Abstract
Background: Adverse childhood experiences (ACEs) such as abuse (defined as emotional, physical, or sexual abuse without distinguishing type or severity) have long been linked to mental health challenges in adulthood. However, less is known about how these effects differ by sex/gender in global samples, particularly using large-scale, multi-country panel data. Objectives: To examine whether the long-term association between childhood abuse and changes in depressive symptoms during adulthood differ between men and women, after adjusting for demographic and socioeconomic factors. Methods: We conducted a secondary analysis of Waves 1 and 2 of the Global Flourishing Study (GFS), a longitudinal panel study covering 22 diverse countries. The sample included adult participants with complete data on childhood abuse (yes/no); depression at baseline and follow-up; sex/gender; and relevant covariates (age; education; marital status; immigration status; smoking status; and employment). Depression was measured using a two-item scale. Multi-group structural equation models were used to test the effect of ACE on changes in depression over time where groups were defined based on sex/gender. Results: Overall, childhood abuse was associated with a statistically significant increase in depression scores between Wave 1 and Wave 2. This association was significant among women but not among men. Conclusions: Our findings suggest that the mental health consequences of childhood abuse extend into adulthood and disproportionately affect women. These sex/gender differences may reflect variations in stress processing; coping; and social roles. Interventions addressing early adversity may need to be tailored to recognize and respond to such sex/gender-specific vulnerabilities.
1. Introduction
Depression is more common among women and girls than men and boys [1], and various biopsychosocial underlying mechanisms have been proposed to explain this disparity, ranging from hormonal differences (sex differences) to patterns of stress exposure (gender differences) [2]. For example, the COVID-19 pandemic has led to increased rates of depression and anxiety, particularly among women. One review explored the underlying contributors to these sex differences, discussing transcriptomic and genetic factors, neuroendocrine regulation, immune function, and cognitive processes. The authors also examined sex differences in antidepressant response and their potential biological underpinnings. They emphasized the critical importance of integrating sex as a biological variable in both preclinical and clinical studies to facilitate the discovery of more effective pharmacotherapies for all genders [3].
Adverse childhood experiences (ACEs) have been consistently linked to poor mental health outcomes in adulthood, particularly depression [4,5]. Experience of abuse during childhood can disrupt developmental and emotional trajectories and increase vulnerability to psychopathology [6,7]. However, growing evidence suggests that these effects are not uniform across population subgroups, particularly those based on sex and gender. One hypothesis suggests that females may be more susceptible to stressors such as adverse childhood experiences (ACEs), including child abuse (defined as emotional, physical, or sexual abuse without distinguishing type or severity), compared to males [8]. It has been proposed that women are more likely to be risk-averse [9] and ruminate in response to stress or loss, which may increase their vulnerability to the effects of ACEs on depression risk [10,11]. According to this perspective, even at the same level of stress exposure, psychological and emotional outcomes such as depression may be more severe for women and girls than for men and boys [11].
Numerous review articles [3,12] and empirical studies [13,14] have examined sex and gender differences in depression. One review emphasized that the adverse consequences of ACEs on adult outcomes are influenced by biological sex, the developmental period during which stress occurs, and the life stage at which outcomes are assessed. The authors highlighted that sex differences in adult depression may be shaped by various mechanisms, including sex hormones, serotonergic pathways (5-HT), the hypothalamic–pituitary–adrenal (HPA) axis, and epigenetic modifications [15]. Findings from epidemiological research document sex-based disparities in the onset, prevalence, and clinical features of depression. While social and behavioral factors contribute to these disparities, several biological systems also appear to play a central role. These include sex-specific brain structures and neural circuitry, reproductive hormones, stress reactivity, immune responses, metabolism, and patterns of fat distribution. The authors argued that reproductive transitions unique to women—such as menstruation, pregnancy, postpartum, and menopause—represent windows of heightened psychological vulnerability. Additional biologically rooted risk factors, including sleep disturbances and exposure to early-life trauma, may also contribute to sex differences in depressive symptoms [16].
Several empirical studies further support these observations. One study using data from the National Longitudinal Study of Adolescent to Adult Health assessed the effects of 10 ACEs on C-reactive protein (CRP) and depressive symptoms in adulthood. Interaction terms and sex-stratified models were used to evaluate sex differences. Emotional abuse and parental incarceration were consistently associated with both CRP and depressive symptoms in both sexes, but other associations were sex-specific. For instance, childhood maltreatment was more strongly linked to depressive symptoms in females, while sexual abuse was more closely associated with inflammation in males. The authors highlighted the importance of considering how ACEs cluster differently by sex and how these differences inform both theory and intervention design [17,18,19,20,21]. In another study involving 826 adults (69.4% women), participants completed self-report measures of stress, psychological abuse, depression, and anxiety. Psychological violence was found to mediate the relationship between recent stress and both depression and anxiety. Importantly, sex moderated these associations, suggesting that interventions should be sensitive to gendered experiences of stress and violence to avoid reinforcing biases in clinical practice [22]. Finally, a psychometric network analysis of data from the Midlife Development in the United States study (N = 1917) examined associations among childhood trauma, major depression, and inflammation markers. Separate network models for men and women revealed both shared and sex-specific associations. Emotional abuse was strongly linked to somatic symptoms, and notable differences emerged in how inflammation and depressive symptom clusters were interconnected across sexes. These findings suggest that sex-disaggregated network models may identify distinct pathways and treatment targets for men and women [13].
Donovan and colleagues have proposed a conceptual framework suggesting that exposure to ACEs such as childhood abuse may influence the risk of depression and substance use differently in males and females [23,24]. Their literature review and theoretical framework highlights biological, psychological, and social factors which may contribute to these disparities. They hypothesize that hormonal differences during puberty and sociocultural influences including gender norms may disproportionately increase women’s rather than men’s vulnerability to the effects of exposure to ACEs on depression and substance use. ACEs may lead to greater hormonal dysregulation in females, potentially increasing the risk of internalizing symptoms and substance use during adolescence and beyond.
