Abstract
Surgical aortic valve replacement (SAVR) was the only symptom relieving and life-prolonging treatment until transcatheter aortic valve implantation (TAVI) became available. This option was introduced to treat old and high-risk patients. In a series of 2500 consecutive patients referred for SAVR with a biologic heart valve (BHV) prosthesis, their age, comorbid conditions, the complexity of the procedure, postoperative outcome, need for resources, and long-term survival were compared in patients before versus after the introduction of TAVI. Although the Carpentier-Edwards valve was used in most patients, the outcomes with respect to several other BHV types were studied. Patients undergoing isolated SAVR (i-SAVR) were studied separately from those who underwent SAVR with a concomitant procedure (c-SAVR). The number of referrals increased over time until 2016, whereafter the reimbursement for TAVI broadened. Age, prior percutaneous coronary interventions, diabetes, and chronic renal disease increased over time in both groups, while atrial fibrillation, the need for emergent SAVR, and other comorbid conditions increased significantly only in the c-SAVR group. Postoperative acute renal injury, conduction defects, and bleeding increased over time in both groups. The need for renal replacement therapy increased in both surgical groups, but this was more pronounced in c-SAVR; the need for a pacemaker implant (p < 0.001), blood products, and reintervention increased only in the c-SAVR group. There was a moderate but non-significant increase in the 30-day mortality for both groups over time. Furthermore, the long-term survival of both groups did not change after the introduction of TAVI. The Carpentier-Edwards Perimount valve showed good long-term results for durability. The Perceval device was used in older patients and showed good hemodynamic results, but the need for a postoperative permanent pacemaker implant was high. The results seem to indicate that a broader reimbursement for TAVI was warranted after its introduction in 2008. Nevertheless, with the development of newer devices for SAVR, surgery will remain one of the major treatment options for aortic valve disease.
1. Introduction
Degenerative or calcified aortic valve disease (CAVD) is a progressive condition, mainly occurring in elderly patients. An annual increase in the CAVD incidence rate of 0.49% was documented by echocardiography. The increase in severity was higher in patients who already had a severe disease [1]. Once CAVD has become symptomatic, especially with symptoms of congestive heart failure (CHF), the prognosis is considered to be poor if the condition is left untreated [2]. Disease progression toward the incremental involvement of the function of the left ventricle, the left atrium, the pulmonary circulation and, finally, the right ventricle, worsens the prognosis [3]. This observation was also made in the first year after surgical aortic valve replacement (SAVR) [4]. The same observation was made for the 5-year survival stage in patients with moderate aortic valve stenosis: all-cause and cardiovascular mortality had markedly increased after adjusting for age, sex, and decreased left ventricular function [5]. Improvement of the cardiac damage after SAVR only occurred in a part of the patients [6]. Before the introduction of transcatheter aortic valve implantation (TAVI), SAVR was the only life-prolonging and symptom-relieving treatment for symptomatic CAVD, even in elderly patients with comorbid conditions. With the implantation of the Carpentier-Edwards Perimount valve, good results have been obtained, as detailed in our earlier reports [7]. The Carpentier-Edwards device underwent several improvements, developing into the Carpentier-Edwards Magna and Magna Ease (CEME) devices. This development is comparable to the improvement of the Sapien balloon expandable percutaneous transcatheter device, into the Sapien XT and Sapien 3 valves. A common aspect was the lowering of the profile in order to clear the ostia of the coronary arteries. In one series, comparing SAVR and TAVI for two age groups, septuagenarians and octogenarians, the CEME device was used throughout for the SAVR, while the successive Sapien devices were used for the TAVI group. The investigated patients were very similar to the current group with respect to age, but coronary artery disease and the association of a CABG or any other procedure were seemingly absent [8]. A very recent report indicated that, even in octogenarian patients, a 5-year survival rate of over 60% could be reached for patients who left the hospital alive [9]. It also confirmed our early view that age in itself is not the only determinant of postoperative mortality [8]. Another of our older reports also indicated that the age and comorbidity of the referred patients increased in the period between 1987 and 2007 [10], until the introduction of TAVI. This procedure came into operation in the region of Antwerp, Belgium, in 2008. The aim of TAVI was to reduce postoperative complications and mortality, and serve as an alternative to SAVR for high-risk patients [11]. One could assume that a good level of penetration by the TAVI would reduce the referral of elderly high-risk patients for SAVR. If so, an improvement in the short and long-term outcomes after SAVR could be anticipated. In spite of this development, one contemporary report from Western society indicated that 30 to 40% of patients needing SAVR did not receive any valve procedure because of the existence of comorbid conditions [12]. Moreover, the bar for the reimbursement of TAVI was high in Belgium in the first few years after its introduction [13]. With this policy in mind, the following research questions need to be addressed with respect to the introduction of TAVI as an alternative to SAVR:
- (1)
- What is the change in the referral pattern for isolated SAVR (i-SAVR) and SAVR with additional procedures (c-SAVR) over time?
- (2)
- What are the changes in the complexity of the surgical procedures for c-SAVR over time?
- (3)
- What are the early and long-term outcomes for both surgical groups?
- (4)
- Is there a difference in the outcomes between the different types of BHV prostheses that were used in the current population?
2. Materials and Methods
This is a retrospective file study involving a series of 2500 consecutive patients, who underwent SAVR with a biological heart valve (BHV) prosthesis in a general hospital, from 1 January 1987 until 6 July 2017. The patients were referred by cardiologists on the basis of the severity of the symptoms and of the severity of the valve disease, which was determined by echocardiography and also through invasive catheter examinations. The patient group was subdivided into patients needing isolated SAVR (i-SAVR, n = 867) and patients with SAVR plus another procedure, such as CABG, mitral valve repair, a procedure on the ascending aorta, or a maze procedure, etc. (c-SAVR, n = 1613). Valves in other positions or mechanical valves in any position were excluded. Left ventricular (LV) function was determined by echocardiography or by ventriculography. Atrial fibrillation or a conduction defect of any type was recorded by ECG. Prior myocardial infarction was biochemically documented or recorded by ECG. An episode of prior CHF was documented in clinical files. Arterial hypertension was defined as a repeated arterial blood pressure > 140/90 mmHg, or being under chronic antihypertensive treatment. Endocarditis was diagnosed according to the modified Duke criteria. Significant coronary (CAD), peripheral, carotid, and left main coronary artery disease were defined as a stenosis of at least 50%, or the need for an invasive procedure. “Urgent” was defined as the need for SAVR at the initial hospital stay, during which the diagnosis of aortic valve disease was established. “Emergent” was defined as the need for SAVR in less than 24 h. A history of prior histologically proven malignancy was documented in a referral letter. Diabetes was defined as a fasting plasma glucose of >125 mg%, or the use of an antidiabetic treatment. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate below 60 mL/min. A CVA was defined as sudden neurologic deficits of >24 h, with documentation on medical imaging. Chronic obstructive pulmonary disease was defined as an FEV1 (forced expiratory volume at 1 s) < 80% of the predicted value. The following associated operative factors were registered: the type of valve prosthesis implanted, a need for CABG, any type of mitral valve repair, any procedure on the ascending aorta, a maze procedure, and the cardiopulmonary bypass (CPB) time. Before the introduction of TAVI, the Carpentier-Edwards Perimount valve, and from 2007 onwards, the Carpentier-Edward Magna Ease valve, were the only valves in use. Both devices were grouped and labeled as CEP devices because of the underlying concept that these devices share. The low stent base of the Magne Ease valve maximized the clearance of the coronary ostia. The type of BHV device implanted after 2008 was at the discretion of the individual surgeon who served in the department. These valves included Mitroflow, Mosaic Ultra, Crown, and Perceval devices. The Perceval prosthesis was selected specifically for elderly and high-risk patients and was, next to CEP valves, the only one in use at the end of the inclusion period. The need for resources was recorded as the number of units of packed cells, the use of plasma derivatives or thrombocyte concentrate, the need for a permanent pacemaker (PPM) implant, and the need for renal replacement therapy. For both i-SAVR and c-SAVR, preoperative, operative, and early postoperative data, as well as pre- and post-2008 parameters were compared using chi-square analysis, with the calculation of the p-value for categorical variables. For continuous variables, Student’s t-test was applied, with the calculation of the p-value and the effect size (Cohen’s D). For the specific outcome on the valve type concerning a PPM, logistic regression analysis was used. For long-term survival, the Kaplan–Meier log-rank test was applied. Cox’s proportional hazards analysis was used to identify the predictors of long-term mortality. The study was approved by the ZNA ethical committee under protocol N° 2656.
