Abstract
The prevalence of individuals with flat feet and high arches is very high (between 15% to 37%), which can often lead to other orthopedic complications. Three-dimensional-printed insoles are being studied and validated for their effects in correcting these highly prevalent foot disorders. Highly customizable parameters while printing the insole allows for precise correction of foot biomechanics. In this study, 200 patients suffering from various foot-related problems and joint pain were given 3d-printed insoles (designed using plantar pressure systems and clinical practitioner’s assessment) to use in their footwear. Tested activities included standing, walking, running, sports, and gym workout. Customization of insoles included custom density, heel cup, heel rise, medial arch height, and lateral wedge. Based on the patient history, additional podiatry elements were provided for patients with diabetes. Each insole was designed as per the insole profile of the shoe with a comfortable fit. These insoles were found to be effective in alleviating pain for more than 90% of the patients and provided a longer life cycle with effective orthotic correction (for >16 months of daily use). This paper presents the post-use effects (6–18 months) of custom 3D-printed insoles.
1. Introduction
Flat foot and high arch problems are very common and have a high prevalence rate. These foot disorders are mainly congenital or hereditary in nature, with other causes being injuries (acquired or acute), rheumatoid arthritis, diabetes, or Achilles tendon injury. These fallen arches often tend to affect the bones and joints of the foot and ankle complex, resulting in pain and discomfort. While for athletes, Achilles tendinopathy and plantar fasciitis were amongst the most common injuries suffered [1]. With growing age, this pain can be observed at the ankle joint, midfoot, knee joint, hip joint as well as lower back of the patient. Increased foot pronation/supination, overweight, intrinsic muscle weakness, and improper footwear alter foot biomechanics. These risk factors cause repetitive tensile stresses on the fascia resulting in microtrauma at its origin, pain, and functional disability [2]. This associated pain has a detrimental impact on health and limits the ability to participate in physical activity and affects productivity. While congenital flat feet or high arches cannot be cured completely, orthoses have been found useful to “correct” foot biomechanics and delay the above-mentioned problems that can arise over time. For patients with diabetic/neuropathic feet, podiatry elements of the insoles, such as a metatarsal bar, metatarsal pad, and weight off-loader rings are useful in the prevention as well as curing of foot ulceration [3]. Orthotic insoles have been prescribed over the years and were made up of cork, leather, rubber, and various types and densities of foam material but have the shortcomings of high labor and time costs. Moreover, customization via digital technology can rarely be achieved in the conventional way of orthosis design. Advanced rapid prototyping technology allows precise and effective solutions, such as 3d-printed insoles. Fused Deposition Modeling (FDM) technology was found useful in designing full contact and orthopedic insoles that provide custom density, allowing excellent shock absorption for the prevention of injury. Foot orthoses with shock absorption were found to provide a 28% reduction in the risk of developing an overall injury and a 41% reduction in the risk of developing a lower limb stress fracture [1]. For designing a custom insole, various parameters need to be taken into account, of which plantar pressure data (for flat foot/high arch as well as patients with diabetic foot) is the most crucial. This data provides static as well as dynamic reports that need to be considered while designing a customized insole. Plantar pressure relief is sensitive to orthotic design decisions that can be achieved in 3d-printed insoles by selecting different densities referring to plantar pressure mapping [3]. Materials such as Polyurethane (including PORON®), polyethylene (including Plastazote®), and Ethylene Vinyl Acetate (EVA) reduce peak pressure beneath varying regions of the foot. Materials were found to influence plantar pressures affecting force and contact area (dependent on the hardness, density, thickness, and ability to contour to the foot) [4]. Three-dimensional-printed insoles designed for this study used variable density in the base insole (Thermoplastic Polyurethane (TPU) material) and top layers of PORON and EVA to combine its effects. Anatomical 3D-printed insoles can be total contact, podiatric, or orthopedic in nature. Being in direct contact with the foot, it supports the body weight, thereby correcting the biomechanical force distribution. Figure 1 shows a plantar pressure scan of one of the subjects involved in this study. It can be seen that the weight distribution in the static position is slightly unbalanced: 48% on the left foot and 52% on the right. On the left foot, the weight distribution is concentrated in the heel, the metatarsal, and, to a lesser extent, the toe. Any weight-bearing excessive physical activity of such individuals can cause extreme discomfort and pain over time. Incorrect support may lead to injuries in the long term, also resulting in osteoarthritis [5].
