Abstract
This study focuses on an individual from the southeastern area of the Roman Suburbium in Late Antiquity (3rd–5th centuries CE), whose skeleton was found in a multiple burial alongside five others. Osteological and CT imaging analyses revealed a significant developmental defect in the left hip, characterized by a shallow, flattened acetabulum and a hypoplastic or aplastic femoral head, with no evidence of infection or postmortem alteration. This rare condition provides a compelling case study demonstrating the effectiveness of an integrated diagnostic approach combining traditional osteology with advanced imaging techniques. Despite prior research into orthopedic pathologies in Roman Imperial and Late Antique populations, no comparable cases have been documented, highlighting a notable gap in the bioarchaeological literature regarding congenital skeletal defects. This case contributes to a broader understanding of disability in ancient communities and raises important questions about social recognition and support for individuals with physical impairments in the past. However, limitations exist due to the absence of certain skeletal elements, which restricts a full assessment of compensatory biomechanical adaptations, such as load redistribution through the trunk or upper limbs. Nevertheless, the findings underscore the growing importance of refining diagnostic standards to better identify and interpret evidence of disability in historical populations.
1. Introduction
Recent technological and methodological advancements in bioarchaeology have significantly enhanced our ability to investigate the health, disease, and lived experiences of past populations, often through the paleopathological analysis of human skeletal remains [1,2,3,4,5,6,7]. Among the most revealing sources of information are limb bones, whose structural changes and pathological alterations provide valuable insights into physical activity patterns, trauma, degenerative diseases, and congenital disorders. In this context, the lower limbs—critical for weight-bearing and mobility—serve as key anatomical regions for detecting biomechanical stress, abnormal load distribution, and compensatory skeletal remodeling. These adaptations, however, rarely occur in isolation: the trunk and spine often participate in the redistribution of mechanical loads and postural adjustments, reflecting systemic compensatory mechanisms that maintain balance and functional alignment across the entire musculoskeletal framework [1,8]. Accordingly, the modifications observed in the skeletal elements should be regarded not merely as anatomical responses but as reflections of the broader patterns of movement, occupational activities, and habitual behaviors that shaped the daily lives and long-term functional adaptations of past individuals.
Modern imaging technologies, particularly computed tomography (CT), have become indispensable in detecting and diagnosing pathological changes that may not be readily visible through macroscopic examination. CT’s ability to generate high-resolution, three-dimensional reconstructions allows for precise visualization of bone morphology and internal structures, enabling the identification of developmental anomalies and chronic musculoskeletal conditions with a level of detail previously unattainable through traditional osteological methods alone [9,10,11]. For instance, CT scans have been essential in studying ancient anatomy, evolutionary changes, and interspecies comparisons [12,13,14].
Increasingly, such noninvasive imaging is recognized not only as a tool for anatomical reconstruction but as a diagnostic instrument in paleopathology, offering biomarkers for skeletal health and disease [15,16]. As a result, paleoimaging is now recommended in numerous national guidelines for the documentation and analysis of archaeological human remains [17,18]. The integration of imaging modalities like CT into paleopathological investigations—collectively termed “paleoimaging” [19]—has now become standard in many archaeological contexts, particularly when dealing with complex or unusual skeletal pathologies [20]. While conventional radiography offers two-dimensional insights into bone structure [21], the layered visualization and spatial accuracy of CT make it especially valuable for assessing overlapping or distorted skeletal features, such as those seen in joint dysmorphisms and congenital malformations [9,11,15,19,22,23], which make these techniques the most applied in post-mortem studies.
Through high-resolution 3D scanning and computed tomography, researchers can investigate the microstructural details of bones without risking physical damage, thereby preserving fragile specimens for future analyses. These approaches allow for the detection of minute surface modifications, post-depositional alterations, and internal degradation patterns that are often imperceptible through traditional observation. Moreover, virtual documentation enables the creation of accurate digital replicas that can be shared, reanalyzed, and compared across research institutions, fostering reproducibility and long-term conservation of bioarchaeological data. This approach has proven particularly valuable in the examination of delicate remains, such as the Iceman [24]. Moreover, the adoption of non-invasive methods, which promote more sustainable research practices by enabling the preservation of both physical specimens and their digital counterparts, can benefit all forms of paleopathological evaluation.
This paper presents a case study of a pathological condition identified in the lower limb bones of an individual buried along the ancient Via Labicana, in the southeastern periphery of the Roman Suburbium, dating to Late Antiquity (3rd–5th centuries CE). The individual, found within a multiple burial context, exhibited an unusual and pronounced dysmorphism of the left hip joint, prompting a detailed analysis integrating osteological and imaging techniques. Following the Italian guidelines for the management of human skeletal remains [17], the remains were assessed for preservation quality, basic demographic characteristics, and morphological anomalies. The visual inspection of the post-cranial skeleton revealed a flattened and shallow acetabulum alongside a hypoplastic or aplastic femoral head—anomalies indicative of a severe defect affecting the hip joint. The absence of secondary pathological signs such as reactive bone formation or infection suggests a non-traumatic, possibly congenital etiology.
2. Materials and Methods
The skeleton was identified during a rescue archaeology activity along the ancient Via Labicana (Figure 1) in 2022 and excavated following the Italian guidelines for the management of human bone remains [17]. Emergency excavations such as that presented here represent a crucial component of archaeological and bioarchaeological practice, undertaken when sites or buried remains face imminent threats of destruction or disturbance. Such situation arose unexpectedly, prompted by infrastructure development, that jeopardized the preservation of cultural and biological heritage. Thus, unlike planned research excavations, the excavation was conducted under constrained conditions, requiring rapid assessment, strategic prioritization, and methodological flexibility, with the principal objective to retrieve and record as much contextual and material information as possible within a limited timeframe, ensuring that the analysis and interpretation remain scientifically valid [25].
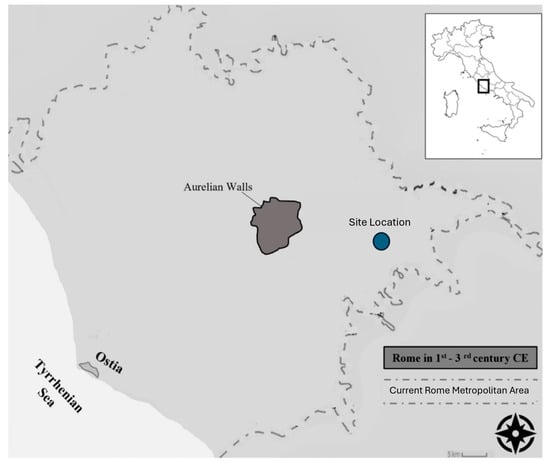
Figure 1.
Location of the site where the individual was excavated.
The osteological material was found in a deep soil pit covered with tiles, which allowed for broad dating by the context of the burial area to the broad Late Antiquity time transect—3rd century up to the 5th century CE. The pit contained the slightly disarticulated bones of at least 4 individuals [26]. Unfortunately, the lack of details on the archeological setting due to the preventive archaeology survey prevents further characterization of the burial ground.