3. Results
3.1. Temporal Trends in the Referral, Preoperative, and Operative Parameters
Figure 1a shows the temporal trend in the referral for c-SAVR; Figure 1b shows this trend for i-SAVR. The vertical line indicates the introduction of TAVI in 2008. The patients depicted in the years 2019–2021 were the same patients who were subject to reoperations due to structural valve degeneration (SVD).
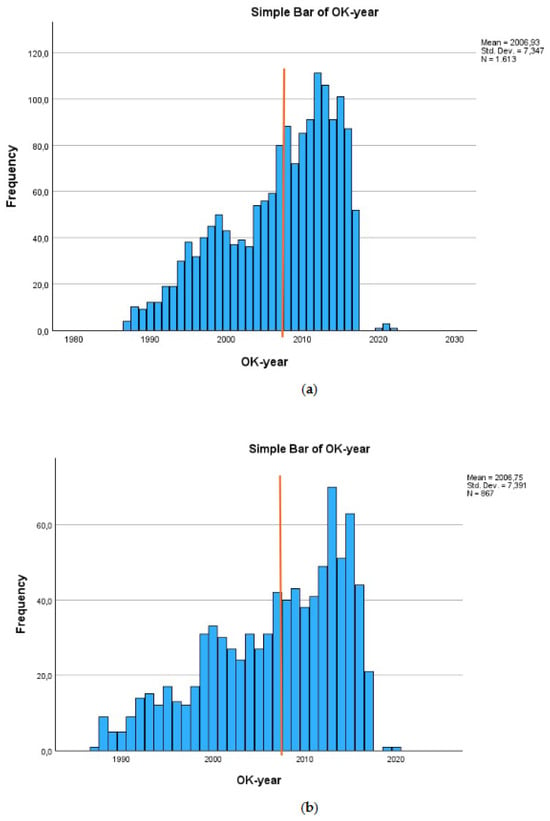
Figure 1.
(a) Temporal trend for referral combined SAVR. The orange bar indicates the introduction of TAVI (OK-year refers to year of operation); (b) temporal trend for referral for isolated SAVR. The bar refers to the introduction of TAVI (OK-year refers to year of operation).
The first five factors in Table 1 show a statistically significant increase over time for isolated SAVR, as well as for the combined procedure. These factors are an age of 80 years or older, prior percutaneous coronary intervention, diabetes, renal dysfunction, and male gender. For both surgical groups, there was also a significant decrease in the severity of the valve disease over time: the aortic valve area (AVA) increased from 71.2 ± 35.0 mm2 to 79.5 ± 25.3 mm2 in patients with a combined procedure (p < 0.001). For patients who underwent i-SAVR, this was 66.9 ± 32.3 mm2 and 72.8 ± 17.9 mm2 (p = 0.009). The last ten factors in the table are the preoperative factors, which increased significantly in the patient group who underwent c-SAVR, but not in the patients who underwent i-SAVR. The LVEF decreased significantly over time in patients who underwent c-SAVR (61.2 ± 16.9% vs. 59.1 ± 15.9%; p = 0.032). In patients who underwent i-SAVR, there was only a slight trend (64.8 ± 14.7% vs. 62.6 ± 15.1%, 0.081). Notably, peripheral artery disease was the only factor that increased significantly in the i-SAVR valve group. There were no significant changes for both surgical groups over time with respect to CHF, prior cardiac surgery, prior PPM implant, pulmonary dysfunction, or prior myocardial infarction. For severe aortic valve insufficiency, the rate before 2008 (c-SAVR) was 27/570 (4.7%), thereafter it was 22/477 (4.6%), which is not statistically significant (p = 0.920). For patients who underwent i-SAVR, this was 35/360 (6.9%) versus 15/273 (5.5%), with p = 0.458. In summary, these results indicate that patients referred for SAVR were increasing in age and their condition was worse over time. This temporal trend was worse in patients needing a c-SAVR, compared to those needing i-SAVR.

Table 1.
Distribution of preoperative factors across the eras.
3.2. Temporal Trends in Short-Term Postoperative Outcomes, Need for Resources, and Long-Term Survival
Table 2 shows the temporal distribution of the surgical parameters. Obviously, an increase in the complexity of the surgery is only observed in patients who underwent a combined procedure. The first five operative factors in Table 2 show the data for the combined procedure. An increase in the need for more than two procedures can be observed. This can be seen for mitral valve repair and for other procedures (mostly maze as a treatment for atrial fibrillation). The association of CABG decreased significantly over time, but the number remained above 90% throughout. The need for a procedure on the ascending aorta did not increase significantly over time (46/5.7 vs. 58/801, p = 0.202). The two factors at the bottom of the table compare the differences in the temporal trends for the operative parameters in both patient groups. Use of the smallest size of valve prosthesis decreased in both groups, but this decrease was non-significant. The increase in complexity in the combined group is also reflected by the significant increase in the need for CPB time of over 120 min, which is not observed in patients who underwent i-SAVR.

Table 2.
Distribution of operative factors across the eras.
A CEP device was the most implanted type of valve (n = 2153) throughout the inclusion period. Of the other valves, the Perceval rapid deployment valve (n = 48) is of most interest. This device came into use in 2013, especially for older patients with a higher risk score, and this is the only other valve used at the end of the inclusion period. All other devices, including Mosaic Ultra (n = 122), Mitroflow (n = 101), and Crown (n = 77) prostheses were discontinued at some time during the inclusion period. Compared to CEP devices, the Perceval valve allowed for a significantly shorter cross-clamp (52.23 ± 22.9 min vs. 68.4 ± 21.0 min, p < 0.001, with a moderate to large effect size, Cohen’s D = 0.763) and bypass time (79.9 ± 29.9 min vs. 121.7 min ± 42.6, p < 0.001, with a large effect size, Cohen’s D = 1.005), while the number of concomitant procedures, such as mitral valve repair and CABG, were not significantly different. The mean age of patients receiving the Perceval device was significantly higher (81.4 ± 4.1 years vs. 75.0 ± 6.4 years, p < 0.001 with a large effect size, Cohen’s D = 1.002). For EuroSCORE II, an increase was also observed for the Perceval device (8.0 ± 9.7% vs. 6.3 ± 7.3%), but this difference was not significant (p = 0.230), and the effect size was smaller (Cohen’s D = 0.230).
The need for postoperative resources (the need for prolonged ventilation or a prolonged stay in the ICU, the need for renal replacement therapy, the need for the transfusion of packed cells or for plasma derivatives) was very similar between the patients receiving a CEP device and the Perceval device, except for the need for a PPM implant. This was at least four times higher in the Perceval group, namely 5/48 (10.4%) vs. 50/2148 (2.3%), with a p-value < 0.001. Moreover, logistic regression analysis could identify only two independent predictors for the need for a postoperative PPM. These were preoperative conduction defects of any type with an odds ratio of 2.22 (1.29–3.82) and a p-value of 0.004, and the implantation of a Perceval device with an odds ratio of 5.29 (1.99–14.01) and a p < 0.001. Thirty-day mortality after implantation of a Perceval device was 5/48 (10.4%), which was twice as high compared to patients receiving a CEP device (105/2152 or 4.9%), but this difference was not significant due to low numbers (p = 0.082) for the Perceval valve. Multivariate analysis (Table 3) shows the predictor for 30-day mortality. The use of a Perceval device had no effect on the outcome (odds ratio of 1.03, with a p-value of 0.961). However, the higher age of the patients receiving the Perceval device has to be taken into account. The peak TVG (mm Hg) in regard to the Perceval device was significantly higher (22.9+/−7.8 vs. 18.6+/−7.6 mm Hg, with p = 0.001), while the mean transvalvular gradient (13.0+/−5.7 vs. 11.0+/−4.3 with p = 0.079) was slightly higher.

Table 3.
Predictors for 30-day mortality.
