Abstract
Cutaneous silica granulomas are a form of foreign-body granulomatous reactions. They are characterized histopathologically by sarcoidal granulomas in association with silica crystals. Asteroid bodies, a classical histopathological feature of sarcoidosis, have not previously been reported in association with silica granulomas. Herein, we present the case of an 83-year-old man with an asymptomatic papule on the vertex scalp. Histopathology revealed a dermal granulomatous reaction to silica crystals. Asteroid bodies were observed in the cytoplasm of multinucleated giant cells. In the absence of systemic symptoms or laboratory findings suggestive of sarcoidosis, a final diagnosis of silica granuloma with asteroid bodies was made. While they have been observed in several other granulomatous reactions, the present case represents a novel association of asteroid bodies with silica granulomas.
1. Introduction
Cutaneous silica granulomas are a subset of foreign-body granulomatous reactions [1,2]. Although silica is a commonly occurring substance in the environment, few cases of cutaneous silica granulomas have been described. Clinically, they present as solitary or multiple papules or nodules months to years after inoculation of the skin with silica-containing materials, often through a traumatic or occupational exposure. History of previous trauma or scarring in the areas can potentially be clinical clues to this diagnosis. Histopathologically, cutaneous silica granulomas are characterized by mixed or sarcoid-like granulomatous infiltrates with multinucleated giant cells in association with irregular translucent crystalline structures of various sizes that are characteristically birefringent on polarized light microscopy.
Despite the close histopathologic resemblance of cutaneous silica granulomas and cutaneous sarcoidal granulomas, asteroid bodies—a typical histopathological feature of sarcoidosis—have not previously been reported in silica granulomas. Herein, we describe a novel case of cutaneous silica granuloma associated with asteroid bodies. Physicians should be aware of the possibility of observing asteroid bodies in both sarcoidosis and foreign-body granulomatous reactions, including cutaneous silica granulomas.
2. Case Report
An 83-year-old man with a history of cutaneous squamous cell carcinoma, prostate cancer, and hypothyroidism presented with an 8 mm depressed pinkish papule on the vertex scalp (Figure 1). Though he admitted to picking at the lesion, he denied any associated symptoms. Given clinical concern for squamous cell carcinoma in situ, a shave biopsy was obtained.

Figure 1.
Clinical image of 8 mm depressed pinkish papule on the vertex scalp, circled in red.
Histologic examination revealed a dermal granulomatous reaction with sarcoidal and tuberculoid granulomas (Figure 2a,b). Multiple asteroid bodies were observed in the cytoplasm of foreign-body-type multinucleated giant cells near translucent amorphous crystalline foreign bodies of various sizes (Figure 2c,d) that were birefringent on polarization (Figure 2e,f), consistent with silica crystals. A review of systems for pulmonary and other systemic symptoms was negative, and radiographs of the chest were unremarkable. Additionally, the patient had no risk factors for tuberculosis or other granulomatous infections. In the absence of systemic symptoms or findings suggestive of sarcoidosis or infectious causes, and given the presence of silica particles on histology, a final diagnosis of silica granuloma with asteroid bodies was made.
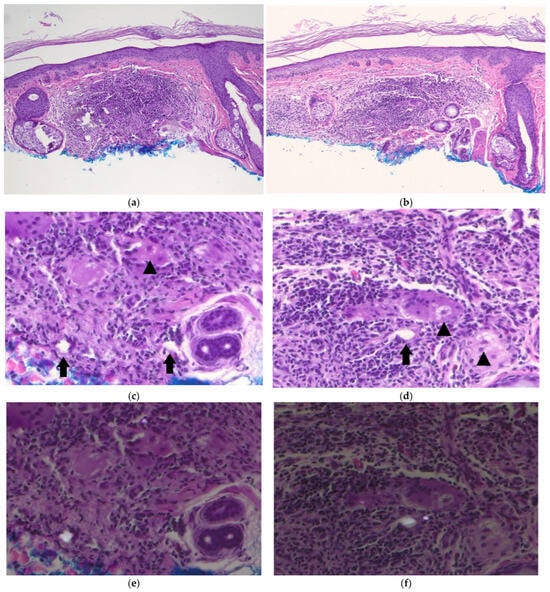
Figure 2.
