Abstract
Background: Farmers are continuously exposed to pesticides during crop production, which can lead to both acute and chronic poisoning. This exposure poses a significant global public health concern. In response, this study aims to achieve two primary objectives: (1) to identify the correlation between pesticide intoxication cases among farmers and their potential causes and (2) to assess the relationship between risk–control measures, hygiene practices, and resulting health effects. Methods: This study employed a cross-sectional mixed-methods observational design, sampling 112 farmers from Bogotá’s rural areas. Data were analyzed using logistic regression in R (version 4.2.1), examining eight associated variables. Results: The use of personal protective equipment (PPE) ranged from approximately 62% to 92%. Additionally, 82% of participants reported changing their workwear and 76% practiced bodily hygiene after exposure. Nevertheless, health complaints persisted—particularly affecting vision (46%), the respiratory system (38%), and the skin (32%). Notably, two out of every three farmers reported experiencing some form of systemic illness associated with pesticide exposure. Conclusion: A strong association was observed between the use of facemasks and changing workwear and the prevention of pesticide-related intoxication. These practices appear to be key in reducing chemical exposure during fumigation activities.
1. Introduction
In Colombia, the agricultural sector contributed 4.5% to the national GDP in 2019 and accounted for 16% of total employment [1,2]. Globally, agriculture holds significant economic and social importance, employing approximately 874 million people—equivalent to 27.4% of the global workforce. Despite its prominence, agriculture remains one of the most hazardous sectors in terms of occupational health. Agricultural workers are twice as likely to experience fatal work-related injuries compared to those in other industries. This elevated risk is largely due to the operation of heavy machinery and extensive exposure to agrochemical substances used for pest control [3]. The danger increases when pesticides are combined to broaden their range and efficacy; however, such practices can also contribute to the development of a variety of adverse health conditions [4].
According to the National Institute of Health of Colombia, an average of 5890 pesticide poisoning cases were reported annually between 2017 and 2022, representing 17.2% of all intoxication cases nationwide during this period. Exposure to pesticides has been consistently associated with the onset of numerous health conditions, as documented in a range of scientific studies. These include various types of cancer [4,5], congenital anomalies and developmental toxicity [6], reproductive disorders [7,8], neurodegenerative diseases such as Parkinson’s and Alzheimer’s [4,9], endocrine disruptions [10], and respiratory ailments [11], among others [4]. Given their high prevalence and significant health impact, pesticide-related poisonings are under special epidemiological surveillance in Colombia (Table 1). Notably, pesticides and agrochemicals currently rank as the third most common cause of intoxication in the country—exceeding incidents involving psychoactive substances and pharmaceuticals—and are believed to be the primary cause of occupational poisoning [12,13,14,15].

Table 1.
Cases of intoxications due to pesticides 2017–2020n in Colombia, Bogotá, and Ciudad Bolivar.
Agriculture remains a vital component of Bogotá’s economy, underscoring the need for the continuous monitoring of pesticide-related poisoning within the city. The rural areas of Bogotá are organized into four main regions—Cerros Orientales, Cuenca Tunjuelo, Sumapaz, and Torca—which together comprise approximately 75% of the city’s total land area and were home to an estimated 30,578 residents in 2022. Agriculture serves as the primary economic activity for these communities [16]. Public health initiatives aimed at reducing pesticide poisoning showed promising results between 2017 and 2020, with a marked decline in reported cases from 397 in 2017 to just 52 in 2020 [17]. Nevertheless, a resurgence in poisoning cases has been documented over the past three years, affecting Bogotá as a whole and Ciudad Bolívar in particular (Table 1). Located within the Cuenca Tunjuelo region, Ciudad Bolívar encompasses 5923 hectares allocated to agricultural production, positioning it as the most agriculturally intensive area among the city’s rural zones [18].
