Abstract
Childhood-onset systemic lupus erythematosus (cSLE) impacts the daily life of children and young people. This study aimed to describe the experiences and perspectives of children and young people living with cSLE. An integrative review guided by Whittemore and Knafl was conducted. Extant empirical research published in peer-reviewed journals from 2000 to 2021 on children’s self-reported experiences living with cSLE was identified from Scopus, CINAHL, Medline via PubMed, and PsycINFO via Ovid databases. Nineteen studies involving over 1400 participants were included. Four themes and fourteen sub-themes were identified: (1) challenging symptoms (disruptions to life and altered self, severity, fatigue, depression, and anxiety), (2) medicines and side effects (dreaded steroids, conflicting feelings, and medication adherence), (3) complicated life (school sports and social, giving things up, lack of understanding, and quality of life) and (4) ways of coping (family and friends, relationships with health providers, and maintaining positivity). While cSLE shares many similarities with adult-onset SLE, awareness of differences in experiences and perceptions of children and young people is crucial. The significant psychological and social impact of the disease and its treatments necessitates a comprehensive, holistic approach to managing cSLE that considers the unique needs of youth.
1. Introduction
Childhood-onset systemic lupus erythematosus (cSLE) is a rare multi-system autoimmune disease that is defined by disease onset before the age of 18 years [1]. It affects approximately 15–20% of SLE patients and has a variable presentation and clinical course [2,3]. Incidences of cSLE are reported as between 0.36 and 2.5 per 100,000 children, with prevalence ranging from 1.89 to 34.1 per 100,000 [4,5,6,7]. Similar to adult onset (aSLE), cSLE is clinically complex, heterogeneous, and characterized by periods of flare and remission [8]; however, cSLE is much more aggressive than aSLE with higher disease activity, more severe organ manifestations, and subsequently increased medication burden [9,10,11]. Childhood-onset systemic lupus erythematosus most commonly affects the skin (including malar and discoid rash), muscles, and joints; however, involvement of major organs is common, with renal inflammation occurring most frequently [2,12]. Other non-specific symptoms of fatigue, pain, weight loss, and fever are frequent and result in significant morbidity [10].
Research in aSLE has examined experiences and outcomes through the analysis of barriers and facilitators, exploration of beliefs, illness perception, and treatment adherence [13,14,15,16]. In addition, studies describe how disease activity, anxiety, social support, sleep quality, and fatigue negatively impact quality of life (QOL) in aSLE [17,18]. In cSLE, much of the focus has been on treatment targets [8], adherence [19,20], health literacy and/or knowledge deficits [21], and the challenges of disease management [22]. Previous studies in other pediatric rheumatological conditions have demonstrated significant disruptions to the trajectory of young people’s lives, impacts on relationships, effects on self-esteem, and the creation of more challenges for children and young people (CYP) in day-to-day life [23,24]. In addition, mental health problems, particularly anxiety and depression, are more common in CYP with pediatric rheumatologic diseases compared to healthy peers [25].
Children and young people with cSLE develop the disease at a young age, have a longer disease course, and therefore have more time to develop long-term complications and multi-system co-morbidities [9,26]. In addition, the physical and psychosocial changes that occur with maturity, the increased likelihood of requiring more intensive drug therapy, and the necessity to have parents and caregivers involved in management contribute to the complexity and equate to a clinical course that is unpredictable and challenging for CYP and their family [27]. Given that CYPs’ needs are different from adults [28] and that physical, psychosocial, and emotional development impacts and influences the way they experience and cope with cSLE [11], it is imperative to view and understand this unique perspective from CYPs’ self-reported experiences to guide practice, research, and theory. Therefore, the aim of this review was to critically appraise and synthesize research that examines CYP’s experience and perspectives of living with cSLE.
2. Materials and Methods
An integrative review design enabled the inclusion of studies from a broad range of methodologies [29]. A comprehensive review of both quantitative and qualitative evidence was considered important in addressing the study’s objectives and identifying new insights and research opportunities. Whittemore and Knafl’s [30] integrative review framework was used, allowing for a rigorous review and synthesis of extant empirical research on the review topic.
2.1. Problem Identification and Search Strategy
An initial scoping review of databases was undertaken to refine the research question and focus the search strategy. A systematic search of databases (Scopus, CINAHL, Medline via PubMed, and PsycINFO via Ovid) was conducted in August 2021. A combination of search terms was utilized for population, exposure, and outcomes/themes; see Table 1. SLE Search terms.

Table 1.
Systemic lupus erythematosus integrative review search terms.
Boolean operators and truncation symbols enhanced search results, while proximity searches increased specificity. Keywords included text words, abbreviations, and truncated text words (Supplementary Table S1. Search Architecture). Limiters to the search included publication dates from 2000 to 2021 and empirical research published in peer-reviewed journals in the English language. Additional records were retrieved from manually reviewing the table of contents of relevant journals and reference lists of papers on the topic.
2.2. Eligibility Criteria
The inclusion criteria were: (1) original qualitative, quantitative, or mixed method research studies reporting on CYP’s experiences and perceptions of cSLE, including pain, lifestyle, activity levels, decision making, medication, quality of life, self-management, social impact, and patient-reported outcome measures; (2) participant’s aged 0–24 (based on children 0–18 and young people 10–24 as defined by WHO and the United Nations) [31,32]; (3) peer-reviewed journals in the English language: (4) published between 2000 and 2021. Abstracts, conference reports, editorial letters, the literature not formally published, and studies where the CYP’s voices could not be extrapolated from a parent–child dyad study were excluded.
2.3. Quality Appraisal
All included articles were appraised for quality using the Mixed Methods Appraisal Tool (MMAT) [33]. The MMAT is a critical appraisal tool that allows studies using various designs to be measured by similar quality appraisals, assessing studies on their generic research approach, individual components, and/or mixed methods approach [34]. Three authors independently assessed the quality of the included articles using the appropriate criteria from the MMAT [34]. (Supplementary Table S2 Mixed Methods Appraisal Tool Combined Results). If there were any disagreements between scores, these were then discussed with the research team until a consensus was agreed upon. No manuscripts were excluded based on a low critical appraisal score.
2.4. Data Management and Extraction
A data extraction form was developed (see Supplementary Materials File S1, data extract form) according to the Joanna Briggs Institute [35] and was categorized into the following subsections: study description, aim, design, sample/participants, location, data/quotes, and analysis against questions/outcomes of the paper. Initially, two authors extracted results from the included papers, and then three authors conducted a secondary review of the extracted data [35]. Results were recorded and exported to EndNote 20.4. (Bld 16297).
2.5. Data Synthesis and Analysis
Following Whittemore and Knafl’s [30] framework, all data from the nineteen articles were extracted and summarised in a data extraction table. This enabled the authors to understand what was known about CYP’s self-reported experience of living with cSLE and set the stage for inductive thematic data analysis [30]. Two authors independently identified initial codes, and all authors discussed the patterns in the data, grouping the codes into themes that encompassed the data.
