Abstract
This systematic review’s primary aim is to examine the interventional studies on the mental health of nurses during the COVID-19 pandemic, and the secondary aim is to determine the interventions that can be planned for future pandemics. For this, databases were searched, and a total of 12 studies meeting the inclusion criteria were included. It was determined that most of the studies were conducted online due to pandemic restrictions. The effects of the interventions (diaphragmatic breathing relaxation, emotional freedom techniques, sending motivational messages, a mobile wellness program, acceptance and commitment therapy, a neuro-meditation program, laughter yoga, gong meditation, distant Reiki, e-aid cognitive behavioral therapy, mindfulness-based breathing, and music therapy) on the parameters affecting the mental health of the nurses working actively in the COVID-19 pandemic were examined. In these studies, the interventions applied to nurses were seen to have positive results on mental health and well-being. The COVID-19 pandemic, which is a traumatic experience for healthcare professionals, shows that more interventional studies are needed to protect and improve the mental health of nurses who take care of critically ill patients during difficult times.
1. Introduction
In 2019, the COVID-19 pandemic emerged as a significant worldwide health issue, bringing with it some urgent concerns. Hospitalizations, the requirement for life support systems, and COVID-19 disease mortality rates were all high globally [1]. It also meant an increased amount of work required by healthcare workers. Nurses who continued to provide care over extended shifts while using inadequate protective equipment were negatively impacted during this time due to the uncertainties brought on by the pandemic [2,3,4]. Studies show that nurses had high levels of stress, anxiety, depression, burnout, and PTSD symptoms early in the COVID-19 pandemic [5,6,7,8,9]. In the later stages of the pandemic, on the other hand, they experienced mental health symptoms. A study conducted in Italy showed that nurses diagnosed with sleep disorders suffered from reduced self-efficacy during the later stages of the COVID-19 pandemic [10]. The findings demonstrate that the pandemic has detrimental impacts on nurses’ mental health as it has on society, politics, and the economy.
Overall health and quality of life are strongly influenced by mental health. In addition to being free from mental illnesses and issues, having coping mechanisms, feeling secure, and maintaining a sense of balance are also considered indicators of good mental health. The intricate interaction between social and psychological elements that protect mental health and the risk factors that imperil it is the foundation of mental health. Nurses have been exposed to various risk factors during the COVID-19 pandemic. Social support and lack of resources might further compound the psychological effects of exposure to risk variables [4,11]. According to the literature, the COVID-19 pandemic negatively impacts nurses’ mental health and well-being, and cost-efficient, simple, quick, easy-to-apply, and successful interventional studies considering the pandemic circumstances must therefore be planned [12,13,14,15,16,17,18,19,20,21,22,23].
Health authorities, professional organizations, and universities have vital roles in preserving the mental health of nurses, providing the care and counseling they require, and coordinating resources and opportunities. Interventional studies with a high level of evidence carried out under pandemic circumstances provide valuable theoretical information resources for nurses. Thus, nurses will be able to take advantage of preventive interventions with successful outcomes in any endemics and pandemics in the future. This systematic review aims to investigate the interventional studies conducted to support nurses’ mental health during the COVID-19 pandemic and to discuss what kinds of studies and plans are needed in this area.
Systematic review question
- What are the interventional studies to protect and improve the mental health of nurses during the COVID-19 pandemic?
2. Materials and Methods
2.1. Research’s Aim and Design
This systematic review seeks to investigate the interventional studies on protecting and improving the mental health of nurses in the COVID-19 pandemic, which has quickly spread over the world, and to discuss the findings and suggest possible solutions for the present and the future.
This systematic review was developed in line with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) checklist’s updated version [24] and the Cochrane manual for systematic review [25]. Additionally, the study was registered in the “Open Science Framework (OSF)” in 2022 (osf.io/entz8).
PICOS:
P: nurses working during the COVID-19 pandemic
I: interventions that improve mental health
C: routine care/other interventions
O: improvement of psychology/mental health outcomes
S: randomized controlled trials, quasi-experimental studies (non-randomized controlled trials), and pre-test/post-test studies.
2.2. Search Method
The publications related to the topic were scanned retrospectively in line with the keywords in Table 1. The literature search was conducted among English-language studies published in the APA Psych, Cochrane Library, Science Direct, Ovid-LWW, Elsevier Clinical Key, Web of Science Core Collection, MEDLINE, Springer, Taylor & Francis, and WILEY Online Library databases between 1 January 2020, and 30 June 2022, as the date of the first report of a COVID-19 case was 31 December 2019.

