Abstract
Introduction: Parkinson’s disease is most prevalent among elderly people, 65 years and over, and leads to an alteration in motor control associated with postural instability. Current evidence shows that postural control decreases with the aging process. In addition, postural control is more altered in healthy aged men than in women. Until today, few studies have evaluated the combined impact of Parkinson’s disease and sex on postural control. This review has allowed to evaluate the impact of Parkinson’s disease and sex on postural control measurements in elderly people. Methodology: Studies have been selected from two main databases: PubMed and EBSCO using the keywords “Parkinson”, “postural control OR balance” and “sex”. Articles related to the evaluation of postural control, including men and women with Parkinson’s aged over 65 years old, regardless of stage, were included (n = 179). Articles were excluded if not written in French or English or not presenting original content. Results: Ten (10) studies out of 179 that fulfilled inclusion and exclusion criteria were reported in the final analysis, which cumulates a total of 944 individuals with Parkinson’s (410 women). In general, results show greater postural instability among people with Parkinson’s compared to healthy subjects, and this according to different objective measurements using stabilographic parameters from force platforms. Only two studies out of ten evaluated postural control while briefly considering distinctions between sex, but without showing a significant difference between men and women with Parkinson’s. Parkinson’s severity, length of time of Parkinson’s disease and cognitive state of the person are the three variables with a negative impact on postural control. Conclusion: Older people with Parkinson’s disease have greater postural instability. Sex does not seem to influence the postural control of elderly people with Parkinson’s, although more studies are necessary.
1. Introduction
The proportion of people aged 65-years-old and over is increasing, worldwide. When following this progression, these people should represent 23.1% in North America by 2031, like the Canadian population [1]. With the natural process of aging, chronic degenerative diseases are more prevalent and further impact the biological changes associated with the proper aging process, such as muscular weakness, mobility impairment and poor balance or postural control [2,3,4]. These changes may predict frailty in the older individual as well as an increase in the risk of falls in this population [5,6,7]. Furthermore, poor postural control is one of the most important risk factors of falls in older adults [8]. Falls can be responsible for 85% of hospitalizations with injury in the elderly [9]. They are associated with multiple injuries and disabilities [10,11,12] as well as physical injuries, social isolation, psychological problems (anxiety, fear and depression) and increased mortality rates [12,13,14,15].
Among chronic and degenerative diseases in older adults, Parkinson’s disease is one of the most prevalent in individuals aged 65 years and over [16,17]. Moreover, the incidence of this disease would be two times higher in older men than in older women [18]. Parkinson’s disease involves a malfunction of the dopaminergic mechanism in the central nervous system [7,19]. As we know, dopaminergic neurotransmitters are essential in the production of coordinated movement [20,21]. Therefore, due to deficiencies in the dopaminergic system, this disease is characterized by motor symptoms such as stiffness, bradykinesia, tremors, coordination deficits and poor balance [20,21,22]. The progression of Parkinson’s disease can be considered according to the severity of symptoms [12,23], such as more important balance, speech, autonomic, cognitive and psychological disorders in more advanced stages [24]. Pharmacologic, surgical, psychological treatments and rehabilitation exist to alleviate the symptoms and limitations caused by the disease, associated or not with the effect of aging, but none aim to recovery [25].
Some evidence reported an impairment of balance among patients due to Parkinson’s disease [12,26,27], and this phenomenon, associated or not to the aging process, often, affects motor function, vision, vestibular system and proprioception of postural control [21,28,29]. In addition, a study reports worse postural control in the older adults with Parkinson’s versus the young Parkinson’s group [30]. However, few studies have assessed the impact of sex on postural control and health condition in older Parkinson individuals [31,32]. The results from these two studies were not completely related to force platform measurements only. In fact, Tassorelli et al. [31], which evaluated the functional balance of 42 individuals suffering from idiopathic Parkinson’s disease (mild-to-moderate severity), reported a greater degree of osteoporosis in their participants males than females (Z-score: M −3.8 ± 1.6, respectively) and that women fell more than men (fallers: 20 F/7 M; non fallers: 4 F/11 M), but not directly comparing the balance themselves. The second study [32] assessed the postural sway during quiet stance with eyes opened and eyes closed under force platform in 28 individuals with Parkinson’s disease and in 32 age- and sex-matched control subjects. The amount of postural sway in the patients was greater than in the control subjects, the higher level being most marked in patients with severe or long-duration of disease. The sex-related to differences on balance were again not reported for these authors. When looking for other types of disease (*ex: respiratory), apparently older women show better postural control under center of pressure measurements with a force platform than men in the same age group [33]. Wolfson et al. [34] (n = 234) demonstrated, however, that elderly healthy women show balance impairments when deprived of somatosensory and visual inputs and tend towards falling compared to elderly men.