3. Results
A total of 1636 articles were screened through database searches. Of these, 1617 were excluded because they did not meet the inclusion criteria (Figure 1). Nineteen studies were included in the review that involved more than 1400 CYP ranging in age from eight to twenty-four years of age [36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]; see Table 2 for Characteristics of Included Studies. Eleven studies used a quantitative design, seven a qualitative design, and one study followed a mixed-methods approach, as represented in Table 2. The studies were conducted across nine countries: the United States of America (11), Brazil (1), Columbia (1), China (1), Italy (1), the United Kingdom (1), Singapore (1), Australia (1), and Turkey (1). The included studies had MMAT scores ranging from four to five, with the Harry et al. (2019) study receiving the lowest score of two (Supplementary Table S2 Mixed Methods Appraisal Tool combined results).
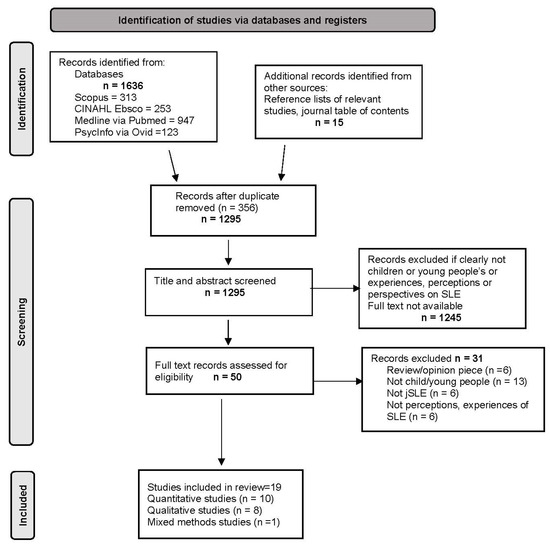
Figure 1.
Preferred reporting items for systematic reviews and meta-analysis (PRISMA) flow chart pre-eligibility screening criteria included.

Table 2.
Characteristics of included studies.
We identified four themes and fourteen sub-themes: (1) challenging symptoms (disruptions to life and altered self, severity, fatigue, depression, and anxiety), (2) medicines and side effects (dreaded steroids, conflicting feelings, and medication adherence), (3) complicated life (school sports and social, giving things up, lack of understanding, and quality of life) and (4) ways of coping (family and friends, relationships with health providers, and maintaining positivity). See Figure 2. Key themes representing young people’s experience of living with cSLE. Selected quotations to illustrate each sub-theme and the articles where the sub-themes were evident are provided in Table 3. Illustrative Quotes.
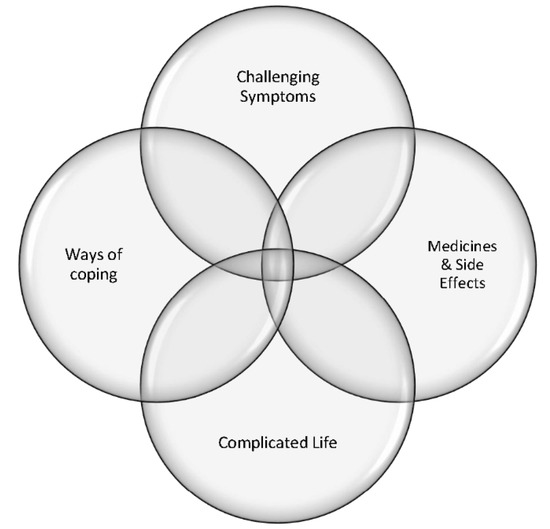
Figure 2.
Key themes representing young people’s experience of living with cSLE.

Table 3.
Illustrative Quotes (place holder).
4. Challenging Symptoms
Disruption to Life and Altered Self. The journey to a diagnosis was the first disruption experienced in the lives of CYP and resulted in feelings of resentment and stress [39,44,54]. Several studies reported that the first symptoms experienced at diagnosis were particularly challenging, as was the period of waiting for a diagnosis and trying to find appropriate treatment [37,49,52,54]. Participants described how at the time of diagnosis, they experienced self-doubt and questioned whether they possibly imagined symptoms [39,43,44,54]. Once the diagnosis was made, CYP found their sense of normalcy disrupted, and although they had confirmation of their symptoms, sharing the diagnosis with others was difficult, with some CYP choosing to keep their condition hidden [39] or preferring not to be defined by it [54].
Skin rashes, joint pain, muscle aches or weakness, loss of mobility, hair loss, and fatigue severely impacted CYPs’ self-perception [44,45,50,52] as they no longer saw themselves as young and healthy but instead sick and incapacitated. The severe emotional impact of cSLE resulted in feelings of grief and resentment towards the disease and a strong wish that cSLE had never entered their lives [50]. Two studies highlighted how symptoms severely influenced how CYP felt about their appearance, including making them feel unattractive [45], giving them a heightened sense of self-consciousness, and contributing to poor self-image [54]. Some CYP experienced being teased, described as a ‘freak’, or told that they looked ‘weird’ in school, which emphasized the feeling that they were different and not similar to their peers. This notion of being different was evident across other studies where CYP were acutely aware that the symptoms of cSLE imposed limitations on their ability to be normal [44,45,52,54].
Severity. The symptoms experienced by CYP were an individual and subjective experience [44,45,52,54]. CYP understood that cSLE had both minor and major symptoms, and although joint pain, muscle aches, weakness, and rashes were considered common, there was variability between ‘levels of disease’ and to what degree individuals were impacted [52,54]. Living with cSLE was therefore described as a very individual experience, with some participants ‘feeling lucky’ [54] about how it manifested in them, whereas others described their cSLE as more severe [44].
Fatigue. Eight of the nineteen studies addressed fatigue and described it as one of the most burdensome symptoms of cSLE [38,41,42,43,44,46,52,54]. Two studies examined fatigue and its relationship to depression and poor health-related quality of life (HRQoL) [38,42]. Furthermore, fatigue was reported to impact school activities, limiting CYP’s capacity to study and perform well at school [46,49,54]. When asked to comment on the strengths and weaknesses of the health-related quality of life/fatigue (Peds QL-FS) measure [52], CYP identified the need for a separate questionnaire to focus on fatigue as the ‘main issue’ with having cSLE [52].
Depression and Anxiety: Five studies reported depressive symptoms, anxiety, and suicidal ideation in CYP living with cSLE [41,42,45,46,47]. Assessment of depression was conducted using the children depression inventory (CDI) [42,45,46,47], the Patient Health Questionnaire-9 (PHQ-9) [41], and the Beck Depression Inventory (BDI-II) [47]. Three of these studies reported higher rates of depression and suicidal ideation among CYP living with cSLE compared to age and sex-matched healthy CYP and found links between depression, medication non-adherence, and appearance concerns [41,45,46]. In contrast, Donnelly et al. [42] and Kohut et al. [47] found near-normal values for both depressive symptoms and anxiety among CYP, noting an association between higher levels of depressive symptoms and reduction in HRQoL. Two studies assessed anxiety using the Screen for Child Anxiety Related Emotional Disorders (SCARED) questionnaire [42,46], where 50% of CYP in the Jones et al. [46] study and 34% of CYP in the Donnelly et al. [42] study reported clinically relevant anxiety levels that impacted on HRQoL.
