Highlights
What are the main findings?
- This review addresses the comorbidity of chronic pain and ADHD in youth, highlighting their negative impact on functioning and the need for further research in this area.
- This study aims to estimate the prevalence of non-headache chronic pain among youth with ADHD and vice versa and to explore potential shared mechanisms between the two conditions.
What is the implication of the main finding?
- In total, eleven studies were included in this review, which indicated a higher prevalence of ADHD in youth experiencing chronic pain and a higher prevalence of chronic pain in youth diagnosed with ADHD.
- This review concludes that while there is an association between chronic pain and ADHD in youth, there is a lack of research on the underlying mechanisms of this comorbidity, suggesting a need for future studies to investigate this aspect.
Abstract
Background: Chronic pain and ADHD are common conditions among youth that negatively impact functioning. This review fills a critical gap by summarizing current research on chronic pain and ADHD comorbidity, and it proposes a conceptual model of shared associations and underlying mechanisms. Objective: The aims of the current study were to: (1) review the extant literature and present estimates of the prevalence of comorbid non-headache chronic pain and ADHD in youth and (2) describe potential shared mechanisms for ADHD and chronic non-headache pain in youth. We also outline future directions to inform future research and interventions directed to youth with comorbid pain and ADHD. Design: A scoping review of the literature was performed in MEDLINE, PsycInfo, and Cochrane Database of Systematic Reviews using a wide range of search terms related to pain, Attention Deficit-Hyperactivity Disorder, childhood, adolescence, and young adulthood. Results: Eleven published studies were included in the review. These studies examined the prevalence of chronic pain among youth with ADHD, the prevalence of ADHD in chronic pain samples, and the association between chronic pain and ADHD among youth. Findings revealed results from studies indicating a higher prevalence of ADHD among youth with chronic pain and a higher prevalence of chronic pain in samples of youth with ADHD. Conclusions: Findings from this scoping review suggest an association between chronic pain and ADHD among youth. Little research was found to examine the etiology of this association. Future studies should examine underlying mechanisms of comorbid chronic pain and ADHD.
1. Introduction
Chronic pain, defined as pain lasting 3 months or longer [1], is common during childhood. Approximately 23% of children and adolescents experience chronic pain [2], and it has a significant impact on psychological, social and economic outcomes [3,4]. The etiology of chronic pain varies, and in 13–33% of cases, there is no known etiology to chronic pain in youth [5,6]. Chronic pain is associated with significant disability as well as poor outcomes that persist into adulthood [7]. Youth with chronic pain are more likely to report poor quality of life, problems with social and school functioning, and poorer mental health [8]. Furthermore, female sex, depression, poor sleep, post-traumatic stress and parental factors [9] are risk factors for developing chronic pain in youth [10,11]. However, the mechanisms by which these risk factors lead to the development of chronic pain among youth are not yet well understood.
ADHD is a neurodevelopmental disorder that impairs cognitive, emotional, and behavioral functioning. It is characterized by either attentional problems (inattentive presentation), hyperactivity (hyperactive presentation), or most commonly both (combined presentation) [12]. Prevalence estimates of ADHD vary depending on country and study methodology, but it affects approximately 3–4% of children and adolescents worldwide [13,14]. Prevalence estimates vary primarily due to year of study, country of origin and diagnostic criteria. The etiology of ADHD is complex and not well understood, but evidence supports theories of delayed brain maturation and dopamine system dysfunction [15,16]. ADHD in childhood and adolescence is associated with a range of adverse health outcomes, including poor academic achievement, social problems, comorbid psychopathology and functional impairment [17], which often persist into adulthood [18]. Untreated ADHD in adulthood is associated with poor quality of life and high risk of substance use [19]. Furthermore, the societal and economic impacts of ADHD are significant across the lifespan [20]. Additional research is needed to investigate etiologies of ADHD and more effective treatment of ADHD.
Chronic Pain and ADHD
Research on pediatric chronic pain suggests comorbidity and related mechanisms with a variety of psychiatric disorders, including depression [21], anxiety disorders [22] and post-traumatic stress disorder (PTSD) [23]. Many of these psychological factors function as risk factors for chronic pain [24]. However, only a few studies have examined the prevalence of ADHD and comorbid chronic pain, and the majority of existing research has been conducted with adults [15]. A 2018 systematic review by Instanes et al. focused on associations between adult ADHD and comorbid medical/somatic diseases [25]. The review found increased prevalence rates of various somatic diseases but did not specifically focus on pain-related conditions. Other studies with adults have found that ADHD is more prevalent among people with various chronic pain conditions [26,27,28,29,30]. Retrospective studies have found that childhood ADHD is associated with higher rates of fibromyalgia in adulthood [31,32]. Moreover, research suggests that ADHD is associated with increased pain perception [33], that chronic pain reduces attention span [30], and that adults with ADHD have significantly higher prevalence of pain reports compared to controls [26]. Similarly, prevalence studies suggest that children with hyperactivity/inattention problems are more likely to experience multiple, recurrent subjective health complaints [34]. Recent reviews of the pediatric literature have also found that ADHD is associated with migraines [35] and other headaches [36]. Prevalence rates of ADHD were found to range between 36.5 and 20% for children diagnosed with primary headache disorders, tension type headaches and migraines. Additionally, ADHD has been suggested as a risk factor for sensory processing disorders and increased prevalence of neurologic disorders among children [37,38]. These conditions might in turn affect the pain experience and possibly the development of chronic pain.
