Proposal of Dental Hygiene Diagnosis for Cancer Patients Based on Dental Hygiene Process of Care in Acute Care Hospitals: A Narrative Review
Abstract
1. Introduction
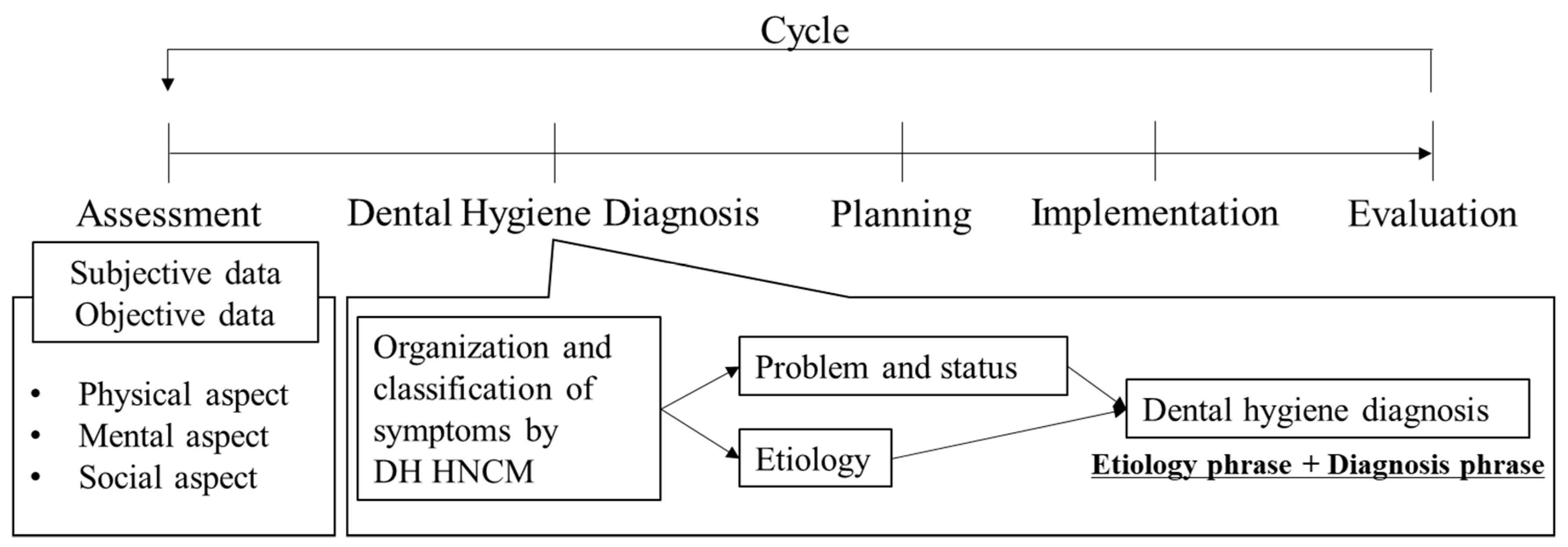
2. Review Process for the Purpose of Developing Diagnoses
3. Proposal of Dental Hygiene Diagnosis for Each Subscale
3.1. Wholesome Facial Image (HN1)
3.2. Protection from Health Risks (HN2)
3.3. Biologically Sound and Functional Dentition (HN3)
3.4. Skin and Mucous Membrane Integrity of the Head and Neck (HN4)
3.5. Freedom from Head and Neck Pain (HN5)
3.6. Freedom from Anxiety and Stress (HN6)
3.7. Responsibility for Oral Health (HN7)
3.8. Conceptualization and Understanding (HN8)
4. Limitations
5. Conclusions
5.1. Scope for Further Research
5.2. Clinical Relevance
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- MacDonald, L.; Bowen, D.M. Theory analysis of the dental hygiene human needs conceptual model. Int. J. Dent. Hyg. 2017, 15, e163–e172. [Google Scholar] [CrossRef] [PubMed]
- Yura, H. Human need theory: A framework for the nurse supervisor. Health Care Superv. 1986, 4, 45–58. [Google Scholar] [PubMed]
- Darby, M.L.; Walsh, M.M. Application of the human needs conceptual model to dental hygiene practice. J. Dent. Hyg. 2000, 74, 230–237. [Google Scholar] [PubMed]
- Sato, Y.; Saito, A.; Nakamura–Miura, A.; Kato, E.; Cathcart, G. Application of the dental hygiene human needs conceptual model and the oral health–related quality of life model to the dental hygiene curriculum in Japan. Int. J. Dent. Hyg. 2007, 5, 158–164. [Google Scholar] [CrossRef]
- Nishimura, T.; Takahashi, C.; Takahashi, E. Dental hygiene residential care in a 3-year dental hygiene education programme in Japan: Towards dysphagia management based on the dental hygiene process of care. Int. J. Dent. Hyg. 2007, 5, 145–150. [Google Scholar] [CrossRef]
- Sensat, M.L. Mobius syndrome: A dental hygiene case study and review of the literature. Int. J. Dent. Hyg. 2003, 1, 62–67. [Google Scholar] [CrossRef]
- Toney-Butler, T.J.; Thayer, J.M. Nursing process. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Huitzi-Egilegor, J.X.; Elorza-Puyadena, M.I.; Urkia-Etxabe, J.M.; Asurabarrena-Iraola, C. Implementation of the nursing process in a health area: Models and assessment structures used. Rev. Lat. Am. Enfermagem 2014, 22, 772–777. [Google Scholar] [CrossRef]
- Malekzadeh, J.; Amouzeshi, Z.; Mazlom, S.R. A quasi–experimental study of the effect of teaching Orem’s self–care model on nursing students’ clinical performance and patient satisfaction. Nurs. Open 2018, 5, 370–375. [Google Scholar] [CrossRef]
- Hogston, R. Nursing diagnosis and classification systems: A position paper. J. Adv. Nurs. 1997, 26, 496–500. [Google Scholar] [CrossRef]
- Kurasawa, Y.; Maruoka, Y.; Sekiya, H.; Negishi, A.; Mukohyama, H.; Shigematsu, S.; Sugizaki, J.; Karakida, K.; Ohashi, M.; Ueno, M.; et al. Pneumonia prevention effects of perioperative oral management in approximately 25,000 patients following cancer surgery. Clin. Exp. Dent. Res. 2020, 6, 165–173. [Google Scholar] [CrossRef]