5. Medicines and Side Effects
Dreaded Steroids. Medication regimes, especially the use of steroidal drugs, raised strong and opposing feelings among CYP [37,40,43,52,53,54]. CYP understood and appreciated the effectiveness of steroids in treating their cSLE [37,52,54] but also loathed the unpleasant side effects of weight gain, swollen face, skin changes (such as acne, striae, and flushing), and increased appetite [39,50,53]. Although the physical side effects were the most distressing aspect of taking steroids, CYP also experienced anxiety, wakefulness, higher physical depressive symptoms, and lower self-esteem [37,47,54]. Ruperto et al. (2004) [51] postulated poorer HRQoL in CYP with active disease or accumulated damage in the renal, central nervous, and musculoskeletal systems, including impaired self-esteem due to changes in body image from the associated side effects of aggressive corticosteroid and immunosuppressive medications. The significant side effects of steroids heightened the sense of self-consciousness, awkwardness, and awareness of being different [44,50].
Conflicting Feelings. Four studies described how cSLE medications posed a paradoxical dilemma for CYP, where being dependent on medications for life, multiple times a day, to maintain their health was described as weird, stressful, and nonsensical [40,52,53,54]. This was especially true when CYP believed their cSLE was too mild to warrant treatment or believed that it would not be a ‘big deal’ if they refrained from taking their medications [43,52,53,54]. Because medications were linked to changes in their face and body, social aspects of their life were further impacted; hence medications were not looked upon favorably [44]. However, CYP also came to appreciate the positive aspect of their medications when they started to feel better, and the right medications finally helped mitigate their symptoms [40,52,54]. CYP felt that sometimes health professionals would state cSLE was the reason for their symptoms when in fact, they believed the medications were the cause which created a situation where CYP felt at odds with the treatment plan [54].
Medication Adherence. CYP stated they did not take their prescribed medications because of forgetfulness, the number of pills, the bad taste, and/or concern about side effects [39,41,43,45,53]. Some CYP doubted the need for medications because they deemed they were not sick enough or felt their cSLE ‘wasn’t that bad’ [52,53], whereas others described a lack of perceived improvement in daily symptoms [43] as a barrier to adherence. Other common issues that impacted adherence were the logistics around taking medications, disruptions to normal activities, and sometimes business and/or getting out of the routine [39,43,53]. Two studies stated that adherence was influenced by a perceived lack of transparency from health professionals about the side effects [53,54].
Case et al. (2021) reported that a trusting patient–provider relationship positively impacted medication adherence, especially when CYP perceived healthcare professionals were working in their best interests. Other key factors that contributed to adherence were: recognizing the benefits through the acquisition of knowledge about cSLE; understanding how medication helped them control their disease, including reducing flares; and appreciating that medications enabled them to engage in activities to achieve their aspirations [40,43,53]. In addition, Tan et al. (2021) reported that parents’ attitudes, involvement, and strict monitoring of medication were critical to adherence.
6. Complicated Life
School, Sports, and Social Activities. The burden of treatment, constant clinic appointments, side effects of medication use, and symptoms all impacted daily life, including school attendance, performance [43,49], and sports and leisure activities [44,54]. CYP described a desire to do well at school but conceded that the unpredictable nature of cSLE resulted in a lack of control over educational pursuits [37,49]. Being able to participate and being included in normal school activities was described as a key way of coping with cSLE in a social context [50].
Giving Things Up. The sense of having to ‘give things up’ or being limited in pursuing life’s usual adventures, such as back packing or living overseas, was a source of frustration [44,50,54]. In addition, the prognostic uncertainty of cSLE led CYP to feel worried about their future and ability to achieve long-term goals [43,44,50,54]. This was reflected in their perceptions of limitations regarding educational and career aspirations, anxiety about the worsening or persistence of disease, concerns about a shorter lifespan, and the potential effect on their ability to have a family of their own [43,44,46,50,54].
Quality of Life. Six studies reported on how cSLE impacted HRQoL [36,38,42,46,48,51]. These studies used both generic tools such as the Pediatric Quality of Life Inventory Generic Core scale (PedsQL-GC) and the Child Health Questionnaire (CHQ) [36,37,42,46,48] as well as rheumatology-specific tools such as the Rheumatology Module (PedsQL-RM) [42,46,48,51] and Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) and British Isles Lupus Activity Group index (BILAG) tools [42,48,51]. Overall, when compared to healthy CYP, those with cSLE had poorer HRQoL across both physical and psychosocial domains [38,42,46,48,51] with the exception of Uzuner et al. (2017) [36], who found no difference in their study. When looking at specific symptoms and/or features of cSLE, the studies reported on a variety of factors that negatively impacted HRQoL, including the presence of musculoskeletal and general symptoms such as pain, mood, fatigue, and anxiety [38,42,46,48]; organ-specific disease damage particularly renal, central nervous, and musculoskeletal systems [38,46,48]; gender; and the use of cyclophosphamide and/rituximab [48].
Lack of Understanding. Coming to understand what cSLE is and how they came to have it resulted in CYP making associations and interpretations based on: what they were told by health professionals [43,44], explanations from parents [37,44], and information sources from the internet [54]. Sometimes these information sources were deemed to be too ‘sciencey’ [43], whereas others claimed they wanted to know everything they possibly could [54]. Children and young people also felt adults did not always provide the full picture, whereas it was important for CYP to know that cSLE was not going to go away [39,54].
Misunderstanding the nature of cSLE, the aetiology, and how it impacted CYP’s lives were commonly encountered [44,54]. There was a sense among CYP that family, friends, teachers, and even health professionals did not appreciate or understand the difficulty of living with cSLE, and consequently, empathy was lacking [39,43,44]. Misinformation created negative feelings, especially when it led to peers frantically wiping down surfaces for fear they would ‘catch’ cSLE [43,50]. This lack of understanding was deemed particularly important in relation to schools where CYP felt that education from health professionals to teachers might help with some of the challenges they faced [43]. More public exposure and the need for disease-specific information about cSLE were considered highly important [43,50,54].
7. Ways of Coping
Family and Friends. CYP described how talking to others with cSLE, either in person or online, was valuable for gaining a sense of belonging, being understood, and enhancing overall wellbeing [37,39,54]. Family members were deemed invaluable for providing emotional and practical support, access to treatment, encouraging medication adherence, and providing information about cSLE [37,39,43,44,50,53,54]. Several studies addressed the role that friends/peers played [39,53,54]. Relationships with peers provided invaluable emotional support that enabled CYP to cope and manage their life with cSLE [39,50]. Being included and encouraged to join normal activities [50] or being ‘cheered up’ about changes in appearance due to medication side effects [53,54] helped to combat feelings of being different from peers.
Relationships with Health Providers. Connectedness and collaborative relationships with health providers were key to coping with cSLE. Having trust and confidence in their health care provider enabled participants to manage cSLE and contributed to treatment adherence [39,43,53,54]. Studies highlighted how CYP highly valued health care professionals who were accommodating and took into consideration individual needs when developing treatment plans [39,43,53]. Connections and relationships with healthcare professionals were noted to be particularly important during the transition from pediatric to adult services [39,43,54]. The transition came with tension and unanticipated challenges for CYP; thus, willingness to transition was strongly influenced by the bonds they had with their first healthcare provider, which was usually the CYP’s rheumatologist [39,54].