If there exists considerable sex and gender difference in the contribution of exposure to ACEs on depression, then interventions addressing ACEs and their consequences may need to be tailored to account for sex/gender-specific pathways [25,26]. Such tailored and sex/gender-specific interventions should consider both biological and sociocultural factors that differently influence the development of depression and substance use behaviors in males and females [27]. Among the moderating factors, sex and gender have emerged as key variables influencing the long-term impact of exposure to ACEs [23,24]. Biological, psychological, and sociocultural differences between men and women may shape their emotional responses, coping mechanisms, and access to support systems following exposure to early trauma. However, most existing studies on sex/gender differences in the mental health consequences of ACEs have been conducted in Western, high-income countries, limiting their generalizability. The Global Flourishing Study (GFS) [28,29,30,31,32,33] provides a unique opportunity to examine these associations in a large, diverse, and globally representative adult sample. This study leverages data from over 200,000 individuals across 23 countries, tracking various indicators of well-being over time, including exposure to childhood abuse (as predictor) and symptoms of depression (as outcome).
In this study, we test whether the association between exposure to childhood abuse and future changes in depressive symptoms during adulthood varies by sex/gender. In line with Donovan et al. [24], we hypothesize that the association between childhood abuse and future increases in depression is stronger among women than men [24]. We also control for demographic and socioeconomic variables that may confound or modify these associations. This study contributes to the literature by examining changes in depression over time, rather than cross-sectional associations, in a globally diverse cohort. The Global Flourishing Study’s multinational design, large sample size, and breadth of demographic representation offer unique insights into how the effects of early adversity on adult mental health may generalize across cultural contexts. Importantly, by linking childhood exposures to adult outcomes, the study underscores the long shadow that early trauma can cast well into midlife and beyond.
2. Methods
2.1. Design
This study used data from the Global Flourishing Study (GFS) [28,29,30,31,32,33], a large, longitudinal, multinational panel study that includes adult participants from 22 countries. The GFS was designed to examine factors related to well-being, mental health, and human flourishing across cultural and social contexts. Participants were surveyed at baseline and followed up approximately one year later, with information collected on demographics, socioeconomic indicators, past experiences of trauma, and mental health status, including depression.
Predictor: Our key exposure was self-reported history of childhood abuse, captured through retrospective items that asked whether participants had experienced emotional, physical, or sexual abuse in childhood. This was reported as a binary (yes/no) variable. The binary variable (yes/no) captures retrospective reports of emotional, physical, or sexual abuse but does not allow differentiation of type or severity, limiting dose–response analyses.
Outcome: The primary outcome was the change in depression over time, measured using a two-item validated depressive symptom scale administered at both baseline and follow-up [34]. Importantly, baseline depression scores were included as covariates in all models to assess relative change in depression rather than absolute levels, offering a longitudinal perspective on worsening mental health. The choice of a brief two-item scale was made to ensure feasibility in a multinational context and comparability across diverse cultures, though it may limit the full capture of the clinical spectrum of depression.
Confounders: Covariates included age, unemployment, marital status, immigration status, smoking status, and educational attainment. Education was categorized into three levels: low (e.g., no formal education or primary education only), mid (e.g., secondary education or some postsecondary), and high (e.g., college degree or above), with low as the reference category. We also controlled for country as fixed effects to account for demographic and contextual variation. All variables were standardized as needed to ensure comparability across countries.
Effect modifier: Sex/gender was the moderator of interest (1 for male and 0 for female).
2.2. Analysis
We employed structural equation modeling (SEM) [35,36,37,38] to estimate the effect of childhood abuse on depressive symptom change over time and to test whether this association varied by sex/gender. Multi-group SEM was used where groups were defined based on sex/gender. We did not fix any paths in our multi-group model [39]. SEM allowed for simultaneous modeling of measurement error and latent constructs while controlling for baseline depression and covariates [40]. A Root Mean Square Error of Approximation (RMSEA) value below 0.04 and a Comparative Fit Index (CFI) value above 0.95 were considered indicators of good model fit. Given the very large sample size, a significant chi-square test was not regarded as poor fit.
3. Results
Data from 124,982 participants across 22 countries were analyzed. On average, the time interval between the two measurement waves was 418 days (SE = 0.28). Table 1 presents the distribution of participants by country. The sample was not evenly distributed, with the largest proportion of participants from the United States (n = 31,970; 25.58%, 95% CI: 25.34–25.82), followed by Japan (n = 13,841; 11.07%, 95% CI: 10.90–11.25) and Sweden (n = 11,539; 9.23%, 95% CI: 9.07–9.39). Kenya (6.13%), Poland (5.14%), India (4.82%), and Tanzania (4.44%) also contributed substantially to the total sample.

Table 1.
Number and percentage of participants across countries.
Several other countries accounted for 2% to 4% of the sample, including China (3.63%), Brazil (3.36%), Germany (4.38%), and Egypt (2.42%). Countries with lower representation included Mexico (1.78%), South Africa (0.77%), Türkiye (0.40%), and Hong Kong (0.56%).
Overall, the dataset reflects considerable global diversity, with participants from Asia, Africa, Europe, North and South America, and Oceania. However, the unequal distribution of participants across countries should be considered when interpreting pooled results or making country-specific inferences.
Table 2 presents descriptive statistics for key study variables. The average age of participants was 49.04 years (SE = 0.05, 95% CI: 48.94–49.13). The mean score for depressed mood at baseline was 1.73 (SE < 0.01), increasing slightly to 1.75 at follow-up (95% CIs: 1.73–1.74 and 1.74–1.75, respectively). Similarly, the average anhedonia score increased from 1.84 at baseline to 1.86 at follow-up (SEs < 0.01; 95% CIs: 1.84–1.85 and 1.86–1.87, respectively). These small but consistent increases suggest a modest rise in depressive symptoms over the follow-up period.