Table 1.
Keywords for search.
2.3. Research Selection and Evaluation
The criteria for study inclusion in the systematic review were as follows:
- Conducted during the COVID-19 pandemic
- Sample: Only nurses who cared for patients diagnosed with COVID-19
- Intervention studies aimed at protecting and improving the mental health of nurses
- The research design: pre-test/post-test studies, quasi-experimental studies (non-randomized controlled trials), or randomized controlled trials
- Original and quantitative quality with full text available online
- Written in English
- Studies published in an international peer-reviewed journal between 1 January 2020–30 June 2022
Exclusion criteria were studies outside this topic, studies not carried out during the pandemic, studies with content not aiming to protect and/or improve mental health, studies that included all healthcare workers, descriptive and/or qualitative studies, case reports, panel presentations, reviews, oral and poster presentations presented at congresses, and unpublished theses.
As a result of the search, a total of 6587 studies were found (APA Psych: 12, Cochrane Library: 67, Science Direct: 835, Ovid-LWW: 312, Elsevier Clinical Key: 950, Web of Science Core Collection: 1282, MEDLINE: 484, Springer Link: 1029, Taylor & Francis: 579, and WILEY Online Library: 1037).
First, the 6587 studies were assessed based on their titles, and 6519 studies whose sample did not exclusively consist of nurses and whose research methodology was inappropriate were eliminated from the study’s preview. Thirty-nine duplicate studies out of a total of 68 studies were removed. The full texts and abstracts of the remaining 29 articles were examined for compliance with the inclusion and exclusion criteria. As a result of the review rejecting two studies that did not focus on the intervention’s content or other factors that had a beneficial impact on the nurses’ mental health, twelve studies meeting the inclusion criteria were identified. Consequently, the study encompassed a total of twelve studies (Figure 1).
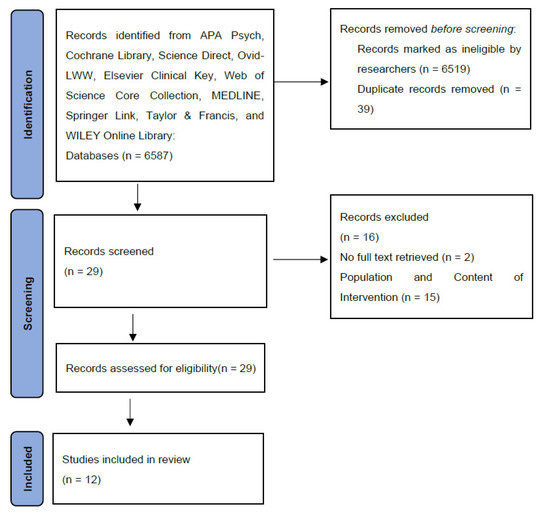
Figure 1.
PRISMA Flow Diagram [24].
3. Results
This systematic review included 12 studies that were published between 1 January 2020, and 30 June 2022, and was about the interventions on nurses’ mental health during the pandemic. Six of these studies were carried out in Turkey, three in China, one in France, one in Korea, and one in Taiwan. The interventions in all of the studies were applied by individuals who were competent in that field. The details of the sample, interventions, and scale/survey information of the included studies are shown in Table 2.

Table 2.
Characteristics of the studies included in the systematic review.
Results from Studies
Effect of diaphragmatic breathing relaxation training: It was determined that DBRT applied to nurses working in the COVID-19 pandemic increased their sleep quality and was effective in reducing their anxiety level, but there was no statistically significant decrease in the level of depression. According to the study, the most important limitation of this study was that the randomized controlled trial design was not used. They included all the nurses who were willing to participate. Additionally, objective data such as respiratory rate, heart rate, and blood pressure were not evaluated [12].
Effect of emotional freedom techniques: EFT, which consists of a short, single session and can be easily applied, was effective in reducing the stress, anxiety, and burnout levels of nurses working during the pandemic. However, the study could have been strengthened by evaluating the objective physiological parameters with scale scores. [13].
Effect of motivational messages: The study by Kose et al. suggested that the motivational messages were effective in increasing the optimism and life satisfaction levels of nurses, as well as reducing their level of hopelessness, while the study by Goktas et al. showed an increase in job satisfaction and development of communication skills, and a reduction in compassion fatigue [14,15].