Table 4 shows the temporal trends for adverse postoperative events and the need for resources, in both surgical groups. In both groups, a modest increase in mortality can be observed, but this is not significant. However, a significant increase in acute renal injury, new or the progression of a preexisting conduction defect, and bleeding were observed for both groups. Postoperative endocarditis did not increase for either surgical groups over time. The overall incidence remained below one percent. A significant increase in need for renal replacement therapy was also observed for both surgical groups. A significantly increased need for a PPM implant, the need for reintervention and procedures associated with it, and the need for plasma or thrombocyte concentrate, were seen in patients who underwent c-SAVR, but not in those patients needing i-SAVR. This indicates that conduction defects and bleeding were less severe in patients who underwent i-SAVR.

Table 4.
Distribution of postoperative adverse events and need for resources across the eras.
Table 5 shows the survival for both surgical groups at 1, 5, and 10 years, with the patients at risk. Figure 2 depicts the same data (upper c-SAVR, lower i-SAVR). Survival after i-SAVR, as well as after the combined procedure was not affected by the era (p = 0.485).

Table 5.
Long-term survival for both surgical groups across the eras.
The five-year survival was higher for patients who had received a CEP device (78.5 ± 0.9%). This was lower in patients who received the Perceval (66.7 ± 7.3%) device. This difference was significant with p = 0.003, but the mean age of these patients was six years higher. SVD (SVD) in relation to the Perimount device was documented by echocardiography in 135/2153 (6.3%) at a mean of 112 (114–131) months. The need for a second valvular procedure (through SAVR or through TAVI) was seen in 54 (2.5%) of the patients at a mean of 113 (46–149) months. The durability of the Mitroflow valve with 11 events at a mean of 73 (65–81) months and the Crown valve with 10 events at a mean of 48 (38–57) months were considerably worse and the use, therefore, was discontinued. For the Perceval device, the number of observations was too low for any analysis concerning SVD, which could be related to the high age and consequently a lower life expectancy. Death could be considered as a competing event for SVD.
Figure 2a,b for all the devices combined:
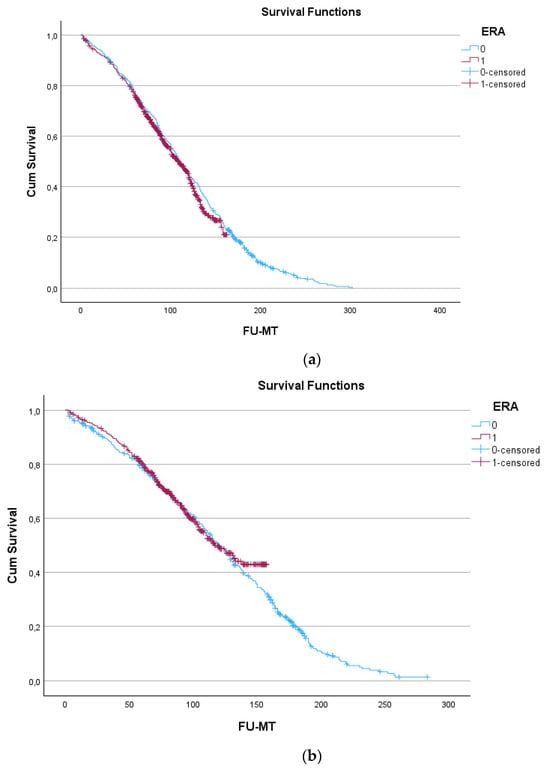
Figure 2.
FU-MT: follow-up in months; blue line: era before 2008 labeled as ‘0’; red line: era after 2008, labeled as ‘1’. Cum: cumulative. (a) top c-SAVR; (b) bottom i-SAVR.
Table 6 shows the predictors for long-term mortality for both eras, separately. An age over 80 years is the dominant predictor in the era before, as well as after, 2008. Chronic renal and pulmonary disease, as well as prior malignancy and peripheral artery disease are common predictors for this outcome in both eras. Diabetes, atrial fibrillation, and atrioventricular block are the only predictors in the later era. The implanted BHV (all types), throughout the series, is not identified as a predictor.

Table 6.
Predictors for long-term mortality in the early and later era.
4. Discussion
The current results describe the increase in referral numbers, patient age, and comorbid conditions, the complexity of the procedures, the increase in postoperative complications, and the increase in the need for postoperative resources, especially after c-SAVR. The CEP device was the only valve type used before 2008. In the later era, other BHV prostheses were introduced, but in addition to CEP devices, only the Perceval device was used for SAVR without a root procedure, until the end of the inclusion period. The 30-day mortality did not increase significantly and long-term survival in both eras was almost identical for i-SAVR, as well as for c-SAVR. The results also illustrate the outcomes for the different valves that were used.
4.1. Numbers of Referrals for Surgery
The first observation in the current series was the increase in the number of patients referred for i-SAVR, as well as for c-SAVR, after the introduction of TAVI in 2008. This increase was documented until 2016, noting that the inclusion of patients ended in June 2017. This observation is the continuation of an earlier and similar observation in our institution [10] and could also be observed in selected patients over 80 years old or patients with a prior malignancy [9,14,15]. Both patient groups could be good candidates for TAVI, because of a higher surgical risk or a lower life expectancy. Referral for TAVI is automatically the case for octogenarians in some institutions [16]. The currently documented increase in the use of SAVR was also observed in several other series [12,17,18,19,20,21,22,23,24,25,26,27,28]. This increase in number was observed in older as well as in younger patients [2,29]. A “halo effect”, i.e., the increased performance of SAVR because of the presence of the possibility for a TAVI-based treatment, could be held responsible [2,26,27]. This effect has been described as attracting more difficult patients to centers offering TAVI as a mode of valve replacement, but in whom SAVR was opted for after diagnostic work by the heart team. This increase seems to be a beneficial evolution, since there has been an underuse of aortic valve replacement by any means in the past [26,30]. However, this temporal trend for SAVR referral after the introduction of TAVI was not uniform [31]. In one series [32], the volume increased only in hospitals that did not perform TAVI. The volume of SAVR did not change significantly in several other series [16,19,33,34], while the volume was reduced in another five series [35,36,37,38,39]. In one recent series, the number of patients referred for SAVR decreased in all age groups (<65 years, 65–80 years, <80 years) between 2016 and 2019, while at the same time the use of TAVI increased for these same age groups.
4.2. Age and Comorbid Conditions
Closely related to the first observation is the significant increase in patients over 80 years, for both i-SAVR and c-SAVR. This trend related to an increase in patient age was already visible before the introduction of TAVI [10] and has also been documented in several more recently published patient series, with an increase of at least one year in age after the introduction of TAVI [17,21,24,26,27,36,40,41,42,43], or an increase in the octogenarian group [44]. However, there is no uniformity in this respect. A decrease in age of at least one year [25,32,38,42,45], or no significant change [12,20,28,33], was documented in several other series. In one series, an initial increase in the referral of octogenarians for SAVR was followed by a decline [46]. The decrease in the number of SAVR patients was most obvious in octogenarians [39]. Age was an important determinant for the use of TAVI in a recent study: the use of SAVR has been reduced to about 3%, while TAVI became almost the exclusive treatment option for octogenarians [22].
The third observation is related to comorbidity. EuroSCORE II was not included in the current series, because pulmonary artery hypertension was not routinely documented in the earlier era. However, this score could be assumed to be lower before 2008, since there was a clear increase over time in regard to age, diabetes, chronic renal dysfunction, peripheral artery disease, emergent status, and complexity of the surgical procedure. This was also reflected by a non-significant lower mortality before 2008 in both i-SAVR and c-SAVR patient groups. However, different trends could be observed in earlier published series. An increase in the risk score of patients referred for SAVR after the introduction of TAVI was demonstrated in several series [20,21,24,26,27,28,32,44,47], even in hospitals with a high TAVI volume [32]. This indicated that TAVI does not always “absorb” all high-risk patients. However, in other reports, the risk scores of patients referred for SAVR showed a decrease in the risk score over time [2,12,30,32,33,37,38,39], indicating that high-risk patients were increasingly referred for TAVI. A non-significant change in the risk score over the years was observed in six other series [12,20,28,29,32,48].