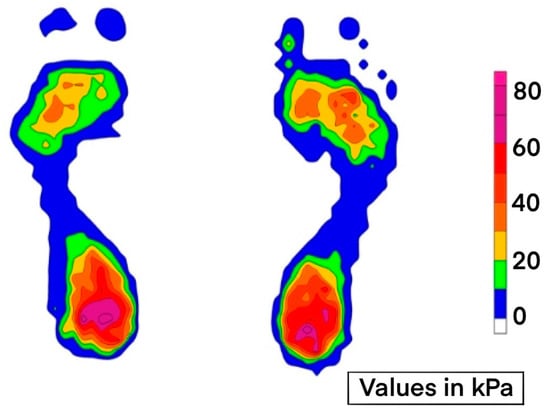
Figure 1.
Plantar pressure scan. Values indicating ground reactive forces in static test. These values can be acquired for various gait events in static as well as dynamic conditions. They help in understanding the altered biomechanics of foot due to foot disorders.
Porous (or mesh) structures were used in the design of the insole as the effective Young’s modulus of TPU alone is beyond the demand of alleviating plantar pressure [6]. Porous structures in the insole can be designed using CAD modeling, or advanced slicing features can be used to add areas of different densities and rigidity for shock absorption and support. This helps reduce the effective modulus, which is necessary for diabetic insoles. For the case in Figure 1, an elevation in the heel area (termed “heel rise”) will improve its midfoot contact area, thereby reducing fatigue and pain in static conditions. In dynamic conditions of the above case, better stability is achieved with heel rise provided in the insole [7]. The pattern and infill percentage affect the tensile strength, hardness, and flexure of the insole [8]. This needs to be customized for every individual by referring to their plantar pressure scans. The shore hardness value of the TPU decides the value of the infill percentage. This ultimately affects the printing time and cost of the insole. The time and cost are not only associated with the design and 3D printing but are also affected by the availability of the plantar pressure systems for data acquisition. The lack of portability of these systems restricts the tests to laboratory or clinical environments [9]. The acquisition is also affected by the “foot targeting effect”, where the users alter their natural gait pattern in order to correctly place the foot on the platform. For designing 3D-printed insoles without any plantar pressure scan, total contact insoles are prescribed. These are developed by acquiring a 3D scan of the foot in a non-weight-bearing condition. This is digitally “corrected” using mesh tools in CAD, and a total contact insole is designed. This method is preferred mainly in patients with diabetes [10,11]. Additional podiatric elements such as metatarsal bars/pads or off-loaders can be added depending on each respective case.
This study involved designing custom 3d-printed insoles for 200 subjects (flat foot/high arch/diabetic foot and those suffering from joint pain). Using a 3D-printed insole was found to improve comfort score and foot function in individuals [12,13]. The above research findings were taken into consideration while designing these insoles for the subject. The orthoses developed included all three types: orthopedic insole (neutral correction and high arch), podiatric insoles, and total contact insoles.
2. Materials and Methods
For this study, scanning (2D and 3D), modeling, and FDM 3D-printing techniques were used. For data acquisition, 2D pressure plantar system (with 3000 and 5000 sensors) and a 3D scanner (Occipital Structure Sensor) were used. This study is based on the previous (undocumented) part of research work on the interdisciplinary design aspects of custom 3d-printed insoles using plantar pressure mapping. It consisted of 10 patients (a mix of flat foot/diabetic foot ulcer and joint pain) as subjects. After a 6-month follow-up and various trials and validation, the same study was scaled up to include a larger number of subjects to understand the commercial viability and potential of FDM as a low-cost solution in foot orthoses. This study was carried out at a leading orthopedic and rehabilitation hospital in Pune, India.
