cholera by US Navy researchers serendipitously used glucose to maintain the osmolality of the resuscitation solution. It was quickly recognized that glucose dramatically increased the absorption of sodium and water as well. This resuscitation strategy was further refined at the SEATO-Pakistan Cholera Research Laboratory in Dhaka and the Johns Hopkins Center for Medical Research and Training in Calcutta. This culminated in the work by Mahalanabis treating refugees of the Bangladeshi War of Independence, which demonstrated the effective use of ORS to treat cholera patients in a severely resource-limited field setting, leading to the widespread adoption of ORS around the world [24,25]. Since this report in 1968, the mortality from diarrhea in children under the age of five has dropped from 4.6 million per year to 500,000 [26].
5. Gut Physiology in Burns
The massive inflammatory response produced following a major burn injury leads to a systemic insult with multiorgan effects. The vasculature is one of the most profoundly and noticeably affected, with increased permeability leading to widespread edema and loss of intravascular volume. This loss of circulating blood volume, combined with variable degrees of myocardial dysfunction and altered systemic vascular resistance, engenders burn shock [27,28,29,30].
Burn shock results in splanchnic vasoconstriction and a nearly 50% reduction in blood flow to the GI tract [31,32]. Autopsies of burn-injured people found that more than 50% had evidence of mucosal ischemia and necrosis, which is consistent with endoscopic findings in living burn-injured patients [33]. This has a wide range of negative effects on the function of the entire GI tract, including global decreases in motility from the stomach to the colon [34,35,36,37,38,39]. More concerning, however, is the potential for increased infectious complications and immunoinflammatory activation.
After a burn injury, there is a breakdown of the physical barrier functions of the intestinal mucosa. In experimental models, increased intestinal permeability and histologic changes can be detected as early as one hour after injury, with decreased tight-junction protein synthesis and more severe histologic changes (e.g., necrosis, epithelial loss) at two hours after injury [40]. This increase in intestinal permeability has also been seen in burn-injured patients and correlates with burn size [41,42]. There is also evidence of pathological shifts and general collapse of the intestinal microbiome with early proliferation of more pathogenic bacterial species (e.g., Gram-negative rods, yeasts), which leads to further mucosal barrier immune dysfunction [43,44,45,46].
Collectively, these mucosal and microbiological changes allow for the translocation of bacteria and endotoxins into lymphatic and ultimately the central circulation, where they are disseminated throughout the body and potentiate organ dysfunction (e.g., acute respiratory distress syndrome, endothelial injury, cardiovascular dysfunction). The translocation of bacteria across the small intestine has been observed in animal models of burn injury with evidence of migration to the mesenteric lymph nodes, liver, spleen, kidneys, and lungs [32,44,47]. Although this gut–lymph translocation pathway has not been examined in burn-injured patients, a study of surgical patients undergoing laparotomy demonstrated translocation of bacteria into the mesenteric lymph nodes [48]. It is hypothesized that this translocation of intestinal bacteria and endotoxins is a key driver of sepsis and multisystem organ dysfunction in burn-injured patients [49,50,51].
Early enteral nutrition plays a key role in mitigating the damage to the gastrointestinal tract after a burn injury. Experimental models suggest that the gut mucosa is primarily fueled by luminal nutrients, and early enteral nutrition can help preserve gut barrier function, resulting in decreased bacterial translocation [52,53]. A trial of early enteral nutrition in burn-injured patients suggested that burn-shock-induced reduction in intestinal blood flow is reversible with early enteral feeding [54]. This improvement in intestinal blood flow and the resultant preservation of mucosal barrier function could explain the reduction in mortality, gastrointestinal hemorrhage, sepsis, and pneumonia in burn-injured patients who receive early enteral nutrition [55]. While ORS lacks many of the components of enteral nutrition formulas, the nutritional support it does contain may provide some of the benefits seen with early enteral nutrition.
Another key difference between EResus and enteral nutrition is that the volumes needed for EResus are significantly higher than those for enteral nutrition (e.g., 300–1200 mL/h versus 50–100 mL/h). The success of EResus relies on the ability of the stressed and damaged gastrointestinal tract to adequately absorb this volume. Fortunately, animal models and extensive experience with the EResus of patients with acute watery diarrhea have demonstrated that the gastrointestinal tract can absorb up to 20 mL/min. The US Army Institute of Surgical Research demonstrated that the gastrointestinal tract of burned pigs was able to absorb volumes commensurate with the Parkland formula (4 mL/kg/% TBSA burned) and with an efficiency similar to IV crystalloid [16]. There is also some evidence that Eresus has positive immunomodulating effects in animal models, but it is unclear if the magnitude of the benefit will be similar to those already receiving early enteral nutrition [56].
6. History of Enteral Resuscitation for People with Burn Injuries
Fluid losses from burn injuries are less visible than those from cholera. This led to the toxin theory of burn shock, which prevailed well into the 20th century. It was not until the Rialto Theatre Fire in 1921 that the toxin theory was challenged by Underhill [57]. Drawing on his experience with chemical-weapon victims during World War I, he noticed the marked hemoconcentration of his burn-injured patients and concluded they were suffering from severe fluid losses from damaged tissues [57]. He concluded that, like other diseases characterized by massive fluid losses, including cholera, the treatment should be “the forcing of fluid by whatever channel possible”, mainly intravenous but also via oral, subdermal, and rectal routes [57,58].
Another disaster, the Cocoanut Grove Nightclub Fire in 1942, marked the next development in burn resuscitation. Hospitals treating the victims of the fire used large volumes of plasma and crystalloid in their resuscitations. This approach was closely studied by the National Research Council in preparation for increased U.S. involvement in World War II. The combined colloid and crystalloid strategy would be battle-tested and ultimately codified in the Evans and Brooke formulas. The role for EResus in this strategy was thought optimal for people with smaller burns (e.g., <20% TBSA) and ideally after initial IV fluid resuscitation [59].
EResus was revived in the years immediately after World War II in response to the looming threat of nuclear warfare. Fearing overwhelming civilian casualties like those seen in Hiroshima and Nagasaki, the medical community was looking for an easy-to-administer, low-resource, safe, and effective treatment for burn shock, particularly for casualties with injuries that could be managed during a catastrophic event. In 1950, the US National Institute of Health (NIH) Surgery Study Section recommended the use of oral electrolyte solution for treatment in a mass-casualty burn scenario after experiments in mouse models demonstrated equivalent results with both enteral and IV resuscitation for burns [60]. Subsequent clinical studies refined the approach to oral resuscitation by using buffered solutions to improve palatability and decrease nausea and vomiting [61,62].
After the NIH statement, several clinical studies examining EResus ensued. Most continued using buffered electrolyte solutions [63,64,65,66,67,68]. Exceptions included work by Sørenson et al., who utilized a combination of a patient-selected clear fluid with salt tablets (7.5 g tablet per liter of fluid) as well as Franke and Kock-Marburn, who utilized an oral electrolyte solution containing glucose well before the development of ORS [69,70]. The limitations of many studies published before 1980 included the use of fixed resuscitation strategies that did not scale with the size of the burn injury and solutions not optimized for maximal gut absorption. This resulted in under-resuscitation and poor outcomes for patients with very large burns [71].
