Abstract
Background: Neoplasms in the head and neck region possess higher glycolytic activity than normal tissue, showing increased glucose metabolism. F-18-Flourodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) can identify an unknown primary tumor (CUP). Aim: The aim of this study was to assess the real-life performance of F-18-FDG-PET/CT in detecting primary sites in patients with cervical lymph node metastasis of CUP. Methods: A retrospective data analysis of 31 patients who received FDG-PET/CT between June 2009 and March 2015 in a CUP context with histologically confirmed cervical lymph node metastasis was included. Results: In 48% of the patients (15/31), PET/CT showed suspicious tracer accumulation. In 52% of the patients (16/31), there was no suspicious radiotracer uptake, which was confirmed by the lack of identification of any primary tumor in 10 cases until the end of follow-up. FDG-PET/CT had a sensitivity of 67%, specificity of 91%, PPV of 92%, and NPV of 63% in detecting the primary tumor. Additionally, PET/CT showed suspicious tracer accumulation according to further metastasis in 32% of the patients (10/31). Conclusion: FDG-PET/CT imaging is a useful technique for primary tumor detection in patients in a cervical CUP context. Furthermore, it provides information on the ulterior metastasis of the disease.
1. Introduction
Most patients with cervical lymph node metastases suffer from a primary tumor in the region of the head and neck, although it is clinically non-detectable in some of these patients. These cases are referred to as carcinoma of unknown primary (CUP). The criteria for CUP syndrome are met when a histologically or cytologically confirmed malignancy is present without a demonstrable primary tumor after the completion of the primary diagnostic workup [1]. “Cervical CUP” is a relatively rare condition, representing between 2 and 9% of all cancers diagnosed in the head and neck, depending on the literature, and 70–90% of these patients are male [2]. The detection of the primary tumor in a CUP setting has extensive consequences for a patient’s therapy and prognosis [3]. In the diagnostic setting, conventional imaging consisting of magnetic resonance imaging (MRI) and computed tomography (CT) can be performed, as well as panendoscopy and functional imaging. The value of F-18-Flourdesoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) in the detection of the primary tumor in a cervical CUP setting is a subject of controversy in the literature. Some studies have demonstrated, in comparably sized patient samples, the performance of F-18-FDG-PET/CT for primary tumor detection in patients with CUP syndrome with cervical lymph node metastases. F-18-FDG-PET/CT can be used to identify an unknown primary tumor, since many neoplasms, including those in the head and neck region, possess high glycolytic activity and therefore demonstrate a high uptake of FDG. In view of the limited data available, the aim of our study is to demonstrate the value of F-18-FDG-PET/CT for primary tumor detection and the value of the additional information obtained in the real-life setting.
2. Materials and Methods
2.1. Patients
We retrospectively evaluated F-18-FDG-PET/CTs performed in the Department of Nuclear Medicine at University Hospital Marburg between June 2009 and March 2015 in a CUP context with histologically confirmed cervical lymph node metastasis (CLNM). Patients with lymphoma or previous carcinoma in the head and neck region that could be clearly related to cervical lymph node metastasis were excluded from this study. The study included 31 patients (Table 1).

Table 1.
Study collective, patient demographics, and diagnostics.
In 25 patients (81%), the sampling date of the CLNM was known; in 16 patients (52%), the lymph node was removed by extirpation; a fine needle aspiration (FNP) was performed in six patients (19%); and a stamping biopsy was performed in three patients (10%). In six patients (19%), the sampling date could not be determined, and the examination was performed at the referring institution. At the point of time of PET/CT performance, the histopathological examination yielded, in 20 patients (65%), the unequivocal result of a metastasis of a squamous cell carcinoma (SCC); in eight patients (26%), it yielded a metastasis of an undifferentiated or not further characterized carcinoma. In one patient each, a metastasis of a malignant melanoma, a small-cell poorly differentiated carcinoma, and an adenocell carcinoma were diagnosed at this time.
All diagnostic procedures performed for the detection of the primary tumor or for the staging of the tumor disease between the diagnosis of CLNM and the F-18-FDG-PET/CT examination were recorded in this study. Nineteen of the thirty-one patients (61%) received a diagnostic evaluation to detect the primary tumor prior to PET/CT examination. In 48% of the patients (15/31), at least one “main diagnostic measure” (and possibly a minor diagnostic test) was performed for primary tumor detection or tumor staging prior to PET/CT examination. This included the following diagnostics: an MRI of the neck and a CT of the thorax and neck.