2.1. Participant Requirement
As a succession to the unpublished research work mentioned above, this study was targeted toward users with foot-related disorders, users who experienced pain in ankle, knee, hip, and lower back joints, and patients with diabetic foot conditions. This research study required 2D plantar pressure scans with patient history and, in some cases (diabetic foot/ulcers/corns, etc.), 3D scanning. Users were briefed about the research aspect and were informed about the follow-up procedure that was needed for further documentation and analysis.
2.2. Insole Design and Development
The most important part of customized 3d-printed insole design is the acquisition of the data for reference design (Figure 2). This data can be qualitative as well as quantitative.
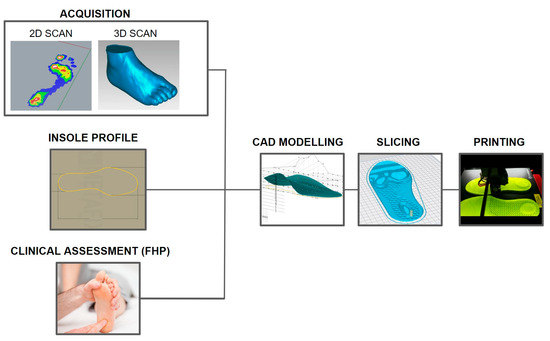
Figure 2.
Manufacturing workflow for designing customized 3d-printed insoles.
2.2.1. Foot Scan and Acquisition
Plantar pressure measurements were recorded for each patient for static and dynamic analysis. Stabilometry test data was also recorded as a part of static foot pressure analysis. This data forms the quantitative feedback for insole design. Plantar pressure measurement was taken for all 200 users. Foot health practitioners provided clinical assessment data. Figure 3 shows the 2D scan for patients. For patients with diabetic foot ulcers, additional 3D scan was required and is must for developing total contact insoles. (A total contact insole is a Boolean subtraction of the 3D foot scan and arch support insole).
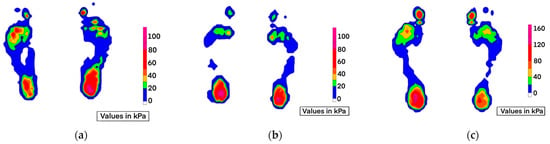
Figure 3.
Static scan <age–gender–diagnosis–Body Mass Index> (a) 38Y–F–Overpronation–Arthritis (BMI 20); (b) 14Y–F–Overpronation–Knee
Hyperextension–Flexible Flat Foot (BMI 28); (c) 28Y–M–Acquired Flat Foot–Badminton Player (BMI 21).
Apart from the static data, the dynamic data also provide important information about the gait parameters, as shown in
Figure 4. Dynamic data is required when designing insoles for sports people or athletes who often come across high ground reactive forces (GRF).
Figure 5 shows the gait response while walking. Abnormality can be clearly seen in weight-loading forces.
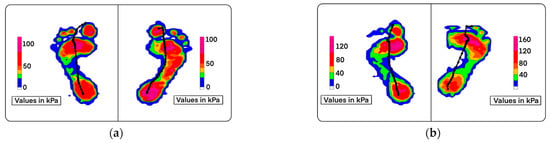
Figure 4.
Dynamic scan <age–gender–diagnosis–Body Mass Index> (a) 44Y–M–Rigid Flat Foot (BMI 27); (b) 35Y–M–Overpronation (BMI 25).
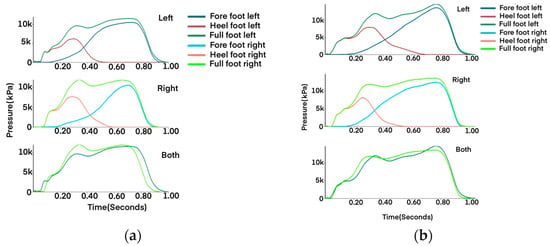
Figure 5.
