Abstract
Introduction: The HIV/AIDS prevention program among pregnant mothers aims to reduce the risk of HIV transmission from mother to baby. It also aims to reduce stigma and discrimination, as well as deaths due to HIV/AIDS. This paper aimed to find out obstacles that occur in the implementation of HIV/AIDS transmission program in Indonesia. Methods: Online literature search was done on Google Scholar, Science Direct and PubMed databases with the keywords related to “HIV/AIDS” and transmission prevention program among mothers to children. The search resulted in a total of 343 articles. Results: After the abstracts were reviewed, there were only 16 articles selected. Conclusions: The implementation of the program in Indonesia has been run but is not yet optimal because of several obstacles i.e., the insufficient number of health workers and poor knowledge of health workers. Figuring out solutions to the obstacles could ease the program implementation to reduce the cases of HIV/AIDS. Obstacles were found in the implementation of the HIV/AIDS prevention program among mothers and children in Indonesia.
Introduction
Acquired immune deficiency syndrome (AIDS) is a disease resulting from the infection with human immunodeficiency virus (HIV) that causes the body’s immune system to weaken. This disease is spread through sex, injection needles, blood transfusions, and pregnancy and delivery from mother to child. [1] According to the latest 2022 report by UNAIDS, the number of children infected with HIV is lower than it was a decade ago. In 2021, the number of new HIV infections among children (ages 0 to 14 years) was approximately 160,000 (110,000-230,000). Previous research reported why and where this infection still occurs. Analysis of data from HIV programmes showed that almost half of new HIV infections in children are due to HIV-positive women not receiving antiretroviral therapy. HIV services are missing these women, many of whom avoid HIV services for fear of stigma and discrimination. [2]
The Ministry of Health Republic of Indonesia data in 2021 among children aged 0 to 14 years estimated new HIV infections around 3200 (2700–3700), deaths due to AIDS around 2400 (2000–2800) and the coverage of receiving antiretroviral treatment (ARV) around 25% (22-27%). Data showed that pregnant women needing ARV for prevention of mother-to-child transmission (PMTCT) represented around 10,000 (8900–12000), while pregnant women who received ARV for PMTCT were around 1520. [3] HIV Prevention Program from Mother to Children aims to reduce the risk of HIV transmission from mother to baby during pregnancy and delivery. Moreover, it reduces stigma and discrimination, as well as deaths. [4]