The potential association between ADHD and pediatric chronic non-headache pain has not yet been systematically reviewed. The aims of the current study were to: (1) review the extant literature and present estimates of the prevalence of comorbid non-headache chronic pain and ADHD in youth and (2) describe potential shared mechanisms for ADHD and non-headache chronic pain in youth. We also outline future directions to inform future research and interventions directed to youth with comorbid pain and ADHD.
2. Aim 1: Scoping Review of the Literature
A substantial body of research has demonstrated associations among youth with chronic pain and internalizing symptoms (e.g., depression [21] and anxiety [22]), but there has been less focus on associations between chronic pain and ADHD. Additionally, little research has focused on children with ADHD and their experience with chronic pain. Given the availability of a recently published systematic review on ADHD and headache in childhood [36], we performed a scoping review to examine the association between ADHD and non-headache chronic pain to help identify gaps in the extant research that may warrant further investigation.
2.1. Methods
This scoping review was conducted between November 2020 and April 2022. The authors created an unregistered search and review protocol based on the methods practices of the Joanna Briggs Institute Manual of Evidence Synthesis [39], and they utilized the framework described by Arksey and O’Malley [40]. MEDLINE, PsycInfo, and the Cochrane Database of Systematic Reviews were searched using a wide range of terms related to pain, Attention Deficit-Hyperactivity Disorder, childhood, adolescence, and young adulthood. Search terms were developed in consultation with an academic librarian. Mean sample ages up to 25 were included in the review because adult samples studying these research questions typically focus on ages 25–64 [41]. The search strategy is detailed in Supplementary Materials. The latest search occurred on 18 January 2022. Duplicates were deleted. Bibliographies of reviews identified during the initial search and articles included were searched for additional articles that met eligibility criteria.
2.1.1. Eligibility Criteria
Inclusion and exclusion criteria were determined by the study team based on the guiding research and an initial assessment of the existing literature. Abstracts of scholarly journal articles were reviewed according to the following inclusion criteria: (1) description of ADHD prevalence in a chronic pain sample, chronic pain prevalence in an ADHD sample, or an analysis of the association between ADHD and chronic pain, (2) mean sample age between 3 and 25 years at recruitment, and (3) observational study design. Studies were excluded if they met the following criteria: (1) pain due to a known disease process (e.g., cancer), (2) pain not characterized as chronic, (3) pain characterized as an adverse effect of psychostimulant medication, (4) ADHD was not defined or measured in the sample, (5) studies for which ADHD was an exclusion criteria, (6) studies of non-human animals, (7) studies in languages other than English or Swedish, (8) case-reports or small (n < 5) case series, and (9) studies on the association between headaches and ADHD were also excluded after recent systematic reviews on this topic were identified [35,36]. Chronic pain was defined as non-headache pain lasting >3 months through patient identification of chronic pain, or diagnosis of a chronic pain condition also met this criteria.
2.1.2. Study Selection
The search strategy yielded 1647 results, from which 45 duplicates were removed. No additional articles were identified through reference searching. 1170 articles were excluded after reading the publication title. 167 were removed during abstract review, with 53 undergoing full text review. Following full-text review, 11 articles were selected for inclusion in the review (see Figure 1).
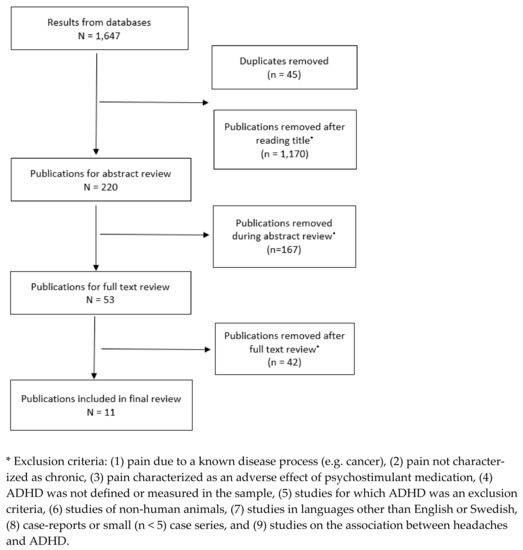
Figure 1.
Study Selection.
Review of all abstracts was performed by one author (PB), and a second author (EB) was consulted when it was not immediately clear whether an article met study criteria or was related to the research question. Full review of the remaining papers was performed by two authors (EB, PB). All disagreements were referred to a third author (AW).
2.2. Results
2.2.1. Characteristics of Included Studies
Table 1 describes the objectives, approach and key results of the 11 included studies. Publication dates were between 1993 and 2021. Study designs included cross-sectional studies, cohort studies, case-control studies and case series. Mean participant ages were 8–15 years, and studies originated from six different countries.

Table 1.
Overview of studies included in review.