- Saunders, D.P.; Rouleau, T.; Cheng, K.; Yarom, N.; Kandwal, A.; Joy, J.; Kayhan, K.B.; van de Wetering, M.; Brito-Dellan, N.; Kataoka, T.; et al. Systematic review of antimicrobials, mucosal coating agents, anesthetics, and analgesics for the management of oral mucositis in cancer patients and clinical practice guidelines. Support. Care Cancer 2020, 28, 2473–2484. [Google Scholar] [CrossRef] [PubMed]
- McGuire, D.B.; Fulton, J.S.; Park, J.; Brown, C.G.; Correa, M.E.P.; Eilers, J.; Elad, S.; Gibson, F.; Oberle-Edwards, L.K.; Bowen, J.; et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients. Support. Care Cancer 2013, 21, 3165–3177. [Google Scholar] [CrossRef] [PubMed]
- Olver, I.; Keefe, D.; Herrstedt, J.; Warr, D.; Roila, F.; Ripamonti, C.I. Supportive care in cancer—A MASCC perspective. Support. Care Cancer 2020, 28, 3467–3475. [Google Scholar] [CrossRef] [PubMed]
- Danser, M.M.; Gomez, S.M.; Van der Weijden, G.A. Tongue coating and tongue brushing: A literature review. Int. J. Dent. Hyg. 2003, 1, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Darby, M.L.; Walsh, M.M. A proposed human needs conceptual model for dental hygiene: Part I. J. Dent. Hyg. 1993, 67, 326–334. [Google Scholar] [PubMed]
- Walsh, M.M.; Darby, M. Application of the human needs conceptual model of dental hygiene to the role of the clinician: Part II. J. Dent. Hyg. 1993, 67, 335–346. [Google Scholar]
- Forastiere, A.; Goepfert, H.; Goffinet, D.; Hong, K.W.; Laramore, G.; Mittal, B.; Pfister, D.G.; Ridge, J.; Schuller, D.; Shah, J.; et al. NCCN practice guidelines for head and neck cancer. National comprehensive cancer network. Oncology 1998, 12, 39–147. [Google Scholar]
- Costa, E.F.; Nogueira, T.E.; de Souza Lima, N.C.; Mendonca, E.F.; Leles, C.R. A qualitative study of the dimensions of patients’ perceptions of facial disfigurement after head and neck cancer surgery. Spec. Care Dent. 2014, 34, 114–121. [Google Scholar] [CrossRef]
- Ishimaru, M.; Matsui, H.; Ono, S.; Hagiwara, Y.; Morita, K.; Yasunaga, H. Preoperative oral care and effect on postoperative complications after major cancer surgery. Br. J. Surg. 2018, 105, 1688–1696. [Google Scholar] [CrossRef]
- Yamada, S.I.; Soutome, S.; Hasegawa, T.; Toujou, I.; Nakahara, H.; Kawakami, M.; Hirose, M.; Fujita, S.; Komori, T.; Kirita, T.; et al. A multicenter retrospective investigation on the efficacy of perioperative oral management in cancer patients. Medicine 2020, 99, e19129. [Google Scholar] [CrossRef]
- Selzer, E.; Liederer, S.; Lemaire, C.; Kren, G.; Radonjic, D.; Kornek, G.; Knocke, T.; Pötter, R.; Bachtiary, B. Incidence of dermatitis in head and neck cancer patients treated with primary radiotherapy and cetuximab. Strahlenther. Onkol. 2011, 187, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Green, C.R.; Hart-Johnson, T.; Loeffler, D.R. Cancer–related chronic pain: Examining quality of life in diverse cancer survivors. Cancer 2011, 117, 1994–2003. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S. Neuropathic caner pain: Is it linked to the recurrence of cancer? Korean J. Pain 2015, 28, 73–74. [Google Scholar] [CrossRef]
- Jansen, F.; Verdonck-de Leeuw, I.M.; Cuijpers, P.; Leemans, C.R.; Waterboer, T.; Pawlita, M.; Penfold, C.; Thomas, S.J.; Waylen, A.; Ness, A.R. Depressive symptoms in relation to overall survival in people with head and neck cancer: A longitudinal cohort study. Psychooncology 2018, 27, 2245–2256. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Karino, M.; Kanno, T. Development and Validation of the Oral Health–Related Self–Efficacy Scale for Cancer Patients. J. Cancer Educ. 2020. [Google Scholar] [CrossRef]