Effect of acceptance and commitment therapy program: The results of acceptance and commitment therapy applied in 10 sessions on a group basis showed that it can reduce the psychological symptoms seen in nurses working during the pandemic and maintain the perceived stress level and psychological resilience. Due to the positive results, it is recommended that this study be designed as a randomized controlled trial. The study can be further improved if the same trainer applies the therapy [16].
Effect of neuro-meditation: It has been shown that guided mindful neuro-meditation, enhanced sleep, and the re-establishment of autonomic control, which was effective on work-related stress symptoms in nurses during the COVID-19 pandemic, affected sleep quality and blood pressure by reducing sympathetic activity [17].
Effect of mobile wellness program: Including health coaching, physical activity programs, and motivational messages, this program, which was carried out with the help of online platforms, encouraged nurses working in the COVID-19 pandemic to increase their level of physical activity and sleep quality. Using both wellness interventions and motivational messages helped to improve nurses’ level of physical activity and sleep quality [18].
Effect of mindfulness-based breathing and music therapy: Mindfulness-based breathing and music therapy programs reduced nurses’ stress levels and work-related strain levels, and increased their well-being. In addition, it was determined that nurses continued this program after the study. The fact that the mindfulness-based breathing and music therapy was applied by the same therapist is an important strength of this study [19].
Effect of laughter yoga: It has been determined that eight sessions of laughter yoga, which is known to be easy, safe, and effective, reduced the perceived stress and burnout levels of nurses and increased the level of life satisfaction [20].
Effect of gong meditation: Gong meditation applied to nurses during the COVID-19 pandemic has been found to reduce stress and occupational burnout levels [21].
Effect of distant Reiki: It has been found that distant Reiki reduced the stress and fatigue levels of nurses. Among the recommendations of this study is conducting randomized controlled studies for a high level of evidence [22].
Effect of e-aid cognitive behavioral therapy (eCBT-I): eCBT-I applied to nurses during the COVID-19 pandemic had positive effects on sleep quality and mood, and improved physical and mental health. In addition, there was highly motivated participation in the prevention and control of the pandemic [23].
4. Discussion
This systematic review addressed the question, “What are the intervention studies to protect and improve the mental health of nurses in the COVID-19 pandemic?” The review included 12 studies with a favorable impact on the mental health of nurses working during the pandemic. Ten of the studies in the systematic review used randomized controlled designs, while two used quasi-experimental designs. There seem to be very diverse interventional studies aimed at improving the mental health of nurses and increasing their well-being during the challenging COVID-19 pandemic era. The results of these studies demonstrate that the interventions have a positive effect on the mental health of the nurses.
It is known that the patients that nurses care for and the preparations they make for the shift and working hours have changed during the COVID-19 pandemic, and they adapted rapidly to this. These circumstances, however, had an impact on nurses’ emotional and physical resilience, in addition to other factors that affect resilience [26,27]. According to the findings of the systematic review, a wide variety of quick, easy, and efficient interventions have been used in various countries to assist nurses in dealing with this scenario. The studies included in the review are the first interventional studies conducted in this period, and therefore, the long-term effects of the interventions were not observed [11,18]. However, most interventions are suitable for nurses to apply individually at home. For this reason, it was suggested that nurses should continue these practices. Within the scope of this review, it is recommended that the taught and applied interventions be recorded in a dedicated system for nurses to access and continue the practice at any time.
In the studies of Ha et al. (2022), Kose et al. (2022), and Goktas et al. (2022), limitations such as reading the motivational messages during work and/or breaks, and the application status of the suggestions given were mentioned [14,15,18]. In particular, nurses may find it difficult to view their mobile phone notifications in protective equipment and in areas where the risk of contamination is high. For this, we suggest integrating motivational messages into the electronic systems where nurses enter their care notes during shifts, ensuring that the messages are continuous. This will allow nurses to receive and apply these messages only during working hours in case of possible shift changes.
It is important that the acceptance and commitment therapy applied to nurses by Han et al. (2022) and the e-aid cognitive behavioral therapies applied by Zhou et al. (2022) are conducted online and that positive results are obtained [16,23]. Thus, it is possible to continue individual and/or group therapies during pandemic periods. However, the fact that the therapies are conducted online and that nurses from different settings are involved, and whether these environments are suitable for therapy create a limitation in the research design. Accordingly, to ensure the continuity of these interventions, it is recommended that there should be practice rooms in healthcare institutions in which nurses and other health professionals can benefit and where therapy services can be received.