The risk of HIV transmission during pregnancy is 5-10%, and it is higher during delivery (10-20%) and breastfeeding (5-20%). The overall risk of HIV transmission from mother to child is 20-50%. [5] An effective intervention to prevent HIV transmission among mothers and children is required. With available interventions, the risk of a child contracting HIV from a mother can be reduced to less than 2%. [6] However, not all countries have similar effective interventions. Indonesia has very low HIV testing coverage among pregnant women when compared to other ASEAN countries that have decentralized HIV services, Indonesia has only 28%. For example, in 2015, Malaysia reached 95%, Thailand 95%, and Myanmar 83%. With the continuation of HIV transmission from mother to child, Indonesia has not been able to break the chain of transmission, which implies that the transmission continues into the next generation. [7]
The program will increase the number of women tested and treated, shorten treatment time, reduce HIV transmission and increase patient satisfaction. Interventions considered strong, simple, and good, may pose positive impacts, but they depend on the norms and values of the implementer. [8]
Interventions will be effective if the government and health workers can identify the barriers that slow down the intervention implementation. Therefore, this literature review aims to determine how far the HIV/AIDS prevention program has progressed in Indonesia and what obstacles remain in its implementation.
Methods
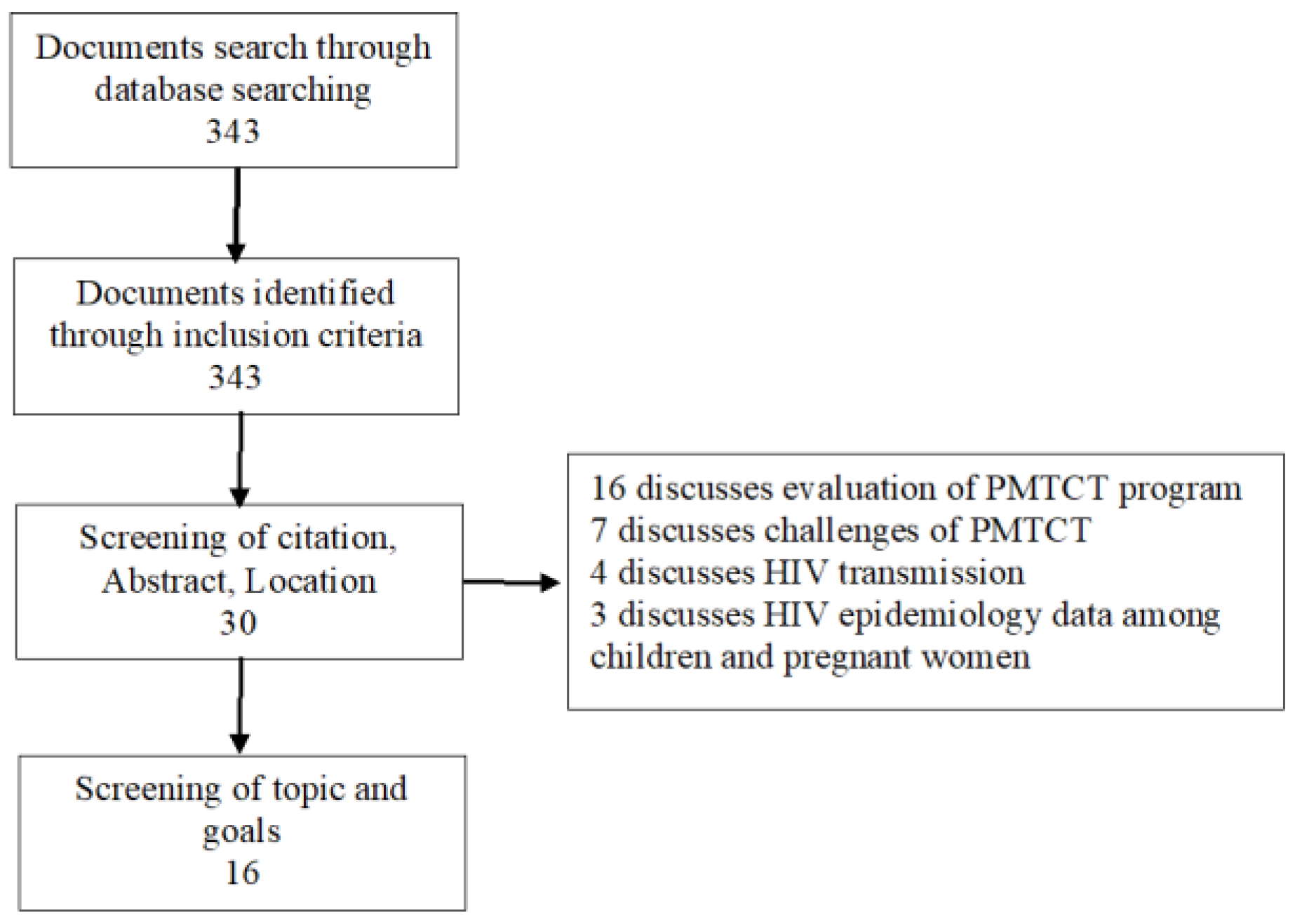
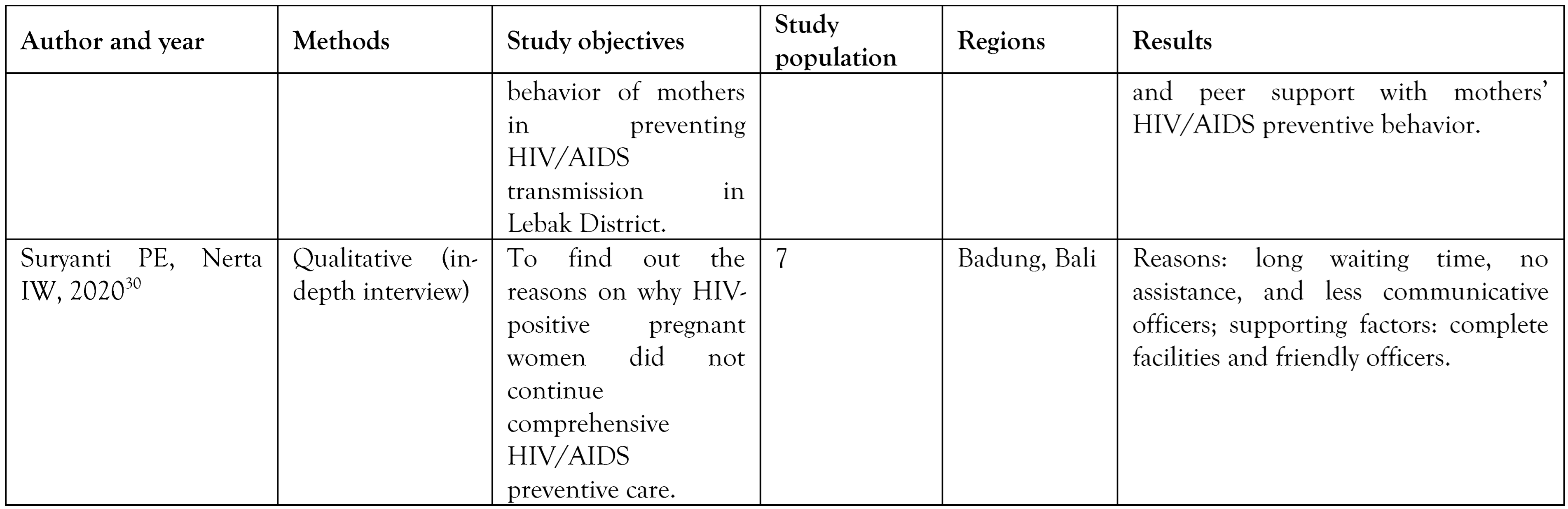
This article is a review of previous research on relevant variables and objectives. The articles were searched on Google Scholar, Science Direct and PubMed. The keywords used to find similar articles were “HIV/AIDS” and “Prevention Program among Mother to Child (PMTCT)”. The search resulted in 343 articles which were then screened according to inclusion criteria. Studies were chosen based on the following inclusion criteria: (1) HIV epidemiology data in the world; (2) the studies of mother-to-child HIV/AIDS prevention programs; (3) the challenge of PMTCT; (4) the full-text of the articles is accessible; and (5) the studies were published in Indonesia and in English between 2013-2022 or within ten years. Studies in the form of case reports/case series were excluded. After the screening, 141 articles were obtained. The abstracts of articles were read again and selected. Considering free full text available, this study obtained 30 articles. Then the final selection step was screening full texts that have relevant variables and objectives. Sixteen articles were finally analyzed (Figure 1).