The skeleton and disarticulated human bones were excavated, and a detailed written and visual description followed the macroscopic examination of each bone [3]. The preservation of the bones limited the range of analytical methods available for assessing basic demographic parameters, such as sex and age-at-death, leading us to focus primarily on the osteological examination of the hip bones and skull. Age assessment was based on the morphological appearance of the pubic symphysis components [27], which presented a billowing surface with horizontal ridges and furrows (Phase 1 in [27]), but showing a slight lower extremity and ventral rampart in process of completion (consistent with Phase 3 by [27]). This evaluation was further supported by the recommendations [28] for the rib ends, and the stage of ectocranial suture closures [29]. The hip bones—despite the diagenetic damages—were evaluated in their greater sciatic notch area and pubic bone morphology for reliable sex estimation [4,30]. The individual’s stature was calculated according to [31], leveraging the length of the long tubular bones not impacted by the anatomical alteration.
A differential diagnosis was performed to assess the observed skeletal alteration. The morphology and anatomical location of the lesion were examined with reference to both pathological and post-mortem processes. Potential etiologies, including congenital conditions, trauma, degenerative joint disease, and infectious processes, were systematically evaluated. Published paleopathological cases were consulted for comparative purposes, enabling a structured assessment of the most plausible diagnosis.
The diagnostic criteria for the developmental dysplasia of the hip involved the identification of a shallow and irregular true acetabulum and alterations on the lateral aspect of the ilium suggestive of the development of a false acetabulum [32]. Additionally, any detectable alterations in the pelvis, lower limb, and spine were documented and compared to radiological changes documented in the existing medical literature [32].
Furthermore, the pelvic district underwent CT scans, which were performed using a 164-slice scanner (GE medical system revolution CT) with the following parameters: slice acquisition 1.25 mm, pitch 0.5; rotation time 0.5 s, tube voltage 100 kVp, tube current-time 100 mAs/rotation. These settings have been demonstrated to be effective in paleoimaging evaluations in other cases treated at the same imaging center [9,15,22,23]. Images were reviewed and reconstructed using the MPR protocol [33], and 3D images were created using the Volume Rendering protocol.
Ethical review and approval were waived for this study due to the use of anonymized archaeological human remains curated in institutional collections. These remains are historical and non-identifiable, and all analyses were conducted in accordance with ethical guidelines for research on human skeletal material, in accordance with Italian national government regulation and institutional protocols [17].
3. Results
The skeletal remains were in a relatively fair state of preservation (Figure 2). Pelvic and cranial morphological traits were consistent with adult female variation. The integrated evaluation of the skeletal traits in the pelvis, along with the degenerative changes in the rib ends and ectocranial suture closures, agreed on the estimation of an age at death of 20–29.

Figure 2.
Left femur and hip bone, showing the hypoplastic head (a), the modified real acetabulum (circled by dashed line) and the false acetabulum pointed by the arrow (b).
Once the individual’s biological sex was estimated, stature was more accurately assessed using osteometric measurements of the right femur and tibia, yielding an estimated height of approximately 157 cm, consistent with averages reported for Late Imperial and Medieval central Italian populations (average stature for females: 154.5; standard deviation: 3.4 [34,35]).
Detailed examination of the skeletal material did not reveal notable non-specific stress markers, suggesting a relatively healthy lifestyle [36].
The left hip bone presents several key features indicative of severe congenital hip dysplasia (DDH). Notably, the acetabulum is shallow and flattened, insufficient to accommodate the femoral head, which is markedly hypoplastic/aplastic. Additionally, secondary changes, such as the antero-lateral shifting of the ischial spine and the formation of a false acetabulum near the anterior inferior iliac spine (AIIS), further suggest long-term skeletal adaptation rather than postmortem distortion (Figure 2 and Figure 3). The groove for the Obturator Externus tendon is entirely flattened, and the acetabular notch is unusually wide, both of which are atypical for traumatic or diagenetic alterations. Aplasia/hypoplasia involved the left femoral head and neck, leading to the shortening of the bone, whose intertrochanteric crest was not fully developed. The uppermost attachment area of the Vastus Lateralis was developed into a flat spike, and the Trochanteric Fossa was not developed, making the superior area of the proximal epiphysis entirely dysmorphic (Figure 2a). CT imaging corroborates these findings, showing a clear flattening of the true acetabulum, as well as significant underdevelopment of the femoral head and neck, without any signs of healing, such as callus formation or other markers of trauma.
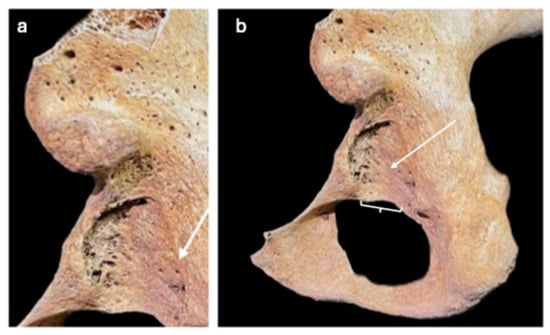
Figure 3.
(a) The arrow shows the flattened groove for the Obturator Externus origin. (b) The acetabular notch was unusually wide (brace); and the acetabulum is modified into a shallow and triangularly shaped area (arrow).
Furthermore, the contralateral hip joint appears normal on both visual inspection and CT (Figure 4), supporting the diagnosis of a unilateral condition. In light of these observations, we considered a range of differential diagnoses, including septic arthritis, hip tuberculosis, Legg–Calvé–Perthes disease, cerebral palsy-related hip dislocation, and traumatic dislocation. However, none of these conditions align with the osteological and imaging findings (Table 1). Specifically, there are no signs of infection, osteopenia, subchondral sclerosis, or any destructive remodeling typically associated with those conditions. The femoral head’s hypoplasia, along with the absence of trauma and inflammatory markers, strongly points to a congenital etiology, most consistent with severe DDH (type III) [37,38,39,40]. The diagnostic criteria used to evaluate this case, outlined in Table 2, were applied rigorously. This comprehensive evaluation—combining osteological features, CT imaging, and the exclusion of trauma or infection—provides a robust case for the diagnosis of DDH, confidently ruling out other potential causes such as infectious or traumatic pathology.

Figure 4.
Frontal view of a CT image reconstruction on the oblique coronal plane of the hip joints. The image shows complete flattening of the left (L) true acetabulum and severe morphological alterations of the femoral head and neck, which showed marked insufficiency. The right (R) hip joint shows normal morphology.

Table 1.
Summary of the characteristics of comparative pathological conditions for the differential diagnosis.

Table 2.
Summary of paleopathological changes resulting from developmental dislocation of the hip, following [32].
In summary, the combination of the morphological, osteological, and imaging data supports a diagnosis of severe congenital hip dysplasia, with no evidence of trauma, infection, or postmortem diagenetic alterations (Table 3).

Table 3.
Summary Table showing the concordance of the Anatomical and Imaging evaluations.