Sustaining the reduction in pesticide-related poisoning—and ultimately aiming for zero cases—is especially critical in Ciudad Bolívar, given its significant contribution to both the rural and urban economies. Due to the occupational nature of most pesticide exposures, it is essential to examine this issue in relation to key sociodemographic and occupational variables, as well as to assess the potential health consequences associated with prolonged or repeated exposure. Given this context, this research project focuses on Ciudad Bolívar with the following objectives: (1) analyze the correlation between pesticide poisoning cases and specific pesticide use and (2) evaluate the relationship between adherence to safety practices (e.g., use of protective equipment, hygiene habits) and identify potential risk factors contributing to intoxication among agricultural workers.
2. Materials and Methods
2.1. Study Areas
The study was conducted in Ciudad Bolívar, a territorial subdivision of Bogotá that is 75% rural [18]. The locality comprises three rural zones—Mochuelo Alto, Quiba, and Pasquilla—which were selected for this study due to their strong agricultural traditions and extensive farmland (Figure 1). Furthermore, the collaboration with community leaders, who provided valuable insights and facilitated access to other farmers, was instrumental in carrying out the research.
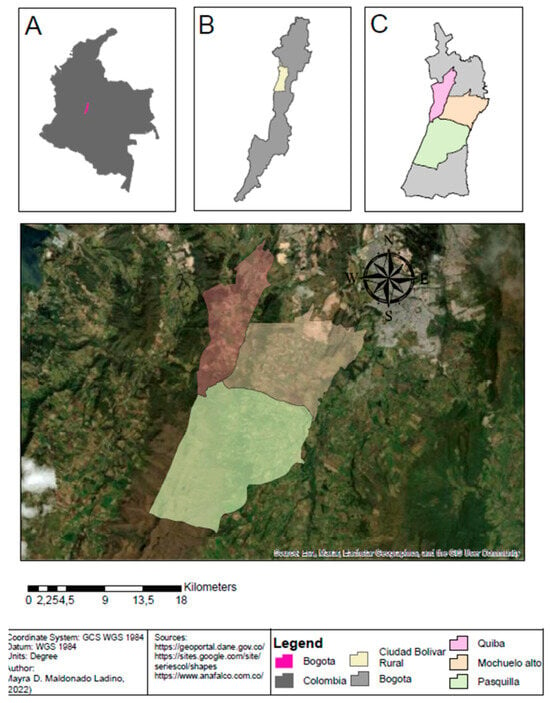
Figure 1.
Map of Mochuelo Alto, Quiba y Pasquilla, in the locality of Ciudad Bolivar.
2.2. Research Desing
The research design is based on a structured, closed-ended questionnaire consisting of 33 questions categorized as follows: (A) sociodemographic and economic characteristics; (B) agricultural practices, pesticide use and handling, safety practices, and hygiene habits during pesticide application; and (C) health conditions related to pesticide exposure and intoxication. The questionnaire was developed based on validated instruments from previous research by Oropesa et al. and Barrón Cuenca et al. [19,20], which were adapted to align with the study’s objectives. During the questionnaire design process, special care was taken to ensure that the closed-ended questions in categories (A) and (B) did not overly constrain responses regarding farmers’ habits. In category (C), which pertains to health conditions and poisoning incidents, the study aimed to investigate the relationship between isolated poisoning events (acute incidents) and chronic systemic health conditions of potential occupational origin. This was assessed through open-ended questions designed to determine whether medical documentation was available to support the etiology of the reported poisoning event or systemic condition.
Additionally, the questionnaire underwent a review and validation process involving community leaders, ensuring the relevance of the questions and refining critical study variables. The questionnaire was administered between 1 August and 30 November 2021, resulting in the collection of 112 responses from the designated study area. The sample was obtained using a snowball sampling method, covering over 10% of the population in contact with pesticides in the study region. As of the study date, the total population in the area was estimated at 1048 individuals, including minors and women engaged in domestic activities.