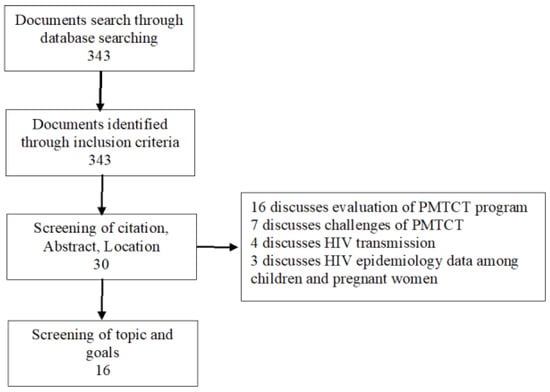
Figure 1.
Article screening diagram.
Results
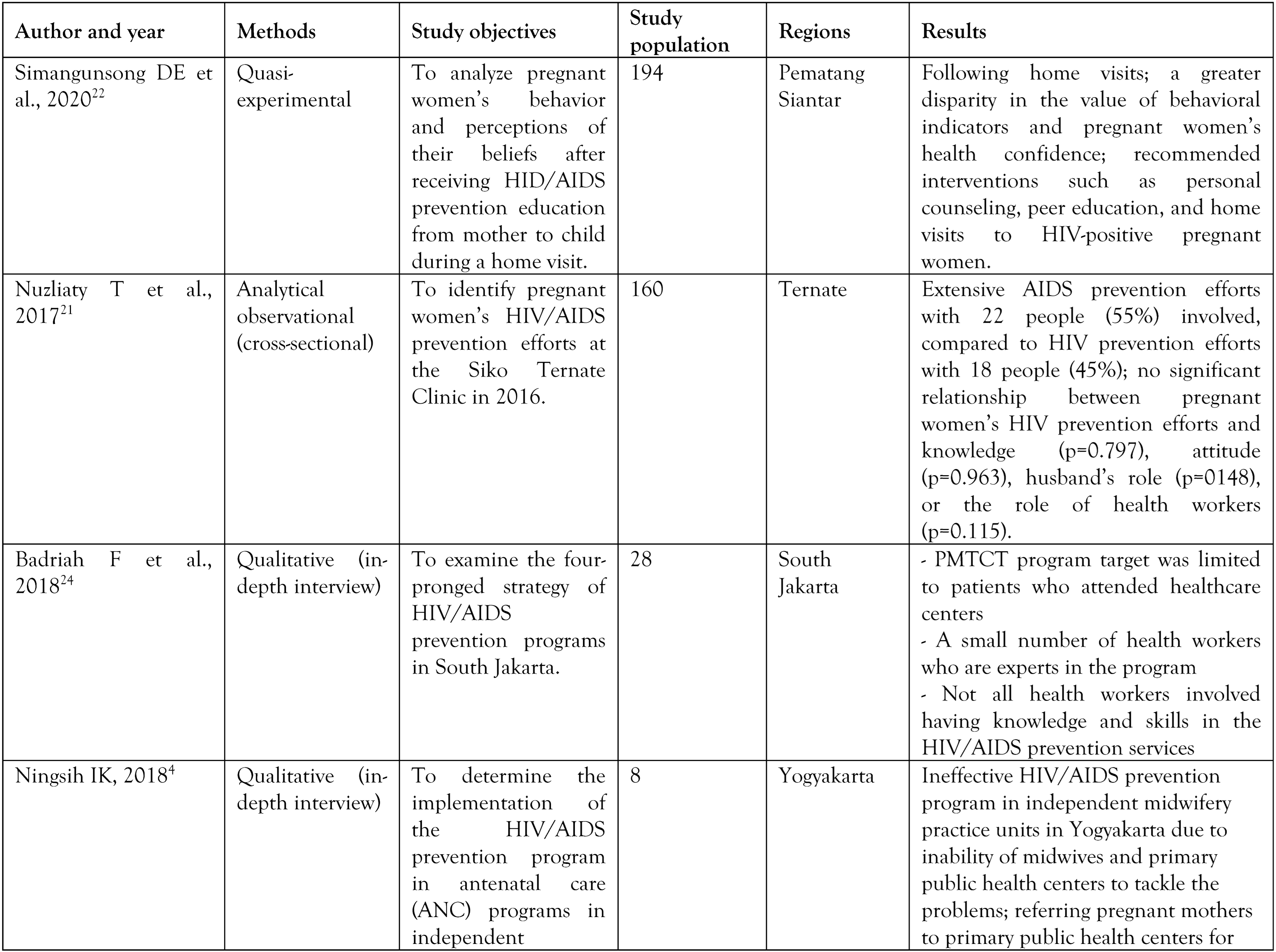
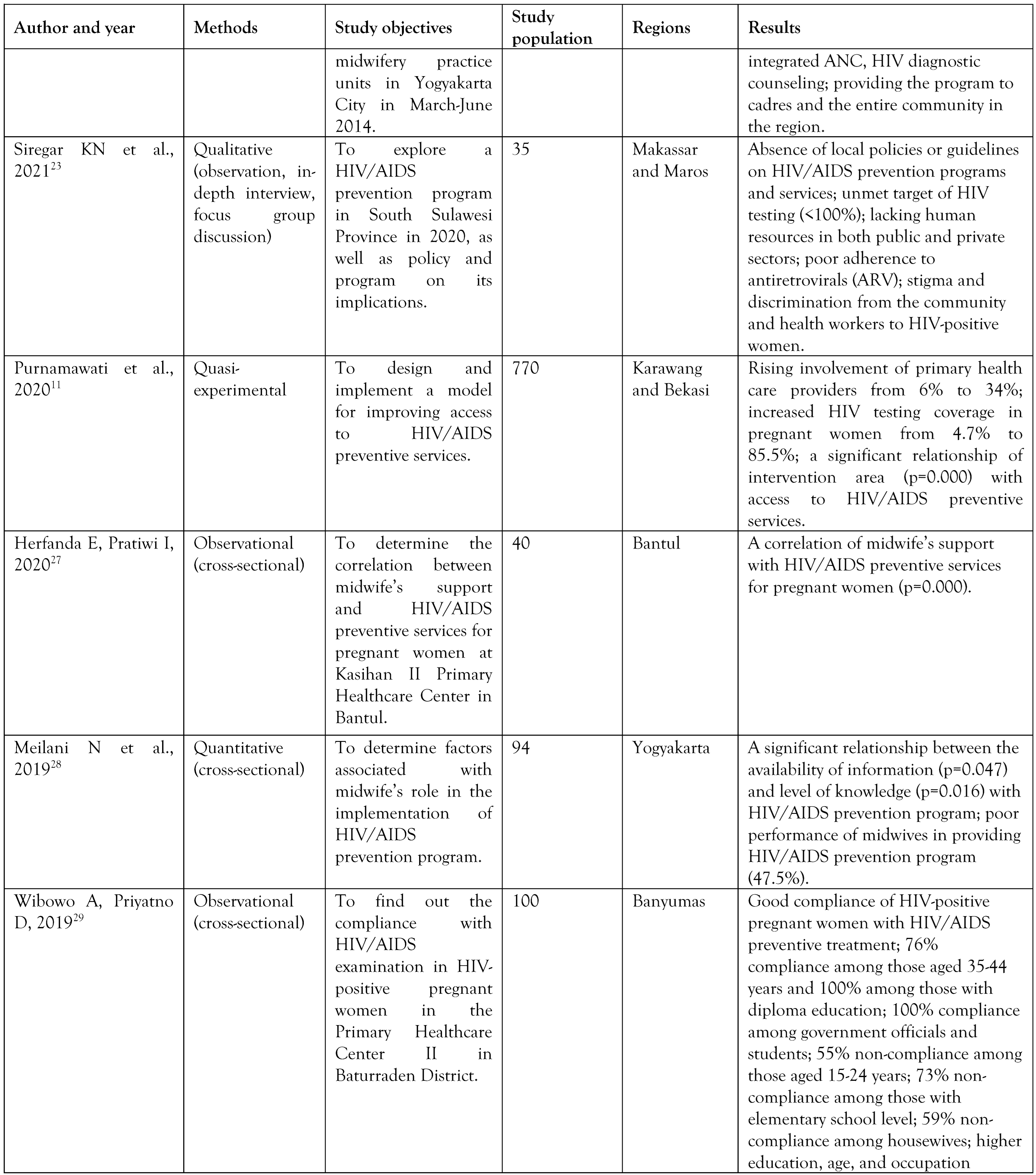
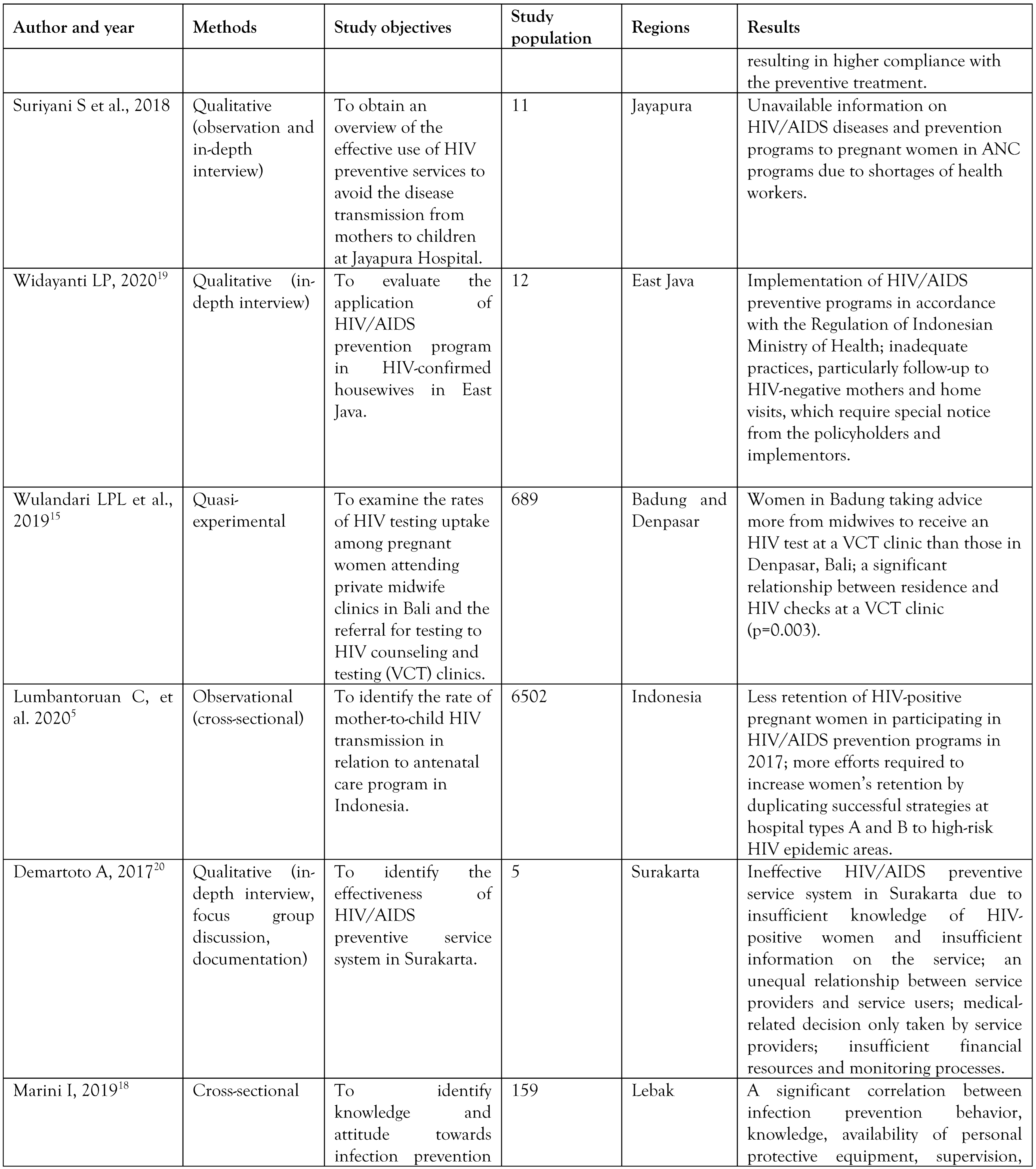
A total of 16 studies investigated HIV/AIDS Prevention Program among mothers and children in Indonesia. Table 1 summarizes the details of the included studies.

Table 1.
Results of literature review.
Discussion
The HIV/AIDS prevention program works to prevent the transmission of HIV/AIDS from mother to baby. In its implementation, the program has four pillars as follows: [9]
- (a)
- Pillar 1: Prevention of HIV transmission in women of reproductive age
The most effective early step to prevent HIV transmission to infants is to avert women of reproductive age from contracting HIV. This primary prevention prevents HIV transmission from an early stage, even before sexual intercourse occurs. It gives precautions to young women of reproductive age, pregnant women and their partners not to be infected by HIV. Thus, the possibility of HIV transmission from mother to baby is lower. [9]
- (b)
- Pillar 2: Preventing unplanned pregnancy in women confirmed with HIV infection