In 13% of the patients (4/31), only a “minor diagnostic test” had been performed prior to the PET/CT examination. These included the following examinations:
Panendoscopy, abdominal diagnostics (abdominal sonography, abdominal CT, diagnostic gastroscopy/colonoscopy), an X-ray of the thorax, MRI cranium, dermatological consultation, bronchoscopy, and CT cranium.
In 29% of the patients (9/31), the F-18-FDG-PET/CT examination was the first further diagnostic examination after a physical examination, ENT examination, and ultrasonography of the neck. In 10% of the patients (3/31), no statement could be obtained about which diagnostic procedure was performed because the diagnosis of CLNM was performed in a different hospital, and the patients were referred to the University Hospital Marburg for further treatment.
In 20 patients (65%), the PET/CT examination was performed within one month after the diagnosis of CLNM. Three patients (10%) received the PET/CT scan within one year of the diagnosis of CLNM. Two patients (6%) had longer intervals between the diagnosis of CLNM and PET/CT examination. In the remaining six patients (19%), precise information on the time interval could not be retrieved because the date of CLNM sample collection was unknown. The median time between diagnosis of CLNM and PET/CT examination was eight days (range: 1–3490 days).
Four of the patients (13%) received radiotherapy and chemotherapy before PET/CT examination. One patient (3%) received radiotherapy only. The remaining 26 patients (84%) did not receive any therapy before PET/CT examination.
Furthermore, 29/31 patients received panendoscopy: 1 ahead of F-18-FDG-PET/CT and 28 after PET/CT for diagnosis confirmation. We define panendoscopy according to the CUP scheme as microlaryngoscopy, esophagoscopy, tracheobronchoscopy, and epi- and oropharyngoscopy, with the collection of samples from the base of the tongue, epipharynx, and bilateral tonsillectomy. Panendoscopy according to the CUP scheme was performed on nine patients and revealed a tumor diagnosis in seven of these patients. In 16 patients, the collection of samples was not performed in concordance with the CUP scheme, but samples were also taken. In 11 of these patients, morphological abnormalities were found and biopsied, revealing the primary tumor in seven cases. In six patients, no samples were taken from the ENT area, although four of these patients received panendocsopy.
The patients were followed until June 2015, specifically to determine the courses of disease in patients without suspicious findings in the PET/CT. The average follow-up period (after PET/CT examination) of the patients was 1.9 years, and the median was 1.28 years (range: 0.04–5.39 years). Ten patients with a true negative PET/CT scan had an average follow-up period of 2.8 years, and the median was 2.9 years (range: 0.11–5.39 years).
The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were computed with their corresponding Agresti–Coull 95% confidence intervals using SPSS Statistics 28.0 (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY, USA: IBM Corp).
2.2. Investigation Protocol
All the investigations were performed according to the guidelines of the German Association of Nuclear Medicine. A median F-18-FDG activity value of 218 MBq (range: 187–265 MBq) was applied. In 23 PET/CT examinations (74%), an iodine-containing contrast medium was additionally used, while 8 examinations (26%) were performed without it due to various contraindications (e.g., known allergy).
2.3. Analysis
Two independent, board-certified nuclear medicine physicians evaluated all of the PET/CT scans. If there was no consensus, a third experienced nuclear physician was involved in the evaluation. Finally, any result that was approved by two nuclear physicians was included. The physicians had no information about the evaluation of the other diagnosticians, the primary tumor position, or the outcome of the patient.
The study was approved by the Ethics Committee of Marburg University Hospital (Az.: RS 22/12).
3. Results
3.1. Primary Tumor Lesion
In total, 18 patients (18/31; 58%) were found to have a localized primary tumor during the course of their medical history (Figure 1 and Figure 2).
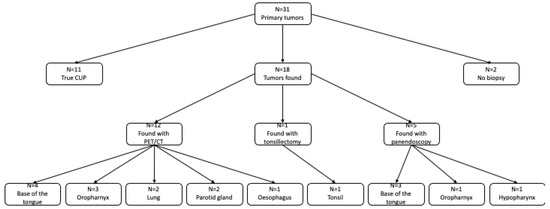
Figure 1.