4.3. Complexity of the Procedure and the Use of Biological Valve Prostheses
The fourth current observation is the increasing complexity of the surgical procedure over time in patients undergoing c-SAVR: these associated procedures included the need for mitral valve repair, a procedure on the ascending aorta, or the maze procedure. This was reflected by a statistically significant increase the cardiopulmonary bypass time in c-SAVR patients, which was not observed in the i-SAVR group. However, the association of CABG did not increase over time in the current series. In most earlier series, only i-SAVR was investigated, which precludes any statement on changes in the complexity [18,19,20,24,25,32,33,34,36,37,40,41,42,44,46,49]. In elderly or high-risk patients for whom SAVR with associated CABG could be considered, TAVI combined with PCI could be an alternative. A CAD incidence of about 60% was observed in our prior surgical series [7,9], which is in line with a review showing that CAD was present in 40 to 75% of TAVI recipients [50]. The sequencing of interventions in patients with combined severe aortic valve disease and CAD is still a matter for debate. Only some observational series are available, and selection bias is possible [51,52].
The increase in the numbers related to our patient group might also reflect another trend: the increase in BHV prosthesis and the decrease in the use of mechanical valves (MHVs) over time. In prior series, the short-term outcome was better after the use of a BHV compared to a MHV [18,26]. However, in young patients receiving a BHV, a second procedure such as a valve-in-valve TAVI should be anticipated because of the risk of SVD. For this reason, the largest possible valves should be implanted. The trend to lower the use of the smallest valve was also observed in the current population, but this could also be related to an increase in the male gender. Although a future valve-in-valve TAVI could be considered [12,47], the long-term results are still unknown [53]. Moreover, surgeons tended to implant more larger-size valves in high-volume centers [28,47]. This should decrease the risk of severe residual transvalvular gradient after a future valve-in-valve procedure, which is a major predictor for SVD. However, re-operative SAVR has not reduced after the introduction of the valve-in-valve procedure. Repeat SAVR is an accepted option with a good outcome [24] in patients with an unsuitable anatomy for valve-in-valve procedures [47]. However, the CEP device has shown good durability in current and prior published series. For the Perceval device, this seemed to be less of an issue since the mean age of the patient receiving this valve was 81 years, indicating that the patients would not outlive their valves. Death could be considered as a competing event for SVD.
4.4. Short-Term Mortality, Adverse Events, and the Need for Resources
A fifth observation is the non-significant increase in the 30-day mortality in our series, after i-SAVR, as well as after c-SAVR. Most series, however, showed a decrease over time in 30-day mortality [2,16,17,18,20,21,23,24,26,32,33,34,38,39,40,44], in spite of an increase in the risk score. This decrease was highest in hospitals with a high-volume TAVI program. This trend toward a lower mortality could be expected if TAVI “absorbs” the high-risk patients. Patients with the highest risk score showed the greatest absolute reduction in mortality over time [34]. With adjustments for risk, this improvement in the outcomes was due to improved surgical techniques [24]. In other series, a non-significant increase in the 30-day mortality was documented [29,45,48,49,54,55]. An increase in the risk score did not lead to an increase in mortality in several series, but this seemed only true for i-SAVR [18,24,26,32,43].
The sixth observation concerns the need for resources, which reflects the severity of postoperative adverse events. The current series showed a highly significant increase in renal replacement therapy after both surgical procedures. This points toward an increase in acute renal injury for both patient groups. A similar observation was also made in a series of octogenarian patients, comparing the postoperative results of pre-TAVI with the early post-TAVI era [33]. One recent article discussed, in extensive detail, the risk factors for acute renal injury after SAVR and the development of CKD during the follow-up. The interesting aspect was the effect of the stage of CKD on the rapidity of the development of acute renal injury. The analysis identified the severity of CKD, as well as CPB, and the cross-clamp times as predictors. This is in line with the current observation that acute renal injury is less common with isolated SAVR, compared to SAVR with an associated procedure. The postoperative acute renal injury rate increased over time, as did the preoperative CKD (both surgical groups) and CPB time (only for combined surgery). The association of other procedures is expected to lead to longer operation times. It is also interesting to observe that, although a high age was identified as a factor with a significant effect, acute renal injury after SAVR is also a problem in younger patient groups (66 ± 11 years), part of whom received a mechanical valve prosthesis [56].
A PPM implant, reintervention, and the need for blood products also showed a significant increase over time, but significantly more after c-SAVR. An increased need for a PPM implant was especially seen after the implantation of a Perceval device. This was also observed earlier in a multicentric series [57]. A severe atrioventricular block and bleeding seemed worse in patients who underwent c-SAVR, since they needed more PPM implants, plasma derivatives, thrombocyte concentrate, and reinterventions. Another series found no increase in postoperative morbidity or mortality and a shorter length of stay in spite of higher comorbidity [20]. The currently observed early mortality after the implantation of Perimount, Mosaic Ultra, Mitroflow, and Perceval devices was not significantly different. Mortality was the highest in patients receiving Perceval valves, but this was due to a higher age and was in line with the postoperative outcomes of an octogenarian population [10]. It seems that the shorter CPB time associated with the Perceval device mitigates the effect of high age on hospital mortality.
4.5. Long-Term Survival and Long-Term Events
The long-term survival in our patient group was not affected by the era of SAVR: the curves were almost identical. This observation applies to both i-SAVR and to c-SAVR. The group that was operated on most recently, obviously had a shorter observation time. There were a few other reports concerning long-term survival. One year survival after an isolated SAVR improved significantly over time [2,12,30], especially in octogenarian patients [43]. Only the Perimount device was used throughout the study, resulting in large numbers with sufficient follow-up. This device was first implanted early in 1987 because of its design properties. The absence of contact between the leaflet and the sutures diminished the risk of leaflet damage. There was also an absence of friction areas over the Dacron stent [7]. For these reasons, this device was preferred, although surgeons had the discretion to use other biologic valve types. One of these HBV prostheses was the Perceval device, which was introduced in 2013 and used until the end of the inclusion period. The patients who received this valve had a shorter survival time, but this was due to the higher mean age. Moreover, only one event concerning valve failure and explantation was observed. Death could be considered as a competing event for the SVD of a Perceval device. One smaller monocentric series recorded the use of different biological devices [42], but without further analysis according to the era or outcome. Another series [47] described the use of different devices, indicating that Perimount and Hancock valves were used mostly throughout the study period, while the use of the Mitroflow valve increased during the later years. There was no analysis concerning the outcomes between these devices. Of more importance was the increase in use of larger diameter prostheses, in order to preserve the options for future valve-in-valve TAVI procedures.
4.6. The Carpentier-Edwards Valve and Other Potential Alternatives
The Carpentier-Edwards Perimount valve has a long track record of proven durability. It has leaflets of bovine origin, which have undergone treatment to reduce calcification and, hence, improve its durability. The Magna Ease device has a lower profile for easy insertion and closure of the aorta. It can be placed in a supra-annular position and allows optimal hemodynamic results. The sewing ring is also narrower. Not long after the introduction of TAVI, the rapid deployment of the sutureless Perceval device occurred. This BHV prosthesis can be implanted with lower cross-clamp and bypass times. It was mainly used in our elderly patients who had a higher EuroSCORE, which could explain why the 30-day mortality rate is not lower compared to the patients who received a Perimount device. The device could allow for minimally invasive SAVR, such as a partial sternotomy or a right anterior mini thoracotomy [56]. The latter approach, however, is technically challenging. In a meta-analysis, the Perceval valve proved to be equal to sutured valves, but better when compared to TAVI with respect to paravalvular leak, the need for a permanent pacemaker implant, postoperative stroke, and infarction [58]. However, the need for postoperative PPM proved to be high in our patients who received the Perceval device. Only two independent predictors were identified: the valve itself and preoperative conduction defects. Proper patient selection for the use of Perceval devices is necessary, since the postoperative need for PPM implantation is not benign. In another relatively small but very recently published series, early postoperative gradients were higher in the Perceval group [59], but these values equalized over time, something we also observed in the current series. We therefore should not expect long-term consequences from this issue. Another second rapid deployment valve, which was not used in the current series, involved the Intuity device, which is based on the frame of the CEME device [60]. The Intuity Elite device has the same properties, combined with the possibility of dry storage and handling, and has a high technical success rate [61]. Only three guiding sutures are needed. A balloon-expandable frame covered with cloth can be mounted in the left ventricular outflow tract (LVOT), which is widened. This improves the hemodynamic properties [56], but the need for PPM implantation remains high [61]. Another interesting and parallel development involved the Inspiris Resilia valve, which is also mounted on the Carpentier-Edwards Magna Ease frame. The tissue has also been glycerolized, which allows the dry storage and handling of the device. To facilitate possible future TAVI procedures, the frame has been made to be expandable by using a cobalt–chromium alloy band. During the TAVI valve-in-valve procedure, a radial force can be applied, allowing for uniform and predictable expansion. The perforated polyester band of the Inspiris Resilia valve is able to expand at each of the three commissures, without the need to achieve a high-pressure valve stent fracture. This reduces the risk for stroke and other procedural complications. The recently published COMMENCE trial showed promising results, with low 30-day mortality, adverse event reoperation rate, and a favorable hemodynamic profile. At 5 years, these results were sustained [62]. In a meta-analysis, no differences in the outcomes were observed compared to the conventional Carpentier-Edwards valve, but long-term studies are needed [63].