Another important point is that these intervention studies cannot be generalized because they are limited to the nurses working in the hospitals included in the study. Therefore, there is a need for studies planned with high evidence designs in which these interventions are applied. Furthermore, it is an important point that the increase in stress levels during emergencies and crises like the COVID-19 pandemic can lead to positive results by increasing the level of resilience in individuals [28].
Limitations
There were some limitations in this systematic review. One of the limitations was that only studies that included nurses, and not all healthcare professionals, were selected. The reason for focusing on nurses is that nurses’ work conditions differ from other healthcare professionals. Another limitation was that only the short-term effects of the interventional studies were evaluated, as these were the first studies in the literature. Thirdly, some of the studies included nurses working in a hospital, which could cause a limitation. The other limitation is that only studies that met the inclusion/exclusion criteria, regardless of methodological quality due to the small number of interventional studies, were included in the review.
5. Conclusions
Interventional studies investigating the variables impacting nurses’ mental health during the COVID-19 pandemic were examined in this review. During the COVID-19 pandemic, which is a difficult time for everyone, these studies were crucial in that they aimed to assist nurses by strengthening them spiritually, teaching positive coping skills against challenging situations and helping to maintain these skills, and preventing primary mental health problems before they occur. Most studies are second-level evidence-based and well-designed randomized controlled trials. These studies were conducted in different countries and demonstrate how vital it is at this time to assist nurses spiritually. It has been determined that more interventional studies are required to protect and improve nurses’ mental health to quickly plan and carry out necessary measures in any future endemic and pandemic.
Author Contributions
Conceptualization: S.K. and M.M.; methodology: S.K. and M.M.; formal analysis: S.K. and M.M.; investigation: M.M.; data curation: M.M.; writing—original draft preparation: M.M.; writing—review and editing: S.K.; supervision: S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jain, V.K.; Iyengar, K.; Vaish, A.; Vaishya, R. Differential mortality in COVID-19 patients from India and western countries. Diabetes Metab. Syndr. 2020, 14, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Tsamakis, K.; Rizos, E.; Manolis, A.J.; Chaidou, S.; Kympouropoulos, S.; Spartalis, E.; Spandidos, D.A.; Tsiptsios, D.; Triantafyllis, A.S. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp. Ther. Med. 2020, 19, 3451–3453. [Google Scholar] [CrossRef] [PubMed]
- Braquehais, M.D.; Vargas-Cáceres, S.; Gómez-Durán, E.; Nieva, G.; Valero, S.; Casas, M.; Bruguera, E. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. QJM 2020, 113, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Chidiebere Okechukwu, E.; Tibaldi, L.; La Torre, G. The impact of COVID-19 pandemic on mental health of Nurses. Clin. Ter. 2020, 171, e399–e400. [Google Scholar] [CrossRef]
- Di Tella, M.; Romeo, A.; Benfante, A.; Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020, 26, 1583–1587. [Google Scholar] [CrossRef]
- Murat, M.; Köse, S.; Savaşer, S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int. J. Ment. Health Nurs. 2021, 30, 533–543. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Goetz, C.M.; Sudan, S.; Arble, E.; Janisse, J.; Arnetz, B.B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. J. Occup. Environ. Med. 2020, 62, 892–897. [Google Scholar] [CrossRef]
- Campos, J.A.D.B.; Martins, B.G.; Campos, L.A.; de Fátima Valadão-Dias, F.; Marôco, J. Symptoms related to mental disorder in healthcare workers during the COVID-19 pandemic in Brazil. Int. Arch. Occup. Environ. Health 2021, 94, 1023–1032. [Google Scholar] [CrossRef]
- Sampaio, F.; Sequeira, C.; Teixeira, L. Impact of COVID-19 outbreak on nurses’ mental health: A prospective cohort study. Environ. Res. 2021, 194, 110620. [Google Scholar] [CrossRef]