To summarize, the results are controversial, as only from one population and task-dependent when the sex is of concern [35,36]. It would be interesting to know the actual profile of the literature review with regard to postural control based in force platform measurement in older people with Parkinson’s disease and if sex can really mediate the results. Thus, the main purpose of this study was to highlight the state-of-the-art literature regarding the results of the impact of Parkinson’s disease on postural control in older people and to determine if the person’s sex as well as other factors can mediate these results of balance.
2. Methodology
This systematic review (not related to a registered protocol) was conducted in alignment with checklist from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
2.1. Search Strategy and Studies Selection
The search was conducted in the form of a search until the years 2020. Two main databases were consulted to conduct this research: PubMed and EBSCO. Various combinations of keywords were used to minimize the risk of selection bias. In general, the following strategy was used: (“Postural Balance”[Mesh] OR “Force plat*” OR postural control OR balance) AND (“Aged”[Mesh] OR elder* OR age* OR Aging) AND (“Parkinson disease”[Mesh] OR “Parkinson” OR Parkinson older) AND (“Sex”[Mesh] OR Gender* OR Men* OR Women). In each database, filters for language (French and English), species (human) and without final publication date were applied. A total of 179 studies were found and analyzed for the first step of this research (see Figure 1).
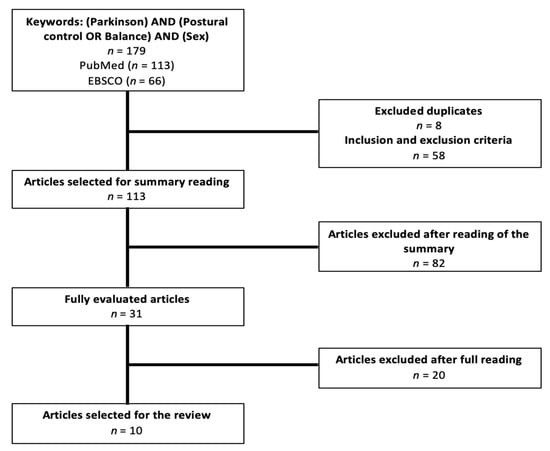
Figure 1.
Articles selection process.
Two reviewers carried out the initial search strategy in the databases, extracting the titles and abstracts. Subsequently, the selection of studies, evaluation, and data extraction, was conducted independently by two evaluators (two physiotherapists), based on the reading of titles and abstracts. Potentially eligible articles were read in full. A manual search was performed in the reference lists of all eligible articles, to find new references. Disagreement between physiotherapist evaluations was resolved through discussion or by consulting a third review author (RDS). The same form for data extraction was used by the authors.
The selection criteria included randomized and non-randomized studies: (i) includes a Parkinson aging population (≥65 years old), [32] includes postural control measurement from force platform, and (iii) men and women in the assessment. The articles were excluded if (i) written in a language other than French or English, [32] they did not present original content (i.e., literature reviews).
The duplicates (n = 8) and articles not respecting inclusion/exclusion criteria (n = 58) were removed to obtain a total of 113 articles corresponding to the research subject. Articles not related with this research subject or containing exclusion criteria were also removed as illustrated in the Table 1. The evaluators also elaborated a list of abbreviation with variables for help in the selection (Table 2). Then, a reading of the entire articles was done (n = 31) and exclusion criteria were applied. An evaluation of study quality was done, namely using the “Quality Assessment Tool for Studies with Diverse Designs” [37] and was finally reported in Table 3. Only 10 articles were ultimately selected for the literature review after final analysis as illustrated in the Figure 1.

Table 1.
Inclusion and exclusion criteria.

Table 2.
List of abbreviations.

Table 3.
Table from Quality Assessment Tool for Studies with Diverse Designs (QATSDD).
2.2. Data Extraction
First, a table reported the characteristics of Parkinson’s participants in the review such as age, sex, Hoehn and Yahr stage of disease and the number of participants for studies analyzed is shown in Table 4. Afterwards, the results for each study were compiled in table form, including the different groups, measurement tools used, goal of the study and main results of the literature (Table 5).

Table 4.
Characteristics of participants and measurements.

Table 5.
Summary of general results from studies.
3. Results
Ten (10) articles were analyzed in this literature review, cumulating 944 participants (534 men and 410 women) with a diagnosis of Parkinson’s disease (n = 665) and 226 participants in the control group. The quality of this study was around 22.1/42 ± 3.2 according to QATSDD, representing a moderate quality. All these studies were based in cross-sectional design so that without to establish the cause-effect on issue.