Weight-loading curve for dynamic scan in Figure 4. (a) 44Y–M–Rigid Flat Foot (BMI 27); (b) 35Y–M–Overpronation (BMI 25). In both cases, lower load values at heel contact are seen as a natural response of the body to overcome heel pain (resulting from static conditions).
2.2.2. Insole Design
For designing a custom 3d-printed insole, five key parameters are taken into consideration: heel cup, medial arch height, lateral wedge height, density, and heel raise. These parameters can be applied when designing orthopedic and podiatric insoles. Total contact insole does not require this level of customization at this stage (CAD design) but is modified during the “slicing” phase of file conversion. CAD software (SolidWorks 2020, Dassault Systemes, Vélizy-Villacoublay, France), was used for designing.
For custom fit, shoe insole is required to make the base profile. For patients with over-pronation, “neutral” correction insoles are recommended. Based on the previous study, it was found that over-pronated patients experience pain in static conditions such as standing when natural correction is provided. (Neutral correction is the term that we have used that reflects 75–80% of the natural correction height for medial arch support.) Figure 6 shows the CAD design parameters of foot contour profile for neutral correction at medial arch but elevated lateral wedge support.
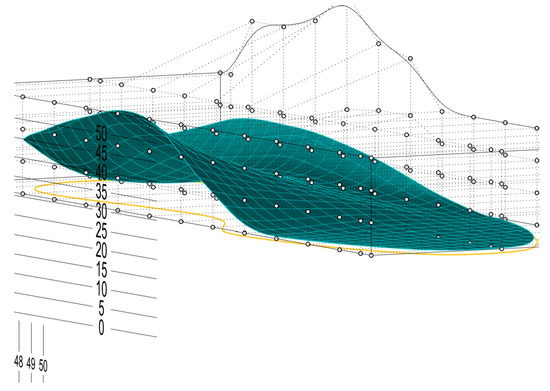
Figure 6.
CAD
modeling: Parametric modeling is used to define the insole form. Focus is on the design of mid-foot and hind-foot anatomical structure support. Bounding box pattern allows for contour adjustment of the profile (the numbers represent the scale in millimeters used as a reference for design and modification).
2.2.3. Slicing
This is the last stage in the manufacturing flow. Slicing is a process where a graphical layer-by-layer code format is generated for the CAD design. This software slices the object model into multiple layers that can be 3D printed. Slicing parameters provide the flexibility of adjusting the “Density” of the insole, which can be mono-pattern or have multi-patterns in the final print. The density does not depend alone on the slicer settings but also on various other factors (nature of the foot problem, Body Mass Index (BMI), type of filament, and type of the insole). This directly affects the printing time and cost of the insole. TPU material is very difficult to print; hence, the topology of the printer plays an important role in achieving successful printing.
Figure 7
shows the “parameters” that are important in customization.
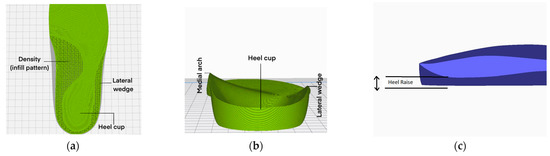
Figure 7.
(a) Insole slicing profile showing the infill pattern; (b) the podiatric parameters in insole design (back view); (c) heel raise (X-Ray side view of the hind part).
For orthopedic insoles, it is of utmost importance to maintain the smooth contour shape of the insole. This reduces any discomfort that may otherwise result while wearing an orthosis.
Figure 8
shows the contour analysis (zebra lines) that shows the smooth transition of the podiatric elements.

Figure 8.
Contour profile for orthopedic insoles. In neutral correction insoles, metatarsal bars/pads are not provided.
