Abstract
Prolonged sitting (PS) in the workplace has been linked to a higher risk of developing non-communicable chronic diseases. Simultaneously, an elevated waist-to-height ratio (WHtR) is considered a reliable measure of increased risk for the same condition. The main objective of this research was to examine the relationship between workplace PS and increased WHtR among male workers from the Spanish region of Castilla y León. The secondary objective was to assess how age affects elevated WHtR in workers. This retrospective observational study was carried out in accordance with the STROBE guidelines. The sample included 85,670 male workers, categorized by job type (with or without PS) and age (<40 years or ≥40 years). Chi-square test (X2), Pearson correlation coefficients, and odd ratios (OR) were used to analyze associations. Among workers with PS, X2 = 0.73 (p = 0.391) and 1.11 (p = 0.292) were reported, and among those without PS, X2 = 0.86 (p = 0.354) and 1.24 (p = 0.265), for the years 2022 and 2023, respectively. Therefore, there was no significant association between workers with or without PS and an elevated WHtR, both in those younger than and older than 40 years of age. Advanced age (≥40 years) showed a significant association with increased WHtR (p < 0.01; OR = 2.6). However, no statistical association was observed between PS and elevated WHtR (p > 0.05; OR = 1.15). These findings suggest that age plays a more prominent role than occupational PS time in WHtR among male workers. Future studies should consider other factors, including physical activity and dietary habits, that could affect WHtR.
1. Introduction
Prolonged sitting (PS) is a common feature in numerous job positions, particularly in occupations that require the continuous use of display screen equipment or professional driving [,]. Occupational PS is defined as remaining seated for more than four consecutive hours during each workday []. In developed countries, it is estimated that, on average, an employee spends between 75% and 85% of their working day seated []. PS has been linked to an increased risk of manifesting chronic non-communicable conditions, including type 2 diabetes mellitus, arterial hypertension, obesity, dyslipidemias, and cardiovascular diseases [,,]. The chronic diseases related to PS are connected to a greater risk of premature mortality []. Moreover, occupational PS has been associated with a poorer self-perception of health status among workers []. This link has aroused growing interest in incorporating the assessment and control of PS into official occupational health surveillance protocols [,]. These protocols are applied in the periodic health examinations carried out on workers with the aim of identifying specific risks associated with each job position [,].
One of the most commonly used anthropometric variables to assess cardiometabolic risk (CMR) is the waist-to-height ratio (WHtR) [,,]. WHtR is obtained by dividing the waist circumference (cm) by the height (cm), and it is considered elevated when it exceeds the threshold value of 0.5 [,,]. The use of WHtR has been recommended due to its simplicity, low cost, and greater reliability compared to other indicators, such as body mass index (BMI) [,,]. Although BMI remains the most commonly applied indicator, it presents significant limitations. It does not distinguish the source of weight (whether fat or muscle), and does not allow differentiation between peripheral obesity and central obesity [,,]. A study determined that 33.1% of men and 51.9% of women with a BMI within the normal range presented abdominal obesity or central obesity []. Moreover, individuals presenting central obesity but a normal BMI have been shown to face a greater risk of developing cardiometabolic conditions than those with elevated BMI yet without central obesity []. In this context, other more reliable indicators such as WHtR are emerging to assess central obesity []. Previous publications propose that an elevated WHtR correlates with an increased risk of disorders including type 2 diabetes, arterial hypertension, obesity, dyslipidemias, acute myocardial infarction, or ischemic stroke [,,,]. Thus, the WHtR is a better predictor than the BMI, especially because its better accounts for the health risks of central abdominal fat, even in people with a healthy BMI [].
In this scenario, the working population becomes a particularly vulnerable group to the increase in WHtR, since, as mentioned above, a large part of their active hours are spent in sedentary occupations [,,]. The World Health Organization (WHO) has emphasized the importance of physical activity in the workplace and recommends implementing measures aimed at reducing PS time []. Although the cardiometabolic risks associated with PS are well documented [,,,,,,], specific evidence on its influence on WHtR remains limited. At the same time, adulthood has been recognized as a stage that significantly elevates CMR [,,,,]. Specifically, it is necessary for Spanish male workers due to the high prevalence of obesity and associated health risks, such as metabolic syndrome, in this population. Understanding this relationship can help inform targeted public health interventions and workplace strategies to combat sedentary lifestyles, reduce health risks, and improve overall well-being in this specific group. The relationship between occupational sedentary behavior, age, and waist-to-height ratio is a key indicator for assessing health risk in this population. Understanding the interaction between age, occupational PS, and elevated WHtR is essential to guide preventive measures and design occupational health promotion strategies tailored to different age groups and types of job positions. This study aimed to assess the prevalence of elevated WHtR in male workers from the region of Castilla y León (Spain) performing tasks involving PS, compared with those in non-sedentary positions, during the years 2022 and 2023. As a secondary objective, the influence of age on the increase in WHtR was examined. The present research intends to establish the basis for future investigation and contribute to the design of effective health promotion interventions in the workplace.
2. Materials and Methods
2.1. Design
A retrospective observational study was carried out in accordance with “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) guidelines (Appendix A) [] The relationship between WHtR values, PS in the workplace, and age was analyzed in male workers. This study will focus specifically on male workers from the Spanish Autonomous Community of Castilla y León. Castilla y León is representative of the Spanish region located in the northwest of the Iberian Peninsula. Castilla y León is Spain’s largest region by area and one of the largest in the European Union, with a population of approximately 2.4 million inhabitants as of 2023. This region is administratively identified as the “Autonomous Community” of Castile and León by the Spanish government. This study was carried out in collaboration with Quirón Prevención, which provided the data from the health examinations conducted on its workers in 2022 and 2023.