It is important to note that the two studies by Galna [38,39] included the same population so we included these results only once. The participants’ characteristics can be found in Table 4, including participants mean age which is 69.1 ± 3.7 years old and the duration of the Parkinson’s diagnosis which varies from 1 to 15 years. From the 10 studies, eight studies observed a Mini Mental State Examination (MMSE) score over 24/30, which included older people with Parkinson’s with cognitive impairment ranging from none to light mental state. A total of 534 men and 410 women took part in these studies. We observed that few studies briefly compared men and women (only two) and, across these, no statistically significant results were present regarding the impact of sex on Parkinson’s disease [31,32]. However, women in the study by Tassorelli et al. [31] demonstrated a lower level of functional independence (FIM = 98.9 ± 15.3 for men and 91.9 ± 16.6 for women), a lower Berg Balance Scale score (BBS = 51.9 ± 11.7 for men and 43.2 ± 12.8 for women) compared to men and a greater fear of falling than men (FES = 10.1 ± 6.7 for men and 20.9 ± 9.9 for women). Apparently, these results were not generalized for force platform measurements.
In addition, many measurement tools have been used among the selected studies to analyze balance and postural control of the participants, such as the GAITRite system, the Vicon, the Vitaport Activity Monitor, force platforms and other standardized tests or measurements (Berg Balance Scale, timed up and go, Unified Parkinson’s Disease Rating Scale, and Hoehn and Yahr Scale). Some studies have also used the inclinometer as a measurement tool of postural instability (Table 4 and Table 5). From these studies, Parkinson’s patients reported poor postural control when compared to those in control groups. It is also observed that severity [32,38,40] and cognitive state [41,42,43] for these patients were other factors that negatively affect postural control, but these studies do not report any differences between the sexes.
Galna et al.’s study (2013) [39] has shown that patients with Parkinson’s disease and with more severe motor impairments have higher postural instability during walking and striding an obstacle compared to the control group. Marchese et al. [41] that analyzed the variation of the pressure center on a force platform under different conditions, reported significant difference between-groups (Parkinson’s group vs. control group) in the variation of the center of pressure during the execution of a double task (associating cognitive and motor skills). Rochester et al. [44] 48also noticed some changes during double tasks (cognitive and motor) such as a decreasing walking speed in Parkinson’s group, supporting the impact of attentional capacity on dynamic balance during walking.
Viitasalo et al.’s study [32], that focused on postural balance with an inclinometer, noted a poor control in patients with a more severe stage of the disease as compared to the control group, without contrasting any differences in sex factor. Morris et al.’s study [45] demonstrated that patients with Parkinson’s disease have more difficulty keeping their balance during simple tasks, double tasks, verbal cognitive tasks, and when the base of support is reduced.
Finally, two studies including Parkinson’s over 10 evaluated the two sexes (males and females) from balance measures (graph length of COP and/or COP sway by force platform or inclinometer). Both studies [31,32] reported no direct comparison between-sexes, while only Viitasalo et al. [32] showed that men and women are comparable on postural control during force platform measurement.
4. Discussion
The aim of this study was to evaluate the impact of Parkinson’s disease on postural control in older adults and verify if sex can mediate the results. An update of the literature was necessary because the last review on this topic was in 2018, even searching up to 2020.
Although balance impairment in Parkinson’s is well known, only 10 articles were selected from this topic for analysis in older people and in sex differences related to balance. The impact of the disease on balance will be discussed first, followed by the impact of sex. In general, Parkinson’s disease alters the postural control of aged people and results are generalized for both sexes (n = 2 studies that compared the effect of sex on postural measures).
4.1. Impact of Parkinson’s Disease
During the process of aging, many factors are associated with a decrease in postural balance, such as the decrease of muscle mass and strength and the alteration of visual, vestibular, and proprioceptive systems [2,4,21,28,29]. It seems that age contributes to a transition between automatic postural control and an attentional, slowing down reaction rate to imbalance [4,41,45]. Parkinson’s disease exacerbates these effects [20,21,22]. Indeed, the literature demonstrates that the decrease in the secretion of dopamine in the substantia nigra in the brainstem is responsible for the main motor symptoms associated with Parkinson’s disease [20,21,22]. The decrease in postural control would be due to several factors, in particular by the increase in rigidity caused by the decrease in neurotransmitter production, which makes the trunk less flexible to disturbances therefore rendering the person with the disease more susceptible to be destabilized [20,21,22,29,46]. A decrease in postural reflexes would also be associated with this phenomenon [21,29,46]. However, although taking Levodopa reduces the severity of symptoms, it is not sufficient to eliminate them, suggesting that other structures may be responsible for the decrease in postural control in Parkinson’s patients [21,47,48].