To ensure sample representativeness, an estimate of the working agricultural population was established. According to DANE [21], 74.7% of Colombia’s rural population is under 20 years of age. Consequently, approximately one-third of the total study area population (691 individuals classified as minors) was excluded, as the study focused exclusively on adults. Additionally, it was assumed that only one individual per household was actively engaged in agriculture, leading to an estimated workforce of 262 individuals. Further assessment during data collection revealed that not all working residents were involved in agriculture—some were engaged in commercial services, livestock farming, or urban employment. As a result, the representativeness of the 112 surveyed farmers was deemed sufficient. Data saturation was achieved, as no additional eligible respondents could be identified beyond those who had already participated in the survey or were not engaged in agricultural work.
Before questionnaire implementation, brief interviews with two community leaders were conducted to gather insights on demographic distribution, agricultural practices, and cultural aspects of the study area. The questionnaire was administered across six visits, with the participation of three lead researchers and five data collection assistants—undergraduate interns in occupational health and safety—who received prior training for data collection. Data collection was carried out using the Kobo Collect application, an open-source platform designed for offline primary data collection in remote areas, compatible with Android devices. The collected data were systematically organized, downloaded, and subsequently analyzed using R software.
2.3. Statistical Analysis
Statistical analysis was performed using R version 4.2.1 for Windows. A quantitative analysis was conducted via logistic regression to establish potential associations between pesticide poisoning (dependent variable) and seven independent variables: work shift, use of facemasks, gloves, and overalls, as well as hygiene practices, including changing work clothes and personal body hygiene.
3. Results
The study population was drawn from the three designated areas under investigation. The final sample consisted of 112 individuals engaged in agriculture-related activities, of whom only 6% were women. Notably, half of the participants were over the age of 51, and the majority (63%) had completed only primary education. In terms of social security, 56% of respondents were affiliated with a healthcare service; however, just 13% had a pension plan, and only 9% were covered by occupational risk insurance (Table 2).

Table 2.
Sociodemographic characteristics of the population.
Among the 112 participants, only 98 reported direct contact with pesticides. Within this subgroup, 22% did not engage in pesticide mixing activities. Most farmers adhered to recommended pesticide application guidelines, with 64% reading product labels and 67% ensuring the dosage did not exceed prescribed limits. The use of personal protective equipment (PPE) was prevalent, with boots being the most used item (92%), followed by gloves (79%). Facemasks were worn by 72% of participants, while 62% reported using overalls.
Observational assessments revealed that facial protection was primarily limited to surgical or cloth facemasks, which offer inadequate protection against pesticide exposure. Most participants adhered to hygiene practices, with 82% changing their clothes and 76% performing regular body cleansing after pesticide application (Figure 2).
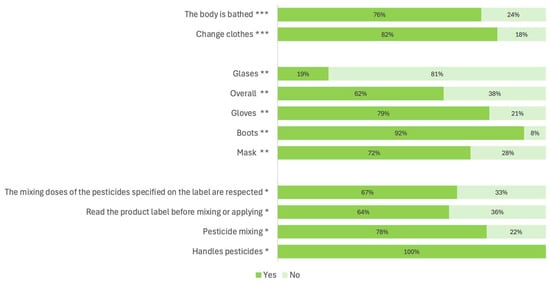
Figure 2.
Use of pesticide *, hygiene habits **, and use of personal protective equipment (PPE) ***.
The participants reported various health conditions attributed to pesticide exposure, including visual impairments (46%), respiratory disorders (38%), dermatological conditions (32%), digestive issues (6%), and neurological symptoms (18%). Notably, two out of three farmers had experienced at least one health condition linked to their agricultural work.
A descriptive analysis of pesticide intoxication indicated that one in five agricultural workers had experienced at least one poisoning event, defined as any clinically significant change following pesticide exposure [22]. For this study, an intoxication event was recorded when a participant received medical attention for acute pesticide exposure. A total of 21 cases were documented, with some individuals reporting multiple intoxication episodes over their work history.