- Miranda, T.P.S.; Caldeira, S.; de Oliveira, H.F.; Iunes, D.H.; Nogueira, D.A.; Chaves, E.D.C.L.; de Carvalho, E.C. Intercessory prayer on spiritual distress, spiritual coping, anxiety, depression and salivary amylase in breast cancer patients during radiotherapy: Randomized clinical trial. J. Relig. Health 2020, 59, 365–380. [Google Scholar] [CrossRef]
- Ellis, M.A.; Sterba, K.R.; Brennan, E.A.; Maurer, S.; Hill, E.G.; Day, T.A.; Graboyes, E.M. A systematic review of patient–reported outcome measures assessing body image disturbance in patients with head and neck cancer. Otolaryngol. Head Neck Surg. 2019, 160, 941–954. [Google Scholar] [CrossRef]
- Arweiler, N.B.; Auschill, T.M.; Sculean, A. Patient self-care of periodontal pocket infections. Periodontology 2000 2018, 76, 164–179. [Google Scholar] [CrossRef]
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese society of gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef]
- Al-Qurayshi, Z.; Walsh, J.; Owen, S.; Kandil, E. Surgical site infection in head and neck surgery: A national perspective. Otolaryngol. Head Neck Surg. 2019, 161, 52–62. [Google Scholar] [CrossRef]
- Haque, M.; McKimm, J.; Godman, B.; Abu Bakar, M.; Sartelli, M. Initiatives to reduce postoperative surgical site infections of the head and neck cancer surgery with a special emphasis on developing countries. Expert Rev. Anticancer Ther. 2019, 19, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Funahara, M.; Yanamoto, S.; Ueda, M.; Suzuki, T.; Ota, Y.; Nishimaki, F.; Kurita, H.; Yamakawa, N.; Kirita, T.; Okura, M.; et al. Prevention of surgical site infection after oral cancer surgery by topical tetracycline: Results of a multicenter randomized control trial. Medicine 2017, 96, e8891. [Google Scholar] [CrossRef]
- Miki, Y.; Makuuchi, R.; Honda, S.; Tokunaga, M.; Tanizawa, Y.; Bando, E.; Kawamura, T.; Yurikusa, T.; Tanuma, A.; Terashima, M. Prospective phase II study evaluating the efficacy of swallow ability screening tests and pneumonia prevention using a team approach for elderly patients with gastric cancer. Gastric Cancer 2018, 21, 353–359. [Google Scholar] [CrossRef]
- Iwata, E.; Hasegawa, T.; Yamada, S.I.; Kawashita, Y.; Yoshimatsu, M.; Mizutani, T.; Nakahara, H.; Mori, K.; Shibuya, Y.; Kurita, H.; et al. Effects of perioperative oral care on prevention of postoperative pneumonia after lung resection: Multicenter retrospective study with propensity score matching analysis. Surgery 2019, 165, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Swan, K.; Cordier, R.; Brown, T.; Speyer, R. Psychometric properties of visuoperceptual measures of videofluoroscopic and fibre–endoscopic evaluations of swallowing: A systematic review. Dysphagia 2019, 34, 2–33. [Google Scholar] [CrossRef]
- Rosa, R.R.; Bueno, M.; Migliorucci, R.R.; Brasolotto, A.G.; Genaro, K.F.; Berretin–Felix, G. Tongue function and swallowing in individuals with temporomandibular disorders. J. Appl. Oral Sci. 2020, 28, e20190355. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Futatsuki, T.; Takesaki, H.; Ooe, T.; Abe, K. Postoperative bleeding after tooth extractions in patients controlled with warfarin—A clinic—Statistical study on the factors influencing postoperative bleeding. Fukuoka Igaku Zasshi 2004, 95, 218–223. [Google Scholar]
