Antenatal Practices Ineffective at Prevention of Plasmodium falciparum Malaria during Pregnancy in a Sub-Saharan Africa Region, Nigeria
Abstract
:1. Introduction
2. Materials and Methods
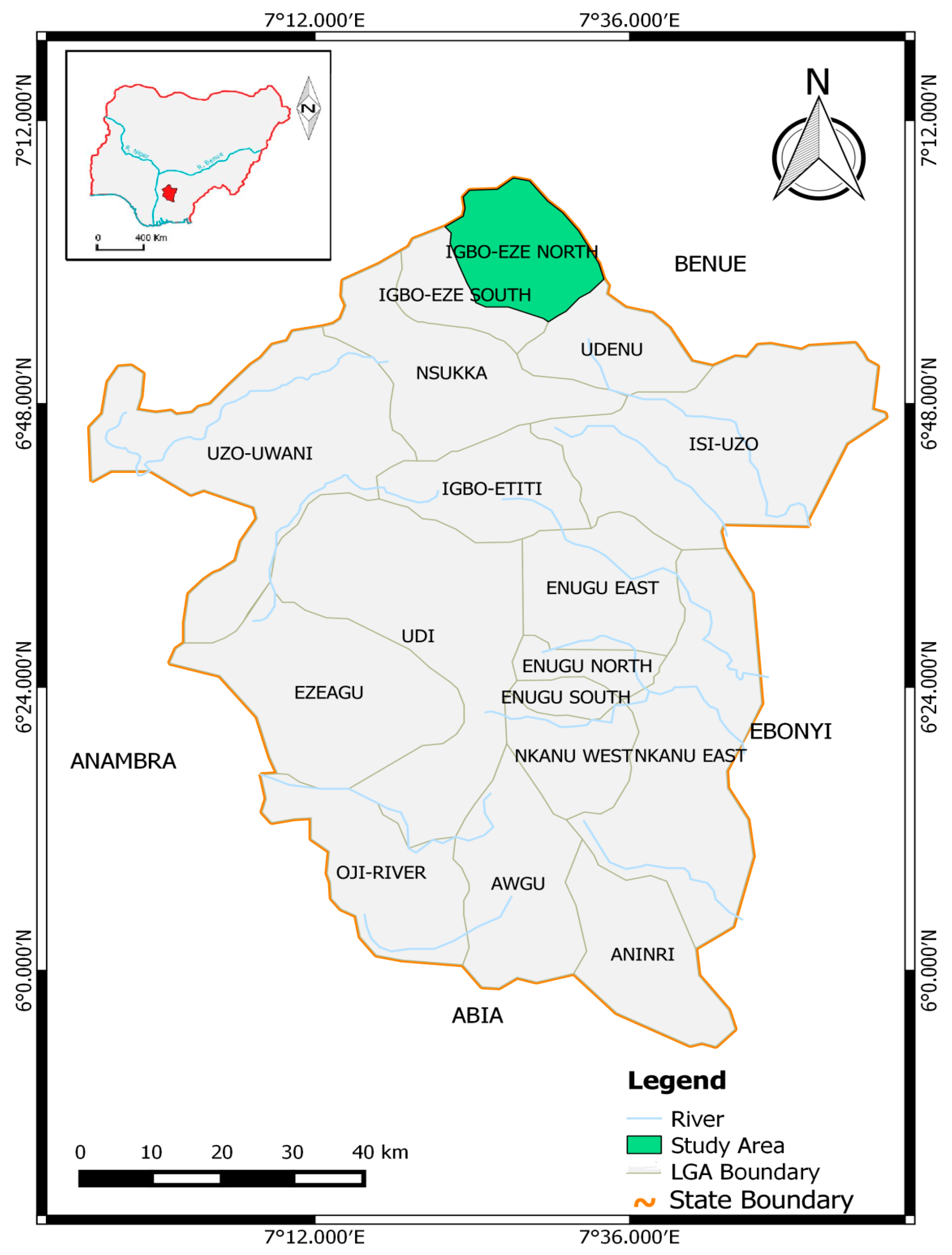
2.1. Study Area
2.2. Study Design and Sample Size
2.3. Ethical Clearance
2.4. Questionnaires
2.5. Malaria Diagnosis
2.6. Statistical Analysis
3. Results
3.1. Prevalence and Density of Pregnancy-Associated Malaria
3.2. Antenatal Visits and Malaria Prevalence
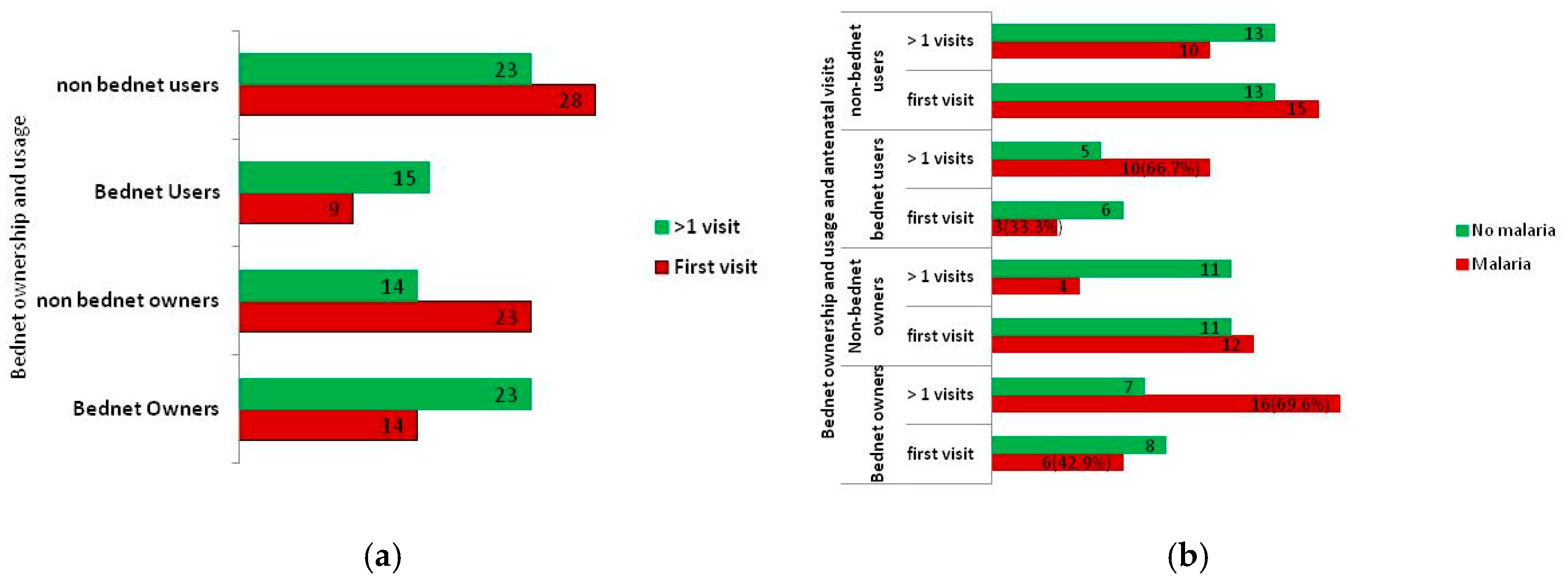
3.3. Mosquito Bed Net Ownership and Usage
3.4. Intermittent Preventive Malaria Chemotherapy
4. Discussion
5. Conclusions
- Sensitization on malaria prevention during the morning antenatal enlightenment class should be introduced;
- Malaria diagnosis during pregnancy should be made routine and carried out at least once every month; and efforts should be made at making it completely free;
- Effort should be made at providing treated mosquito bed nets;
- Finally, antenatal attendees should be enlightened and encouraged to take malaria preventive chemotherapy in accordance with WHO recommendations.