- Simonetti, V.; Durante, A.; Ambrosca, R.; Arcadi, P.; Graziano, G.; Pucciarelli, G.; Simeone, S.; Vellone, E.; Alvaro, R.; Cicolini, G. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: A large cross-sectional study. J. Clin. Nurs. 2021, 30, 1360–1371. [Google Scholar] [CrossRef]
- Tokay Argan, M.; Mersin, S. Life satisfaction, life quality, and leisure satisfaction in health professionals. Perspect. Psychiatr. Care 2021, 57, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Jiang, T.T.; Shi, T.Y.; Liu, Y.N.; Liu, X.M.; Xu, G.J.; Li, F.L.; Wang, Y.L.; Wu, X.Y. The effectiveness of diaphragmatic breathing relaxation training for improving sleep quality among nursing staff during the COVID-19 outbreak: A before and after study. Sleep Med. 2021, 78, 8–14. [Google Scholar] [CrossRef]
- Dincer, B.; Inangil, D. The effect of Emotional Freedom Techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: A randomized controlled trial. Explore 2021, 17, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Köse, S.; Gezginci, E.; Göktaş, S.; Murat, M. The effectiveness of motivational messages to intensive care unit nurses during the COVID-19 pandemic. Intensive Crit. Care Nurs. 2022, 69, 103161. [Google Scholar] [CrossRef] [PubMed]
- Goktas, S.; Gezginci, E.; Kartal, H. The effects of motivational messages sent to emergency nurses during the COVID-19 pandemic on job satisfaction, compassion fatigue, and communication skills: A randomized controlled trial. J. Emerg. Nurs. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Zhang, L.; Liu, Y.; Zhang, C.; Zhang, Y.; Tang, R.; Bi, L. Effect of a group-based acceptance and commitment therapy programme on the mental health of clinical nurses during the COVID-19 sporadic outbreak period. J. Nurs. Manag. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Nesi, X.; Dubois, A.; Duforez, F.; Rougier, Y.; Slattery, K. Four weeks of a Neuro-Meditation program improves sleep quality and reduces hypertension in nursing staff during the COVID-19 pandemic: A parallel randomized controlled trial. Front. Psychol. 2022, 13, 854474. [Google Scholar] [CrossRef]
- Ha, Y.; Lee, S.H.; Lee, D.H.; Kang, Y.H.; Choi, W.; An, J. Effectiveness of a Mobile Wellness Program for nurses with rotating shifts during COVID-19 pandemic: A pilot cluster-randomized trial. Int. J. Environ. Res. Public Health 2022, 19, 1014. [Google Scholar] [CrossRef]
- Yıldırım, D.; Çiriş Yıldız, C. The effect of Mindfulness-Based Breathing and Music Therapy Practice on nurses’ stress, work-related strain, and psychological well-being during the COVID-19 pandemic: A randomized controlled trial. Holist. Nurs. Pract. 2022, 36, 156–165. [Google Scholar] [CrossRef]
- Sis Çelik, A.; Kılınç, T. The effect of laughter yoga on perceived stress, burnout, and life satisfaction in nurses during the pandemic: A randomized controlled trial. Complementary Ther. Clin. Pract. 2022, 49, 101637. [Google Scholar] [CrossRef]
- Hsieh, H.F.; Huang, Y.T.; Ma, S.C.; Wang, Y.W. Occupational burnout and stress of nurses in Taiwan regarding COVID-19: An intervention with gong medication. J. Nurs. Manag. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bektaş Akpınar, N.; Özcan Yüce, U.; Yurtsever, S. The Effect of Distant Reiki on the stress and fatigue levels of nurses working in COVID-19 clinics: A randomized-controlled, single-blind study. Holist. Nurs. Pract. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Kong, J.; Wan, Y.; Zhang, X.; Liu, X.; Qu, B.; Wang, B.; Xue, R. Positive impacts of e-aid cognitive behavioural therapy on the sleep quality and mood of nurses on site during the COVID-19 pandemic. Sleep Breath 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version, 6.3; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2022. [Google Scholar]
- Labrague, L.J. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J. Nurs. Manag. 2021, 29, 1893–1905. [Google Scholar] [CrossRef]
- Baskin, R.G.; Bartlett, R. Healthcare worker resilience during the COVID-19 pandemic: An integrative review. J. Nurs. Manag. 2021, 29, 2329–2342. [Google Scholar] [CrossRef]
- Fino, E.; Bonfrate, I.; Fino, V.; Bocus, P.; Russo, P.M.; Mazzetti, M. Harnessing distress to boost growth in frontline healthcare workers during COVID-19 pandemic: The protective role of resilience, emotion regulation and social support. Psychol. Med. 2021, 1–3. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).