- Schoenfeld, B.J.; Grgic, J. Effects of range of motion on muscle development during resistance training interventions: A systematic review. SAGE Open Med. 2020, 8, 2050312120901559. [Google Scholar] [CrossRef]
- Prahlow, J.A.; Prahlow, T.J.; Rakow, R.J.; Prahlow, N.D. Case study: Asphyxia caused by inspissated oral and nasopharyngeal secretions. Am. J. Nurs. 2009, 109, 38–43. [Google Scholar] [CrossRef]
- John, M.T.; Michalowicz, B.S.; Kotsakis, G.A.; Chu, H. Network meta–analysis of studies included in the clinical practice guideline on the nonsurgical treatment of chronic periodontitis. J. Clin. Periodontol. 2017, 44, 603–611. [Google Scholar] [CrossRef]
- Schenkel, A.B.; Veitz-Keenan, A. Dental cavity liners for Class I and Class II resin—Based composite restorations. Cochrane Database Syst. Rev. 2019, 3, CD010526. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, G.; Ugolini, A.; Sforza, C.; Gbinigie, O.; Pluddemann, A. Long-Term effects of functional appliances in treated versus untreated patients with Class II malocclusion: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0221624. [Google Scholar] [CrossRef] [PubMed]
- Bollen, A.M. Effects of malocclusions and orthodontics on periodontal health: Evidence from a systematic review. J. Dent. Educ. 2008, 72, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Abt, E.; Carr, A.B.; Worthington, H.V. WITHDRAWN: Interventions for replacing missing teeth: Partially absent dentition. Cochrane Database Syst. Rev. 2019, 7, CD003814. [Google Scholar] [PubMed]
- Carrasco-Garcia, A.; Castellanos-Cosano, L.; Corcuera-Flores, J.R.; Rodriguez-Perez, A.; Torres-Lagares, D.; Machuca-Portillo, G. Influence of marginal bone loss on peri-implantitis: Systematic review of literature. J. Clin. Exp. Dent. 2019, 11, e1045–e1071. [Google Scholar] [CrossRef] [PubMed]
- Dorocka-Bobkowska, B.; Medynski, D.; Prylinski, M. Recent advances in tissue conditioners for prosthetic treatment: A review. Adv. Clin. Exp. Med. 2017, 26, 723–728. [Google Scholar] [CrossRef]
- Limones, A.; Saez-Alcaide, L.M.; Diaz-Parreno, S.A.; Helm, A.; Bornstein, M.M.; Molinero-Mourelle, P. Medication-related osteonecrosis of the jaws (MRONJ) in cancer patients treated with denosumab VS. zoledronic acid: A systematic review and meta–analysis. Med. Oral Patol. Oral Cir. Bucal. 2020, 25, e326–e336. [Google Scholar] [CrossRef]
- Jensen, S.B.; Pedersen, A.M.L.; Vissink, A.; Andersen, E.; Brown, C.G.; Davies, A.N.; Dutilh, J.; Fulton, J.S.; Jankovic, L.; Lopes, N.N.; et al. A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: Management strategies and economic impact. Support. Care Cancer 2010, 18, 1061–1079. [Google Scholar] [CrossRef]
- Pontini, A.; Reho, F.; Giatsidis, G.; Bacci, C.; Azzena, B.; Tiengo, C. Multidisciplinary care in severe pediatric electrical oral burn. Burns 2015, 41, e41–e46. [Google Scholar] [CrossRef] [PubMed]
- Antikainen, A.; Patinen, P.; Pakkila, J.; Tjaderhane, L.; Anttonen, V. The types and management of dental trauma during military service in Finland. Dent. Traumatol. 2018, 34, 87–92. [Google Scholar] [CrossRef]