Maintaining Positivity. Despite the many challenges of living with cSLE, CYP strived to maintain a positive attitude by viewing cSLE as not merely a challenge to overcome but also a means of developing self-confidence, empathy, resilience, and self-care abilities [39,44,50,53,54]. Thus, important life skills such as coping, empathy, and resiliency were acquired [39]. Further, CYP gained self-management skills, such as learning about their body and how to take care of it [44]. Others described how being focused and positive about learning to self-manage their medications prevented their family members from worrying [53]. In addition, some CYP experienced a recalibration of mindset and considered themselves ‘lucky’ to have cSLE rather than something they deemed more serious, such as cancer [39,44,54]. Finding a way to focus on the positive aspects of life, being grateful for the little things, and re-evaluating priorities were described as ways of coping [44,49,53,54].
8. Discussion
It is evident within this review that CYP living with cSLE experience a wide range of visible and invisible symptoms, including pain, fatigue, rashes, depression, anxiety, and altered body image that disrupts their normal psychosocial, emotional, physical, and developmental growth, and places them at higher risk of bullying, and adverse mental health outcomes than their peers. These findings are similar to the experiences of CYP with other rheumatological diseases where fatigue, anxiety, and depression have been shown to have a significant impact not only on HRQoL but day-to-day emotional and psychosocial wellbeing [23,55,56,57]. The impact and severity of cSLE were highlighted by this review as highly unique and, in the wider literature, influenced by individual demographic and illness characteristics, with a level of impact being strongly linked to disease activity and organ damage [2,58,59]. In addition, gender, age of diagnosis, type of immunosuppressive medication, number of flares, and ethnicity are factors that influence CYP’s likelihood of increased mortality [58,59,60].
Children and young people stated that the first step into their cSLE journey was waiting for a diagnosis, having their symptoms confirmed, and commencing treatment which triggered emotional turmoil, feelings of relief, and significant frustration. The difficulty in making an initial diagnosis of cSLE in CYP has been attributed to its multi-system involvement, atypical symptoms, variability in clinical presentation [2,58,61], as well as other factors, including demographic, clinical, and socioeconomic characteristics [62]. Given the importance of prompt diagnosis to prevent disease-related morbidity, Hussain et al. (2022) recommended the need for screening guidelines and policies to improve healthcare outcomes for CYP.
Medications played an important part in the management of cSLE and CYP’s experiences of living with it, including their self-perception, self-esteem, and relationships with healthcare providers. Children and young people described feeling anxious and worried about the side effects of medications particularly the Cushingoid features that accompanied the use of glucocorticoids. The changes to their body, mood, and sense of self related to steroid treatment represented a confronting and psychologically distressing aspect of cSLE. Glucocorticosteroids remain a foundational treatment in SLE [63]; however, it is increasingly recognized that the dose should be kept as low as possible in order to minimize both short and long-term side effects [64]. In addition, there is a recognized need to evaluate the side effects and benefits of steroid use from CYP’s perspective [65]. Given that most CYP in this review were adolescents, concerns about physical appearance and disturbance in body image were not surprising. Children and young people are extremely sensitive to and focused on changes to their appearance and the opinions of peers [66]. Alterations to their self and body image and to the psychological distress that may accompany changes potentially place them at increased risk of depression when compared to their healthy peers [67,68] and those with adult-onset SLE [69]. This points to the need for routine psychosocial screening of CYP with cSLE by health professionals to ensure at-risk and psychologically compromised CYP are identified and supported [24,70]. In addition, there is a need for increased awareness in practice and further research to identify strategies for improving early intervention for depression and anxiety in CYP with cSLE [57].
The conflicting feelings surrounding medication adherence were related to the burden of having to take medications every day, the disruption to normal life, and the potential risk of side effects; however, positive effects were experienced when medication improved CYP’s condition. Treatment adherence was influenced by having a trusting relationship with healthcare providers, feeling involved with decision-making about treatment, and developing personal knowledge and understanding about cSLE. These findings are consistent with adult studies and those related to other rheumatological conditions that describe the importance of resilience [71], the healthcare provider–patient relationship [72], and patient empowerment [73] as positively impacting medication adherence. Increasing CYPs’ knowledge about cSLE and medications and addressing concerns about side effects have been described as important ways to improve communication between CYP and healthcare professionals and improve adherence [16,74,75]. For CYP, this may require consideration of different approaches and broader access to educational material, such as online or web-based interventions and the use of social media, shown to enhance adherence and support young people in managing their cSLE medications [76,77]. Many CYP living with cSLE will never achieve an inactive disease state; therefore, medication adherence is a particularly important aspect of care, especially when using high immunosuppressive treatments [58,60].
Disruptions and interruptions to normal activities due to the burden of treatment, clinic appointments, side effects of medications, and feeling restricted in their ability to achieve future goals and aspirations created a complicated life for CYP living with cSLE. A correlation between neuropsychiatric symptoms, cognitive disorders, and poor academic performance in maths, learning, attention, information processing, memory, and completing school or college degrees has been reported in the literature as a significant factor for CYP with cSLE being unable to reach academic outcomes and aspirations [49,78,79]. Many CYP in this review spoke about how they felt school, family, and friends did not fully understand or appreciate the difficulties they faced living with cSLE and expressed concern about the lack of public knowledge regarding their disease. This was echoed in a study from the United Kingdom, where CYP felt that greater public awareness and wider communication about rheumatic conditions were needed, believing this would enable them to manage their daily challenges more easily [80]. Children and young people also recommended that research should focus on the lived experience of CYP to gain a greater understanding of the psychosocial impact of the illness, with CYP being actively consulted, included, and viewed as expert informants (64).
Social support systems, including peers, family, and cSLE support groups, were found to be necessary and important for coping with cSLE by CYP in this review. Organized events, such as camps for CYP with cSLE, were beneficial in providing social support through shared experiences and helping young people to normalize their life [81,82]. Camps for CYP offer opportunities for peer acceptance and social inclusion, and these benefits have been similarly described in studies in other long-term conditions such as diabetes [83], celiac disease [84], bleeding disorders [85], and epilepsy [86]. It is reported in the literature that CYP with cSLE has shown high coping scores for emotion-focused coping strategies (0.6 ± 0.2) and socially supported coping strategies (0.5 ± 0.2) linked to high happiness scores on the Brief Coping Orientation to Problems Experienced (COPE) questionnaire and the Subjective Happiness Scale (SHS) [87]. Remaining grateful and building on one’s self-confidence, resiliency, and self-care abilities in managing medications, treatment, and symptoms were some of the problem-focused coping strategies identified in this review. Similarly, CYP with cSLE had high self-reported coping scores for problem-focused coping (0.7 ± 0,2) associated with high levels of happiness (r = 0.564, p = 0.002) [87]. Despite these positive findings, CYP living with cSLE require individualized, multi-dimensional interventions and support to develop coping strategies to enhance their ability to respond to the multiple challenges imposed by cSLE. This includes the skills needed to effectively transition from CYP services to adult care [82,87,88].
This review highlighted that a multidisciplinary approach is needed that includes routine assessment of both physical and psychosocial symptoms as an essential approach to care, given that early intervention for depression has the potential to improve outcomes. Ongoing psychosocial support, health education, adherence interventions, and personalized treatment plans are necessary components of holistic care for CYP living with cSLE. In addition, there needs to be greater awareness and education to the public and general practitioners about the nature of cSLE, the early symptoms, complications, and treatment strategies. Future health care and research should focus on psychosocial and developmental wellbeing, resiliency, and practical strategies for managing and living with cSLE, fatigue, interventions to promote peer support networks, and medication adherence. Future research needs to be inclusive of CYPs’ voice, including the voices of younger children, and conducted in collaboration with service providers to ensure the best outcomes for CYP living with cSLE.