The concept of surgically implanting a biologic valve prosthesis in younger patients is also evolving. One interesting manuscript dealt with several problems, addressing the complication rates, reoperation rate, and reduced survival after aortic valve procedures in relatively young patients. These patients have a longer exposure to potential valve-related complications, which could be mitigated by the application of aortic valve repair, the Ross procedure, or the implantation of tissue-engineered heart valves [64]. However, the current patient population is older, with a much more limited life expectancy and suffers mainly from degenerative aortic valve disease with stenosis. This precludes the use of aortic valve repair or the Ross procedure, which also involves the pulmonary valve. Furthermore, no long-term animal models for tissue-engineered heart valves are available. Although the implantation of a mechanical valve was an exclusion criterion for the current series, it is noteworthy that a loss of life expectancy after implantation of an aortic valve prosthesis results in a loss of life expectancy, which is worse after a biological valve, compared to a mechanical prosthesis. With biological valve prostheses, there is also a higher reintervention rate. The use of valve-in-valve TAVI might be promising in this respect, but this issue still remains to be documented by long-term observations [65]. One remaining issue is the use of stentless aortic valve prostheses in patients with small annuli. In our patient population, this was not a routine procedure. Stentless valves show better hemodynamic performance during exercise, but are technically more demanding to implant and require more postoperative permanent pacemaker implants. These devices seem less suitable for elderly patients, who have a limited exercise capacity. In one series, the patient population receiving a stentless device was considerable younger compared to ours (61+/−12 y) and there was a much higher proportion of redo-surgery (31%). The rate of preoperative infective endocarditis was also higher (27%). Operation times were also considerably longer, which is undesirable in elderly patients. The comparison between stented and stentless devices did not offer long-term advantages with respect to survival, the adverse event rate, and the reoperation rate. The need for permanent pacemaker implantation in the stentless group [66] was one of the reasons for us not to use these devices routinely in patients with small annuli.
5. Future Prospects
In a 30-year time span, a clear increase in referrals for i-SAVR, as well as for c-SAVR, could be observed in the current series. The increase in the rate of preoperative comorbid conditions was more pronounced in patients who underwent c-SAVR, compared to those who underwent i-SAVR. For the c-SAVR group, the complexity of the procedure also increased. These observations could be linked to an increase in postoperative comorbid events, which were most pronounced in the c-SAVR group. The increase in the need for resources followed a comparable pattern. There was, for both surgical groups, a modest and non-significant increase in the 30-day mortality rate. The long-term survival curve before and after the introduction of TAVI were almost identical for both groups. The reimbursement policy could have a major effect on the referral for SAVR after the introduction of TAVI. The Belgian policy [13] was very strict until at least 2017: advice was given in the past not to reimburse symptomatic aortic valve patients for TAVI, even if these patients had serious comorbid conditions with high operative risk. According to the authors, these patients should be referred for SAVR, and the TAVI procedure should be reserved for patients deemed inoperable for anatomical reasons. This differed largely from other countries, such as Germany, where the sum of valve procedures increased over time in all age classes, mostly in patients older than 80 years. TAVI even outpaced SAVR, while surgical procedures decreased moderately [39]. For patients with associated CAD, the approach is more complicated, since there is still no consensus concerning the timing of PCI with respect to the TAVI procedure.
One remarkable and recently published analysis showed that octogenarian patients who were initially referred for TAVI and redirected toward SAVR did better than octogenarian patients who were referred for SAVR. The preoperative multidisciplinary assessment, by a heart team, of octogenarians was associated with lower in-hospital mortality and adverse events after SAVR. Although the numbers were relatively small, the conclusion was strengthened by propensity score match analysis [67]. These findings, as well as several recently published surgical series [2,14,15,21,22,23,24,25,29,33,44,45], support our own finding that even in elderly and high-risk patients, SAVR can offer acceptable long-time survival, with potential consequent development of adverse events such as SVD. The surgical option still has a competitive value for the foreseeable future for both older and younger patients. Perimount valves have proven their value in this respect [63]. The rapid deployment of valves, such as the Perceval BHV, with a minimally invasive approach seems a good option for relatively old patients, while the Inspiris Resilia valve can be offered to their younger counterparts. With the development of this device, a valve-in-valve TAVI could be anticipated in the case of future SVD, especially when these patients are older and more frail. However, coronary complications such as infarction and severe patient prosthesis mismatch should always be anticipated. A redo-SAVR might be a better option in younger and low-risk patients, since this option has better safety and efficacy. Long-term results, however, are still lacking. All these developments (minimal surgical access, rapid deployment, sutureless devices, expandable valves) indicate that SAVR has a viable future. These surgical developments should be part of a comprehensive strategy to treat aortic valve disease, complementary to TAVI, especially when future procedures, such as redo-SAV or valve-in-valve TAVI, are anticipated. The involvement of a heart team and the potential redirection of patients from TAVI toward SAVR confirm this view.
6. Conclusions
Surgical aortic valve replacement remains a viable option for the future. The Carpentier-Edwards Perimount device has a proven track record concerning its durability and hemodynamic profile. In selected elderly and high-risk patients, implantation of the Perceval device remains an option. The need for postoperative PPM implantation is an area of concern. The recent development of other rapid deployment valves and expandable BHV devices, which anticipate a future valve-in-valve TAVI, offer other viable surgical options.
7. Limitations
Because of the long inclusion period, the improvement in peri and postoperative care could affect the postoperative outcomes. Standard long mechanical ventilation was replaced by fast-track anesthesia in 1996. The standard length of stay in ICU and within a hospital was shortened, accordingly. These parameters were not comparable and were, therefore, not included in the analysis. The use of opioids was reduced from 2000 onwards. The measurement of pulmonary artery pressure was not a routine in the earliest era. For this reason, EuroSCORE II was not included as a parameter. Comparable improvements have also been made in regard to TAVI, with the expansion of this approach for lower risk groups. The recording of survival was obviously shorter in terms of the more recent era. The choice of the biologic device was at the discretion of the individual surgeon, hence there is no randomization in relation to the device. Furthermore, within the time span of 30 years, the surgical team underwent changes. Only the Perimount device was used throughout the study. The Perceval device was introduced later but remained in use until the end of the inclusion period. In spite of the low numbers for this device, the findings concerning the need for PPM implant and a favorable hemodynamic profile are relevant. A comparison of the Perceval device with the standard biologic prosthesis would require propensity score match analysis. With the low numbers in this study, this would not result in meaningful conclusions. However, logistic regression analysis is a good alternative for propensity score match analysis. This revealed that an age over 80, chronic renal and pulmonary disease, congestive heart failure, and need for urgent SAVR were independent predictors of 30-day mortality. The use of a Perceval device had no effect at all on mortality. One could safely assume that the use of a Perceval device with shorter operation times would neutralize the effect of an age over 80 years on the outcome. We also can conclude that the use of a Perceval device should be avoided in patients who had an earlier SAVR. The other devices were also lower in number, with limited long-term data because of their discontinuation. The major strength is the population size, the length of the follow-up, and the details on the need for resources.
Author Contributions
Conceptualization, W.M.; methodology, W.M. and I.D.; formal analysis, W.M. and I.D.; investigation, W.M., I.D., K.D. and A.V.; data curation, W.M., I.D., K.D. and A.V.; writing—original draft preparation, W.M.; writing—review and editing, W.M., I.D., K.D. and A.V.; visualization, supervision, project administration, funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the ZNA Ethical Committee under the number 2656 in 2001 and extended in 2011 and 2017.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study and rigorous anonymization by the ZNA Ethical Committee.