Indeed, cholinergic cortical denervation would be an important marker of the slowing of walking in Parkinson’s disease [49]. Additionally, another post-mortem study on monkeys and patients with the disease demonstrated the importance of the role that cholinergic neurons of the pedunculopontine nucleus play walking and postural control deficits [48]. Damage to these structures would be, like the dopamine deficit, responsible for the appearance of rigidity, a reduction in stride length and a recurved posture, this affecting the patients’ ability to regain balance, in the event of a disturbance of the center of gravity [21,29,48]. Abnormalities would be more marked in people with an increased severity of the disease, explaining why anti-parkinsonian medication is not sufficient in these patients [21,47].
From the article selection, some studies evaluated the postural control by objective measurement using different tools, such as a force platform and GaitRite system to discriminate the differences between the Parkinson’s group versus the healthy-control group. A study of Tassoreli et al. evaluated stability with a stabilometric platform. Results showed significantly higher values (p < 0.001) for the Parkinson’s group compared to the control group for the graph length (1303.9 ± 656 mm vs. 987.3 ± 356 mm), amplitude of antero-posterior (29.7 ± 21.6 mm vs. 16.2 ± 6.4) and transverse oscillations (33.4 ± 17.1 mm vs. 15.2 ± 9.3 mm). In general, these studies showed a difference regarding postural oscillations in people with Parkinson’s disease compared to the control group when evaluated with a vertical inclinometer or placed at the waist [32,43], with a force platform [39] or with a motion analysis system in 3D VICON [32]. Indeed, balance is more affected in people with Parkinson’s than in healthy people during a static standing posture and during double tasks (opened and closed eyes, countdown, motor task: Thumb to fingers) on a force platform [31,41] or with other measurement methods [39,45]. These results are partly explained by the fact that people with Parkinson’s use conscious attentional strategies to compensate the impairment of basal ganglions, saturating their attention and making cortical control less efficient, highlighting balance impairments, especially during double tasks [41].
It is the same with internal perturbations, such as climbing over an obstacle, or external ones, which suggests that people with Parkinson’s disease have more difficulty managing disturbances on their center of mass and, therefore, more difficulty correcting their center of pressure to maintain balance [38,39]. Experimental balance conditions such as tandem or semi-tandem and one-legged stance tasks could discriminate a better impact of the disease on postural control than simple balance conditions, such as bipodal. In addition, unilateral impairment from the disease can affect the capacity to maintain such leg positions during balance performance [45]. Only the study of Tassorelli et al. [31] observed non-significant differences on oscillation speed, but range and length of range were higher in Parkinson’s disease people. These results seem to indicate that affected people oscillate at the same speed as the other group, but they take more time to react, which increases their oscillation distance.
The duration of the disease would have an impact on performance during different balance tasks [32,45]. Indeed, the duration of the disease (>5 years) would have a strong correlation between the increase of range and velocity of postural oscillations resulting in increased postural instability. However, it seems that severity would have a higher impact than duration of the disease on postural balance. Hiorth et al. [40] evaluated people with new and old diagnoses of Parkinson’s disease and a history of falls. This study concluded that fallers had a more severe manifestation of Parkinson’s disease. This conclusion suggests that postural instability would be more important when the disease and symptoms progress and would be characterized by higher and faster mediolateral oscillations. This would be due to a widespread pathology of the nervous system. Galna et al. (2013) [39] state the hypothesis that the more motor symptoms progress, the slower the postural reactions, leading to a greater imbalance.
In addition, the Unified Parkinson Disease Rating Scale (UPDRS), including the Hoehn and Yahr stage (UPDRS V), was used by many studies to determine the severity and the stage of disease progression [31,32,40,41,43]. From the 10 studies, three studies used at least one section of the UPDRS to quantify the severity of symptoms. However, only one completed all questionnaires. Tassoreli et al. [31] observed that the UPDRS score (mean = 30.8) was negatively correlated to the result of the Berg test and of the functional independence measure. They also observed a positive correlation between UPDRS and Fall Efficacy Scale. Viitasalo et al. [32] demonstrated that a UPDRS motor examination score above 10 corresponds to higher and faster oscillations compared to group control and patients with UPDRS motor examination score > 10. This is also true for the Parkinson’s disease group with a score over 25 [32]. Indeed, presence of a fall in the last year and presence of freezing were associated to a UPDRS score higher [43]. Hoehn and Yahr’s stage alone also had a significant impact on velocity, length, and area of postural oscillations during opened eyes tasks [32]. These results supports the impact of the severity and the stage of Parkinson’s disease on postural control.
According to several studies, the presence of a cognitive impairment in an individual with Parkinson’s disease increases the risk of falls [12,19,41,43]. For example, the mean time to perform TUG in Parkinson’s patients with dementia is significantly increased [42]. In addition, postural instability during a cognitive dual task in PD patients with cognitive impairment is greater than in PD patients without cognitive impairment or in the healthy elderly population [43]. Although the present study would concentrate on sex differences, it must be remembered that balance deficits in this population are more likely to be linked to dynamic and anticipatory postural adjustments during functional tasks, mainly when cognitive status is affected [41,42,43]. In short, the presence of cognitive impairment negatively impacts postural balance and increases the risk of falls in individuals with Parkinson’s [12,19,41,43].