There have been relatively few studies examining the EResus of people with burn injuries since the dissemination of ORS worldwide in the 1970s and 1980s. Of the studies performed after 1970, three used glucose-containing solutions for resuscitation [72,73,74]. Ahnefeld demonstrated that one of the major limitations of EResus was poor tolerance in patients presenting after two hours and those in clinical shock (e.g., hypotension). This could be mitigated, however, with the continuous nasogastric administration of resuscitation fluids [72]. El-Sonbaty’s study comparing IV resuscitation using the Parkland formula and EResus using the World Health Organization ORS (WHO-ORS) was limited to only moderate burns, but it demonstrated no differences in key outcomes between the enteral and IV resuscitation strategies [73]. Moghazy combined the use of ORS with salt tablets and showed no difference in vital signs or urine output when compared to a control group receiving IV fluids alone [74].
7. Application of Enteral Resuscitation in the Austere Setting
As there have been no large randomized clinical trials to guide therapy, EResus indications, contraindications, and strategies vary widely. Resource availability may, therefore, dictate the strategy used. For patients with burns < 10–15% TBSA, oral intake ad libitum (i.e., to thirst) is usually the only resuscitation needed. For larger burns (>15–20% TBSA in adults and >10–15% TBSA in children), formal resuscitation with salt-containing fluids should be administered [75]. Lactated Ringer’s remains the principal resuscitation fluid even in low-resource settings, and IV access should be established as soon as possible to facilitate both resuscitation and pain management, as indicated [75]. In the event of limited IV fluid availability, EResus becomes a vital adjunct that permits the optimization of scarce resources while achieving key resuscitation endpoints (e.g., target urine output, normal vital signs indicative of adequate end-organ perfusion) and potentially mitigating the risks of gastrointestinal mucosal barrier and immunological dysfunction. Certain patients, particularly those with smaller burns, may be able to receive all their resuscitation enterally, and those with larger burns may have decreased IV fluid requirements with supplemental enteral resuscitation.
8. Solutions
A wide variety of solutions can be used during enteral resuscitation, but WHO-ORS is most optimized for intestinal absorption. The newer reduced-osmolarity ORS is generally preferred to the older formulation (i.e., 245 mOsm/L rather than 311 mOsm/L) but also has less sodium (75 mmol/L rather than 90 mmol/L). Reduced-osmolarity ORS has proven to be more efficacious in patients with acute watery diarrhea and is associated with reduced stool output, reduced vomiting, and a reduced need for IV fluid; however, there are concerns that it increases the risk of hyponatremia [76,77]. While there is some evidence of increases in mild biochemical hyponatremia (Sodium < 130 mmol/L), this does not appear to lead to increases in cases of symptomatic hyponatremia [77,78]. This may have implications for patients undergoing major burn resuscitation, among whom hyponatremia is common [79]. No EResus studies in burn patients have used the newer ORS formulation, but Sonbaty compared the old ORS formula against standard of care IV resuscitation using lactated Ringer’s and found equivalent rates of hyponatremia [73].
ORS is the most ubiquitous EResus solution and is widely available globally, given its status in the World Health Organization Model List of Essential Medicines. If prepared sachets are not available, ORS can be made with commonly accessible ingredients using the recipe in Figure 1 (e.g., (1 L of water + 0.5 teaspoon of salt + 6 teaspoons of sugar) or (1 L of water + 0.25 teaspoon of salt + 0.25 teaspoon of baking soda + 6 teaspoons of sugar or honey)). Care must be taken when using homemade solutions, however, as mixing failures are reported in studies that used family members to mix ORS [80]. Other solutions such as rice water, thin soups, or sports drinks (supplemented with ¼ tsp of both salt and baking soda per quart bottle) may also be used during a crisis when ORS is not immediately available but are less effective given that the ratios of sodium, potassium, and glucose are not optimized for gastrointestinal absorption [81]. Additionally, large volumes of hyperosmolar solutions may generate diarrhea, particularly in patients with ineffective brush border enzymes, and hyponatremic fluids can lead to systemic hyponatremia when administered in large volumes. When not using ORS, it is important to supplement every liter of fluid with 7.5 g of salt per Sørenson’s formula to avoid hyponatremia [73,75].

Figure 1.
Steps for making oral rehydration solution from readily available ingredients.
Several considerations are worth mentioning, including palatability, temperature, and route of administration. Numerous factors contribute to palatability, including electrolyte composition, sweetness, flavoring, temperature, and patient preferences [82]. Palatability is negatively affected by the high sodium content of enteral resuscitation fluids (>50 mmol/L) [83]. Commercial solutions touting improved palatability (e.g., drip drop, liquid IV) should be used with caution due to their lower sodium content (40–60 mmol/L vs. 75–90 mmol/L) than WHO-ORS, which could increase the risk of developing hyponatremia. Citrus-flavored solutions have higher palatability than unflavored solutions [84,85]. Room temperature (15–20 °C) to slightly cooler fluids are generally preferred [86]. Some patients find it easier to consume through a straw, particularly those with hand and/or face injuries. Nasogastric tube administration via either an enteral feeding pump or hourly gavage is useful for those who are intubated, have altered mental status, are unable to use their hands or arms, are without a buddy to help, or are sleeping.
9. Fluid Rates
EResus can be administered in accordance with fluid resuscitation formulas such as the modified Brooke (2 mL/kg/%TBSA burned, first 24 h) or Parkland (4 mL/kg/%TBSA burned, first 24 h) and adjusted according to resuscitation endpoints based on serial assessments (Figure 2). A simplified formula created by the US Army Institute of Surgical Research called the Rule of 10’s can also be used to determine the initial fluid rate for adults using the following formula: first, estimate burn size to the nearest 10; second, multiply the burn size (% TBSA) by 10 for the initial rate in mL/h; third, add 100 mL/h for every 10 kg over 80 kg [87].
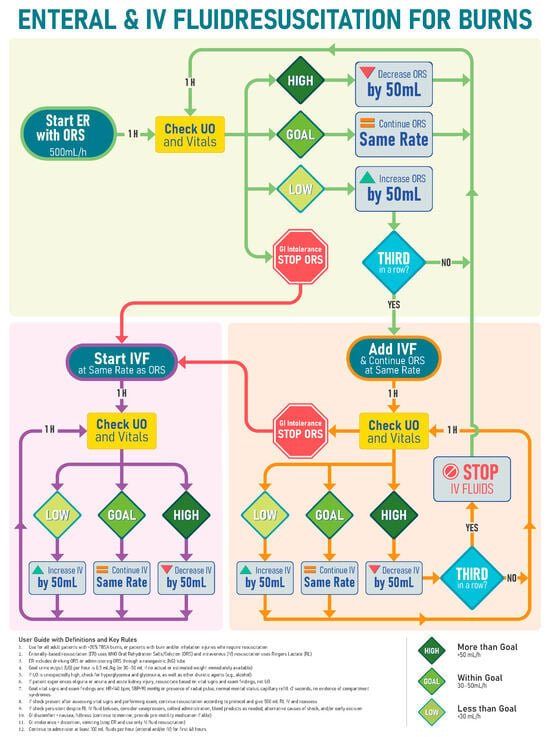
Figure 2.