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. WHO Policy Brief for the Implementation of Intermittent Preventive of Malaria in Pregnancy Using Sulfadoxine-Pyrimethamine (IPTp-SP); WHO Global Malaria Programme; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Smereck, J. Malaria in pregnancy: Update on emergency management. J. Emerg. Med. 2011, 40, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Saba, N.; Sultana, A.; Mahsud, I. Outcome and complications of malaria in pregnancy. Gomal J. Med. Sci. 2008, 6, 98–101. [Google Scholar]
- Schantz-Dunn, J.; Nour, N.M. Malaria and pregnancy: A global health perspective. Rev. Obstet. Gynecol. 2009, 2, 186–192. [Google Scholar] [PubMed]
- Ayoola, O.O.; Whatmore, A.; Balogun, W.O.; Jarrett, O.O.; Cruickshank, J.K.; Clayton, P.E. Maternal malaria status and metabolic profile in pregnancy and in cord blood: Relationships with birth size in Nigeria infants. Malar. J. 2012, 11, 75. [Google Scholar] [CrossRef] [PubMed]
- McClure, E.M.; Meshnick, S.R.; Mungai, P.; King, C.L.; Hudgens, M.; Goldberg, R.L.; Siega-Riz, A.-M.; Dent, A.E. A cohort study of Plasmodium falciparum malaria pregnancy and association with uteroplacental blood flow and fetal anthropometric in Kenya. Int. J. Gynecol. Obstet. 2014, 126, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, H.L.; Snow, R.W. Impart of malaria during pregnancy on low birth weight in sub-Saharan Africa. Clin. Microbiol. Rev. 2004, 17, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Brabin, B.J.; Romangosa, C.; Abdelgail, S.; Menends, C.; Verhoeff, F.H.; McGready, R.; Fletcher, K.A.; Owens, S.; D’Alessendro, U.; Nosten, F.; et al. The sick placenta-the role of malaria. Placenta 2004, 25, 359–378. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Malaria: Malaria Fact Sheet No 94. Available online: www.who.int/mediacentre/factsheets/fso94/en/ (accessed on 12 May 2015).
- World Health Organization. Factsheet on World Malaria Report 2013. Available online: www.who.int/malaria/media/worldmalariareport2013/en/ (accessed on 22 January 2015).
- Walker, P.G.T.; Cairns, M. Value of additional chemotherapy for malaria in pregnancy. Lancet Glob. Health 2015, 3, e116–e117. [Google Scholar] [CrossRef]
- Igwenagu, C.M. Trend analysis of rainfall pattern in Enugu State, Nigeria. Eur. J. Stat. Probab. 2015, 3, 12–18. [Google Scholar]
- National Population Commission. 2006 Population and Housing Census Priority Table Volume III: Population Distribution by Sex, State, Local Government Area and Senatorial District (Electronic Version). National Population Commission: Abuja, Nigeria, 2010; p. 53. [Google Scholar]
- National Population Commission. 2006 Population and Housing Census Priority Table Volume IV: Population Distribution by Age and Sex (State and Local Government Area) (Electronic Version). National Population Commission: Abuja, Nigeria, 2010; pp. 125–132. [Google Scholar]
- National Population Commission [Nigeria] and ICF International. Nigeria Demographic and Health Survey 2013; National Population Commission and ICF International: Rockville, MD, USA, 2014; pp. 1–2.
- National Population Commision [Nigeria] and ORC Macro. Nigeria Demographic and Health Survey 2003; National Population Commission and ORC Macro: Calverton, MD, USA, 2004; pp. 1–77.