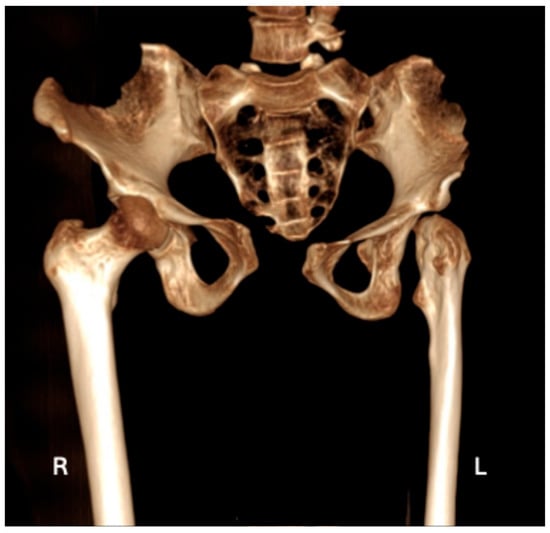
Figure 5.
Three-dimensional volume rendering image on the frontal view illustrating the morphological alterations in the left (L) hip joint, with a regular right (R) hip joint for comparison; it should be noted that portions of the ilia are missing due to taphonomic processes.
Table 3.
Summary Table showing the concordance of the Anatomical and Imaging evaluations.
| Paleopathological Finding | Anatomical Evaluation | Imaging Evaluation |
|---|---|---|
| Shallow, flattened real acetabulum (Figure 2b) | X | X |
| False acetabulum AIIS (Figure 2b) | X | X |
| Antero-lateral shifting of the ischial spine | X | X |
| Flattened groove for the Obturator Externus (Figure 3a) | X | X |
| Widening of the acetabular notch (Figure 3a) | ||
| Lack of bony deposit around the joint (Figure 3b) | X | |
| Contralateral hip joint is definitively unaffected (Figure 4 and Figure 5) | X | X |
| Periarticular osteoporosis (Figure 4) | X | |
| Hypoplastic/aplastic femoral head (Figure 2b) | X | X |
| Subchondral sclerosis (Figure 4) | X | |
| Lack of development of the intertrochanteric crest (Figure 2a and Figure 4) | X | X |
| Lack of development of the trochanteric fossa (Figure 2a and Figure 4) | X | X |
| Occult fractures (Figure 4) | X | |
| Uppermost origin area for Vastus Lateralis as a flat spike (Figure 2a) | X |
4. Discussion
To explore the differential diagnosis for the skeletal outcome and exclude septic arthritis, bone tuberculosis, or traumatic dislocation, we appealed to both the osteologic evaluation and paleoimaging.
Indeed, the characterization of macroscopic bone structures affected by morphological alterations greatly benefitted from the paleoimaging analyses. Such approaches a) excluded traumatic signatures within the internal bone structure, and b) investigated the inner and three-dimensional architecture via CT scanning to identify features associated with deformities resulting from bony resorption or osteolytic lesions by providing non-destructive, high-resolution insights into bone morphology otherwise invisible to the naked eye. Furthermore, the resolution of paleoimaging examinations remained critical for reconstructions of bony structures, supporting more robust diagnostic assessments [46,47,48,49,50,51,52].
The simultaneous existence of a false acetabulum, the characteristics of the preserved but modified sections of the true acetabulum, and the alterations in the proximal femur align with the diagnosis of hip dislocation in developmental dysplasia of the hip (DDH) [32]. Hip dysplasia could be related to those defects as they may present with an absent or modified hip bone, femoral neck pseudoarthrosis, and absent or shortened femur. DDH is definitely tightly coupled with the proximal femoral growth disturbance (PFGD), characterizing defects in the primary ossification center of the proximal femur [53,54], which is one of the most devastating complications of DDH, even though the relationship between DDH and PFGD is multifaceted, involving a bidirectional interaction between the two conditions [55,56]. Specifically, DDH is characterized by hip joint instability due to abnormal femoral-acetabular alignment, which can lead to compensatory mechanical alterations. These changes often affect the proximal femoral growth plate, resulting in growth disturbances that manifest as limb deformities, such as limb length discrepancies, angular deformities, or femoral neck abnormalities. This relationship underscores the potential for DDH to lead to PFGD, especially in severe or untreated cases [57]. However, PFGD can exacerbate DDH pathology. When growth disturbances at the proximal femur lead to deformities like femoral head or neck abnormalities, they can alter the biomechanics of the hip joint. This misalignment places additional stress on the acetabulum, exacerbating the existing joint instability and further impairing hip congruency. Consequently, PFGD can worsen the clinical presentation of DDH, contributing to increased joint instability and higher risks of dislocation or degenerative changes [58].
Furthermore, the diagnostic hypothesis of DDH is further reinforced by the fact that the left hip is generally more frequently affected [39,40].
Notably, the hip joint components develop embryonically from the same primitive mesenchymal cells [59], and the blood supply to the proximal femur is a critical element for proper development [54]. Multiple exogenous and endogenous factors such as infection, trauma, rheumatoid defects, and congenital abnormalities may impact the development of that body district [60,61,62,63,64].
This untreated condition might have resulted in morphological alterations affecting the joints and bones of the entire left leg [65,66]. Notably, if left unaddressed, DDH may increase the risk of early degenerative hip arthritis due to altered stress on the bones [61,67], affecting walking practice and resulting in significant pain, potentially limiting activities and negatively impacting the individual lifestyles and that of their families [68]. Specifically, the skeleton showed subchondral sclerosis occurring at the joint margins on the femoral and tibial articular surfaces of the knee (Figure 6), and both medial and lateral joint erosion on the tibial plate can be noted bilaterally, particularly in the left joint. These findings, linked to repeated microtrauma caused by the imbalanced weight load on the left knee joint [39,40], might be attributed to secondary osteoarthritis from abnormal mechanical forces produced by hip dysplasia [39], which might have impacted the tibial varism due to posture alterations with medial overload during walking [38]. However, to date we have no biomechanical data for attributing bilateral knee joint erosion and tibial varism solely to altered mechanics from DDH. Although DDH-related abnormal gait mechanics can potentially contribute to these changes, other alternative causes, such as age-related degenerative processes or systemic conditions (i.e., metabolic bone disorders), should also be considered as potential contributors. Tibial varism, in particular, is not commonly a direct consequence of DDH and often arises from other factors, including genetic predispositions or secondary musculoskeletal alterations [69,70]. As such, the interpretation of tibial varism and knee joint erosion found in the skeletal individual should be approached cautiously.
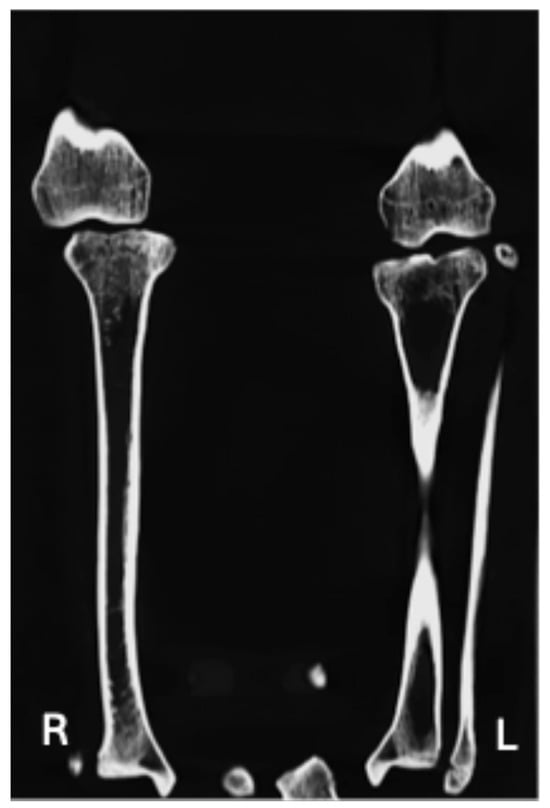
Figure 6.