Silica granuloma with asteroid bodies: (a,b) low-power view showing dense granulomatous infiltrate in the dermis (H&E, ×100); (c,d) high-power image of the infiltrate, composed of lymphocytes, eosinophils, and histiocytes with foreign-body-type giant cells, highlighting representative anisotropic crystalline material (arrows) and asteroid bodies (arrowheads) found within the granulomatous inflammation (H&E, ×400); (e,f) partial polarization of (c,d) to show polarization of silica crystals (H&E, ×400).
3. Discussion
Asteroid bodies are classically associated with sarcoidosis, but they are not at all pathognomonic, as our case highlights. The association of silica granulomas with asteroid bodies, to our knowledge, has not previously been reported, though it is not unexpected given the reports of asteroid bodies in several other types of foreign-body granulomas. Asteroid bodies have also been noted in various infectious and other granulomatous conditions (Table 1) [3,4].

Table 1.
Various conditions in which asteroid bodies have been described.
The composition of asteroid bodies and the mechanisms of their formation remain a matter of ongoing investigation. Some existing evidence suggests they are products of microtubular disarray, collagen trapping, or ubiquitin-associated cytoskeletal abnormalities [5,6,7]. Others have postulated that the unique morphology of giant cell asteroid bodies may be attributable to hydrophobic properties of complex lipid constituents, which presumably accumulate within upon fusion of macrophages into giant cells [8,9].
Cutaneous silica granulomas have been sparsely described, though some have proposed they are underreported and underdiagnosed [2,10]. Despite the paucity of cases in the literature, silica is widely prevalent in the environment, and exposure can thus occur in a multitude of environments. Cutaneous silica granulomas often occur in individuals with a history of traumatic introduction of glass, sand, or other silica-containing particles into the skin. Silica implantation may occur even with minor trauma, often many years prior to cutaneous granuloma formation; as a result, exposure events may not be readily identified in the clinical history, as was the case in our patient [1,11,12]. The pathogenesis of cutaneous silica granuloma and its prolonged latency time remains elusive; theories include conversion to colloidal silica over time, eventually leading to a granulomatous reaction, or a type of delayed hypersensitivity response [11,13]. Given the wide discrepancy between the frequency of silica in the environment and the occurrence of silica granulomas, it is plausible that certain individuals are predisposed to this type of foreign-body reaction [11,14].
Silica foreign-body granulomas and sarcoidal granulomas can have near-identical histopathologic pictures, differentiated primarily by the presence of polarizable foreign bodies in the former. This finding was once generally understood to exclude a diagnosis of sarcoidosis, though more recent reports suggest that the boundaries may not be so clear. Several cases of systemic sarcoidosis have been reported in which polarizable foreign bodies are detected in cutaneous granulomatous lesion specimens [15,16,17]. Additionally, cases of cutaneous silica granuloma evolving into systemic sarcoidosis have been reported [18]. Our observation of asteroid bodies in silica granulomas adds to a histopathological picture that overlaps with sarcoidosis, highlighting the importance of clinico-pathological correlation.
The optimal management of patients with cutaneous silica granulomas remains unclear. For limited cutaneous disease, excision is often performed with good effect, though recurrences are not uncommon [19]. Spontaneous resolution over several months has been noted in several cases [19].
While rare, the present case suggests that asteroid bodies can occur in silica foreign-body reactions in the absence of sarcoidosis. Clinicians and pathologists should be mindful of the overlapping presentation of foreign-body granulomas and sarcoidosis, which requires clinicopathological correlation.