Example resuscitation strategy for use in austere settings that combines enteral and intravenous fluid and does not require estimation of burn size or calculations.
A formula based on burn size can be difficult to implement without trained burn providers and in challenging operational environments [88,89,90]. The International Society for Burn Injuries (ISBI) guidelines recommend that patients with major burn injuries drink 15% of their body weight (in kilograms, that is, in liters) daily for the first two days after the burn injury [75]. A WHO Technical Working Group on Burns (TWGB) proposed an alternative formula of 100 mL/kg (~10% body weight) daily [91]. As can be seen in Figure 3, the strategy proposed by the TGWB is optimized for 20–50% TBSA injuries based on the assumption that patients with ≥60% TBSA burned are unlikely to survive in a burn disaster [92]. The simplest strategy, however, is the American Burn Association prehospital strategy, which recommends basing the initial fluid rate based on patient age (500 mL/h for age > 14 years, 250 mL/h for ages 6–13 years, and 125 mL/h for age <5 years) [93]. The performance of this age-based strategy diminishes at the extremes of weight (Figure 3) and should be adjusted to one of the above formulas as more information on the patient is obtained.
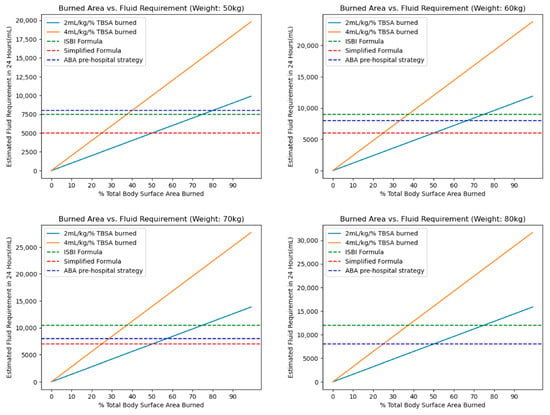
Figure 3.
Comparison of the modified Brooke (2 mL × kg × %TBSA), Parkland (4 mL × kg × %TBSA), International Society for Burn Injuries formula, World Health Organization Technical Working Group for Burns simplified formula proposal, and the American Burn Association prehospital fluid rate for adults across a range of weights. Abbreviations: total body surface area (TBSA), International Society for Burn Injuries (ISBI), American Burn Association (ABA).
It should be emphasized that resuscitation is different from ad libitum fluid intake. Thirst is stimulated relatively late in dehydration [82]. As a result, humans are often poor at replacing ongoing fluid losses [94]. Intake should therefore be encouraged proactively and recorded using a protocol such as the one in Figure 4. If the patient develops severe gastrointestinal intolerance such as refractory nausea, vomiting, or diarrhea, then it may be necessary to stop EResus and transition to IV resuscitation. Once the GI intolerance subsides (1–2 h), enteral intake and resuscitation can typically be restarted.
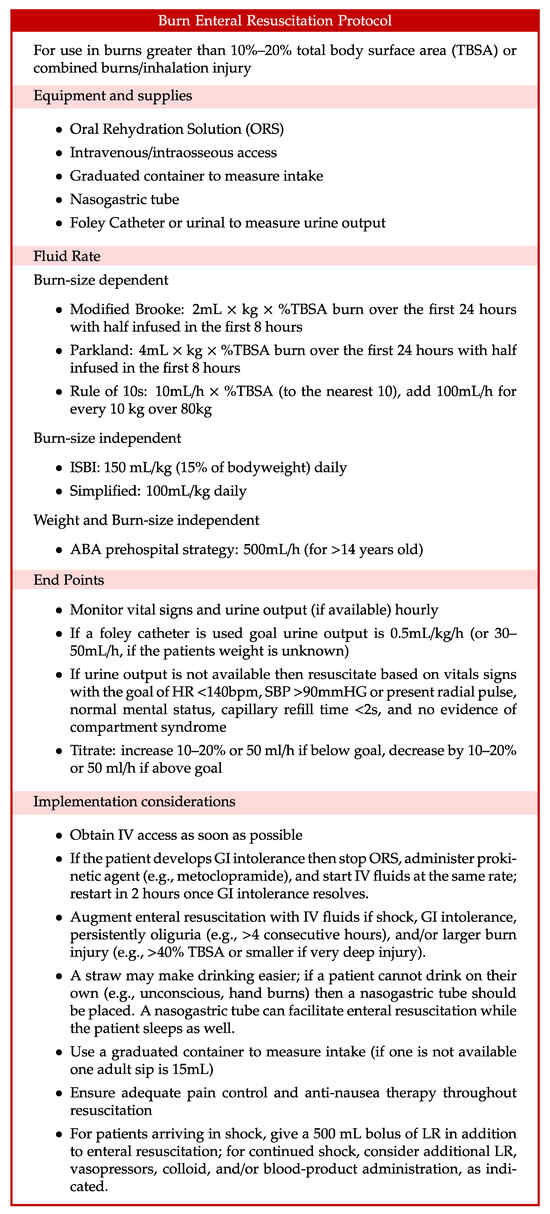
Figure 4.
Example enteral resuscitation strategy. Abbreviations: American Burn Association (ABA), gastrointestinal (GI), International Society for Burn Injuries (ISBI), intravenous (IV), lactated Ringer’s (LR), oral rehydration solution (ORS), total body surface area (TBSA).
10. Implications for Civilians in Conflict Settings
EResus has important implications for the care of civilian casualties in conflict settings. Burn-injured patients are among the most vulnerable subpopulations in war. A comprehensive analysis of humanitarian care provided by the U.S. military during the wars in Iraq and Afghanistan found that children under 12 were disproportionately affected by burn injuries (16% vs. 5% among all civilians) [95]. Children with war-related burns have been demonstrated to have mortality as high as 47%, compared to 11% mortality among all children with conflict-related injuries [96,97]. Due to the resource-intensive nature of burn care and the high associated mortality in low-resource settings, resuscitation (or comfort-focused care) of people with TBSA > 60% is one of only two criteria on which standards of trauma care vary for local nationals versus coalition forces personnel treated at deployed military treatment facilities [95]. Armed conflict in the 21st century is characterized by the increasing use of explosive weapons with wide-ranging effects on civilian populations. These munitions frequently inflict associated thermal injuries. In this context, it is critical that strategies such as EResus with the potential to improve survival among this population be pursued, scaled, and incorporated into trauma training designed for low-resource settings.