Frontal CT image reconstruction on the oblique coronal plane of the Left (L) and Right (R) tibio-femural joint. Subchondral sclerosis occurring at the joint margins on the femoral and tibial articular surfaces and both medial and lateral joint erosion on the tibial plate can be noted bilaterally, particularly in the left joint.
However, the left tibia and femur were reduced in length compared to the contralateral; this aspect is typical of congenital diseases that might also cause underdevelopment during the individual’s growth phase [37,39].
The paleopathological literature has primarily described dislocations resulting from developmental dysplasia of the hip (DDH) as sporadic. A dysplastic hip dating back to Neolithic times is shown in the British Museum, where also a bronze figurine depicting congenital dislocation from the Hellenistic era is preserved [71].
More recently, Hippocrates (460–357 BC) extensively detailed the incapacitating effects of hip dislocation, noting distinctions between anterior and posterior dislocations and describing treatments based on traction, leverage, and pressure; cases in which reduction was unsuccessful or neglected were often associated with major disability [68,71]. Remarkably, two extensive skeletal collections from medieval England and France showed a prevalence of dislocation associated with developmental dysplasia at 2.7‰ and 13.1‰, respectively [71,72,73]. Similarly, two cases from an Italian convent in the 10th century AD [74] were reported, and only some Italian sporadic cases were reported for later centuries [75,76].
Recently, a collection of orthopedic pathologies in the Roman Imperial Age (1st–3rd centuries CE) [77] was published, even though no comparable cases were reported. Similarly, no specific reference to that alteration can be found in the military medical records [78].
Accordingly, to the best of our knowledge, the reported case study represents the most ancient individual from Italy suffering from that health issue and the only one described with massive dysplastic/aplastic changes in the femoral head.
While the diachronic series examination suggests that the prevalence of developmental dysplasia of the hip (DDH) may have remained relatively stable over the centuries, we acknowledge that this claim could be an oversimplification. Sampling biases, differences in detection methods over time, and cultural variations in the recognition and reporting of the condition may all contribute to the observed prevalence estimates, influencing the consistency of historical data [72]. However, substantial differences in prevalence are observed among populations globally [79], maybe due to the differential perception of child swaddling, which can be considered one of the major triggering and risk factors for DDH, especially when the child’s legs are not free to bend and flex [80,81].
Taken together, the anatomical evidence related to the skeletal individual suggest that the individual lived with a significant and long-term mobility impairment. While the physical manifestations of DDH can be described in anatomical terms, understanding what this condition meant within the lived experience of the individual requires a broader interpretive framework to move beyond clinical description and to consider the social dimensions of impairment in antiquity. Following the social model of disability developed by British disability theorists in the 1970s [82], a distinction can be drawn between impairment—the physiological condition observable in the skeleton—and disability, which arises from the social and cultural processes that shape how bodily difference is perceived and accommodated. Within this model, the disabling factor is not the body itself but the societal structures that stigmatize or limit it. Paleopathological analysis can therefore document impairment, but the recognition of disability depends on contextual evidence, on how communities responded to, cared for, or integrated individuals with physical differences [83,84,85].
Given the severity of the joint alteration, it is likely that the person experienced impaired mobility, enduring constant pain and displaying a noticeable limp, which might have exposed the individual to societal labeling, marking them as distinct from others. Indeed, some cultures outright rejected individuals with disabilities, others marginalized them, and in certain societies, they were viewed as burdens and reluctantly sustained by their families [86]. Conversely, in other societies, they were accepted as financial burdens and kept alive by their families or community [87,88,89].
Although the emergency nature of the excavation limited opportunities for detailed contextual reconstruction, the longevity of the individual—who survived into reproductive adult age—nonetheless provides meaningful evidence for sustained care and maybe also social integration. Within the framework of the bioarchaeology of care, such survival implies that others assisted this person in ways that enabled continued participation in community life, whether through physical aid, shared labor, or social inclusion [90]. Rather than viewing impairment as a marker of exclusion, this perspective foregrounds the relational and cooperative aspects of human communities and their capacity to accommodate bodily diversity. However, survival alone does not necessarily demonstrate compassion [91]; care may stem from pragmatism, mutual dependence, or even moral obligation as much as from empathy. Consequently, it is challenging to fully understand how society perceived the individual’s impaired gait in this Late Antiquity Roman community. The burial inside a pit, along with disarticulated bones from other individuals, may suggest an intentional disregard for the recognition of this person’s individual identity [92], highlighting how the mortuary management for people suffering from physical disability in the Roman and Late Antiquity periods is far from being fully understood [87,88,89,93,94,95]. Nevertheless, the presence of this individual within their community setting reveals that the physical difference was not inherently incompatible with belonging. Interpreted through the lens of disability theory and the bioarchaeology of care, this case contributes to a still growing anthropological understanding of how ancient communities negotiated interdependence, resilience, and the social meanings of embodied variation [96]. However, we must acknowledge the inherent bias in interpreting the treatment of individuals with disabilities based solely on a single burial. This individual’s remains and the associated community may not be fully representative of broader societal practices, and the social context surrounding this burial could significantly influence our understanding of their treatment. Therefore, it is crucial to exercise caution when extrapolating definitive conclusions about societal attitudes toward disability in Late Antiquity from isolated cases. Such interpretations may not fully capture the diversity of cultural norms or the variability in practices across different communities.
Although a detailed characterization of the lesion can be provided, the main limitation of this study relies on the preservation status of the skeleton, for which the upper skeletal elements were not well preserved. Indeed, the biomechanical effects stemming from such an early age issue indicate that the repercussions of a malformed hip are generally extensive [97]. The lack of some bony regions makes it hard to recognize dysmorphic characteristics related to the unbalanced distribution of the loads (i.e., scoliosis of the spine [98]), which could eventually be supported by altered strategies involving the trunk and upper limbs.
The osteological and structural diagnosis of the dysmorphic feature seems to be not sensitive to those limitations, as the diagnostic criteria for DDH are substantially met, allowing for a relatively precise diagnosis. However, it should be borne in mind that the loss of the femoral head and neck, along with failure to form a normal shaped acetabulum, would also be related to septic arthritis in infancy, where the pus can destroy the femoral head and neck, even though the ultrastructure analyses by imaging is consistent in ruling out this diagnostic hypothesis.
The comprehensive investigations on the prevalence of developmental defects in ancient Roman populations are still an unmatched topic in the bioarcheological and paleopathological literature, so we could not compare the case study with coeval individuals suffering from such a similar disability. However, the increasing awareness and refinement of the diagnostic guidelines for skeletal samples [32,99] certainly represent a pivotal step in recognizing subjects suffering from physical disabilities such as the one from Rome we present, which are going to merit focused investigation by biological anthropologists examining historical communities to contribute to unveiling their social recognition and support hypothesis related to the perception of disability in the past.