Logistic regression was performed using intoxication as the dependent variable and seven explanatory independent variables, as represented in Equation (1). Most independent variables were dichotomous (yes/no responses) and were selected based on exposure control factors such as PPE use, hygiene practices, and work shift duration. Exposure time emerged as a key factor, showing a proportional increase in intoxication risk.
Equation (1). Logistic regression based on the dependent variable of intoxication
: work shift length; : facemask use; : glove use; : eye protection equipment use; : use of overalls; : workwear change; : body cleaning.
Initially, regression analysis was conducted on an imbalanced dataset, where the number of non-intoxicated cases (77) was nearly four times higher than intoxicated cases [23]. This imbalance influenced the regression model, leading to a confusion matrix (Figure 3) that improved the prediction of factors associated with intoxication (Table 3). The model achieved a 79% accuracy in predicting intoxication events; however, statistical evidence for specific risk factors remained inconclusive. The coefficient estimates demonstrated an inverse relationship between intoxication and the use of protective measures, but with a low correlation (p = 0.2439) (Table 4).

Figure 3.
Confusion matrix plot.

Table 3.
Logistic correlation coefficients.

Table 4.
Data structure versus logistic regression.
To improve correlation, the dataset was balanced in R software, resulting in an enhanced model with an 82% prediction accuracy for intoxication. Among the explanatory variables, facemask use, and workwear changes had negative beta coefficients, indicating a reduced intoxication risk when these measures were implemented. Conversely, glove use and body hygiene had positive coefficients, suggesting an increased risk of intoxication despite these practices. Work shift duration was the only non-dichotomous variable with a direct correlation to intoxication probability (Table 5).

Table 5.
Logistic correlation coefficients (balanced data).
The revised confusion matrix (Figure 4) indicated an overall accuracy of 82.3% in predicting intoxication events and 70.8% accuracy in correctly identifying non-intoxicated cases. The model’s statistical significance was reinforced, with a p-value of 0.00994 and an R2 value of 0.756, confirming the robustness and explanatory power of the logistic regression model (Table 6).
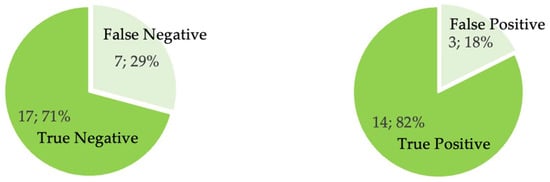
Figure 4.
Confusion matrix plot (balanced data).

Table 6.
Data structure (balanced data) versus logistic regression.
4. Discussion
This study highlights critical factors associated with pesticide exposure among Bogotá’s rural farming communities and identifies occupational risks faced by agricultural workers. One key finding is the association between education level and pesticide risk awareness. The high prevalence (63%) of incomplete elementary education aligns with previous studies by Miguel et al. [22] and Zambrano [23], which reported similar trends in other agricultural populations. Limited education reduces farmers’ ability to understand pesticide hazards, as evidenced by the 36% who did not read product labels before use. This is consistent with findings by Fernández Aravena in Ecuador, who observed a strong association between low education levels and failure to read pesticide labels (27%) [24,25].
This study also identified four prevalent systemic health conditions among participants: neurological, respiratory, digestive, and dermatological disorders. Notably, 46% of respondents reported visual symptoms and 38% reported respiratory issues, with 66% experiencing at least one adverse health effect. These findings align with prior research by Miguel et al., which documented multiple neurological and digestive symptoms in 81.3% of cases, and Alvarado [26], who reported a 96% incidence of acute neurological intoxication and a 44% prevalence of dermatological or digestive conditions among Mexican farmers exposed to organophosphates. Similarly, Barrón Cuenca found that 84% of Bolivian farmers had experienced acute intoxication symptoms, with 52% reporting multiple simultaneous symptoms [18].