- Ferreira, E.B.; Vasques, C.I.; Gadia, R.; Chan, R.J.; Guerra, E.N.S.; Mezzomo, L.A.; Canto, G.D.L.; dos Reis, P.E.D. Topical interventions to prevent acute radiation dermatitis in head and neck cancer patients: A systematic review. Support. Care Cancer 2017, 25, 1001–1011. [Google Scholar] [CrossRef]
- Mosa, A.S.M.; Hossain, A.M.; Lavoie, B.J.; Yoo, I. Patient–related risk factors for chemotherapy–induced nausea and vomiting: A systematic review. Front. Pharmacol. 2020, 11, 329. [Google Scholar] [CrossRef]
- Billingham, M.J.; Billingham, S.J. Congruence between preferred and actual place of death according to the presence of malignant or non–malignant disease: A systematic review and meta–analysis. BMJ Support. Palliat. Care 2013, 3, 144–154. [Google Scholar] [CrossRef]
- Yilmaz, S.D.; Bal, M.D.; Beji, N.K.; Arvas, M. Ways of coping with stress and perceived social support in gynecologic cancer patients. Cancer Nurs. 2015, 38, E57–E62. [Google Scholar] [CrossRef]
- Karabulutlu, E.Y. Coping with stress of family caregivers of cancer patients in Turkey. Asia Pac. J. Oncol. Nurs. 2014, 1, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Macek, M.D.; Haynes, D.; Wells, W.; Bauer-Leffler, S.; Cotten, P.A.; Parker, R.M. Measuring conceptual health knowledge in the context of oral health literacy: Preliminary results. J. Public Health Dent. 2010, 70, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Jomar, R.T.; Gomes, R.A.F.; Leite, D.C.; Gomes, H.F.; Peres, E.M.; Junior, E.F.P. Nursing diagnoses in adult/elderly patients undergoing outpatient antineoplastic chemotherapy: A review. Ecancermedicalscience 2017, 11, 736. [Google Scholar]
- Leinweber, K.A.; Columbo, J.A.; Kang, R.; Trooboff, S.W.; Goodney, P.P. A review of decision aids for patients considering more than one type of invasive treatment. J. Surg. Res. 2019, 235, 350–366. [Google Scholar] [CrossRef] [PubMed]
- Shunmuga, S.C.; Dhillon, H.M.; Butow, P.N.; Sundaresan, P.; Rutherford, C. A systematic review of body image measures for people diagnosed with head and neck cancer (HNC). Support. Care Cancer 2019, 27, 3657–3666. [Google Scholar] [CrossRef] [PubMed]
| Human Needs (HN) | Contents |
|---|---|
| HN1 | Wholesome facial image |
| HN2 | Protection from health risks |
| HN3 | Biologically sound and functional dentition |
| HN4 | Skin and mucous membrane integrity of the head and neck |
| HN5 | Freedom from head and neck pain |
| HN6 | Freedom from anxiety and stress |
| HN7 | Responsibility for oral health |
| HN8 | Conceptualization and understanding |
| NANDA-I | Contents |
|---|---|
| Pattern 1 | Health perception/health management pattern |
| Pattern 2 | Nutritional/metabolic pattern |
| Pattern 3 | Elimination pattern |
| Pattern 4 | Activity/exercise pattern |
| Pattern 5 | Sleep/rest pattern |
| Pattern 6 | Cognitive/perceptual pattern |
| Pattern 7 | Self-perception pattern |
| Pattern 8 | Role/relationship pattern |
| Pattern 9 | Sexuality/reproductive pattern |
| Pattern 10 | Coping/stress tolerance pattern |
| Pattern 11 | Value/belief pattern |
| Human Needs (HN) Conceptual Model | Diagnosis | Defining Characteristics | Reference |
|---|---|---|---|