Data Availability Statement
These results have been derived from a multipurpose database, from which several more publications will be derived. These data are not yet publicly available.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Eveborn, G.W.; Schirmer, H.; Heggelund, G.; Lunde, P.; Rasmussen, K. The evolving epidemiology of valvular aortic stenosis. The Tromsø Study. Heart 2013, 99, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.Y.; Chow, V.; Brieger, D.; Yan, T.D.; Kritharides, L.; Ng, A.C. Outcomes of 16,436 patients requiring isolated aortic valve surgery: A statewide cohort study. Int. J. Cardiol. 2021, 326, 55–61. [Google Scholar] [CrossRef]
- Amanullah, M.R.; Pio, S.M.; Ng, A.C.; Sin, K.Y.; Marsan, N.A.; Ding, Z.P.; Leon, M.B.; Généreux, P.; Delgado, V.; Ewe, S.H.; et al. Prognostic Implications of Associated Cardiac Abnormalities Detected on Echocardiography in Patients With Moderate Aortic Stenosis. JACC Cardiovasc. Imaging 2021, 14, 1724–1737. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Pibarot, P.; Redfors, B.; Mack, M.J.; Makkar, R.R.; A Jaber, W.; Svensson, L.G.; Kapadia, S.; Tuzcu, E.M.; Thourani, V.H.; et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur. Heart J. 2017, 38, 3351–3358. [Google Scholar] [CrossRef]
- Strange, G.; Stewart, S.; Celermajer, D.; Prior, D.; Scalia, G.M.; Marwick, T.; Ilton, M.; Joseph, M.; Codde, J.; Playford, D.; et al. National Echocardiography Database of Australia contributing sites. Poor Long-Term Survival in Patients With Moderate Aortic Stenosis. J. Am. Coll. Cardiol. 2019, 74, 1851–1863. [Google Scholar] [CrossRef]
- Généreux, P.; Pibarot, P.; Redfors, B.; Bax, J.J.; Zhao, Y.; Makkar, R.R.; Kapadia, S.; Thourani, V.H.; Mack, M.J.; Nazif, T.M.; et al. Evolution and Prognostic Impact of Cardiac Damage After Aortic Valve Replacement. J. Am. Coll. Cardiol. 2022, 80, 783–800. [Google Scholar] [CrossRef] [PubMed]
- Mistiaen, W.; Van Cauwelaert, P.; Muylaert, P.; Wuyts, F.; Harrisson, F.; Bortier, H. Risk factors and survival after aortic valve replacement in octogenarians. J. Heart Valve Dis. 2004, 13, 538–544. [Google Scholar] [PubMed]
- Jiritano, F.; Serraino, G.F.; Sorrentino, S.; Napolitano, D.; Costa, D.; Ielapi, N.; Bracale, U.M.; Mastroroberto, P.; Andreucci, M.; Serra, R. Risk of Bleeding in Elderly Patients Undergoing Transcatheter Aortic Valve Implantation or Surgical Aortic Valve Replacement. Prosthesis 2024, 6, 175–185. [Google Scholar] [CrossRef]
- Mistiaen, W.; Deblier, I.; Dossche, K.; Vanermen, A. Clinical Outcomes after Surgical Aortic Valve Replacement in 681 Octogenarians: A Single-Center Real-World Experience Comparing the Old Patients with the Very Old Patients. Geriatrics 2024, 9, 44. [Google Scholar] [CrossRef]
- Mistiaen, W.P.; Van Cauwelaert, P.; Muylaert, P. One Thousand Carpentier-Edwards Pericardial Valves in the Aortic Position: What has Changed in the Past 20 years, and What are the Effects on Hospital Complications? J. Heart Valve Dis. 2007, 16, 417–420. [Google Scholar]
- Mylotte, D.; Osnabrugge, R.L.; Windecker, S.; Lefèvre, T.; de Jaegere, P.; Jeger, R.; Wenaweser, P.; Maisano, F.; Moat, N.; Søndergaard, L.; et al. Transcatheter Aortic Valve Replacement in Europe Adoption Trends and Factors Influencing Device Utilization. J. Am. Coll. Cardiol. 2013, 62, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Si, S.; Hillis, G.S.; Sanfilippo, F.M.; Smith, J.; Tran, L.; Reid, C.M.; Briffa, T. Surgical aortic valve replacement in Australia, 2002–2015: Temporal changes in clinical practice, patient profiles and outcomes. ANZ J. Surg. 2019, 89, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Neyt, M.; Van Brabandt, H.; Van De Sande, S.; Devriese, S. Transcatheter Aortakunstklep Implantatie (TAVI): Een Health Technology Assessment Actualisatie; Health Technology Assessment (HTA); KCE Reports 163A. D/2011/10.273/46; Federaal Kenniscentrum voor de Gezondheidszorg (KCE): Brussel, Belgium, 2011. [Google Scholar]
- Mistiaen, W.P.; Deblier, I.; Dossche, K.; Vanermen, A. Is it worthwhile to perform surgical aortic valve replacement in elderly patients with symptomatic aortic valve disease and malignancy: A short and long-term study in 2500 patients. Eur. Heart J. 2022, 43 (Suppl. S2), ehac544.1605. [Google Scholar] [CrossRef]
- Masraf, H.; Sef, D.; Chin, S.L.; Hunduma, G.; Trkulja, V.; Miskolczi, S.; Velissaris, T.; Luthra, S. Long-Term Survival among Octogenarians Undergoing Aortic Valve Replacement with or without Simultaneous Coronary Artery Bypass Grafting: A 22-Year Tertiary Single-Center Experience. J. Clin. Med. 2023, 12, 4841. [Google Scholar] [CrossRef] [PubMed]
- De Backer, O.; Luk, N.H.V.; Olsen, N.T.; Olsen, P.S.; Søndergaar, L. Choice of Treatment for Aortic Valve Stenosis in the Era of Transcatheter Aortic Valve Replacement in Eastern Denmark (2005 to 2015). JACC Cardiovasc. Interv. 2016, 9, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Brennan, J.M.; Holmes, D.R.; Sherwood, M.W.; Edwards, F.H.; Carroll, J.D.; Grover, F.L.; Tuzcu, E.M.; Thourani, V.; Brindis, R.G.; Shahian, D.M.; et al. The Association of Transcatheter Aortic Valve Replacement Availability and Hospital Aortic Valve Replacement Volume and Mortality in the United States. Ann. Thorac. Surg. 2014, 98, 2016–2022. [Google Scholar] [CrossRef] [PubMed]
- Culler, S.D.; Cohen, D.J.; Brown, P.P.; Kugelmass, A.D.; Reynolds, M.R.; Ambrose, K.; Schlosser, M.L.; Simon, A.W.; Katz, M.R. Trends in Aortic Valve Replacement Procedures Between 2009 and 2015: Has Transcatheter Aortic Valve Replacement Made a Difference? Ann. Thorac. Surg. 2018, 105, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.E.; McAlexander, W.W.; Sasse, M.F.; Leesar, M.A.; Melby, S.J.; Singh, S.P.; Jernigan, L.B.; Booker, O.J.; Alli, O.O. Impact of Transcatheter Aortic Valve Replacement on Surgical Volumes and Outcomes in a Tertiary Academic Cardiac Surgical Practice. J. Am. Coll. Surg. 2016, 222, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Dagenais, F.; Voisine, P.; Dumont, E.; Charbonneau, E.; Baillot, R.; Kalavrouziotis, D.; Mohammadi, S. Surgical aortic valve replacement outcomes in the transcatheter era. J. Thorac. Cardiovasc. Surg. 2015, 150, 1582–1588. [Google Scholar] [CrossRef]
- Mullan, C.W.; Mori, M.; Oichert, M.D.; Bin Mahmood, S.U.; Yousef, S.; Geirsson, A. United States national trends in comorbidity and outcomes of adult cardiac surgery patients. J. Cardiac Surg. 2020, 35, 2248–2253. [Google Scholar] [CrossRef]
- Sharma, T.; Krishnan, A.M.; Lahoud, R.; Polomsky, M.; Dauerman, H.L. National Trends in TAVR and SAVR for Patients With Severe Isolated Aortic Stenosis. J. Am. Coll. Cardiol. 2022, 80, 2054–2056. [Google Scholar] [CrossRef] [PubMed]