Considering Parkinson’s disease and its deficiencies, most of the pharmacologic treatments include L-Dopa to ease motor symptoms. Indeed, several studies showed positive results with PD patients under L-Dopa treatments [50]. A study of Fahn et al. suggest that levodopa medication has prolonged effect on symptoms of Parkinson’s disease [51]. A recent study of Fowler et al. (2018) evaluate the effect of levodopa response on gait and balance of PD patients. They evaluated patients using the Mobility Lab System, equipped with sensors, to compare medications ON and OFF states. Results showed improvements in gait and balance such as speed, foot strike and stride length, but also, lumbar and trunk range of motion in balance [52].
4.2. Comparison between Sexes
Only two studies out of 10 assessed the two sexes from impact of Parkinson’s disease on balance. According to their brief investigation on the comparison between men and women, Viitasalo et al. [32] as well as Tassorelli et al. [31] demonstrated no statistically significant results between men and women. According to QATSDD, the quality of these studies is low to moderate (21/42 and 17/42), respectively. However, according to the results of Tassorelli et al. [31], women with Parkinson’s demonstrated a lower level of functional independence and of Berg Balance Scale score than men, as well as a greater fear of falling. The authors suggest that the difference between men and women is probably due to the phenotypical expression of the disease. Women presented the tremor-dominant phenotype, which affected the results of study. They also demonstrated a positive correlation between female sex and the frequency of falls. In fact, older women tend to fall more frequently than older men, which can lead to a greater fear of falling, as well as a decreased level of functional independence [53]. This tendency could be explained by a higher level of frailty in women compared to men, predisposing them to a higher risk of falling [54]. On the contrary, some studies have shown that older women have better postural control than older men when using a gold standard measure of balance such as force platform measures [54,55]. Apparently, women perform better than men in static balance tests under force platform measures. This could be due to the integration of the systems responsible for maintaining balance (vestibular, proprioceptive, and visual) which would be different in men and women. Women would be better at integrating information from different systems to maintain balance, while men perform better in dynamic balance tests compared to women, due in part to their often higher strength and muscle mass [33]. Therefore, more studies are needed to better distinguish the differences between sexes on postural control mainly in older people with Parkinson’s disease. Unfortunately, the conclusions from only two studies are very limited.
5. Conclusions
This review identified that older people with Parkinson’s have poor postural control through greater postural oscillations than those without the disease. The impact of sex should be further explored. The main clinical application of these results is that the interpretation of an evaluation of postural control on a force platform would be generalized for both sexes. However, more studies are needed to better answer this relevant research question on rehabilitation for older individuals with Parkinson’s when sex is of concern.
Author Contributions
Conceptualization, R.A.d.S., M.D., G.G., É.F., J.N.; methodology, M.D., G.G., É.F.; validation, S.M.S.S., H.A.G.d.O.A., M.R.d.O., S.N., J.B.; formal analysis, M.D., G.G., É.F.; investigation, M.D., R.A.d.S., J.B., S.N., S.C.,A.-F.S., J.N.; resources, G.G., É.F.; writing—original draft preparation, M.D., R.A.d.S.; writing—review and editing, A.-F.S., S.C., S.M.S.S., H.A.G.d.O.A., M.R.d.O., S.N., J.B., R.A.d.S., M.D.; visualization, S.C., A.-F.S., J.N.; supervision, R.A.d.S., S.N.; project administration, R.A.d.S., J.B.; funding acquisition, R.A.d.S.. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by [PDSMU CIUSSS SLSJ, QC, Canada] grant number [#300756] and M.D. was funded by OPPQ and PDSMU, QC, Canada [Master fellowship].
Conflicts of Interest
The authors declare no conflict of interest.
References
- Statistique Canada. Chiffres Selon L’âge et le Sexe, et Selon le Type de Logement: Fait saillants du Recensement de 2016. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/170503/dq170503a-fra.htm (accessed on 25 August 2021).
- Larsson, L.; Degens, H.; Li, M.; Salviati, L.; Lee, Y.I.; Thompson, W.; Kirkland, J.L.; Sandri, M. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 2018, 99, 427–511. [Google Scholar] [CrossRef] [PubMed]
- Harman, D. The aging process. Proc Natl Acad Sci USA 1981, 78, 7124–7128. [Google Scholar] [CrossRef] [PubMed]
- Baudry, S. Aging Changes the Contribution of Spinal and Corticospinal Pathways to Control Balance. Exerc. Sport Sci. Rev. 2016, 44, 104–109. [Google Scholar] [CrossRef]
- Gonzalez-Usigli, H.A. Maladie de Parkinson. Available online: https://www.merckmanuals.com/fr-ca/professional/troubles-neurologiques/troubles-du-mouvement-et-troubles-cérébelleux/maladie-de-parkinson (accessed on 25 August 2021).