| HN1: Wholesome facial image | Disturbed body image | The condition in which there is confusion in regard to the mental picture of one’s physical self. | [28] |
| HN2: Protection from health risks | Risk for infection | The condition in which there is an increased risk of being invaded by pathogenic organisms. | [20,29,30,31] |
| Delayed surgical recovery | The condition of vulnerability to an extension of the number of postoperative days required to initiate and perform activities that maintain life, health, and well-being, which may compromise health. | [32,33] | |
| Risk for aspiration | The condition of being at risk for entry of gastrointestinal secretions, oropharyngeal secretions, solids, or fluids into tracheobronchial passages. | [30,34] | |
| Ineffective self-oral health management | The condition in which patients cannot express the desire to manage oral health for treatment and prevention of complications. | - | |
| Ineffective family self-oral health management | The condition in which families cannot achieve the goal of oral health or are at risk. | - | |
| Risk for ventilator associated pneumonia | The condition of being at risk for ventilator-associated pneumonia by aspiration. | [35] | |
| Swallowing disorder *CP | The condition in which there has been a diagnosis of swallowing disorder. The condition in which a patient complains about deglutition. | [36] | |
| Feeding self-care deficit | The condition in which the ability to perform or complete feeding activities is impaired. | [37] | |
| Risk for oral bleeding | The condition in which there is postoperative oral bleeding or oral bleeding due to low platelet count during chemotherapy. | [38] | |
| Impaired physical mobility *CP | The condition in which there is a diagnosis of impaired physical mobility. The condition in which there is a limit to intentional body movements and limb movements that can be executed by patients themselves. | [39] | |
| Risk for ineffective respiratory function | The condition in which air passage through the respiratory tract is threatened. | [40] | |
| Ineffective airway clearance | The condition of inability to remove secretions or obstructions from the respiratory tract. | [40] | |
| Readiness for enhanced nutrition | The condition in which nutrition intake is sufficient for metabolism and further strengthening is possible. | - | |
| Impaired communication | The condition of inability to exchange ideas and requests with others. | - | |
| Impaired verbal communication | The condition in which any or all of the ability to receive, process, and convey words or letter sounds is diminished. | - | |
| HN3: Biologically sound and functional dentition | Periodontal disease *CP | The condition in which diagnosis of periodontal disease has been made by a dentist. | [41] |
| Caries *CP | The condition in which diagnosis of caries has been made by a dentist. | [42] | |
| Malocclusion *CP | The condition in which diagnosis of malocclusion has been made by a dentist. | [43] | |
| Malalignment *CP | The condition in which diagnosis of malalignment has been made by a dentist. | [44] | |
| Missing teeth *CP | The condition in which diagnosis of missing teeth has been made by a dentist. | [45] | |