- Akintoye, E.; Ando, T.; Sandio, A.; Adegbala, O.; Salih, M.; Zubairu, J.; Oseni, A.; Sistla, P.; Alqasrawi, M.; Egbe, A.; et al. Aortic Valve Replacement for Severe Aortic Stenosis Before and During the Era of Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2020, 126, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; O’Brien, S.M.; Wu, C.; Sikora, J.A.H.; Griffith, B.P.; Gammie, J.S. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: Changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J. Thorac. Cardiovasc. Surg. 2009, 137, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Guimaron, S.; De Brux, J.; Verhoye, J.; Guihaire, J. Surgical aortic valve replacement in the modern era: Insights from the French Registry EPICARD. J. Card. Surg. 2021, 36, 4573–4581. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-García, R.; Perez-Farinos, N.; De Miguel-Díez, J.; Hernándezbarrera, V.; Méndez-Bailón, M.; Jimenez-Trujillo, I.; De Miguel-Yanes, J.M.; López-De-Andrés, A. National Trends in Utilization and In-Hospital Outcomes of Surgical Aortic Valve Replacements in Spain, 2001–2015. Braz. J. Cardiovasc. Surg. 2020, 35, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Siregar, S.; de Heer, F.; Groenwold, R.H.; Versteegh, M.I.; Bekkers, J.A.; Brinkman, E.S.; Bots, M.L.; van der Graaf, Y.; van Herwerden, L.A. Trends and outcomes of valve surgery: 16-year results of Netherlands Cardiac Surgery National Database. Eur. J. Cardiothorac. Surg. 2014, 46, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Tam, D.Y.; Rocha, R.V.; Wijeysundera, H.C.; Austin, P.C.; Dvir, D.; Fremes, S.E. Surgical valve selection in the era of transcatheter aortic valve replacement in the Society of Thoracic Surgeons Database. J. Thorac. Cardiovasc. Surg. 2019, 159, 416–427.e8. [Google Scholar] [CrossRef] [PubMed]
- Formica, F.; Mariani, S.; D’alessandro, S.; Singh, G.; Di Mauro, M.; Cerrito, M.G.; Messina, L.A.; Scianna, S.; Papesso, F.; Sangalli, F. Does additional coronary artery bypass grafting to aortic valve replacement in elderly patients affect the early and long-term outcome? Heart Vessels 2020, 35, 487–501. [Google Scholar] [CrossRef] [PubMed]
- Czarnecki, A.; Qiu, F.; Koh, M.; Alter, D.A.; Austin, P.C.; Fremes, S.E.; Tu, J.V.; Wijeysundera, H.C.; Yan, A.T.; Ko, D.T. Trends in the incidence and outcomes of patients with aortic stenosis hospitalization. Am. Heart J. 2019, 199, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Mistiaen, W. Referral of Patients for Surgical Aortic Valve Replacement before and after Introduction of the Transcatheter Aortic Valve Implantation-Changing Patterns of Preoperative Characteristics and Volume and Postoperative Outcome. J. Cardiovasc. Dev. Dis. 2023, 22, 223. [Google Scholar] [CrossRef]
- Kundi, H.; Strom, J.B.; Valsdottir, L.R.; Elmariah, S.; Popma, J.J.; Shen, C.; Yeh, R.W. Trends in Isolated Surgical Aortic Valve Replacement According to Hospital-Based Transcatheter Aortic Valve Replacement Volumes. JACC Cardiovasc. Interv. 2018, 11, 2148–2156. [Google Scholar] [CrossRef] [PubMed]
- Khounlaboud, M.; Donal, E.; Auffret, V.; Anselmi, A.; Ingels, A.; Flécher, E.; Verhoye, J.-P.; Daubert, C.; Le Breton, H.; Mabo, P.; et al. Comparison of Preoperative and Postoperative Characteristics in Octogenarians Having Isolated Surgical Aortic Valve Replacement Before Versus After Introduction of Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2015, 116, 933–937. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Bin Mahmood, S.U.; Geirsson, A.; Yun, J.J.; Cleman, M.W.; Forrest, J.K.; Mangi, A.A. Trends in volume and risk profiles of patients undergoing isolated surgical and transcatheter aortic valve replacement. Catheter. Cardiovasc. Interv. 2019, 93, E337–E342. [Google Scholar] [CrossRef] [PubMed]
- Gandjian, M.; Verma, A.; Tran, Z.; Sanaiha, Y.; Downey, P.; Shemin, R.J.; Benharash, P. Influence of center surgical aortic valve volume on outcomes of transcatheter aortic valve replacement. JTCVS Open 2022, 11, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.R.; Chew, D.P.; Horsfall, M.J.; Chuang, A.M.-Y.; Sinhal, A.R.; Joseph, M.X.; A Baker, R.; Bennetts, J.S.; Selvanayagam, J.B.; Lehman, S.J. Multidisciplinary transcatheter aortic valve replacement heart team programme improves mortality in aortic stenosis. Open Heart 2019, 6, e000983. [Google Scholar] [CrossRef] [PubMed]
- Gaede, L.; Blumenstein, J.; Kim, W.-K.; Liebetrau, C.; Dörr, O.; Nef, H.; Hamm, C.; Elsässer, A.; Möllmann, H. Trends in aortic valve replacement in Germany in 2015: Transcatheter versus isolated surgical aortic valve repair. Clin. Res. Cardiol. 2017, 106, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.; Willner, N.; Eltchaninoff, H.; Burwash, I.G.; Michel, M.; Durand, E.; Gilard, M.; Dindorf, C.; Iung, B.; Cribier, A.; et al. Trends in aortic valve replacement for aortic stenosis: A French nationwide study. Eur. Heart J. 2022, 43, 666–679. [Google Scholar] [CrossRef] [PubMed]
- Reinöhl, J.; Kaier, K.; Reinecke, H.; Schmoor, C.; Frankenstein, L.; Vach, W.; Cribier, A.; Beyersdorf, F.; Bode, C.; Zehender, M. Effect of Availability of Transcatheter Aortic-Valve Replacement on Clinical Practice. N. Engl. J. Med. 2015, 373, 2438–2447. [Google Scholar] [CrossRef]
- Attias, D.; Maillet, J.-M.; Copie, X.; Bonnet, N.; Mesnildrey, P.; Benvenuti, C.; Benacerraf, M.; Scheublé, A.; Digne, F.; Stratiev, V.; et al. Prevalence, clinical characteristics and outcomes of high-risk patients treated for severe aortic stenosis prior to and after transcatheter aortic valve implantation availability. Eur. J. Cardiothorac. Surg. 2015, 47, e212. [Google Scholar] [CrossRef][Green Version]
- Englum, B.R.; Ganapathi, A.M.; Schechter, M.A.; Harrison, J.K.; Glower, D.D.; Hughes, G.C. Changes in Risk Profile and Outcomes of Patients Undergoing Surgical Aortic Valve Replacement from the Pre- to Post-Transcatheter Aortic Valve Replacement Eras. Ann. Thorac. Surg. 2015, 101, 110–117. [Google Scholar] [CrossRef][Green Version]
- Heinze, G.; Christ, T.; Leonards, C.O.; Dohmen, P.M.; Konertz, W. Risk and Outcome of Aortic Valve Surgery in the Transcatheter Valve Era: The Gender Aspect. Ann. Thorac. Cardiovasc. Surg. 2015, 21, 446–451. [Google Scholar] [CrossRef][Green Version]
- Wang, T.K.M.; Sathanathan, J.; Ramanathan, T.; Webster, M.; Ruygrok, P. Isolated Aortic Valve Replacement in Octogenarians Before and After the Introduction of Trans-catheter Aortic Valve Implantation. Heart Lung Circ. 2014, 23, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Dimagli, A.; Sinha, S.; Caputo, M.; Angelini, G.D.; Benedetto, U. Trend in morbidity and mortality in surgical aortic valve replacement: A retrospective, observational, single-centre study. Interact. Cardiovasc. Thorac. Surg. 2020, 31, 796–802. [Google Scholar] [CrossRef]