2.2.4. Three-Dimensional Printing and Post-Processing
Every user was given a customized 3D-printed insole for trial and validation. The diagnosis and data acquisition were carried out as explained in the above sections. Six 3D printers, FDM (JGMaker, Ultimaker, and Raise3D printers), Cartesian, and Core-XY topology, were used for printing 200 insoles. In Core-XY system, the belt moves the print head along X and Y coordinates, reducing the moving mass while printing the object, whereas in Cartesian, the print bed moves, making it less stable mechanism. As TPU material is difficult to print, direct extrusion printers can be considered for printing. Two types of TPU material were used for printing the insoles of 90A and 95A shore hardness. The prints from the TPU filament diameter of 1.75 and 2.85 were similar and showed no or little difference. There was more post-processing for the Cartesian style printers compared to finer finished Core-XY print. Post-processing involved grinding, buffing, and pasting of padding sheets as a top layer of the insole. The padding sheet used was of EVA sheet (1 mm and 2 mm thick) and PORON sheet (2 mm thick). These materials combined with the correct slicing parameters showed excellent durability and satisfactory improvement rate of over 95% of the validated trials [14]. In few users, as a special request, suede leather was used as a padding material. Every insole was post-processed and fitted in shoes of the users by certified prosthetist and orthotist.
2.3. Tools and Procedure
For the analysis of the conditions post use of these 3d-printed insoles, the standard American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot score was used. This scale includes 9 items that are further divided into 3 sub-scales of pain, function, and alignment. Having patient-reported and physician-reported parts, it is assessed on the final score for the user, ranging from 0 to 100. Lower score indicates severe pain and impairment, while a high score indicates no pain symptoms or impairment. The pain subscale consists of maximum of 40 points, indicating no pain. Functionality is assessed over seven items, with a maximum score of 50 points. Alignment subscale has a maximum score of 10 points.
3. Results
This study was carried out on 200 subjects with varying foot-related problems, and customized 3d-printed insoles were fitted into their daily use footwear (this study is restricted to the use of 3d-printed insoles fitted in the “shoe” and not sandals, as the shoe provides ankle and navicular stability that is required for patients with the overpronated flat foot condition). The designed insoles and fitment for this study are shown in Figure 9.
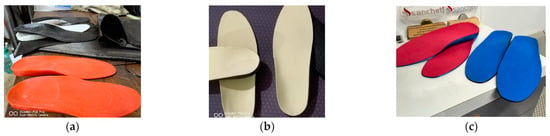
Figure 9.
Customized insoles: (a) raw 3d-printed insoles; (b) EVA foam-padded insoles; (c) PORON foam-padded insoles.
The following section describes the insole fitting and results post usage for the subjects. The data covers the feedback score for custom 3D-printed insoles after a minimum of 6 months of daily usage. Telephone follow-up was conducted every month for the first six months. As a continuation of this research study, a follow-up clinical examination after every four months was carried out. These subjects were evaluated based on the AOFAS Ankle-Hindfoot scale. A descriptive statistical analysis is made on the findings of this research study.
3.1. Flat Foot, High Arch
Out of the 200 users, 166 were diagnosed with a flat foot condition (overpronation, flexible flatfoot, rigid flatfoot, or hallux valgus), and 16 were diagnosed with a high arch. This included users from the age group of 12 years to 77 years. Many complained about some or another sort of joint pain, and some were advised by doctors for orthoses. Qualitative and quantitative analysis diagnosed them with flat foot and high arch problems. The navicular drop was the most common problem seen in patients with hyperlaxity. Hallux valgus was persistent in more than 90% of patients with overpronation. The lateral wedge in the insole was found to be the most efficient and comfortable as it provided stability and correction for navicular drop [15,16]. High-ankle shoes with 3D-printed insoles were prescribed to these patients. Shoes with wider toe boxes and rigid medial and lateral supports were prescribed. Cloth material/cotton slip-ons were strictly not recommended for any of the patients.
3.2. Diabetic/Neuropathic Foot
Diabetic-specific 3d-printed insoles were fitted to 18 users. This included patients from the 38–69 years age group. A study based on the Finite Element (FE) approach used soft plugs in areas with high plantar pressure (in patients with diabetes) and tested it for various Young’s moduli [17]. Slicing options in 3D printing allow variable density printing, thereby avoiding the need to use any extra material for diabetic insole fabrication. Elements for corn pressure relief, metatarsal bar, and pads were included in the insole design. The top layer of the PORON sheet helps reduce peak pressure points. This padding increases the durability of the insoles and can be replaced if needed. Abandonment was found in two patients, and both had three ulcers and lived with obesity.