Author Contributions
Conceptualization, F.D.A., L.F. and A.B.; methodology, F.D.A. and L.F.; software, L.F., F.G. and G.M.; validation, L.F., F.G. and G.M.; formal analysis, F.D.A., L.F., A.B., F.C., A.C. and M.P.; investigation, S.I. and M.P.; resources, C.D.; data curation, F.D.A., L.F., A.B. and S.I.; writing—original draft preparation, F.D.A.; writing—review and editing, F.D.A., L.F. and S.I.; visualization, L.F., F.C. and A.C.; supervision, M.P., V.G., F.G. and G.M.; funding acquisition, V.G. All authors have read and agreed to the published version of the manuscript.
Funding
This article is part of PRIN 2022—project code 202255L4YW—‘Early-life adversities: writing a biological history of childhood through a transdisciplinary approach’ (PI V. Gazzaniga) Financed by European Union—Next Generation EU, Mission 4 Component 1 CUP.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. F.D.A. was supported by the project: MNESYS—a multiscale integrated approach to the study of the nervous system in health and disease (PNRR).
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Abbreviations
The following abbreviations are used in this manuscript:
| AIIS | Anterior Inferior Iliac Spine |
| CT | Computed tomography |
| DDH | Developmental dysplasia of the hip |
| PFGD | Proximal femoral growth disturbance |
References
- Afshar, Z. Bioarchaeology: Scientific Studies of Archaeological Human Skeletal Remains. J. Res. Archaeom. 2018, 4, 81–92. [Google Scholar] [CrossRef][Green Version]
- Stodder, A.L.W.; Byrnes, J.F. (Re)Discovering Paleopathology: Integrating Individuals and Populations in Bioarchaeology. In Evaluating Evidence in Biological Anthropology: The Strange and the Familiar; Willermet, C., Lee, S.-H., Eds.; Cambridge Studies in Biological and Evolutionary Anthropology; Cambridge University Press: Cambridge, UK, 2019; pp. 103–125. ISBN 978-1-108-47684-3. [Google Scholar]
- Buikstra, J.E. Bioarchaeologists Speak Out: Deep Time Perspectives on Contemporary Issues; Bioarchaeology and Social Theory; Springer International Publishing: Cham, Switzerland, 2019; ISBN 978-3-319-93011-4. [Google Scholar]
- Buikstra, J.; Ubelaker, D. Standards for Data Collection from Human Skeletal Remains: Proceedings of a Seminar at the Field Museum of Natural History, Organized by Jonathan Haas; Arkansas Archeological Survey: Fayetteville, AK, USA, 1994. [Google Scholar]
- Buikstra, J.E. A Bioarchaeological Perspective: What’s in a Name? Annu. Rev. Anthropol. 2024, 53, 1–19. [Google Scholar] [CrossRef]
- Armelagos, G.J. Bioarchaeology as Anthropology. Archeol. Pap. Am. Anthropol. Assoc. 2003, 13, 27–40. [Google Scholar]
- Armelagos, G.J.; Gerven, D.P.V. A Century of Skeletal Biology and Paleopathology: Contrasts, Contradictions, and Conflicts. Am. Anthropol. 2003, 105, 53–64. [Google Scholar] [CrossRef]
- Michalik, R.; Rissel, V.; Migliorini, F.; Siebers, H.L.; Betsch, M. Biomechanical Evaluation and Comparison of Clinically Relevant versus Non-Relevant Leg Length Inequalities. BMC Musculoskelet. Disord. 2022, 23, 174. [Google Scholar] [CrossRef]
- Filograna, L.; Pugliese, L.; Muto, M.; Tatulli, D.; Guglielmi, G.; Thali, M.J.; Floris, R. A Practical Guide to Virtual Autopsy: Why, When and How. In Seminars in Ultrasound, CT and MRI; WB Saunders: Philadelphia, PA, USA, 2019; Volume 40, pp. 56–66. [Google Scholar] [CrossRef]
- Giovannetti, G.; Guerrini, A.; Minozzi, S.; Panetta, D.; Salvadori, P.A. Computer Tomography and Magnetic Resonance for Multimodal Imaging of Fossils and Mummies. Magn. Reson. Imaging 2022, 94, 7–17. [Google Scholar] [CrossRef]
- Shelmerdine, S.C.; Gerrard, C.Y.; Rao, P.; Lynch, M.; Kroll, J.; Martin, D.; Miller, E.; Filograna, L.; Martinez, R.M.; Ukpo, O.; et al. Joint European Society of Paediatric Radiology (ESPR) and International Society for Forensic Radiology and Imaging (ISFRI) Guidelines: Paediatric Postmortem Computed Tomography Imaging Protocol. Pediatr. Radiol. 2019, 49, 694–701. [Google Scholar] [CrossRef]
- Profico, A.; Buzi, C.; Di Vincenzo, F.; Boggioni, M.; Borsato, A.; Boschian, G.; Marchi, D.; Micheli, M.; Cecchi, J.M.; Samadelli, M.; et al. Virtual Excavation and Analysis of the Early Neanderthal Cranium from Altamura (Italy). Commun. Biol. 2023, 6, 316. [Google Scholar] [CrossRef]
- Montiel, G.; Lorenzo, C. A New Virtual Reconstruction of the Ndutu Cranium. Heritage 2023, 6, 2822–2850. [Google Scholar] [CrossRef]
- Buzi, C.; Boggioni, M.; Borsato, A.; Boschian, G.; Marchi, D.; Moggi-Cecchi, J.; Profico, A.; Riga, A.; Samadelli, M.; Manzi, G. Virtual Paleoanthropology in Karstic Environments. The Challenging Case of the Neanderthal Skeleton from Altamura (Southern Italy). Quat. Sci. Rev. 2024, 338, 108833. [Google Scholar] [CrossRef]
- Filograna, L.; Manenti, G.; Mecchia, D.; Tatulli, D.; Pasqualetto, M.; Perlangeli, V.; Rossi, P.F.; De Angelis, F.; Floris, R. Investigation of Human Remains from the Archaeological Areas of “Parco Archeologico Di Ostia Antica”: The Role of CT Imaging. Forensic Imaging 2022, 31, 200521. [Google Scholar] [CrossRef]
- Singh, S.; Bray, T.J.P.; Hall-Craggs, M.A. Quantifying Bone Structure, Micro-Architecture, and Pathophysiology with MRI. Clin. Radiol. 2018, 73, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Ministero Italiano Cultura. I Resti Scheletrici Umani: Dallo Scavo al Laboratorio al Museo; Ministero Della Cultura ICCD—Istituto Centrale per Il Catalogo e La Documentazione ICA—Istituto Centrale per l’Archeologia: Rome, Italy, 2022. [Google Scholar]
- Mitchell, P.; Brickley, M. Professional Practice Papers|Chartered Institute for Archaeologists. Available online: https://www.archaeologists.net/publications/papers (accessed on 25 January 2023).