2.2. Legal and Ethical Considerations
The Clinical Research Ethics Committee (CEIC) of the University of León, Spain approved this study (REF: ETICA-ULE-17-2022). All workers belonged to the mutual health insurance company “Quirón Prevención,” S.L.U. which is responsible for health assessments. For this reason, this study was also authorized by Director of the Occupational Health Area of “Quirón Prevención” S.L.U. on 4 October 2024. The study was conducted in accordance with the Declaration of Helsinki (2008) and its Fortaleza update (2013) []. All participants signed informed consent individually, which required the researchers to provide them with all relevant information in a clear and understandable manner before they agreed to participate in the study. This process, which must be voluntary and free of coercion, is an ethical and legal requirement to ensure that the participant makes an informed and autonomous decision about their participation.
2.3. Participants
The study participants were male workers aged 18–70 years. Recruitment was carried out in January 2025 using data from the 2022 and 2023 health examinations provided by Quirón Prevención. All employees had undergone a mandatory health assessment to determine their fitness for duty or to identify any health issues that could affect their work, thus ensuring compliance with the health and safety regulations of the Spanish Ministry of Labor. These health checks are standardized by Spanish law. Participants were included if (i) active workers ≥ 18 years; (ii) male; (iii) availability of information on age, job position, and WHtR. Participants were excluded if (i) they had musculoskeletal injuries that required job adaptations resulting in spending more hours seated; (ii) they did not provide informed consent.
Out of a total of 85,913 participants, 243 were excluded. A total of 127 subjects did not provide informed consent, 40 were under 18 years of age, and complete data on age, job position, and WHtR were not obtained for 76. The final sample consisted of 85,670 participants (Figure 1). Participants were categorized into two groups based on their job position: (i) workers with prolonged sitting (those whose job positions require remaining seated for more than four consecutive hours per day [], such as display screen equipment workers and drivers [,]); (ii) other job positions (workers who remain seated for less than four consecutive hours per day). In parallel, participants were assigned to two groups according to age: workers under 40 years and workers aged 40 years or older (Figure 1). Age 40 was chosen as a logical categorization point for employee health, as it is an age at which the cumulative effects of a sedentary lifestyle become significant enough to substantially increase the risk of chronic disease [,,]. Also, The choice of the age 40 cutoff is based on the international guidelines such as: USPSTF [] and CTFPHC [], which recommend including cardiometabolic risk assessment in periodic health examinations for healthy, active individuals starting at age 40.
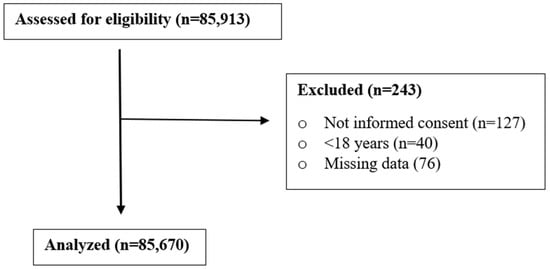
Figure 1.
Flow diagram of the participants recruited according to the STROBE guidelines [].
2.4. Data Collection
Three researchers (A.A.S., G.S.G., and D.F.-L.) examined the health examinations provided by Quirón Prevención. The following information was extracted from each examination: age, job position, occupational risk protocols, abdominal circumference, and height (anthropometric measurements necessary to calculate WHtR). Height was measured with a stadiometer, and abdominal circumference with a measuring tape. All data was compiled in an Excel spreadsheet for subsequent statistical analysis.
The study’s independent variables were age (<40 years; ≥40 years) and type of job position (with PS; without PS). The dependent variable was WHtR, categorized as normal (≤0.5) and elevated (>0.5), according to the criteria established in previous studies [,,].
2.5. Statistical Analysis
Data collected from the study participants were coded in Excel spreadsheets and then exported for analysis to the software “Statistical Package for Social Sciences” (SPSS) version 26.0 for Windows (IBM SPSS Statistics 2019). The characteristics of the sample were described using percentages. Associations between WHtR, age, and job position were assessed using the chi-square test and Pearson’s Correlation coefficient. The odds ratio was used to analyze whether having job positions with PS and older age (≥40 years) represented a risk factor for elevated WHtR. Results with p-values less than 0.05 were considered statistically significant.
3. Results
3.1. Sample Description
The data related to age, WHtR, and type of job position in the sample are presented in Table 1. The workers’ data were divided according to the years of collection, 2022 and 2023. Starting with 2022, 37.9% (n = 14,454) of the workers were under 40 years old. Elevated WHtR was observed in 32.8% (n = 4749) of workers under 40 years and in 62.5% (n = 14,837) of workers aged 40 years or older. Among workers with elevated WHtR, 22.4% (n = 1065) of those under 40 years and 23.8% (n = 3534) of those aged 40 years or older held job positions with PS. In 2023, 36.7% (n = 17,431) of the workers analyzed were under 40 years old. Elevated WHtR was found in 34.7% (n = 6047) of workers under 40 years and in 63.5% (n = 19,078) of those aged 40 years or older. Among workers under 40 years with elevated WHtR, 24.2% (n = 1464) held positions with PS, while in those aged 40 years or older the proportion was 25.1% (n = 4794).