Women living with HIV and their partners need to plan carefully before deciding to have children. They need special pregnancy care to ensure their safety in childbirth, postpartum and breastfeeding. One of the medical concerns they have to be aware of is to avoid pregnancy complications and low immunity; they can still continue their lives, socialize and work as usual if they receive regular proper treatment and care. They can also have children who are free of HIV if they plan their pregnancy properly. To propel their behavior to these goals, they need to take advantage of services that provide contraceptive information and means of preventing unplanned pregnancies. [9]
- (c)
- Pillar 3: Preventing mother-to-baby HIV and syphilis transmission
In pregnant women with HIV who do not receive preventive treatment and care, the risk of transmission to infants ranges from 20-50%. In contrast, with proper measures, the risk of transmission can be reduced to less than 2%. With regular ARV treatment and good care, pregnant women with HIV infection can give birth to HIV-free children through vaginal delivery and potentially continue breastfeeding their babies after delivery. Moreover, providing adequate therapy for mothers with syphilis can prevent the occurrence of congenital syphilis in their babies. [9]
- (d)
- Pillar 4: Psychological, social, medical and nursing support
Mothers with HIV infection need psychosocial support to get along and live their lives as usual. Medical support and care are needed to prevent complications due to decreased immunity. Hence, such support needs to be given to children and their families. [9]
According to the current findings, districts in Indonesia are still not ready to implement the HIV/AIDS prevention program as seen from the availability of infrastructure and facilities, attitudes and communication of officers, waiting time for access to service, and assistance from facilitators. [10] In fact, many present obstacles in the practice include limited numbers of human resources, lack of information, and lack of supporting facilities. Since few health workers are experts in HIV/AIDS preventive measures, the information on the subject is little explored. Moreover, the absence of local policies and guidelines makes the program undirected to target populations.