Limitations. This study, as with all integrative reviews, is limited by search terms, selected databases, and applied search strategy methods. In addition, this review is limited by including only empirical peer-reviewed studies published in English. Most of the instruments were well described, and reliability and validity were reported; however, due to the range and variability of instruments used, a meta-analysis of results was not possible. Not all studies described participants’ SLEDAI or SDI; therefore, it is not possible to draw comparisons between CYP’s experiences in terms of disease activity scores. Finally, CYP living with cSLE were not consulted on the results of this integrative review, given that the project commenced during the COVID-19 pandemic. Despite these limitations, the procedure undertaken by the authors in this review was rigorous and followed a systematic process.
9. Conclusions
While cSLE shares many similarities with adult-onset SLE, there are essential differences in terms of morbidity, impact of symptoms, and medication side effects that disrupt CYP’s day-to-day life. An awareness of the differences in experiences and perceptions of CYP is crucial. The significant psychological and social impact of cSLE and its treatment necessitates a comprehensive, holistic approach to managing care that considers the unique needs of CYP. Studies describe fatigue as the most common symptom among adults with SLE [89,90] and highlight the significant impact of depression and anxiety on quality and daily life [91,92]. There is an opportunity for children and young people to identify these symptoms earlier and potentially prevent these impacts as children grow into adulthood. The review highlights significant anxiety, fatigue, and depression among CYP due to cSLE and points to the need for further research and exploration to understand CYPs’ experiences and their support needs to more fully direct practice, research, policy, and knowledge.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children10061006/s1, Table S1: Search architecture; Table S2: MMAT combined results; File S1: Data extraction form.
Author Contributions
All authors made substantial contributions to the concept and design of the study. S.N. undertook the initial search of the literature. J.B. conducted a confirmatory search. J.B., M.F. and A.D. reviewed and evaluated the selected articles. J.B. and M.F. extracted data. J.B., M.F. and A.D. analyzed and developed the themes. J.B. drafted the article, and then M.F., A.D. and S.N. made edits. All authors have read and agreed to the published version of the manuscript.
Funding
This research received AUT School of Clinical Sciences PBRF funding for open access publication fees.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data available in a publicly accessible repository.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Silva, C.A.; Avcin, T.; Brunner, H.I. Taxonomy for systemic lupus erythematosus with onset before adulthood. Arthritis Care Res. 2012, 64, 1787–1793. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.M.D.; Lythgoe, H.; Midgley, A.; Beresford, M.W.; Hedrich, C.M. Juvenile-onset systemic lupus erythematosus: Update on clinical presentation, pathophysiology and treatment options. Clin. Immunol. 2019, 209, 108274. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, D.; O’Connor, C.; Nertney, L.; MacDermott, E.J.; Mullane, D.; Franklin, O.; Killeen, O.G. Juvenile systemic lupus erythematosus presenting as pancarditis. Pediatr. Rheumatol. 2019, 17, 71. [Google Scholar] [CrossRef] [PubMed]
- Hiraki, L.T.; Feldman, C.H.; Liu, J.; Alarcón, G.S.; Fischer, M.A.; Winkelmayer, W.C.; Costenbader, K.H. Prevalence, incidence, and demographics of systemic lupus erythematosus and lupus nephritis from 2000 to 2004 among children in the US medicaid beneficiary population. Arthritis Rheum. 2012, 64, 2669–2676. [Google Scholar] [CrossRef]
- Pineles, D.; Valente, A.; Warren, B.; Peterson, M.; Lehman, T.; Moorthy, L. Worldwide incidence and prevalence of pediatric onset systemic lupus erythematosus. Lupus 2011, 20, 1187–1192. [Google Scholar] [CrossRef]
- Huemer, C.; Huemer, M.; Dorner, T.; Falger, J.; Schacherl, H.; Bernecker, M.; Artacker, G.; Pilz, I. Incidence of pediatric rheumatic diseases in a regional population in Austria. J. Rheumatol. 2001, 28, 2116–2119. [Google Scholar]
- Concannon, A.; Rudge, S.; Yan, J.; Reed, P. The incidence, diagnostic clinical manifestations and severity of juvenile systemic lupus erythematosus in New Zealand Maori and Pacific Island children: The Starship experience (2000−2010). Lupus 2013, 22, 1156–1161. [Google Scholar] [CrossRef]
- Golder, V.; Tsang-A-Sjoe, M.W.P. Treatment targets in SLE: Remission and low disease activity state. Rheumatology 2020, 59 (Suppl. S5), v19–v28. [Google Scholar] [CrossRef]
- Brunner, H.I.; Gladman, D.D.; Ibañez, D.; Urowitz, M.D.; Silverman, E.D. Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum. 2008, 58, 556–562. [Google Scholar] [CrossRef]
- Tucker, L.B.; Uribe, A.G.; Fernández, M.; Vilá, L.M.; McGwin, G.; Apte, M.; Fessler, B.J.; Bastian, H.M.; Reveille, J.D.; Alarcón, G.S. Adolescent onset of lupus results in more aggressive disease and worse outcomes: Results of a nested matched case-control study within LUMINA, a multiethnic US cohort (LUMINA LVII). Lupus 2008, 17, 314–322. [Google Scholar] [CrossRef]
- McGill, G.; Ambrose, N. The management of lupus in young people. Br. J. Gen. Pract. 2018, 68, 96. [Google Scholar] [CrossRef]
- Ali, A.; Sayyed, Z.; Ameer, M.A.; Arif, A.W.; Kiran, F.; Iftikhar, A.; Iftikhar, W.; Ahmad, M.Q.; Malik, M.B.; Kumar, V.; et al. Systemic Lupus Erythematosus: An Overview of the Disease Pathology and Its Management. Cureus 2018, 10, e3288. [Google Scholar] [CrossRef]
- Robinson, D., Jr.; Aguilar, D.; Schoenwetter, M.; Dubois, R.; Russak, S.; Ramsey-Goldman, R.; Navarra, S.; Hsu, B.; Revicki, D.; Cella, D.; et al. Impact of systemic lupus erythematosus on health, family, and work: The patient perspective. Arthritis Care Res. 2010, 62, 266–273. [Google Scholar] [CrossRef]
- Yelin, E.; Yazdany, J.; Trupin, L. Relationship Between Poverty and Mortality in Systemic Lupus Erythematosus. Arthritis Care Res. 2018, 70, 1101–1106. [Google Scholar] [CrossRef] [PubMed]