3.3. Patients with Joint Pain
Altered biomechanics of the foot and ankle complex can lead to joint pain (ankle, midfoot, knee, hip, and lower back pain). Of the 200 subjects in this study, 126 patients had visited the doctor to address the joint pain they suffered, totally unaware of their foot condition. This shows unawareness about foot and ankle problems, as joint pains are often seen and treated as orthopedic problems, totally ignoring the foot diagnosis. The effects of 3D-printed insoles on this set of users who already faced joint pain are presented separately in the results section.
Table 1
shows the AOFAS score of the patients. The scores assessment showed that more than 90% of the patients experienced pain, discomfort, and limited functionality.

Table 1.
AOFAS Ankle-Hindfoot score before use of insole.
Overall, 22 subjects showed poor scores, a maximum from rigid flat foot and overpronated foot problems. The clinical examination followed up post six months showed much-improved scores on the AOFAS scale.
Table 2
shows the scores after a minimum of 6 months of usage.

Table 2.
AOFAS Ankle-Hindfoot score after use of insole for minimum of six months.
A substantial improvement in the scores was observed after using the customized 3D-printed insoles. For a flexible flat foot, the height of the medial arch was kept at 100% of the expected correction. The medial arch infill was selected at the lowest possible acceptable rigidity value. A total of 93% of the AOFAS scores for this group were found to be excellent and good, compared to 65% before the use of the insoles. In the case of rigid and overpronated cases, 75% of the expected correction height was provided for the medial arch, with semi-rigid support. This approach helped improve the AOFAS “Excellent” score from 14% to 65%.
For patients suffering from joint pain due to foot problems, insoles were designed specifically for their physical activities.
Table 3
shows AOFAS scores for subjects with persistent pain. Many complained about their restricted ability to participate in activities (few subjects involved in high GRF sports).

Table 3.
AOFAS Ankle-Hindfoot score before use of insole, for subjects with persistent pain.
Table 4 shows the scores after the use of insoles. While the scores improved, activities that involved jumps and high values of GRF witnessed instability while using the insoles.

Table 4.
AOFAS Ankle-Hindfoot score after use of insole for minimum of six months, for subjects with persistent pain.
Around 96% of the subjects reported relief from joint pain post use of insoles. Overall improvement of 93% was observed with patients using the insole for more than 5 h (average weight-bearing time), while 5% (suffering from ankle, knee, and lower back pain) reported a slight improvement in their conditions. Hallux valgus cases showed substantial improvement post 2 months of usage of the insoles and prescribed footwear. Among the 200 subjects, 17 subjects wanted softer insoles, while many expressed their desire to have an insole that can fit multiple shoes. There were two cases of abandonment of insoles observed, both amongst patients with diabetic foot ulcers. Four insoles were replaced in the first month’s post fitting due to design-level errors. Three-dimensional-printed insoles customized and developed following the above procedure (plantar pressure assessment, different levels of customization and design, and use of TPU and PORON) have been found to be effective, durable as well as affordable. After the follow-up clinical examination (6 months), the curative effects of customized 3d-printed insoles are found to be satisfactory with promising results and should soon surpass the traditional insole manufacturing process.