The high incidence of ocular symptoms in this study differs from previous research on pesticide exposure, necessitating further investigation. Pesticides commonly used in Colombia, as identified by the Colombian Agricultural Institute [27], contain active ingredients such as azoxystrobin [28], glyphosate [29], mancozeb [30], difenoconazole [31], and imidacloprid [32], all classified as ocular irritants according to PubChem of the National Center for Biotechnology Information.
4.1. Personal Protective Equipment and Occupational Safety
This study confirmed the widespread use of personal protective equipment (PPE), particularly boots, gloves, and facemasks. These findings are consistent with previous research by Pastor et al. [25], who reported that 78% of farmers used at least one protective item, and Varona Uribe [33], who found that 91% of farmers utilized body protection. The existing literature underscores the importance of PPE as a key factor in mitigating pesticide exposure [34,35,36,37]. However, the effectiveness of protective measures depends on their suitability for the level of exposure, including duration, frequency of pesticide use, and the type of equipment used. Cohecha Cárdenas et al. [4] observed that although farmers frequently employ PPE, it is often inadequate for safe pesticide handling. Similarly, Varona Uribe [26] emphasized the limited protective capacity of surgical and cloth masks, highlighting the need for increased access to more effective respiratory protection.
4.2. Study Strengths and Limitations
A major strength of this study is its collection of primary data on pesticide poisoning and systemic health effects, addressing a gap in localized exposure assessments. While national poisoning reports exist, detailed local-level causative factors are often missing. Additionally, the study achieved robust logistic regression correlations, enabling accurate intoxication predictions based on explanatory variables.
However, several limitations were noted. Limited prior research in the study area posed challenges in estimating the working population and geographic distribution of agricultural activities. The reluctance of participants to undergo toxicological testing, coupled with financial constraints, restricted biological exposure assessments.
Methodologically, the use of non-probabilistic sampling may have introduced selection bias, reducing the generalizability of findings. The voluntary nature of participation may have further skewed results, as individuals with health concerns may have been overrepresented. Furthermore, participants were required to provide informed consent, which may have led to sample limitations.
One of the main limitations of this study concerns the selection of independent variables included in the logistic regression model. While multiple factors may influence pesticide exposure—such as the type of pesticide used, application methods, equipment involved, and prior training—this research prioritized variables that were both observable and directly related to workers’ routine practices in the field. Specifically, this analysis focused on personal protective equipment (PPE) use and hygiene habits, which are considered immediate determinants of exposure and are more easily assessed in rural settings with limited access to technical data and formal education. However, the exclusion of other potentially relevant factors may have limited the explanatory power of the model and introduced some degree of bias. Future studies should consider incorporating a broader range of exposure determinants, including detailed information on pesticide types, frequency of use, application techniques, and training history, to enhance the robustness of risk assessments.
Another important consideration is that health outcomes were self-reported by participants, which may introduce recall or subjective interpretation bias. Although open-ended questions were used to allow detailed descriptions of symptoms and participants were asked whether they had received medical attention for reported conditions, no clinical assessments were performed to confirm diagnoses. This may help explain the high prevalence of certain symptoms, such as visual impairments, which were reported by 46% of participants. According to respondents, these issues primarily included eye irritation, redness, and blurred vision following pesticide application. While such data are valuable in highlighting workers’ perceived health impacts, they must be interpreted with caution. Future research would benefit from incorporating clinical evaluations or validated diagnostic tools to objectively verify the presence and severity of pesticide-related health effects.
5. Conclusions
Pesticide exposure among farmers is influenced by external factors such as sociodemographic conditions, inadequate protective measures, and limited risk awareness, all of which significantly impact agricultural workers’ health. This study confirms that appropriate PPE use is essential in reducing intoxication risk (82.3% probability). However, PPE must be tailored to specific chemical hazards.
Systemic health effects—including visual, respiratory, and dermatological conditions—are prevalent among agricultural workers. Two out of three farmers in Ciudad Bolívar reported experiencing adverse health effects following pesticide exposure. These findings highlight the need for continuous monitoring by local authorities and further research to develop targeted interventions aimed at enhancing occupational safety. Despite methodological limitations, this study provides critical insights into pesticide exposure risks, supporting evidence-based policy recommendations for occupational health interventions at local and national levels.