- Okeibunor, J.C.; Onyenehu, N.G.; Okonofua, F.E. Policy and programs for reducing maternal mortality in Enugu State, Nigeria. Afr. J. Reprod. Health 2010, 14, 19–30. [Google Scholar]
- Centers for Disease Control and Prevention. Laboratory Diagnosis of Malaria: Preparation of Blood Smears. Available online: www.cdc.gov/dpdx/resources/pdf/benchaids/malaria/malariaproceduresbenchaid.pdf (accessed on 11 July 2015).
- World Health Organization. New Perspectives Malaria Diagnosis. In Report of a Joint WHO/USAID Informal Consultation, 25–27 October 1999; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Research Malaria Microscopy Standard Working Group. Microscopy for the Detection, Identification and Quantification of Malarial Parasites on Stained Thick and Thin Films. World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Ivoke, N.; Ivoke, O.N.; Okereke, N.C.; Eyo, J.E. Plasmodium malaria parasitaemia among pregnant women attending clinics in a Guinea-Savannah zone, Southern Ebonyi State, Nigeria. Int. J. Sc. Eng. Res. 2013, 4, 1876–1883. [Google Scholar]
- Adefioye, O.A.; Adeyeba, O.A.; Hassan, W.O.; Oyeniran, O.A. Prevalence of malaria parasite infection among pregnant women in Oshogbo, southwest, Nigeria. Am.-Eurasian J. Sci. Res. 2007, 2, 43–45. [Google Scholar]
- Alaku, I.A.; Abdullahi, A.G.; Kana, H.A. Epidemiology of malaria parasites infection among pregnant women in some part of Nasarawa State, Nigeria. Dev. Ctries. Stud. 2015, 5, 30–33. [Google Scholar]
- Agomo, C.O.; Oyibo, W.A.; Anorlu, R.I.; Agomo, P.U. Prevalence of malaria in pregnant women in Lagos, south-west Nigeria. Korean J. Parasitol. 2009, 47, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, S.W.; Wilkins, H.A.; Zieler, H.A.; Daly, R.J.; Petrarca, V.; Byass, P. Ability of Anopheles gambiae to transmit malaria during the dry and wet seasons in an area of irrigated rice cultivation in the Gambia. J. Trop. Med. Hyg. 1991, 94, 313–324. [Google Scholar]
- Awodu, O.A.; Enosolease, M.E. Seasonal variation of malaria parasitaemia in an urban tropical city. Niger. J. Clin. Pract. 2003, 6, 30–33. [Google Scholar]
- Odongo-Aginya, E.; Ssegwanyi, G.; Kategere, P.; Vuzi, P.C. Relationship between malaria infection and intensity and rainfall pattern in Eastern peninsula, Uganda. Afr. Health Sci. 2005, 5, 238–245. [Google Scholar] [PubMed]
- Pakistan Antimicrobial Resistance Network. Laboratory Diagnosis of Malaria. Available online: www.parn.org.pk/index_files/Laboratory%20Diagnosis%20of%20Malaria.html (accessed on 13 September 2015).
- World Health Organization. Malaria T3: Test. Treat. Track. Scaling up Diagnostic Testing, Treatment and Surveillance for Malaria. Available online: www.who.int/malaria/publications/atoz/t3-brochure/en/ (accessed on 18 May 2015).
- Centers for Disease Control and Prevention. Diagnosis and Treatment of Malaria in the Malaria-Endemic World. Available online: https://www.cdc.gov/malaria/malaria_worldwide/reduction/dx_tx.html (accessed 11 May 2015).