Table 1.
Sample description.
3.2. Relationship Between Prolonged Sitting, Age, and Waist-to-Height Ratio
To determine if elevated WHtR was significantly associated with occupational PS, the chi-square test was applied (Table 2). In 2022, among workers with PS, the chi-square test showed a value of X2 = 0.73 (p = 0.391), and among those without PS, a value of X2 = 0.86 (p = 0.354). Similarly, in 2023, the X2 value was 1.11 (p = 0.292) for workers with PS and 1.24 (p = 0.265) for workers without PS. These results suggest no significant relationship between workers with or without PS and elevated WHtR, both in those under and over 40 years of age.

Table 2.
Chi-square test for the association between elevated waist-to-height ratio and prolonged sitting.
Alternatively, Pearson’s correlation coefficient (Table 3) revealed a strong positive association between age and WHtR in both 2022 (r = 0.62) and 2023 (r = 0.64). In contrast, the correlation between PS and WHtR was weakly positive, with values of r = 0.15 in 2022 and r = 0.17 in 2023. These results indicate that although both age and PS are associated with WHtR, the magnitude of the association is substantially greater for age.

Table 3.
Pearson’s correlation coefficient for the association between waist-to-height ratio, age, and prolonged sitting.
To assess the effect of age and PS on the likelihood of presenting an elevated WHtR, a logistic regression analysis was performed (Table 4), allowing the association to be adjusted for potential confounding factors. The results showed that workers over 40 years had a significantly higher risk of having an elevated WHtR, with an OR of 2.5 in 2022 and 2.6 in 2023 (p < 0.01 in both periods). In contrast, PS was not significantly associated with elevated WHtR, showing an OR of 1.15 in 2022 (p = 0.42) and 1.18 in 2023 (p = 0.39). These findings indicate that age is a risk factor for elevated WHtR, whereas PS does not increase this probability.

Table 4.
Odds ratio of age and prolonged sitting for elevated waist-to-height ratio.
4. Discussion
After analyzing 85,670 workers, it was observed that the presence of elevated WHtR is significantly associated (p < 0.01) with workers’ age, while no clear association was found between WHtR and PS in the workplace. These results suggest that, in the working population, age may have a greater influence on CMR than PS in the workplace.
With regard to age, the findings of this study are in agreement with previous research, which identifies aging as a key factor in the increase in visceral fat and CMR [,,]. As age advances, physiological changes occur that favor the accumulation of abdominal fat. Among them, the progressive decrease in basal metabolic rate stands out, which is related to the loss of muscle mass and reduced efficiency in energy utilization []. The decrease in energy expenditure facilitates fat accumulation even without significant changes in lifestyle []. In parallel, with age adipose tissue is redistributed, resulting in a lower proportion of subcutaneous fat and a higher proportion of visceral fat [,,,]. While subcutaneous fat appears to exert a protective effect against type 2 diabetes mellitus, insulin resistance, and cardiovascular diseases, excess visceral fat significantly increases the risk of these conditions [,,]. Therefore, the rise in visceral fat and the reduction in subcutaneous fat during aging could determine an increase in CMR [].
Another key element is the phenomenon known as inflammaging, marked by a low-grade chronic inflammation during aging [,]. It is characterized by an increase in inflammatory biomarkers, particularly interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) []. Visceral fat contributes to this pro-inflammatory environment by releasing these two mediators and adipokines [], which in turn promote insulin resistance, impair mitochondrial function, and favor atherogenesis [,,]. In this way, inflammation and visceral fat maintain a bidirectional relationship: the accumulation of visceral fat enhances the inflammatory response [], whereas the inflammatory state facilitates visceral fat deposition by inhibiting lipolysis []. In addition, TNF-α hinders the replication and differentiation of preadipocytes, which reduces subcutaneous fat and reinforces the predominance of visceral fat [,].
Age-related hormonal changes, including decreased testosterone in men and reduced estrogen in women, promote visceral fat accumulation and muscle mass loss, increasing the fat-muscle ratio in the body []. This process is enhanced by the progressive reduction in physical activity levels in adulthood [,]. The result is a vicious circle in which functional capacity and energy expenditure decrease, while visceral fat accumulation and CMR increase []. In this context, BMI may provide a distorted view of CMR. As mentioned in the introduction, BMI does not distinguish between muscle mass and fat, nor does it provide information about the location of fat tissue (visceral or subcutaneous) [,]. It is common for older adults with sarcopenia to present normal BMI values despite having an excess of visceral fat and the consequent CMR []. In the adult population, WHtR is a more sensitive and specific indicator to identify central obesity and CMR [,]. WHtR directly reflects the accumulation of abdominal fat, regardless of variations in muscle mass. It has been observed that WHtR predicts the onset of type 2 diabetes mellitus, arterial hypertension, cardiovascular diseases, dyslipidemias, and metabolic syndrome better than BMI [,,,]. For all the above, the systematic monitoring of WHtR should be considered a priority tool in occupational health prevention and promotion programs, especially in workers over 40 years of age.