2.2.2. ADHD Prevalence in Samples of Youth with Chronic Pain
Eight studies reported on the prevalence of ADHD in youth with chronic pain, with estimates ranging between 15 and 25%. Lipsker et al. [47] reported a prevalence of 19.9% (n = 126) using the Conners-3 parent report, and Low Kapalu et al. [48] found a prevalence of 18% (n = 94) based on a neuropsychological battery. Similar rates were found in smaller samples; Woodbury et al. [51] found a prevalence of 18% (n = 50) of children with functional abdominal pain using clinical interviews and the Conners-3 rating scale. Ghanizadeh et al. [45] used the semi-structured Schedule for Affective Disorders and Schizophrenia for School Age Children (K-SADS) and described a prevalence of ADHD in 15.6% (n = 45) of youth in a similar pain sample of functional abdominal pain compared to controls (0%; n = 45). Conversely, Galli et al. [44] did not find significantly higher rates of ADHD among youth with abdominal pain when compared with healthy controls. Of note, this study utilized only the CBCL checklist as a measure of ADHD, which is a less rigorous diagnostic mechanism than other studies (see Table 1). In a study of 17 female youth with Complex Regional Pain Syndrome (CRPS) by Cruz et al. [43], 23.5% had previously diagnosed ADHD, and neuropsychological testing revealed that 36% of the participants were at risk for poor attention and working memory deficits. However, only 11 participants completed the study tasks. A study of youth diagnosed with Developmental Coordination Disorder (DCD) found that children who met criteria for DCD and Ehlers–Danlos syndrome (Joint Hypermobility Syndrome; n = 19) were significantly more likely to meet criteria for ADHD than the youth in the DCD-only (n = 22) group (89% vs. 36%) [42]. Similarly, in a review of children with Ehlers–Danlos Syndrome/Joint Hypermobility Syndrome (n = 201), high rates of ADHD diagnoses based on chart reviews were identified in the sample, ranging from 11% to 46% (increasing with age) [46]. Compared to prevalence rates in large epidemiological studies [13,14], these studies show higher rates of ADHD among youth with chronic pain compared to the general population. Studies included in this review varied widely in the measurement approaches for assessing ADHD and chronic pain. For instance, ADHD diagnoses were determined through a variety of validated self- and proxy-report measures, ICD-code chart review, or comprehensive psychological evaluations. Similarly, the presence of chronic pain was identified through ICD-codes, questionnaires, or comprehensive medical evaluations (see Table 1).
2.2.3. Chronic Pain Prevalence in Samples of Youth with ADHD
Two studies identified in the current review that recruited from psychiatric samples described the prevalence of chronic pain in youth with ADHD. Mangerud et al. [49] reported that 65.9% (n = 216) of a sample of adolescents referred for ADHD (using ICD-10 codes) met chronic pain criteria (at least weekly pain lasting >3 months). In a second study, Asztely et al. [30] (n = 74) found that women who were recruited and diagnosed with ADHD between ages 3 and 18 years (using diagnostic semi-structured interviews) reported a high prevalence of chronic pain (>3 months of musculoskeletal pain, headaches or abdominal pain) in adulthood (M age = 27). Compared to prevalence rates in the general population in epidemiological research [13,14], these studies show higher rates of chronic pain than in individuals with ADHD, suggesting there may be higher pain prevalence in individuals with ADHD.
Asztély et al. also measured the effect of stimulants in their sample. They found lower rates of chronic pain among those treated with stimulants. However, the small sample size and lack of controls in the study design are limitations. Conversely, Wolff et al. [50] found that youth with ADHD had reduced pain perception. However, the effect disappeared if youth with ADHD were treated with stimulant medication. These studies offer very preliminary evidence that the use of stimulant medications may influence chronic pain experiences in youth with ADHD.
2.2.4. Additional Relevant Studies of Pain Symptomatology and ADHD That Did Not Meet Identified Criteria for Standard Definitions of Chronic Pain
In addition to the ADHD and chronic pain prevalence studies reviewed above, our review identified a number of studies that were of interest but did not meet the inclusion criteria for chronic pain as described above (e.g., did not specify pain duration >3 months). Significant associations have been found between ADHD and experiences of abdominal pain [52], physical complaints [53] and stomach aches [54]. However, a study with 474 children with ADHD seen at psychiatric clinics found that 29.1% reported clinically significant pain in the past month, but that the severity of ADHD symptoms was not associated with pain intensity [55].
Studies with case control designs and non-inclusionary pain presentations have mixed findings. Nationwide claims data in Germany [56] revealed that children with ADHD (n = 258,662) were more likely to be diagnosed with several somatic diseases compared to matched controls, including musculoskeletal system and connective tissue diagnoses (e.g., auto-inflammatory syndromes). Meanwhile, 165 children in Canada with ADHD reported bodily pain/discomfort that did not differ significantly from the standardized population mean [57]. Similarly, 76 youth with non-cardiac chest pain reported no difference of ADHD symptoms compared to controls [58].
Although these additional studies are heterogeneous and comparisons between them cannot easily be made, the overall findings are consistent with studies focused on ADHD and chronic pain that met our definition for inclusion, such as findings from Asztely et al.’s work. These findings suggest that ADHD is associated with a wide range of pain symptomatology.
3. Aim 2: Potential Associations between Chronic Pain and ADHD over Time
We suggest two potential co-occurring factors (cognitive–affective and motor regulation) that influence pain and ADHD over time. We also propose one potential underlying shared mechanism (neuroinflammation) that may influence the association between ADHD and chronic pain and comorbidity (See Figure 2).
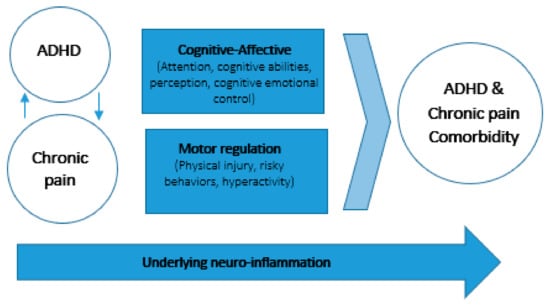
Figure 2.
