The Prognostic Implications of the Geriatric Nutritional Risk Index in Patients with Prostate Cancer: A Single-Center Retrospective Cohort Study
Abstract
1. Introduction
- (1)
- Lower GNRI scores are associated with a higher incidence of postoperative complications;
- (2)
- GNRI-defined nutritional risk is independently associated with increased healthcare utilization, including prolonged hospital stay and higher hospitalization costs.
2. Materials and Methods
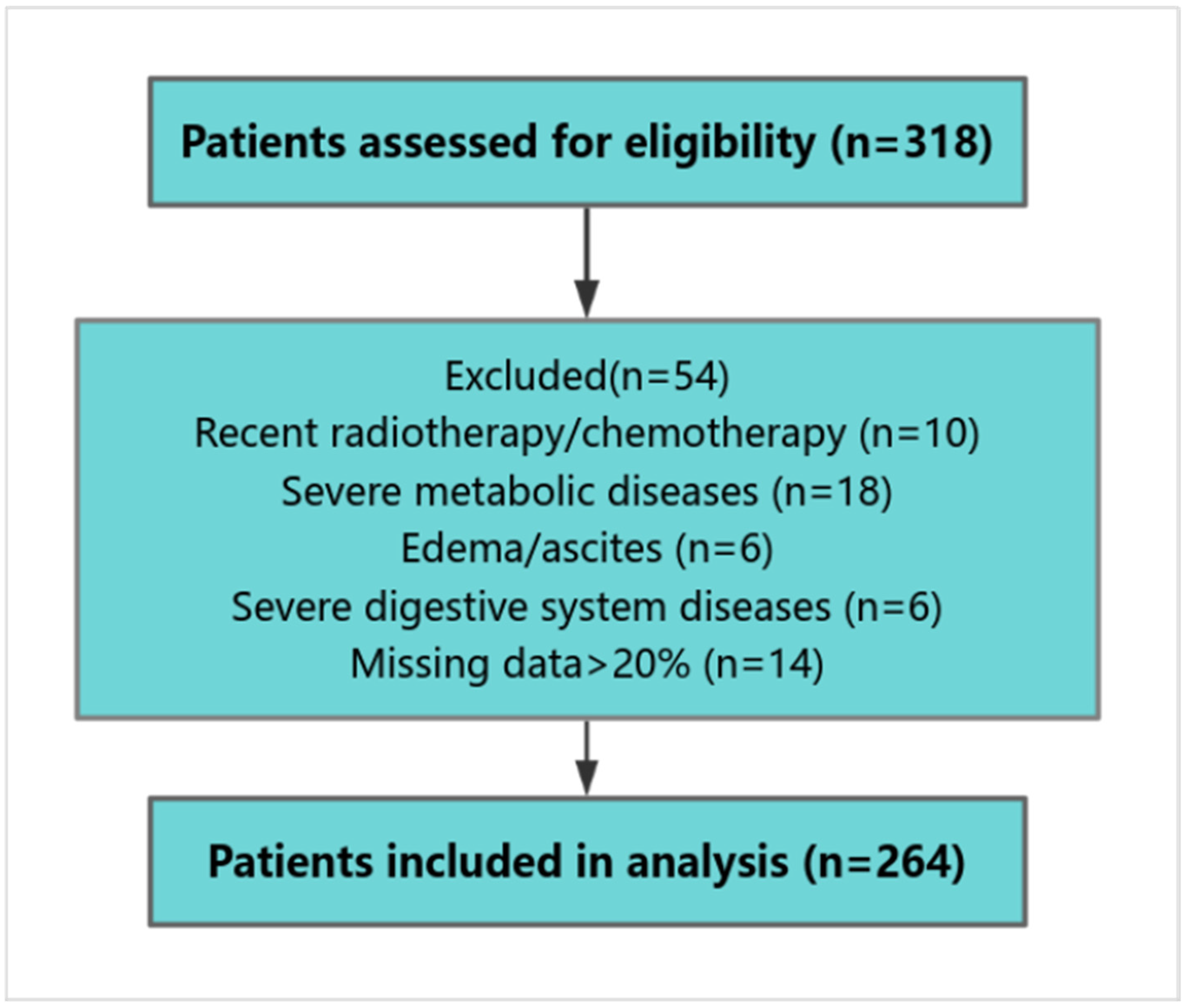
2.1. Patients
- (1)
- Histologically confirmed prostate cancer;
- (2)
- Localized disease (cT1–T2N0M0) on preoperative imaging;
- (3)
- Completion of GNRI assessment prior to surgery.