- Gatto, M.; Zen, M.; Iaccarino, L.; Doria, A. New therapeutic strategies in systemic lupus erythematosus management. Nat. Rev. Rheumatol. 2019, 15, 30–48. [Google Scholar] [CrossRef] [PubMed]
- Farinha, F.; Freitas, F.; Águeda, A.; Cunha, I.; Barcelos, A. Concerns of patients with systemic lupus erythematosus and adherence to therapy—A qualitative study. Patient Prefer. Adherence 2017, 11, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Olesińska, M.; Saletra, A. Quality of life in systemic lupus erythematosus and its measurement. Reumatologia 2018, 56, 45–54. [Google Scholar] [PubMed]
- Gomez, A.; Qiu, V.; Cederlund, A.; Borg, A.; Lindblom, J.; Emamikia, S.; Enman, Y.; Lampa, J.; Parodis, I. Adverse Health-Related Quality of Life Outcome Despite Adequate Clinical Response to Treatment in Systemic Lupus Erythematosus. Front. Med. 2021, 8, 651249. [Google Scholar] [CrossRef] [PubMed]
- Bugni, V.M.; Ozaki, L.S.; Okamoto, K.Y.; Barbosa, C.M.; Hilário, M.O.; Len, C.A.; Terreri, M.T. Factors associated with adherence to treatment in children and adolescents with chronic rheumatic diseases. J. Pediatr. 2012, 88, 483–488. [Google Scholar] [CrossRef]
- Costedoat-Chalumeau, N.; Pouchot, J.; Guettrot-Imbert, G.; Le Guern, V.; Leroux, G.; Marra, D.; Morel, N.; Piette, J.C. Adherence to treatment in systemic lupus erythematosus patients. Best Pract. Res. Clin. Rheumatol. 2013, 27, 329–340. [Google Scholar] [CrossRef]
- Ciosek, A.L.; Makris, U.E.; Kramer, J.; Bermas, B.L.; Solow, E.B.; Wright, T.; Bitencourt, N. Health Literacy and Patient Activation in the Pediatric to Adult Transition in Systemic Lupus Erythematosus: Patient and Health Care Team Perspectives. ACR Open Rheumatol. 2022, 4, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, T.B.; Knight, A.M. Disparities in Childhood-Onset Lupus. Rheum. Dis. Clin. N. Am. 2020, 46, 661–672. [Google Scholar] [CrossRef]
- Fair, D.C.; Rodriguez, M.; Knight, A.M.; Rubinstein, T.B. Depression and Anxiety in Patients with Juvenile Idiopathic Arthritis: Current Insights and Impact on Quality of Life, A Systematic Review. Open Access Rheumatol. 2019, 11, 237–252. [Google Scholar] [CrossRef]
- Davis, A.M.; Rubinstein, T.B.; Rodriguez, M.; Knight, A.M. Mental health care for youth with rheumatologic diseases—Bridging the gap. Pediatr. Rheumatol. 2017, 15, 85. [Google Scholar] [CrossRef] [PubMed]
- Treemarcki, E.B.; Danguecan, A.N.; Cunningham, N.R.; Knight, A.M. Mental Health in Pediatric Rheumatology: An Opportunity to Improve Outcomes. Rheum. Dis. Clin. N. Am. 2022, 48, 67–90. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.M.D.; Egbivwie, N.; Cowan, K.; Ramanan, A.V.; Pain, C.E. Research priority setting for paediatric rheumatology in the UK. Lancet Rheumatol. 2022, 4, e517–e524. [Google Scholar] [CrossRef]
- Groot, N.; Shaikhani, D.; Teng, Y.K.O.; de Leeuw, K.; Bijl, M.; Dolhain, R.; Zirkzee, E.; Fritsch-Stork, R.; Bultink, I.E.M.; Kamphuis, S. Long-Term Clinical Outcomes in a Cohort of Adults With Childhood-Onset Systemic Lupus Erythematosus. Arthritis Rheumatol 2019, 71, 290–301. [Google Scholar] [CrossRef]
- Kirk, S.; Fraser, C. Hospice support and the transition to adult services and adulthood for young people with life-limiting conditions and their families: A qualitative study. Palliat. Med. 2014, 28, 342–352. [Google Scholar] [CrossRef]
- Neville, S.; Napier, S.; Adams, J.; Wham, C.; Jackson, D. An integrative review of the factors related to building age-friendly rural communities. J. Clin. Nurs. 2016, 25, 2402–2412. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K.A. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- World Health Organization. Adolescence: A Period Needing Special Attention. Available online: http://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html (accessed on 6 April 2022).
- United Nations. Convention on the Rights of the Child 1989. Available online: https://www.unicef.org/child-rights-convention (accessed on 5 August 2016).
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; et al. Improving the content validity of the mixed methods appraisal tool: A modified e-Delphi study. J. Clin. Epidemiol. 2019, 111, 49–59.e1. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Pearson, A.; White, H.; Bath-Hextall, F.; Apostolo, J.; Salmond, S.; Kirkpatrick, P. Methodology for JBI mixed methods systematic reviews. Joanna Briggs Inst. Rev. Man. 2014, 1, 5–34. [Google Scholar]
- Uzuner, S.; Sahin, S.; Durcan, G.; Adrovic, A.; Barut, K.; Kilicoglu, A.G.; Bilgic, A.; Bahali, K.; Kasapcopur, O. The impact of peer victimization and psychological symptoms on quality of life in children and adolescents with systemic lupus erythematosus. Clin. Rheumatol. 2017, 36, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- Beckerman, N.; Sarracco, M. Listening to lupus patients and families: Fine tuning the assessment. Soc. Work Health Care 2012, 51, 597–612. [Google Scholar] [CrossRef]
- Brunner, H.I.; Higgins, G.C.; Wiers, K.; Lapidus, S.K.; Olson, J.C.; Onel, K.; Punaro, M.; Ying, J.; Klein-Gitelman, M.S.; Seid, M. Health-related quality of life and its relationship to patient disease course in childhood-onset systemic lupus erythematosus. J. Rheumatol. 2009, 36, 1536–1545. [Google Scholar] [CrossRef] [PubMed]
- Case, S.; Sinnette, C.; Phillip, C.; Grosgogeat, C.; Costenbader, K.H.; Leatherwood, C.; Feldman, C.H.; Son, M.B. Patient experiences and strategies for coping with SLE: A qualitative study. Lupus 2021, 30, 1405–1414. [Google Scholar] [CrossRef]
- Ceppas Resende, O.L.; Barbosa, M.T.; Simões, B.F.; Velasque, L.S. The representation of getting ill in adolescents with systemic lupus erythematosus. Rev. Bras. Reum. Engl. Ed. 2016, 56, 398–405. [Google Scholar] [CrossRef]
- Davis, A.M.; Graham, T.B.; Zhu, Y.; McPheeters, M.L. Depression and medication nonadherence in childhood-onset Systemic Lupus Erythematosus. Lupus 2018, 27, 1532–1541. [Google Scholar] [CrossRef]
- Donnelly, C.; Cunningham, N.; Jones, L.T.; Ji, L.; Brunner, H.I.; Kashikar-Zuck, S. Fatigue and depression predict reduced health-related quality of life in childhood-onset lupus. Lupus 2018, 27, 124–133. [Google Scholar] [CrossRef]