On the other hand, PS constitutes a widely studied risk factor linked to the development of obesity and cardiometabolic diseases [,,,,,]. Specifically, 71% of people with obesity have a sedentary behavior [] and physical inactivity accounts for approximately 30% of ischemic heart diseases and 27% of diabetes cases []. Despite this, our study did not reveal a significant link between WHtR and occupational PS. We defined occupational PS as remaining seated for more than 4 consecutive hours during the workday. The lack of results could be due to the fact that this definition of occupational PS does not allow for precise knowledge of the actual sitting time of the workers. Total daily sitting time was not considered, as hours of sitting outside the workplace were not analyzed. It is possible that the workers in our sample compensated for sitting time at work with physical activity outside working hours. In fact, the scientific literature states that the negative effects of PS at work progressively decrease in physically active individuals and are completely overcome in those who perform 60–75 min of moderate-to-vigorous physical activity daily []. Therefore, it is possible that a high level of physical activity outside of work neutralized the negative effects of occupational PS on WHtR.
The scientific evidence analyzing the role of PS on WHtR is still very limited. To our knowledge, only three studies evaluated this relationship [,,]. The three studies have taken into account total sitting time, both inside and outside the workplace, unlike us who focused exclusively on occupational PS. Phaswana et al. [] and Mirzaei et al. [] found that sitting for over 10 h per day significantly augmented the risk of presenting an elevated WHtR. Specifically, Mirzaei et al. [] reported an OR of 1.8, whereas sitting between 1 and 3 h per day appears to be a protective factor (OR = 0.5) []. These results suggest that the total amount of sitting time is decisive for the increase in visceral fat. In contrast, Wanner et al. [] did not show a relationship between total sitting time and WHtR. In this study, it was observed that participants who engaged in physical activity during their leisure time had significantly lower WHtR values, regardless of daily sitting time []. This supports the hypothesis formulated in the previous paragraph, namely that physical activity performed outside of work can neutralize the harmful effects of occupational PS.
Other studies have evaluated occupational PS exclusively, as we did. However, they analyzed parameters such as BMI or waist circumference without considering WHtR [,]. Hirata et al. [] they found that truck drivers had a mean BMI of 27.2 kg/m2, considered overweight, and that 18.8% of the participants had an elevated waist circumference. It has been observed that this group spends 13 h sitting per day on workdays and 8 h on non-workdays []. This could partly explain the differences observed compared to our results, since in our study PS was defined as starting from 4 h. In addition, this study did not take into account other determining factors for the increase in visceral fat, such as age. On the other hand, Van Uffelen et al. [] conducted a systematic review finding contradictory results. Five studies found a positive relationship between occupational PS and increased BMI, while another five observed no association []. This lack of consensus is probably due to variability in the definition of PS. In summary, the available scientific literature suggests that the impact of occupational PS alone on WHtR is uncertain and may be conditioned by total daily sitting time and, above all, by physical activity performed outside working hours. Future research are necessary to assess the effect of PS both inside and outside the workplace on WHtR and CMR, analyzing variables that may have an influence such as physical activity, diet, or sleep quality.
4.1. Practical Applications
Taking all the above into account, it is recommended to monitor WHtR in the field of occupational health, highlighting the importance of doing so especially in workers over 40 years of age due to its relevance for occupational safety. From this age onward, recommendations aimed at promoting a healthy lifestyle should be reinforced: engaging in regular physical activity, following a balanced diet, ensuring adequate nighttime rest, and eliminating alcohol and tobacco consumption [,,,]. Observations indicate that over 50% of the general population fail to meet the WHO’s weekly recommendations for physical activity (150 min of moderate and 75 min of vigorous activity) []. In addition, a study stated that, on average, adults spend more than half of their waking time sitting []. Therefore, although in our study occupational PS was not associated with an increase in WHtR, it is still recommended to adopt occupational risk prevention measures to reduce sitting time at work, given its relevance for occupational safety. Some of the proposed preventive measures are: (i) remain seated for less than 50% of the working day, (ii) avoid sitting for long periods by standing up at least once every 20–30 min, (iii) stand for at least 10 min after sitting for 2 h, (iv) avoid sitting more than 5 h per day, and (v) change position while sitting []. It should not be overlooked that occupational PS also entails other health risks, particularly musculoskeletal ones such as low back pain or neck stiffness [,]. It has also been linked with mental health problems, decreased concentration, and an increased number of errors [,]. Therefore, PS is crucial for occupational safety as it negatively impacts workers’ quality of life and their work productivity [].
In Spain, occupational risk monitoring is the responsibility of the Labor and Social Security Inspectorate and the Health and Safety Committees in companies with more than 50 employees. These committees could implement prevention plans, including strategies we have described to mitigate risks such as sedentary workplace behavior, through measures such as health monitoring, promoting healthy habits, and assessing psychosocial risks. Generally, in Spain, I could suggest official policies that promote a less sedentary culture: (i) offer flexible schedules: adjust schedules to dedicate time to physical activity; (ii) mandatory “reinforcement breaks,” i.e., group/individual breaks of 10 to 15 min for movement during the workday, scheduled by a health sciences or occupational medicine professional; (iii) organize active meetings, with activities such as walking or creating specific meeting areas that allow for this; (iv) provide height-adjustable desks or exercise equipment to incorporate movement into their daily tasks [].
4.2. Limitations and Strengths
This study has certain limitations that should be taken into account when interpreting the results. Only PS time at work was analyzed, without considering hours of PS outside the workplace. Since total daily sitting time may significantly influence WHtR, this omission could have conditioned the results. Second, relevant variables that could act as confounding factors, such as dietary habits or physical activity, were not collected. In addition, the sample consisted exclusively of men, despite obesity having a higher prevalence in women [], which limits the extrapolation of the findings to the entire working population. Finally, the use of data from different medical teams could have increased inter-examiner variability. Nevertheless, the recommendations of the STROBE guidelines were followed, and a large, representative cohort of the male employees, consisting of 85,670 participants, was included.