Author Contributions
Conceptualization, M.D.M. and K.M.-O.; methodology, M.D.M.; software, D.M.B.; validation, M.D.M., K.M.-O. and D.M.B.; formal analysis, M.D.M.; investigation, M.D.M.; resources, D.M.B.; data curation, M.D.M.; writing—original draft preparation, M.D.M., K.M.-O., D.M.B., J.d.D.V. and A.B.C.; writing—review and editing, M.D.M., K.M.-O., D.M.B., J.d.D.V. and A.B.C.; funding acquisition, A.B.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research has been funded by Dirección General de Investigaciones of Universidad Santiago de Cali under call No. DGI-01-2025.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Fundación Universitaria San Martin (protocol code 12SH and date of approval 20 November 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Data are available under request.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Departamento Administrativo Nacional de Estadísticas (DANE). Producto Interno Bruto -PIB-Nacional Trismestral. 2022. Cuentas Nacionales Trimestrales. ProductoInterno Bruto desde el Enfoque de la Producción a Precios Corrientes. Available online: https://www.dane.gov.co/index.php/estadisticas-por-tema/cuentas-nacionales/cuentas-nacionales-trimestrales/pib-informacion-tecnica (accessed on 29 August 2022).
- Banco Mundial. Empleos en Agricultura [Internet]. 2022. Available online: https://datos.bancomundial.org/indicador/SL.AGR.EMPL.ZS (accessed on 29 August 2022).
- OIT. La Agricultura: Un Trabajo Peligroso [Internet]. 2015. Available online: http://www.ilo.org/global/topics/safety-and-health-at-work/areasofwork/hazardous-work/WCMS_356566/lang--es/index.htm (accessed on 20 August 2022).
- Cohecha Cárdenas, A.K.; Niño Martínez, S.V.; De Arco Canoles, O. Efectos en la salud de los agricultores latinoamericanos expuestos a plaguicidas: Una revisión sistemática 1991–2018. Rev. Toxicol. 2021, 38, 22–28. [Google Scholar]
- Polanco Rodríguez, A.G.; Magaña Castro, T.V.; Cetz Luit, J.; Quintal López, R. Uso de agroquímicos cancerígenos en la región agrícola de Yucatán, México. Cent. Agr. 2019, 46, 72–83. [Google Scholar]
- Rojas, R.A.; Ojeda, B.M.E.; Barraza, O.X. Malformaciones congénitas y exposición a pesticidas. Rev. Méd. Chile 2000, 128, 399–404. [Google Scholar] [CrossRef]
- Paparella, C.V.; Pavesi, A.B.; Feldman, R.N.; Bouvet, B.R. El efecto de los agroquímicos en la espermatogénesis. Rev. Habanera Cienc. Méd. 2011, 10, 190–200. [Google Scholar]
- Miranda-Contreras, L.; Gómez-Pérez, R.; Rojas, G.; Cruz, I.; Berrueta, L.; Salmen, S.; Colmenares, M.; Barreto, S.; Balza, A.; Zavala, L.; et al. Occupational Exposure to Organophosphate and Carbamate Pesticides Affects Sperm Chromatin Integrity and Reproductive Hormone Levels among Venezuelan Farm Workers. J. Occup. Health 2013, 55, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Iknurov Mollov, A.; Martinez Ponce, D.C.; Serrano Puebla, J.M.; Elias Salcedo, S. Exposición a pesticidas en el ámbito laboral, expresión genética y enfermedad de Parkinson. Med. Segur. Trabajo 2017, 63, 68–84. [Google Scholar]
- Farokhi, F.; Taravati, A. Pesticide exposure and thyroid function in adult male sprayers. Int. J. Med. Investig. 2014, 3, 127–132. [Google Scholar]
- Buralli, R.J.; Ribeiro, H.; Mauad, T.; Amato-Lourenço, L.F.; Salge, J.M.; Diaz-Quijano, F.A.; Leão, R.S.; Marques, R.C.; Silva, D.S.; Guimarães, J.R.D. Respiratory Condition of Family Farmers Exposed to Pesticides in the State of Rio de Janeiro, Brazil. Int. J. Environ. Res. Public Health 2018, 15, 1203. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Salud. Informe de Evento Intoxicaciones por Sustancias Químicas, Colombia, 2017 [Internet]. Bogotá. 2017. Available online: https://www.ins.gov.co/buscador-eventos/Informesdeevento/INTOXICACIONES%202017.pdf (accessed on 1 April 2025).