- Chahine, J.; Jedeon, Z.; Fiocchi, J.; Shaffer, A.; Knoper, R.; John, R.; Yannopoulos, D.; Raveendran, G.; Gurevich, S. A retrospective study on the trends in surgical aortic valve replacement outcomes in the post-transcatheter aortic valve replacement era. Health Sci. Rep. 2022, 5, e660. [Google Scholar] [CrossRef]
- Nguyen, T.C.; Terwelp, M.D.; Thourani, V.H.; Zhao, Y.; Ganim, N.; Hoffmann, C.; Justo, M.; Estrera, A.L.; Smalling, R.W.; Balan, P.; et al. Clinical trends in surgical, minimally invasive and transcatheter aortic valve replacement†. Eur. J. Cardiothorac. Surg. 2017, 51, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Silashi, M.; Conrad, L.; Treede, H.; Reiter, B.; Schaefer, U.; Blankenberg, S.; Reichenspurner, H. Trends in Surgical Aortic Valve Replacement in More Than 3000 Consecutive Cases in the Era of Transcatheter Aortic Valve Implantations. Thorac. Cardiovasc. Surg. 2016, 64, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Malaisrie, S.C.; Tuday, E.; Lapin, B.; Wang, E.; Lee, R.; McGee, E.C.; Davidson, C.; McCarthy, P.M. Transcatheter aortic valve implantation decreases the rate of unoperated aortic stenosis. Eur. J. Cardiothorac. Surg. 2011, 40, 43–48. [Google Scholar] [CrossRef][Green Version]
- D’Onofrio, A.; Alfieri, O.R.; Cioni, M.; Alamanni, F.; Fusari, M.; Tarzia, V.; Rizzoli, G.; Gerosa, G. The impact of transcatheter aortic valve implantation on patients’ profiles and outcomes of aortic valve surgery programmes: A multi-institutional appraisal. Interact. Cardiovasc. Thorac. Surg. 2013, 16, 608–611. [Google Scholar] [CrossRef]
- Goel, S.S.; Ige, M.; Tuzcu, E.M.; Ellis, S.G.; Stewart, W.J.; Svensson, L.G.; Lytle, B.W.; Kapadia, S.R. Severe aortic stenosis and coronary artery disease–implications for management in the transcatheter aortic valve replacement era: A comprehensive review. J. Am. Coll. Cardiol. 2013, 62, 1–10. [Google Scholar] [CrossRef]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, J.; Iung, B.; Lancellotti, P.; Lansac, E.; Munoz, D.R.; et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Weserling, M.; Hamm, C.W.; Kim, W.K. Percutaneous Coronary Intervention in Transcatheter Aortic Valve Implantation Patients: Overview and Practical Management. Front. Cardiovasc. Med. 2021, 8, 653768. [Google Scholar] [CrossRef]
- Durko, A.P.; Osnabrugge, R.L.; Van Mieghem, N.M.; Milojevic, M.; Mylotte, D.; Nkomo, V.T.; Kappetein, A.P. Annual number of candidates for transcatheter aortic valve implantation per country: Current estimates and future projections. Eur. Heart J. 2018, 39, 2635–2642. [Google Scholar] [CrossRef]
- Maximus, S.; Milliken, J.C.; Danielsen, B.; Shemin, R.; Khan, J.; Carey, J.S. Implementation of transcatheter aortic valve replacement in California: Influence on aortic valve surgery. J. Thorac. Cardiovasc. Surg. 2018, 155, 1447–1456. [Google Scholar] [CrossRef]
- Thourani, V.H.; Suri, R.M.; Gunter, R.L.; Sheng, S.; O’brien, S.M.; Ailawadi, G.; Szeto, W.Y.; Dewey, T.M.; Guyton, R.A.; Bavaria, J.E.; et al. Contemporary Real-World Outcomes of Surgical Aortic Valve Replacement in 141,905 Low-Risk, Intermediate-Risk, and High-Risk Patients. Ann. Thorac. Surg. 2015, 99, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Lacquaniti, A.; Ceresa, F.; Campo, S.; Smeriglio, A.; Trombetta, D.; Patanè, F.; Monardo, P. Surgical Aortic Valve Replacement and Renal Dysfunction: From Acute Kidney Injury to Chronic Disease. J. Clin. Med. 2024, 13, 2933. [Google Scholar] [CrossRef]
- Berretta, P.; Meuris, B.; Kappert, U.; Andreas, M.; Fiore, A.; Solinas, M.; Misfeld, M.; Carrel, T.P.; Villa, E.; Savini, C.; et al. Sutureless Versus Rapid Deployment Aortic Valve Replacement: Results From a Multicenter Registry. Ann. Thorac. Surg. 2022, 114, 758–765. [Google Scholar] [CrossRef]
- Dokollari, A.; Ramlawi, B.; Torregrossa, G.; Sá, M.P.; Sicouri, S.; Prifti, E.; Gelsomino, S.; Bonacchi, M. Benefits and Pitfalls of the Perceval Sutureless Bioprosthesis. Front. Cardiovasc. Med. 2022, 8, 789392. [Google Scholar] [CrossRef] [PubMed]
- Kapadia, S.J.; Salmasi, M.Y.; Zientara, A.; Roussin, I.; Quarto, C.; Asimakopoulos, G. Perceval sutureless bioprosthesis versus Perimount sutured bioprosthesis for aortic valve replacement in patients with aortic stenosis: A retrospective, propensity-matched study. J. Cardiothorac. Surg. 2024, 19, 95. [Google Scholar] [CrossRef]
- Pelce, E.; Porto, A.; Gariboldi, V.; Ben Lagha, A.; Amanatiou, C.; Collart, F.; Theron, A. Five-year outcomes of rapid-deployment aortic valve replacement with the Edwards Intuity valve. J. Card Surg. 2021, 36, 2826–2833. [Google Scholar] [CrossRef] [PubMed]
- Klop, I.D.G.; Kougioumtzoglou, A.M.; Kloppenburg, G.T.L.; van Putte, B.P.; Sprangers, M.A.G.; Klein, P.; Nieuwkerk, P.T. Short-term outcome of the intuity rapid deployment prosthesis: A systematic review and meta-analysis. Interact Cardiovasc. Thorac. Surg. 2020, 31, 427–436. [Google Scholar] [CrossRef]
- Bavaria, J.E.; Griffith, B.; Heimansohn, D.A.; Rozanski, J.; Johnston, D.R.; Bartus, K.; Girardi, L.N.; Beaver, T.; Takayama, H.; Mumtaz, M.A.; et al. COMMENCE Trial Investigators. Five-year Outcomes of the COMMENCE Trial Investigating Aortic Valve Replacement With RESILIA Tissue. Ann. Thorac. Surg. 2023, 115, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Sef, D.; Thet, M.S.; Klokocovnik, T.; Luthra, S. Early and mid-term outcomes after aortic valve replacement using a novel tissue bioprosthesis: A systematic review. Eur. J. Cardiothorac. Surg. 2024, 65, ezae045. [Google Scholar] [CrossRef] [PubMed]
- Lansac, E.; Youssefi, P.; de Heer, F.; Bavaria, J.; De Kerchove, L.; El-Hamamsy, I.; Elkhoury, G.; Enriquez-Sarano, M.; Jondeau, L.d.G.; Kluin, J.; et al. Aortic Valve Repair Research Network Investigators from the Heart Valve Society, Collaborators. Aortic Valve Surgery in Nonelderly Patients: Insights Gained From AVIATOR. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Persson, M.; Glaser, N.; Nilsson, J.; Friberg, Ö.; Franco-Cereceda, A.; Sartipy, U. Comparison of Long-term Performance of Bioprosthetic Aortic Valves in Sweden From 2003 to 2018. JAMA Netw. Open 2022, 5, e220962. [Google Scholar] [CrossRef] [PubMed]
- Sansone, F.; Dato, G.M.A.; Zingarelli, E.; Ferrero, E.; Prot, S.; Ceresa, F.; Patanè, F.; Casabona, R. Long-term follow-up of stentless prosthesis. J. Cardiol. 2014, 63, 365–372. [Google Scholar] [CrossRef]
- Porterie, J.; Kalavrouziotis, D.; Dumont, E.; Paradis, J.M.; De Larochellière, R.; Rodés-Cabau, J.; Mohammadi, S. Clinical impact of the heart team on the outcomes of surgical aortic valve replacement among octogenarians. J. Thorac. Cardiovasc. Surg. 2023, 165, 1010–1019.e5. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).