- Beckett, R.G. Paleoimaging: A Review of Applications and Challenges. Forensic Sci. Med. Pathol. 2014, 10, 423–436. [Google Scholar] [CrossRef]
- Villa, C.; Frohlich, B.; Lynnerup, N. Chapter 7—The Role of Imaging in Paleopathology. In Ortner’s Identification of Pathological Conditions in Human Skeletal Remains, 3rd ed.; Buikstra, J.E., Ed.; Academic Press: San Diego, CA, USA, 2019; pp. 169–182. ISBN 978-0-12-809738-0. [Google Scholar]
- Bansal, G.J. Digital Radiography. A Comparison with Modern Conventional Imaging. Postgrad. Med. J. 2006, 82, 425–428. [Google Scholar] [CrossRef]
- Filograna, L.; Tartaglione, T.; Vetrugno, G.; Guerra, C.; Fileni, A.; Bonomo, L. Freshwater Drowning in a Child: A Case Study Demonstrating the Role of Post-Mortem Computed Tomography. Med. Sci. Law 2015, 55, 304–311. [Google Scholar] [CrossRef]
- Filograna, L.; Guglielmi, G.; Floris, R.; Marchetti, D. The Development of Forensic Imaging in Italy. A Systematic Review of the Literature. J. Forensic Radiol. Imaging 2018, 15, 14–20. [Google Scholar] [CrossRef]
- Villa, C.; Larsen, S.; Zink, A.; Lynnerup, N. Ötzi the Iceman: Forensic 3D Reconstructions of a 5300-Year-Ago Murder Case. Int. J. Legal Med. 2025, 139, 2263–2271. [Google Scholar] [CrossRef]
- Thompson, M.W. N.P. Stanley Price (Ed.): Conservation on Archaeological Excavations, with Particular Reference to the Mediterranean Area. Rome: ICCROM, 1984, 158 pp., Illustrated. Antiquity 1985, 59, 59–60. [Google Scholar] [CrossRef]
- Nicolosi, T.; Mariotti, V.; Talamo, S.; Miari, M.; Minarini, L.; Nenzioni, G.; Lenzi, F.; Pietrobelli, A.; Sorrentino, R.; Benazzi, S.; et al. On the Traces of Lost Identities: Chronological, Anthropological and Taphonomic Analyses of the Late Neolithic/Early Eneolithic Fragmented and Commingled Human Remains from the Farneto Rock Shelter (Bologna, Northern Italy). Archaeol. Anthropol. Sci. 2023, 15, 36. [Google Scholar] [CrossRef]
- Brooks, S.; Suchey, J.M. Skeletal Age Determination Based on the Os Pubis: A Comparison of the Acsádi-Nemeskéri and Suchey-Brooks Methods. Hum. Evol. 1990, 5, 227–238. [Google Scholar] [CrossRef]
- Işcan, M.Y.; Loth, S.R.; Wright, R.K. Age Estimation from the Rib by Phase Analysis: White Females. J. Forensic Sci. 1985, 30, 853–863. [Google Scholar] [CrossRef] [PubMed]
- Meindl, R.S.; Lovejoy, C.O. Ectocranial Suture Closure: A Revised Method for the Determination of Skeletal Age at Death Based on the Lateral-Anterior Sutures. Am. J. Phys. Anthropol. 1985, 68, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Djurić, M.; Djonić, D.; Nikolić, S.; Popović, D.; Marinković, J. Evaluation of the Suchey-Brooks Method for Aging Skeletons in the Balkans. J. Forensic Sci. 2007, 52, 21–23. [Google Scholar] [CrossRef]
- Trotter, M.; Gleser, G.C. A Re-Evaluation of Estimation of Stature Based on Measurements of Stature Taken during Life and of Long Bones after Death. Am. J. Phys. Anthropol. 1958, 16, 79–123. [Google Scholar] [CrossRef]
- Redfern, R. Diagnostic Criteria for Developmental Dislocation of the Hip in Human Skeletal Remains. Int. J. Osteoarchaeol. 2008, 18, 61–71. [Google Scholar] [CrossRef]
- Dalrymple, N.C.; Prasad, S.R.; Freckleton, M.W.; Chintapalli, K.N. Informatics in Radiology (infoRAD): Introduction to the Language of Three-Dimensional Imaging with Multidetector CT. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2005, 25, 1409–1428. [Google Scholar] [CrossRef]
- Giannecchini, M.; Moggi-Cecchi, J. Stature in Archeological Samples from Central Italy: Methodological Issues and Diachronic Changes. Am. J. Phys. Anthropol. 2008, 135, 284–292. [Google Scholar] [CrossRef]
- Danubio, E.; Martella, M. Sanna Changes in Stature from the Upper Paleolithic to the Medieval Period in Western Europe. J. Anthropol. Sci. Riv. Antropol. JASS 2017, 95, 269–280. [Google Scholar] [CrossRef]
- Edinborough, M.; Rando, C. Stressed Out: Reconsidering Stress in the Study of Archaeological Human Remains. J. Archaeol. Sci. 2020, 121, 105197. [Google Scholar] [CrossRef]
- Beltran, L.S.; Rosenberg, Z.S.; Mayo, J.D.; De Tuesta, M.D.; Martin, O.; Neto, L.P.; Bencardino, J.T. Imaging Evaluation of Developmental Hip Dysplasia in the Young Adult. Am. J. Roentgenol. 2013, 200, 1077–1088. [Google Scholar] [CrossRef]
- Binder, H.; Schurz, M.; Aldrian, S.; Fialka, C.; Vécsei, V. Physeal Injuries of the Proximal Humerus: Long-Term Results in Seventy Two Patients. Int. Orthop. 2011, 35, 1497–1502. [Google Scholar] [CrossRef]
- Murphy, S.B.; Ganz, R.; Müller, M.E. The Prognosis in Untreated Dysplasia of the Hip. A Study of Radiographic Factors That Predict the Outcome. J. Bone Joint Surg. Am. 1995, 77, 985–989. [Google Scholar] [CrossRef]
- Wedge, J.H.; Wasylenko, M.J. The Natural History of Congenital Dislocation of the Hip: A Critical Review. Clin. Orthop. 1978, 137, 154–162. [Google Scholar] [CrossRef]
- Momodu, I.I.; Savaliya, V. Septic Arthritis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Saraf, S.K.; Tuli, S.M. Tuberculosis of Hip: A Current Concept Review. Indian J. Orthop. 2015, 49, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.; Burroughs, K.E. Legg-Calve-Perthes Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Pountney, T.; Green, E.M. Hip Dislocation in Cerebral Palsy. BMJ 2006, 332, 772–775. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Amoah, K.; Raszewski, J.; Duplantier, N.; Waddell, B.S. Dislocation of the Hip: A Review of Types, Causes, and Treatment. Ochsner J. 2018, 18, 242–252. [Google Scholar] [CrossRef]