11. Future Directions
EResus is a practical solution for resuscitation in austere settings and a promising intervention in situations when early enteral feeding is not possible, particularly during prolonged-field-care scenarios and burn disasters. In addition to the clinical trials covered above, there are an increasing number of animal studies demonstrating some benefit with EResus [56,60,98,99,100,101,102,103,104,105,106]. However, limited evidence exists to create strong guidelines. Randomized controlled trials are underway in Nepal and Ghana to further our understanding of its safety, effectiveness, and implementation strategies. Additional translational research is needed as well, particularly regarding the effect of enteral resuscitation on intestinal mucosal barrier function, gut microbiome, and systemic immunoinflammatory activation.
Given the difficulty of conducting controlled trials, especially in operational settings, interventional and observational studies in other low-resource contexts will play a key role in refining therapy as it is applied on the battlefield. This will be difficult, however, and will require improvements in data collection systems. Even in large deployed medical facilities, data capture can be challenging, and this is only amplified for medical units closer to the front line. This difficulty is reflected in the diminishing quality and availability of data for U.S. soldiers treated in Role 2 (i.e., Forward Surgical Teams) and prehospital settings [107,108]. As the military focuses on prolonged field care, which encompasses EResus, data collection in austere environments will be crucial for process improvement.
Another area of ongoing research is the WHO-ORS formulation itself, which was transitioned to a low-osmolarity formula in 2002. There is now a push for the addition of resistant starches to the ORS formulation [22]. These starches would be fermented by gut bacteria into short-chain fatty acids (SCFA) that would be absorbed in the colon by active cotransport with sodium—a process similar to the way glucose is absorbed in the small intestine [109]. SCFA are also important inflammatory mediators in the gut and have been shown to improve barrier function [43]. Other groups focusing specifically on burn and trauma resuscitation have examined the addition of pyruvate to EResus formulas with promising results in animal models [102,103,104,105,106,110].
The interaction between early enteral feeding and enteral resuscitation will also need investigation. When gastric emptying and intestinal transit were compared between tube feeding formulas and enteral resuscitation fluids in a rat model, there was a significant delay in both gastric emptying and transit time with tube-feeding formulas [37].
12. Conclusions
Intravenous fluid resuscitation is a logistically difficult therapy to administer on the modern battlefield and in other austere settings. The crystalloid solutions conventionally used in burn resuscitation are bulky and will become increasingly scarce as blood products become the primary resuscitative fluid for hemorrhage. This means that those caring for conflict casualties may need to rely on alternative strategies for resuscitation after burn injuries, such as EResus. Previous studies on animal models suggest that enteral resuscitation using salt-containing solutions is effective for up to 40% TBSA burns. Relatively few studies have been conducted with ORS, which maximizes fluid and electrolyte absorption. While further research is needed to generate the evidence base for refinement of this technique, medical personnel should provide EResus using available resources when IV fluid therapy is not available.
Author Contributions
Conceptualization: I.F.J., K.N. (Kiran Nakarmi), H.B.W., K.N. (Kwesi Nsaful), K.M., R.S., D.R. and B.T.S. Writing-original draft preparation: I.F.J., H.B.W. Writing-review and editing: I.F.J., K.N. (Kiran Nakarmi), H.B.W., K.N. (Kwesi Nsaful), K.M., R.S., D.R. and B.T.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest. The views expressed in this article reflect the opinions of the authors and do not reflect the official policy or position of the U.S. Army, Department of Defense, or U.S. Government.
References
- Cancio, L.C.; Horvath, E.E.; Barillo, D.J.; Kopchinski, B.J.; Charter, K.R.; Montalvo, A.E.; Buescher, T.M.; Brengman, M.L.; Brandt, M.-M.; Holcomb, J.B. Burn Support for Operation Iraqi Freedom and Related Operations, 2003 to 2004. J. Burn Care Rehabil. 2005, 26, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.E.; Cancio, L.C.; Pruitt, B.A. Epidemiological, Demographic and Outcome Characteristics of Burns. In Total Burn Care; Elsevier: Amsterdam, The Netherlands, 2018; pp. 14–27.e2. ISBN 978-0-323-47661-4. [Google Scholar]
- Owen-Smith, M.S. Armoured Fighting Vehicle Casualties. J. R. Army Med. Corps 1977, 123, 65–76. [Google Scholar] [CrossRef]
- Chapman, C.W. Burns and Plastic Surgery in the South Atlantic Campaign 1982. J. R. Nav. Med. Serv. 1983, 69, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Eldad, A.; Torem, M. Burns in the Lebanon War 1982: “The Blow and the Cure”. Mil. Med. 1990, 155, 130–132. [Google Scholar] [CrossRef]
- Perez, K.G.; Eskridge, S.L.; Clouser, M.C.; Cancio, J.M.; Cancio, L.C.; Galarneau, M.R. Burn Injuries in US Service Members: 2001–2018. Burns 2023, 49, 461–466. [Google Scholar] [CrossRef]
- McLean, A.D. Burns and Military Clothing. J. R. Army Med. Corps 2001, 147, 97–106. [Google Scholar] [CrossRef]
- Tien, H.; Beckett, A. Medical Support for Future Large-Scale Combat Operations. J. Mil. Veteran Fam. Health 2022, 8, 18–28. [Google Scholar] [CrossRef]
- Thomas, B. Preparing for the Future of Combat Casualty Care: Opportunities to Refine the Military Health System’s Alignment with the National Defense Strategy; RAND Corporation: Santa Monica, CA, USA, 2021; ISBN 978-1-977406-86-6. [Google Scholar]
- Atiyeh, B.S.; Gunn, S.W.A.; Hayek, S.N. Military and Civilian Burn Injuries During Armed Conflicts. Ann. Burns Fire Disasters 2007, 20, 203–215. [Google Scholar]
- Guha-Sapir, D.; Schlüter, B.; Rodriguez-Llanes, J.M.; Lillywhite, L.; Hicks, M.H.-R. Patterns of Civilian and Child Deaths Due to War-Related Violence in Syria: A Comparative Analysis from the Violation Documentation Center Dataset, 2011–2016. Lancet Glob. Health 2018, 6, e103–e110. [Google Scholar] [CrossRef]
- McIntyre, J. Syrian Civil War: A Systematic Review of Trauma Casualty Epidemiology. BMJ Mil. Health 2020, 166, 261–265. [Google Scholar] [CrossRef]
- Donaldson, R.I.; Hung, Y.W.; Shanovich, P.; Hasoon, T.; Evans, G. Injury Burden During an Insurgency: The Untold Trauma of Infrastructure Breakdown in Baghdad, Iraq. J. Trauma Acute Care Surg. 2010, 69, 1379. [Google Scholar] [CrossRef] [PubMed]
- Stewart, B.T.; Lafta, R.; Shatari, S.A.E.A.; Cherewick, M.; Burnham, G.; Hagopian, A.; Galway, L.P.; Kushner, A.L. Burns in Baghdad from 2003–2014: Results of a Randomized Household Cluster Survey. Burns J. Int. Soc. Burn Inj. 2016, 42, 48–55. [Google Scholar] [CrossRef]
- Ignoring Red Lines Violence Against Health Care in Conflict 2022; Safeguarding Health in Conflict Coalition and Insecurity Insight; Safeguarding Health in Conflict Coalition: Baltimore, MD, USA, 2022; Available online: https://insecurityinsight.org/wp-content/uploads/2023/05/SHCC-Report-Ignoring-Red-Lines.pdf (accessed on 7 October 2023).