- (1)
- Receipt of chemotherapy or radiotherapy within 3 months prior to surgery;
- (2)
- Severe metabolic disorders (e.g., diabetic ketoacidosis, thyrotoxic crisis);
- (3)
- Lower extremity edema or imaging evidence of effusion (pleural, peritoneal);
- (4)
- Chronic gastrointestinal conditions (e.g., liver failure, Crohn’s disease);
- (5)
- Missing >20% of required clinical data.
2.2. Clinical and Laboratory Data Collection
- Primary outcomes: These outcomes included postoperative complications and health economic indicators. Postoperative complications—such as delirium, persistent fever ≥ 38.5 °C, lower-limb deep venous thrombosis, incomplete intestinal obstruction, and poor wound healing—were clinically diagnosed and documented in electronic medical records by attending physicians. These events were further verified based on routine clinical assessments, laboratory tests, and imaging examinations when applicable.
- Economic outcomes: Length of hospital stay and direct inpatient costs (surgery, medications, diagnostics, nursing care) were assessed. Indirect costs (e.g., productivity loss, caregiving, rehabilitation) were excluded. Costs were recorded in Chinese Yuan (CNY); an approximate exchange rate of USD 1 ≈ CNY 7.2 was used for international reference. Due to the right-skewed distributions, both length of stay and costs were dichotomized using their medians. Scatter plots were generated to visualize the continuous relationship between the GNRI and these economic variables.
2.3. Definition of GNRI
2.4. Statistical Analysis
2.5. Ethics Approval
3. Results
3.1. Differences in Baseline Characteristics Between the Two Patient Groups
3.2. Differences in Postoperative Outcomes Between Patients with and Without Nutritional Risk
3.3. Multivariate Regression Analysis of Postoperative Outcomes
4. Discussion
4.1. The Prevalence of Nutritional Risk Is High Among Older Patients with Prostate Cancer
4.2. Mechanistic Links Between Nutritional Risk and Postoperative Complications
4.3. Nutritional Risk and Healthcare Resource Utilization
4.4. Clinical Implications and Implementation Strategies
4.5. Study Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lowrance, W.; Dreicer, R.; Jarrard, D.F.; Scarpato, K.R.; Kim, S.K.; Kirkby, E.; Buckley, D.I.; Griffin, J.C.; Cookson, M.S. Updates to Advanced Prostate Cancer: AUA/SUO Guideline (2023). J. Urol. 2023, 209, 1082–1090. [Google Scholar] [CrossRef]
- Culp, M.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent global patterns in prostate cancer incidence and mortality rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef]
- Brinkers, M.; Pfau, G.; Schilling, T.; Meyer, F. Risiken perioperativer Benzodiazepin-Abhängigkeit beim alten Menschen—was der Chirurg hierzu wissen sollte. Zentralblatt Chir. 2016, 141, 75–81. [Google Scholar] [CrossRef]