- Instituto Nacional de Salud. Informe de Evento Intoxicaciones por Sustancias Químicas, Colombia, 2019 [Internet]. Bogotá. 2019. Available online: https://www.ins.gov.co/buscador-eventos/Informesdeevento/INTOXICACIONES_2019.pdf (accessed on 1 April 2025).
- Instituto Nacional de Salud. Informe de Evento Intoxicaciones por Sustancias Químicas, Colombia, 2018 [Internet]. Bogotá. 2018. Available online: https://www.ins.gov.co/buscador-eventos/Informesdeevento/INTOXICACIONES_2018.pdf (accessed on 1 April 2025).
- Instituto Nacional de Salud. Lineamientos Pro Intoxicaciones. 2025. Available online: https://www.ins.gov.co/buscador-eventos/Lineamientos/Pro_Intoxicaciones%20agudas%20por%20sustancias%20qu%C3%ADmicas%202024.pdf (accessed on 13 March 2025).
- Secretaría Distrital de Planeación. Panorama de la Ruralidad Bogotana: Una Radiografía Socioeconómica. 2025. Available online: https://sdp.gov.co/sites/default/files/1._panorama_economico_ruralidad_digital.pdf (accessed on 13 March 2025).
- Secretaría Distrital de Salud de Bogotá. SaluData Observatorio de Bogotá. 2022. Observatorio de Salud de Bogotá—SaluData. Available online: https://saludata.saludcapital.gov.co/osb/ (accessed on 1 April 2025).
- Alcaldía Local de Ciudad Bolívar. Alcaldía Local de Ciudad Bolívar. Alcaldía Mayor de Bogotá, D.C. 2022. Conociendo mi localidad. Available online: http://www.ciudadbolivar.gov.co/mi-localidad/conociendo-mi-localidad/historia (accessed on 2 September 2022).
- Oropesa Jiménez, A.; Soler Rodríguez, F.; Haro Castuera, M. Estimación del grado de conocimiento sobre el riesgo químico en trabajadores de Badajoz. Rev. Toxicol. 2011, 28, 158–165. [Google Scholar]
- Barrón Cuenca, J.; Tirado, N.; Vikström, M.; Lindh, C.H.; Stenius, U.; Leander, K.; Berglund, M.; Dreij, K. Pesticide exposure among Bolivian farmers: Associations between worker protection and exposure biomarkers. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 730–742. [Google Scholar] [CrossRef] [PubMed]
- DANE. Mujeres Rurales en Colombia. 2025. Available online: https://www.dane.gov.co/files/investigaciones/notas-estadisticas/oct-2021-nota-estadistica-situacion-mujeres-rurales-colombia-resumen.pdf (accessed on 3 March 2025).
- da Silva Miguel, E.; Carmo, D.L.; Lopes, S.O.; Santos, R.H.; Franceschini, S.; Castro, L.C.V.; Costa, G.D.; Priore, S.E. Intoxication symptoms and health conditions of family farmers associated with the use of pesticides: A study conducted in Zona da Mata Mineira, Brazil. Res. Soc. Dev. 2022, 11, e31011830923. [Google Scholar] [CrossRef]
- Byrne, R.; Kirschner, K. 27—Unusual Behaviors. In Nelson Pediatric Symptom-Based Diagnosis [Internet]; Kliegman, R.M., Lye, P.S., Bordini, B.J., Toth, H., Basel, D., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 421–438.e1. Available online: https://www.sciencedirect.com/science/article/pii/B9780323399562000273 (accessed on 1 April 2025).