- Thomas, S.J.; Kramer, G.C.; Herndon, D.N. Burns: Military Options and Tactical Solutions. J. Trauma Acute Care Surg. 2003, 54, S207. [Google Scholar] [CrossRef]
- Lairet, J.R.; Bebarta, V.S.; Burns, C.J.; Lairet, K.F.; Rasmussen, T.E.; Renz, E.M.; King, B.T.; Fernandez, W.; Gerhardt, R.; Butler, F.; et al. Prehospital Interventions Performed in a Combat Zone: A Prospective Multicenter Study of 1003 Combat Wounded. J. Trauma Acute Care Surg. 2012, 73, S38–S42. [Google Scholar] [CrossRef] [PubMed]
- Lairet, K.F.; Lairet, J.R.; King, B.T.; Renz, E.M.; Blackbourne, L.H. Prehospital Burn Management in a Combat Zone. Prehosp. Emerg. Care 2012, 16, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.E.; Mileski, J.P. Mortality Determinants in Massive Pediatric Burns. Ann. Surg. 1997, 225, 554–569. [Google Scholar] [CrossRef]
- Charney, A.N. Intestinal “Bioavailability” of Solutes and Water: We Know How but Not Why. Yale J. Biol. Med. 1996, 69, 329–335. [Google Scholar]
- Foëx, B.A. How the Cholera Epidemic of 1831 Resulted in a New Technique for Fluid Resuscitation. Emerg. Med. J. 2003, 20, 316–318. [Google Scholar] [CrossRef][Green Version]
- Binder, H.J.; Brown, I.; Ramakrishna, B.S.; Young, G.P. Oral Rehydration Therapy in the Second Decade of the Twenty-First Century. Curr. Gastroenterol. Rep. 2014, 16, 376. [Google Scholar] [CrossRef]
- Water with Sugar and Salt. Lancet 1978, 312, 300–301. [CrossRef]
- Ruxin, J.N. Magic Bullet: The History of Oral Rehydration Therapy. Med. Hist. 1994, 38, 363–397. [Google Scholar] [CrossRef]
- Nalin, D.R. The History of Intravenous and Oral Rehydration and Maintenance Therapy of Cholera and Non-Cholera Dehydrating Diarrheas: A Deconstruction of Translational Medicine: From Bench to Bedside? Trop. Med. Infect. Dis. 2022, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Glass, R.I.; Stoll, B.J. Oral Rehydration Therapy for Diarrheal Diseases: A 50-Year Perspective. JAMA 2018, 320, 865–866. [Google Scholar] [CrossRef] [PubMed]
- Lund, T.; Reed, R.K. Acute Hemodynamic Effects of Thermal Skin Injury in the Rat. Circ. Shock 1986, 20, 105–114. [Google Scholar] [PubMed]
- Hilton, J.G.; Marullo, D.S. Effects of Thermal Trauma on Cardiac Force of Contraction. Burns. Incl. Therm. Inj. 1986, 12, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Adams, H.R.; Baxter, C.R.; Izenberg, S.D. Decreased Contractility and Compliance of the Left Ventricle as Complications of Thermal Trauma. Am. Heart J. 1984, 108, 1477–1487. [Google Scholar] [CrossRef]
- Merriam, T.W. Myocardial Function Following Thermal Injury. Circ. Res. 1962, 11, 669–673. [Google Scholar] [CrossRef]
- Morris, S.E.; Navaratnam, N.; Herndon, D.N. A Comparison of Effects of Thermal Injury and Smoke Inhalation on Bacterial Translocation. J. Trauma 1990, 30, 639–643; discussion 643–645. [Google Scholar]
- Jones, W.G.; Minei, J.P.; Barber, A.E.; Fahey, T.J.; Shires, G.T.; Shires, G.T. Splanchnic Vasoconstriction and Bacterial Translocation after Thermal Injury. Am. J. Physiol. 1991, 261, H1190–H1196. [Google Scholar] [CrossRef]
- Desai, M.H.; Herndon, D.N.; Rutan, R.L.; Abston, S.; Linares, H.A. Ischemic Intestinal Complications in Patients with Burns. Surg. Gynecol. Obstet. 1991, 172, 257–261. [Google Scholar]
- Chen, C.F.; Chapman, B.J.; Munday, K.A.; Fang, H.S. The Effects of Thermal Injury on Gastrointestinal Motor Activity in the Rat. Burns. Incl. Therm. Inj. 1982, 9, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, H.M.; Sallam, H.S.; Espana-Tenorio, J.; Chinkes, D.; Chung, D.H.; Chen, J.D.Z.; Herndon, D.N. Gastric and Small Bowel Ileus after Severe Burn in Rats: The Effect of Cyclooxygenase-2 Inhibitors. Burns J. Int. Soc. Burn Inj. 2009, 35, 1180–1184. [Google Scholar] [CrossRef] [PubMed]
- Sallam, H.S.; Oliveira, H.M.; Liu, S.; Chen, J.D.Z. Mechanisms of Burn-Induced Impairment in Gastric Slow Waves and Emptying in Rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R298–R305. [Google Scholar] [CrossRef]
- Sallam, H.S.; Kramer, G.C.; Chen, J.D.Z. Gastric Emptying and Intestinal Transit of Various Enteral Feedings following Severe Burn Injury. Dig. Dis. Sci. 2011, 56, 3172–3178. [Google Scholar] [CrossRef]
- Huang, H.-H.; Lee, Y.; Chen, C.-Y. Effects of Burns on Gut Motor and Mucosa Functions. Neuropeptides 2018, 72, 47–57. [Google Scholar] [CrossRef]
- Cummins, C.B.; Gu, Y.; Wang, X.; Lin, Y.-M.; Shi, X.-Z.; Radhakrishnan, R.S. Burn-Induced Impairment of Ileal Muscle Contractility Is Associated with Increased Extracellular Matrix Components. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2020, 24, 188–197. [Google Scholar] [CrossRef]
- Huang, Y.; Feng, Y.; Wang, Y.; Wang, P.; Wang, F.; Ren, H. Severe Burn-Induced Intestinal Epithelial Barrier Dysfunction Is Associated with Endoplasmic Reticulum Stress and Autophagy in Mice. Front. Physiol. 2018, 9, 441. [Google Scholar]
- Deitch, E.A. Intestinal Permeability Is Increased in Burn Patients Shortly after Injury. Surgery 1990, 107, 411–416. [Google Scholar] [CrossRef]
- Ryan, C.M.; Yarmush, M.L.; Burke, J.F.; Tompkins, R.G. Increased Gut Permeability Early after Burns Correlates with the Extent of Burn Injury. Crit. Care Med. 1992, 20, 1508–1512. [Google Scholar] [CrossRef]