- Mori, Y.; Tarasawa, K.; Tanaka, H.; Mori, N.; Fushimi, K.; Aizawa, T.; Fujimori, K. Nationwide database study of postoperative sequelae and in-hospital mortality in super-elderly hip fracture patients. J. Bone Miner. Metab. 2025, 43, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.L.; Zhang, D.; Zhang, K.Y.; Yan, T.; Qiang, W.-S.; Zhang, T.; Zhang, B.-F. The association between admission serum albumin and preoperative deep venous thrombosis in geriatrics hip fracture: A retrospective study. BMC Musculoskelet. Disord. 2023, 24, 672. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.N.; Kufeldt, J.; Kisser, U.; Hornung, H.-M.; Hoffmann, J.; Andraschko, M.; Werner, J.; Rittler, P. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition 2016, 32, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Xu, X.; Gong, H.; Chen, R.; Guan, L.; Yan, X.; Zhou, L.; Yang, Y.; Wang, J.; Zhou, J.; et al. Global epidemiological features and impact of osteosarcopenia: Acomprehensive meta-analysis and systematic review. J. Cachexia Sarcopenia Muscle 2024, 15, 8–20. [Google Scholar] [CrossRef]
- Cusack, B.; Buggy, D.J. Anaesthesia, analgesia, and the surgical stress response. BJA Educ. 2020, 20, 321–328. [Google Scholar] [CrossRef]
- Fukuta, K.; Daizumoto, K.; Sasaki, Y.; Izumi, K.; Kadoriku, F.; Utsunomiya, S.; Shiozaki, K.; Nakashima, T.; Fukawa, T.; Nakanishi, R.; et al. Geriatric Nutritional Risk Index Predicts Postoperative Complications in Elderly Patients Undergoing Robot-Assisted Radical Cystectomy. Int. J. Urol. 2025, 32, 944–950. [Google Scholar] [CrossRef]
- Subwongcharoen, S.; Areesawangvong, P.; Chompoosaeng, T. Impact of nutritional status on surgical patients. Clin. Nutr. ESPEN 2019, 32, 135–139. [Google Scholar] [CrossRef]
- Yoon, S.; Ko, N.G.; Lee, Y.J. Geriatric nutritional risk index as a possible predictor of decline in kidney function in older people. Ann. Geriatr. Med. Res. 2024, 28, 164. [Google Scholar] [CrossRef]
- Pellegrinelli, A.; Mancin, S.; Brolese, A.; Marcucci, S.; Roat, O.; Morenghi, E.; Morales Palomares, S.; Cattani, D.; Lopane, D.; Dacomi, A.; et al. Impact of Preoperative Malnutrition on Patients with Pancreatic Neoplasms Post-Duodenopancreatectomy: A Retrospective Cohort Study. Nutrients 2024, 16, 1839. [Google Scholar] [CrossRef] [PubMed]
- Karanikki, E.; Frountzas, M.; Lidoriki, I.; Kozadinos, A.; Mylonakis, A.; Tsikrikou, I.; Kyriakidou, M.; Toutouza, O.; Koniaris, E.; Theodoropoulos, G.E.; et al. The Predictive Role of Preoperative Malnutrition Assessment in Postoperative Outcomes of Patients Undergoing Surgery Due to Gastrointestinal Cancer: A Cross-Sectional Observational Study. J. Clin. Med. 2024, 13, 7479. [Google Scholar] [CrossRef] [PubMed]
- Hori, T.; Makino, T.; Fujimura, R.; Takimoto, A.; Urata, S.; Miyagi, T. Favorable impact on postoperative abdominal symptoms in robot-assisted radical prostatectomy using enhanced recovery after surgery protocol. Cancer Diagn. Progn. 2022, 2, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Bignante, G.; Orsini, A.; Lasorsa, F.; Lambertini, L.; Pacini, M.; Amparore, D.; Pandolfo, S.D.; Del Giudice, F.; Zaytoun, O.; Buscarini, M.; et al. Robotic-assisted surgery for the treatment of urologic cancers: Recent advances. Expert Rev. Med. Devices 2024, 21, 1165–1177. [Google Scholar] [CrossRef]
- Liao, C.K.; Chern, Y.J.; Hsu, Y.J.; Lin, Y.C.; Yu, Y.L.; Chiang, J.M.; Yeh, C.Y.; You, J.F. The clinical utility of the Geriatric Nutritional Risk Index in predicting postoperative complications and long-term survival in elderly patients with colorectal cancer after curative surgery. Cancers 2021, 13, 5852. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, L.; Jin, Q.; He, Y.; Wu, M.; Peng, H.; Li, Y. The prognostic value of the GNRI in patients with stomach cancer undergoing surgery. J. Pers. Med. 2023, 13, 155. [Google Scholar] [CrossRef]