Patient collective.
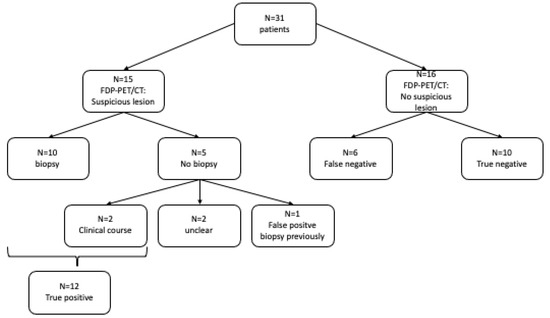
Figure 2.
Primary tumor.
The most frequent primary tumor location was the oropharynx. A total of twelve primary tumors (12/18; 67%) were located in the oropharyngeal region. Of these, seven (7/18; 39%) were assigned to the base of the tongue and one (1/18; 6%) to the tonsils. In the remaining four patients (4/18; 22%) with a primary tumor in the oropharynx, the exact location was not documented.
Three primary tumors (3/18; 17%) were found outside the oropharynx but in the ENT region. Of these, two tumors (2/18; 11%) were detected in the parotid region and one (1/18; 6%) in the hypopharyngeal region. The TN and HPV status of the histologically confirmed tumors of the ENT area at initial diagnosis are given in Table 2.

Table 2.
T and N and HPV status of histologically proven ENT tumors.
In addition, three primary tumors (3/18; 17%) were detected outside the head and neck region: two in the lungs and one in the esophagus.
Of the 18 primary tumors found, 12 (12/18; 67%) were detected by a PET/CT scan, 5 (5/18; 28%) by panendoscopy following a PET/CT scan, and 1 primary tumor (1/18; 6%) by tonsillectomy.
In two patients (2/31; 6%), the area of FDG uptake in the PET/CT scan was not biopsied after the examination; no definitive statement about the final primary tumor location can be established for these patients.
In 11 patients (11/31; 35%), no primary tumor could be found in the course of the patient history; thus, these patients were considered to suffer from a “true” CUP syndrome; 10/11 had a true negative PET/CT, while 1 patient had a false positive scan.
In 48% of patients (15/31), the PET/CT scan showed a suspicious lesion; a subsequent biopsy was performed in ten patients. In all biopsy samples, malignant cells indicative of a primary tumor were found.
Of the five patients who did not undergo biopsy, in two cases, the primary tumor in the area identified by PET/CT was confirmed clinically in the further course of the disease. In two other patients, the location remained unclear because the area of FDG accumulation was not biopsied; these were not considered in the evaluation (the determination of the detection quality of the PET/CT examination related to the primary tumor position). The fifth patient was the only one in this study who showed a false positive result in the PET/CT scan. Retrospectively, the suspected tumor lesion was related to a previously performed panendoscopy with biopsy and was then misinterpreted as the primary tumor.
In 52% of the patients (16/31), there was no suspicious tracer accumulation. This diagnosis was confirmed in ten cases by the end of the follow-up. In six patients, a primary tumor was found despite a negative PET/CT scan.
This results in a sensitivity of 67% (95% confidence interval 43.6–83.9%), specificity of 91%, (95% confidence interval 60.1–100%), a positive predictive value (PPV) of 92% (95% confidence interval 64.6–100%), and a negative predictive value (NPV) of 63% (95% confidence interval 38.5–81.6%), as well as an accuracy of 79% for the F-18-FDG-PET/CT (Table 3).

Table 3.
PET/CT with regard to previous diagnostic and therapy.
3.2. Prior Diagnostics
In 15 patients (48%) and in 16 foci (52%), suspicion regarding the primary tumor position was raised during the course of diagnostics prior to PET/CT examination. In three patients, the suspicion could be refuted in the course of diagnostics before PET/CT examination by the resection of the lesion. In seven patients, the initial suspicion could be refuted with the help of the PET/CT examination. In three patients, the primary tumor was confirmed by the PET/CT examination at the assumed position by other diagnostic procedures and was confirmed in the course of further medical history.
In two patients, a probable primary tumor position was mentioned in a previously performed diagnostic test that was not detected in the PET/CT scan. The suspicion of pre-diagnosis was confirmed in these two patients during the course of the medical history; thus, these PET/CT scans were evaluated as false negatives.