Implementation of the PMTCT program in Indonesia
The HIV/AIDS Prevention Program is a comprehensive service that includes Mother Child Health (MCH), family planning, reproductive health, and adolescent health. This service package must be implemented by all health facilities, government and private parties to promote public health and prevent such infectious diseases. [11] All stakeholders need to prepare infrastructure and facilities, officers who have positive attitudes and communication, effective service duration, and assistance to implement the program. [12]
The program could be one of the featured services in independent midwifery practice units in Indonesia. Thus, midwives are expected to provide counseling and support to women who are not infected with HIV or who are already infected with HIV. [10] They need to provide complete HIV and AIDS information to their clients until they will have to undergo testing. This is in line with research by Wardani (2019), stating that the higher level of knowledge about HIV, the higher the respondent’s interest in taking an HIV/AIDS test and vice versa. [13] Midwives also need to serve their clients friendly to attract their interest. Compliance of pregnant women with HIV/AIDS screening can reduce the transmission rates of HIV/AIDS, especially from mothers to children. [14]
Research conducted in South Sulawesi shows more frequent involvement of primary healthcare officers in HIV/AIDS preventive services increased from 6% to 34%. Additionally, the proportion of pregnant women who wished to have an HIV test also rose from 4.7% to 85.5%. Besides involvement of primary healthcare officers, a significant relationship was also found between regions where intervention takes place and access to the services. [11] For example, women living in Badung followed midwives’ advice more if considering an HIV test at a counseling and testing (VCT) clinic than those in Denpasar. Another study supports this finding, where place of residence is related to the frequency of HIV testing. [15]
In addition, midwife support may affect HIV testing too. Hence, midwives have a responsibility to accompany mothers and explain the HIV testing procedures. According to the current study, most midwives recommended pregnant women to get an HIV test as part of their antenatal care (ANC) program. In addition, midwives have to obtain consent from them before and after counseling and testing. They also need to encourage their clients’ husbands to participate in the prevention program. In carrying out the HIV testing procedures, midwives, however, fail to use appropriate protection equipment, such as gloves as prescribed in universal precautions. [15] This is in line with research done in Medan, where midwives did not perform the services according to psychological and social support guidelines. [16]
Obstacles in the implementation of the HIV/AIDS prevention program in Indonesia
Several obstacles remain in the HIV/AIDS Prevention Program in Indonesia. Due to limited numbers of human resources in both public and private services, it is not successfully run; the number of the program experts and skilled health workers in the fields is rare. [17] As a result, access to the HIV/AIDS preventive services is restricted to some groups, for example women who attended maternal and child services. [9]
The presence of midwives also determines the program success. Otherwise, pregnant women are referred to a primary healthcare center for ANC. [4] Research has revealed a relationship between midwife support and access to HIV/AIDS preventive services. [9] Besides, health workers’ knowledge about the service is also a contributing factor to a successful program in Indonesia. [18]
Furthermore, lack of local policies and guidelines for HIV/AIDS prevention programs and services leads to unmet HIV testing targets among pregnant women. Consequently, targeted groups lose their interest to use the services. [19] Additionally, the limited information about the PMTCT program also creates misunderstanding that women should have an HIV test only once they are pregnant. [20] Meanwhile, they have to have initiative to check their health beforehand.
Given the perception that antenatal care is only provided to women, most husbands feel no need to accompany their wives to prenatal check-ups. Whereas, their role is very important, especially in decision-making process. Their involvement is useful to avoid HIV transmission from mothers to children. [21]
Moreover, HIV-positive mothers also need to realize that the virus will remain in their body for the rest of their lives. Health workers might put stigma and discrimination against them because of this health state. As a result, infected mothers might face stumbling blocks in applying HIV/AIDS testing programs and later use health services less. [22]
Siregar et al. mention midwives refused HIV patients or were concerned when serving them. Stigma and discrimination from the community may prompt them to conceal their status. [23] Fear and shame on different treatment by health workers at worse cause HIV patients to skip follow-up appointments. [24] With good psychosocial support, HIV-positive mothers may be optimistic and eager to fill their lives and maintain their health and their children’s. [25]
Strategies to reduce the spread of HIV/AIDS
A study revealed that the best management strategy to tackle the spread of HIV/AIDS is to conduct cross-sectoral cooperation. Cooperation is carried out by involving three main elements: government elements through the District Health Office, health centers, hospitals, and other health services; community elements including community organizations, community leaders, and religious leaders; and youth elements including youth organizations, village cadres, and youth organizations in each region. The functions of each managerial item in tackling the spread of HIV/AIDS include 1) Planning: Health services conduct human resource planning, budget planning, and facilities and infrastructure planning; 2) Organizing: Each sector of the health service is in charge of conducting counseling, health checks, and recording. The village head, village officials, and sub-district head support the activities. Community organizations are tasked with assisting the campaign against the spread of HIV/AIDS after receiving knowledge about HIV/AIDS; 3) Actuating: The process of implementing HIV/AIDS countermeasures is based on two methods, namely, promotive and preventive. While the form of activities consists of counseling, examination, and assistance; 4) Controlling: Controlling is done to ensure the process of preventing the transmission of HIV/AIDS every month at regular intervals. [26]
Factors that support the successful prevention of HIV/AIDS transmission from mother to child
Internal factors: the motivation from within the patient to survive, a high level of awareness about the benefits of treatment, faith in religion or belief, and the motivation within the patient to recover are factors that play an important role in increasing compliance with taking medication and routinely checking their health by consulting the nearest service. Mothers with HIV/AIDS’s perception of the severity of the disease and belief in the benefits of treatment affect whether or not a person regularly attends treatment and consultation.
External factors: family support can provide encouragement in reducing pain and accelerating the healing process of a disease. Everyone who experiences pain needs encouragement from others, especially the closest people (family). The emotional pressure of HIV/AIDS sufferers due to stigma and shame can be reduced with the support of those closest to them.
The current results are important for policy makers in evaluating HIV/AIDS prevention program. In implementing this program, the first thing to consider is the availability and competency of health workers and experts in providing services and information to pregnant women with HIV/AIDS. In addition, services and facilities for mothers with HIV infection also need to be improved.