| Crown fracture *CP | The condition in which diagnosis of crown fracture has been made by a dentist. | [42] | |
| Ill-fitting prosthesis *CP | The condition in which diagnosis of ill-fitting prosthesis has been made by a dentist. | [42] | |
| Peri-implantitis *CP | The condition in which diagnosis of peri-implantitis has been made by a dentist. | [46] | |
| Ill-fitting denture *CP | The condition in which diagnosis of ill-fitting denture has been made by a dentist. | [47] | |
| Masticatory disturbance *CP | The condition in which diagnosis of masticatory disturbance has been made by a dentist. | [30] | |
| HN4: Skin and mucous membrane integrity of the head and neck | Oral mucositis *CP | The condition in which diagnosis of oral mucositis has been made by a dentist or medical doctor. | [12] |
| Surgical site infection *CP | The condition in which diagnosis of surgical site infection has been made by a dentist or medical doctor. | [32,33] | |
| Osteonecrosis of the jaws *CP | The condition in which diagnosis of osteonecrosis of the jaws has been made by a dentist or medical doctor. | [48] | |
| Dry mouth | The condition in which the salivary glands in the mouth do not make enough saliva to keep the mouth wet. | [49] | |
| Abnormal tongue shape and color | The condition in which the tongue turns red, yellow, purple, or another color and changes shape. | - | |
| Stomatitis *CP | The condition in which diagnosis of stomatitis has been made by a dentist or medical doctor. | [12] | |
| Bite wound *CP | The condition in which diagnosis of bite wound has been made by a dentist or medical doctor. | - | |
| Oral burn *CP | The condition in which diagnosis of oral burn has been made by a dentist or medical doctor. | [50] | |
| Oral trauma *CP | The condition in which diagnosis of oral trauma has been made by a dentist or medical doctor. | [51] | |
| Radiodermatitis *CP | The condition in which diagnosis of radiodermatitis has been made by a dentist or medical doctor. | [52] | |
| HN5: Freedom from head and neck pain | Acute pain | The condition in which a patient complains about acute pain. | - |
| Chronic pain | The condition in which a patient complains about chronic pain. | - | |
| HN6: Freedom from anxiety and stress | Nausea and vomiting | The condition in which a patient complains about stomach discomfort and the sensation of wanting to vomit or vomiting. | [53] |
| Powerlessness | The condition of lacking self-control, which is caused by stress in patients with cancer. | [54] | |
| Death anxiety | The condition in which one experiences a feeling of dread, apprehension, or solicitude (i.e., anxiety) when one thinks of the process of dying or ceasing. | [54] | |
| Anxiety | The condition in which a patient experiences a feeling of worry, nervousness, or unease about something with an uncertain outcome. | [54] | |
| Fear | The condition in which a patient experiences a feeling of unpleasant emotion caused by the threat of danger, pain, or harm. | [54] | |
| Ineffective coping | The condition in which a patient is unable to realistically assess stressors and use available resources to cope with stress. | [55] | |
| Readiness for enhanced coping | The condition in which there are cognitive and behavioral efforts to manage demands that are sufficient for well-being and that can be strengthened. | [55] | |