- Huang, Z.; Huang, Y.; Chen, J.; Tang, Z.; Chen, Y.; Liu, H.; Huang, M.; Qing, L.; Li, L.; Wang, Q.; et al. The Role and Therapeutic Potential of Gut Microbiome in Severe Burn. Front. Cell Infect. Microbiol. 2022, 12, 974259. [Google Scholar] [CrossRef]
- Earley, Z.M.; Akhtar, S.; Green, S.J.; Naqib, A.; Khan, O.; Cannon, A.R.; Hammer, A.M.; Morris, N.L.; Li, X.; Eberhardt, J.M.; et al. Burn Injury Alters the Intestinal Microbiome and Increases Gut Permeability and Bacterial Translocation. PLoS ONE 2015, 10, e0129996. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Ogura, H.; Asahara, T.; Nomoto, K.; Matsushima, A.; Hayakawa, K.; Ikegawa, H.; Tasaki, O.; Kuwagata, Y.; Shimazu, T. Gut Microbiota and Environment in Patients with Major Burns—A Preliminary Report. Burns J. Int. Soc. Burn Inj. 2015, 41, e28–e33. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Sun, K.; Yin, S.; Jiang, B.; Chen, Y.; Gong, Y.; Chen, Y.; Yang, Z.; Chen, J.; Yuan, Z.; et al. Burn Injury Leads to Increase in Relative Abundance of Opportunistic Pathogens in the Rat Gastrointestinal Microbiome. Front. Microbiol. 2017, 8, 1237. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Xiao, G.X.; Wang, W.D.; Li, N. Endogenous Microbial Dissemination Following Severe Burns in Rats. Burns. Incl. Therm. Inj. 1986, 12, 325–329. [Google Scholar] [CrossRef]
- O’Boyle, C.J.; MacFie, J.; Mitchell, C.J.; Johnstone, D.; Sagar, P.M.; Sedman, P.C. Microbiology of Bacterial Translocation in Humans. Gut 1998, 42, 29–35. [Google Scholar] [CrossRef]
- Mittal, R.; Coopersmith, C.M. Redefining the Gut as the Motor of Critical Illness. Trends Mol. Med. 2014, 20, 214–223. [Google Scholar] [CrossRef]
- McMahan, R.H.; Boe, D.M.; Walrath, T.M.; Idrovo, J.-P.; Kovacs, E.J. Aging, Cutaneous Burn Injury and Multi-Organ Complications: The Role of the Gut. Adv. Geriatr. Med. Res. 2022, 4, e220004. [Google Scholar] [CrossRef]
- Magnotti, L.J.; Deitch, E.A. Burns, Bacterial Translocation, Gut Barrier Function, and Failure. J. Burn Care Rehabil. 2005, 26, 383–391. [Google Scholar] [CrossRef]
- Johnson, L.R.; Copeland, E.M.; Dudrick, S.J.; Lichtenberger, L.M.; Castro, G.A. Structural and Hormonal Alterations in the Gastrointestinal Tract of Parenterally Fed Rats. Gastroenterology 1975, 68, 1177–1183. [Google Scholar]
- Gianotti, L.; Alexander, J.W.; Nelson, J.L.; Fukushima, R.; Pyles, T.; Chalk, C.L. Role of Early Enteral Feeding and Acute Starvation on Postburn Bacterial Translocation and Host Defense: Prospective, Randomized Trials. Crit. Care Med. 1994, 22, 265–272. [Google Scholar] [CrossRef]
- Andel, H.; Rab, M.; Andel, D.; Felfernig, M.; Hörauf, K.; Felfernig, D.; Schramm, W.; Zimpfer, M. Impact of Early High Caloric Duodenal Feeding on the Oxygen Balance of the Splanchnic Region after Severe Burn Injury. Burns J. Int. Soc. Burn Inj. 2001, 27, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Pu, H.; Doig, G.S.; Heighes, P.T.; Allingstrup, M.J. Early Enteral Nutrition Reduces Mortality and Improves Other Key Outcomes in Patients with Major Burn Injury: A Meta-Analysis of Randomized Controlled Trials. Crit. Care Med. 2018, 46, 2036–2042. [Google Scholar] [CrossRef]
- Gómez, B.I.; Harrington, B.K.; Chao, T.; Chung, K.K.; Dubick, M.A.; Boggs, N.A.; Burmeister, D.M. Impact of Oral Resuscitation on Circulating and Splenic Leukocytes after Burns. Burns 2020, 46, 567–578. [Google Scholar] [CrossRef]
- Underhill, F.P. The significance of anhydremia in extensive superficial burns. JAMA J. Am. Med. Assoc. 1930, 95, 852. [Google Scholar] [CrossRef]
- Churchill, E.D. Surgeon to Soldiers: Diary and Records of the Surgical Consultant Allied Force Headquarters, World War II, 1st ed.; J.B. Lippincott Company: Philadelphia, PA, USA, 1972. [Google Scholar]
- Reiss, E.; Stirmann, J.A.; Artz, C.P.; Davis, J.H.; Amspacher, W.H. Fluid and Electrolyte Balance in Burns. J. Am. Med. Assoc. 1953, 152, 1309–1313. [Google Scholar] [CrossRef]
- Rosenthal, S.M. Experimental Chemotherapy of Burns and Shock. IV. Production of Traumatic Shock in Mice. V. Therapy with Mouse Serum and Sodium Salts. Public Health Rep. 1896–1970 1943, 58, 1429–1436. [Google Scholar] [CrossRef]
- Moyer, C.A. Recent Advances in the Chemical Supportive Therapy of Thermal Injury. Tex. State J. Med. 1949, 45, 635–639. [Google Scholar] [PubMed]
- Fox, C.L., Jr. Oral Sodium Lactate in the Treatment of Burn Shock. J. Am. Med. Assoc. 1944, 124, 207–212. [Google Scholar] [CrossRef]
- Markley, K.; Bocanegra, M.; Bazan, A.; Temple, R.; Chiappori, M.; Morales, G.; Carrion, A. Clinical Evaluation of Saline Solution Therpay in Burn Shock. J. Am. Med. Assoc. 1956, 161, 1465–1473. [Google Scholar] [CrossRef]
- Wilson, B.J.; Stirman, J.A. Initial Treatment of Burns. J. Am. Med. Assoc. 1960, 173, 509–516. [Google Scholar] [CrossRef]
- Davies, J.W. Blood Volume Changes in Patient with Burns Treated with Either Colloid or Saline Solutions. Clin. Sci. 1964, 26, 429–443. [Google Scholar]
- Jackson, D.; Cason, J.; Wallace, A.; Wilkinson, A. The Treatment of Burns Shock with Oral Hypotonic Saline-Bicarbonate Solution. In Research in Burns; E. Livingstone, Ltd.: London, UK, 1966; pp. 61–70. [Google Scholar]
- Monafo, W.W. The treatment of burn shock by the intravenous and oral administration of hypertonic lactated saline solution. J. Trauma Acute Care Surg. 1970, 10, 575. [Google Scholar]