Table 2.
Descriptive data.
Gender distribution was relatively balanced, with 51.09% identifying as female (SE = 0.14, 95% CI: 50.82–51.37) and 48.91% as male (SE = 0.14, 95% CI: 48.63–49.18).
Educational attainment varied, with 14.40% of the sample reporting low education levels (95% CI: 14.20–14.59), 54.93% reporting medium education (95% CI: 54.65–55.21), and 30.67% reporting high education (95% CI: 30.42–30.93).
More than half of the participants (57.83%) were married at baseline (SE = 0.14, 95% CI: 57.56–58.11), while 42.17% were not (SE = 0.14, 95% CI: 41.89–42.44).
Unemployment was relatively uncommon in the sample, with only 7.02% of participants unemployed at baseline (SE = 0.07, 95% CI: 6.88–7.17), compared to 92.98% who were not unemployed (95% CI: 92.83–93.12).
Regarding adverse childhood experiences (ACE), 14.11% of participants reported having experienced abuse (SE = 0.10, 95% CI: 13.92–14.31), while 85.89% did not (SE = 0.10, 95% CI: 85.69–86.08).
4. Structural Equation Modeling (SEM) in Females
Table 3 presents the SEM findings among females. ACE was significantly associated with a larger increase in depression (B = 0.009, p = 0.044). Immigration status did not show a statistically significant association (B = 0.006, p = 0.098). As expected, baseline depression was a strong predictor of follow-up depression (B = 0.677, p < 0.001) (Figure 1).

Table 3.
Summary of SEM in females.
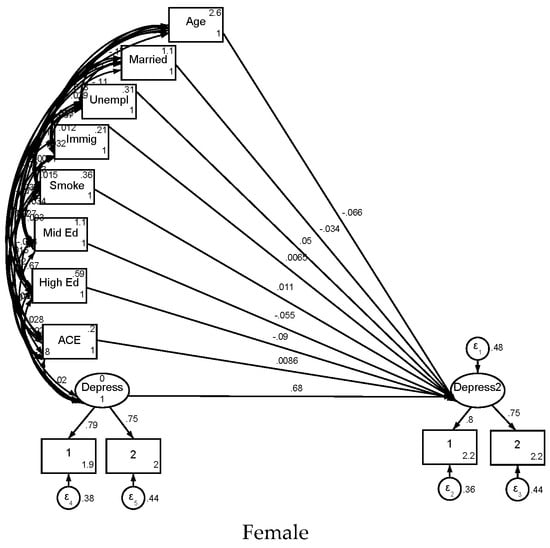
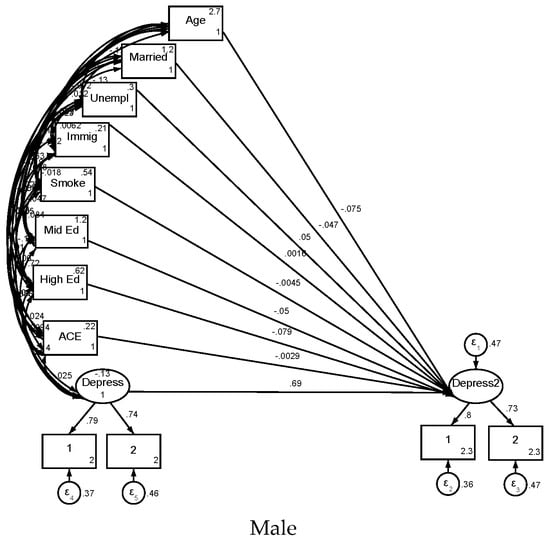
Figure 1.
Summary of SEM in female and male participants.
Higher educational attainment at baseline was significantly associated with fewer depressive symptoms at follow-up. Compared to women with low education, those with mid-level education had lower follow-up depression (B = −0.055, 95% CI: −0.066 to −0.045, p < 0.001), and the association was even stronger for those with high education (B = −0.090, 95% CI: −0.100 to −0.079, p < 0.001).
Other significant predictors of lower depression scores included older age (B = −0.066, p < 0.001) and being married at baseline (B = −0.034, p < 0.001). In contrast, unemployment (B = 0.050, p < 0.001) and smoking (B = 0.011, p = 0.011) were associated with higher depressive symptoms.
The measurement model showed high factor loadings for both depressed mood and anhedonia on the latent depression construct at baseline and follow-up. Depression strongly predicted both depressed mood (B = 0.800) and anhedonia (B = 0.749) at follow-up and baseline (B = 0.788 for depressed mood; B = 0.750 for anhedonia), all p < 0.001.
5. Structural Equation Modeling (SEM) in Males
As shown in Table 4, results among males were similar in many respects. However, ACE was not significantly associated with an increase in depression in males (B = −0.003, p = 0.524). Baseline depression remained the strongest predictor of follow-up depression (B = 0.688, p < 0.001).

Table 4.
Summary of SEM in males.
Baseline educational attainment remained protective: mid-level education was associated with lower depression at follow-up (B = −0.050, 95% CI: −0.061 to −0.039, p < 0.001), and the effect was stronger for high education (B = −0.079, 95% CI: −0.090 to −0.068, p < 0.001).
Older age (B = −0.075, p < 0.001) and being married (B = −0.047, p < 0.001) were also associated with fewer depressive symptoms. Unemployment was linked to more depressive symptoms (B = 0.050, p < 0.001), while immigration status and smoking were not statistically significant (B = 0.002, p = 0.685 and B = −0.005, p = 0.279, respectively).