| Disabled family coping | The condition in which caregiver’s experience stress when patients cannot cope with the symptoms they are experiencing. | [56] | |
| HN7: Responsibility for oral health | Low oral-health-related self-efficacy | The condition in which the patients cannot execute courses of oral health action required to deal with prospective situations. | [26] |
| Low oral literacy | The condition in which individuals have the capacity to obtain, process, and understand basic oral health information and services needed to make appropriate oral health decisions. | [57] | |
| Deficient knowledge | The condition in which individuals have a lack of cognitive information or psychomotor ability needed for health restoration, preservation, or health promotion. | [58] | |
| Readiness for enhanced knowledge | The condition in which the presence or acquisition of cognitive information related to the oral health topic is sufficient for meeting health-related goals and can be strengthened. | [58] | |
| Readiness for enhanced oral self-care | The condition in which a patient is able to regulate and integrate a therapeutic regimen into their daily living for the treatment of illness and its sequelae in a way that is sufficient for meeting health-related goals and that can be strengthened. | [58] | |
| HN8: Conceptualization and understanding | Decisional conflict | The condition in which there is uncertainty about which course of action to take when the choice among competing actions involves risk, loss, or a challenge to one’s values and beliefs. | [59] |
| Disturbed self-concept | The condition in which there is a negative state of change about the way a person feels, thinks, or views him or herself. | [60] | |
| Spiritual distress | The condition in which the ability to experience and integrate meaning and purpose in life through connectedness with self, others, art, music, literature, nature, and/or a power greater than oneself is impaired. | [58] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuda, Y.; Karino, M.; Okuma, S.; Ikebuchi, K.; Takeda, M.; Kanno, T. Proposal of Dental Hygiene Diagnosis for Cancer Patients Based on Dental Hygiene Process of Care in Acute Care Hospitals: A Narrative Review. Healthcare 2020, 8, 217. https://doi.org/10.3390/healthcare8030217
Matsuda Y, Karino M, Okuma S, Ikebuchi K, Takeda M, Kanno T. Proposal of Dental Hygiene Diagnosis for Cancer Patients Based on Dental Hygiene Process of Care in Acute Care Hospitals: A Narrative Review. Healthcare. 2020; 8(3):217. https://doi.org/10.3390/healthcare8030217
Chicago/Turabian StyleMatsuda, Yuhei, Masaaki Karino, Satoe Okuma, Kumi Ikebuchi, Mayu Takeda, and Takahiro Kanno. 2020. "Proposal of Dental Hygiene Diagnosis for Cancer Patients Based on Dental Hygiene Process of Care in Acute Care Hospitals: A Narrative Review" Healthcare 8, no. 3: 217. https://doi.org/10.3390/healthcare8030217
APA StyleMatsuda, Y., Karino, M., Okuma, S., Ikebuchi, K., Takeda, M., & Kanno, T. (2020). Proposal of Dental Hygiene Diagnosis for Cancer Patients Based on Dental Hygiene Process of Care in Acute Care Hospitals: A Narrative Review. Healthcare, 8(3), 217. https://doi.org/10.3390/healthcare8030217