- Chandrasiri, U.P.; Randall, L.M.; Saad, A.A.; Bashir, A.M.; Rogerson, S.J.; Adam, I. Low antibody levels to pregnancy-specific malaria antigens and heightened cytokine response associated with severe malaria in pregnancy. J. Infect. Dis. 2014. [Google Scholar] [CrossRef] [PubMed]
- Fried, M.; Duffy, P.E. Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science 1996, 272, 1502–1504. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.A.; Grevstad, B.; A-Elgadir, T.M.E.; Kurtzhals, J.A.L.; Giha, H.; Staalsoe, T.; Hviid, L.; Theander, T.G. Differential induction of immunoglobulin G to Plasmodium falciparum variant surface antigen during the transmission season in Daraweesh, Sudan. JID 2005, 192, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.J.; Theiler, R.N.; Rasmussen, S.A. Emerg. infections and pregnancy. Emerging Infect. Dis. 2006, 12, 1638–1643. [Google Scholar] [CrossRef] [PubMed]
- Maestre, A.; Carmona-Fonseca, J. Immune response during gestational malaria: A review of the current knowledge and future trend of research. J. Infect. Dev. Ctries. 2014, 8, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Shimaoka, Y.; Hidaka, Y.; Tada, H.; Nakamura, T.; Mitsuda, N.; Morimoto, Y.; Murata, Y.; Amino, N. Changes in cytokine production during and after normal pregnancy. Immunology 2000, 44, 143–147. [Google Scholar] [CrossRef]
- Sykes, L.; MacIntyre, D.A.; Yap, X.J.; Ponnampalam, S.; Taoh, T.G.; Bennett, P.R. Changes in the Th1: Th2 cytokine bias in pregnancy and the effects of the anti-inflammatory cyclopentanone prostaglandin 15-deoxy-Δ12,14-prostagladin J2. Mediat. Inflamm. 2012, 2012, 416739. [Google Scholar] [CrossRef] [PubMed]
- Moreau, E.; Chauvin, A. Immunity against helminthes: Interactions with the host and the incurrent infections. J. Biomed. Biotechnol. 2010, 2010, 428593. [Google Scholar] [CrossRef]
| No. Examined (%) | No. Infected (%) * | Parasite Density (/µL) × 103 | ||
|---|---|---|---|---|