The measurement model also showed robust factor loadings: follow-up depression was strongly associated with both depressed mood (B = 0.801) and anhedonia (B = 0.730), and baseline depression similarly predicted its respective indicators (B = 0.794 for depressed mood; B = 0.735 for anhedonia), all p < 0.001.
6. Discussion
This longitudinal analysis of a large and diverse global sample highlights a key finding: childhood abuse is associated with increased depressive symptoms in adulthood among women, but not among men. For women, childhood abuse was associated with a 0.009-unit increase in depression scores (p = 0.044), whereas the effect was non-significant in men (B = −0.003, p = 0.524), indicating that women experienced, on average, a 1.2% greater increase in depressive symptoms compared to men. This observed sex/gender difference suggests a potentially unequal psychological burden of early-life adversity across sexes. While the overall link between childhood abuse and depression is well established, fewer studies have examined whether such adversity predicts changes in depression over time during adulthood, particularly in a global context.
The association between childhood abuse and greater depressive symptoms has been well documented in prior research [41,42,43]. Traumatic experiences early in life are thought to disrupt emotional development, heighten vulnerability to stress, and undermine long-term psychological well-being [44,45,46]. Within the framework of developmental psychopathology, adverse childhood environments are believed to interfere with the maturation of coping mechanisms and alter neurobiological systems involved in emotion regulation, such as stress-response pathways and mood-related brain circuits [47,48,49].
Our results are in line with many reviews [3,12] and empirical studies [13,14] on sex and gender differences in depression. Reviews highlight that the effects of ACEs on adult depression are modified by sex and associated biological mechanisms such as hormones, neurotransmission, the HPA axis, and epigenetics [22]. Such differences span prevalence, symptoms, treatment response, and neurobiology, including transcriptional patterns, immune signatures, and brain structure [12,14]. For instance, fluctuations in estrogen may amplify activation of the hypothalamic–pituitary–adrenal (HPA) axis in women, leading to heightened stress sensitivity following exposure to ACEs [50,51]. Additionally, societal norms that encourage women to internalize stress, in contrast to men who often adopt externalizing behaviors, may exacerbate vulnerability to depression [52].
However, unlike much of the existing literature that focuses on cross-sectional associations between ACEs and depression, our study specifically examined whether childhood abuse predicts future changes in depressive symptoms during adulthood. This focus on within-person change over time distinguishes our work from prior studies and adds new insight into the long-term emotional consequences of early adversity.
The sex/gender-specific pattern observed in our findings adds nuance to this literature [24,53]. Several plausible mechanisms may explain why women appear more vulnerable to the long-term mental health consequences of childhood abuse [54,55,56]. Biologically, sex hormones such as estrogen and progesterone influence the activity of the hypothalamic–pituitary–adrenal (HPA) axis, a central stress-regulation system [57,58]. These hormonal differences may amplify emotional reactivity and the internalization of distress among females following early trauma [59]. Neurodevelopmental studies have also shown sex-specific responses in brain regions critical to emotional regulation, such as the amygdala and prefrontal cortex, suggesting that early adversity may be encoded differently in male and female brains [60,61,62].
Sociocultural factors may further shape these divergent trajectories. Women are often socialized to express emotions inwardly and may be more likely to internalize stress and adversity, increasing the risk for depressive symptoms [63,64]. In contrast, men may be encouraged to suppress emotional expression or cope through externalizing behaviors, potentially masking the psychological impact of early trauma in typical depression scales [65,66,67]. Moreover, societal expectations and caregiving roles may increase chronic stress exposure for women, compounding the effects of childhood adversity [68,69]. Differences in coping styles may also play a role, as women are more likely to engage in rumination, a known risk factor for depression, while men may adopt distraction or avoidance strategies [70,71].
Together, these findings underscore the importance of considering sex and gender as central factors in understanding the long-term effects of childhood adversity. They also suggest that mental health interventions targeting the consequences of early trauma may need to be gender-sensitive to effectively address the distinct vulnerabilities and needs of women and men. This study adds to growing evidence that childhood adversity has long-term effects on mental health but highlights that these effects may not be experienced equally by men and women. By demonstrating a stronger association between childhood abuse and later depression among women, our findings point to the importance of sex/gender-sensitive approaches in both research and practice. Understanding and addressing these differences is crucial for reducing the lifelong burden of childhood trauma.
7. Policy and Practice Implications
Our findings have important implications for mental health policy and prevention. While childhood abuse should be prevented universally, our results suggest that particular attention is needed for girls, who may face more enduring psychological consequences. Mental health screening and trauma-informed interventions should be made available to adults with a history of childhood adversity—especially women—even many years after the original exposure. Sex/gender-responsive programming that acknowledges these disparities may improve outcomes and reduce the mental health burden associated with ACEs.
8. Strengths and Limitations
This study offers several notable strengths. The longitudinal design of the study allows for an examination of changes in depressive symptoms over time, rather than relying solely on cross-sectional associations. The international scope—with participants drawn from a diverse range of cultural, geographic, and socioeconomic backgrounds—adds important global context to the findings and increases their generalizability. The large sample size further strengthens the statistical power and precision of the estimates, enabling the detection of even modest effects and interactions, such as those observed by sex/gender.
Despite these strengths, several limitations warrant consideration. The uneven distribution of participants, with 25.58% from the USA, may affect the generalizability of findings, as cultural norms and healthcare systems in high-income countries may differ from those in low- or middle-income countries. Additionally, the lack of data on race, ethnicity, gender expression, or sexual orientation limits our ability to explore intersecting identities that may modify the impact of ACEs. Childhood abuse was assessed retrospectively using a single-item measure, which may be prone to recall bias or cultural interpretations of abuse, and provides limited information regarding the type, severity, frequency, and timing of abuse. This restricts our ability to explore dose–response relationships or to differentiate between forms of abuse (e.g., physical vs. emotional). The measure of depressive symptoms was also brief, based on only two self-reported items, which may not capture the full clinical range of depressive experiences and may be influenced by cross-cultural variation in emotional expression, mental health stigma, or help-seeking norms. Additionally, the follow-up period was relatively short—approximately one year—which may limit the ability to observe longer-term mental health trajectories following childhood adversity.