- Tsukagoshi, M.; Araki, K.; Igarashi, T.; Ishii, N.; Kawai, S.; Hagiwara, K.; Hoshino, K.; Seki, T.; Okuyama, T.; Fukushima, R.; et al. Lower Geriatric Nutritional Risk Index and Prognostic Nutritional Index Predict Postoperative Prognosis in Patients with Hepatocellular Carcinoma. Nutrients 2024, 16, 940. [Google Scholar] [CrossRef]
- Naiki, T.; Takahara, K.; Watanabe, H.; Nakane, K.; Sugiyama, Y.; Koie, T.; Shiroki, R.; Miyake, H.; Yasui, T. The Geriatric Nutritional Risk Index predicts prognosis in Japanese patients with LATITUDE high-risk metastatic hormone-sensitive prostate cancer: A multi-center study. Cancers 2023, 15, 5333. [Google Scholar] [CrossRef]
- Shu, W.; Tao, W.; Chunyan, H.; Jie, F.; Yuan, L.; Yan, X.; Huan, Z.; Liang, X. Preoperative nutritional evaluation of prostate cancer patients undergoing laparoscopic radical prostatectomy. PLoS ONE 2022, 17, e0262630. [Google Scholar] [CrossRef]
- Calcaterra, L.; van Kan, G.A.; Steinmeyer, Z.; Angioni, D.; Proietti, M.; Sourdet, S. Sarcopenia and poor nutritional status in older adults. Clin. Nutr. 2024, 43, 701–707. [Google Scholar] [CrossRef]
- Palmer, A.K.; Jensen, M.D. Metabolic changes in aging humans: Current evidence and therapeutic strategies. J. Clin. Investig. 2022, 132, e158451. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Pyun, W.Y.; Park, H.W. Cancer metabolism: Phenotype, signaling and therapeutic targets. Cells 2020, 9, 2308. [Google Scholar] [CrossRef] [PubMed]
- Bologna, E.; Ditonno, F.; Licari, L.C.; Franco, A.; Manfredi, C.; Mossack, S.; Pandolfo, S.D.; De Nunzio, C.; Simone, G.; Leonardo, C.; et al. Tissue-Based Genomic Testing in Prostate Cancer: 10-Year Analysis of National Trends on the Use of Prolaris, Decipher, ProMark, and Oncotype DX. Clin. Pract. 2024, 14, 508–520. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- García-Montero, C.; Fraile-Martínez, O.; Gómez-Lahoz, A.M.; Pekarek, L.; Castellanos, A.J.; Noguerales-Fraguas, F.; Coca, S.; Guijarro, L.G.; García-Honduvilla, N.; Asúnsolo, A.; et al. Nutritional components in Western diet versus Mediterranean diet at the gut microbiota–Immune system interplay. Nutrients 2021, 13, 699. [Google Scholar] [CrossRef]
- Song, Y.X.; Wang, Q.; Ma, Y.L.; Chen, K.S.; Liu, M.; Zhou, X.F.; Zhao, H.; Lou, J.S.; Li, H.; Liu, Y.H.; et al. Preoperative prognostic nutritional index predicts postoperative delirium in aged patients after surgery: A matched cohort study. Gen. Hosp. Psychiatry 2024, 86, 58–66. [Google Scholar] [CrossRef]
- Maldonado, J.R. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. Int. J. Geriatr. Psychiatry 2018, 33, 1428–1457. [Google Scholar] [CrossRef]
- Takano, Y.; Kobayashi, Y.; Kudo, T.; Takahashi, S.; Kanno, H.; Hanyu, N. The role of Geriatric Nutritional Risk Index as a predictor for postoperative outcomes in gastrointestinal emergencies. World J. Surg. 2024, 48, 40–47. [Google Scholar] [CrossRef]
- Zenilman, M.E. Invited commentary: A new pathway for our elderly patients. J. Am. Coll. Surg. 2023, 237, 181–182. [Google Scholar] [CrossRef]