| Within Obstetric | Within Malaria | |||
| Gravidity | ||||
| Primi | 21 (28.0) | 8 (38.1) | (21.1) | 268.13 ± 58.23 a |
| Secundi | 14 (18.7) | 7 (50.0) | (18.4) | 92.14 ± 4.72 ab |
| Multi | 40 (53.3) | 23 (57.5) | (60.5) | 65.22 ± 20.17 b |
| Total | 75 (100) | 38 (50.7) | (100) χ2 = 2.078, p = 0.354 | 112.89 ± 22.90 |
| Parity | ||||
| Nulli | 26 (34.7) | 12 (46.2) | (31.6) | 225.00 ± 48.25 a |
| Primi | 10 (13.3) | 4 (40.0) | (10.5) | 26.25 ± 8.26 b |
| Multi | 39 (52.0) | 22 (56.4) | (57.9) | 67.50 ± 20.97 b |
| Total | 75 (100) | 38 (50.7) | (100) χ2 = 1.182, p = 0.554 | 112.89 ± 22.90 |
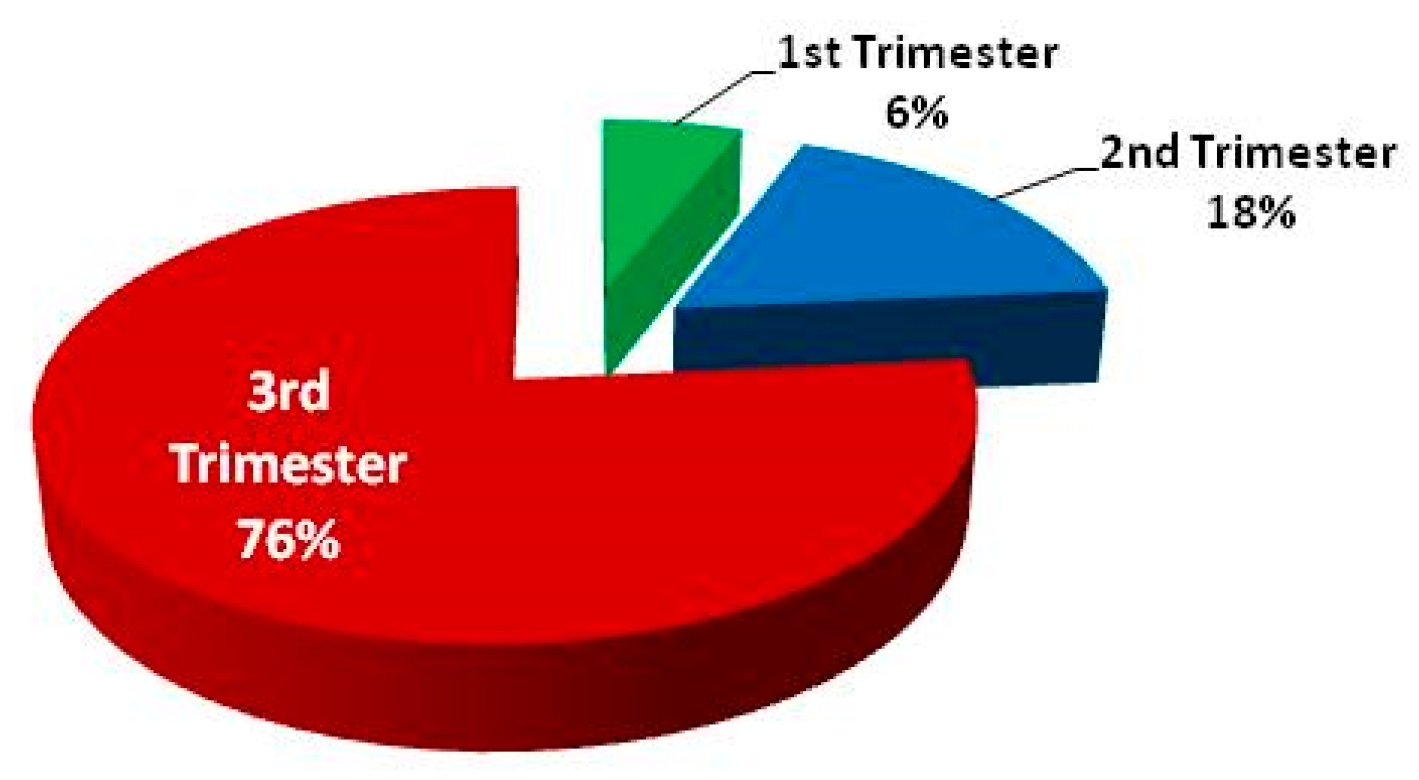
| Trimester | ||||
| 2nd | 34 (46.6) | 13 (38.2) | (36.1) | 105.77 ± 39.02 |
| 3rd | 39 (53.4) | 23 (59.0) | (63.9) | 125.65 ± 30.65 |
| Total | 73 (100) | 36 (49.3) | (100) χ2 = 3.126, p = 0.077 | 118.19 ± 23.87 |
| Age (Year) | ||||
| < 20 | 9 (12.0) | 2 (22.2) | (5.3) | 415.00±15.00 |
| 20–29 | 34 (45.3) | 18 (52.9) | (47.4) | 133.61±37.21 |
| 30–39 | 32 (42.7) | 18 (56.2) | (47.4) | 58.61±15.12 |
| Total | 75 (100) | 38 (50.7) | (100) χ2 = 3.383, p = 0.184 | 112.89±22.90 |
| BMI (kg/m2) | ||||
| 18.5–24.9 | 22 (29.3) | 11 (50.0) | (28.9) | 174.54 ± 6.11 |
| 25.0–29.9 | 34 (45.3) | 18 (52.9) | (47.4) | 94.72 ± 23.61 |
| ≥ 30 | 19 (25.3) | 9 (47.4) | (23.7) | 73.89 ± 36.19 |
| Total | 75 (100) | 38 (50.7) | (100) χ2 = 0.157, p = 0.925 | 112.89 ± 22.90 |
| Antenatal Visits | No. Examined (%) | No. Infected (%) | Parasite Density (/µL) × 103 |
|---|---|---|---|
| First | 37 (49.3) | 18 (48.6) | 75.28 ± 28.74 |
| More than one | 38 (50.7) | 20 (52.6) | 146.75 ± 33.86 |
| χ2 = 0.119, p = 0.730 |
| No. Examined (%) | Bed Net Owner (%) | Bed Net Users (%) | |
|---|---|---|---|
| Gravidity | |||
| Primi | 21 (28.0) | 8 (38.1) | 5 (23.8) |
| Secundi | 14 (18.7) | 6 (42.9) | 3 (21.4) |
| Multi | 40 (53.3) | 23 (57.5) | 16 (40.0) |
| Total | 75 (100) | 37 (49.3) | 24 (32.0) |
| χ2 = 2.363, p = 0.307 | χ2 = 2.543, p= 0.280 | ||