5. Conclusions
After analyzing 85,670 male workers, it was observed that the increase in WHtR is significantly associated with older age. However, no clear association was found between WHtR and PS in the workplace. This may be explained by the fact that physical activity outside of work may neutralize the negative effects of occupational PS. Future studies are needed to analyze the effects of PS both inside and outside the workplace on WHtR and how physical activity influences it.
Author Contributions
Conceptualization, D.F.-L. and J.S.-C.; methodology, A.d.A.S., G.S. and D.F.-L.; software, A.d.A.S. and D.F.-L.; validation, G.S., R.C.M., Á.L.-L., E.J.-C., L.M.C. and D.F.-L.; formal analysis, A.d.A.S., J.S.-C., L.M.C., R.C.M. and D.F.-L.; investigation, A.d.A.S., E.J.-C., G.S., D.F.-L. and J.S.-C.; project administration, J.S.-C., R.C.M., D.F.-L. and L.M.C.; funding acquisition, J.S.-C. and D.F.-L. Writing—original draft, G.S. and D.F.-L.; prepared figures and/or tables, D.F.-L. and G.S.; Writing—revision, A.d.A.S., G.S. and D.F.-L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Department of Education of the Junta de Castilla & León and the European Regional Development Fund (ERDF) under the TCUE Plan 2023–2027 (grant no. 067/230003). The principal investigator was Diego Fernández-Lázaro.
Institutional Review Board Statement
The study was approved by the Clinical Research Ethics Committee (CEIC) of the University of León (Ref: ETHICS-ULE-017-2022). All subjects provided written informed consent in accordance with the Declaration of Helsinki and the 2013 Fortaleza revision.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Data Availability Statement
Data supporting the findings of this study are available within the paper.
Acknowledgments
The authors wish to thank the Spain Conference of Deans of Physiotherapy Faculties and Physiotherapy Department, Institute of Biomedicine (IBIOMED), University of León (León, Spain) for their support in advising on the methodological design and result interpretation.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
STROBE Statement-Checklist of Items That Should Be Included in Reports of Cross-Sectional Studies.
Table A1.
STROBE Statement-Checklist of Items That Should Be Included in Reports of Cross-Sectional Studies.
| Item Nº | Recommendation | |
|---|---|---|
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | ||
| Introduction | ||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses |
| Methods | ||
| Study design | 4 | Present key elements of study design early in the paper |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection |
| Participants | 6 | Give the eligibility criteria, and the sources and methods of selection of participants |
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable |
| Data sources/measurement | 8 * | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group |
| Bias | 9 | Describe any efforts to address potential sources of bias |
| Study size | 10 | Explain how the study size was arrived at |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding |
| (b) Describe any methods used to examine subgroups and interactions | ||
| (c) Explain how missing data were addressed | ||
| (d) If applicable, describe analytical methods taking account of sampling strategy | ||
| (e) Describe any sensitivity analyses | ||
| Results | ||
| Participants | 13 * | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed |
| (b) Give reasons for non-participation at each stage | ||
| (c) Consider use of a flow diagram | ||
| Descriptive data | 14 * | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders |
| (b) Indicate number of participants with missing data for each variable of interest | ||
| Outcome data | 15 * | Report numbers of outcome events or summary measures |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95% confidence interval). Make clear which confounders were adjusted for and why they were included |
| (b) Report category boundaries when continuous variables were categorized | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | ||
| Other analyses | 17 | Report other analyses done—e.g., analyses of subgroups and interactions, and sensitivity analyses |
| Discussion | ||
| Key results | 18 | Summarise key results with reference to study objectives |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results |
| Other information | ||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based |
* Give information separately for exposed and unexposed groups.
References
- Di Tecco, C.; Fontana, L.; Adamo, G.; Petyx, M.; Iavicoli, S. Gender differences and occupational factors for the risk of obesity in the Italian working population. BMC Public Health 2020, 20, 706. [Google Scholar] [CrossRef]
- Badr, H.E.; Rao, S.; Manee, F. Gender differences in quality of life, physical activity, and risk of hypertension among sedentary occupation workers. Qual. Life Res. 2021, 30, 1365–1377. [Google Scholar] [CrossRef] [PubMed]
- Peereboom, K.; Langen, N.; Bortkiewicz, A. Prolonged Static Sitting at Work. Health Effects and Good Practice Advice; European Agency for Safety and Health at Work: Bilbao, Spain, 2021. [Google Scholar]
- Phaswana, M.; Gordon, N.F.; Gradidge, P.J.L. Sedentary Behavior, Physical Activity Patterns, and Cardiometabolic Risk Factors in South African Office-Based Workers. Am. J. Lifestyle Med. 2023, 1–8. [Google Scholar] [CrossRef]
- Hadgraft, N.T.; Winkler, E.; Climie, R.E.; Grace, M.S.; Romero, L.; Owen, N.; Dunstan, D.; Healy, G.; Dempsey, P.C. Effects of sedentary behaviour interventions on biomarkers of cardiometabolic risk in adults: Systematic review with meta-analyses. Br. J. Sports Med. 2021, 55, 144–154. [Google Scholar] [CrossRef]
- Kallings, L.V.; Blom, V.; Andersson, G.; Wallin, P.; Ekblom-Bak, E. O9-5 Workplace sitting associated with self-rated perceived global health. Eur. J. Public Health 2022, 32, ckac094.069. [Google Scholar] [CrossRef]
- Castile and León Health. Specific Health Surveillance Protocols 2024. Available online: https://www.saludcastillayleon.es/profesionales/es/saludlaboral/protocolos-vigilancia-salud-especifica (accessed on 15 September 2025).