- Maksimov, P.I. Comparative effectiveness of various methods of fluid therapy in the treatment of moderate and severe burn shock. Khirurgiia 1989, 3, 87–90. [Google Scholar]
- Sørensen, B. Saline Solutions and Dextran Solutions in the Treatment of Burn Shock. Ann. N. Y. Acad. Sci. 1968, 150, 865–873. [Google Scholar] [CrossRef]
- Franke, D.; Koch, H. Results of Almost Exclusive Peroral Fluid Intake through the Gastric Catheter in the Treatment of Burns in Children. Langenbecks Arch. Klin. Chir. Ver. Mit Dtsch. Z. Chir. 1964, 308, 55–60. [Google Scholar]
- Kramer, G.C.; Michell, M.W.; Oliveira, H.; Brown, T.L.H.; Herndon, D.; Baker, R.D.; Muller, M. Oral and Enteral Resuscitation of Burn Shock The Historical Record and Implications for Mass Casualty Care. Eplasty 2010, 10, e56. [Google Scholar]
- Ahnefeld, F.; Borst, R.; Bardua, R.; Vrabec, R.; Konícková, Z.; Moserová, J. Oral Ingestion of an Electrolyte Solution as Shock Prophylaxis in Burn Patients. In Proceedings of the Symposium for Treatment of Burns Held in Prauge, Prague, Czech Republic, 13–15 September 1973; pp. 74–79. [Google Scholar]
- El-Sonbaty, M. Oral Rehydration Therapy in Moderately Burned Children. Ann. Mediterr. Burn Club 1991, 4, 29. [Google Scholar]
- Moghazy, A.M.; Adly, O.A.; Elbadawy, M.A.; Hashem, R.E. Evaluation of Who Oral Rehydration Solution (ORS) and Salt Tablets in Resuscitating Adult Patients with Burns Covering More than 15% of Total Body Surface Area (TBSA). Ann. Burns Fire Disasters 2016, 29, 43–47. [Google Scholar] [PubMed]
- ISBI Practice Guidelines Committee; Ahuja, R.B.; Gibran, N.; Greenhalgh, D.; Jeng, J.; Mackie, D.; Moghazy, A.; Moiemen, N.; Palmieri, T.; Peck, M.; et al. ISBI Practice Guidelines for Burn Care. Burns 2016, 42, 953–1021. [Google Scholar] [CrossRef]
- Hahn, S.; Kim, Y.; Garner, P. Reduced Osmolarity Oral Rehydration Solution for Treating Dehydration Due to Diarrhoea in Children: Systematic Review. BMJ 2001, 323, 81–85. [Google Scholar]
- Musekiwa, A.; Volmink, J. Oral Rehydration Salt Solution for Treating Cholera: ≤270 mOsm/L Solutions vs. ≥310 mOsm/L Solutions. Cochrane Database Syst. Rev. 2011, 2011, CD003754. [Google Scholar] [CrossRef]
- Alam, N.H.; Yunus, M.; Faruque, A.S.G.; Gyr, N.; Sattar, S.; Parvin, S.; Ahmed, J.U.; Salam, M.A.; Sack, D.A. Symptomatic Hyponatremia During Treatment of Dehydrating Diarrheal Disease with Reduced Osmolarity Oral Rehydration Solution. JAMA 2006, 296, 567–573. [Google Scholar] [CrossRef]
- Sen, S.; Tran, N.; Chan, B.; Palmieri, T.L.; Greenhalgh, D.G.; Cho, K. Sodium Variability Is Associated with Increased Mortality in Severe Burn Injury. Burns Trauma 2017, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Meyers, A.; Sampson, A.; Saladino, R.; Dixit, S.; Adams, W.; Mondolfi, A. Safety and Effectiveness of Homemade and Reconstituted Packet Cereal-Based Oral Rehydration Solutions: A Randomized Clinical Trial. Pediatrics 1997, 100, E3. [Google Scholar] [CrossRef]
- Cancio, L.C.; Kramer, G.C.; Hoskins, S.L. Gastrointestinal Fluid Resuscitation of Thermally Injured Patients. J. Burn Care Res. 2006, 27, 561–569. [Google Scholar] [CrossRef][Green Version]
- Baker, L.B.; Jeukendrup, A.E. Optimal Composition of Fluid-Replacement Beverages. In Comprehensive Physiology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014; pp. 575–620. ISBN 978-0-470-65071-4. [Google Scholar]
- Wemple, R.D.; Morocco, T.S.; Mack, G.W. Influence of Sodium Replacement on Fluid Ingestion Following Exercise-Induced Dehydration. Int. J. Sport Nutr. 1997, 7, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Sohar, E.; Kaly, J.; Adar, R. The Prevention of Voluntary Dehydration. In Proceedings of the Lucknow Symposium, Lucknow, India, 7–13 December 1962; Volume 129, p. 135. [Google Scholar]
- Gyedu, A.; Mehta, K.; Baidoo, H.; Addo, D.; Abdullah, M.; Mesic, A.; Samosorn, A.; Cancio, L.C.; Nakarmi, K.; Stewart, B.T. Preferences for Oral Rehydration Drinks among Healthy Individuals in Ghana: A Single-Blind, Cross-Sectional Survey to Inform Implementation of an Enterally Based Resuscitation Protocol for Burn Injury. Burns 2022. [Google Scholar] [CrossRef]
- Boulze, D.; Montastruc, P.; Cabanac, M. Water Intake, Pleasure and Water Temperature in Humans. Physiol. Behav. 1983, 30, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.K.; Salinas, J.; Renz, E.M.; Alvarado, R.A.; King, B.T.; Barillo, D.J.; Cancio, L.C.; Wolf, S.E.; Blackbourne, L.H. Simple Derivation of the Initial Fluid Rate for the Resuscitation of Severely Burned Adult Combat Casualties: In Silico Validation of the Rule of 10. J. Trauma 2010, 69 (Suppl. S1), S49–S54. [Google Scholar] [CrossRef]
- Collis, N.; Smith, G.; Fenton, O.M. Accuracy of Burn Size Estimation and Subsequent Fluid Resuscitation Prior to Arrival at the Yorkshire Regional Burns Unit. A Three Year Retrospective Study. Burns 1999, 25, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.R.; Willand, L.; Gonzalez, B.; Sandhu, J.; Mosier, M.J. Quantitative Analysis of Estimated Burn Size Accuracy for Transfer Patients. J. Burn Care Res. 2017, 38, e30–e35. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, D.; Kamolz, L.-P.; Giretzlehner, M.; Haller, H.L.; Trop, M.; Selig, H.; Nagele, P.; Lumenta, D.B. The Potential Impact of Wrong TBSA Estimations on Fluid Resuscitation in Patients Suffering from Burns: Things to Keep in Mind. Burns 2014, 40, 241–245. [Google Scholar] [CrossRef]