Potential associations between chronic pain and ADHD over time.
3.1. Cognitive–Affective Models of Pain Highlight the Role of Attention
The relationship between cognitive function and the pain experience is important since attention appears to play a major role in pain processing. Cognitive-affective models of pain suggest that attentional processes are negatively impacted by pain and that pain might affect brain regions related to cognition [59,60]. Research across multiple chronic pain conditions in adults suggests that persistent pain might contribute to diminished cognitive abilities, which can change perceptive and interoceptive states and alter inhibition of top–down cognitive control of emotional states [59]. Research with youth demonstrate similar patterns, where impaired attention is demonstrated in a range of pediatric chronic pain conditions [61,62].
3.2. Motor Regulation, Injury and Pain
Motor regulation problems are common among youth with ADHD [63,64,65] and may increase risk for physical injury across the lifespan [66,67]. ADHD also appears to increase risk for motor regulation problems and pain experiences in adulthood [26,68]. Research suggests that the underlying mechanism for this pattern involves ADHD symptoms (specifically inattention, hyperactivity and impulsivity), the role of comorbid psychiatric disorders (e.g., conduct disorder, oppositional defiance disorder, depression), risky driving behaviors, and parental risk factors (permissive parenting style, parent diagnosis of ADHD) [67]. Similar motor problems have been observed in youth with juvenile fibromyalgia [69].
3.3. Neuroinflammation
Considerable evidence points to the central role of neuroinflammation in the pathophysiology of both chronic pain and ADHD. Its role in pain has been demonstrated primarily through mechanisms related to central sensitization, pro-inflammatory cytokines, and impairment to the dopaminergic system [70,71]. Research on ADHD points to neuroinflammatory mechanisms as risk factors for developing ADHD [72,73]. Central components of neuroinflammation relevant to ADHD include glial activation, increased oxidative stress and neurotransmitter metabolism [74]. Kerkes et al. [15] suggest that in individuals with ADHD, central neuroinflammation underlies altered pain perception and pain sensitization.
4. Discussion and Future Directions
This review sought to examine the potential association between ADHD and pediatric pain and provide a scoping review of the current literature. The findings from the scoping review reveal several important considerations. First, the quality of the studies in this review varied in regard to sample size, design (i.e., cross-sectional, case control), and measurement approaches for assessing pain and ADHD. Despite heterogeneity between studies, the majority of findings suggest there is an association between chronic pain and ADHD with comorbidity of both conditions significantly above average population prevalence. However, assessment of comorbid chronic non-headache pain in youth with ADHD has received little attention in the literature. Furthermore, limitations of this review ought to be noted, such as the inclusion bias for prevalence, as there might be unpublished work with null findings. Additionally, most samples in these studies are overwhelmingly white and from industrialized countries.
Secondly, despite the potential mechanisms for the association between chronic pain and ADHD, not many studies tested these theories. For example, comprehensive neuropsychological testing used in work by Low Kapalu et al. and Cruz et al. suggest that evidence of cognitive deficits can be found in a chronic pain population, but the methodology of the studies does not offer enough evidence to support the cognitive–affective model. Moreover, assessed stimulant use [30] reported cross-sectional data only, without controlled methods to assess the possible mechanisms of stimulant use effects on pain. However, Wolff et al. [50] did include control groups and suggest that ADHD reduces pain perception, leading to higher risk tolerance and higher risk behaviors. They posit that since the effect disappears for youth with ADHD on stimulant medication treatment, the mechanism is possibly attributable to differential dopamine release. Although the study utilized controls, it was not a randomized design. Furthermore, no studies were found that used objective measures (e.g., fMRI, biomarkers of inflammation) that could elucidate the hypothesis of central neuroinflammation.
Third, due to the lack of prospective, longitudinal and controlled research with large samples, the potential for ADHD as a potential risk factor for chronic pain over time is not well understood. The majority of the studies rely on retrospective or cross-sectional reports where temporal inferences cannot be made. Moreover, sex differences among youth with chronic pain and ADHD have not been addressed. While females are at higher risk for chronic pain, and males are at higher risk for ADHD, the sex differences for both are complicated and not yet well understood [75,76,77]. It is crucial to investigate how sex differences as differential risk/protective factors might intersect with the relationship between chronic pain and ADHD.
Based on the findings in this review, we propose several considerations for next steps and future research. We suggest future work implements research designs that carefully assess for ADHD diagnoses and chronic pain onset and uses matched controls. These designs need robust and well-established diagnostic criteria for chronic pain and ADHD. Furthermore, for a more robust assessment of chronic pain and its effects, it would be important to look at pain-related impairment as well. Other psychiatric comorbidities (e.g., depression, anxiety) that affect chronic pain should be integrated to the model assessing for the interactions of ADHD and chronic pain. As previous research has shown, interaction effects of psychiatric comorbidities are present in both chronic pain and ADHD research [8,17]. Moreover, it is essential to examine whether the models proposed in this review are generalizable across chronic pain conditions or if specific chronic pain conditions need to include specific mechanisms. For example, a recent model by Baeza-Velasco [78] offers a framework for several neurodevelopmental disorders and joint hypermobility, hypermobility spectrum disorders, and Ehlers–Danlos syndromes. It highlights hypo- and hyperactivity symptoms and how they might play a role in these chronic pain conditions. It is unknown if this conceptualization is relevant to other chronic pain experiences. Therefore, more research is needed to determine if there are differential effects in associations of ADHD symptoms and chronic pain. Finally, future research could aid in screening youth and identifying screening approaches if ADHD is found to increase risk for chronic pain. Findings can lead to the development of early intervention for both ADHD and pain.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children10010142/s1.