- Ministry of Labor Government of Spain. Specific Surveillance Protocols for Workers. Available online: https://www.insst.es/stp/protocolos-de-vigilancia-especifica-de-los-trabajadores (accessed on 15 September 2025).
- Alzeidan, R.; Fayed, A.; Rabiee, F.; Hersi, A.; Elmorshedy, H. Diagnostic performance of waist-to-height ratio in identifying cardiovascular risk factors and metabolic syndrome among adult Saudis. Saudi Med. J. 2020, 41, 253–260. [Google Scholar] [CrossRef]
- Rodríguez-López, C.P.; González-Torres, M.C.; Cruz-Bautista, I.; Nájera-Medina, O. Visceral obesity, skeletal muscle mass and resistin in metabolic syndrome development. Nutr. Hosp. 2019, 36, 43–50. [Google Scholar] [CrossRef]
- Abdi Dezfouli, R.; Mohammadian Khonsari, N.; Hosseinpour, A.; Asadi, S.; Ejtahed, H.S.; Qorbani, M. Waist to height ratio as a simple tool for predicting mortality: A systematic review and meta-analysis. Int. J. Obes. 2023, 47, 1286–1301. [Google Scholar] [CrossRef]
- Sweatt, K.; Garvey, W.T.; Martins, C. Correction: Strengths and Limitations of BMI in the Diagnosis of Obesity: What is the Path Forward? Curr. Obes. Rep. 2024, 13, 831. [Google Scholar] [CrossRef]
- Macek, P.; Biskup, M.; Terek-Derszniak, M.; Krol, H.; Smok-Kalwat, J.; Gozdz, S.; Zak, M. Optimal cut-off values for anthropometric measures of obesity in screening for cardiometabolic disorders in adults. Sci. Rep. 2020, 10, 11253. [Google Scholar] [CrossRef]
- Farhangiyan, Z.; Latifi, S.M.; Rashidi, H.; Shahbazian, H. The most appropriate cut-off point of anthropometric indices in predicting the incidence of metabolic syndrome and its components. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2739–2745. [Google Scholar] [CrossRef]
- Chan, V.; Cao, L.; Wong, M.M.H.; Lo, K.; Tam, W. Diagnostic Accuracy of Waist-to-Height Ratio, Waist Circumference, and Body Mass Index in Identifying Metabolic Syndrome and Its Components in Older Adults: A Systematic Review and Meta-Analysis. Curr. Dev. Nutr. 2024, 8, 102061. [Google Scholar] [CrossRef]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef]
- Luengo-Pérez, L.M.; Fernández-Bueso, M.; Ambrojo, A.; Guijarro, M.; Ferreira, A.C.; Pereira-da-Silva, L.; Moreira-Rosário, A.; Faria, A.; Calhau, C.; Daly, A.; et al. Body Composition Evaluation and Clinical Markers of Cardiometabolic Risk in Patients with Phenylketonuria. Nutrients 2023, 15, 5133. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.Y.; Huxley, R.R.; Wildman, R.P.; Woodward, M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: A meta-analysis. J. Clin. Epidemiol. 2008, 61, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Sommer, I.; Teufer, B.; Szelag, M.; Nussbaumer-Streit, B.; Titscher, V.; Klerings, I.; Gartlehner, G. The performance of anthropometric tools to determine obesity: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 12699. [Google Scholar] [CrossRef] [PubMed]
- Dybala, M.P.; Brady, M.J.; Hara, M. Disparity in Adiposity among Adults with Normal Body Mass Index and Waist-to-Height Ratio. iScience 2019, 21, 612–623. [Google Scholar] [CrossRef]
- Zhang, S.; Fu, X.; Du, Z.; Guo, X.; Li, Z.; Sun, G.; Zhou, Y.; Yang, H.; Yu, S.; Zheng, L.; et al. Is waist-to-height ratio the best predictive indicator of cardiovascular disease incidence in hypertensive adults? A cohort study. BMC Cardiovasc. Disord. 2022, 22, 214. [Google Scholar] [CrossRef]
- Yoo, E.G. Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk. Korean J. Pediatr. 2016, 59, 425–431. [Google Scholar] [CrossRef]
- Cai, J.; Lin, C.; Lai, S.; Liu, Y.; Liang, M.; Qin, Y.; Liang, X.; Tan, A.; Gao, Y.; Lu, Z.; et al. Waist-to-height ratio, an optimal anthropometric indicator for metabolic dysfunction associated fatty liver disease in the Western Chinese male population. Lipids Health Dis. 2021, 20, 145. [Google Scholar] [CrossRef]
- Lu, Y.; Liu, S.; Qiao, Y.; Li, G.; Wu, Y.; Ke, C. Waist-to-height ratio, waist circumference, body mass index, waist divided by height0.5 and the risk of cardiometabolic multimorbidity: A national longitudinal cohort study. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2644–2651. [Google Scholar] [CrossRef]
- Campbell, S.D.I.; Brosnan, B.J.; Chu, A.K.Y.; Skeaff, C.M.; Rehrer, N.J.; Perry, T.L.; Peddie, M.C. Sedentary Behavior and Body Weight and Composition in Adults: A Systematic Review and Meta-Analysis of Prospective Studies. Sports Med. 2018, 48, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.A.; Mendonça, C.R.; Delpino, F.M.; Elias Souza, G.V.; Pereira de Souza Rosa, L.; de Oliveira, C.; Noll, M. Sedentary behavior, physical inactivity, abdominal obesity and obesity in adults and older adults: A systematic review and meta-analysis. Clin. Nutr. ESPEN 2022, 50, 63–73. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Guidelines on Physical Activity and Sedentary Behavior: At a Glance. Available online: https://www.who.int/es/publications/i/item/9789240014886 (accessed on 15 September 2025).