- Hughes, A.; Almeland, S.K.; Leclerc, T.; Ogura, T.; Hayashi, M.; Mills, J.-A.; Norton, I.; Potokar, T. Recommendations for Burns Care in Mass Casualty Incidents: WHO Emergency Medical Teams Technical Working Group on Burns (WHO TWGB) 2017–2020. Burns 2021, 47, 349–370. [Google Scholar] [CrossRef]
- Leclerc, T.; Potokar, T.; Hughes, A.; Norton, I.; Alexandru, C.; Haik, J.; Moiemen, N.; Almeland, S.K. A Simplified Fluid Resuscitation Formula for Burns in Mass Casualty Scenarios: Analysis of the Consensus Recommendation from the WHO Emergency Medical Teams Technical Working Group on Burns. Burns 2021, 47, 1730–1738. [Google Scholar] [CrossRef]
- American Burn Association. Advanced Burn Life Support: Provider Manual; American Burn Association: Chicago, IL, USA, 2018. [Google Scholar]
- Greenleaf, J.E.; Sargent, F. Voluntary Dehydration in Man. J. Appl. Physiol. 1965, 20, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.M.; Graf, V.; Staudt, A.M.; Trevino, J.D.; VanFosson, C.A.; Wild, H.; Wren, S.M. Characterization of Humanitarian Trauma Care by US Military Facilities During Combat Operations in Afghanistan and Iraq. Ann. Surg. 2022, 276, 732–742. [Google Scholar] [CrossRef]
- Wild, H.; Stewart, B.T.; LeBoa, C.; Stave, C.D.; Wren, S.M. Pediatric Casualties in Contemporary Armed Conflict: A Systematic Review to Inform Standardized Reporting. Injury 2021, 52, 1748–1756. [Google Scholar] [CrossRef] [PubMed]
- Buyukbese Sarsu, S.; Budeyri, A. Mortality Risk Factors in War-Related Pediatric Burns: A Comparative Study among Two Distinct Populations. Burns J. Int. Soc. Burn Inj. 2018, 44, 1210–1227. [Google Scholar] [CrossRef]
- Gómez, B.; Harringtion, B.K.; Chao, T.; Little, J.S.; Heard, T.C.; Dubick, M.A.; Burmeister, D.M. Enteral Fluid Resuscitation Alters Splenic Function and Leukocyte Populations Post-Burn in Swine. J. Burn Care Res. 2018, 39, S82. [Google Scholar] [CrossRef]
- Michell, M.W.; Oliveira, H.M.; Kinsky, M.P.; Vaid, S.U.; Herndon, D.N.; Kramer, G.C. Enteral Resuscitation of Burn Shock Using World Health Organization Oral Rehydration Solution: A Potential Solution for Mass Casualty Care. J. Burn Care Res. 2006, 27, 819–825. [Google Scholar] [CrossRef]
- Gómez, B.I.; McIntyre, M.K.; Gurney, J.M.; Chung, K.K.; Cancio, L.C.; Dubick, M.A.; Burmeister, D.M. Enteral Resuscitation with Oral Rehydration Solution to Reduce Acute Kidney Injury in Burn Victims: Evidence from a Porcine Model. PLoS ONE 2018, 13, e0195615. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Chai, J.; Hu, S.; Zhou, G.; Sheng, Z. Oral Hypertonic Electrolyte-Glucose/Mosapride Complex Solution for Resuscitation of Burn Shock in Dogs. J. Burn Care Res. 2012, 33, e63–e69. [Google Scholar] [CrossRef]
- Liu, R.; Wang, S.-M.; Li, Z.-Y.; Yu, W.; Zhang, H.-P.; Zhou, F.-Q. Pyruvate in Reduced Osmolarity Oral Rehydration Salt Corrected Lactic Acidosis in Sever Scald Rats. J. Surg. Res. 2018, 226, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Hu, S.; Xie, Z.-Y.; He, Z.-J.; Luo, H.-M.; Lin, H.-Y.; Zhou, F.-Q.; Sheng, Z.-Y. Pyruvate Oral Rehydration Solution Improved Visceral Function and Survival in Shock Rats. J. Surg. Res. 2015, 193, 344–354. [Google Scholar] [CrossRef]
- Liu, R.; Hu, X.-H.; Wang, S.-M.; Guo, S.-J.; Li, Z.-Y.; Bai, X.-D.; Zhou, F.-Q.; Hu, S. Pyruvate in Oral Rehydration Salt Improves Hemodynamics, Vasopermeability and Survival after Burns in Dogs. Burns 2016, 42, 797–806. [Google Scholar] [CrossRef]
- Hu, S.; Liu, W.; Zhao, Y.; Lin, Z.; Luo, H.; Bai, X.; Sheng, Z.; Zhou, F. Pyruvate-Enriched Oral Rehydration Solution Improved Intestinal Absorption of Water and Sodium during Enteral Resuscitation in Burns. Burns J. Int. Soc. Burn Inj. 2014, 40, 693–701. [Google Scholar] [CrossRef]
- Hu, S.; Lin, Z.-L.; Zhao, Z.-K.; Liu, R.; Ma, L.; Luo, H.-M.; Zhou, F.-Q.; Bai, X.-D. Pyruvate Is Superior to Citrate in Oral Rehydration Solution in the Protection of Intestine via Hypoxia-Inducible Factor-1 Activation in Rats with Burn Injury. JPEN J. Parenter. Enteral Nutr. 2016, 40, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Mann-Salinas, E.A.; Le, T.D.; Shackelford, S.A.; Bailey, J.A.; Stockinger, Z.T.; Spott, M.A.; Wirt, M.D.; Rickard, R.; Lane, I.B.; Hodgetts, T.; et al. Evaluation of Role 2 (R2) Medical Resources in the Afghanistan Combat Theater: Initial Review of the Joint Trauma System R2 Registry. J. Trauma Acute Care Surg. 2016, 81, S121–S127. [Google Scholar] [CrossRef] [PubMed]
- Schauer, M.S.G.; April, M.M.D.; Naylor, M.J.F.; Oliver, C.J.J.; Fisher, M.A.D.; Kotwal, R.S. A Descriptive Analysis of Data from the Department of Defense Joint Trauma System Prehospital Trauma Registry. US Army Med. Dep. J. 2017, 92–97. [Google Scholar]
- Rao, M.C. Physiology of Electrolyte Transport in the Gut: Implications for Disease. In Comprehensive Physiology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 947–1023. ISBN 978-0-470-65071-4. [Google Scholar]
- Zhou, F.-Q. Advantages of Pyruvate-Based Fluids in Preclinical Shock Resuscitation-A Narrative Review. Front. Physiol. 2022, 13, 1027440. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).