Author Contributions
Conceptualization, E.A.J.B., P.C.M.B., A.L.H. and A.C.W.; methodology, P.C.M.B.; formal analysis, P.C.M.B. and E.A.J.B.; writing—original draft, E.A.J.B. and P.C.M.B.; writing—review and editing, E.A.J.B., P.C.M.B., A.L.H. and A.C.W.; supervision, A.C.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
The data presented in this manuscript can be provided by the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986, 3, S1.
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; Macdonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Groenewald, C.B.; Wright, D.R.; Palermo, T.M. Health care expenditures associated with pediatric pain-related conditions in the United States. Pain 2015, 156, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.S. RELIEVING PAIN IN AMERICA: A BLUEPRINT FOR TRANSFORMING PREVENTION, CARE, EDUCATION, AND RESEARCH. J. Pain Palliat. Care Pharmacother. 2012, 26, 197–198. [Google Scholar] [CrossRef]
- Holley, A.L.; Wilson, A.C.; Cho, E.; Palermo, T.M. Clinical Phenotyping of Youth With New-Onset Musculoskeletal Pain. Clin. J. Pain 2017, 33, 28–36. [Google Scholar] [CrossRef]
- Becker, A.J.; Heathcote, L.C.; Timmers, I.; Simons, L.E. Precipitating events in child and adolescent chronic musculoskeletal pain. Pain Rep. 2018, 3, e665. [Google Scholar] [CrossRef]
- Murray, C.B.; Groenewald, C.B.; de la Vega, R.; Palermo, T.M. Long-term impact of adolescent chronic pain on young adult educational, vocational, and social outcomes. Pain 2020, 161, 439–445. [Google Scholar] [CrossRef]
- Forgeron, P.A.; King, S.; Stinson, J.N.; McGrath, P.J.; Macdonald, A.J.; Chambers, C.T. Social Functioning and Peer Relationships in Children and Adolescents with Chronic Pain: A Systematic Review. Pain Res. Manag. 2010, 15, 27–41. [Google Scholar] [CrossRef]
- Cordts, K.P.; Stone, A.L.; Beveridge, J.K.; Wilson, A.C.; Noel, M. The (Parental) Whole Is Greater Than the Sum of Its Parts: A Multifactorial Model of Parent Factors in Pediatric Chronic Pain. J. Pain 2019, 20, 786–795. [Google Scholar] [CrossRef]
- Holley, A.L.; Wilson, A.C.; Palermo, T.M. Predictors of the transition from acute to persistent musculoskeletal pain in children and adolescents: A prospective study. Pain 2017, 158, 794–801. [Google Scholar] [CrossRef]
- Holley, A.; Wilson, A.; Noel, M.; Palermo, T. Post-traumatic stress symptoms in children and adolescents with chronic pain: A topical review of the literature and a proposed framework for future research. Eur. J. Pain 2016, 20, 1371–1383. [Google Scholar] [CrossRef]
- The American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5TM, 5th ed.; The American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Erskine, H.E.; Ferrari, A.; Nelson, P.; Polanczyk, G.V.; Flaxman, A.D.; Vos, T.; Whiteford, H.; Scott, J. Research Review: Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study. J. Child Psychol. Psychiatry 2013, 54, 1263–1274. [Google Scholar] [CrossRef]
- Polanczyk, G.V.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef]
- Kerekes, N.; Sanchéz-Pérez, A.M.; Landry, M. Neuroinflammation as a possible link between attention-deficit/hyperactivity disorder (ADHD) and pain. Med. Hypotheses 2021, 157, 110717. [Google Scholar] [CrossRef]
- Nigg, J.T. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin. Psychol. Rev. 2013, 33, 215–228. [Google Scholar] [CrossRef]
- O’Neill, S.; Rajendran, K.; Mahbubani, S.M.; Halperin, J.M. Preschool Predictors of ADHD Symptoms and Impairment During Childhood and Adolescence. Curr. Psychiatry Rep. 2017, 19, 95. [Google Scholar] [CrossRef]
- Merrill, B.M.; Molina, B.S.G.; Coxe, S.; Gnagy, E.M.; Altszuler, A.R.; Macphee, F.L.; Morrow, A.S.; Trucco, E.M.; Pelham, W.E. Functional Outcomes of Young Adults with Childhood ADHD: A Latent Profile Analysis. J. Clin. Child Adolesc. Psychol. 2020, 49, 215–228. [Google Scholar] [CrossRef]
- Asherson, P.; Akehurst, R.; Kooij, J.J.S.; Huss, M.; Beusterien, K.; Sasané, R.; Gholizadeh, S.; Hodgkins, P. Under Diagnosis of Adult ADHD. J. Atten. Disord. 2012, 16, 20S–38S. [Google Scholar] [CrossRef]
- Doshi, J.A.; Hodgkins, P.; Kahle, J.; Sikirica, V.; Cangelosi, M.J.; Setyawan, J.; Erder, M.H.; Neumann, P.J. Economic Impact of Childhood and Adult Attention-Deficit/Hyperactivity Disorder in the United States. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 990–1002. [Google Scholar] [CrossRef]