- Rahmani, R.; Aliabadi, M.; Golmohammadi, R.; Babamiri, M.; Farhadian, M. Body physiological responses of city bus drivers subjected to noise and vibration exposure in working environment. Heliyon 2022, 8, e10329. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.W.; Shivgulam, M.E.; Domínguez, A.H.; Liu, H.; Waghorn, J.; Courish, M.; Tovar-Díaz, J. Impact of Sedentary Behaviors on Blood Pressure and Cardiovascular Disease: An Umbrella Review of Systematic Reviews and Meta-Analyses. Sports Med. 2024, 54, 3097–3110. [Google Scholar] [CrossRef]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Jingjie, W.; Yang, L.; Jing, Y.; Ran, L.; Yiqing, X.; Zhou, N. Sedentary time and its association with risk of cardiovascular diseases in adults: An updated systematic review and meta-analysis of observational studies. BMC Public Health 2022, 22, 286. [Google Scholar] [CrossRef]
- Burgard, S.A.; Sonnega, A. Occupational Differences in BMI, BMI Trajectories, and Implications for Employment Status among Older U.S. Workers. Work Aging Retire. 2018, 4, 21–36. [Google Scholar] [CrossRef]
- Eanes, L. CE: Too Much Sitting: A Newly Recognized Health Risk. Am. J. Nurs. 2018, 118, 26–34. [Google Scholar] [CrossRef]
- Costantino, S.; Paneni, F.; Cosentino, F. Ageing, metabolism and cardiovascular disease. J. Physiol. 2016, 594, 2061–2073. [Google Scholar] [CrossRef]
- Geng, S.; Chen, X.; Shi, Z.; Bai, K.; Shi, S. Association of anthropometric indices with the development of multimorbidity in middle-aged and older adults: A retrospective cohort study. PLoS ONE 2022, 17, e0276216. [Google Scholar] [CrossRef]
- Sinclair, A.J.; Abdelhafiz, A.H. Cardiometabolic disease in the older person: Prediction and prevention for the generalist physician. Cardiovasc. Endocrinol. Metab. 2020, 9, 90–95. [Google Scholar] [CrossRef]
- Palmer, A.K.; Jensen, M.D. Metabolic changes in aging humans: Current evidence and therapeutic strategies. J. Clin. Investig. 2022, 132, e158451. [Google Scholar] [CrossRef] [PubMed]
- Kallio, P.; Pahkala, K.; Heinonen, O.J.; Tammelin, T.H.; Pälve, K.; Hirvensalo, M.; Juonala, M.; Loo, B.M.; Magnussen, C.G.; Rovio, S.; et al. Physical inactivity from youth to adulthood and adult cardiometabolic risk profile. Prev. Med. 2021, 145, 106433. [Google Scholar] [CrossRef] [PubMed]
- Elm, E.; Altman, D.; Egger, M.; Pocock, S.; Gotzsche, P.; Vandenbroucke, J. Strengthening the Reporting of Observational Studies n Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Daneshmandi, H.; Choobineh, A.; Ghaem, H.; Karimi, M. Adverse Effects of Prolonged Sitting Behavior on the General Health of Office Workers. J. Lifestyle Med. 2017, 7, 69–75. [Google Scholar] [CrossRef]
- Park, S.; Lee, S.; Woo, S.; Webster-Dekker, K.; Chen, W.; Veliz, P.; Larson, J.L. Sedentary behaviors and physical activity of the working population measured by accelerometry: A systematic review and meta-analysis. BMC Public Health 2024, 24, 2123. [Google Scholar] [CrossRef]
- Araujo, G.C.; Ribeiro, C.B.; Costa, M.C.M.; Evangelista, M.L.P.; Lima, M.F.; De Paula, M.C.; Ferreira, V.L.; Araujo, F.A.G. Evidence-Based Periodic Health Examinations for Adults: A Practical Guide. Cureus 2025, 17, e79963. [Google Scholar] [CrossRef]
- United States Preventive Services Task Force (USPSTF). Available online: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-a-and-b-recommendations (accessed on 31 October 2024).
- Canadian Task Force on Preventive Health Care (CTFPHC). Available online: https://canadiantaskforce.ca/guidelines/published-guidelines/ (accessed on 31 October 2024).