- Zambrano Tigua, S.L. Diagnóstico de Aplicación de Agroquímicos e n Cultivos de Ciclo Corto y su Impacto en la Salud Ambiental Cantagallo. 2018. Available online: http://repositorio.unesum.edu.ec/handle/53000/1299 (accessed on 11 May 2022).
- Fernández Aravena, C.I. Alteraciones Tiroideas en Agricultores de Cotopaxi y su Relación con el Uso de Plaguicidas. Revista San Gregorio [Internet]. 30 de Marzo de 2021. Available online: https://revista.sangregorio.edu.ec/index.php/REVISTASANGREGORIO/article/view/1396 (accessed on 17 August 2022).
- Alvarado, J.; Valencia, C.A.; Castillo, M.R.; Luna, P.; Borboa, J.; Mexia, M.; Ruiz Sandoval, N.C. Agroquímicos Organofosforados y su Potencial Daño en la Salud de Trabajadores Agrícolas del Campo Sonorense. CIENCIA Ergo-Sum, Revista Científica Multidisciplinaria de Prospectiva [Internet]. 2019; Volume 26. Available online: https://www.redalyc.org/jatsRepo/104/10456899008/html/index.html (accessed on 14 September 2021).
- Instituto Colombiano Agropecuario. (s.f.). Reporte Plaguicidas Químicos de Uso Agrícola [Dashboard interactivo]. AnalítICA. 2025. Available online: https://www.ica.gov.co (accessed on 24 March 2025).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 3034285, Azoxystrobin. 2025. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Azoxystrobin (accessed on 24 March 2025).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 3496, Glyphosate. 2025. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Glyphosate (accessed on 24 March 2025).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 13307026, zinc;manganese(2+);N-[2-(sulfidocarbothioylamino)ethyl]carbamodithioate. 2025. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/mancozeb (accessed on 25 March 2025).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 86173, Difenoconazole. 2025. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Difenoconazole (accessed on 24 March 2025).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 86287518, Imidacloprid. 2025. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Imidacloprid (accessed on 24 March 2025).
- Pastor, S.; Gutiérrez, S.; Creus, A.; Xamena, N.; Piperakis, S.; Marcos, R. Cytogenetic analysis of Greek farmers using the micronucleus assay in peripheral lymphocytes and buccal cells. Mutagenesis 2001, 16, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Varona Uribe, M.; Castro, R.A.; Paéz, I.; Carvajal, N.; Barbosa, E.; León, L.M.; Diaz, S.M. Impacto en la salud y el medio ambiente por exposición a plaguicidas e implementación de buenas prácticas agrícolas en el cultivo de tomate, Colombia, 2011. Rev. Chil. Salud Púb. 2012, 16, 96–106. [Google Scholar] [CrossRef]
- Bolognesi, C.; Landini, E.; Perrone, E.; Roggieri, P. Cytogenetic biomonitoring of a floriculturist population in Italy: Micronucleus analysis by fluorescence in situ hybridization (FISH) with an all-chromosome centromeric probe. Mutat. Res. 2004, 557, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Simoniello, M.F.; Kleinsorge, E.C.; Scagnetti, J.A.; Grigolato, R.A.; Poletta, G.L.; Carballo, M.A. DNA damage in workers occupationally exposed to pesticide mixtures. J. Appl. Toxicol. 2008, 28, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Pastor, S.; Gutiérrez, S.; Creus, A.; Cebulska-Wasilewska, A.; Marcos, R. Micronuclei in peripheral blood lymphocytes and buccal epithelial cells of Polish farmers exposed to pesticides. Mutat. Res. 2001, 495, 147–156. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).