- Soltani, S.; Kopala-Sibley, D.C.; Noel, M. The Co-occurrence of Pediatric Chronic Pain and Depression: A Narrative Review and Conceptualization of Mutual Maintenance. Clin. J. Pain 2019, 35, 633–643. [Google Scholar] [CrossRef]
- Jastrowski Mano, K.E.; O’Bryan, E.M.; Gibler, R.C.; Beckmann, E. The Co-occurrence of Pediatric Chronic Pain and Anxiety: A Theoretical Review of a Developmentally Informed Shared Vulnerability Model. Clin. J. Pain 2019, 35, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Vinall, J.; Pavlova, M.; Asmundson, G.J.G.; Rasic, N.; Noel, M. Mental Health Comorbidities in Pediatric Chronic Pain: A Narrative Review of Epidemiology, Models, Neurobiological Mechanisms and Treatment. Children 2016, 3, 40. [Google Scholar] [CrossRef] [PubMed]
- McKillop, H.N.; Banez, G.A. A Broad Consideration of Risk Factors in Pediatric Chronic Pain: Where to Go from Here? Children 2016, 3, 38. [Google Scholar] [CrossRef] [PubMed]
- Instanes, J.T.; Klungsøyr, K.; Halmøy, A.; Fasmer, O.B.; Haavik, J. Adult ADHD and Comorbid Somatic Disease: A Systematic Literature Review. J. Atten. Disord. 2016, 22, 203–228. [Google Scholar] [CrossRef] [PubMed]
- Stray, L.L.; Kristensen, Ø.; Lomeland, M.; Skorstad, M.; Stray, T.; Tønnessen, F.E. Motor regulation problems and pain in adults diagnosed with ADHD. Behav. Brain Funct. 2013, 9, 18. [Google Scholar] [CrossRef]
- Lensing, M.B.; Zeiner, P.; Sandvik, L.; Opjordsmoen, S. Quality of Life in Adults Aged 50+ With ADHD. J. Atten. Disord. 2015, 19, 405–413. [Google Scholar] [CrossRef]
- Stickley, A.; Koyanagi, A.; Takahashi, H.; Kamio, Y. ADHD symptoms and pain among adults in England. Psychiatry Res. 2016, 246, 326–331. [Google Scholar] [CrossRef]
- Stickley, A.; Koyanagi, A.; Takahashi, H.; Ruchkin, V.; Inoue, Y.; Kamio, Y. Attention-deficit/hyperactivity disorder and physical multimorbidity: A population-based study. Eur. Psychiatry 2017, 45, 227–234. [Google Scholar] [CrossRef]
- Asztély, K.; Kopp, S.; Gillberg, C.; Waern, M.; Bergman, S. Chronic Pain And Health-Related Quality Of Life In Women With Autism And/Or ADHD: A Prospective Longitudinal Study. J. Pain Res. 2019, 12, 2925–2932. [Google Scholar] [CrossRef]
- Reyero, F.; Ponce, G.; Rodriguez-Jimenez, R.; Fernandez-Dapica, P.; Taboada, D.; Martin, V.; Navio, M.; Jiménez-Arriero, M.; Hoenicka, J.; Palomo, T. High frequency of childhood ADHD history in women with fibromyalgia. Eur. Psychiatry 2010, 26, 482–483. [Google Scholar] [CrossRef]
- Karaş, H.; Çetingök, H.; İlişer, R.; Çarpar, E.; Kaşer, M. Childhood and adult attention deficit hyperactivity disorder symptoms in fibromyalgia: Associations with depression, anxiety and disease impact. Int. J. Psychiatry Clin. Pract. 2020, 24, 257–263. [Google Scholar] [CrossRef]
- Moore, D.J.; Meints, S.M.; Lazaridou, A.; Johnson, D.; Franceschelli, O.; Cornelius, M.; Schreiber, K.; Edwards, R.R. The Effect of Induced and Chronic Pain on Attention. J. Pain 2019, 20, 1353–1361. [Google Scholar] [CrossRef]
- Petanidou, D.; Giannakopoulos, G.; Tzavara, C.; Dimitrakaki, C.; Kolaitis, G.; Tountas, Y. Adolescents’ multiple, recurrent subjective health complaints: Investigating associations with emotional/behavioural difficulties in a cross-sectional, school-based study. Child Adolesc. Psychiatry Ment. Health 2014, 8, 3. [Google Scholar] [CrossRef]
- Salem, H.; Vivas, D.; Cao, F.; Kazimi, I.F.; Teixeira, A.L.; Zeni, C.P. ADHD is associated with migraine: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2017, 27, 267–277. [Google Scholar] [CrossRef]
- Jacobs, H.; Singhi, S.; Gladstein, J. Medical Comorbidities in Pediatric Headache. Semin. Pediatr. Neurol. 2016, 23, 60–67. [Google Scholar] [CrossRef]
- Shimizu, V.T.; Bueno, O.F.A.; Miranda, M.C. Sensory processing abilities of children with ADHD. Braz. J. Phys. Ther. 2014, 18, 343–352. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Calkins, M.E.; Burstein, M.; He, J.-P.; Chiavacci, R.; Lateef, T.; Ruparel, K.; Gur, R.C.; Lehner, T.; Hakonarson, H.; et al. Comorbidity of Physical and Mental Disorders in the Neurodevelopmental Genomics Cohort Study. Pediatrics 2015, 135, e927–e938. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Évid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child. Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef]