Author Contributions
Conceptualization, C.D.; methodology, C.D.; writing—original draft preparation, F.A.; writing—review and editing, F.A. and C.D.; visualization, C.D.; supervision, C.D.; project administration, C.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This article does not qualify as human subjects research and is therefore exempt from review per IRB guidelines.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Finley, J.; Knabb, J. Cutaneous Silica Granuloma. Plast. Reconstr. Surg. 1982, 69, 340–343. [Google Scholar] [CrossRef] [PubMed]
- Mowry, R.G.; Sams, W.M., Jr.; Caulfield, J.B. Cutaneous Silica Granuloma: A Rare Entity or Rarely Diagnosed? Report of Two Cases With Review of the Literature. Arch. Dermatol. 1991, 127, 692–694. [Google Scholar] [CrossRef] [PubMed]
- Rolim, L.S.A.; da Silva Barros, C.C.; Pinheiro, J.C.; de Oliveira, P.T.; de Souza, L.B.; de Andrade Santos, P.P. Analysis of nine cases of oral foreign body granuloma related to biomaterials. J. Biosci. 2019, 44, 78. [Google Scholar] [CrossRef]
- Shahrabi-Farahani, S.; Lerman, M.A.; Noonan, V.; Kabani, S.; Woo, S.B. Granulomatous foreign body reaction to dermal cosmetic fillers with intraoral migration. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2014, 117, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.W. Weedon’s Skin Pathology, 5th ed.; Elsevier Limited: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Gadde, P.S.; Moscovic, E.A. Asteroid bodies: Products of unusual microtubule dynamics in monocyte-derived giant cells. An immunohistochemical study. Histol. Histopathol. 1994, 9, 633–642. [Google Scholar] [PubMed]
- Okamoto, K.; Hirai, S.; Yoshida, T.; Iizuka, T.; Tanaka, S. Asteroid Bodies in Silicone-induced Granuloma are Ubiquitinated. Acta Pathol. Jpn. 1992, 42, 688–689. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.S.; Drachenberg, C.B.; Papadimitriou, J.C. Structural Similarities between Hematoidin Crystals and Asteroid Bodies: Evidence of Lipid Composition. Exp. Mol. Pathol. 2001, 70, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Papadimitriou, J.C.; Drachenberg, C.B. Ultrastructural analysis of asteroid bodies: Evidence for membrane lipid bilayer nature of components. Ultrastruct. Pathol. 1992, 16, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Boztepe, G.; Rakhshanfar, M.; Erkin, G.; Ozkaya, O.; Sahin, S. Cutaneous silica granuloma: A lesion that might be clinically underdiagnosed. Eur. J. Dermatol. 2005, 15, 194–195. [Google Scholar] [PubMed]
- Wang, Z.S.; Li, J. Firm Papules and Nodules on Face, Neck, and Thorax. JAMA Dermatol. 2018, 154, 953–954. [Google Scholar] [CrossRef] [PubMed]
- Morales-Neira, D. It’s elemental! Siliceous diatom frustules producing sarcoid-like granulomas in the subcutis. J. Cutan. Pathol. 2021, 48, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Shelley, W.B.; Hurley, H.J. The Pathogenesis of Silica Granulomas in Man: A Non-Allergic Colloidal Phenomenon *. J. Invest Dermatol. 1960, 34, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, L.; Barnadas, M.; Vidal, D.; Sancho, F.; Fontarnau, R.; Alomar, A. Simultaneous Presentation of Silicone and Silica Granuloma. Dermatology 2002, 205, 162–165. [Google Scholar] [CrossRef] [PubMed]
- Marcoval, J.; Mañá, J.; Moreno, A.; Gallego, I.; Fortuño, Y.; Peyrí, J. Foreign Bodies in Granulomatous Cutaneous Lesions of Patients With Systemic Sarcoidosis. Arch. Dermatol. 2001, 137, 427–430. [Google Scholar]
- Kim, Y.C.; Triffet, M.K.; Gibson, L.E. Foreign Bodies in Sarcoidosis. Am. J. Dermatopathol. 2000, 22, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Colboc, H.; Moguelet, P.; Bazin, D.; Bachmeyer, C.; Frochot, V.; Weil, R.; Letavernier, E.; Jouanneau, C.; Daudon, M.; Bernaudin, J.F. Physicochemical characterization of inorganic deposits associated with granulomas in cutaneous sarcoidosis. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Payne, C.M.; Thomas, R.H.; Black, M.M. From silica granuloma to scar sarcoidosis. Clin. Exp. Dermatol. 1983, 8, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Bovenmyer, D.A.; Landas, S.K.; Bovenmyer, J.A. Spontaneous resolution of silica granuloma. J. Am. Acad. Dermatol. 1990, 23 Pt 1, 322–324. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).