- Agence de la santé publique du Canada. Système Canadien de Surveillance des Maladies Chroniques le Parkinsonisme au Canada, y Compris la Maladie de Parkinson. Available online: https://www.canada.ca/fr/sante-publique/services/publications/maladies-et-affections/parkinsonisme.html (accessed on 25 August 2021).
- Lew, M. Overview of Parkinson’s disease. Pharmacotherapy 2007, 27, 155S–160S. [Google Scholar] [CrossRef]
- Lima, M.G.; Barros, M.B.; Cesar, C.L.; Goldbaum, M.; Carandina, L.; Ciconelli, R.M. Impact of chronic disease on quality of life among the elderly in the state of Sao Paulo, Brazil: A population-based study. Rev. Panam. Salud Publica 2009, 25, 314–321. [Google Scholar] [CrossRef]
- Agrément Canada; Institut Canadien d’Information sur la santé; Institut Canadien Pour la séCurité des Patients. Prévention des Chutes: Des Données Probantes à L’amélioration des Soins de Santé au Canada. Canada. 2014. Available online: https://www.patientsafetyinstitute.ca/fr/toolsresources/Pages/Falls-resources-Getting-Started-Kit.aspx (accessed on 25 August 2021).
- Friedman, S.M.; Munoz, B.; West, S.K.; Rubin, G.S.; Fried, L.P. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J. Am. Geriatr. Soc. 2002, 50, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, N.; Metter, E.J.; Lauretani, F.; Bandinelli, S.; Guralnik, J.; Ferrucci, L. Activity restriction induced by fear of falling and objective and subjective measures of physical function: A prospective cohort study. J. Am. Geriatr. Soc. 2008, 56, 615–620. [Google Scholar] [CrossRef]
- Allen, N.E.; Schwarzel, A.K.; Canning, C.G. Recurrent falls in Parkinson’s disease: A systematic review. Parkinsons Dis. 2013, 2013, 906274. [Google Scholar] [CrossRef] [PubMed]
- Ministère de la Santé et des Services Sociaux (MSSS). La Prévention des Chutes Dans un Continuum de Services Pour les Aînés Vivant à Domicile; MSSS: Quebec, QC, Canada, 2005. [Google Scholar]
- Li, F.; Fisher, K.J.; Harmer, P.; McAuley, E.; Wilson, N.L. Fear of falling in elderly persons: Association with falls, functional ability, and quality of life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, P283–P290. [Google Scholar] [CrossRef]
- Murphy, S.L.; Williams, C.S.; Gill, T.M. Characteristics associated with fear of falling and activity restriction in community-living older persons. J. Am. Geriatr. Soc. 2002, 50, 516–520. [Google Scholar] [CrossRef]
- Statistique Canada Tableau 17-10-0134-01 Estimations de la Population (Recensement de 2016 et Données Administratives), Selon le Groupe d’âge et le Sexe au 1er Juillet, Canada, Provinces, Territoires, Régions Sociosanitaires (Limites de 2018) et Groupes de Régions Homologues. Available online: https://www150.statcan.gc.ca/t1/tbl1/fr/tv.action?pid=1710013401 (accessed on 24 September 2019).