| Parity | |||
| Nulli | 26 (34.7) | 10 (38.5) | 5 (19.2) |
| Primi | 10 (13.3) | 5 (50.0) | 4 (40.0) |
| Multi | 39 (52.0) | 22 (56.4) | 15 (38.5) |
| Total | 75 (100) | 37 (49.3) | 24 (32.0) |
| χ2 = 2.013, p = 0.366 | χ2 = 2.991, p = 0.224 | ||
| Trimester | |||
| 2nd | 34 (46.6) | 11 (32.4) | 9 (26.5) |
| 3rd | 39 (53.4) | 24 (61.5) | 14 (35.9) |
| Total | 73 (100) | 35 (47.9) | 23 (31.5) |
| χ2 = 6.199, p = 0.013 | χ2 = 0.748, p = 0.387 | ||
| Age group (year) | |||
| < 20 | 9 (12.0) | 1 (11.1) | 1 (11.1) |
| 20–29 | 34 (45.3) | 17 (50.0) | 10 (29.4) |
| 30–39 | 32 (42.7) | 19 (59.4) | 13 (40.6) |
| Total | 75 (100) | 37 (49.3) | 24 (32.0) |
| χ2 = 6.557, p = 0.038 | χ2 = 3.003, p = 0.223 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguzie, I.O.N.; Ivoke, N.; Onyishi, G.C.; Okoye, I.C. Antenatal Practices Ineffective at Prevention of Plasmodium falciparum Malaria during Pregnancy in a Sub-Saharan Africa Region, Nigeria. Trop. Med. Infect. Dis. 2017, 2, 15. https://doi.org/10.3390/tropicalmed2020015
Aguzie ION, Ivoke N, Onyishi GC, Okoye IC. Antenatal Practices Ineffective at Prevention of Plasmodium falciparum Malaria during Pregnancy in a Sub-Saharan Africa Region, Nigeria. Tropical Medicine and Infectious Disease. 2017; 2(2):15. https://doi.org/10.3390/tropicalmed2020015
Chicago/Turabian StyleAguzie, Ifeanyi Oscar Ndimkaoha, Njoku Ivoke, Grace C. Onyishi, and Ikem C. Okoye. 2017. "Antenatal Practices Ineffective at Prevention of Plasmodium falciparum Malaria during Pregnancy in a Sub-Saharan Africa Region, Nigeria" Tropical Medicine and Infectious Disease 2, no. 2: 15. https://doi.org/10.3390/tropicalmed2020015
APA StyleAguzie, I. O. N., Ivoke, N., Onyishi, G. C., & Okoye, I. C. (2017). Antenatal Practices Ineffective at Prevention of Plasmodium falciparum Malaria during Pregnancy in a Sub-Saharan Africa Region, Nigeria. Tropical Medicine and Infectious Disease, 2(2), 15. https://doi.org/10.3390/tropicalmed2020015