Our models were adjusted for core demographic and socioeconomic variables, but several important sources of heterogeneity were not included. Data on race, ethnicity, rural versus urban residence, gender expression, and sexual orientation were not available or were inconsistently collected across countries. These unmeasured factors may interact with both exposure and outcome, contributing to residual confounding or effect modification. Furthermore, the study focused only on childhood abuse and did not assess other types of adverse childhood experiences (ACEs) such as emotional neglect, household dysfunction, parental incarceration, or community violence, which are also known to impact adult mental health. The exclusion of these variables may underestimate the broader impact of early adversity and obscure potential cumulative or synergistic effects.
9. Future Research Directions
Future research should build on these findings by incorporating more detailed assessments of childhood adversity, including different forms of abuse, neglect, and household dysfunction, to better understand the cumulative and specific effects of adverse experiences. Prospective longitudinal studies, where possible, would help reduce the limitations of retrospective recall and provide a clearer temporal sequence between adversity and later outcomes. In addition, more work is needed to uncover the mechanisms behind the observed sex/gender differences, including investigations of biological stress systems, neuroendocrine functioning, and sexualized/gendered patterns of emotion regulation and socialization. Research should also explore how intersecting identities—such as race, ethnicity, class, gender expression, and sexual orientation—may compound or buffer the effects of ACEs on mental health. Future research may incorporate a more gender-inclusive perspective, recognizing the limitations of binary categorization. In addition, future sensitivity analyses ought to assess the robustness of the results against possible memory biases or underreporting in men. Future studies expanding participation in countries beyond the oversampled Western cultures would help to increase the generalizability of findings. Finally, future studies could evaluate the effectiveness of trauma-informed and sex/gender-responsive interventions across different cultural and health system contexts to identify strategies that are most effective in globally reducing the long-term mental health consequences of childhood abuse.
10. Conclusions
This study underscores the need for gender-sensitive mental health interventions addressing the greater vulnerability of women to the long-term consequences of childhood abuse. Policymakers should prioritize prevention and screening programs targeting adults with a history of ACEs, particularly women, while future research should focus on non-Western countries to explore cultural differences in the impact of ACEs and evaluate the effectiveness of tailored interventions.
Author Contributions
Conceptualization: S.A., A.D., and B.N.; Analysis: S.A., Resources: A.D., First Draft: S.A., Revision: B.N., S.A., and A.D.; Approval of the Final Version: B.N., S.A., and A.D. All authors have read and agreed to the published version of the manuscript.
Funding
Alexandra Donovan is funded by the National Institutes of Health, National Institute on Drug Abuse Substance Abuse Research Training (SART) program (1R25DA050723), and National Institute on Minority Health and Health Disparities grant to the Urban Health Institute (S21 MD000103), both at Charles R. Drew University. Shervin Assari’s research is partially supported by the Regents of the University of California, Tobacco-Related Diseases Research Program, Grant Number No. T32IR5355. The opinions, findings, and conclusions herein are those of the authors and do not necessarily represent The Regents of the University of California, or any of its programs. Assari is also supported by the Clinical Research Education and Career Development (CRECD) program at Charles R. Drew University of Medicine and Science through the NIMHD/NIH Award number R25 MD007610 (PIs = Mohsen Bazargan and Roberto Vargas). In this role, he provides methodological and statistical guidance and support for CRECD scholars. The Global Flourishing Study was supported by funding from the John Templeton Foundation (grant no. 61665), Templeton Religion Trust (no. 1308), Templeton World Charity Foundation (no. 0605), Well-Being for Planet Earth Foundation, Fetzer Institute (no. 4354), Well Being Trust, Paul L. Foster Family Foundation and the David and Carol Myers Foundation.
Institutional Review Board Statement
The present study utilized data from the Global Flourishing Study (GFS), which is publicly available and fully deidentified. The parent study received Institutional Review Board (IRB) approval from Harvard University, and all data were collected anonymously. Ethical review and approval were waived for this study due to the de-identified and publicly accessible nature of the dataset; this secondary analysis was classified as not involving human subjects research.
Informed Consent Statement
For this analysis, consent was waived due to the fact that this is a secondary analysis of deidentified publicly available data.