4. Discussion
In this research study, customized insoles were designed, developed, tested, and validated to treat foot-related musculoskeletal ailments in patients, as well as patients with diabetic foot problems. A detailed process from assessment, data acquisition, CAD design, slicing, and printing was optimized to develop these insoles. The reason for post-processing techniques was to enhance durability, flexibility, and comfort for the end user. The methodology explains the FDM technique for 3D printing, but the customized insoles can be manufactured via various 3D printing techniques. FDM is effective for the insoles to be used in daily routine life. They are found to be effective in alleviating pain arising from static weight-bearing activity as well as walking. The SLS method is preferred for high GRF activities where the design of the insole is of “extrusion” type. The extrusion type of insole is primarily a 2–3 mm thick foot profile contour (similar to Figure 6 with added thickness). This mechanical form helps provide support to the arch as well as store and release energy during the gait cycle. The static, as well as dynamic, assessment can help in further customizing the 3D-printed insole for activity-specific use. High variations in foot pressure distribution were observed in the users, with higher plantar pressure in patients with diabetes compared to healthy, non-diabetic patients with foot problems. This signifies the prevalence of foot ulcer problems in patients with diabetes. A research study based on an in-shoe pressure measurement device reported a similar finding [18]. These devices can be used to assess the forces acting at the interface of the plantar fascia and the 3D-printed insole and understand the cause of corns and ulcers in diabetic patients. Custom 3d-printed insoles can, thus, be prescribed to treat a variety of foot problems that may lead to musculoskeletal ailments in healthy public as well as in patients with diabetic foot.
4.1. Limitations
While extrusion-type insoles can universally fit in footwear, the TPU-based solid insole has its limitations. It is a universal problem as various shoe manufacturers have different shoe sole profiles. Any dimensional tolerance of more than 3 mm inside the shoe will make it uncomfortable for the user. It is important to note that none of the footwear prescribed or fitted with insole during this study had a ready arch support or a very narrow midfoot insole profile. The reason behind not prescribing narrow midfoot sports shoes is that the insoles are not able to provide the required vertical support, as narrower midfoot means the arch structure becomes unstable and ultimately collapses on the sidewalls of the shoe.
4.2. Conclusions
The custom 3D-printed insoles designed and prescribed to the users provided biomechanical correction and were found to be useful in alleviating pain caused by foot problems. The durability of 3D-printed insoles can be exceptionally good with certain precautionary measures taken by the users. TPU insoles must not be exposed to water, as it will affect their elasticity performance; moreover, the internal infill structures will not work as expected. Few of the subjects from the above study tend to use these insoles (21 months since the beginning of the study in June 2021), and no visible deformation is seen (except in two cases where the shoes got wet; TPU can attract moisture resulting in temporary deformation of the shape). For subjects with higher BMI, it is advised to replace the insoles after 18 months of regular use. The scope of this paper was limited to FDM printed insoles, but a similar flow can be used to design insoles using SLA, PolyJET, and SLS technology.
Author Contributions
Conceptualization, Validation, Design, Printing: S.S.; Analysis, Investigation, Assessments, and Comparative Analysis: S.S. and B.J.; Writing, Review, Editing, Supervision: S.S. and A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Research Review Committee (Ethical Clearance (Non-Invasive-Survey based trials)) by Vikalp Rehabilitation Center (Application: APR_0221/5 April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the validation.
Data Availability Statement
Data for the conducted trials can be obtained via email at 3drs@metafix.io. The data is made available upon request and only for research and academic use.