- Wong, S.L.; Gilmour, H.; Ramage-Morin, P.L. La Maladie de Parkinson: Prévalence, Diagnostic et Conséquences; Stastique Canada: Ottawa, ON, Canada, 2014; Rapports sur la santé; Volume 25, pp. 11–16. [Google Scholar]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression, and mortality. Neurology 2001, 57, S11–S26. [Google Scholar]
- Rinne, J.O.; Portin, R.; Ruottinen, H.; Nurmi, E.; Bergman, J.; Haaparanta, M.; Solin, O. Cognitive impairment and the brain dopaminergic system in Parkinson disease: [18F]fluorodopa positron emission tomographic study. Arch. Neurol. 2000, 57, 470–475. [Google Scholar] [CrossRef] [PubMed]
- de Morand, A. Pratique de la Rééducation Neurologique, 2nd ed.; Elsevier Masson: Paris, France, 2014. [Google Scholar]
- Cabeleira, M.E.P.; Pagnussat, A.S.; do Pinho, A.S.; Asquidamini, A.C.D.; Freire, A.B.; Pereira, B.T.; de Mello Rieder, C.R.; Schifino, G.P.; Fornari, L.H.T.; Junior, N.D.S.; et al. Impairments in gait kinematics and postural control may not correlate with dopamine transporter depletion in individuals with mild to moderate Parkinson’s disease. Eur. J. Neurosci. 2019, 49, 1640–1648. [Google Scholar] [CrossRef]
- Levine, C.B.; Fahrbach, K.R.; Siderowf, A.D.; Estok, R.P.; Ludensky, V.M.; Ross, S.D. Diagnosis and treatment of Parkinson’s disease: A systematic review of the literature. Evid. Rep. Technol. Assess. 2003, 57, 1–4. [Google Scholar]
- de Almeida, I.A.; Terra, M.B.; de Oliveira, M.R.; da Silva Júnior, R.A.; Ferraz, H.B.; Santos, S.M.S. Comparing postural balance among older adults and Parkinson’s disease patients. Mot. Rev. Educ. Física 2016, 22, 261–265. [Google Scholar] [CrossRef]
- Wilczynski, J.; Pedrycz, A.; Mucha, D.; Ambrozy, T.; Mucha, D. Body Posture, Postural Stability, and Metabolic Age in Patients with Parkinson’s Disease. Biomed. Res. Int. 2017, 2017, 3975417. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, H.B.; Ferraresi, J.R.; Prata, M.G.; Scheicher, M.E. Postural balance and functional independence of elderly people according to gender and age: Cross-sectional study. Sao Paulo Med. J. 2017, 135, 260–265. [Google Scholar] [CrossRef]
- Santos, S.M.; da Silva, R.A.; Terra, M.B.; Almeida, I.A.; de Melo, L.B.; Ferraz, H.B. Balance versus resistance training on postural control in patients with Parkinson’s disease: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2017, 53, 173–183. [Google Scholar] [PubMed]
- Duncan, R.P.; Leddy, A.L.; Cavanaugh, J.T.; Dibble, L.E.; Ellis, T.D.; Ford, M.P.; Foreman, K.B.; Earhart, G.M. Detecting and predicting balance decline in Parkinson disease: A prospective cohort study. J. Parkinsons Dis. 2015, 5, 131–139. [Google Scholar] [CrossRef]
- Jiang, X.; Cooper, J.; Porter, M.M.; Ready, A.E. Adoption of Canada’s Physical Activity Guide and Handbook for Older Adults: Impact on functional fitness and energy expenditure. Can. J. Appl. Physiol. 2004, 29, 395–410. [Google Scholar] [CrossRef][Green Version]
- Hwang, S.; Agada, P.; Grill, S.; Kiemel, T.; Jeka, J.J. A central processing sensory deficit with Parkinson’s disease. Exp. Brain Res. 2016, 234, 2369–2379. [Google Scholar] [CrossRef]
- Roland, K.P.; Jones, G.R.; Jakobi, J.M. Parkinson’s disease and sex-related differences in electromyography during daily life. J. Electromyogr. Kinesiol. 2013, 23, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; Berlangieri, M.; Buscone, S.; Bolla, M.; De Icco, R.; Baricich, A.; Pacchetti, C.; Cisari, C.; Sandrini, G. Falls, fractures and bone density in Parkinson’s disease—A cross-sectional study. Int. J. Neurosci. 2017, 127, 299–304. [Google Scholar] [CrossRef]
- Viitasalo, M.K.; Kampman, V.; Sotaniemi, K.A.; Leppavuori, S.; Myllyla, V.V.; Korpelainen, J.T. Analysis of sway in Parkinson’s disease using a new inclinometry-based method. Mov. Disord. 2002, 17, 663–669. [Google Scholar] [CrossRef]
- de Castro, L.A.; Ribeiro, L.R.; Mesquita, R.; de Carvalho, D.R.; Felcar, J.M.; Merli, M.F.; Fernandes, K.B.; da Silva, R.A.; Teixeira, D.C.; Spruit, M.A.; et al. Static and Functional Balance in Individuals with COPD: Comparison with Healthy Controls and Differences According to Sex and Disease Severity. Respir. Care 2016, 61, 1488–1496. [Google Scholar] [CrossRef]
- Wolfson, L.; Whipple, R.; Derby, C.A.; Amerman, P.; Nashner, L. Gender differences in the balance of healthy elderly as demonstrated by dynamic posturography. J. Gerontol. 1994, 49, M160–M167. [Google Scholar] [CrossRef]