- Tessema, T.T.; Alamdo, A.G.; Yirtaw, T.G.; Deble, F.A.; Mekonen, E.B.; Abessa, T.G.; Lema, T.B. The effects of psychosocial stimulation on the development, growth, 436 and treatment outcome of children with severe acute malnutrition age 6–59 months in southern Ethiopia: A parallel group cluster randomized control trial (EPSoSAMC study). BMC Public Health 2019, 19, 1610. [Google Scholar] [CrossRef]
- Gebregziabher, Z.; Nane, D.; Dake, S.K.; Handiso, Y.H. Effect of malnutrition at admission on length of hospital stay among adult surgical patients in Wolaita Sodo University Comprehensive Specialized Hospital, South Ethiopia: Prospective cohort study. Front. Nutr. 2024, 11, 1451463. [Google Scholar] [CrossRef]
- de Camargo, J.B.B. Protein supplementation in addition to strength training programs for improving body composition in older adults: What else is left to know? A brief update review of the current evidence. J. Aging Phys. Act. 2023, 31, 866–877. [Google Scholar] [CrossRef]
- Yee, S.L.; Schmidt, R.C.; Satalich, J.; Krumme, J.; Golladay, G.J.; Patel, N.K. Improved outcomes with perioperative dietitian-led interventions in patients undergoing total joint arthroplasty: A systematic review. J. Orthop. 2024, 56, 12–17. [Google Scholar] [CrossRef]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.G.; et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin. Nutr. 2021, 40, 4745–4761. [Google Scholar] [CrossRef]
- Lester, P.E.; Ripley, D.; Grandelli, R.; Drew, L.A.; Keegan, M.; Islam, S. Interdisciplinary Protocol for Surgery in Older Persons: Development and Implementation. J. Am. Med. Dir. Assoc. 2022, 23, 555–562. [Google Scholar] [CrossRef]
- Gumuskaya, O.; Skendri, S.; Birkenhead, K.; Sarkies, M.N. Perioperative nutrition in older patients: What are the priorities? Curr. Opin. Clin. Nutr. Metab. Care 2025, 28, 6–13. [Google Scholar] [CrossRef]
- Kim, C.-H.; Lee, B.-R.; Park, J.-S.; Kim, J.-B.; Kwon, S.-W.; Kim, W.-J.; Jung, K.-J.; Jang, B.-W.; Hong, C.-H. Efficacy of Postoperative Oral Nutritional Supplements in Geriatric Hip Fracture Patients Undergoing Total Hip Arthroplasty. J. Clin. Med. 2024, 13, 5580. [Google Scholar] [CrossRef]


| Variable | Category | Frequency/ Mean (Total) | Nutritional Risk | χ2/t | p | |
|---|---|---|---|---|---|---|
| NNg (n = 172) | MNg (n = 92) | |||||
| Age (years) | 71.7 ± 4.5 | 70.8 ± 4.0 | 73.6 ± 4.8 | 5.002 b | 0.018 | |
| Education | Primary school and below | 97 | 62 | 35 | 0. 108 a | 0.948 |
| Smoking | High school | 109 | 72 | 37 | ||
| University degree | 58 | 38 | 20 | |||
| No | 172 | 112 | 60 | 0.000 a | 0.987 | |
| Yes | 92 | 60 | 32 | |||
| Alcohol consumption | No Yes | 202 62 | 130 42 | 72 20 | 0.239 a | 0.625 |
| Sleep | Normal Abnormal | 171 93 | 117 55 | 54 38 | 2.286 a | 0.131 |
| Comorbidity | No Yes | 143 121 | 95 77 | 48 44 | 0.226 a | 0.635 |
| Polypharmacy | No Yes | 213 51 | 150 22 | 63 29 | 13.49 a | 0.001 |
| ASA | II | 99 | 76 | 23 | 2.278 a | 0.131 |
| III | 165 | 96 | 69 | |||
| <150 | 6 | 1 | 5 | |||
| Prealbumin (mg/L) | ≥150 | 258 | 171 | 87 | 6.357 a | 0.012 |
| Hb (g) | <120 ≥120 | 39 225 | 18 154 | 21 71 | 7.274 a | 0.007 |
| White blood cell count | <3.5 | 8 | 4 | 4 | ||
| (×109 g/L) | 3.5–9.5 | 208 | 137 | 71 | 0.862 a | 0.650 |