In one patient, the primary tumor was not found, and the FDG-positive lesion was not biopsied, meaning that a conclusive result regarding the probable primary tumor position prior to PET/CT cannot be obtained.
3.3. Distant Metastasis
Altogether, PET/CT examination raised suspicion of distant metastasis in 32% of patients (10/31). Seven (7/31; 23%) of these ten patients had findings that were not previously known; in five (5/31; 16%) of these, seven distant metastases were confirmed histologically or clinically.
3.4. Secondary Carcinoma
In 26% (8/31) of the patients, a secondary carcinoma was diagnosed in addition to the CUP in the course of the patient’s history. In one patient, the diagnosis of a secondary carcinoma was firstly indicated by PET/CT examination.
3.5. Summary
Regarding all the information obtained by PET/CT, it provided additional information in 24/31 (77%) patients: in 12 patients (12/31, 39%), the primary tumor was found; in 5 patients (16%), a previously unknown metastasis was detected; 1 patient (3%) was diagnosed with a secondary carcinoma; 10 patients (32%) had a true negative result (diagnosis of CUP syndrome); and 7 patients (23%) showed a suspected primary tumor position from a previously refuted diagnosis (Table 4).

Table 4.
Information obtained by F-18-FDG-PET/CT.
4. Discussion
The aim of the present study was to analyze the diagnostic value and the real-life performance of FDG-PET/CT in the setting of CUP with cervical lymph node metastasis. Our results show the high impact that PET/CT can have on patients with cervical CUP, due to the possible detection of the primary tumor, metastasis, and/or second malignancies.
There is remarkable heterogeneity (Table 5) in the data of previously published studies [4,5,6,7,8,9]. Comparing our results with these other studies is challenging due to the differences in the extent of diagnostics used prior to PET/CT. A possible explanation for the differing results could be the relatively small patient collectives investigated (range: n = 18–n = 78), the variable definitions of CUP disease, the different follow-up periods, and a non-uniform understanding of a true-negative PET/CT scan. Nevertheless, the results of the present study align well with those of other publications. Furthermore, the examined collective of patients is similar to the groups of patients examined in the literature, as 84% of the presented patient population were male, 87% between 50 and 80 years of age, and also squamous cell carcinoma was the most common diagnosis (70%) after histopathological lymph node examination. Similarly, cervical lymph node level II was the most commonly reported affected cervical lymph level both in this study and in the literature [10].

Table 5.
Overview of various studies.
A meta-analysis reported the detection of 74 primary tumors in 302 patients with CUP and CLNM using FDG-PET, resulting in a sensitivity of 88.3%, specificity of 74.9%, and accuracy of 78.8% [11]. Nikolova et al. reported a sensitivity of 70% and specificity of 84% for primary tumor detection in patients with CUP and CLNM using PET/CT [12].
Roh et al. were able to reach a sensitivity of 87.5% and specificity of 82.1% in patients without precedent therapy and showed distant metastasis in six of six patients [6]. To achieve comparability, we performed a second analysis, excluding the patients with precedent therapy and a long time lag (>1 year) between the diagnosis of CLNM and PET/CT. For this modified group of patients, FDG-PET/CT reached a sensitivity of 71% and specificity of 86% (Table 3 and Table 5). This led to an increase in sensitivity and a reduction in specificity, and therefore to comparably high values for sensitivity and specificity in our real-life data.
We also performed further analysis comparing the FDG-PET/CT results of patients who did or did not undergo previous diagnostics: the sensitivity, specificity, and positive predictive value were higher for the group without previous diagnostic tests (Table 3). Yabuki et al. reported a sensitivity of 80.8% and specificity of 76.9% for a PET scan in 24 patients with cervical CUP and inconspicuous previous diagnostic procedures (clinical investigations, CT, MRI, panendoscopy), concluding satisfactory statistical values even after previous diagnostics [13].
PET/CT compares favorably to conventional imaging modalities such as CT and MRI in the setting of CUP with CLNM regarding both the identification of primary tumors and the detection of lymph node metastases.
According to the meta-analysis of Burglin et al., PET/CT was able to identify the primary tumor in approximately 41% of cases [14]. This seems superior to reports for CT and MRI, where the rates of the successful localization of squamous cell carcinomas using CT or MRI were 22% and 36%, respectively [15].