- Celletti, C.; Mari, G.; Ghibellini, G.; Celli, M.; Castori, M.; Camerota, F. Phenotypic variability in developmental coordination disorder:Clustering of generalized joint hypermobility with attention deficit/hyperactivity disorder, atypical swallowing and narrative difficulties. Am. J. Med. Genet. C Semin. Med. Genet. 2015, 169, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Cruz, N.; O’Reilly, J.; Slomine, B.S.; Salorio, C.F. Emotional and Neuropsychological Profiles of Children With Complex Regional Pain Syndrome Type-I in an Inpatient Rehabilitation Setting. Clin. J. Pain 2011, 27, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Galli, F.; D’Antuono, G.; Tarantino, S.; Viviano, F.; Borrelli, O.; Chirumbolo, A.; Cucchiara, S.; Guidetti, V. Headache and Recurrent Abdominal Pain: A Controlled Study by the Means Of The Child Behaviour Checklist (CBCL). Cephalalgia 2007, 27, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh, A.; Moaiedy, F.; Imanieh, M.H.; Askani, H.; Haghighat, M.; Dehbozorgi, G.; Dehghani, S.M. Psychiatric disorders and family functioning in children and adolescents with functional abdominal pain syndrome. J. Gastroenterol. Hepatol. 2008, 23, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Kindgren, E.; Perez, A.Q.; Knez, R. Prevalence of ADHD and Autism Spectrum Disorder in Children with Hypermobility Spectrum Disorders or Hypermobile Ehlers-Danlos Syndrome: A Retrospective Study. Neuropsychiatr. Dis. Treat. 2021, 17, 379–388. [Google Scholar] [CrossRef]
- Lipsker, C.W.; Bölte, S.; Hirvikoski, T.; Lekander, M.; Holmström, L.; Wicksell, R.K. Prevalence of autism traits and attention-deficit hyperactivity disorder symptoms in a clinical sample of children and adolescents with chronic pain. J. Pain Res. 2018, 11, 2827–2836. [Google Scholar] [CrossRef]
- Kapalu, C.M.L.; Hall, J.J.; Wallace, D.P. Neuropsychological Functioning of Youth Receiving Intensive Interdisciplinary Pain Treatment. J. Pediatr. Psychol. 2018, 43, 870–881. [Google Scholar] [CrossRef]
- Mangerud, W.L.; Bjerkeset, O.; Lydersen, S.; Indredavik, M.S. Chronic pain and pain-related disability across psychiatric disorders in a clinical adolescent sample. BMC Psychiatry 2013, 13, 272. [Google Scholar] [CrossRef]
- Wolff, N.; Rubia, K.; Knopf, H.; Hölling, H.; Martini, J.; Ehrlich, S.; Roessner, V. Reduced pain perception in children and adolescents with ADHD is normalized by methylphenidate. Child Adolesc. Psychiatry Ment. Health 2016, 10, 24. [Google Scholar] [CrossRef]
- Woodbury, M.M. Recurrent Abdominal Pain in Child Patients Seen at a Pediatric Gastroenterology Clinic: Observations of 50 Children and Their Families. Psychosomatics 1993, 34, 485–493. [Google Scholar] [CrossRef]
- Holmberg, K.; Hjern, A. Health complaints in children with attention-deficit/hyperactivity disorder. Acta Paediatr. 2006, 95, 664–670. [Google Scholar] [CrossRef]
- Kaplan, B.J.; McNICOL, J.; Conte, R.A.; Moghadam, H.K. Physical Signs and Symptoms in Preschool-Age Hyperactive and Normal Children. J. Dev. Behav. Pediatr. 1987, 8, 305–310. [Google Scholar] [CrossRef]
- Egger, H.L.; Costello, E.J.; Erkanli, A.; Angold, A. Somatic Complaints and Psychopathology in Children and Adolescents: Stomach Aches, Musculoskeletal Pains, and Headaches. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 852–860. [Google Scholar] [CrossRef]
- Yeh, Y.-C.; Huang, M.-F.; Wu, Y.-Y.; Hu, H.-F.; Yen, C.-F. Pain, Bullying Involvement, and Mental Health Problems Among Children and Adolescents With ADHD in Taiwan. J. Atten. Disord. 2019, 23, 809–816. [Google Scholar] [CrossRef]
- Akmatov, M.K.; Ermakova, T.; Bätzing, J. Psychiatric and Nonpsychiatric Comorbidities Among Children With ADHD: An Exploratory Analysis of Nationwide Claims Data in Germany. J. Atten. Disord. 2021, 25, 874–884. [Google Scholar] [CrossRef]
- Klassen, A.F.; Miller, A.; Fine, S. Health-Related Quality of Life in Children and Adolescents Who Have a Diagnosis of Attention-Deficit/Hyperactivity Disorder. Pediatrics 2004, 114, e541–e547. [Google Scholar] [CrossRef]
- Kenar, A.; Örün, U.A.; Yoldaş, T.; Kayalı, Ş.; Bodur, Ş.; Karademir, S. Anxiety, depression, and behavioural rating scales in children with non-cardiac chest pain. Cardiol. Young 2019, 29, 1268–1271. [Google Scholar] [CrossRef]