Data Availability Statement
Data of the Global Flourishing Study ARE available through the Center for Open Science upon submission of a pre-registration (https://doi.org/10.17605/OSF.IO/3JTZ8) and will be openly available without pre-registration beginning 2026. Please see https://www.cos.io/gfs-access-data (accessed on 9 June 2025) for more information about data access.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Parker, G.; Brotchie, H. Gender differences in depression. Int. Rev. Psychiatry 2010, 22, 429–436. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- Pavlidi, P.; Kokras, N.; Dalla, C. Sex Differences in Depression and Anxiety. Curr. Top. Behav. Neurosci. 2023, 62, 103–132. [Google Scholar] [CrossRef]
- Felitti, V.J. The Relation Between Adverse Childhood Experiences and Adult Health: Turning Gold into Lead. Perm. J. 2002, 6, 44–47. [Google Scholar] [CrossRef]
- Chapman, D.P.; Whitfield, C.L.; Felitti, V.J.; Dube, S.R.; Edwards, V.J.; Anda, R.F. Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect. Disord. 2004, 82, 217–225. [Google Scholar] [CrossRef]
- Sheffler, J.L.; Piazza, J.R.; Quinn, J.M.; Sachs-Ericsson, N.J.; Stanley, I.H. Adverse childhood experiences and coping strategies: Identifying pathways to resiliency in adulthood. Anxiety Stress Coping 2019, 32, 594–609. [Google Scholar] [CrossRef]
- Iob, E.; Lacey, R.; Giunchiglia, V.; Steptoe, A. Adverse childhood experiences and severity levels of inflammation and depression from childhood to young adulthood: A longitudinal cohort study. Mol. Psychiatry 2022, 27, 2255–2263. [Google Scholar] [CrossRef]
- McEwen, B.S.; Milner, T.A. Hippocampal formation: Shedding light on the influence of sex and stress on the brain. Brain Res. Rev. 2007, 55, 343–355. [Google Scholar] [CrossRef] [PubMed]
- Sapienza, P.; Zingales, L.; Maestripieri, D. Gender differences in financial risk aversion and career choices are affected by testosterone. Proc. Natl. Acad. Sci. USA 2009, 106, 15268–15273. [Google Scholar] [CrossRef]
- Verma, R.; Balhara, Y.P.; Gupta, C.S. Gender differences in stress response: Role of developmental and biological determinants. Ind. Psychiatry J. 2011, 20, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Gan, A.K.X.; Gibb, B.E. Stress sensitivity in women with a history of recurrent versus first-episode major depression. Psychiatry Res. 2025, 345, 116382. [Google Scholar] [CrossRef] [PubMed]
- Eid, R.S.; Gobinath, A.R.; Galea, L.A.M. Sex differences in depression: Insights from clinical and preclinical studies. Prog. Neurobiol. 2019, 176, 86–102. [Google Scholar] [CrossRef] [PubMed]
- O’Shields, J.D.; Graves, B.D.; Mowbray, O.P. Sex differences in childhood maltreatment, inflammation, and adulthood depression: A network analysis. Brain Behav. Immun. Health 2023, 29, 100611. [Google Scholar] [CrossRef]
- Gronewold, J.; Duman, E.E.; Engel, M.; Engels, M.; Siegrist, J.; Erbel, R.; Jöckel, K.H.; Hermann, D.M. Association between life events and later depression in the population-based Heinz Nixdorf Recall study-The role of sex and optimism. PLoS ONE 2022, 17, e0271716. [Google Scholar] [CrossRef] [PubMed]
- An, X.; Guo, W.; Wu, H.; Fu, X.; Li, M.; Zhang, Y.; Li, Y.; Cui, R.; Yang, W.; Zhang, Z.; et al. Sex Differences in Depression Caused by Early Life Stress and Related Mechanisms. Front. Neurosci. 2022, 16, 797755. [Google Scholar] [CrossRef]
- Jarkas, D.A.; Villeneuve, A.H.; Daneshmend, A.Z.B.; Villeneuve, P.J.; McQuaid, R.J. Sex differences in the inflammation-depression link: A systematic review and meta-analysis. Brain Behav. Immun. 2024, 121, 257–268. [Google Scholar] [CrossRef]
- Wang, R.; Kogler, L.; Derntl, B. Sex differences in cortisol levels in depression: A systematic review and meta-analysis. Front. Neuroendocr. 2024, 72, 101118. [Google Scholar] [CrossRef]
- O’Shields, J.D.; Slavich, G.M.; Mowbray, O. Adverse childhood experiences, inflammation, and depression: Evidence of sex- and stressor specific effects in a nationally representative longitudinal sample of U.S. adolescents. Psychol. Med. 2025, 55, e140. [Google Scholar] [CrossRef]
- Donovan, A.; Assari, S.; Shaheen, M.; Grella, C.; Richter, L.; Friedman, T.C. 8256 Early Life Stress and Pubertal Predictors of Youth Substance Use Initiation: Does Sex Moderate the Relationship Between ELS, Puberty, and Substance Use Initiation? J. Endocr. Soc. 2024, 8, bvae163.1194. [Google Scholar] [CrossRef]
- Assari, S.; Sheikhattari, P. Sex Differences in the Relationship Between Nucleus Accumbens Volume and Youth Tobacco or Marijuana Use Following Stressful Life Events. J. Ment. Health Clin. Psychol. 2024, 8, 1–13. [Google Scholar] [CrossRef]
- Campioni, M.R.; Xu, M.; McGehee, D.S. Stress-induced changes in nucleus accumbens glutamate synaptic plasticity. J. Neurophysiol. 2009, 101, 3192–3198. [Google Scholar] [CrossRef]
- Magalhães, E.; Ferreira, C.; Antunes, C.; Jongenelen, I.; Castro, E. Stressful Events During Last Year, Violence and Anxiety and Depression: A Moderated Mediation Model by Sex. Violence Vict. 2022, 37, 610–624. [Google Scholar] [CrossRef] [PubMed]
- Donovan, A.; Assari, S.; Grella, C.; Shaheen, M.; Richter, L.; Friedman, T.C. Early life stress and pubertal predictors of subsequent substance use in a national diverse sample of adolescents: Sex and substance type matter. Drug Alcohol. Depend. 2025, 268, 112551. [Google Scholar] [CrossRef] [PubMed]