Acknowledgments
This study was largely supported by Rahul Saroj and Sushant Raut, experienced prosthetists and orthotists whose help made the trials be conducted in the given time. Shalini Balgude and Hrishikesh Garud, biomedical engineers with a specialization in Biomechanics, provided design and printing support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bonanno, D.; Landorf, K.B.; Munteanu, S.; Murley, G.S.; Menz, H. Effectiveness of foot orthoses and shock-absorbing insoles for the prevention of injury: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, S.; Sumer, E.; Zengin, H.Y.; Bek, N. Intensive physiotherapy versus home-based exercise and custom-made orthotic insoles in patients with plantar fasciitis: Pilot study. Foot 2022, 51, 101906. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Santos, A.; Preece, S.; Nester, C.J. Evaluation of orthotic insoles for people with diabetes who are at-risk of first ulceration. J. Foot Ankle Res. 2019, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Gerrard, J.M.; Bonanno, D.R.; Whittaker, G.A.; Landorf, K.B. Effect of different orthotic materials on plantar pressures: A systematic review. J. Foot Ankle Res. 2020, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Davia-Aracil, M.; Hinojo-Pérez, J.J.; Jimeno-Morenilla, A.; Mora-Mora, H. 3D printing of functional anatomical insoles. Comput. Ind. 2018, 95, 38–53. [Google Scholar] [CrossRef]
- Ma, Z.; Lin, J.; Xu, X.; Ma, Z.; Tang, L.; Sun, C.; Li, D.; Liu, C.; Zhong, Y.; Wang, L. Design and 3D printing of adjustable modulus porous structures for customized diabetic foot insoles. Int. J. Lightweight Mater. Manuf. 2019, 2, 57–63. [Google Scholar] [CrossRef]
- Jin, H.; Xu, R.; Wang, S.; Wang, J. Use of 3D-Printed Heel Support Insoles Based on Arch Lift Improves Foot Pressure Distribution in Healthy People. Experiment 2019, 25, 7175–7181. [Google Scholar] [CrossRef] [PubMed]
- Yarwindran, M.; Sa’aban, N.A.; Ibrahim, M.; Periyasamy, R. Thermoplastic elastomer infill pattern impact on mechanical properties 3D printed customized orthotic insole. ARPN J. Eng. Appl. Sci. 2016, 11, 6519–6524. [Google Scholar]
- Leal-Junior, A.G.; Díaz, C.R.; Marques, C.; Pontes, M.J.; Frizera, A. 3D-printed POF insole: Development and applications of a low-cost, highly customizable device for plantar pressure and ground reaction forces monitoring. Opt. Laser Technol. 2019, 116, 256–264. [Google Scholar] [CrossRef]
- Zuñiga, J.; Moscoso, M.; Padilla-Huamantinco, P.G.; Lazo-Porras, M.; Tenorio-Mucha, J.; Padilla-Huamantinco, W.; Tincopa, J.P. Development of 3D-Printed Orthopedic Insoles for Patients with Diabetes and Evaluation with Electronic Pressure Sensors. Designs 2022, 6, 95. [Google Scholar] [CrossRef]
- Singh, S.; Mali, H.S. 3D printed orthotic insoles for foot rehabilitation. In 3D Printing in Podiatric Medicine, 1st ed.; Sandhu, K., Singh, S., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 211–219. [Google Scholar] [CrossRef]
- Daryabor, A.; Kobayashi, T.; Saeedi, H.; Lyons, S.M.; Maeda, N.; Naimi, S.S. Effect of 3D printed insoles for people with flatfeet: A systematic review. Assist. Technol. 2022, 35, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Xu, R.; Wang, J. The Effects of Short-Term Wearing of Customized 3D Printed Single-Sided Lateral Wedge Insoles on Lower Limbs in Healthy Males: A Randomized Controlled Trial. Experiment 2019, 25, 7720–7727. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jiang, W.; Gan, Y.; Yu, Y.; Dai, K. Clinical Observation of 3D Printing Technology in Insoles for Flexible Flatfoot Patients. J. Shanghai Jiaotong Univ. Sci. 2021, 26, 398–403. [Google Scholar] [CrossRef]
- Jandova, S.; Mendricky, R. Benefits of 3D Printed and Customized Anatomical Footwear Insoles for Plantar Pressure Distribution. 3D Print. Addit. Manuf. 2022, 9, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Wang, C.S.; Lin, K.W.; Chien, M.J.; Wei, S.H.; Chen, C.S. Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities. Bioengineering 2022, 9, 563. [Google Scholar] [CrossRef] [PubMed]
- Geiger, F.; Kebbach, M.; Vogel, D.; Weissmann, V.; Bader, R. Efficient Computer-Based Method for Adjusting the Stiffness of Subject-Specific 3D-Printed Insoles during Walking. Appl. Sci. 2023, 13, 3854. [Google Scholar] [CrossRef]
- Gupta, S.; Jayaraman, R.; Sidhu, S.S.; Malviya, A.; Chatterjee, S.; Chhikara, K.; Singh, G.; Chanda, A. Diabot: Development of a Diabetic Foot Pressure Tracking Device. J 2023, 6, 32–47. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).