| >9.5 | 48 | 31 | 17 | |||
| Lymphocyte count | <1.1 | 71 | 41 | 30 | ||
| 1.1–3.2 | 189 | 129 | 60 | 2.920 a | 0.232 | |
| (×109 g/L) | >3.2 | 2 | 2 | 2 | ||
| <125 | 13 | 6 | 7 | |||
| Platelet count (×109 g/L) | 125–135 >135 | 13 238 | 8 158 | 5 80 | 2.301 a | 0.316 |
| Operation duration (min) | 143.36 ± 10.99 | 142.86 ± 11.17 | 144.30 ± 10.63 | −1.017 b | 0.310 | |
| Outcome Variable | Category | Nutritional Risk | χ2 | p | |
|---|---|---|---|---|---|
| NNg (n = 172) | MNg (n = 92) | ||||
| Postoperative complications | NO YES | 138 34 | 45 47 | 27.65 | <0.001 |
| Hospital stays (days) | <9 ≥9 | 96 76 | 18 74 | 32.10 | <0.001 |
| Hospitalization costs (CNY) | ≤52,361.5 >52,361.5 | 113 59 | 22 70 | 41.882 | <0.001 |
| Group | Postoperative Complications | ||||
|---|---|---|---|---|---|
| Delirium | DVT | T ≥ 38.5 °C | Incomplete Intestinal Obstruction | Poor Wound Healing | |
| MNg (n = 92) | 25 (27.17%) | 11 (11.96%) | 19 (20.65%) | 7 (7.61%) | 5 (5.43%) |
| NNg (n = 172) | 29 (16.9%) | 1 (0.58%) | 18 (10.47%) | 4 (2.33%) | 2 (1.16%) |
| χ2 | 3.918 | 17.875 | 5.162 | 4.190 | 4.238 |
| p | =0.048 | <0.001 | =0.023 | =0.041 | =0.040 |
| Variable | Category | B | S.E | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Comorbidity ASA | No Yes II III | 1.382 3.404 | 0.420 0.667 | 0.001 <0.001 | 1 3.982 1 30.086 | 1.746~9.078 8.138~ 111.225 |
| Hb (g) | <150 ≥150 | −1.176 | 0.529 | 0.026 | 1 0.308 | 0.109~0.871 |
| Nutritional risk | NO YES | 1.050 | 0.388 | 0.007 | 1 2.859 | 1.335~6.121 |
| Variable | Category | B | S.E | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Nutritional risk | NO YES | 1.543 | 0.331 | <0.001 | 1 4.678 | 2.443~8.955 |
| Comorbidity | NO Yes | 0.649 | 0.315 | 0.040 | 1 1.914 | 1.032~3.551 |
| Variable | Category | B | S.E | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Comorbidity | NO Yes | 1.111 | 0.330 | 0.001 | 1 3.037 | 1.590~5.800 |
| Nutritional risk | NO YES | 1.583 | 0.330 | <0.001 | 1 4.867 | 2.547~9.301 |
| ASA | II III | 1.217 | 0.299 | <0.001 | 1 3.377 | 1.878~6.073 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, R.; Zhou, Y.; Yue, X.; Wang, M.; Zhang, Y.; Liu, C. The Prognostic Implications of the Geriatric Nutritional Risk Index in Patients with Prostate Cancer: A Single-Center Retrospective Cohort Study. Healthcare 2025, 13, 3266. https://doi.org/10.3390/healthcare13243266
Zhou R, Zhou Y, Yue X, Wang M, Zhang Y, Liu C. The Prognostic Implications of the Geriatric Nutritional Risk Index in Patients with Prostate Cancer: A Single-Center Retrospective Cohort Study. Healthcare. 2025; 13(24):3266. https://doi.org/10.3390/healthcare13243266
Chicago/Turabian StyleZhou, Rong, Yanqiong Zhou, Xiao Yue, Mei Wang, Yucong Zhang, and Chang Liu. 2025. "The Prognostic Implications of the Geriatric Nutritional Risk Index in Patients with Prostate Cancer: A Single-Center Retrospective Cohort Study" Healthcare 13, no. 24: 3266. https://doi.org/10.3390/healthcare13243266
APA StyleZhou, R., Zhou, Y., Yue, X., Wang, M., Zhang, Y., & Liu, C. (2025). The Prognostic Implications of the Geriatric Nutritional Risk Index in Patients with Prostate Cancer: A Single-Center Retrospective Cohort Study. Healthcare, 13(24), 3266. https://doi.org/10.3390/healthcare13243266