- Donovan, A.; Assari, S.; Grella, C.; Shaheen, M.; Richter, L.; Friedman, T.C. Neuroendocrine mechanisms in the links between early life stress, affect, and youth substance use: A conceptual model for the study of sex and gender differences. Front. Neuroendocrinol. 2024, 73, 101121. [Google Scholar] [CrossRef]
- Manoli, D.S.; Tollkuhn, J. Gene regulatory mechanisms underlying sex differences in brain development and psychiatric disease. Ann. N. Y. Acad. Sci. 2018, 1420, 26–45. [Google Scholar] [CrossRef] [PubMed]
- López-Cerdán, A.; Andreu, Z.; Hidalgo, M.R.; Soler-Sáez, I.; de la Iglesia-Vayá, M.; Mikozami, A.; Guerini, F.R.; García-García, F. An integrated approach to identifying sex-specific genes, transcription factors, and pathways relevant to Alzheimer’s disease. Neurobiol. Dis. 2024, 199, 106605. [Google Scholar] [CrossRef]
- Baker, T.; Mundell, N.; Koorts, H.; Pebole, M.; Rosenbaum, S.; Ganakas, E.; Teychenne, M. Targeting mental health and wellbeing in women who have experienced gender-based violence through moderate-vigorous physical activity: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2025, 22, 49. [Google Scholar] [CrossRef]
- Levin, J.; Bradshaw, M.; Johnson, B.R. Association between Jewish religious observance and mental health among Israeli adults: Findings from the Global Flourishing Study. Int. J. Psychiatry Med. 2025, 60, 338–355. [Google Scholar] [CrossRef] [PubMed]
- Lomas, T.; Bradshaw, M.; Case, B.; Cowden, R.G.; Crabtree, S.; English, C.; Fogleman, A.; Johnson, K.A.; Ritter, Z.; Johnson, B.R. The development of the Global Flourishing Study questionnaire: Charting the evolution of a new 109-Item inventory of human flourishing. BMC Glob. Public. Health 2025, 3, 30. [Google Scholar] [CrossRef]
- Johnson, B.R.; VanderWeele, T.J. The global flourishing study: A new era for the study of well-being. Int. Bull. Mission Res. 2022, 46, 272–275. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Johnson, B.R.; Bialowolski, P.T.; Bonhag, R.; Bradshaw, M.; Breedlove, T.; Case, B.; Chen, Y.; Chen, Z.J.; Counted, V. The Global Flourishing Study: Study profile and initial results on flourishing. Nat. Ment. Health 2025, 1–18. [Google Scholar] [CrossRef]
- Levin, J.; Bradshaw, M.; Johnson, B.R. Religious Differences in Physical and Mental Health among Israeli Jews: Findings from the Global Flourishing Study. J. Relig. Health 2024, 63, 2544–2558. [Google Scholar] [CrossRef] [PubMed]
- Padgett, R.N.; Cowden, R.G.; Chattopadhyay, M.; Han, Y.; Honohan, J.; Ritter, Z.; Srinivasan, R.; Johnson, B.R.; VanderWeele, T.J. Survey sampling design in wave 1 of the Global Flourishing Study. Eur. J. Epidemiol. 2025, 40, 391–406. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Ullman, J.B.; Bentler, P.M. Structural equation modeling. In Handbook of Psychology, 2nd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012; Volume 2. [Google Scholar]
- Hair Jr, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S.; Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. An introduction to structural equation modeling. In Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1–29. [Google Scholar]
- Mueller, R.O.; Hancock, G.R. Structural equation modeling. In The reviewer’s Guide to Quantitative Methods in the Social Sciences; Routledge: Oxford, UK, 2018; pp. 445–456. [Google Scholar]
- Bowen, N.K.; Guo, S. Structural Equation Modeling; Oxford University Press: Oxford, UK, 2011. [Google Scholar]
- Velayutham, S.; Aldridge, J.M.; Fraser, B. Gender differences in student motivation and self-regulation in science learning: A multi-group structural equation modeling analysis. Int. J. Sci. Math. Educ. 2012, 10, 1347–1368. [Google Scholar] [CrossRef]
- Tu, Y.K.; Baelum, V.; Gilthorpe, M.S. A structural equation modelling approach to the analysis of change. Eur. J. Oral. Sci. 2008, 116, 291–296. [Google Scholar] [CrossRef]
- Lee, M.-A.; Song, R. Childhood abuse, personality traits, and depressive symptoms in adulthood. Child Abus. Negl. 2017, 65, 194–203. [Google Scholar] [CrossRef]
- Shapero, B.G.; Black, S.K.; Liu, R.T.; Klugman, J.; Bender, R.E.; Abramson, L.Y.; Alloy, L.B. Stressful life events and depression symptoms: The effect of childhood emotional abuse on stress reactivity. J. Clin. Psychol. 2014, 70, 209–223. [Google Scholar] [CrossRef]
- Van Dam, D.; van Nierop, M.; Viechtbauer, W.; Velthorst, E.; van Winkel, R.; Bruggeman, R.; Cahn, W.; De Haan, L.; Kahn, R.; Meijer, C. Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychol. Med. 2015, 45, 1363–1377. [Google Scholar] [CrossRef]
- He, C.; Fan, D.; Liu, X.; Wang, Q.; Zhang, H.; Zhang, H.; Zhang, Z.; Xie, C. Insula network connectivity mediates the association between childhood maltreatment and depressive symptoms in major depressive disorder patients. Transl. Psychiatry 2022, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Linn, K.A.; Shinohara, R.T.; Oathes, D.J.; Cook, P.A.; Duprat, R.; Moore, T.M.; Oquendo, M.A.; Phillips, M.L.; McInnis, M. Childhood trauma history is linked to abnormal brain connectivity in major depression. Proc. Natl. Acad. Sci. USA 2019, 116, 8582–8590. [Google Scholar] [CrossRef]
- Wang, Q.; Qi, L.; He, C.; Fan, D.; Zhang, H.; Zhang, H.; Cheng, W.; Xie, C. Occipital connectivity networks mediate the neural effects of childhood maltreatment on depressive symptoms in major depressive disorder. Asian J. Psychiatry 2024, 97, 104093. [Google Scholar] [CrossRef]