Furthermore, the sensitivity of PET/CT (95%) exceeds the sensitivity of MRI (79%) in the detection of lymph node metastases according to Antoch et al. [16], and also appeared to be preferable to CT and MRI in a meta-analysis by Kyzas et al. [17]. Gödény et al. compared FDG-PET/CT to multiparametric MRI in the detection of the primary tumor in patients with CLNM in CUP and recommended PET/CT as the method of choice due to its higher sensitivity and whole-body approach, with the possibility of identifying metastases or second malignancies [18]. Our study highlights these advantages since the suspicion of the localization of a primary tumor expressed in the preliminary examination was refuted by PET/CT in seven patients.
A major benefit of PET/CT, in addition to accurate detection, is the possibility of further evaluation of distant metastasis [18,19]. Distant metastases are associated with an overall poor prognosis; they typically occur in advanced-stage carcinomas. In a study by Al Kadah et al., 10% of the patients with a CUP of the head and neck had distant metastasis [20]. In our study, 10 patients (32%) were suspected to show distant metastases in the PET/CT; in 7 patients (23%), the distant metastases were unknown beforehand. Consequently, PET/CT provided important new information, even in a larger percentage than was to be expected from the literature. Due to the possible identification of metastases, PET/CT plays an important role in tumor staging, but additional multiplanar MRI may be required to examine local tumor invasion [18].
The presence of a second primary tumor in patients with cervical CUP is a crucial prognostic factor since the five-year survival rate in the presence of a second malignancy is only 20–30% [21]. Known noxious agents that promote the development of squamous cell carcinoma include alcohol consumption and nicotine abuse—in particular, the combination of frequent alcohol and concurrent tobacco consumption [22]. Another factor associated with its development is the human papillomavirus (HPV) [23]. Because of this pathogenesis (alcohol, smoking, HPV), the risk of a second primary carcinoma is increased for the entire upper aerodigestive tract. Synchronous second malignancies are found in 5–10% of patients with head and neck squamous cell carcinomas [24,25]. In the presence of a second carcinoma, the management approach is modified and adapted in up to 80% of cases; thus, PET/CT can provide decisive information for further therapy planning [25,26,27].
In conclusion, PET/CT offers a comprehensive diagnostic assessment with regard to the detection of a primary tumor, its staging, and possible second primary tumors simultaneously [28,29].
In order to define a clinically authentic, realistic patient population in regard to achieving our aim of a real-life investigation, the inclusion criteria of this study were intentionally defined “more broadly”. Cervical CUP syndrome is a relatively rare condition, resulting in a relatively small but still representative patient group investigated here. Since this study was carried out as a retrospective analysis, any disadvantages associated with this study design must be mentioned in a critical evaluation of the respective findings. Nevertheless, this study provides important information on a relevant number of cases under authentic circumstances.
5. Conclusions
Our real-life analysis highlights the potential of FDG-PET/CT as an accurate imaging modality that enables proper treatment planning for an optimized patient outcome. Furthermore, it is proven to be suitable for the detection of lymph node metastases and distant metastases and also for the detection of second malignancies.
FDG-PET/CT should be considered as a first-line diagnostic tool in CUP with CLNM.
FDG-PET/CT may detect the primary tumor, metastases, and second malignancies.
Author Contributions
Conceptualization: F.E., F.E.N., D.L., M.L. and A.P.; Methodology: F.E., F.E.N., S.H., M.L. and A.P.; Investigation: F.E., F.E.N., D.L., S.H., M.L. and A.P.; Data Curation: F.E., F.E.N., D.L. and A.P.; Writing—Original Draft Preparation: F.E. and A.P.; Writing—Review and Editing: F.E., D.L., J.W., S.H., M.L. and A.P.; Visualization: F.E. and A.P.; Supervision: S.H. and D.L.; Project Administration: F.E., F.E.N., M.L. and A.P.; Formal analysis: J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Philipps University Hospital of Marburg (Az.: RS 22/12).