Some mandatory responsibilities of health workers in this program are providing information about HIV and its testing, administering HIV tests, sharing test results and serving clients with post-test counseling, making referrals to higher healthcare units, and giving support and treatment if test results are positive. The program could be reinforced through an integrated ANC program with counseling and mandatory HIV testing for pregnant women during the first ANC. Post-test counseling for pregnant women whose results are positive could address means of preventing the transmission of sexually transmitted diseases. Policies and local guidelines are needed in every region to guard the program implementation. Studies currently reviewed were located in the last five years, so further research needs to update the program evaluation in Indonesia.
The weakness of this study is that the studies did not investigate HIV/AIDS prevention programs in all regions of Indonesia. Therefore, the results do not represent the whole program implementation throughout the country.
Conclusions
In general, the majority of HIV/AIDS Prevention Program agenda were carried out in accordance with the Regulation of the Indonesian Ministry of Health. However, it is constrained by various obstacles such as limited numbers of health workers and poor knowledge of health workers and pregnant women about the program. Some aspects in the program that require improvement include follow-up in mentoring, home visits, and local policies. Therefore, the government has to formulate policies and provide education and training to health workers to improve their communication competence in serving patients. Additionally, they need to identify obstacles in the program implementation in each region to get better solutions.
Author Contributions
I.K.U. made contributions to research conceptualization, design, literature review and writing. R.R.I. made contributions to review and revise the manuscript. N.A. made contributions to review and revise the manuscript. A.N.H. made contributions to research conceptualization, design and revise the manuscript. N. made contributions to research conceptualization, design and revise the manuscript. S.Q.K. made contributions to research conceptualization, design, and approval of the final manuscript. All authors read and approved the final version of the manuscript.
Funding
None to declare.
Acknowledgments
The authors would like to acknowledge Research Center on Global Emerging and Re-emerging Infectious Diseases, Institute of Tropical Disease—Universitas Airlangga to facilitate this study.
Conflicts of Interest
All authors—none to declare.
Availability of Data
The data supporting the findings of this study are available within the article.
References
- World Health Organization. HIV and AIDS. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/hivaids (accessed on 1 March 2023).
- Joint United Nations Programme on HIV/AIDS. UNAIDS Global AIDS update 2022. 2022. Available online: https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update_en.pdf (accessed on 1 March 2023).
- Joint United Nations Programme on HIV/AIDS. UNAIDS Indonesia. 2021. Available online: https://www.unaids.org/en/regionscountries/countries/indonesia (accessed on 1 March 2023).
- Ningsih, I.K. Kajian Pencegahan Penularan HIVdari Ibu ke Anak pada Antenatal Care Oleh Bidan Praktik Mandiri di Yogyakarta. J Adm Kesehat Indones. 2018, 6, 61. [Google Scholar] [CrossRef]
- Lumbantoruan, C.; Kelaher, M.; Kermode, M.; Budihastuti, E. Pregnant women’s retention and associated health facility characteristics in the prevention of mother-to- child HIV transmission in Indonesia: Cross-sectional study. BMJ Open 2020, 10, e034418. [Google Scholar] [CrossRef] [PubMed]
- Negara, I.K.S.; Anantasika, A.; Putra, A.; Wiradnyana, A.; Tunas, I.K. Characteristics of pregnant women with HIV infection following prevention of mother to child transmission of HIV (PMTCT) program in Sanglah General Hospital 2005-2014. Bali Med J. 2016, 5, 147–151. [Google Scholar] [CrossRef]
- Gliddon, H.D.; Peeling, R.W.; Kamb, M.L.; Toskin, I.; Wi, T.E.; Taylor, M.M. A systematic review and meta-analysis of studies evaluating the performance and operational characteristics of dual point-of care tests for HIV and syphilis. Sex Transm Infect. 2017, 93, S3–S15. [Google Scholar] [CrossRef]
- Wiraharja, R.S.; Trisnantoro, L.; Mahendradhata, Y.; Praptoharjo, I. Challenges of PMTCT and MCHS integration in Indonesia, analysis by integration analysis framework and CFIR. J Kesehat Masy. 2019, 14, 359–368. [Google Scholar] [CrossRef]
- Ministry of Health Republic Indonesia. Guidelines for Prevention Program of Transmission of HIV, Syphilis and Hepatitis B from Mother to Child. 2019. Available online: https://siha.kemkes.go.id/portal/ppia# (accessed on 1 March 2023).