- Hageman, P.A.; Leibowitz, J.M.; Blanke, D. Age and gender effects on postural control measures. Arch. Phys. Med. Rehabil. 1995, 76, 961–965. [Google Scholar] [CrossRef]
- Palazzo, F.; Nardi, A.; Lamouchideli, N.; Caronti, A.; Alashram, A.; Padua, E.; Annino, G. The effect of age, sex and a firm-textured surface on postural control. Exp. Brain Res. 2021, 239, 2181–2191. [Google Scholar] [CrossRef] [PubMed]
- Sirriyeh, R.; Lawton, R.; Gardner, P.; Armitage, G. Reviewing studies with diverse designs: The development and evaluation of a new tool. J. Eval. Clin. Pract. 2012, 18, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Galna, B.; Murphy, A.T.; Morris, M.E. Obstacle crossing in people with Parkinson’s disease: Foot clearance and spatiotemporal deficits. Hum. Mov. Sci. 2010, 29, 843–852. [Google Scholar] [CrossRef]
- Galna, B.; Murphy, A.T.; Morris, M.E. Obstacle crossing in Parkinson’s disease: Mediolateral sway of the centre of mass during level-ground walking and obstacle crossing. Gait Posture 2013, 38, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Hiorth, Y.H.; Lode, K.; Larsen, J.P. Frequencies of falls and associated features at different stages of Parkinson’s disease. Eur. J Neurol. 2013, 20, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Marchese, R.; Bove, M.; Abbruzzese, G. Effect of cognitive and motor tasks on postural stability in Parkinson’s disease: A posturographic study. Mov. Disord. 2003, 18, 652–658. [Google Scholar] [CrossRef]
- Fritz, N.E.; Kegelmeyer, D.A.; Kloos, A.D.; Linder, S.; Park, A.; Kataki, M.; Adeli, A.; Agrawal, P.; Scharre, D.W.; Kostyk, S.K. Motor performance differentiates individuals with Lewy body dementia, Parkinson’s and Alzheimer’s disease. Gait Posture 2016, 50, 1–7. [Google Scholar] [CrossRef]
- Latt, M.D.; Lord, S.R.; Morris, J.G.; Fung, V.S. Clinical and physiological assessments for elucidating falls risk in Parkinson’s disease. Mov. Disord. 2009, 24, 1280–1289. [Google Scholar] [CrossRef] [PubMed]
- Rochester, L.; Hetherington, V.; Jones, D.; Nieuwboer, A.; Willems, A.M.; Kwakkel, G.; Van Wegen, E. Attending to the task: Interference effects of functional tasks on walking in Parkinson’s disease and the roles of cognition, depression, fatigue, and balance. Arch. Phys. Med. Rehabil. 2004, 85, 1578–1585. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.; Iansek, R.; Smithson, F.; Huxham, F. Postural instability in Parkinson’s disease: A comparison with and without a concurrent task. Gait Posture 2000, 12, 205–216. [Google Scholar] [CrossRef]
- Rodriguez-Oroz, M.C.; Jahanshahi, M.; Krack, P.; Litvan, I.; Macias, R.; Bezard, E.; Obeso, J.A. Initial clinical manifestations of Parkinson’s disease: Features and pathophysiological mechanisms. Lancet Neurol. 2009, 8, 1128–1139. [Google Scholar] [CrossRef]
- Kempster, P.A.; Frankel, J.P.; Bovingdon, M.; Webster, R.; Lees, A.J.; Stern, G.M. Levodopa peripheral pharmacokinetics and duration of motor response in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 1989, 52, 718–723. [Google Scholar] [CrossRef]
- Karachi, C.; Grabli, D.; Bernard, F.A.; Tande, D.; Wattiez, N.; Belaid, H.; Bardinet, E.; Prigent, A.; Nothacker, H.P.; Hunot, S.; et al. Cholinergic mesencephalic neurons are involved in gait and postural disorders in Parkinson disease. J. Clin. Investig. 2010, 120, 2745–2754. [Google Scholar] [CrossRef]
- Bohnen, N.I.; Frey, K.A.; Studenski, S.; Kotagal, V.; Koeppe, R.A.; Scott, P.J.; Albin, R.L.; Muller, M.L. Gait speed in Parkinson disease correlates with cholinergic degeneration. Neurology 2013, 81, 1611–1616. [Google Scholar] [CrossRef]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef]
- Fahn, S.; Oakes, D.; Shoulson, I.; Kieburtz, K.; Rudolph, A.; Lang, A.; Olanow, C.W.; Tanner, C.; Marek, K. Levodopa and the progression of Parkinson’s disease. N. Engl. J. Med. 2004, 351, 2498–2508. [Google Scholar] [PubMed]
- Fowler, A.; Gernon, S.; Pahwa, R.; Lyons, K. Objective Evaluation of Levodopa Response on Gait and Balance (P2.041). Neurology 2018, 90, P2.041. [Google Scholar]
- Peel, N.M. Epidemiology of Falls in Older Age. Rev. Can. Vieil. 2011, 30, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Pereira, C.; Silva, R.A.D.; de Oliveira, M.R.; Souza, R.D.N.; Borges, R.J.; Vieira, E.R. Effect of body mass index and fat mass on balance force platform measurements during a one-legged stance in older adults. Aging Clin. Exp. Res. 2018, 30, 441–447. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).