Informed Consent Statement
Patient consent was waived due to anonymized retrospective evaluation.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, F.E., upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fries, F. Cervical CUP syndrome. Radiologe 2020, 60, 1047–1051. [Google Scholar]
- Mozet, C.; Wichmann, G.; Stumpp, P. Cervical CUP syndrome. Onkologe 2013, 19, 44–51. [Google Scholar]
- Golusinski, P.; Di Maio, P.; Pehlivan, B. Evidence for the approach to the diagnostic evaluation of squamous cell carcinoma occult primary tumors of the head and neck. Oral Oncol. 2019, 88, 145–152. [Google Scholar]
- Gutzeit, A.; Antoch, G.; Kuhl, H.; Egelhof, T.; Fischer, M.; Hauth, E.; Goehde, S.; Bockisch, A.; Debatin, J.; Freudenberg, L. Unknown primary tumors: Detection with dual-modality PET/CT—Initial experience. Radiology 2005, 234, 227–234. [Google Scholar] [CrossRef]
- Nassenstein, K.; Veit-Haibach, P.; Stergar, H.; Gutzeit, A.; Freudenberg, L.; Kuehl, H.; Fischer, M.; Barkhausen, J.; Bockisch, A.; Antoch, G. Cervical lymph node metastases of unknown origin: Primary tumor detection with whole-body positron emission tomography/computed tomography. Acta. Radiol. 2007, 48, 1101–1108. [Google Scholar] [CrossRef]
- Roh, J.-L.; Kim, J.S.; Lee, J.H.; Cho, K.-J.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y. Utility of combined 18F-fluorodeoxyglucose-positron emission tomography and computed tomography in patients with cervical metastases from unknown primary tumors. Oral Oncol. 2009, 45, 218–224. [Google Scholar] [CrossRef]
- Keller, F.; Psychogios, G.; Linke, R.; Lell, M.; Kuwert, T.; Iro, H.; Zenk, J. Carcinoma of unknown primary in the head and neck: Comparison between positron emission tomography (PET) and PET/CT. Head Neck 2010, 33, 1569–1575. [Google Scholar] [CrossRef]
- Wong, W.; Sonoda, L.; Gharpurhy, A.; Gollub, F.; Wellsted, D.; Goodchild, K.; Lemon, C.; Farrell, R.; Saunders, M. 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the assessment of occult primary head and neck cancers—An audit and review of published studies. Clin. Oncol. R. Coll. Radiol. 2012, 24, 190–195. [Google Scholar] [CrossRef]
- Lee, J.R.; Kim, J.S.; Roh, J.-L.; Lee, J.H.; Baek, J.H.; Cho, K.-J.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y. Detection of occult primary tumors in patients with cervical metastases of unknown primary tumors: Comparison of 18F FDG PET/CT with contrast-enhanced CT or CT/MR imaging—Prospective study. Radiology 2015, 274, 764–771. [Google Scholar] [CrossRef]
- Sprave, T.; Rühle, A.; Hees, K. Radiotherapeutic management of cervical lymph node metastases from an unknown primary site—Experiences from a large cohort treated with modern radiation techniques. Radiat. Oncol. 2020, 15, 80. [Google Scholar]
- Rusthoven, K.E.; Koshy, M.; Paulino, A.C. The role of fluorodeoxyglucose positron emission tomography in cervical lymph node metastases from an unknown primary tumor. Cancer 2004, 101, 2641–2649. [Google Scholar] [CrossRef]
- Nikolova, P.N.; Hadzhiyska, V.H.; Mladenov, K.B.; Ilcheva, M.G.; Veneva, S.; Grudeva, V.V.; Dineva, S.E.; Asenov, Y.N. The impact of 18F-FDG PET/CT in the clinical management of patients with lymph node metastasis of unknown primary origin. Neoplasma 2021, 68, 180–189. [Google Scholar] [CrossRef]
- Yabuki, K.; Tsukuda, M.; Horichui, C. Role of 18F-FDG pet in detecting primary site in the patient with primary unknown carcinoma. Eur. Arch. Otorhinolaryngol. 2010, 267, 1785–1792. [Google Scholar]