- Biko, D.M.; Davidson, R.; Pena, A.; Jaramillo, D. Proximal Focal Femoral Deficiency: Evaluation by MR Imaging. Pediatr. Radiol. 2012, 42, 50–56. [Google Scholar] [CrossRef]
- Huser, A.J.; Kwak, Y.H.; Rand, T.J.; Paley, D.; Feldman, D.S. Anatomic Relationship of the Femoral Neurovascular Bundle in Patients with Congenital Femoral Deficiency. J. Pediatr. Orthop. 2021, 41, e111–e115. [Google Scholar] [CrossRef]
- Jarraya, M.; Hayashi, D.; Roemer, F.W.; Crema, M.D.; Diaz, L.; Conlin, J.; Marra, M.D.; Jomaah, N.; Guermazi, A. Radiographically Occult and Subtle Fractures: A Pictorial Review. Radiol. Res. Pract. 2013, 2013, e370169. [Google Scholar] [CrossRef]
- Park, J.-M.; Im, G.-I. The Correlations of the Radiological Parameters of Hip Dysplasia and Proximal Femoral Deformity in Clinically Normal Hips of a Korean Population. Clin. Orthop. Surg. 2011, 3, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Berritto, D.; Russo, A.; Riccitiello, F.; Caruso, M.; Paola Belfiore, M.; Roberto Papapietro, V.; Carotti, M.; Pinto, F.; Giovagnoni, A.; et al. Traumatic Fractures in Adults: Missed Diagnosis on Plain Radiographs in the Emergency Department. Acta Bio Medica Atenei Parm. 2018, 89, 111–123. [Google Scholar] [CrossRef]
- Subbarao, K. Proximal Femoral Focal Deficiency (PFFD). J. Med. Sci. Res. 2015, 3, 90–93. [Google Scholar] [CrossRef]
- Uduma, F.U.; Dim, E.M.; Njeze, N.R. Proximal Femoral Focal Deficiency—A Rare Congenital Entity: Two Case Reports and a Review of the Literature. J. Med. Case Rep. 2020, 14, 27. [Google Scholar] [CrossRef]
- Baumgart, M.; Wiśniewski, M.; Grzonkowska, M.; Badura, M.; Małkowski, B.; Szpinda, M. Quantitative Anatomy of the Primary Ossification Center of the Femoral Shaft in Human Fetuses. Surg. Radiol. Anat. 2017, 39, 1235–1242. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A. Proximal Femoral Growth Disturbance in Developmental Dysplasia of the Hip: What Do We Know? J. Child. Orthop. 2018, 12, 331–341. [Google Scholar] [CrossRef]
- Cheng, R.; Huang, M.; Kernkamp, W.A.; Li, H.; Zhu, Z.; Wang, L.; Tsai, T.-Y. The Severity of Developmental Dysplasia of the Hip Does Not Correlate with the Abnormality in Pelvic Incidence. BMC Musculoskelet. Disord. 2020, 21, 623. [Google Scholar] [CrossRef]
- Dygut, J.; Piwowar, M. Distinction Between Dysplasia, Malformation, and Deformity—Towards the Proper Diagnosis and Treatment of Hip Development Disorders. Diagnostics 2025, 15, 1547. [Google Scholar] [CrossRef]
- Ren, N.; Zhang, Z.; Li, Y.; Zheng, P.; Cheng, H.; Luo, D.; Zhang, J.; Zhang, H. Effect of Hip Dysplasia on the Development of the Femoral Head Growth Plate. Front. Pediatr. 2023, 11, 1247455. [Google Scholar] [CrossRef]
- England, P.; Schaeffer, E.; Price, C.; Mulpuri, K.; Sankar, W.N. Proximal Femoral Growth Alterations Can Be Seen Prior to Treatment of Developmental Dysplasia of the Hip: A Multicenter Cohort Study. J. Pediatr. Orthop. Soc. N. Am. 2024, 5, 669. [Google Scholar] [CrossRef]
- Strayer, L.M. The Embryology of the Human Hip Joint. Yale J. Biol. Med. 1943, 16, 13–26.6. [Google Scholar] [CrossRef]
- Ahmed, M.F.; Ferdous, S.; Azad, A.K. Progressive Pseudo-Rheumatoid Dysplasia: Two Cases in One Family. Mymensingh Med. J. 2020, 29, 734–737. [Google Scholar]
- Lievense, A.M.; Bierma-Zeinstra, S.M.A.; Verhagen, A.P.; Verhaar, J.A.N.; Koes, B.W. Influence of Hip Dysplasia on the Development of Osteoarthritis of the Hip. Ann. Rheum. Dis. 2004, 63, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Nandhagopal, T.; De Cicco, F.L. Developmental Dysplasia of The Hip. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Pone, M.V.d.S.; Gomes da Silva, T.O.; Ribeiro, C.T.M.; de Aguiar, E.B.; Mendes, P.H.B.; Gomes Junior, S.C.D.S.; Hamanaka, T.; Zin, A.A.; Pereira Junior, J.P.; Moreira, M.E.L.; et al. Acquired Hip Dysplasia in Children with Congenital Zika Virus Infection in the First Four Years of Life. Viruses 2022, 14, 2643. [Google Scholar] [CrossRef] [PubMed]
- Trousdale, R.T.; Ganz, R. Posttraumatic Acetabular Dysplasia. Clin. Orthop. 1994, 305, 124–132. [Google Scholar] [CrossRef]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef]
- Pineda, C.; Espinosa, R.; Pena, A. Radiographic Imaging in Osteomyelitis: The Role of Plain Radiography, Computed Tomography, Ultrasonography, Magnetic Resonance Imaging, and Scintigraphy. Semin. Plast. Surg. 2009, 23, 80–89. [Google Scholar] [CrossRef]
- Cooperman, D.R.; Wallensten, R.; Stulberg, S.D. Acetabular Dysplasia in the Adult. Clin. Orthop. Relat. Res. 1983, 175, 79. [Google Scholar] [CrossRef]
- Bakarman, K.; Alsiddiky, A.M.; Zamzam, M.; Alzain, K.O.; Alhuzaimi, F.S.; Rafiq, Z. Developmental Dysplasia of the Hip (DDH): Etiology, Diagnosis, and Management. Cureus 2023, 15, e43207. [Google Scholar] [CrossRef]
- Killen, M.-C.; DeKiewiet, G. Genu Varum in Children. Paediatr. Child Health 2022, 32, 141–150. [Google Scholar] [CrossRef]
- Ferguson, J.; Wainwright, A. Tibial Bowing in Children. Orthop. Trauma 2013, 27, 30–41. [Google Scholar] [CrossRef]
- Bowen, J.R. Developmental Dysplasia of the Hip Book. Available online: https://www.thriftbooks.com/w/developmental-dysplasia-of-the-hip_j-richard-bowen/38321599/ (accessed on 22 November 2023).