- Harry, O.; Crosby, L.E.; Smith, A.W.; Favier, L.; Aljaberi, N.; Ting, T.V.; Huggins, J.L.; Modi, A.C. Self-management and adherence in childhood-onset systemic lupus erythematosus: What are we missing? Lupus 2019, 28, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Hernández Zapata, L.J.; Alzate Vanegas, S.I.; Eraso, R.M.; Yepes Delgado, C.E. Lupus: “like a cancer but tinier”. Perceptions of systemic lupus erythematosus among adolescents nearing transition to adult care. Rev. Colomb. Reumatol. 2018, 25, 151–160. [Google Scholar] [CrossRef]
- Ji, L.; Lili, S.; Jing, W.; Yanyan, H.; Min, W.; Juan, X.; Hongmei, S. Appearance concern and depression in adolescent girls with systemic lupus erythematous. Clin. Rheumatol. 2012, 31, 1671–1675. [Google Scholar] [CrossRef]
- Jones, J.T.; Cunningham, N.; Kashikar-Zuck, S.; Brunner, H.I. Pain, Fatigue, and Psychological Impact on Health-Related Quality of Life in Childhood-Onset Lupus. Arthritis Care Res. 2016, 68, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Kohut, S.; Williams, T.S.; Jayanthikumar, J.; Landolt-Marticorena, C.; Lefebvre, A.; Silverman, E.; Levy, D.M. Depressive symptoms are prevalent in childhood-onset Systemic Lupus Erythematosus (cSLE). Lupus 2013, 22, 712–720. [Google Scholar] [CrossRef]
- Moorthy, L.N.; Baldino, M.E.; Kurra, V.; Puwar, D.; Llanos, A.; Peterson, M.G.E.; Hassett, A.L.; Lehman, T.J. Relationship between health-related quality of life, disease activity and disease damage in a prospective international multicenter cohort of childhood onset Systemic Lupus Erythematosus patients. Lupus 2017, 26, 255–265. [Google Scholar] [CrossRef]
- Moorthy, L.N.; Peterson, M.G.; Hassett, A.; Baratelli, M.; Lehman, T.J. Impact of lupus on school attendance and performance. Lupus 2010, 19, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, L.N.; Robbins, L.; Harrison, M.J.; Peterson, M.G.E.; Cox, N.; Onel, K.B.; Lehman, T.J.A. Quality of life in paediatric lupus. Lupus 2004, 13, 234–240. [Google Scholar] [CrossRef]
- Ruperto, N.; Buratti, S.; Duarte-Salazar, C.; Pistorio, A.; Reiff, A.; Bernstein, B.; Maldonado-Velázquez, M.R.; Beristain-Manterola, R.; Maeno, N.; Takei, S.; et al. Health-related quality of life in juvenile-onset systemic lupus erythematosus and its relationship to disease activity and damage. Arthritis Rheum. 2004, 51, 458–464. [Google Scholar] [CrossRef]
- Smith, E.M.D.; Gorst, S.L.; Al-Abadi, E.; Hawley, D.P.; Leone, V.; Pilkington, C.; Ramanan, A.V.; Rangaraj, S.; Sridhar, A.; Beresford, M.W.; et al. “It is good to have a target in mind”: Qualitative views of patients and parents informing a treat to target clinical trial in JSLE. Rheumatology 2021, 60, 5630–5641. [Google Scholar] [CrossRef]
- Tan, Q.E.C.; Gao, X.; Ang, W.H.D.; Lau, Y. Medication adherence: A qualitative exploration of the experiences of adolescents with systemic lupus erythematosus. Clin. Rheumatol. 2021, 40, 2717–2725. [Google Scholar] [CrossRef] [PubMed]
- Tunnicliffe, D.J.; Singh-Grewal, D.; Chaitow, J.; MacKie, F.; Manolios, N.; Lin, M.W.; O’Neill, S.G.; Ralph, A.F.; Craig, J.C.; Tong, A. Lupus Means Sacrifices: Perspectives of Adolescents and Young Adults with Systemic Lupus Erythematosus. Arthritis Care Res. 2016, 68, 828–837. [Google Scholar] [CrossRef]
- Nakayama, A.; Tunnicliffe, D.J.; Thakkar, V.; Singh-Grewal, D.; O’Neill, S.; Craig, J.C.; Tong, A. Patients’ Perspectives and Experiences Living with Systemic Sclerosis: A Systematic Review and Thematic Synthesis of Qualitative Studies. J. Rheumatol. 2016, 43, 1363. [Google Scholar] [CrossRef] [PubMed]
- Fawole, O.A.; Reed, M.V.; Harris, J.G.; Hersh, A.; Rodriguez, M.; Onel, K.; Lawson, E.; Rubinstein, T.; Ardalan, K.; Morgan, E.; et al. Engaging patients and parents to improve mental health intervention for youth with rheumatological disease. Pediatr. Rheumatol. 2021, 19, 19. [Google Scholar] [CrossRef]
- Quilter, M.C.; Hiraki, L.T.; Korczak, D.J. Depressive and anxiety symptom prevalence in childhood-onset systemic lupus erythematosus: A systematic review. Lupus 2019, 28, 878–887. [Google Scholar] [CrossRef]
- Cann, M.P.; Sage, A.M.; McKinnon, E.; Lee, S.J.; Tunbridge, D.; Larkins, N.G.; Murray, K.J. Childhood Systemic Lupus Erythematosus: Presentation, management and long-term outcomes in an Australian cohort. Lupus 2022, 31, 246–255. [Google Scholar] [CrossRef]
- Li, W.; Liu, S.; Zhong, L.; Chen, C. Clinical and laboratory features, disease activity, and outcomes of juvenile systemic lupus erythematosus at diagnosis: A single-center study from southern China. Clin. Rheumatol. 2021, 40, 4545–4552. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, N.; Beresford, M.W.; Leone, V. Challenges of achieving clinical remission in a national cohort of juvenile-onset systemic lupus erythematosus patients. Lupus 2019, 28, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Nahar, D.N.; Nahar, P.N. A Children’s Tale: Unusual Presentation of Juvenile SLE. J. Rheum. Dis. Treat. 2022, 8, 96. [Google Scholar]
- Hussain, A.; Maheshwari, M.V.; Khalid, N.; Patel, P.D.; Alghareeb, R. Diagnostic Delays and Psychosocial Outcomes of Childhood-Onset Systemic Lupus Erythematosus. Cureus 2022, 14, e26244. [Google Scholar] [CrossRef]
- Felten, R.; Sagez, F.; Gavand, P.-E.; Martin, T.; Korganow, A.-S.; Sordet, C.; Javier, R.-M.; Soulas-Sprauel, P.; Rivière, M.; Scher, F.; et al. 10 most important contemporary challenges in the management of SLE. Lupus Sci. Med. 2019, 6, e000303. [Google Scholar] [CrossRef]
- van Vollenhoven, R.F.; Mosca, M.; Bertsias, G.; Isenberg, D.; Kuhn, A.; Lerstrøm, K.; Aringer, M.; Bootsma, H.; Boumpas, D.; Bruce, I.N.; et al. Treat-to-target in systemic lupus erythematosus: Recommendations from an international task force. Ann. Rheum. Dis. 2014, 73, 958. [Google Scholar] [CrossRef] [PubMed]
- Mathias, S.D.; Berry, P.; De Vries, J.; Askanase, A.; Pascoe, K.; Colwell, H.H.; Chang, D.J. Development of the Systemic Lupus Erythematosus Steroid Questionnaire (SSQ): A novel patient-reported outcome tool to assess the impact of oral steroid treatment. Health Qual. Life Outcomes 2017, 15, 43. [Google Scholar] [CrossRef]