- Burglin, S.A.; Hess, S.; Høilund-Carlsen, P.F.; Gerke, O. 18F-FDG PET/CT for detection of the primary tumor in adults with extracervical metastases from cancer of unknown primary. Medicine 2017, 96, e6713. [Google Scholar] [CrossRef]
- Kwee, T.C.; Kwee, R.M. Combined FDG-PET/CT for the detection of unknown primary tumors: Systematic review and meta-analysis. Eur. Radiol. 2009, 19, 731–744. [Google Scholar] [CrossRef] [Green Version]
- Antoch, G.; Vogt, F.M.; Freudenberg, L.S.; Nazaradeh, F.; Goehde, S.C.; Barkhausen, J.; Dahmen, G.; Bockisch, A.; Debatin, J.F.; Ruehm, S.G. Whole-body dual-modality PET/CT and whole-body MRI for tumor staging in oncology. JAMA 2003, 290, 3199. [Google Scholar] [CrossRef]
- Kyzas, P.A.; Evangelou, E.; Denaxa-Kyza, D.; Ioannidis, J.P.A. 18F-fluorodeoxyglucose positron emission tomography to evaluate cervical node metastases in patients with head and neck squamous cell carcinoma: A meta-analysis. JNCI J. Natl. Cancer Inst. 2008, 100, 712–720. [Google Scholar] [CrossRef]
- Gődény, M.; Lengyel, Z.; Polony, G. Impact of 3T multiparametric MRI and FDG-PET-CT in the evaluation of occult primary cancer with cervical node metastasis. Cancer Imaging 2016, 16, 38. [Google Scholar] [CrossRef]
- Evangelista, L.; Cervino, A.R.; Chondrogiannis, S. Comparison between anatomical cross-sectional imaging and 18F-FDG PET/CT in the staging, restaging, treatment response, and long-term surveillance of squamous cell head and neck cancer: A systematic literature overview. Nucl. Med. Commun. 2014, 35, 123–134. [Google Scholar]
- Al Kadah, B.; Papaspyrou, G.; Linxweiler, M.; Schick, B.; Rübe, C.; Büchler, B.S.; Niewald, M. Cancer of unknown primary (CUP) of the head and neck: Retrospective analysis of 81 patients. Eur. Arch. Otorhinolaryngol. 2017, 274, 2557–2566. [Google Scholar] [CrossRef]
- Chuang, S.C.; Scelo, G.; Tonita, J.M. Risk of second primary cancer among patients with head and neck cancers: A pooled analysis of 13 cancer registries. Int. J. 2008, 123, 2390–2396. [Google Scholar]
- Matthias, C.; Harréus, U.; Strange, R. Influential factors on tumor recurrence in head and neck cancer patients. Eur. Arch. Otorhinolaryngol. 2006, 263, 37–42. [Google Scholar] [CrossRef]
- Rettig, E.M.; D’Souza, G. Epidemiology of head and neck cancer. Surg. Oncol. Clin. N. Am. 2015, 24, 379–396. [Google Scholar]
- Castaldi, P.; Leccisotti, L.; Bussu, F.; Miccichè, F.; Rufini, V. Role of 18F-FDG PET-CT in head and neck squamous cell carcinoma. Acta Otorhinolaryngol. Ital. 2013, 33, 1–8. [Google Scholar]
- Strobel, K.; Haerle, S.K.; Stoeckli, S.J.; Schrank, M.; Soyka, J.D.; Veit-Haibach, P.; Hany, T.F. Head and neck squamous cell carcinoma (HNSCC)—Detection of synchronous primaries with 18F-FDG-PET/CT. Eur. J. Nucl. Med. Moll. Imaging 2009, 36, 919–927. [Google Scholar] [CrossRef]
- Dietl, B.; Marienhagen, J.; Kühnel, T.; Schreyer, A.; Kölbl, O. The impact of FDG-PET/CT on the management of head and neck tumours: The radiotherapist’s perspective. Oral Oncol. 2008, 44, 504–508. [Google Scholar] [CrossRef]
- Xu, G.Z.; Guan, D.E.; He, Z.Y. 18FDG-PET/CT for detecting distant metastases and second primary cancersin patients with head and neck cancer. A meta-analysis. Oral Oncol. 2011, 47, 560–565. [Google Scholar]
- Send, T.; Kreppel, B.; Gaertner, F.C.; Bundschuh, R.A.; Strunk, H.; Bootz, F.; Essler, M. PET-CT in head and neck cancer. HNO 2017, 65, 504–513. [Google Scholar]
- Johansen, J.; Buus, S.; Loft, A. Prospective study of 18FDG-PET in the detection and management of patients with lymph node metastases to the neck from unknown primary tumor. Results form the DAHANCA-13 study. Head Neck 2008, 30, 471–478. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).