- Mitchell, P.D.; Redfern, R.C. The Prevalence of Dislocation in Developmental Dysplasia of the Hip in Britain over the Past Thousand Years. J. Pediatr. Orthop. 2007, 27, 890–892. [Google Scholar] [CrossRef] [PubMed]
- Mafart, B.; Kéfi, R.; Béraud-Colomb, E. Palaeopathological and Palaeogenetic Study of 13 Cases of Developmental Dysplasia of the Hip with Dislocation in a Historical Population from Southern France. Int. J. Osteoarchaeol. 2007, 17, 26–38. [Google Scholar] [CrossRef]
- Saccheri, P.; Travan, L. The Limping Nuns. Two Cases of Hip Dislocation in a Medieval Female Monastery. Ital. J. Anat. Embryol. 2022, 126, 81–91. [Google Scholar] [CrossRef]
- Traversari, M.; Feletti, F.; Vazzana, A.; Gruppioni, G.; Frelat, M.A. Trois cas de dysplasie développementale de la hanche chez des individus partiellement momifiés (Roccapelago, Modène, 18e siècle): Étude des indicateurs paléopathologiques par analyses directe et virtuelle. BMSAP 2016, 28, 202–212. [Google Scholar] [CrossRef]
- Cesana, D.; Benedictow, O.J.; Bianucci, R. The Origin and Early Spread of the Black Death in Italy: First Evidence of Plague Victims from 14th-Century Liguria (Northern Italy). Anthropol. Sci. 2017, 125, 15–24. [Google Scholar] [CrossRef]
- Piccioli, A.; Gazzaniga, V.; Catalano, P. Bones: Orthopaedic Pathologies in Roman Imperial Age; Softcover Reprint of the Original 1st ed. 2015 Edition; Springer: Berlin/Heidelberg, Germany, 2016; ISBN 978-3-319-36802-3. [Google Scholar]
- Belfiglio, V.J. Orthopedic Surgery in Ancient Roman Military Hospitals: 27 BCE to 476 CE. Int. J. Interdiscip. Cult. Stud. 2023, 18, 81–90. [Google Scholar] [CrossRef]
- Mitchell, P.D.; Redfern, R.C. Brief Communication: Developmental Dysplasia of the Hip in Medieval London. Am. J. Phys. Anthropol. 2011, 144, 479–484. [Google Scholar] [CrossRef]
- Van Sleuwen, B.E.; Engelberts, A.C.; Boere-Boonekamp, M.M.; Kuis, W.; Schulpen, T.W.J.; L’Hoir, M.P. Swaddling: A Systematic Review. Pediatrics 2007, 120, e1097–e1106. [Google Scholar] [CrossRef]
- Laes, C. Infants Between Biological and Social Birth in Antiquity: A Phenomenon of the “Longue Durée”. Hist. Z. Alte Gesch. 2014, 63, 364–383. [Google Scholar] [CrossRef]
- Lawson, A.; Beckett, A.E. The Social and Human Rights Models of Disability: Towards a Complementarity Thesis. Int. J. Hum. Rights 2021, 25, 348–379. [Google Scholar] [CrossRef]
- Bohling, S.; Croucher, K.; Buckberry, J. The Bioarchaeology of Disability: A Population-Scale Approach to Investigating Disability, Physical Impairment, and Care in Archaeological Communities. Int. J. Paleopathol. 2022, 38, 76–94. [Google Scholar] [CrossRef] [PubMed]
- Upson-Saia, K.; Goodey, C.F.; Rose, M.L. Review of Disabilities in Roman Antiquity: Disparate Bodies. A Capite Ad Calcem. Mnemosyne, Supplements, History and Archaeology of Classical Antiquity, 356. Bull. Hist. Med. 2014, 88, 570–572. [Google Scholar]
- Laes, C. Mobility Impairments: History of Pain and Toil. In Disabilities and the Disabled in the Roman World: A Social and Cultural History; Cambridge University Press: Cambridge, UK, 2018; pp. 149–167. ISBN 978-1-107-16290-7. [Google Scholar]
- Munyi, C.W. Past and Present Perceptions Towards Disability: A Historical Perspective. Disabil. Stud. Q. 2012, 32. [Google Scholar] [CrossRef]
- Gismondi, A.; D’Agostino, A.; Di Marco, G.; Scuderi, F.; De Angelis, F.; Rickards, O.; Catalano, P.; Canini, A. Archaeobotanical Record from Dental Calculus of a Roman Individual Affected by Bilateral Temporo-Mandibular Joint Ankylosis. Quat. Int. 2023, 653–654, 82–88. [Google Scholar] [CrossRef]
- López-Chamizo, S. Caring for the Dead, Understanding the Living: Bioarchaeology of Care in a 2nd–3rd Century CE Burial from Roman Malaca. J. Archaeol. Sci. Rep. 2025, 66, 105254. [Google Scholar] [CrossRef]
- Laes, C. Disabilities and the Disabled in the Roman World: A Social and Cultural History; Cambridge University Press: Cambridge, UK, 2018; ISBN 978-1-107-16290-7. [Google Scholar]
- Tilley, L. Theory and Practice in the Bioarchaeology of Care; Bioarchaeology and Social Theory; Springer International Publishing: Cham, Switzerland, 2015; ISBN 978-3-319-18859-1. [Google Scholar]
- Dettwyler, K.A. Can Paleopathology Provide Evidence for “Compassion”? Am. J. Phys. Anthropol. 1991, 84, 375–384. [Google Scholar] [CrossRef]
- Brent, L. Disturbed, Damaged and Disarticulated: Grave Reuse in Roman Italy. Theor. Roman Archaeol. J. 2017, 2016, 37–50. [Google Scholar] [CrossRef]
- Draycott, J. Reconstructing the Lived Experience of Disability in Antiquity: A Case Study from Roman Egypt. Greece Rome 2015, 62, 189–205. [Google Scholar] [CrossRef][Green Version]
- Shrader, M.J. Moving Beyond the Medical Model: Assessing the Bioarchaeology of Disability in the Roman Empire; Texas Tech University Libraries: Lubbock, TX, USA, 2023. [Google Scholar]
- Sáez, R.; Edén Fernández Suárez, M.; David Candela, G.; Andrea Barrio Fioresta, P.; León-Cristóbal, A.; Romero, J.; Velayos Castelo, C. Care in Late Antiquity: Applying the Bioarchaeology of Care Method in the Case of an Unprecedented Pathology in an Individual from Herrera de Pisuerga, Northern Spain. J. Archaeol. Sci. Rep. 2024, 60, 104867. [Google Scholar] [CrossRef]
- Cilione, M.; Gazzaniga, V. Conceptualizing Disabilities from Antiquity to the Middle Ages: A Historical-Medical Contribution. Int. J. Paleopathol. 2023, 40, 41–47. [Google Scholar] [CrossRef]
- Verbruggen, S.W.; Kainz, B.; Shelmerdine, S.C.; Arthurs, O.J.; Hajnal, J.V.; Rutherford, M.A.; Phillips, A.T.M.; Nowlan, N.C. Altered Biomechanical Stimulation of the Developing Hip Joint in Presence of Hip Dysplasia Risk Factors. J. Biomech. 2018, 78, 1–9. [Google Scholar] [CrossRef]
- Haber, C.K.; Sacco, M. Scoliosis: Lower Limb Asymmetries during the Gait Cycle. Arch. Physiother. 2015, 5, 4. [Google Scholar] [CrossRef]
- Rossetti, N.; Fusco, R.; Messina, C.; Vanni, A.; Licata, M. Health and Heritage: The Bioarchaeological Discovery of a Probable Case of Developmental Dysplasia in an Adult Subject. Heritage 2024, 7, 5295–5306. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).