- Ariningtyas, N. Kendala Pelayanan Program PPIA Pada Antenatal Care Di Puskesmas Kota Yogyakarta Tahun 2015. J Kesehat Samodra Ilmu. 2017, 8, 137548. [Google Scholar]
- Purnamawati, D.; Djuwita, R.; Siregar, K.; Kamso, S.; Utomo, B.; Pratomo, H.; et al. Improving access to PMTCT services via a novel implementation model: Organizational support, health education, and HIV testing at the community level of West Java, Indonesia. Int J Heal Promot Educ. 2020, 58, 282–292. [Google Scholar] [CrossRef]
- Suryanti, Putu Emi IN. Reasons for HIV positive pregnant women not continuing comprehensive PMTCT care in the aspect of health services Institute of Hindu Dharma Negeri Denpasar I. 2020; 3, 13–21. [Google Scholar]
- Irnawati, Y.; Wulan, R. The Relationship between motivation and knowledge about PMTCT (prevention of mother-to child transmission of HIV) and willing to follow PMTCT in pregnant women satisfied with IMS Pati District. Community Publ Nurs. 2020, 8, 282–288. [Google Scholar] [CrossRef]
- Yuriati, P.; Handayani, O.W.K.; Raffy, R.E. Evaluation of the implementation of prevention of mother to child transmission (PMTCT) activities in pregnant women in Tanjungpinang City. Public Heal Perspect J. 2016, 1, 29–34. [Google Scholar]
- Wulandari, L.P.L.; Lubis, D.S.M.; Widarini, P.; Widyanthini, D.N.; Wirawan, I.M.A.; Wirawan, D.N. HIV testing uptake among pregnant women attending private midwife clinics: Challenges of scaling up universal HIV testing at the private sectors in Indonesia. Int J Health Plann Manage. 2019, 34, 1399–1407. [Google Scholar] [CrossRef]
- Harahap, S.; Tukiman, M.K.; Syarah, V. Perilaku Bidan KIA/KB dalam Pelaksanaan Program Prevention of Mother to Child Transmission (PMTCT) di Rumah Sakit Haji Kota Medan Tahun 2013. 2013; 34, 1–10. [Google Scholar]
- Ardani, I.; Handayani, S. Stigma terhadap Orang dengan HIV/AIDS (ODHA) sebagai Hambatan Pencarian Pengobatan. Bul Penelit Kesehat. 2017, 45, 81–88. [Google Scholar] [CrossRef]
- Marini, I. Hubungan Pengetahuan dan Sikap Bidan dengan Perilaku Pencegahan Infeksi dan Pencegahan Penularan HIV dari Ibu ke Anak (PPIA). J Midpro. 2019, 11, 54. [Google Scholar] [CrossRef]
- Widayanti, L.P. Evaluasi PMTCT (Prevention Mother To Child Transmission) pada IRT dengan HIV di Jatim. J Heal Sci Prev. 2020, 4, 32–41. [Google Scholar] [CrossRef]
- Demartoto, A. The representation of prevention-of-mother-to-child transmission service system in Surakarta Indonesia. J Kesehat Masy. 2017, 13, 191–200. [Google Scholar] [CrossRef]
- Nuzliaty, T.; Nurkila, S.; Karimah, S. Upaya Ibu Hamil Dalam Pencegahan Penularan Hiv Dari Ibu Ke Bayi Di Puskesmas Siko Ternate Tahun 2016. Link. 2017, 13, 51. [Google Scholar] [CrossRef][Green Version]
- Simangunsong, D.E.; Sianipar, K.; Purba, J. Preventions of HIV/AIDS transmission from mother to child in Pematangsiantar City, Indonesia. Glob J Health Sci. 2020, 12, 83. [Google Scholar] [CrossRef]
- Siregar, K.N.; Hanifah, L.; Rikawarastuti; Wahyuniar, L. Prevention of HIV transmission from mother to child: Challenges to the successful program implementation and practice in Indonesia. J Int Assoc Provid AIDS Care. 2021, 20, 23259582211040701. [Google Scholar] [CrossRef]
- Badriah, F.; Tahangnacca, M.; Alkaff, R.; Abe, T.; Hanifah, L. Implementation of program for the prevention of mother-to-child transmission of HIV in South Jakarta. Kesmas 2018, 12, 159–164. [Google Scholar] [CrossRef]
- Wati, Y.I.; Wulan, R. Hubungan Motivasi dan Pengetahuan tentang PMTCT (Prevention of Mother-To Child Transmission of HIV) dengan Kesediaan mengikuti PMTCT pada Ibu Hamil Penderita IMS (Infeksi Menular Seksual) di Kabupaten Pati. Coping Community Publ Nurs. 2020, 8, 282. [Google Scholar] [CrossRef]
- Pps, J.; Ripnowati, D.; Hartati, C.S.; Putro, G. Manajemen Pelayanan Penanggulangan HIV/AIDS Dalam Upaya Screening Di Puskesmas Temayang Kabupaten Bojonegoro. J Manajerial Bisnis. 2019, 2, 230–243. [Google Scholar] [CrossRef]
- Herfanda, E.; Pratiwi, I. Hubungan dukungan bidan dengan pemeriksaan PMTCT pada ibu hamil. J Kebidanan Kestra. 2020, 3, 6–12. [Google Scholar] [CrossRef]
- Meilani, N.; Setiyawati, N.; Barasa, S.O. Midwife’s role in the mother-to-child transmission prevention program in primary health care in Yogyakarta. Kesmas. 2019, 14, 88–94. [Google Scholar] [CrossRef]
- Wibowo, A.; Priyatno, D. Gambaran Kepatuhan Pemeriksaan PPIA (Pencegahan Penularan HIV dari Ibu Ke Anak) Ibu Hamil dengan Risiko HIV (Human Immunodeficiency Virus). Jar Lab Medis. 2019, 1, 38. [Google Scholar] [CrossRef]
- Suryanti, P.E.; Nerta, I. Alasan Ibu Hamil HIV Positif Tidak Melanjutkan Perawatan PPIA Komprehensif dalam Aspek Layanan Kesehatan. J Yoga dan Kesehat. 2020, 3, 13–21. [Google Scholar] [CrossRef]
© GERMS 2023.