- Andrews, J.L.; Foulkes, L.; Blakemore, S.J. Peer Influence in Adolescence: Public-Health Implications for COVID-19. Trends Cogn. Sci. 2020, 24, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Weiss, P.; Morales, K.; Gerdes, M.; Gutstein, A.; Vickery, M.; Keren, R. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: A cross-sectional study. Pediatr. Rheumatol. 2014, 12, 42. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.M.; Xie, M.; Mandell, D.S. Disparities in Psychiatric Diagnosis and Treatment for Youth with Systemic Lupus Erythematosus: Analysis of a National US Medicaid Sample. J. Rheumatol. 2016, 43, 1427–1433. [Google Scholar] [CrossRef]
- Knight, A.M.; Trupin, L.; Katz, P.; Yelin, E.; Lawson, E.F. Depression Risk in Young Adults With Juvenile- and Adult-Onset Lupus: Twelve Years of Followup. Arthritis Care Res. 2018, 70, 475–480. [Google Scholar] [CrossRef]
- Yeo, M.S.; Bond, L.M.; Sawyer, S.M. Health risk screening in adolescents: Room for improvement in a tertiary inpatient setting. Med. J. Aust. 2005, 183, 427–429. [Google Scholar] [CrossRef]
- Mendoza-Pinto, C.; García-Carrasco, M.; Campos-Rivera, S.; Munguía-Realpozo, P.; Etchegaray-Morales, I.; Ayón-Aguilar, J.; Alonso-García, N.E.; Méndez-Martínez, S. Medication adherence is influenced by resilience in patients with systemic lupus erythematosus. Lupus 2021, 30, 1051–1057. [Google Scholar] [CrossRef]
- Georgopoulou, S.; Prothero, L.; D’Cruz, D.P. Physician-patient communication in rheumatology: A systematic review. Rheumatol. Int. 2018, 38, 763–775. [Google Scholar] [CrossRef]
- Náfrádi, L.; Nakamoto, K.; Schulz, P.J. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE 2017, 12, e0186458. [Google Scholar] [CrossRef]
- Daleboudt, G.M.; Broadbent, E.; McQueen, F.; Kaptein, A.A. Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Res. 2011, 63, 342–350. [Google Scholar]
- Emamikia, S.; Gentline, C.; Enman, Y.; Parodis, I. How Can We Enhance Adherence to Medications in Patients with Systemic Lupus Erythematosus? Results from a Qualitative Study. J. Clin. Med. 2022, 11, 1857. [Google Scholar] [CrossRef]
- Scalzi, L.V.; Hollenbeak, C.S.; Mascuilli, E.; Olsen, N. Improvement of medication adherence in adolescents and young adults with SLE using web-based education with and without a social media intervention, a pilot study. Pediatr. Rheumatol. Online J. 2018, 16, 18. [Google Scholar] [CrossRef]
- Stinson, J.; Wilson, R.; Gill, N.; Yamada, J.; Holt, J. A systematic review of internet-based self-management interventions for youth with health conditions. J. Pediatr. Psychol. 2009, 34, 495–510. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.S.; Aranow, C.; Ross, G.S.; Barsdorf, A.; Imundo, L.F.; Eichenfield, A.H.; Kahn, P.J.; Diamond, B.; Levy, D.M. Neurocognitive impairment in childhood-onset systemic lupus erythematosus: Measurement issues in diagnosis. Arthritis Care Res. 2011, 63, 1178–1187. [Google Scholar] [CrossRef]
- Frittoli, R.B.; de Oliveira Peliçari, K.; Bellini, B.S.; Marini, R.; Fernandes, P.T.; Appenzeller, S. Association between academic performance and cognitive dysfunction in patients with juvenile systemic lupus erythematosus. Rev. Bras. Reum. Engl. Ed. 2016, 56, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Parsons, S.; Thomson, W.; Cresswell, K.; Starling, B.; McDonagh, J.E.; On behalf of the Barbara Ansell National Network for Adolescent Rheumatology. What do young people with rheumatic disease believe to be important to research about their condition? A UK-wide study. Pediatr. Rheumatol. 2017, 15, 53. [Google Scholar] [CrossRef] [PubMed]
- Saez, C.; Nassi, L.; Wright, T.; Makris, U.E.; Kramer, J.; Bermas, B.L.; Solow, E.B.; Bitencourt, N. Therapeutic recreation camps for youth with childhood-onset systemic lupus erythematosus: Perceived psychosocial benefits. Pediatr. Rheumatol. 2022, 20, 39. [Google Scholar] [CrossRef]
- Bitencourt, N.; Ciosek, A.; Kramer, J.; Solow, E.B.; Bermas, B.; Wright, T.; Nassi, L.; Makris, U. “You Just Have to Keep Going, You Can’t Give Up”: Coping mechanisms among young adults with lupus transferring to adult care. Lupus 2021, 30, 2221–2229. [Google Scholar] [CrossRef]
- Barone, M.T.; Vivolo, M.A.; Madden, P.B. Are diabetes camps effective? Diabetes Res. Clin. Pract. 2016, 114, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Shani, M.; Kraft, L.; Müller, M.; Boehnke, K. The potential benefits of camps for children and adolescents with celiac disease on social support, illness acceptance, and health-related quality of life. J. Health Psychol. 2020, 27, 1635–1645. [Google Scholar] [CrossRef] [PubMed]
- Faith, M.A.; Boone, D.M.; Kalin, J.A.; Healy, A.S.; Rawlins, J.; Mayes, S. Improvements in Psychosocial Outcomes Following a Summer Camp for Youth with Bleeding Disorders and Their Siblings. J. Pediatr. Nurs. 2021, 61, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Cushner Weinstein, S.; Berl, M.; Salpekar, J.; Johnson, J.; Pearl, P.; Conry, J.; Kolodgie, M.; Scully, A.; Gaillard, W.; Weinstein, S. The benefits of a camp designed for children with epilepsy: Evaluating adaptive behaviors over 3 years. Epilepsy Behav. 2007, 10, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Poole, B.D.; Silva, B.; Figueiredo-Braga, M. Specific coping strategies in JSLE depression and anxiety–the untold story of brave soldiers. J. Immunol. 2021, 206, 66.15. [Google Scholar] [CrossRef]
- Pratsidou-Gertsi, P. Transition of the patient with Childhood-onset SLE. Mediterr. J. Rheumatol. 2016, 27, 94–97. [Google Scholar] [CrossRef]
- Alain, C.; Jeanette, A.; Kirsi, M.; Angela, E.; Laurent, A. Living with systemic lupus erythematosus in 2020: A European patient survey. Lupus Sci. Med. 2021, 8, e000469. [Google Scholar]
- Raymond, K.; Park, J.; Joshi, A.V.; White, M.K. Patient Experience With Fatigue and Qualitative Interview-Based Evidence of Content Validation of The FACIT-Fatigue in Systemic Lupus Erythematosus. Rheumatol. Ther. 2021, 8, 541–554. [Google Scholar] [CrossRef]
- Figueiredo-Braga, M.; Cornaby, C.; Cortez, A.; Bernardes, M.; Terroso, G.; Figueiredo, M.; Mesquita, C.D.S.; Costa, L.; Poole, B.D. Depression and anxiety in systemic lupus erythematosus: The crosstalk between immunological, clinical, and psychosocial factors. Medicine 2018, 97, e11376. [Google Scholar] [CrossRef]
- Zhang, L.; Fu, T.; Yin, R.; Zhang, Q.; Shen, B. Prevalence of depression and anxiety in systemic lupus erythematosus: A systematic review and meta-analysis. BMC Psychiatry 2017, 17, 70. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).