- Lin, J.; Huang, J.; Wu, Y.; Zhou, L.; Qiao, C.; Xie, J.; Hu, C. Exploring the neural link between childhood maltreatment and depression: A default mode network rs-fMRI study. Front. Psychiatry 2024, 15, 1450051. [Google Scholar] [CrossRef] [PubMed]
- Weder, N.; Zhang, H.; Jensen, K.; Yang, B.Z.; Simen, A.; Jackowski, A.; Lipschitz, D.; Douglas-Palumberi, H.; Ge, M.; Perepletchikova, F. Child abuse, depression, and methylation in genes involved with stress, neural plasticity, and brain circuitry. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 417–424.e415. [Google Scholar] [CrossRef]
- Wu, Z.; Luo, Q.; Wu, H.; Wu, Z.; Zheng, Y.; Yang, Y.; He, J.; Ding, Y.; Yu, R.; Peng, H. Amplitude of low-frequency oscillations in major depressive disorder with childhood trauma. Front. Psychiatry 2021, 11, 596337. [Google Scholar] [CrossRef] [PubMed]
- Heck, A.L.; Handa, R.J. Sex differences in the hypothalamic–pituitary–adrenal axis’ response to stress: An important role for gonadal hormones. Neuropsychopharmacology 2019, 44, 45–58. [Google Scholar] [CrossRef]
- Oyola, M.G.; Handa, R.J. Hypothalamic–pituitary–adrenal and hypothalamic–pituitary–gonadal axes: Sex differences in regulation of stress responsivity. Stress 2017, 20, 476–494. [Google Scholar] [CrossRef]
- Obeidallah, D.A.; McHale, S.M.; Silbereisen, R.K. Gender role socialization and adolescents’ reports of depression: Why some girls and not others? J. Youth Adolesc. 1996, 25, 775–785. [Google Scholar] [CrossRef]
- Dedovic, K.; Wadiwalla, M.; Engert, V.; Pruessner, J.C. The role of sex and gender socialization in stress reactivity. Dev. Psychol. 2009, 45, 45. [Google Scholar] [CrossRef]
- Christiansen, D.M.; McCarthy, M.M.; Seeman, M.V. Where sex meets gender: How sex and gender come together to cause sex differences in mental illness. Front. Psychiatry 2022, 13, 856436. [Google Scholar] [CrossRef] [PubMed]
- Rincón-Cortés, M.; Herman, J.P.; Lupien, S.; Maguire, J.; Shansky, R.M. Stress: Influence of sex, reproductive status and gender. Neurobiol. Stress. 2019, 10, 100155. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Mendenhall, S.; Myers, C.A. The effects of sex and gender role identity on perceived stress and coping among traditional and nontraditional students. J. Am. Coll. Health 2016, 64, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Young, E.; Korszun, A. Sex, trauma, stress hormones and depression. Mol. Psychiatry 2010, 15, 23–28. [Google Scholar] [CrossRef]
- Mengelkoch, S.; Slavich, G.M. Sex differences in stress susceptibility as a key mechanism underlying depression risk. Curr. Psychiatry Rep. 2024, 26, 157–165. [Google Scholar] [CrossRef]
- Guo, L.; Chen, Y.-X.; Hu, Y.-T.; Wu, X.-Y.; He, Y.; Wu, J.-L.; Huang, M.-L.; Mason, M.; Bao, A.-M. Sex hormones affect acute and chronic stress responses in sexually dimorphic patterns: Consequences for depression models. Psychoneuroendocrinology 2018, 95, 34–42. [Google Scholar] [CrossRef]
- Marrocco, J.; McEwen, B.S. Sex in the brain: Hormones and sex differences. Dialogues Clin. Neurosci. 2016, 18, 373–383. [Google Scholar] [CrossRef]
- McEwen, B.S.; Milner, T.A. Understanding the broad influence of sex hormones and sex differences in the brain. J. Neurosci. Res. 2017, 95, 24–39. [Google Scholar] [CrossRef]
- Sinclair, D.; Purves-Tyson, T.D.; Allen, K.M.; Weickert, C.S. Impacts of stress and sex hormones on dopamine neurotransmission in the adolescent brain. Psychopharmacology 2014, 231, 1581–1599. [Google Scholar] [CrossRef]
- Liddon, L.; Kingerlee, R.; Barry, J.A. Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. Br. J. Clin. Psychol. 2018, 57, 42–58. [Google Scholar] [CrossRef]
- Gibbons, S.W.; Barnett, S.D.; Hickling, E.J.; Herbig-Wall, P.L.; Watts, D.D. Stress, coping, and mental health-seeking behaviors: Gender differences in OEF/OIF health care providers. J. Trauma. Stress 2012, 25, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Bennett, K.M. “No sissy stuff”: Towards a theory of masculinity and emotional expression in older widowed men. J. Aging Stud. 2007, 21, 347–356. [Google Scholar] [CrossRef]
- Jakupcak, M.; Tull, M.T.; Roemer, L. Masculinity, Shame, and Fear of Emotions as Predictors of Men’s Expressions of Anger and Hostility. Psychol. Men Masculinity 2005, 6, 275. [Google Scholar] [CrossRef]
- De Boise, S.; Hearn, J. Are men getting more emotional? Critical sociological perspectives on men, masculinities and emotions. Sociol. Rev. 2017, 65, 779–796. [Google Scholar] [CrossRef]
- Lee, C. Social context, depression and the transition to motherhood. Br. J. Health Psychol. 1997, 2, 93–108. [Google Scholar] [CrossRef]
- Schwartz, S. Women and depression: A Durkheimian perspective. Soc. Sci. Med. 1991, 32, 127–140. [Google Scholar] [CrossRef]
- Shors, T.J.; Millon, E.M.; Chang, H.Y.M.; Olson, R.L.; Alderman, B.L. Do sex differences in rumination explain sex differences in depression? J. Neurosci. Res. 2017, 95, 711–718. [Google Scholar] [CrossRef]
- Papadakis, A.A.; Prince, R.P.; Jones, N.P.; Strauman, T.J. Self-regulation, rumination, and vulnerability to depression in adolescent girls. Dev. Psychopathol. 2006, 18, 815–829. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).