- Janse, R.J.; Hoekstra, T.; Jager, K.J.; Zoccali, C.; Tripepi, G.; Dekker, F.W.; Van Diepen, M. Conducting correlation analysis: Important limitations and pitfalls. Clin. Kidney J. 2021, 14, 2332–2337. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation coefficients: Appropriate use and interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Gitsi, E.; Kokkinos, A.; Konstantinidou, S.K.; Livadas, S.; Argyrakopoulou, G. The Relationship between Resting Metabolic Rate and Body Composition in People Living with Overweight and Obesity. J. Clin. Med. 2024, 13, 5862. [Google Scholar] [CrossRef]
- Jang, S.Y.; Choi, K.M. Impact of Adipose Tissue and Lipids on Skeletal Muscle in Sarcopenia. J. Cachexia Sarcopenia Muscle 2025, 16, e70000. [Google Scholar] [CrossRef]
- Nguyen, H.P.; Lin, F.; Yi, D.; Xie, Y.; Dinh, J.; Xue, P.; Sul, H.S. Aging-dependent regulatory cells emerge in subcutaneous fat to inhibit adipogenesis. Dev. Cell 2021, 56, 1437–1451.e3. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Q.; Wang, Y.; Ma, C.; Zhao, Q.; Yin, H.; Li, L.; Wang, D.; Huang, Y.; Zhao, Y.; et al. Interleukin-6 promotes visceral adipose tissue accumulation during aging via inhibiting fat lipolysis. Int. Immunopharmacol. 2024, 132, 111906. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.X.; Ou, M.Y.; Yang, Z.H.; Sun, Y.; Li, Q.F.; Zhou, S.B. Adipose tissue aging is regulated by an altered immune system. Front. Immunol. 2023, 14, 1125395. [Google Scholar] [CrossRef]
- Sadie-Van Gijsen, H. Is Adipose Tissue the Fountain of Youth? The Impact of Adipose Stem Cell Aging on Metabolic Homeostasis, Longevity, and Cell-Based Therapies. Adv. Exp. Med. Biol. 2021, 1286, 225–250. [Google Scholar] [CrossRef]
- Frasca, D.; Blomberg, B. Adipose tissue, immune aging and cellular senescence. Semin. Immunopathol. 2020, 42, 573–587. [Google Scholar] [CrossRef]
- Yang, H.; Xin, Z.; Feng, J.P.; Yang, J.K. Waist-to-height ratio is better than body mass index and waist circumference as a screening criterion for metabolic syndrome in Han Chinese adults. Medicine 2017, 96, e8192. [Google Scholar] [CrossRef]
- Khanna, D.; Peltzer, C.; Kahar, P.; Parmar, M.S. Body Mass Index (BMI): A Screening Tool Analysis. Cureus 2022, 14, e22119. [Google Scholar] [CrossRef]
- Saunders, T.J.; McIsaac, T.; Douillette, K.; Gaulton, N.; Hunter, S.; Rhodes, R.E.; Prince, S.A.; Carson, V.; Chaput, J.P.; Chastin, S.; et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020, 45, S197–S217. [Google Scholar] [CrossRef]
- Butler, K.M.; Ramos, J.S.; Buchanan, C.A.; Dalleck, L.C. Can reducing sitting time in the university setting improve the cardiometabolic health of college students? Diabetes, Metab. Syndr. Obes. 2018, 11, 603–610. [Google Scholar] [CrossRef]
- Mirzaei, M.; Askari, M.; Namiranian, N.; ali Mahmoudi Kohani, H. Relationship between sitting time and anthropometric indices: Findings of Yazd health study (YaHS). Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2220–2225. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M.; Ding, D.; Heath, G.; et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- Wanner, M.; Martin, B.W.; Autenrieth, C.S.; Schaffner, E.; Meier, F.; Brombach, C.; Stolz, D.; Bauman, A.; Rochat, T.; Schindler, C.; et al. Associations between domains of physical activity, sitting time, and different measures of overweight and obesity. Prev. Med. Rep. 2016, 3, 177–184. [Google Scholar] [CrossRef]
- Varela-Mato, V.; O’Shea, O.; King, J.A.; Yates, T.; Stensel, D.J.; Biddle, S.J.; Nimmo, M.A.; Clemes, S.A. Cross-sectional surveillance study to phenotype lorry drivers’ sedentary behaviours, physical activity and cardio-metabolic health. BMJ Open 2017, 7, e013162. [Google Scholar] [CrossRef]
- Hanssen, H. Lifestyle recommendations as treatment for arterial hypertension: A time to review. Eur. J. Prev. Cardiol. 2023, 30, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Tronieri, J.S.; Butryn, M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 2020, 75, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.H.; Kahan, S. Guideline Recommendations for Obesity Management. Med. Clin. N. Am. 2018, 102, 49–63. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M.; Bhatt, D.L. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e367–e386. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Coenen, P.; Howie, E.; Williamson, A.; Straker, L. The short term musculoskeletal and cognitive effects of prolonged sitting during office computer work. Int. J. Environ. Res. Public Health 2018, 15, 1678. [Google Scholar] [CrossRef]
- Prince, S.A.; Rasmussen, C.L.; Biswas, A.; Holtermann, A.; Aulakh, T.; Merucci, K.; Coenen, P. The effect of leisure time physical activity and sedentary behaviour on the health of workers with different occupational physical activity demands: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 100. [Google Scholar] [CrossRef]
- Zhu, X.; Yoshikawa, A.; Qiu, L.; Lu, Z.; Lee, C.; Ory, M. Healthy workplaces, active employees: A systematic literature review on impacts of workplace environments on employees’ physical activity and sedentary behavior. Build. Environ. 2020, 168, 106455. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).