- Simons, L.E.; Elman, I.; Borsook, D. Psychological processing in chronic pain: A neural systems approach. Neurosci. Biobehav. Rev. 2014, 39, 61–78. [Google Scholar] [CrossRef]
- Eccleston, C.; Crombez, G. Pain demands attention: A cognitive–affective model of the interruptive function of pain. Psychol. Bull. 1999, 125, 356–366. [Google Scholar] [CrossRef]
- Ho, G.H.Y.; Bennett, S.M.; Cox, D.; Poole, G. Brief Report: Cognitive Functioning and Academic Achievement in Children and Adolescents with Chronic Pain. J. Pediatr. Psychol. 2009, 34, 311–316. [Google Scholar] [CrossRef]
- Beckmann, E.; Jastrowski Mano, K.E. Advancing the Measurement of Executive Functioning in Pediatric Chronic Pain. Children 2021, 8, 630. [Google Scholar] [CrossRef] [PubMed]
- Demers, M.M.; McNevin, N.; Azar, N.R. ADHD and Motor Control: A Review of the Motor Control Deficiencies Associated With Attention Deficit/Hyperactivity Disorder and Current Treatment Options. Crit. Rev. Phys. Rehabilit. Med. 2013, 25, 231–239. [Google Scholar] [CrossRef]
- Fliers, E.A.; Franke, B.; Lambregts-Rommelse, N.N.; Altink, M.E.; Buschgens, C.J.; der Sanden, M.W.N.-V.; Sergeant, J.A.; Faraone, S.V.; Buitelaar, J.K. Undertreatment of Motor Problems in Children with ADHD. Child Adolesc. Ment. Health 2010, 15, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Neto, F.R.; Goulardins, J.B.; Rigoli, D.; Piek, J.P.; de Oliveira, J.A. Motor development of children with attention deficit hyperactivity disorder. Rev. Bras. de Psiquiatr. 2015, 37, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Allan, C.C.; DeShazer, M.; Staggs, V.S.; Nadler, C.; Crawford, T.P.; Moody, S.; Chacko, A. Accidental Injuries in Preschoolers: Are We Missing an Opportunity for Early Assessment and Intervention? J. Pediatr. Psychol. 2021, 46, 835–843. [Google Scholar] [CrossRef]
- Brunkhorst-Kanaan, N.; Libutzki, B.; Reif, A.; Larsson, H.; McNeill, R.V.; Kittel-Schneider, S. ADHD and accidents over the life span–A systematic review. Neurosci. Biobehav. Rev. 2021, 125, 582–591. [Google Scholar] [CrossRef]
- Dahan, A.; Ryder, C.H.; Reiner, M. Components of Motor Deficiencies in ADHD and Possible Interventions. Neuroscience 2016, 378, 34–53. [Google Scholar] [CrossRef]
- Sil, S.; Thomas, S.; DiCesare, C.; Strotman, D.; Ting, T.V.; Myer, G.; Kashikar-Zuck, S. Preliminary Evidence of Altered Biomechanics in Adolescents With Juvenile Fibromyalgia. Arthritis Care Res. 2015, 67, 102–111. [Google Scholar] [CrossRef]
- Matsuda, M.; Huh, Y.; Ji, R.-R. Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. J. Anesthesia 2018, 33, 131–139. [Google Scholar] [CrossRef]
- Ji, R.-R.; Nackley, A.; Huh, B.Y.; Terrando, N.; Maixner, D.W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018, 129, 343–366. [Google Scholar] [CrossRef]
- Dunn, G.A.; Nigg, J.T.; Sullivan, E.L. Neuroinflammation as a risk factor for attention deficit hyperactivity disorder. Pharmacol. Biochem. Behav. 2019, 182, 22–34. [Google Scholar] [CrossRef]
- Gustafsson, H.C.; Sullivan, E.L.; Battison, E.A.; Holton, K.F.; Graham, A.M.; Karalunas, S.L.; Fair, D.A.; Loftis, J.M.; Nigg, J.T. Evaluation of maternal inflammation as a marker of future offspring ADHD symptoms: A prospective investigation. Brain Behav. Immun. 2020, 89, 350–356. [Google Scholar] [CrossRef]
- Leffa, D.T.; Torres, I.L.; Rohde, L.A. A Review on the Role of Inflammation in Attention-Deficit/Hyperactivity Disorder. Neuroimmunomodulation 2019, 25, 328–333. [Google Scholar] [CrossRef]
- Boerner, K.; Eccleston, C.; Chambers, C.; Keogh, E. Sex differences in the efficacy of psychological therapies for the management of chronic and recurrent pain in children and adolescents: A systematic review and meta-analysis. Pain 2017, 158, 569–582. [Google Scholar] [CrossRef]
- May, T.; Adesina, I.; McGillivray, J.; Rinehart, N.J. Sex differences in neurodevelopmental disorders. Curr. Opin. Neurol. 2019, 32, 622–626. [Google Scholar] [CrossRef]
- Carbonneau, M.L.; Demers, M.; Bigras, M.; Guay, M.-C. Meta-Analysis of Sex Differences in ADHD Symptoms and Associated Cognitive Deficits. J. Atten. Disord. 2021, 25, 1640–1656. [Google Scholar] [CrossRef]
- Baeza-Velasco, C. Neurodevelopmental atypisms in the context of joint hypermobility, hypermobility spectrum disorders, and Ehlers–Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2021, 187, 491–499. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).